Abstract
Background
Many mechanistic steps underlying nutrient-stimulated insulin secretion (NSIS) are poorly understood. The influence of intracellular pH (pHi) on insulin secretion is widely documented, and can be used as an investigative tool. This study demonstrates previously unknown effects of pHi-alteration on insulin secretion in mouse islets, which may be utilized to correct defects in insulin secretion.
Methods
Different components of insulin secretion in mouse islets were monitored in the presence and absence of forced changes in pHi. The parameters measured included time-dependent potentiation of insulin secretion by glucose, and direct insulin secretion by different mitochondrial and non-mitochondrial secretagogues. Islet pHi was altered using amiloride, removal of medium Cl-, and changing medium pH. Resulting changes in islet pHi were monitored by confocal microscopy using a pH-sensitive fluorescent indicator. To investigate the underlying mechanisms of the effects of pHi-alteration, cellular NAD(P)H levels were measured using two-photon excitation microscopy (TPEM). Data were analyzed using Student's t test.
Results
Time-dependent potentiation, a function normally absent in mouse islets, can be unmasked by a forced decrease in pHi. The optimal range of pHi for NSIS is 6.4–6.8. Bringing islet pHi to this range enhances insulin secretion by all mitochondrial fuels tested, reverses the inhibition of glucose-stimulated insulin secretion (GSIS) by mitochondrial inhibitors, and is associated with increased levels of cellular NAD(P)H.
Conclusions
Pharmacological alteration of pHi is a potential means to correct the secretory defect in non-insulin dependent diabetes mellitus (NIDDM), since forcing islet pHi to the optimal range enhances NSIS and induces secretory functions that are normally absent.
Background
Nutrient-stimulated insulin secretion (NSIS) in the pancreatic β cell consists of three distinct components with different underlying mechanisms. These components include a) an initial peak (first phase) triggered by Ca2+, b) augmentation of the Ca2+-triggered response (second phase), and c) a memory that persists after removal of the nutrient, causing enhancement of subsequent secretory responses (time-dependent potentiation) [1-4]. The first phase of the insulin response is initiated by ATP derived from glucose metabolism, which leads to membrane depolarization through closure of ATP-dependent K+ channels (KATP channels) and consequent entry of extracellular Ca2+ through voltage-gated Ca2+ channels. This influx of Ca2+ triggers the release of a small pool of secretory granules, thus producing the initial peak of the insulin response [1]. This peak is followed by a sustained second phase of insulin release that lasts through the duration of exposure to the nutrient, believed to be mediated through augmentation of the Ca2+-triggered first-phase response [1]. Time-dependent potentiation (TDP), a positive memory induced during this acute response, magnifies subsequent secretory responses to all secretagogues [2,4-6].
While any secretagogue that causes an adequate increase in Ca2+ will stimulate the first phase insulin release, the complete range of secretory functions (initiation, augmentation and TDP) can only be produced by compounds that enhance cellular metabolism. The mechanisms underlying the augmentation and memory pathways are poorly understood. Both augmentation and TDP are independent of KATP channels [7-9]. The glucose-induced augmentation pathway has both Ca2+-dependent and Ca2+-independent components [10,11], while TDP is largely independent of Ca2+ [12-14]. These functions show considerable species variation. TDP is present only in certain species such as humans and rats, while the nature of the augmentation response differs between species [1-3,15-17]. Elucidating the mechanisms of these different secretory pathways is important in designing new therapeutic measures for diabetes, since NIDDM affects each pathway differently [2,5,18]. TDP is of particular physiological importance. While the direct insulin response to glucose is usually impaired in NIDDM, the potentiating function of glucose can remain intact. In some diabetic subjects, the defective insulin response to glucose can be restored to normal by inducing TDP [18,19]. A potential therapeutic approach for such cases is to stimulate TDP by means other than glucose, thus enhancing the secretory ability of the β cell and enabling the body to better handle the hyperglycemia. In other forms of NIDDM, both the acute insulin release and TDP are impaired [20-22] and the correction of the defect in the TDP pathway may automatically correct the defect in direct insulin release.
There is strong evidence that NSIS is influenced by pHi. Most reports on this subject show that a decrease of pHi is favorable for GSIS and related functions such as Ca2+ influx and K+ retention, while intracellular alkalinization is inhibitory to all these functions [23-31]. The optimal pHi for insulin secretion by both glucose and alpha-ketoisocaproate (αKIC) in rat islets is reported to be 0.09 units below basal [32]. Glucose-stimulated TDP in rat islets is critically dependent on an appropriate pHi [12], and TDP produced by other mitochondrial fuels also show similar pHi-dependence [Unpublished observations: SC Gunawardana, YJ Liu, SG Straub and GWG Sharp].
While these studies clearly demonstrate that pHi affects insulin secretion, further work is necessary to determine a) the specific components of each secretory pathway affected by pHi, b) the underlying mechanisms of such effects, and c) the possible therapeutic value of the influence of pHi on insulin release. Furthermore, information on the effects of pHi in mouse islets is somewhat limited, and, although the majority of the literature indicates that below-basal pHi is favorable for insulin secretion, there are some reports to the contrary [32-34]. Such discrepancies may be due to the differences in media and pHi-measurement techniques used. In this study, using a more accurate modern technique of pHi-measurement [35], we have investigated the effects of pHi on different components of NSIS in mouse islets, and explored the possible mechanisms of such effects. Specific aims were to determine whether pHi-manipulation would a) enable glucose to induce TDP in mouse islets, where it is normally absent; b) influence direct insulin secretion via both mitochondrial and non-mitochondrial signals; and c) produce changes in cellular metabolism, as indicated by NAD(P)H levels.
