Abstract
Background
Depression is associated with substance use problems; however, the specific individual characteristics influencing this association are not well identified. Empirical evidence and theory suggest that gender and distress tolerance—defined behaviorally as an individual’s ability to persist in goal-directed behavior while experiencing negative affective states—are important underlying factors in this relationship. Hence, the purpose of the current study was to examine whether gender and distress tolerance moderate the relationship between depressive symptoms and substance use problems.
Methods
Participants included 189 substance users recruited from a residential substance abuse treatment center. The Short Inventory of Problems-Alcohol and Drugs scale was used to measure self-reported substance use problems. The Beck Depression Inventory was used to assess self-reported depressive symptoms. Gender was self-reported, and distress tolerance was behaviorally indexed by the Computerized Paced Auditory Serial Addition Task.
Results
Hierarchical linear regression analysis indicated a significant three-way interaction of depressive symptoms, gender, and distress tolerance on substance use problems, adjusting for relevant demographic variables, anxiety symptoms, impulsivity, as well as DSM-IV psychiatric disorders. Probing of this three-way interaction demonstrated a significant positive association between depressive symptoms and substance use problems among females with low distress tolerance.
Conclusion
Findings indicate that female treatment-seeking substance users with high levels of depressive symptoms exhibit greater substance use problems if they also evidence low distress tolerance. Study implications are discussed, including the development of prevention and intervention programs that target distress tolerance skills.
Keywords: Substance Abuse, Negative Affect, Depression, Inpatient Treatment
1. INTRODUCTION
A large proportion of the United States population engages in substance use, and heavy use of substances is especially a concern for African American adults (Substance Abuse and Mental Health Services Administration [SAMHSA], 2012). Indeed, 13.7% of African American males and 5.5% of African American females meet criteria for past year substance abuse or dependence. Importantly, among substance users in both community (Gillespie et al., 2007; Hagman et al., 2009) and clinical (Alterman et al., 2009; Bender et al., 2007) settings, heavy use of substances is associated with increased substance use problems (SUP), defined hereafter as negative physical (e.g., poor eating habits, declining physical health), psychological (e.g., mood changes, feelings of guilt), and social (e.g., damaged relationships and social life) consequences of substance use (Blanchard et al., 2003; Gillespie et al., 2007; Newcomb and Locke, 2005; Office of National Drug Control Policy, 2004). Substance use problems are a particular concern among African American substance users receiving treatment, who also evidence high rates of comorbid psychopathology (Chen et al., 2011). Previous study shows that elevated SUP are associated with poor treatment retention, even after accounting for clients’ drug and alcohol severity and their readiness to change (Kiluk et al., 2013), highlighting the need to investigate the underlying factors and conditions related to SUP in this at-risk group.
One risk factor for SUP is elevated depressive symptoms. In addition to prospective studies indicating that depression significantly predicts the development and maintenance of substance use (King et al., 2004; Worley et al., 2012), cross-sectional studies demonstrate that depressive symptoms relate to greater alcohol use problems (Buckner et al., 2007; Gorka et al., 2012) and marijuana use problems (Buckner et al., 2007). Importantly, gender is associated with both depression and SUP among substance users. Female substance users in residential treatment have higher rates of comorbid depression and anxiety disorders than males (e.g., Zilberman et al., 2003), and they evidence significantly higher levels of SUP than their male counterparts (Kiluk et al., 2013).
A theoretical perspective that may be appropriate when examining differences in vulnerability for SUP among depressed substance users is the negative reinforcement model. The negative reinforcement model is extensively utilized in the substance use literature to understand the initiation and maintenance of substance use (Baker et al., 2004; review in Magidson et al., 2013). According to this theoretical model, the primary motivational basis for substance use is the reduction or avoidance of negative affective states, such as feelings of irritability, anxiety, and stress (Baker et al., 2004). The negative reinforcement model has also been extended to understand the occurrence of SUP (Ali et al., 2012; Gorka et al., 2012). For instance, individuals may engage in problematic behavior that aids in reducing negative affect either directly (e.g., risky sexual behavior, getting in fights), or indirectly (e.g., engaging in illegal activity to obtain substances). A commonly used method of assessing the propensity to engage in behaviors motivated by negative reinforcement is measuring an individual’s distress tolerance, defined behaviorally as the ability to persist in goal-directed activity while experiencing negative affective states (Daughters et al., 2005a).
