Abstract
Objective
Emotion regulation difficulties have been implicated in theoretical models of anorexia nervosa (AN) development/maintenance, and several treatments for AN have been designed to target emotion dysregulation. However, no research has used longitudinal methodology to examine whether emotion regulation difficulties predict the maintenance of AN symptoms, or vice versa. The current study evaluated dynamic longitudinal relations between emotion dysregulation and AN symptom severity over the year following discharge from intensive treatment in order to enhance theoretical models and treatments for AN.
Method
Participants were 191 patients with AN recruited during intensive treatment. Assessments including the Eating Disorders Examination and the Difficulties in Emotion Regulation Scale were completed at discharge from treatment and at 3-, 6-, and 12-month follow-ups. Bivariate latent change score models were used to examine the direction of associations between emotion dysregulation and AN symptom severity across time.
Results
Emotion dysregulation predicted change in AN symptom severity, but the reverse relationship did not occur. Individuals with high levels of emotion dysregulation experienced an increase and subsequent maintenance of AN psychopathology, whereas low emotion dysregulation predicted a decreasing AN symptom trajectory. Importantly, these dynamic temporal relationships could not be accounted for by body mass index or depressive symptoms and were present for patients with the restricting and binge-eating/purging subtypes of AN.
Conclusions
Emotion regulation difficulties appear to be involved in the maintenance of AN symptom severity over time. Findings provide support for an increasing emphasis on emotion regulation in the development of novel treatments for AN.
Keywords: anorexia nervosa, emotion regulation difficulties, maintenance processes, latent change score models
Anorexia nervosa (AN) is a serious psychiatric disorder associated with significant morbidity and mortality, as well as high public health costs (Agras, 2001; Arcelus, Mitchell, Wales, & Nielsen, 2011; Mitchell & Crow, 2006). Yet, there are few evidence-based treatments for AN, particularly for older adolescents and adults who comprise the majority of individuals with the illness (Attia, 2010). Studies examining the efficacy of specialist outpatient treatments for AN typically report full recovery rates between 0-36% (Fairburn et al., 2013; McIntosh et al., 2005; Schmidt et al., 2012; Zipfel et al., 2014), and a recent review estimated that 20-40% of AN patients drop-out from individual therapy (DeJong, Broadbent, & Schmidt, 2012). Moreover, approximately 20% of patients with AN remain chronically ill (Steinhausen, 2002), suggesting that current treatments do not result in lasting improvement for a significant proportion of patients.
Given the critical need for the development of effective interventions for AN, there has been an emerging interest in identifying underlying mechanisms of dysfunction that contribute to the expression and maintenance of AN symptoms and could be targeted in novel interventions. This approach is timely in light of current efforts to develop new classification systems based on pathophysiological mechanisms in order to isolate specific treatment targets, as well as patient subgroups that might benefit most from particular treatments (Insel et al., 2010; Sanislow et al., 2010). One potential mechanism that has garnered substantial attention in recent theoretical models of AN is emotion dysregulation (Haynos & Fruzzetti, 2011). Several models have proposed that individuals with AN possess personality traits (e.g., high levels of negative emotionality, anxiety, and harm avoidance) that predispose them to engage in eating-disordered behaviors as a means of regulating emotions, and AN symptoms may be maintained through the formation of functional emotion-behavior relationships (Engel et al., 2013; Schmidt & Treasure, 2006; Treasure & Schmidt, 2013; Wildes & Marcus, 2011). Moreover, a number of treatments for AN have been developed that target emotion regulation deficits in order to enhance skills and decrease reliance on eating disorder behaviors (Corstorphine, 2006; Davies et al., 2012; Schmidt et al., 2012; Wildes, Marcus, Cheng, McCabe, & Gaskill, in press).
Numerous abilities contribute to the effective regulation of emotional experiences (Cole, Martin, & Dennis, 2004; Gross, 1998). Consequently, multidimensional models of emotion dysregulation have been developed, including those with particular relevance to psychopathology (Gratz & Roemer, 2004). Research suggests that AN is associated with broad impairments in the ability to monitor, evaluate, and modulate emotional experiences, with similar deficits observed in AN patients and other patient populations with significant emotion dysregulation (e.g., borderline personality disorder; Harrison, Sullivan, Tchanturia, & Treasure, 2009; Svaldi, Griepenstroh, Tuschen-Caffier, & Ehring, 2012). First, extant data indicate that patients with AN have deficits in the ability to recognize and understand emotional experiences, within themselves and others (Gilboa-Schechtman, Avnon, Zubery, & Jeczmien, 2006; Oldershaw et al., 2011). Second, individuals with AN seem to pay less attention to, and thus are less aware of, their emotional experiences (Gilboa-Schechtman et al., 2006). Third, maladaptive core beliefs about the value of experiencing emotions may lead to non-acceptance of emotional experiences (Corstorphine, 2006), which could contribute to the avoidance of emotions and situations that trigger strong emotions (Wildes, Ringham, & Marcus, 2010). Finally, individuals with AN endorse the perception of being unable to access appropriate strategies to regulate negative emotions when they arise (Gilboa-Schechtman et al., 2006; Harrison et al., 2009).
Despite evidence that AN is related to emotion regulation difficulties across a variety of domains, there is a notable absence of prospective longitudinal data on whether emotion regulation difficulties predict the progression and maintenance of AN symptoms over time or, conversely, whether features of the illness state account for or exacerbate emotion regulation difficulties. Examining the direction of this relationship is critical for clarifying whether emotion regulation deficits play a role in the maintenance of AN and thus represent viable mechanisms to target in AN treatments. Several studies have compared emotion regulation difficulties in ill and recovered individuals with AN in order to indirectly examine whether emotion regulation deficits represent predictors versus consequences of AN, but results have been conflicting (Brockmeyer et al., 2012; Harrison, Tchanturia, & Treasure, 2010). Ecological momentary assessment (EMA) data indicate that emotions precipitate eating disorder behaviors in individuals with AN, and decreases in negative emotions, as well as increases in positive emotions, after the occurrence of these behaviors suggest that reinforcement processes may maintain AN symptoms (Engel et al., 2013; Selby et al., in press). Although EMA studies are ideal for examining proximal relations between emotions and AN symptoms, they cannot directly investigate whether emotion dysregulation predicts the maintenance of AN symptoms over more extended time frames (e.g., one year). Further, AN symptoms may effectively regulate emotions in the short-term, but they may increase emotion dysregulation over time. Consequently, there is a pressing need for multi-wave prospective longitudinal studies to explore dynamic temporal associations between emotion regulation difficulties and AN symptoms.