Our results demonstrate a strong dependence of NSIS on pHi, and the ability of the appropriate pHi to allow secretory functions that are otherwise absent. They also suggest that enhanced nutrient metabolism plays a role in the favorable effects of below-basal pHi on NSIS.
Methods
Animals
Male C57BL6 mice aged 4–8 weeks obtained from Harlan Laboratories (Indianapolis, IN) were used for all experiments. The animals were cared for according to the guidelines of the Vanderbilt Institutional Animal Care and Use Committee.
Media
Islets were isolated in Hanks Balanced Salt solution, and HEPES-buffered Krebs Ringer Bicarbonate solution (KRBH) was used for the major part of the static incubations in secretion experiments. The components of KRBH are as follows: 128.8 mM NaCl; 4.8 mM KCl; 1.2 mM KH2PO4; 1.2 mM MgSO4; 2.5 mM CaCl2; 5 mM NaHCO3- and 10 mM HEPES. In the Cl--free KRBH medium used for intracellular alkalinization, gluconate salts were used in place of Cl- salts. The medium pH was maintained at 7.4, except in the media used for intracellular alkalinization where the pH was raised above 8.3 by addition of NaOH. Basal KRBH used for pre-incubation and non-stimulated controls contained 2.8 mM glucose, while the stimulating media contained either 16.7 mM glucose, or other secretagogues as indicated in the presence of 2.8 mM glucose. In pHi-alteration experiments, 40 μM di-methyl amiloride (DMA) was added to the medium to produce intracellular acidification, and a Cl--free medium, a high pH (>8.3) medium, or a combination of both, were used for intracellular alkalinization. In preparation for imaging experiments, islets were cultured in RPMI 1640 culture medium supplemented with 10% fetal bovine serum, 100 U/ml penicillin, 0.1 g/L streptomycin and 11 mM glucose.
Secretagogues
In addition to 16.7 mM glucose, the following mitochondrial secretagogues were used to stimulate direct insulin secretion. a) methyl pyruvate (MP), the methylated form of the glycolytic end product of glucose, b) leucine, an amino acid metabolized solely in the mitochondria, c) αKIC, a metabolic product of leucine, and d) 2-amino-bicyclo[2,2,1]heptane-2-carboxylic acid (BCH), a non-metabolizable analog of leucine which enhances TCA cycle activity only through allosteric activation of glutamate dehydrogenase (GDH) [36-38]. None of these compounds are metabolized in the cytosol, and their metabolic effects are exerted solely in the mitochondria. The non-mitochondrial secretagogues used were a) high K+, which directly stimulates insulin secretion through depolarization-induced Ca2+-influx, activating the first phase of insulin release, and b) glucose combined with inhibitors that prohibit the entry of glycolytically-derived pyruvate and NAD(P)H into mitochondria, thus eliminating the mitochondrial component of glucose metabolism while leaving the glycolytic component intact [39]. The inhibitors included α-hydroxycyanocinnamic acid (CHC), an inhibitor of mitochondrial pyruvate transport, and amino-oxy acetic acid (AOA), an inhibitor of the malate aspartate shuttle that transports glycolytic NAD(P)H into mitochondria [39].
Isolation of islets
A modified version of the collagenase digestion method described by Lacy and Kostianovsky [40] was used. Mice were anesthetized with intra-peritoneal injection of Ketamine/Xylazine (80/20 mg/Kg). Pancreas was removed, placed in ice-cold Hanks solution and minced with scissors. Collagenase (3 mg/ml) was added and the mixture shaken in a 37°C water bath until the tissue was adequately digested. The mixture was then centrifuged, supernatant removed and the pellet re-suspended in Hanks solution. Centrifugation and re-suspension were repeated several times to remove exocrine tissue. The final pellet was re-suspended either in basal KRBH medium for secretion experiments or RPMI medium for islet culture. Islets were hand picked under a stereomicroscope.
Culture of islets
The method described by Arkhammar et al. 1998 [41] was used with minor modifications [39,42]. 35 mm culture dishes with glass-bottomed wells (Mat-Tek corporation) were used. The dishes were pre-prepared by coating the wells with human extracellular matrix (BD Biosciences). Freshly isolated islets were placed carefully in each well, covered with RPMI medium containing 11 mM glucose, and cultured at 37°C in 95% O2 and 5% CO2. Under these conditions, the cells in the islet spread out within 14 days, greatly reducing the islet thickness and making it particularly suitable for imaging with confocal microscopy. An advantage of this culture technique is that it does not significantly disrupt islet architecture, thus allowing islet cells to maintain normal functions. Although the islet spreads out over the matrix, islet cells do not separate from each other, and the gap junctions between cells continue to function. Islets cultured for two weeks under these conditions exhibit normal responses of Ca2+, NAD(P)H and insulin release to glucose stimulation [39,41,42], providing an excellent model for imaging studies whose results can be safely extrapolated to fresh islets.