Previous studies consistently find a significant relation between low distress tolerance and adverse substance use outcomes (Abrantes et al., 2008; Brown et al., 2002, 2009; Daughters et al., 2005a, 2005b), including higher levels of SUP (Buckner et al., 2007; Bujarski et al., 2012; Howell et al., 2010; Simons and Gaher, 2005). Further, among community adults with low distress tolerance, depressive symptoms are significantly associated with alcohol use problems (Gorka et al., 2012). However, the interacting effect of distress tolerance with depressive symptoms and gender on SUP has yet to be examined in vulnerable clinical populations, such as African American treatment-seeking substance users. Therefore, the current study aims to examine the role of gender and distress tolerance in the relation between depressive symptoms and SUP among African American substance users in a residential substance abuse treatment center. Given the aforementioned empirical evidence, it was hypothesized that the relation of depressive symptoms to SUP will vary as a function of gender and distress tolerance, with greater depressive symptoms relating to increased SUP specifically among females with low distress tolerance.
2. METHODS
2.1. Participants
A total of 189 participants (67.20% males) were recruited from a residential substance abuse treatment facility in Washington, DC. Treatment at this facility lasts between 30 and 180 days, and includes programs incorporating strategies from Alcoholics Anonymous and Narcotics Anonymous, as well as group sessions focusing on relapse prevention. Participants were recruited during their first week of treatment. The current study utilized baseline data collected for an ongoing longitudinal study that aims to assess the long-term impact of a clinical intervention to improve substance use outcomes. Eligibility criteria for the study included: 1) minimum of 18 years of age, 2) the ability to speak and read English sufficiently to complete study procedures, and 3) no current psychotic symptoms, as these symptoms may affect responses on the self-report measures and performance on the behavioral task assessing distress tolerance.
2.2. Procedure
All participants completed a screening interview administered by trained doctoral level graduate students or senior research staff during the first week of treatment. The interview consisted of the Structured Clinical Interview for DSM-IV (SCID-IV; First et al., 1995) SCID-IV to assess mood disorders, anxiety disorders, psychotic symptoms, substance use disorders, borderline personality and antisocial personality disorders, as well as the Beck Depression Inventory (Beck et al., 1996). Following the interview, participants were invited to participate in research. Eligible participants were provided with a verbal description of the study, and interested participants provided written informed consent. Participants then completed a battery of self-report measures and a computerized behavioral distress tolerance task. The study protocol was reviewed and approved by the University Institutional Review Board.
2.3. Measures
2.3.1. Substance Use Problems (SUP)
The dependent variable, SUP, was assessed using a 15-item self-report measure, the Short Inventory of Problems - Alcohol and Drugs (SIP-AD; Blanchard et al., 2003). This measure captures consequences of multiple drugs, including alcohol, across five domains: interpersonal (e.g., “My family has been hurt by my drinking or drug use”), intrapersonal (e.g., “I have been unhappy because of my drinking or drug use”), physical (e.g., “My physical health has been harmed by my drinking or drug use”), impulse control (e.g., “I have taken foolish risks when I have been drinking or using drugs”), and social (e.g., “I have failed to do what is expected of me because of my drinking or drug use”). Participants indicated how often each of the listed consequences occurred during the past 12 months due to their alcohol and drug use, responding on a scale ranging from 0–3 (“never,” “once or a few times,” “once or twice a week,” and “daily or almost daily”). The sum of the items provided the total score. The SIP-AD has demonstrated excellent psychometric properties in previous studies (Blanchard et al., 2003; Kiluk et al., 2013), as well as good internal consistency in the current study (α = 0.96).
2.3.2. Depressive Symptoms
The primary independent variable, depressive symptoms, was determined using the 21-item self-report measure, the Beck Depression Inventory (BDI-II; Beck et al., 1996). Participants reported on the level of a variety of symptoms in the past week, including “sadness” and “loss of pleasure.” The sum of the items was used as the total score, and a higher score indicated greater depressive symptoms. The instrument has shown excellent psychometric properties in previous studies (Beck et al., 1996; Sprinkle et al., 2002), and good internal consistency in this study (α = 0.93).
2.3.3. Distress Tolerance
Distress tolerance was measured using the Computerized Paced Auditory Serial Addition Task (PASAT-C; Lejuez et al., 2003). The PASAT-C has been shown to reliably increase participant distress levels and has repeatedly been used as a behavioral measure of distress tolerance (Daughters et al., 2005a, 2009, 2008). In sum, participants are exposed to an increasingly difficult working memory task, accompanied by forced failure and negative auditory feedback. There are three levels in this task. Participants are given the option to quit the task on the final and most difficult level (i.e., low distress tolerance) or to persist for the entire duration for an undefined reward (i.e., high distress tolerance). The reader is referred to Daughters et al. (2005a) for a detailed description of the task.
2.3.4. Demographics
Participants self-reported their gender, age, race, marital status, income, and level of education.