The current study investigated longitudinal, reciprocal associations between emotion regulation difficulties and AN symptom severity during a one-year naturalistic follow-up of AN patients following discharge from intensive treatment. Dynamic latent change score (LCS) models (Ferrer & McArdle, 2010; McArdle, 2009) were used to test the following competing hypotheses regarding the direction of emotion dysregulation/AN symptom severity relationships: 1) emotion dysregulation predicts subsequent increases in AN symptom severity; 2) AN symptom severity predicts subsequent worsening of emotion regulation; 3) both emotion dysregulation and AN symptom severity predict changes in one another across time. LCS modeling allowed for the consideration of time-dependent relations between emotion dysregulation and AN symptom severity while also accounting for constant change in both variables and individual differences in constant change over time (McArdle, 2009). To our knowledge, this is the first prospective longitudinal study to examine associations between emotion regulation difficulties and AN symptoms, and findings have the potential to enhance existing theoretical models and treatments for AN that consider emotion regulation to be a potential mechanism for symptom improvement.
Methods
Participants
Participants were enrolled in a longitudinal study examining the short-term naturalistic course of AN following inpatient or day hospital treatment (reference removed for masked review). Study inclusion criteria were: 1) age ≥ 16 years, 2) BMI < 18.5 or BMI percentile < 10 (patients aged 16-19 years) upon admission to treatment, 3) medical stability, and 4) meeting DSM-IV-TR criteria for AN with two exceptions: a) amenorrhea was not required and b) individuals with a BMI < 17.5 who denied fear of fatness were included, consistent with descriptions of non-fat-phobic AN (Becker, Thomas, & Pike, 2009). After the study was described, 194 individuals (75.8% of those approached) signed consent forms approved by the local Institutional Review Board (assent for individuals under 18 years) and completed admission assessments, including the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (First, Spitzer, Gibbon, & Williams, 2007) and an investigator-designed questionnaire to document demographics and treatment history.
Participants were 191 patients with data available for at least one of the included time points (see Procedures). The mean age of the sample was 26.5 years (SD = 10.2). Participants were primarily female (n = 182; 95.3%) and non-Hispanic Caucasian (n = 182; 95.3%). The majority were employed (n = 48; 25.1%) or in school (n = 84; 44.0%). With respect to clinical characteristics, participants reported that they had been ill for a mean of 8.6 years (SD = 9.0; range = 0-45 years), and nearly half the sample (n = 91; 47.6%) had at least one previous hospitalization for an eating disorder. Of note, 84 participants (44.0%) reported a duration of eating disorder symptoms ≥ 7 years, which corresponds to recent definitions of severe and enduring AN (Touyz et al., 2013). With regards to comorbid psychopathology, 79.6% (n = 152) of participants had a lifetime mood disorder, 63.4% (n = 121) had a lifetime anxiety disorder, and 36.1% (n = 69) had a lifetime substance use disorder. Descriptive statistics for the primary study measures and potential explanatory variables (see Measures) are included in Table 1.
Table 1. Descriptive Statistics for Clinical Characteristics (N=191).
| Variable | Admission | Discharge | 3 months | 6 months | 12 months | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| M (S.D) | Range | M (S.D) | Range | M (S.D) | Range | M (S.D) | Range | M (S.D) | Range | |
| EDE Global score | 3.07 | 0-5.59 | 2.53 | 0-5.52 | 2.60 | 0-5.67 | 2.53 | 0-5.89 | 2.43 | 0-5.90 |
| (1.45) | (1.50) | (1.54) | (1.58) | (1.59) | ||||||
| DERS Total score | 110.71 | 44-171 | 104.38 | 40-170 | 103.72 | 37-163 | 100.18 | 37-169 | 99.45 | 36-173 |
| (24.13) | (26.83) | (29.01) | (29.89) | (32.07) | ||||||
| Body Mass Index | 15.71 | 9.39- | 18.06 | 12.14- | 17.83 | 11.34- | 17.71 | 9.62- | 17.94 | 11.62- |
| (1.82) | 18.42 | (1.53) | 22.39 | (2.23) | 23.69 | (2.48) | 24.63 | (2.70) | 24.58 | |
| BDI-II Score | 30.52 | 0-60 | 23.29 | 0-60 | 24.37 | 0-62 | 23.52 | 0-57 | 22.83 | 0-61 |
| (13.40) | (14.84) | (14.95) | (15.39) | (15.92) | ||||||
Note. EDE = Eating Disorder Examination; DERS = Difficulties in Emotion Regulation Scale; BDI-II = Beck Depression Inventory-Second Edition. Data from the admission assessment were not included in the current study, but are presented for comparisons to other AN patient samples.
Procedures
The current study examined data collected at discharge from intensive treatment and at 3, 6, and12 months post-discharge. We did not include admission data because we were interested in examining naturalistic associations between emotion regulation difficulties and eating disorder symptoms over time, and the interval from admission to discharge represented a period of intensive treatment for all participants (see Hawley, Ho, Zuroff, & Blatt, 2007 for an example).1 Of the 191 participants included in the study, 187 (97.9%) completed discharge assessments, 162 (84.8%) completed 3-month follow-up assessments, 160 (83.7%) completed 6-month follow-up assessments, and 152 (79.6%) completed 12-month follow-up assessments. More than 90% of the sample (n = 176; 92.1%) completed at least one follow-up assessment. There were no significant differences between participants who completed all follow-up assessments versus those missing data for at least one assessment on either emotion regulation difficulties or AN symptom severity at discharge (p's > .40).2
To maximize participant retention, follow-up assessments were conducted in-person or by phone (interviews) and mail (questionnaires). Telephone interviews have been shown to be equivalent to in-person interviews in terms of validity, reliability, precision of estimates, and response rates (Keel, Crow, Davis, & Mitchell, 2002). Interviewers were bachelor's-, master's-, or doctoral-level research clinicians who were trained and supervised by two experienced psychologists during weekly consensus meetings. Interviews were audiotaped, and 10% were randomly selected and re-rated by independent clinicians to establish inter-rater reliability.
Treatment
Although the current study did not examine changes in emotion dysregulation and AN symptoms during the period from admission to discharge (see Procedures), we describe the inpatient and day hospital programs at our center to facilitate comparisons to other studies (see reference removed for masked review for additional details). The two milieus are similar in that they are informed by cognitive behavioral and dialectical behavior therapy principles, and the primary treatment modalities are group therapy and meal support. The inpatient setting provides 24-hour care, and the day hospital program operates 32 hours per week. Many patients step-down to the day hospital program following inpatient treatment, but some low-weight patients are managed exclusively with day hospital care, and others receive inpatient treatment only. In the current sample, 118 (61.8%) participants received inpatient treatment only, 21 (11.0%) received day hospital treatment only, and 52 (27.2%) received both inpatient and day hospital treatment. Of the participants who provided follow up data, 99% (n = 175/176) participated in treatment during the post-discharge period. Approximately half of the sample (n = 93/176; 52.8%) received additional intensive treatment (i.e., inpatient, day hospital, or residential treatment) during the one-year follow-up period.3
Measures
AN symptom severity
The Eating Disorder Examination (EDE), 16th edition (EDE; Fairburn & Cooper, 2008) was administered at each assessment point to comprehensively evaluate AN symptoms. The EDE comprises four subscales (Restraint, Eating Concern, Shape Concern, and Weight Concern) and a Global score calculated as the mean of the four subscales. EDE subscale items are rated on a 7-point scale based on symptom frequency/severity over the past 28 days,4 with higher scores indicating greater pathology. We focused on the EDE Global score as a composite measure of AN symptom severity, given that EDE subscales are highly correlated with the Global Score (r's = .80-.94) and represent both cognitive (e.g., weight concerns) and behavioral (e.g., dietary restraint) symptoms of AN. The psychometric properties of the EDE are well-established (for a review, see Berg, Peterson, Frazier, & Crow, 2012). Internal consistency (α's = .94-.95) and inter-rater reliability estimates (intraclass coefficients (ICCs) = .99) for the EDE Global score were excellent in the current study.