Intracellular pH measurements
The changes in islet pHi produced by each secretagogue and by different pHi-alteration techniques were monitored by confocal microscopy, using carboxy-seminaphthorhodofluor-5 (SNARF5) [35], a pH-sensitive fluorescent indicator. Prior to imaging, cultured islets were maintained in RPMI medium containing 5 mM glucose for 48 hours. On the day of the experiment, RPMI medium was removed, and islets were washed and placed in basal KRBH medium. SNARF5-AM (5 μM final concentration) was added and incubated for one hour at 37°C. Loaded islets were placed on a warmed stage in a humidified and temperature-controlled chamber at 37°C, and monitored with a F-Fluar 40 × 1.3 NA oil immersion lens of a LSM510 confocal laser-scanning microscope (Zeiss). Islets were excited at 514 nm with an argon laser, and the emission fluorescence was collected in the band-widths 568–589 nm and 621–643 nm (peak emission at 580 and 630 nm) using the Meta detector (Zeiss). Time-series images (2.56 μs/pixel) were collected for 5–20 minutes as was suitable for each experiment. A stable baseline was obtained before the actual recording for each experimental condition started. LSM software was used to calculate the ratio between the two emission fluorescence values from selected well-loaded regions in each islet. This ratio was proportional to the islet pHi. The results were analyzed using LSM software, Graphpad Prism, and Microsoft Excel. One representative recording for each experimental condition is shown in the results section, and the value n denotes the number of recordings done with different islets for each condition. The pHi change for each condition is the difference between the average pHi of the baseline and the average pHi over a stable region of the recording after treatment. The pHi changes from n recordings were averaged to obtain the "average pHi change" shown in the results section and in the legend for each figure. A standard curve was prepared by fixing the islet pHi at known values (ranging from 5.5 to 9, with 5–10 islets for each pH), using a KRBH medium containing 100 mM K+ and 20 mM nigericin to equilibrate the pH inside and outside cells.
Secretion measurements
All incubations were done in a 37°C water bath. Freshly isolated islets were pre-incubated for one hour in basal KRBH containing 2.8 mM glucose. Islets were then divided into groups and stimulated with different compounds as indicated in the results section, for one hour. Control group was maintained in basal glucose. At the end of the stimulation period, samples were collected for insulin measurement by radio-immuno-assay (performed by the DRTC Core facility at Vanderbilt University). Islet insulin content was measured after freezing islets overnight in 2% Triton-X. Insulin secretion was expressed as fractional release, i.e. the percentage of total insulin content released over the period of stimulation. In the experiments monitoring TDP, after pre-incubation islets were exposed to high (16.7 mM) glucose with or without intracellular acidification for 40 minutes, while the control group was exposed to basal glucose. Subsequently all groups were rested in basal glucose for 30 minutes, and stimulated with high glucose for one hour prior to collection of samples for insulin assay. The value n denotes the number of times each experiment was repeated using islets from different mice.
Imaging of NAD(P)H
Experiments were performed using TPEM combined with techniques developed in our lab. a) Two-photon fluorescence imaging: Prior to imaging, cultured islets were maintained in RPMI medium containing 5 mM glucose for 24–48 hours. On the day of the experiment, RPMI medium was removed, and islets were washed and placed in basal KRBH medium. Two-photon imaging was done using a Plan-Apochromat 60 × 1.4 NA oil immersion lens of a LSM510 confocal laser-scanning microscope (Zeiss). Islets were kept at 37°C and high humidity using a temperature controlled stage and objective warmer (Zeiss). Sequential images of autofluorescence were collected using 710 nm excitation with a Coherent Mira laser tuned to 710 nm. Each image was collected with a single scan using slow speed (6.4 μs/pixel) and 0.1 μm/pixel. The laser power used provides ~3.5 mW to the surface, at which power no observable damage is caused to the islet [43] even after 60 minutes of continuous imaging [44]. Non-descanned NAD(P)H fluorescence was collected through a custom 380- to 550-nm filter (Chroma). b) Standard Curve: Standard solutions of NADH bound to yeast alcohol dehydrogenase were imaged in deep well slides using live cell data collection settings. This solution closely resembles cellular NAD(P)H since a majority of NAD(P)H is enzyme bound in the cellular environment [45]. NADH was titrated into a solution of ~100 mg/ml alcohol dehydrogenase, 10 mM ethanol, 100 mM isobutyramide, 6 mM semicarbazide, and 10 mM HEPES (pH 9.0). c) Image Analysis: Images were exported in tagged image file format (tiff) for analysis using MetaMorph software (version 5.0). Images were filtered using a 5 × 5 median filter. An intensity threshold was first set in the NAD(P)H image to isolate the bright mitochondria. In each image the maximum intensity from the mitochondrial regions was averaged. This average represents the best average intensity of the in focus mitochondria for the image. A threshold was set on the median filtered image to isolate cytoplasmic NAD(P)H intensity. The low end of this threshold excluded nuclear regions and the high end partially excluded brighter mitochondrial regions. A binary mask was made from the threshold. This mask was then eroded, dilated, and segmented to remove noise pixels in the background regions and generate a number of cytoplasmic regions. These regions were transferred to the median filtered image and the mean intensity of these regions was calculated as the average cytoplasmic NAD(P)H intensity.
Statistical analysis
Values are expressed as mean ± SEM. Groups were compared using paired Student's t test. In secretion studies, n denotes the number of times each experiment was repeated with islets from different mice. In imaging experiments for pHi and NAD(P)H, n denotes the number of islets imaged for each condition.
Results
SNARF5-AM as a pHi-indicator for islets
SNARF5-AM loaded efficiently into a significant portion of the β cell-rich region of each islet, and emitted bright fluorescence when excited at 514 nm. Changes in the emission ratio 630/580 were directly proportional to changes in islet pHi, indicating SNARF5-AM to be a suitable dye to monitor pHi in mouse islets. (Fig. 1). The basal pHi in islets (in KRBH with basal glucose) fell within the range of 6.9–7.2 with an average of 7.09 ± 0.01 (n = 72), and remained stable until additions/changes were made.
Figure 1.
Changes in emission fluorescence of SNARF5, in response to changes in intracellular pH: Islets loaded with SNARF5-AM (5 μM) were fixed at known intracellular pH values by placing them in KRBH solutions containing 100 mM K+ and 20 μM nigericin, adjusted to different pH values. Islets were excited at 514 nm, and emission fluorescence recorded at 580 and 630 nm. Emission fluorescence at 580 and 630 nm are denoted by red and green respectively. Top: Islets at intracellular pH 6, 7, and 8. As pH increases, red fluorescence decreases and green fluorescence increases. Bottom: Standard curve prepared using islets fixed at pHi values ranging from 5.5–9.0. n = 5–10 islets for each pH.