2.3.5. Other Potential Covariates
Other potential covariates included psychiatric comorbidity and self-reported anxiety symptoms and impulsivity. The Structured Clinical Interview for the DSM-IV was used to assess for current Axis I disorders and Axis II disorders (SCID-IV; First et al., 1995). The following Axis I disorders were assessed: bipolar I, psychotic symptoms, panic disorder, social phobia, obsessive compulsive disorder, posttraumatic stress disorder, generalized anxiety disorder, and substance dependence. Diagnoses were only given when the disorder was not substance-induced or not due to a general medical condition. Axis II disorders that were assessed included borderline personality disorder and antisocial personality disorder. These Axis II disorders were selected for assessment since they are particularly prevalent among substance users (Kokkevi et al., 1998; Torrens et al., 2011). All SCID-IV interviewers underwent extensive training supervised by clinical psychology faculty prior to conducting independent interviews. The training certification process included viewing the complete video protocol for SCID-IV (First et al., 1995), observing two full interviews and conducting mock interviews with certified interviewers, conducting a final certification practice interview, and being observed while conducting two interviews with clients at the substance use treatment center. Interviewers also participated in weekly SCID-IV supervision throughout the duration of the study.
Self-reported anxiety symptoms and impulsivity were also examined given their association with SUP (Marmorstein et al., 2010; Petry, 2001; Stoltenberg et al., 2011). Anxiety symptoms were measured using the Beck Anxiety Inventory (BAI; Beck et al., 1988). Responses on this 21-item measure were obtained on a scale of 0–3, ranging from “not at all” to “severely.” The sum of the items was used as the total score, and higher score indicated increased anxiety symptoms. This instrument has shown good psychometric properties in previous studies (Steer and Beck, 1997; Fydrich et al., 1992), and excellent internal consistency in this study (α = 0.95). Impulsivity was assessed using the Eysenck Impulsiveness Scale (EIS; Eysenck et al., 1985). In this 19-item measure, participants were asked to respond yes/no to each item. Total score ranged from 0 to 19 with higher score indicating lower impulsivity. This impulsivity measure possesses good psychometric properties (Eysenck and Eysenck, 1978) and provided acceptable internal consistency in this study (α = 0.81).
2.4. Data Analysis Plan
All continuous data were first assessed for normality. Potential covariates, including demographic variables, psychiatric diagnoses, anxiety symptoms, and impulsivity were examined for associations with SUP. The main and interactive effects of depressive symptoms, gender, and distress tolerance on SUP were examined using hierarchical linear regression. Analyses examining the interactive effects are limited to depressive symptoms (i.e., BDI score) due to the small sample size of male (n = 1) and female (n = 1) participants who met both criteria for major depressive disorder and demonstrated low distress tolerance. Probing of the three-way interaction was conducted using the PROCESS macro for SPSS (Hayes, 2012), a regression-based path analysis macro. All analyses were conducted using SPSS version 21.
3. Results
3.1. Study Descriptive Data
The majority of the sample was male (67.20%) and African American (95.80%), with the mean age of 42.96 years (SD = 11.72). Nearly half reported being a high school graduate or receiving their GED (49.20%); a quarter obtained less than a high school education (24.90%) and the remainder of the sample (25.90%) pursued education beyond high school. Descriptive data for other study variables are presented in Table 1.
Table 1.
Descriptive data of the study variables by gender.
| Variable | % / Mean (SD) | ||
|---|---|---|---|
| All (N=189) | Males (n=127) | Females (n=62) | |
| Current Bipolar I Disorder | 3.20% | 1.60% | 6.50% |
| Current Psychotic Symptoms | 5.30% | 5.50% | 4.80% |
| Current Obsessive-Compulsive Disorder | 0.50% | 0.00% | 1.60% |
| Current Posttraumatic Stress Disorder | 6.90% | 4.70% | 11.30% |
| Current Panic Disorder* | 2.10% | 0.00% | 6.50% |
| Current Social Phobia | 4.20% | 4.70% | 3.20% |
| Current Generalized Anxiety Disorder | 10.10% | 7.90% | 14.50% |
| Current Alcohol Dependence | 32.30% | 29.90% | 37.10% |
| Current Sedative Dependence | 1.10% | 0.00% | 3.20% |
| Current Cannabis Dependence | 11.60% | 15.00% | 4.80% |
| Current Stimulant Dependence | 0.00% | 0.00% | 0.00% |
| Current Opioid Dependence | 10.60% | 10.20% | 11.30% |
| Current Cocaine Dependence** | 32.30% | 24.40% | 48.40% |
| Current Hallucinogen Dependence* | 13.80% | 9.40% | 22.60% |
| Current Borderline Personality Disorder* | 8.50% | 4.70% | 16.10% |
| Current Antisocial Personality Disorder | 31.20% | 34.60% | 24.20% |
| PASAT-C quit | 21.20% | 18.10% | 27.40% |
| BDI Depressive Symptoms | 10.35 | 9.52 | 12.06 |
| (SD = 10.16) | (SD = 9.92) | (SD = 10.50) | |
| BAI Anxiety Symptoms* | 9.17 | 7.92 | 11.73 |
| (SD = 12.14) | (SD = 11.47) | (SD = 13.14) | |
| Eysenck Impulsivity* | 9.37 | 9.86 | 8.35 |
| (SD = 4.39) | (SD = 4.47) | (SD = 4.08) | |
| SIP Total Score | 23.72 | 22.88 | 25.45 |
| (SD = 13.77) | (SD = 14.00) | (SD = 13.23) | |
p < .05,
p < .01
3.2 Depressive Symptoms
As shown in Table 1, the mean BDI total score was 10.35 (SD = 10.16). BDI total score did not vary by gender [F(1,187) = 2.64, p > 0.05]. One-way ANOVA and Pearson’s correlation showed that higher levels of SIP total score was significantly related to a higher BDI total score (r = 0.46, p < 0.001).