Emotion regulation difficulties
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) is a 36-item self-report questionnaire that comprehensively assesses the multi-dimensional construct of emotion dysregulation, including difficulties in the ability to monitor, evaluate, and modulate emotional experiences given the demands of a specific context or set of goals (Stevens et al., 2013). The DERS provides a total score and six subscales in the following domains: 1) lack of clarity, 2) lack of emotional awareness, 3) non-acceptance of emotional responses, 4) impulse control difficulties when upset, 5) difficulties engaging in goal-directed behavior when upset, and 6) limited access to emotion regulation strategies (Gratz & Roemer, 2004). DERS items are rated on a 5-point scale ranging from “almost never (0-10%)” to “almost always (91-100%).” The current study examined the DERS Total score as a measure of overall emotion regulation difficulties, given that previous research provides support for broad emotion regulation deficits in AN using the DERS (Harrison et al., 2009; Svaldi et al., 2012). Further, DERS subscales correlated highly with the total score in our sample (r's = .71-.91 at discharge), with a slightly lower correlation for lack of emotional awareness (r = .54). Reliability and validity of the DERS have been established (Gratz & Roemer, 2004). Internal consistency estimates were excellent across assessment points in the current study (α's = .95-.97).5
Explanatory and moderating variables
BMI and depressive symptoms were investigated as potential time-varying explanatory variables in the relationship between emotion dysregulation and AN symptom severity. Maintenance of a low BMI following discharge from treatment may explain elevated eating disorder psychopathology and continued emotion regulation difficulties, such that starvation could account for dynamic relations between these variables. At discharge, height and weight measurements were collected by medical chart review. During in-person follow-up assessments, research staff measured height via a stationary stature board and weight via a digital scale. If assessments were completed by phone and mail, participants were asked to provide a release of information for current height and weight to be collected from a physician, therapist, or other treatment professional. In-person or verified height/weight data were obtained for approximately 90% of participants at each follow-up assessment. Self-reported heights and weights, which demonstrate validity in AN samples (McCabe, McFarlane, Polivy, & Olmsted, 2001; Wildes, Forbush, & Markon, 2013), were used in the remaining cases.
Depressive symptomatology could also explain longitudinal emotion dysregulation/AN symptom associations. Indeed, a previous study found that depressive symptoms accounted for relations between emotion regulation deficits and eating disorder severity (Gilboa-Schechtman et al., 2006). Therefore, it is important to determine whether emotion dysregulation and AN psychopathology are uniquely related to one another, over and above the effects of depression. The Beck Depression Inventory-Second Edition (BDI-II) was used to assess depressive symptoms at each study time point. Internal consistency estimates were excellent across assessment points in the current study (α's = .91-.94).
AN subtype (i.e., restricting (AN-R) versus binge-eating/purging (AN-B/P)) was examined as a possible moderator of the dynamic relationship between emotion dysregulation and AN symptom severity. Binge eating and purging are the eating disorder symptoms most frequently linked to emotion regulation difficulties (Engel et al., 2013; Smyth et al., 2007), and it is possible that emotion dysregulation and global eating disorder psychopathology may be longitudinally related only in patients with AN-B/P. AN subtype was determined based on the endorsement of objective binge episodes or purging episodes upon presentation to treatment (i.e., at least 1 episode/month for 3 months). Eighty-two (42.9%) participants were diagnosed with AN-R, and 109 (57.1%) participants were diagnosed with AN-B/P at admission.
Statistical Analyses
A dynamic bivariate LCS model (Ferrer & McArdle, 2010; McArdle, 2009) was used to examine longitudinal relations between emotion dysregulation and AN symptom severity over one year. LCS models combine features of autoregressive cross-lagged models within a latent growth curve modelling framework, in that they allow for the examination of time-dependent relations between two variables while simultaneously considering within-variable trajectories of change and individual differences in change trajectories. With this modeling approach, we were able to consider transactional relationships between changes in emotion dysregulation and AN psychopathology while controlling for natural change that might occur in these variables following discharge from intensive treatment.
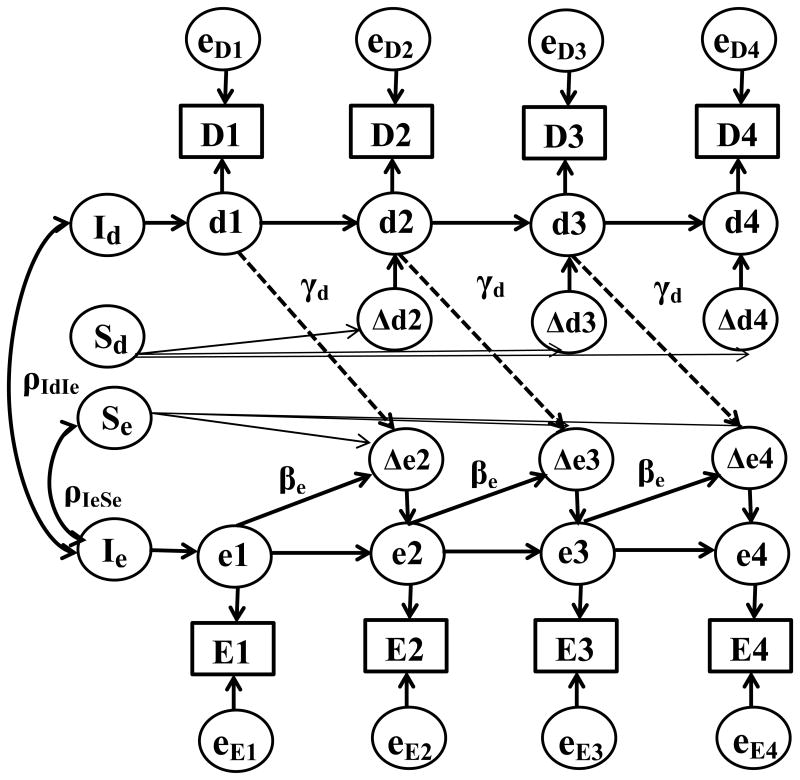
LCS modeling begins by partitioning observed scores, for example AN symptom severity at time 2 (i.e., 3 months) or E2, into a latent or “true” score (e2) and measurement error (eE2; see Figure 1). Latent change scores (LCSs) represent the difference between the latent score at a particular time point and the latent score at the previous time point (Δe2 = e2-e1). When latent change in one variable is modeled (e.g., AN symptom severity), LCSs may be influenced by two sources of internal change: proportional change (βe), or change that is proportional to the latent score at the previous time point, and constant change (Se), or systematic change that occurs as a function of time (see Figure 1). This “dual change” LCS model can be compared to other univariate LCS models to establish the most appropriate model of change for the series given the observed data: a) constant change model (i.e., constant underlying change parameter, no proportional change); b) proportional change model (i.e., proportional change parameter(s), no underlying change trajectory); and c) no change model (i.e., previous latent scores perfectly predict scores at subsequent time points).