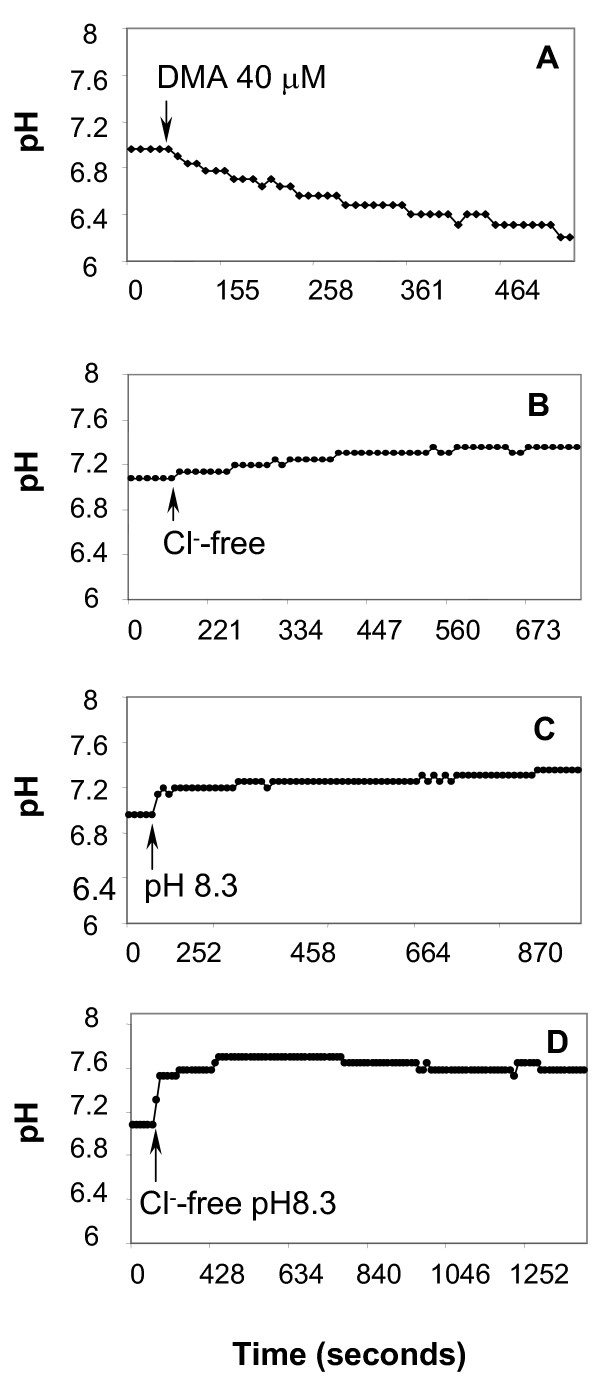
Selecting methods for pHi-alteration
We tested several traditional methods of pHi-alteration, including the addition of weak acids or amiloride derivatives (inhibitors of the Na+/H+ exchanger) for acidification, and addition of weak bases, removal of medium Cl-, or raising the medium pH for intracellular alkalinization. The pHi changes produced by weak acids or bases were sharp but very transient (data not shown), making these methods unsuitable for altering pHi over a long period. In contrast, DMA produced a slow, steady and sustained decrease of pHi, bringing it down by 0.2–1.0 pH units from baseline, with an average decrease of 0.5 ± 0.07 pH units (Fig. 2A). Removal of medium Cl-, or raising the medium pH above 8.3, both produced sustained increases in pHi, but the magnitude of the change was small, ranging from 0.1–0.4 units, with an average increase of 0.3 ± 0.05 and 0.24 ± 0.03, respectively (Fig. 2B &2C). Therefore, none of the traditional pHi-increasing methods appeared suitable for producing a sufficient increase in pHi for one hour. However, combination of the latter two methods, i.e. using a Cl--free high pH medium, proved to be an effective technique for prolonged increase of pHi by 0.3–0.7 units, with an average change of 0.5 ± 0.06. (Fig. 2D)
Figure 2.