3.3. Distress Tolerance
Participants persisted on the PASAT-C for an average of 357.44 seconds (SD = 136.50) and 21.20% (n = 40) quit the task before the 7 minutes expired. As shown in Table 1, 18.10% of males and 27.40% of females quit the PASAT-C prior to task termination [χ2(1) = 2.16, p > 0.05]. A paired t-test indicated that there was a significant increase in negative affect during the PASAT-C [t(188) = −3.23, p < 0.01], suggesting that the task successfully induced distress. Skill on the PASAT-C was indexed by the latency between number presentations (M = 4.53, SD = 0.58). T-test analyses showed that there was no significant relationship between skill on the PASAT-C and distress tolerance [t(187) = −0.19, p > 0.05] nor a significant relationship between baseline negative affect and distress tolerance [t(187) = 0.03, p > 0.05]. In addition, a repeated measures analysis indicated that the change from baseline to experimental negative affect was not related to distress tolerance [F(1,187) = 1.59, p > 0.05]. These findings indicate that distress tolerance was not related to skill on the task or task-induced changes in negative affect.
3.4. Identification of Covariates
Results from Pearson’s correlations showed that higher SIP total score was significantly correlated with older age (r = 0.31, p < 0.001), lower income (r = −0.22, p < 0.01), increased BAI total score (r = 0.38, p < 0.001), and increased EIS total score (r = −0.32, p < 0.001). A series of one-way ANOVAs examined the relationship of SUP with demographics and psychiatric disorders. Higher SIP total score was significantly related to posttraumatic stress disorder [F(1,187) = 13.87, p < 0.001], generalized anxiety disorder [F(1,187) = 13.46, p < 0.001], alcohol dependence [F(1,187) = 16.02, p < 0.001], cannabis dependence [F(1,187) = 4.97, p < 0.05], cocaine dependence [F(1,187) = 14.06, p < 0.001], and antisocial personality disorder [F(1,187) = 3.92, p < 0.05]. These significant covariates were included in subsequent analyses.
3.5. Depressive Symptoms, Gender, Distress Tolerance and SUP
The unique and interactive effects of gender and distress tolerance on the relation between depressive symptoms and SUP were examined using hierarchical linear regression analysis. The BDI total score, gender, PASAT-C quit status (i.e., distress tolerance), and covariates were entered in Step 1 (ΔR2 = 0.41, p < 0.001). All possible two-way interactions were entered in Step 2 (ΔR2 = 0.00, p > 0.05), and the BDI total score x gender x PASAT-C quit status variable was entered in the third and final step. The final model provided a significant increase in the variance in SIP total score as explained by the model (ΔR2 = 0.02, p < 0.01) and showed that the three-way interaction between depressive symptoms, gender, and distress tolerance was significantly associated with SUP, controlling for covariates (b = −1.34, t = −2.62, p < 0.01). Results from this regression analysis are displayed in Table 2.
Table 2.
Linear regression examining predictors of substance use problems.