Figure 1. Path diagram of the best-fitting bivariate latent change score (LCS) model in which latent Difficulties in Emotion Regulation Scale (DERS) scores predict rate of change in Eating Disorder Examination (EDE) scores.
D and E represent observed DERS and EDE scores; respectively; d and e represent latent scores; eD and eE represent error variances; Δd and Δe represent LCSs; ρId,Ie represents the DERS and EDE intercept covariance; ρIe,Se represents the EDE intercept and slope covariance; βe represents the EDE time-invariant proportional coefficient; γd represents the DERS to EDE coupling coefficient. Unlabeled paths were set to 1. Error variances for DERS and EDE observed scores were equated across time, respectively, and DERS and EDE error variances within each time point were correlated and set equal over time.
Once the nature of the change process for each longitudinal series has been established (e.g., Hawley et al., 2007), bivariate LCS models can examine the “longitudinal coupling” between two sets of variables; in our case, emotion dysregulation and AN symptom severity. In the bivariate model, the longitudinal coupling between the variables may also contribute to the LCSs. For example, change in AN symptom severity is now also influenced by the emotion dysregulation score at the previous time point (γd) in addition to the two sources of internal change. In the bivariate LCS model, the equations for change are as follows:
The nature of the longitudinal coupling between emotion dysregulation and AN symptom severity can be evaluated by imposing restrictions on the full bivariate LCS model, which includes bidirectional or transactional coupling between the variables (γd ≠ 0; γe ≠ 0). Specifically, the following models can be considered: a) unidirectional coupling from emotion dyresgulation to change in AN symptom severity (γd ≠ 0; γe = 0); b) unidirectional coupling from AN symptom severity to change in emotion dysregulation (γd = 0; γe ≠ 0); and c) no dynamic coupling between emotion dysregulation and AN symptoms (γd = 0; γe = 0).
Models were fit using Mplus version 6.0 (Muthén & Muthén, 2010). Full information maximum likelihood (ML) estimation was used as this method allows for the use of all available data and accounts for missing data under the assumption that data are missing at random (Little Rubin, 1987). The degree of model fit was assessed using the chi-square (χ2) goodness of fit statistic, the comparative fit index (CFI; Bentler, 1990), and the root-mean-square error of approximation (RMSEA; Browne & Cudeck, 1993). Hu and Bentler (1999) suggest that CFI values ≥ 0.95 and RMSEA values ≤ 0.06 indicate good model fit. Nested model comparisons were conducted by calculating a χ2 difference test (Δχ2). Statistically significant Δχ2 values lead to the rejection of the nested (i.e., more restrictive model) in favor of the less restrictive model, whereas non-significant Δχ2 values indicate preference for the more parsimonious model. Akaike's Information Criteria (AIC) also was consulted when conducting nested model comparisons, and AIC is smaller in the best-fitting models.
Results
Univariate LCS Models: Characterizing the Nature of Within-Variable Change
Prior to evaluating the bivariate LCS model, we fit a series of univariate LCS models to separately examine change in emotion dysregulation and AN symptomatology (Hawley, Ho, Zuroff, & Blatt, 2006; Kouros, Quasem, & Garber, 2013; Sbarra & Allen, 2009). A dual change score model provided the best fit to the data for AN symptom severity (χ2 (5) = 6.30; CFI = 1.00; RMSEA = 0.04; AIC = 1960.48), compared to the constant change (Δχ2 (3) = 8.44; P =.04; AIC = 1962.91), proportional change (Δχ2 (3) = 15.94, P = .001; AIC = 1970.41), and no change models (Δχ2 (6) = 19.84; p = .003; AIC = 1968.31). Constraining the proportional change coefficients to be equal to one another across time did not significantly worsen model fit (χ2 (2) = 4.98; p = .08; AIC = 1961.46). Parameter estimates indicate that, on average, AN symptom severity scores increased linearly over time (Se = 1.43; p = .01) and decreased proportionally from the previous latent AN symptom score (βe = -0.57, p = .01). In other words, there was a slight trend for increasing scores across the sample, although high AN symptom severity scores were associated with a decrease relative to the previous score.
In contrast, the constant change model best described change in emotion dysregulation (χ2 (8) = 7.33; CFI = 1.00; RMSEA = 0; AIC = 2759.61). The constant change model did not fit significantly worse than the dual change model (Δχ2 (3) = 2.48, p = .48; AIC = 2763.13), but provided a substantially better fit to the data than the no change model (Δχ2 (3) = 28.68, p < .001; AIC = 2782.29). The constant change parameter indicates that emotion dysregulation scores exhibited a decreasing trajectory across time (Sd = -0.15, p = .01). Taken together, univariate LCS models revealed that the trajectory of AN symptoms is best described as a combination of two internal change processes (i.e., constant change and proportional self-feedback), whereas change in emotion dysregulation is characterized solely by constant change over time.
Bivariate LCS Model: Dynamic Coupling across Time
A bivariate LCS model was used to examine dynamic, longitudinal relations between emotion dysregulation and AN symptom severity over time (e.g., Kouros et al., 2013). Table 2 presents fit statistics for the four models that were compared to investigate the nature of the longitudinal coupling (i.e., full (bidirectional) coupling model, DERS predicting EDE model, EDE predicting DERS model, no coupling model).6 The best-fitting, most parsimonious model was the DERS predicting EDE model.7 Dropping the DERS to EDE coupling parameter resulted in a significant decrement in model fit, whereas dropping the EDE to DERS coupling parameter did not significantly worsen model fit (see Table 2). Thus, change in AN symptom severity over time is predicted by emotion dysregulation at the previous time point; however, change in emotion dysregulation does not appear to be impacted by AN symptom severity.8
Table 2. Fit Indices for Bivariate Latent Change Score Models Examining Coupling between Emotion Dysregulation and Anorexia Nervosa Symptom Severity.
| Model | χ2 | df | CFI | RMSEA | Δχ2 (Δdf) | AIC |
|---|---|---|---|---|---|---|
| Bidirectional model | 23.64 | 28 | 1.00 | 0 | -- | 4599.11 |
| DERS predicting EDE Model | 24.17 | 29 | 1.00 | 0 | 0.53 (1) | 4598.02 |
| EDE predicting DERS Model | 36.90 | 29 | .99 | .04 | 13.26 (1)*** | 4610.75 |
| No Coupling model | 40.42 | 30 | .99 | .04 | 16.78 (2)*** | 4612.27 |
Note. χ2 = chi square statistic; df = degrees of freedom; CFI = Comparative Fit Index; RMSEA = Root Mean Square Error of Approximation; Δχ2 = chi-square difference statistic; Δdf = change in degrees of freedom; AIC = Akaike Information Criteria; DERS = Difficulties in Emotion Regulation Scale; EDE = Eating Disorder Examination. Best-fitting model is indicated by bold text.
p < .001
Figure 1 presents the path diagram for the best-fitting unidirectional coupling model, and parameter estimates (along with 95% confidence intervals) from this model are presented in Table 3. Latent change in AN symptom severity consisted of a negative constant slope (Se = -1.09) and a negative proportional coefficient (βe = -0.83), indicating a constant decreasing AN symptom trajectory that is accelerated by a negative self-feedback process (i.e., higher EDE scores result in more negative change). Of greatest importance to the current study, the positive coupling parameter (γd = 0.31) indexing the effect of emotion dysregulation on rate of change in AN symptom severity indicates that individuals with higher emotion dysregulation scores will exhibit less negative change or an increase in AN symptom severity over time.