Effect on islet pHi by different pH-altering methods: Islets loaded with SNARF5-AM were placed in basal KRBH, excited at 514 nm and emission fluorescence recorded at 580 and 630 nm. After a steady baseline was established, additions/substitutions were made as denoted in each figure. One representative recording for each condition is shown. A. 40 μM DMA: n = 16, average pH change = 0.5 ± 0.07; B. Removal of medium Cl-: n = 5, average pH change = 0.3 ± 0.06; C. Switching to a high pH (>8.3) medium: n= 6, average pH change = 0.24 ± 0.03; D. Switching to a Cl--free and high pH (>8.3) medium: n = 8, average pH change = 0.5 ± 0.06
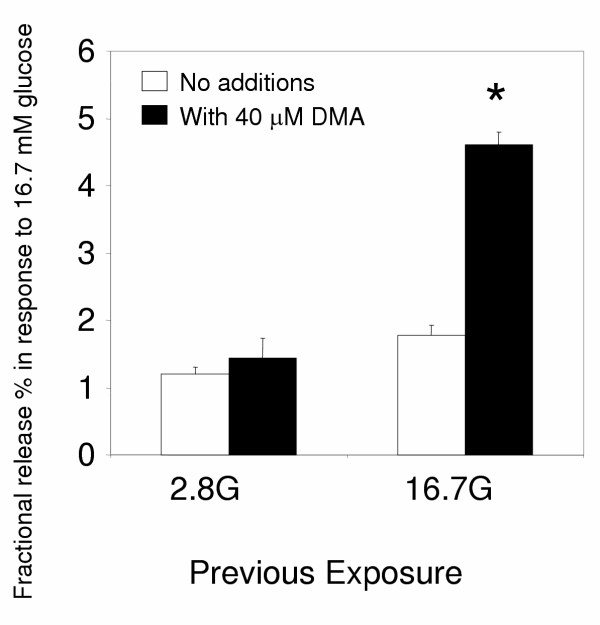
Effect of pHi on glucose-induced TDP
As has been shown before, TDP does not occur in mouse islets [15-17]. Remarkably, glucose induced a strong TDP response in mouse islets in the presence of intracellular acidification by DMA (Fig. 3). In other words, while the secretory response in mouse islets is not normally affected by a previous exposure to glucose, it was greatly magnified when the previous exposure to glucose was combined with lowered pHi. It is noteworthy that the pHi change caused by DMA does not persist once DMA is removed from the medium (data not shown), so that the enhancement of the subsequent secretory response to glucose is caused purely by a memory effect. Since lowering pHi can induce/unmask a secretory function which is normally absent, it is very likely that pHi has a strong influence on direct insulin secretion as well.
Figure 3.
Glucose induces TDP in mouse islets in the presence of DMA: Insulin secretion in response to 16.7 mM glucose, from freshly isolated islets that were previously exposed to different conditions as denoted in the X axis. All groups were first pre-incubated in basal glucose for one hour. During the next 40 minutes, islets were exposed to 2.8 or 16.7 mM glucose with and without 40 μM DMA. Following a subsequent rest period of 30 minutes in basal glucose, all groups were exposed to 16.7 mM glucose for one hour and samples collected for insulin assay. Insulin secretion is expressed as fractional release %, i.e. the percentage of the total insulin content released over the one-hour period of stimulation with 16.7 mM glucose. n = 8; G = mM glucose; * = p < 0.0001, compared with all other groups.
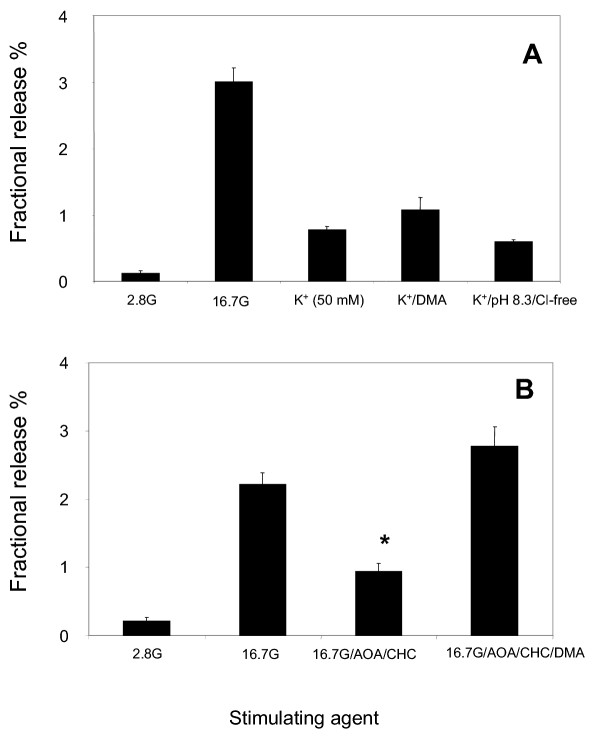
Effect of pHi-alteration on direct insulin secretion by mitochondrial secretagogues, and effect of different mitochondrial fuels on pHi
Previous studies have shown that GSIS is enhanced by intracellular acidification and inhibited by intracellular alkalinization [23-32]. Our preliminary studies confirmed this, and showed that even weak methods of alkalinization (such as removal of medium Cl- or raising the medium pH above 8.3) significantly inhibit GSIS (Fig. 4A).
Figure 4.
Effect of experimental alteration of pHi on direct insulin secretion by mitochondrial secretagogues: Insulin secretion from freshly isolated islets, in response to different secretagogues as indicated, with and without intracellular pH altered. Controls are in 2.8 mM and 16.7 mM glucose, and test groups are in leucine, αKIC or BCH, 20 mM each. Intracellular acidification was produced by 40 μM DMA. Intracellular alkalinization was produced by either a Cl--free medium (A), a high pH (>8.3) medium (A), or a combination of both (B-D). All groups were first pre-incubated in basal glucose for one hour, and subsequently exposed to each condition denoted in the X axes for one hour, followed by sample collection for insulin assay. Insulin secretion is expressed as fractional release %, i.e. the percentage of the total insulin content released over the one-hour period of stimulation with different agents. G = mM glucose; Leu = leucine. A) Glucose: n = 6; * = p < 0.001; and † = p < 0.05, compared to stimulated control in high glucose without pHi-alteration. B) Leucine: n = 5; * = p < 0.001, and † = p < 0.05, compared to leucine without pHi-alteration. C) BCH: n = 5; * = p < 0.001, compared to BCH without pHi-alteration. D) αKIC: n = 8; * = p < 0.001, and † = p < 0.05, compared to αKIC without pHi-alteration.
Among the mitochondrial secretagogues tested, leucine, αKIC (metabolic product of leucine) and BCH (non-metabolizable analog of leucine) all produced significant insulin secretion, to a lesser degree than glucose. As expected, insulin secretion by all these agents showed a strong correlation with pHi. Decrease of pHi by DMA caused a marked increase in the insulin secretion, making the magnitude of the secretory response close to that of glucose. Insulin release by all three agents was significantly inhibited by a strong increase in pHi, as produced by a Cl--free high pH medium (Fig. 4B,4C &4D).