| Variable | b | SE | β | t-value | ΔR2 |
|---|---|---|---|---|---|
| Step 1: | 0.41*** | ||||
| Sex (Male) | 0.81 | 1.87 | 0.03 | 0.43 | |
| Age | 0.26 | 0.08 | 0.22 | 3.35** | |
| Income | −0.33 | 0.34 | −0.06 | −0.98 | |
| Current Posttraumatic Stress Disorder | 4.03 | 3.73 | 0.07 | 1.08 | |
| Current Generalized Anxiety Disorder | 0.55 | 3.27 | 0.01 | 0.17 | |
| Current Alcohol Dependence | 2.36 | 1.85 | 0.08 | 1.27 | |
| Current Cannabis Dependence | −6.02 | 2.77 | −0.14 | −2.17* | |
| Current Cocaine Dependence | 4.27 | 1.93 | 0.15 | 2.21* | |
| Antisocial Personality Disorder | 1.43 | 1.87 | 0.05 | 0.76 | |
| PASAT-C Quit | −2.14 | 2.01 | −0.06 | −1.07 | |
| BDI Depressive Symptoms | 0.30 | 0.11 | 0.22 | 2.84** | |
| BAI Anxiety Symptoms | 0.18 | 0.08 | 0.16 | 2.24* | |
| Eysenck Impulsivity | −0.46 | 0.21 | −0.15 | −2.15* | |
| Step 2: | 0.00 | ||||
| Gender x BDI Depressive Symptoms | 0.03 | 0.17 | 0.02 | 0.18 | |
| PASAT-C Quit x BDI Depressive Symptoms | −0.06 | 0.24 | −0.02 | −0.25 | |
| Gender x PASAT-C Quit | −2.62 | 4.33 | −0.06 | −0.61 | |
| Step 3: | 0.02** | ||||
| Gender x PASAT-C Quit x BDI Depressive Symptoms | −1.34 | 0.51 | −0.30 | −2.62** |
p < .05,
p < .01,
p < .001.
Further probing of this three-way interaction was performed using the PROCESS macro for SPSS, which allows all covariates and study variables to be entered simultaneously. Accordingly, all potential covariates found to be significantly related to SUP were included simultaneously with gender, distress tolerance, and depressive symptoms. When entering these variables, SIP total score was the dependent variable, BDI total score was the primary independent variable, and gender and PASAT-C quit status were labeled as the moderators. All other variables were considered as the covariates. The macro generated a regression model that provided the final model with simple slope effects. Simple slope analysis revealed that the conditional effect of the interaction between depressive symptoms and distress tolerance was significant for females (b = 0.81, t = 1.99, p < 0.05), but not for males (b = −0.53, t = −1.79, p > 0.05). Specifically, the conditional effect of depressive symptoms on SUP was significant among females who exhibited low distress tolerance (b = 1.01, t = 2.63, p < 0.01), but not among females with high distress tolerance (b = 0.20, t = 1.29, p > 0.05). Figure 1 illustrates the relationship between depressive symptoms and SUP as a function of distress tolerance in females.
Figure 1.
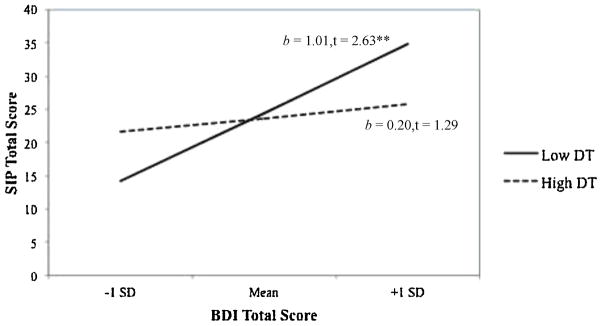
The relation between substance use problems and depressive symptoms as a function of distress tolerance among females.
Note. SIP = Short Inventory of Problems; BDI = Beck Depression Inventory; DT = Distress tolerance as indexed by PASAT-C; SD = Standard Deviation; **p < .01.
4. DISCUSSION
Substance use problems are an often overlooked, yet imperative public health issue. This issue is a greater concern among African American substance users who experience substance use disparity. The current study aimed to examine theoretically derived factors that may underlie SUP, namely the interaction of depressive symptoms, gender, and distress tolerance, in an understudied sample of minority, residential treatment-seeking substance users. Findings indicate that higher levels of depressive symptoms are significantly associated with greater SUP among females with low, but not high, distress tolerance.
To gain a better understanding of the role of gender in this relation, it is helpful to consider previous research that has demonstrated that for comorbid depression and substance use, depression is more often primary in women; whereas in men, depression is secondary to the primary substance use diagnosis (Zilberman, et al., 2003). The distinction between a primary versus secondary substance use diagnosis refers to the fact that symptoms or disorders that are secondary to substance use are unlikely to persist once an individual is abstinent from drugs or alcohol for a prolonged period. By contrast, a psychiatric disorder with onset prior to a substance use disorder that continues during periods of abstinence is considered to be an independent and primary diagnosis, requiring targeted treatment. Research shows that females in substance use treatment who use alcohol are more likely to experience depression prior to developing alcohol disorders compared to men (Zilberman et al., 2003). Further support for higher primary depression in female substance users comes from gender differences in reported motivations for using substances. Males report sensation-seeking and antisocial motivations for substance use more often, and females are more likely to attribute their substance use to environmental stressors, such as greater relationship problems and traumatic events or stressors (Kauffman et al., 1997; Lex, 1991).