Table 3. Parameter Estimates from the Bivariate Latent Change Score Model Examining Emotion Dysregulation as a Predictor of Change in AN Symptom Severity.
| Parameters Estimates | Emotion Dysregulation → AN Symptom Severity | |
|---|---|---|
|
| ||
| DERS | EDE | |
| M (S.E) [95% CIs] | M (S.E) [95% CIs] | |
| Initial Mean (μI) | 10.42 (0.19) [10.04,10.80] | 2.54 (0.11) [2.32, 2.76] |
| Slope Mean (μS) | -0.16 (.06) [-0.27, -0.05] | -1.09 (0.35) [-1.78, -0.40] |
| Initial Variance (Φ2I) | 6.01 (0.70) [4.64, 7.38] | 1.88 (0.24) [1.41, 2.37] |
| Slope Variance (Φ2S) | 0.21 (0.06) [0.10, 0.33] | 0.80 (0.31) [0.20, 1.41] |
| Error variance (σ2) | 1.64 (0.13) [1.39, 1.88] | 0.44 (0.04) [0.37, 0.52] |
| Proportional Change (β) | -- | -0.83 (0.16) [-1.15, -0.52] |
| Coupling (γ) | 0.31 (0.06) [0.19, 0.44] | -- |
| Correlations | ||
| DERS Intercept-EDE Intercept (ρId,Ie) | .62 [.51, .73] | |
| EDE Intercept-EDE Slope (ρIe,Se) | .66 [.52, .77] | |
| DERS Residual-EDE Residual (ρd,e) | .23 [.23, .33] | |
Note. DERS = Difficulties in Emotion Regulation Scale; EDE = Eating Disorder Examination; CIs = confidence intervals. 95% CIs that do not overlap with 0 indicate statistical significance at p < .05.
To further explore the meaning and clinical significance of the relationship between emotion dysregulation and change in AN symptom severity, we can use the parameter estimates to examine the expected trajectories of change in AN symptomatology among individuals with high versus low levels of emotion dysregulation. The parameter estimates can be used to generate the following change equation:
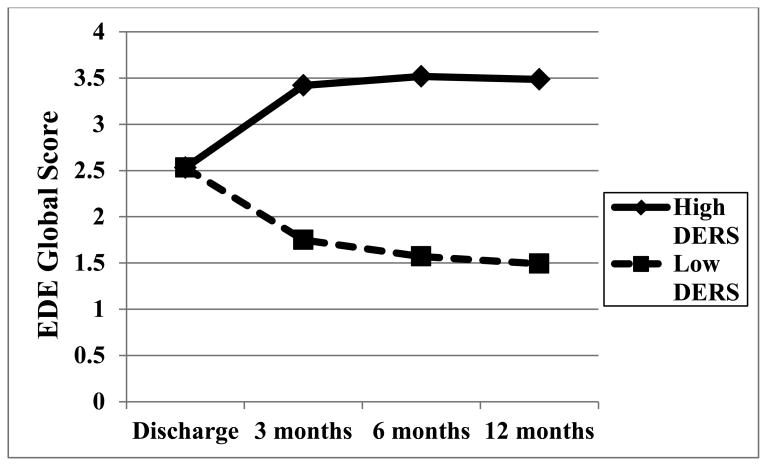
As depicted in Figure 2, individuals with an average level of AN symptoms and high emotion dysregulation (i.e., 1 SD above the mean) at discharge experience an initial increase and subsequent maintenance of AN symptomatology in the year following discharge from treatment (cumulative increase = 0.95 EDE units or 0.63 SD). In contrast, individuals with average AN symptoms and low emotion dysregulation (i.e., 1 SD below the mean) exhibit a decreasing AN symptom trajectory over follow-up (cumulative decrease = 1.04 EDE units or 0.70 SD).
Figure 2. Expected change trajectory in AN symptom severity over time.
Trajectories are plotted for individuals with average Eating Disorder Examination (EDE) Global Scores at discharge. High DERS is defined as a Difficulties in Emotion Regulation Scale (DERS) Total score 1 SD above the mean, and low DERS is defined as a DERS Total score 1 SD below the mean.
Explanatory Variables: BMI and Depressive Symptoms
Next, we considered the possibility that BMI or depressive symptoms might account for the longitudinal relationship between emotion dysregulation and change in AN symptom severity. Given that BMI and depressive symptoms were measured at all assessment points, we examined the lagged effect of these variables at each time point on the emotion dysregulation and AN symptom severity LCSs at the subsequent time point (e.g., BMI at discharge as a predictor of LCSs at 3 months; BMI at 3 months as a predictor of LCSs at 6 months). DERS and EDE intercepts were also regressed on to BMI/BDI-II scores at discharge. Both the models including BMI and BDI-II scores as explanatory variables provided an acceptable fit to the data (BMI model: χ2 (49) = 43.85; CFI=1.0; RMSEA = 0; BDI-II Model: χ2 (49) = 90.40; CFI = .97; RMSEA = .08). BMI did not significantly influence initial level or change in emotion dysregulation and AN symptom severity, and the magnitude of the longitudinal coupling remained unchanged (γd = .31; p = .001) in the BMI model. In contrast, depressive symptoms significantly predicted initial status and latent change in emotion dysregulation and AN symptom severity. The effect of emotion dysregulation on AN symptom severity remained significant but decreased in magnitude (γd = .15; p = .02). Therefore, emotion dysregulation influences maintenance of AN symptomatology independent of BMI and depressive symptoms.
Moderating Variable: AN Subtype
Multigroup bivariate LCS analyses examined whether the relationship between emotion dysregulation and change in AN symptoms differed for patients with AN-R compared to AN-B/P. Multigroup structural equation models use a series of increasingly restrictive models to compare the equivalence of sets of parameters (e.g., means, variances, path coefficients). A model that freely estimates parameters in both groups is compared to a model that constrains a set of parameters to be equal across groups. Using chi-square difference testing, equality constraints that do not significantly degrade model fit are retained and are cumulatively held in place when testing subsequent parameter equivalence. The final multigroup model provided an excellent fit to the data (χ2 (68) = 71.26; CFI = 1.00; RMSEA = .02). Most parameters were equivalent across groups, although individuals with AN-B/P had greater initial levels of emotion dysregulation and AN symptoms as well a stronger baseline correlation between these variables than those with AN-R. Further, the coupling parameter was slightly larger in the AN-B/P group (γd = 0.33, p < .001) compared to the AN-R group (γd = 0.29, p < .001). Nonetheless, emotion dysregulation predicted subsequent change in AN symptom severity across both AN subtypes.