Interestingly, weaker methods of alkalinization were not sufficient to inhibit the insulin release by leucine, KIC and BCH, unlike with glucose (data not shown). This difference can be explained by the direct effect of each nutrient on intracellular pH. As shown in Table 1, glucose produced a significant increase in pHi. This was further increased even by weaker methods of alkalinization, so that high glucose in a high pH medium (Table 1) or Cl--free medium (data not shown) resulted in a prolonged increase of pHi to 7.5 or higher. A high pH medium (Table 1) or Cl--free medium (data not shown) alone was not adequate to produce such a rise in pHi, with or without the presence of other fuels such as leucine, BCH or αKIC. Therefore, while any method of alkalinization combined with glucose can drive the pHi above the range favorable for secretion, weaker methods of alkalinization still maintain the pHi within this favorable range in the presence of other mitochondrial fuels (Table 1). Insulin release by these compounds could be inhibited only when pHi was driven above 7.5 by a Cl--free high pH medium (Fig. 4B,4C &4D).
Table 1.
Islet pHi (mean ± SEM) in the presence of each secretagogue
| Nutrient | In Basal pH medium | In High pH medium |
| Glucose 16.7 mM | 7.32 ± 0.04 | 7.55 ± 0.03 |
| Leucine 20 mM | 7.09 ± 0.03 | 7.23 ± 0.04 |
| BCH 20 mM | 7.06 ± 0.03 | 7.24 ± 0.03 |
| αKIC 20 mM | 6.99 ± 0.02 | 7.18 ± 0.03 |
Islets loaded with SNARF5-AM were placed in KRBH medium of either basal pH (7.4) or high pH (8.3), containing each secretagogue. Islets were excited at 514 nm and emission fluorescence recorded at 580 and 630 nm. Average intracellular pH was calculated over a stable region of each recording, and these values from n recordings were averaged to obtain the pH values shown in the table. n = 10 for glucose; 6 for leucine and BCH; 5 for αKIC.
The inability of pyruvate to stimulate insulin release is puzzling, and has been widely studied [39,46,47]. We used the methylated form of pyruvate (MP), which is known to penetrate cellular membranes better than pyruvate [48-51], as one of the mitochondrial stimulants. In our hands, MP did not stimulate insulin secretion, with or without acidification by DMA (Fig. 5A). Interestingly, MP caused a dramatic and prolonged decrease in pHi (ranging from 0.7–1.7 units from baseline, with an average decrease of 1.0 ± 0.08 pH units), providing a possible explanation for its lack of secretion (Fig. 5B). If the lack of secretion by MP is due to inappropriately low pHi, then a forced increase of pHi should allow it to stimulate insulin release. While the weaker methods of alkalinization were not adequate to reverse the acidifying effect of MP, a Cl--free high pH medium did reverse it, bringing the pH back to the range of 6.4–7.0 (Fig. 5C,5D &5E). As expected, reversing the acidifying effect of MP by a Cl--free high pH medium did allow MP to stimulate significant insulin secretion. (Fig. 5F).
Figure 5.
Insulin secretion and pHi-changes produced by MP: A. MP does not stimulate insulin release, even with intracellular acidification: Insulin secretion in response to 20 mM MP with and without intracellular acidification, from freshly isolated islets. Controls were exposed to 2.8 mM and 16.7 mM glucose. All groups were first pre-incubated in basal glucose for one hour, and subsequently exposed to each condition denoted in the X axis for one hour, followed by sample collection for insulin assay. Insulin secretion is expressed as fractional release %, i.e. the percentage of the total insulin content released over the one-hour period of stimulation with different agents. Intracellular acidification was produced by addition of 40 μM DMA. G = mM glucose. n = 6. B. MP produces a drastic decrease in intracellular pH: Islets loaded with SNARF5-AM were placed in basal KRBH, excited at 514 nm and emission fluorescence recorded at 580 and 630 nm. After a steady baseline was established, 20 mM MP was added where indicated. One representative recording is shown. n = 16; average decrease in pHi = 1.0 ± 0.08. C and D. MP-induced acidification is not affected by traditional methods of alkalinization: Same procedure as in B. Islets were switched to Cl--free medium (C) or high pH (>8.3) medium (D), as indicated, before addition of MP. One representative recording for each condition is shown. C: n = 3; D: n = 4. E. MP-induced acidification is reversed by a Cl--free high pH medium: Islets loaded with SNARF5-AM were placed in Cl--free KRBH of pH above 8.3, excited at 514 nm and emission fluorescence recorded at 580 and 630 nm. 20 mM MP was added where indicated. One representative recording is shown. n = 8. Average pHi in Cl--free high pH medium = 7.5 ± 0.04; Average lowest pHi after addition of MP = 6.1 ± 0.12; Average pHi after recovery = 6.9 ± 0.1; pHi range after recovery = 6.4–7.0 F. MP stimulates insulin secretion when pHi is brought back to 6.4–7.0 by strong alkalinization: Same procedure as in A. Intracellular alkalinization was produced by exposure to a Cl--free high pH (>8.3) medium. G = mM glucose; n = 8; * = p < 0.001, compared to MP without alkalinization or basal glucose control.
Effect of pHi-alteration on direct insulin secretion by non-mitochondrial secretagogues
High K+ causes insulin exocytosis via depolarization-induced Ca2+-influx, and does not involve nutrient metabolism or ATP production. K+-induced insulin secretion was slightly but not significantly enhanced by intracellular acidification, and was not affected by alkalinization (Fig. 6A).