Also in the current study, distress tolerance emerges as a risk factor that may maintain psychopathology and SUP among female substance users. Distress tolerance is highlighted as an important component of emotion regulation (Leyro et al., 2010), with previous studies consistently finding a significant relation between low distress tolerance and adverse substance use outcomes (Abrantes et al., 2008; Brown et al., 2002; 2009; Daughters et al., 2005a, 2005b), including increased alcohol and marijuana use problems (Buckner et al., 2007; Bujarski et al., 2012; Howell et al., 2010; Simons and Gaher, 2005). The findings of the study support research on gender differences with regard to negative reinforcement processes. Previous work indicates that female substance users report greater negative emotionality, such as stress reaction and alienation (Lejuez et al., 2007), and experience greater SUP (Kiluk et al., 2013) than their male substance users. Combined with the finding that higher levels of motivation to use substances as a coping mechanism in women are associated with greater SUP (Bujarski et al., 2012), the results of the current study are in line with research on gender differences in negative reinforcement processes.
Taken together, among depressed female substance users, primary depression may motivate substance use as a means of reducing negative affect. However, substance use only provides temporary relief from negative affective states, and does not address the high levels of punishment and low levels of positive reinforcement, which are characteristic of the environments for individuals with elevated depressive symptoms (Kauffman et al., 1997). Given the tendency to engage in negative reinforcement behavior, depressed females with low distress tolerance may be more likely to engage in additional problematic behaviors to obtain substances or directly reduce negative affective states, such as neglecting responsibilities at home or at work and engaging in risky sexual behavior.
4.1. Limitations
The findings in the current study should be considered along with several limitations. The study’s cross-sectional design limits the ability to infer causality or to establish temporal links between depressive symptoms, distress tolerance, and SUP. Future work should utilize a longitudinal design to examine the interacting role of depressive symptoms, gender, and distress tolerance in the development of SUP. This study also did not assess the onset of SUP versus depressive symptoms; hence, we were unable to determine whether our sample exhibited a gender difference with greater primary depression in females. Moreover, the study was not powered to detect this relation for major depressive disorder. As such, future research is encouraged to replicate this finding in a sample with higher rates of major depressive disorder. In addition, the study sample evidenced high rates of psychiatric disorders, including alcohol dependence, cocaine dependence, and antisocial personality disorder. Although this may be viewed as a strength, as it characterizes an understudied at-risk sample of urban African American treatment seeking substance users, it may be uncharacteristic of substance users in other settings. As such, replication of these findings in other samples is needed prior to generalizing our findings.
We encourage future studies to examine these relationships with greater specificity in regard to SUP, as well as accounting for additional variables that may influence distress tolerance among females. Specifically, as the study utilized a composite measure of SUP, consisting of negative physical, psychological, and social consequences of substance use, we do not answer important questions regarding the specific subtypes of substance related problematic behavior as a function of distress tolerance across depression and gender. Future studies are encouraged that help delineate what specific behaviors and consequences are most likely to occur among depressed females with low distress tolerance. Moreover, this nuanced approach may uncover specific SUPs and psychopathology more relevant to men. In addition, the current study did not account for many environmental stressors characteristic of psychopathology in this population, such as perceived discrimination and trauma (Chou et al., 2012), which may be a strong contributor to these findings.
4.2. Conclusions
To our knowledge, this study is the first to investigate the interacting role of gender and distress tolerance in the relation between depressive symptoms and SUP in a clinical residential sample of substance users. This is a significant addition to past work in this area that has focused on community or college student samples, as the SUP of clinical populations are more severe and more costly (Blanchard et al., 2003; National Drug Intelligence Center, 2011). The study underscores the importance of identifying female substance users with elevated depressive symptoms and low distress tolerance as individuals at heightened risk for experiencing greater SUP, providing a target for intervention programs to reduce SUP. Specifically, depressed females with low distress tolerance could benefit from treatment that aims to improve distress tolerance (e.g., Bornovalova et al., 2012), and increase access to alternative positive reinforcers when experiencing negative affect (e.g., Daughters et al., 2008).