Discussion
There is growing interest in understanding whether emotion regulation difficulties represent mechanisms underlying the maintenance of AN symptoms that could be targeted in novel treatments (Haynos & Fruzzetti, 2011; Treasure & Schmidt, 2013; Wildes et al., in press). However, to our knowledge, this study is the first to investigate the presence of dynamic, longitudinal relations between emotion dysregulation and AN symptom severity. Emotion regulation difficulties significantly predicted change in AN symptom severity over the year following intensive treatment, but there was no relationship between AN symptom severity and change in emotion dysregulation. Importantly, the longitudinal coupling between emotion dysregulation and AN symptoms was independent of BMI and depressive symptoms and was observed for both the AN-R and AN-B/P subtypes. Findings highlight the importance of emotion regulation difficulties in the maintenance of AN symptoms and provide support for an increasing emphasis on emotion regulation in the development of novel treatments for AN.
Using bivariate LCS modeling, we found that naturalistic change in AN symptom severity over one year is influenced by three sources: constant underlying change, change that is proportional to one's AN symptom severity score at the previous time point, and change that is related to one's emotion dysregulation score at the previous time point. Thus, a critical finding is that level of emotion dysregulation influences rate of change in AN symptom severity above and beyond two internal sources of change. Specifically, individuals in our sample with low emotion dysregulation experienced a decrease in AN symptom severity over time, whereas patients with high emotion dysregulation scores increased and subsequently maintained high levels of AN symptomatology. These relationships are not trivial. Our data suggest that a patient with average AN symptom severity and low levels of emotion dysregulation at discharge will experience a cumulative decrease of 1.04 EDE units, meaning that EDE Global scores will normalize (i.e., fall within 1 SD of community norms or < 1.74; Couturier & Lock, 2006; Fairburn & Cooper, 2008) after 1 year. In contrast, a patient with average AN symptoms and high emotion dysregulation will experience a cumulative increase of 0.95 EDE units and will maintain EDE scores that are 2 SD above community norms (i.e., > 2.54; Fairburn & Cooper, 2008). Thus, improvements in emotion regulation in the context of treatment are likely to have a significant impact on the longitudinal course of AN symptoms.
Until recently, emotion regulation deficits have been linked almost exclusively to bulimia nervosa (BN) and binge eating disorder (BED), and treatments that target emotion dysregulation (e.g., Dialectical Behavior Therapy, Integrative Cognitive-Affective Therapy; Safer, Telch, & Agras, 2001; Telch, Agras, & Linehan, 2001; Wonderlich et al., 2014) have been primarily designed for or applied to these eating disorder populations. Newly developed treatments for AN that postulate a role for emotions and emotion regulation difficulties include the Maudsley Model for Anorexia Nervosa Treatment for Adults (MANTRA; Schmidt et al., 2012) and Emotion Acceptance Behavior Therapy (EABT; Wildes et al., in press). MANTRA was designed to target several sets of AN maintenance factors, including socio-emotional impairments (e.g., avoidance of emotions and expression of emotions in close relationships), and EABT aims to increase emotional awareness and decrease emotional avoidance. Our results provide support for these treatment approaches by suggesting that difficulties in emotion regulation are related to the progression and maintenance of AN symptomatology over time and, as such, are likely to represent viable treatment targets. However, given that we examined a composite measure of emotion dysregulation, our findings also point to the potential utility of focusing more broadly on emotion regulation impairments in treatments for AN, perhaps by incorporating approaches traditionally used to treat BN and BED. This suggestion is bolstered by the fact that emotion dysregulation predicted change in AN symptom severity among both AN-R and AN-B/P subtypes (although coupling was slightly stronger in the AN-B/P compared to the AN-R group).
Although longitudinal data can be used to identify “determinants” (e.g., emotion dysregulation) of the dynamic change in a particular variable (e.g., AN symptom severity), true causal associations cannot be established due to the possible influence of unmeasured third variables (Ferrer & McArdle, 2010). For this reason, we considered two critical explanatory variables (i.e., BMI and depressive symptoms) that could plausibly account for longitudinal relations between emotion dysregulation and AN symptom severity in order to strengthen the conclusions that can be drawn from our study. Consistent with previous cross-sectional findings (Harrison et al., 2010; Racine & Wildes, 2013), BMI was unrelated to emotion dysregulation and did not impact the longitudinal coupling between emotion dysregulation and AN symptom severity. Not surprisingly, depressive symptoms significantly influenced initial status and change in emotion regulation difficulties and AN symptoms, and partially accounted for the effect of emotion dysregulation on change in AN symptom severity. Nonetheless, independent emotion dysregulation/AN symptom associations suggest that maladaptive regulation of emotions, over and above general emotional distress, is critical for the maintenance of AN symptomatology.
Strengths of the current study include examination of a large sample of AN patients assessed across multiple time points over one year, as well as the use of self-report ratings of emotion regulation difficulties and clinician ratings of AN symptoms, which reduced shared method variance. Further, our analytic approach provided a stringent test of dynamic coupling relationships between emotion dysregulation and AN symptom severity by controlling for relevant sources of internal change, as well as baseline correlations between the variables. Nonetheless, several limitations of the present study must be noted. First, given that we examined a currently or recently ill patient sample, our results only address the influence of emotion dysregulation on the maintenance of AN symptoms over time. Thus, future prospective research is needed to understand the potential role of emotion dysregulation in increasing vulnerability for the initial development of AN symptoms. Arguably, however, understanding maintenance (versus etiology) is most critical when developing novel treatments (Shafran & de Silva, 2003), as it is the specific mechanisms that influence persistence versus remission in AN patients that are likely to be important treatment targets (Stice, 2002).
Second, AN patients were assessed for one-year following discharge from intensive treatment, and results might not generalize to emotion dysregulation/AN relationships across different time frames. For example, although our findings do not suggest that AN symptomatology predicts change in emotion dysregulation over one year, EMA studies are better suited to investigate hypotheses about the emotion regulating/reinforcing properties of AN symptoms. Examining momentary emotion dysregulation, in addition to the experience of emotion (e.g., Engel et al., 2013), in EMA studies may elucidate immediate relationships between levels of emotion dysregulation and AN symptoms.