Figure 6.
Effect of experimental alteration of pHi on insulin secretion by non-mitochondrial secretagogues: A. Insulin secretion by high K+ is not significantly influenced by pHi-alteration: Insulin secretion in response 50 mM K+ with and without pHi-alteration techniques (40 μM DMA for acidification and a Cl--free high pH medium for alkalinization) from freshly isolated islets. Control groups were exposed to 2.8 mM and 16.7 mM glucose. All groups were first pre-incubated in basal glucose for one hour, and subsequently exposed to each condition denoted in the X axis for one hour, followed by sample collection for insulin assay. Insulin secretion is expressed as fractional release %, i.e. the percentage of the total insulin content released over the one-hour period of stimulation with different agents. n = 7; G = mM glucose. B. GSIS is inhibited by AOA and CHC. This inhibition is reversed by DMA: Insulin secretion in response to glucose combined with AOA and CHC (5 mM each) in the presence or absence of 40 μM DMA, from freshly isolated islets. All groups were first pre-incubated in basal glucose for one hour, and subsequently exposed to each condition denoted in the X axis for one hour, followed by sample collection for insulin assay. Insulin secretion is expressed as fractional release %, i.e. the percentage of the total insulin content released over the one-hour period of stimulation with different agents. G = mM glucose. n = 5; * = p < 0.001, compared with high glucose alone, or with high glucose with inhibitors and DMA added.
Glucose is converted to a non-miotchondrial secretagogue by combining with the mitochondrial inhibitors AOA and CHC [39]. As expected, the presence of these inhibitors caused a significant reduction in the insulin response by glucose. Remarkably, intracellular acidification by DMA not only reversed this inhibition, but enhanced the insulin secretion further than that produced by glucose alone (Fig. 6B). This suggests that the effect of pHi is not limited to mitochondrially-derived signals, and that extra-mitochondrial signals alone can induce significant insulin secretion when pHi is within the favorable range.
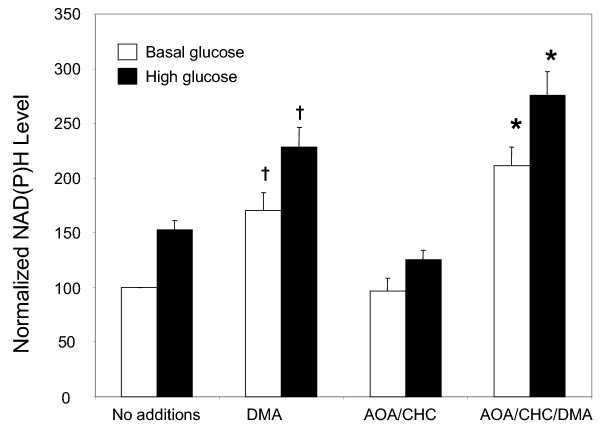
Effect of intracellular acidification on cellular NAD(P)H levels
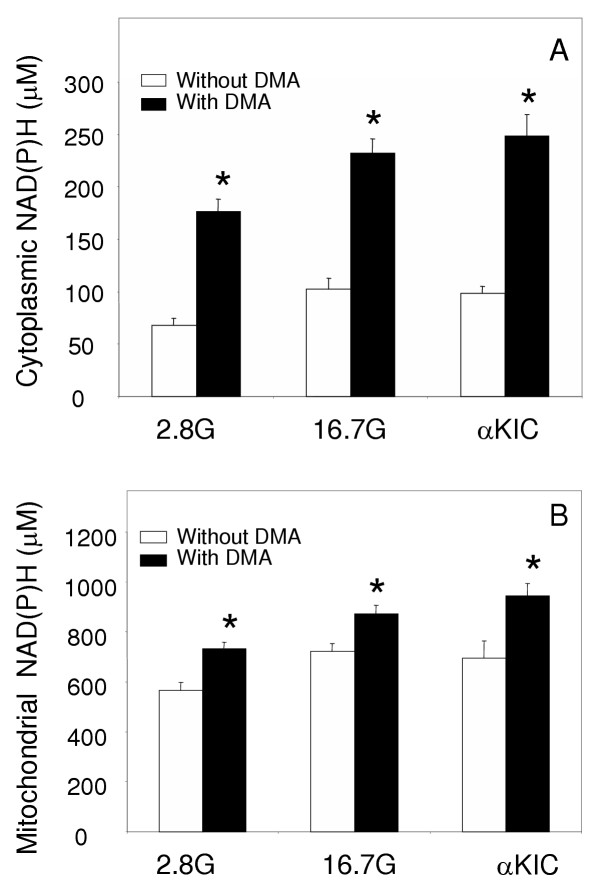
To explore the mechanisms whereby DMA reversed the inhibition of GSIS by AOA and CHC, we monitored insulin secretion and cellular NAD(P)H response in the presence/absence of DMA and the inhibitors. While DMA enables glucose to stimulate insulin release in the presence of inhibitors (Fig. 6B), DMA alone does not stimulate insulin secretion (Fig. 4A). As shown in fig. 7, however, DMA did increase whole cell NAD(P)H levels in all situations tested, including basal or high glucose with and without inhibitors. It is interesting that DMA increased NAD(P)H at basal glucose levels (Open bars: no additions vs. DMA, and AOA/CHC vs. AOA/CHC/DMA). This is likely due to an increase in NADPH rather than NADH, based on the fact that DMA alone does not cause insulin secretion. High glucose induced similar increases in NAD(P)H in the absence or presence of DMA, suggesting that DMA does not stimulate glucose utilization beyond normal. However, when glucose metabolism is inhibited with AOA and CHC, DMA treatment allowed glucose to induce similar changes as those observed in the absence of the inhibitors. This suggests that DMA treatment somehow enables the full utilization of glucose. To further investigate the metabolic effect of low pHi, we looked at the effect of DMA on cytosolic and mitochondrial NAD(P)H levels in the presence and absence of nutrients whose secretory ability is enhanced at low pHi. Both in the presence and absence of nutrients (16.7 mM glucose or 20 mM αKIC), DMA produced a dramatic increase in cytoplasmic NAD(P)H levels (Fig. 8A), and a smaller but significant increase in the mitochondrial NAD(P)H levels (Fig. 8B). Again, glucose-induced increases in the NAD(P)H response (both cytoplasmic and mitochondrial) were of similar magnitude in the absence or presence of DMA.