References
- Abrantes AM, Strong DR, Lejuez CW, Kahler CW, Carpenter LL, Price LH, Niaura R, Brown RA. The role of negative affect in risk for early lapse among low distress tolerance smokers. Addict Behav. 2008;33:1394–1401. doi: 10.1016/j.addbeh.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali B, Ryan JS, Beck KH, Daughters SB. Trait aggression and problematic alcohol use: the moderating effect of distress tolerance. Alcohol Clin Exp Res. 2013;37:2138–2144. doi: 10.1111/acer.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alterman AI, Cacciola JS, Ivey MA, Habing B, Lynch KG. Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. J Stud Alcohol Drugs. 2009;70:304–307. doi: 10.15288/jsad.2009.70.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psych. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory—II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bender RE, Griffin ML, Gallop RJ, Weiss RD. Assessing negative consequences in patients with substance use and bipolar disorders: psychometric properties of the Short Inventory of Problems (SIP) Am J Addict. 2007;16:503–509. doi: 10.1080/10550490701641058. [DOI] [PubMed] [Google Scholar]
- Blanchard KA, Morgenstern J, Morgan TJ, Labouvie EW, Bux DA. Assessing consequences of substance use: psychometric properties of the Inventory of Drug Use Consequences. Psychol Addict Behav. 2003;17:328–331. doi: 10.1037/0893-164X.17.4.328. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Hunt ED, Lejuez CW. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug Alcohol Depend. 2012;122:70–76. doi: 10.1016/j.drugalcdep.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–185. [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Strong DR, Kahler CW, Zvolensky MJ, Carpenter LL, Niaura R, Price LH. A prospective examination of distress tolerance and early smoking lapse in self-quitters. Nicotine Tob Res. 2009;11:493–502. doi: 10.1093/ntr/ntp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J, Keough M, Schmidt N. Problematic alcohol and cannabis use among young adults: the roles of depression and discomfort and distress tolerance. Addict Behav. 2007;32:1957–1963. doi: 10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujarski SJ, Norberg MM, Copeland J. The association between distress tolerance and cannabis use-related problems: the mediating and moderating roles of coping motives and gender. Addict Behav. 2012;37:1181–1184. doi: 10.1016/j.addbeh.2012.05.014. [DOI] [PubMed] [Google Scholar]
- Chen KW, Banducci AN, Guller L, Macatee RJ, Lavelle A, Daughters SB, Lejuez CW. An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program. Drug Alcohol Depend. 2011;118:92–99. doi: 10.1016/j.drugalcdep.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou T, Asnaani A, Hofmann SG. Perception of racial discrimination and psychopathology across three U.S. ethnic minority groups. Cultur Divers Ethnic Minor Psychol. 2012;18:74–81. doi: 10.1037/a0025432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Bornovalova MA, Kahler CW, Strong DR, Brown R. Distress tolerance as a predictor of early treatment dropout in a residential substance abuse treatment facility. J Abnorm Psych. 2005a;114:729–734. doi: 10.1037/0021-843X.114.4.729. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Kahler C, Strong D, Brown R. Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment seeking substance abusers. Psychol Addict Behav. 2005b;19:208–211. doi: 10.1037/0893-164X.19.2.208. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Danielson CK, Zvolensky, Lejuez CW. Distress tolerance and early adolescent externalizing and internalizing symptoms: the moderating role of gender and ethnicity. Behav Res Ther. 2009;47:198–205. doi: 10.1016/j.brat.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Sargeant MN, Bornovalova MA, Gratz KL, Lejuez CW. The relationship between distress tolerance and antisocial personality disorder among male inner-city treatment seeking substance users. J Pers Disord. 2008;22:509–524. doi: 10.1521/pedi.2008.22.5.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck SBG, Eysenck HJ. Impulsiveness and venturesomeness: their position in a dimensional system of personality description. Psychol Rep. 1978;43:1247–1255. doi: 10.2466/pr0.1978.43.3f.1247. [DOI] [PubMed] [Google Scholar]
- Eysenck SBG, Pearson PR, Easting G, Allsopp JF. Age norms for impulsiveness, venturesomeness, and empathy in adults. Pers Indiv Differ. 1985;6:613–619. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Fydrich T, Dowdall D, Chambless DL. Reliability and validity of the Beck Anxiety Inventory. J Anxiety Disord. 1992;6:55–61. [Google Scholar]
- Gillespie W, Holt JL, Blackwell RL. Measuring outcomes of alcohol, marijuana, and cocaine use among college students: a preliminary test of the Shortened Inventory of Problems—Alcohol and Drugs (SIP-AD) J Drug Issues. 2007;37:549–567. [Google Scholar]
- Gorka SM, Ali B, Daughters SB. The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychol Addict Behav. 2012;26:621–626. doi: 10.1037/a0026386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagman BT, Kuerbis AN, Morgenstern J, Bux DA, Parsons JT, Heidinger BE. An item response theory (IRT) analysis of the Short Inventory of Problems-Alcohol and Drugs (SIP-AD) among non-treatment seeking men-who-have-sex-with-men: evidence for a shortened 10-item SIP-AD. Addict Behav. 2009;34:948–954. doi: 10.1016/j.addbeh.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A Versatile Computational Tool For Observed Variable Mediation, Moderation, And Conditional Process Modeling [White Paper] 2012 Retrieved September 2, 2013 from http://www.afhayes.com/public/process2012.pdf.