Third, our analyses focused on composite measures of emotion dysregulation (i.e., DERS Total Score) and AN symptom severity (i.e., EDE Global Score) and thus cannot speak to differential temporal dynamics between particular emotion regulation deficits and specific eating disorder symptoms (e.g., binge eating, purging, BMI). For example, results from a previous cross-sectional study suggested that impulse control difficulties when upset specifically predict the presence of binge eating and purging in AN (Racine & Wildes, 2013). Unfortunately, given that approximately half of our sample did not engage in binge or purge episodes, we could not examine changes in these behaviors across the study. Further, non-significant relationships between emotion dysregulation and BMI (see Results) may be due to a restricted range of BMIs in our AN sample (see Table 1). In addition, the DERS focuses primarily on emotion dysregulation with regards to negative affect, although positive emotion dysregulation also has recently been implicated in AN (Selby et al., in press). Thus, it will be important for future studies to investigate dynamic longitudinal relations between additional emotion regulation deficits and particular eating disorder symptoms in AN and other eating disorder populations. Finally, given that our participants reported a long duration of illness and were recruited from inpatient and day hospital treatment settings, our findings may not generalize to patients with less severe forms of eating disturbance who do not receive intensive treatment.
In sum, findings from this study point to the existence of dynamic longitudinal associations between emotion dysregulation and AN symptom severity. Specifically, emotion dysregulation predicted change in AN symptom severity over time, but the reverse relationship did not occur. Overall, results provide support for the development of novel treatments for AN that teach skills to help develop adaptive emotion regulation strategies in an effort to decrease reliance on eating disorder behaviors. Ultimately, treatments that are designed to target the underlying mechanisms that maintain AN symptoms hold promise for improving short- and long-term outcomes in AN patients and for reducing the significant morbidity and mortality associated with this debilitating disorder.
Public Health Significance Statement.
Difficulties with emotion regulation predict the maintenance of anorexia nervosa (AN) symptoms over the year following intensive treatment. Findings provide support for recently developed treatments for AN that target emotion dysregulation in hopes of improving outcomes for this debilitating disorder.
Acknowledgments
This research was supported by K01 MH080020 and T32 MH018269 from the National Institute of Mental Health. We would like to acknowledge and thank Dr. Kelsie Forbush for statistical consultation and comments on an earlier draft of the manuscript as well as Dr. Aidan Wright for statistical consultation.
Footnotes
Author Note: Portions of this manuscript were presented at the Eating Disorders Research Society Meeting, Bethesda, MD, September 19-21, 2013.
Typically, LCS modeling estimates one set of coupling parameters to index the “average” longitudinal coupling between two processes over time, and including a time of expected change for all participants is likely to bias these parameters.
Models were re-run including only participants with complete data, and results were identical to those presented herein (data available upon request). Thus, our proportion of missing data did not unduly influence results.
Including initial level of care and re-admission to intensive treatment as covariates in our models produced identical results to those presented herein (data available upon request).
A modified EDE designed to cover the time since the admission assessment (up to a maximum of 28 days) was administered at discharge.
For all analyses, DERS Total Scores were divided by 10 to facilitate model convergence, given the significant discrepancy in the scales used to measure emotion dysregulation and AN symptom severity (see Table 1).
The following covariance parameters were non-significant and thus set to zero in all models: DERS intercept with DERS slope; DERS intercept with EDE slope; DERS slope with EDE intercept; DERS slope with EDE slope.
Coupling parameters were constrained to be equal across time points, as this constraint did not significantly worsen model fit compared to a model with time-varying coupling effects (Δχ2(2) = 1.38; p = .50).
The same pattern of results was obtained when examining dynamic longitudinal relations between emotion dysregulation and each EDE subscale (i.e., Restraint, Eating Concern, Shape Concern, Weight Concern; data available upon request).
References
- Agras WS. The consequences and costs of the eating disorders. Psychiatric Clinics of North America. 2001;24:371–379. doi: 10.1016/S0193-953X(05)70232-X. [DOI] [PubMed] [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Attia E. Anorexia nervosa: Current status and future directions. Annual Review of Medicine. 2010;61:425–435. doi: 10.1146/annurev.med.050208.200745. [DOI] [PubMed] [Google Scholar]
- Becker AE, Thomas JJ, Pike KM. Should non-fat-phobic anorexia nervosa be included in DSM-V? International Journal of Eating Disorders. 2009;42:620–635. doi: 10.1002/eat.20727. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. International Journal of Eating Disorders. 2012;45:428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockmeyer T, Holtforth MG, Bents H, Kämmerer A, Herzog W, Friederich HC. Starvation and emotion regulation in anorexia nervosa. Comprehensive Psychiatry. 2012;53:496–501. doi: 10.1016/j.comppsych.2011.09.003. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Thousand Oaks, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: Methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Corstorphine E. Cognitive–emotional–behavioural therapy for the eating disorders: Working with beliefs about emotions. European Eating Disorders Review. 2006;14:448–461. doi: 10.1002/erv.747. [DOI] [Google Scholar]
- Couturier J, Lock J. What is recovery in adolescent anorexia nervosa? International Journal of Eating Disorders. 2006;39:550–555. doi: 10.1002/eat.20309. [DOI] [PubMed] [Google Scholar]
- Davies H, Fox J, Naumann U, Treasure J, Schmidt U, Tchanturia K. Cognitive remediation and emotion skills training for anorexia nervosa: An observational study using neuropsychological outcomes. European Eating Disorders Review. 2012;20:211–217. doi: 10.1002/erv.2170. [DOI] [PubMed] [Google Scholar]
- DeJong H, Broadbent H, Schmidt U. A systematic review of dropout from treatment in outpatients with anorexia nervosa. International Journal of Eating Disorders. 2012;45:635–647. doi: 10.1002/eat.20956. [DOI] [PubMed] [Google Scholar]
- Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, et al. The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. Journal of Abnormal Psychology. 2013;122:709–719. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. Eating Disorder Examination (Edition 16.0D) In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008. pp. 265–308. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, O'Connor ME, Palmer RL, Dalle Grave R. Enhanced cognitive behaviour therapy for adults with anorexia nervosa: A UK–Italy study. Behaviour Reserarch and Therapy. 2013;51:R2–R8. doi: 10.1016/j.brat.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer E, McArdle JJ. Longitudinal modeling of developmental changes in psychological research. Current Directions in Psychological Science. 2010;19:149–154. doi: 10.1177/0963721410370300. [DOI] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Structured Clinical interview for DSM-IV Axis I Disorders-Patient Edition with Psychotic Screen. New York: Biometrics Research Department; 2007. [Google Scholar]
- Gilboa-Schechtman E, Avnon L, Zubery E, Jeczmien P. Emotional processing in eating disorders: Specific impairment or general distress related deficiency? Depression and Anxiety. 2006;23:331–339. doi: 10.1002/da.20163. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2:271–299. doi: 10.1037/1089-2680.2.3.271. [DOI] [Google Scholar]
- Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotion recognition and regulation in anorexia nervosa. Clinical Psychology & Psychotherapy. 2009;16:348–356. doi: 10.1002/cpp.628. [DOI] [PubMed] [Google Scholar]
- Harrison A, Tchanturia K, Treasure J. Attentional bias, emotion recognition, and emotion regulation in anorexia: State or trait? Biological Psychiatry. 2010;68:755–761. doi: 10.1016/j.biopsych.2010.04.037. [DOI] [PubMed] [Google Scholar]
- Hawley LL, Ho MHR, Zuroff DC, Blatt SJ. The relationship of perfectionism, depression, and therapeutic alliance during treatment for depression: Latent difference score analysis. Journal of Consulting Clinical Psychology. 2006;74:930–942. doi: 10.1037/0022-006X.74.5.930. [DOI] [PubMed] [Google Scholar]
- Hawley LL, Ho MHR, Zuroff DC, Blatt SJ. Stress reactivity following brief treatment for depression: Differential effects of psychotherapy and medication. Journal of Consulting and Clinical Psychology. 2007;75:244–256. doi: 10.1037/0022-006X.75.2.244. [DOI] [PubMed] [Google Scholar]
- Haynos AF, Fruzzetti AE. Anorexia nervosa as a disorder of emotion dysregulation: Evidence and treatment implications. Clinical Psychology: Science and Practice. 2011;18:183–202. doi: 10.1111/j.1468-2850.2011.01250.x. [DOI] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Insel TR, Cuthbert BN, Garvey MA, Heinssen RK, Pine DS, Quinn KJ, et al. Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Keel PK, Crow S, Davis TL, Mitchell JE. Assessment of eating disorders: Comparison of interview and questionnaire data from a long-term follow-up study of bulimia nervosa. Journal of Psychosomatic Research. 2002;53:1043–1047. doi: 10.1016/s0022-3999(02)00491-9. doi:S0022399902004919 [pii] [DOI] [PubMed] [Google Scholar]
- Kouros CD, Quasem S, Garber J. Dynamic temporal relations between anxious and depressive symptoms across adolescence. Development and Psychopathology. 2013;25:683–697. doi: 10.1017/S0954579413000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: Wiley; 1987. [Google Scholar]
- McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- McCabe RE, McFarlane T, Polivy J, Olmsted MP. Eating disorders, dieting, and the accuracy of self-reported weight. International Journal of Eating Disorders. 2001;29:59–64. doi: 10.1002/1098-108X(200101)29:1<59::AID-EAT9>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- McIntosh VV, Jordan J, Carter FA, Luty SE, McKenzie JM, Bulik CM, et al. Three psychotherapies for anorexia nervosa: A randomized, controlled trial. American Journal of Psychiatry. 2005;162:741–747. doi: 10.1176/appi.ajp.162.4.741. [DOI] [PubMed] [Google Scholar]
- Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Current Opinion in Psychiatry. 2006;19:438–443. doi: 10.1097/01.yco.0000228768.79097.3e. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Software (Version 6.0) Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Oldershaw A, Hambrook D, Stahl D, Tchanturia K, Treasure J, Schmidt U. The socio-emotional processing stream in anorexia nervosa. Neuroscience & Biobehavioral Reviews. 2011;35:970–988. doi: 10.1016/j.neubiorev.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Racine SE, Wildes JE. Emotion dysregulation and symptoms of anorexia nervosa: The unique roles of lack of emotional awareness and impulse control difficulties when upset. International Journal of Eating Disorders. 2013;46:713–720. doi: 10.1002/eat.22145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. American Journal of Psychiatry. 2001;158:632–634. doi: 10.1176/appi.ajp.158.4.632. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, et al. Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Sbarra DA, Allen JJ. Decomposing depression: On the prospective and reciprocal dynamics of mood and sleep disturbances. Journal of Abnormal Psychology. 2009;118:171–192. doi: 10.1037/a0014375. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Oldershaw A, Jichi F, Sternheim L, Startup H, McIntosh V, et al. Outpatient psychological therapies for adults with anorexia nervosa: Randomised controlled trial. The British Journal of Psychiatry. 2012;201:392–399. doi: 10.1192/bjp.bp.112.112078. [DOI] [PubMed] [Google Scholar]
- Schmidt U, Treasure J. Anorexia nervosa: Valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice. British Journal of Clinical Psychology. 2006;45:343–366. doi: 10.1348/014466505X53902. [DOI] [PubMed] [Google Scholar]
- Selby EA, Wonderlich SA, Crosby RD, Engel SG, Panza E, Mitchell JE, et al. Nothing tastes as good as thin feels: Low positive emotion differentiation and weight-loss activities in anorexia nervosa. Clinical Psychological Science. doi: 10.1177/2167702613512794. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafran R, de Silva P. Cognitive behavioural models. In: Treasure J, Schmidt U, Van Furth E, editors. Handbook of Eating Disorders. Chichester: Wiley; 2003. pp. 121–139. [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC. The outcome of anorexia nervosa in the 20th century. American Journal of Psychiatry. 2002;159:1284–1293. doi: 10.1176/appi.ajp.159.8.1284. [DOI] [PubMed] [Google Scholar]
- Stevens NR, Gerhart J, Goldsmith RE, Heath NM, Chesney SA, Hobfoll SE. Emotion regulation difficulties, low social support, and interpersonal violence mediate the link between childhood abuse and posttraumatic stress symptoms. Behavior Therapy. 2013;44:152–161. doi: 10.1016/j.beth.2012.09.003. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: A marker of eating pathology or general psychopathology? Psychiatry Research. 2012;197:103–111. doi: 10.1016/j.psychres.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1061–1065. doi: 10.1037/0022-006X.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Touyz S, Le Grange D, Lacey H, Hay P, Smith R, Maguire S, et al. Treating severe and enduring anorexia nervosa: A randomized controlled trial. Psychological Medicine. 2013;43:2501–2511. doi: 10.1017/S0033291713000949. [DOI] [PubMed] [Google Scholar]
- Treasure J, Schmidt U. The Cognitive-Interpersonal Maintenance Model of Anorexia Nervosa Revisited: A summary of the evidence for cognitive, socio-emotional and interpersonal predisposing and perpetuating factors. Journal of Eating Disorders. 2013;1:1–10. doi: 10.1186/2050-2974-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Forbush KT, Markon KE. Characteristics and stability of empirically-derived anorexia nerovsa subtypes: Towards the identification of homogenous low-weight eating disorder phenotypes. Journal of Abnormal Psychology. 2013;122:1031–1041. doi: 10.1037/a0034676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD. Development of emotion acceptance behavior therapy for anorexia nervosa: A case series. International Journal of Eating Disorders. 2011;44:421–427. doi: 10.1002/eat.20826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Cheng Y, McCabe EB, Gaskill JA. Emotion acceptance behavior therapy for anorexia nervosa: A pilot study. International Journal of Eating Disorders. doi: 10.1002/eat.22241. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildes JE, Ringham RM, Marcus MD. Emotion avoidance in patients with anorexia nervosa: Initial test of a functional model. International Journal of Eating Disorders. 2010;43:398–404. doi: 10.1002/eat.20730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich S, Peterson C, Crosby R, Smith T, Klein M, Mitchell J, et al. A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychological Medicine. 2014:543–553. doi: 10.1017/S0033291713001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zipfel S, Wild B, Groß G, Friederich HC, Teufel M, Schellberg D, et al. Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa (ANTOP study): Randomised controlled trial. The Lancet. 2014;383:127–137. doi: 10.1016/S0140-6736(13)61746-8. [DOI] [PubMed] [Google Scholar]