- Howell A, Leyro T, Hogan J, Buckner J, Zvolensky M. Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addict Behav. 2010;35:1144–1147. doi: 10.1016/j.addbeh.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauffman SE, Silver P, Poulin J. Gender differences in attitudes toward alcohol, tobacco, and other drugs. Soc Work. 1997;42:231–241. doi: 10.1093/sw/42.3.231. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Dreifuss JA, Weiss RD, Morgenstern J, Carroll KM. The Short Inventory of Problems - revised (SIP-R): psychometric properties within a large, diverse sample of substance use disorder treatment seekers. Psychol Addict Behav. 2013;27:307–314. doi: 10.1037/a0028445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Stefanis N, Anastasopoulou E, Kostogianni C. Personality disorders in drug abusers: prevalence and their association with AXIS I disorders as predictors of treatment retention. Addict Behav. 1998;23:841–853. [PubMed] [Google Scholar]
- Lejuez CW, Kahler CW, Brown RA. A modified computer version of the Paced Auditory Serial Addition Task (PASAT) as a laboratory-based stressor: Implications for behavioral assessment. Behav Ther. 2003;26:290–293. [Google Scholar]
- Lex BW. Gender differences and substance abuse. Adv Subst Abuse. 1991;4:225–296. [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychol Bull. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magidson JF, Ali B, Listhaus A, Daughters SB. Distress tolerance. In: MacKillop J, De Wit H, editors. Handbook of Addiction Psychopharmacology. Wiley-Blackwell; Hoboken, NJ: 2013. pp. 233–256. [Google Scholar]
- Marmorstein NR, White H, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. J Abnorm Child Psych. 2010;38:211–224. doi: 10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Drug Intelligence Center. The Economic Impact Of Illicit Drug Use On American Society. 2011 Retrieved December 18, 2013 from http://www.justice.gov/archive/ndic/pubs44/44731/44731p.pdf.
- Newcomb MD, Locke T. Health, social, and psychological consequences of drug use and abuse. In: Sloboda Z, editor. Epidemiology Of Drug Abuse. Springer Publishing Co; New York, NY: 2005. pp. 45–59. [Google Scholar]
- Office of National Drug Control Policy. Executive Office of the President (Publication No. 207303) Washington, DC: 2004. The Economic Costs Of Drug Abuse In The United States, 1992–2002. [Google Scholar]
- Petry N. Substance abuse, pathological gambling, and impulsiveness. Drug Alcohol Depend. 2001;63:29–38. doi: 10.1016/s0376-8716(00)00188-5. [DOI] [PubMed] [Google Scholar]
- Simons J, Gaher R. The Distress Tolerance Scale: development and validation of a self-report measure. Motivat Emot. 2005;29:83–102. [Google Scholar]
- Sprinkle SD, Lurie D, Insko SL, Atkinson G, Jones GL, Logan AR, Bissada NN. Criterion validity, severity cut scores, and test-retest reliability of the Beck Depression Inventory-II in a university counseling center sample. J Counsel Psychol. 2002;49:381–385. [Google Scholar]
- Steer RA, Beck AT. Beck Anxiety Inventory. In: Zalaquett CP, Wood R, editors. Evaluating stress: A Book Of Resources. Scarecrow Education; Lanham, MD: 1997. pp. 23–40. [Google Scholar]
- Stoltenberg SF, Lehmann MK, Christ CC, Hersrud SL, Davies GE. Associations among types of impulsivity, substance use problems and Neurexin-3 polymorphisms. Drug Alcohol Depend. 2011;119:e31–e38. doi: 10.1016/j.drugalcdep.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health, 2012. ICPSR34933-v2. Inter-university Consortium for Political and Social Research; Ann Arbor, MI. 2012. [Google Scholar]
- Torrens M, Gilchrist G, Domingo-Salvany A. Psychiatric comorbidity in illicit drug users: substance-induced versus independent disorders. Drug Alcohol Depend. 2011;113:147–156. doi: 10.1016/j.drugalcdep.2010.07.013. [DOI] [PubMed] [Google Scholar]
- Worley MJ, Trim RS, Roesch SC, Mrnak-Meyer J, Tate SR, Brown SA. Comorbid depression and substance use disorder: longitudinal associations between symptoms in a controlled trial. J Subst Abuse Treat. 2012;43:291–302. doi: 10.1016/j.jsat.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilberman ML, Tavares H, Blume SB, el-Guebaly N. Substance use disorders: sex differences and psychiatric comorbidities. Can J Psychiatry. 2003;48:5–13. doi: 10.1177/070674370304800103. [DOI] [PubMed] [Google Scholar]