Figure 7.
DMA increases whole cell NAD(P)H, both in the presence and absence of inhibitors: Islets were placed in basal KRBH with or without mitochondrial inhibitors (AOA and CHC, 5 mM each) and/or 40 μM DMA, and NAD(P)H auto-fluorescence was measured by TPEM before and after addition of 16.7 mM glucose. NAD(P)H auto-fluorescence for each condition is expressed as a percentage of the control (basal glucose with no additions). n = 6; † = p < 0.05 and * = p < 0.002, when compared to the same condition without DMA.
Figure 8.
DMA increases cytoplasmic and mitochondrial NAD(P)H production: Islets were placed in basal KRBH with or without 40 μM DMA. NAD(P)H auto-fluorescence in cytoplasmic (A) and mitochondrial (B) regions was measured by TPEM before and after addition of 16.7 mM glucose or 20 mM αKIC. A. n = 6; * = p < 0.001, compared to same condition without DMA. B. n = 6 ; * = p < 0.05, compared to same condition without DMA.
Discussion
Even though the influence of pHi on GSIS has been known for many years, there is some controversy on the nature of these effects, and little attention has been paid to the mechanisms and physiological implications of such effects. This could be due in part to the lack of accurate methods for monitoring pHi. Previous methods used for measuring pHi include carboxyfluorescein, BCECF, and intracellular microelectrodes. SNARF, a relatively new class of pH indicators, is more suitable due to efficient loading and retention in the cells, as well as being a ratio-metric dye which minimizes variation due to differences in loading or fluctuations of laser intensity. Simple carboxy SNARF-AM esters are particularly suitable for measuring cytosolic pH exclusively, as these compounds, loaded under the current conditions, remain localized in the cytosol. (The more complex carboxy SNARF-calcein-AM form, which accumulates in cellular organelles, is better suited for measuring pH in selected organelles). Carboxy SNARF-AM esters diffuse through the cell membrane and are hydrolyzed by cytosolic esterases, consequently getting trapped in the cytosol with minimal leakage or compartmentalization [52-56]. Recently developed SNARF5 [35], with a pKa of 7.2, is most suitable for monitoring the physiological pHi range (compared to SNARF1 (pKa 7.5), SNARF4 (pKa 6.4) or carboxyfluorescein (pKa 6.5)). In our experiments, SNARF5-AM loaded efficiently into the cultured islets, even though the center of most islets remained largely unstained due to the short loading time. The pHi-calculations were done using regions-of-interest chosen from selected well-loaded areas closer to the center of each islet. Since the interior of mouse islets consists almost entirely of β cells (other cell types being concentrated on the outside) this technique ensured the pH measurements being performed in β cells. Islets loaded with SNARF5 showed consistent visible changes in emission fluorescence proportional to changes of pHi (Fig. 1).
A remarkable finding in this study was that TDP by glucose, a function normally absent in mouse islets, could be induced simply by lowering the pHi with DMA. This indicates that the absence of TDP in mouse islets is not due to lack of the necessary mechanisms, but that these mechanisms are normally inactive, and require the proper pHi range for activation. This finding complements the results of previous studies where a TDP-like function was unmasked in mouse islets by activation of PKC [15,57], and where TDP normally present in rat islets was greatly enhanced by lowering pHi [12]. Since the induction of TDP has been known to correct the secretory defect in certain diabetic patients [2,18,19], it should be worthwhile to explore the therapeutic value of inducing TDP using pHi-lowering drugs combined with non-glucose secretagogues.
In addition to unmasking TDP, decrease of pHi significantly influenced direct insulin release by mitochondrial fuels. DMA produced a fall of islet pHi by 0.2–1.0 pH units, bringing it down from the basal range of 6.9–7.2 to the lower range of 6.4–6.8. All the mitochondrial fuels tested produced strong insulin secretion when the pHi was in this lower range, indicating a below-basal pHi to be optimal for insulin secretion. MP, which failed to produce insulin secretion, presumably due to its strong acidifying effect, could be made to stimulate insulin release by forcing the pHi back to this favorable range (Fig. 5). The magnitude of insulin secretion normally produced by leucine, αKIC and BCH, compounds that produce no significant change in islet pHi, was also greatly enhanced by bringing the pHi to the lower range with DMA (Fig. 4). Furthermore, NSIS was consistently inhibited by raising the pH above 7.5. These results demonstrate that nutrients can produce insulin secretion only within a certain range of islet pHi whose upper margin is 7.5. The lower margin may possibly fall around 6.3, as indicated by the data with MP. The most favorable pHi range for secretion (as well as for unmasking TDP) is near the lower end of this range, between 6.4–6.8, as is the case when MP is combined with a Cl--free high pH medium or when other non-acidifying nutrients are combined with DMA. These results are in agreement with many previous studies that showed a decrease of pHi being associated with enhanced insulin secretion, Ca2+-influx and electrical activity [23-31]. One early study of particular relevance [32] indicated that a below basal pHi is optimal for insulin secretion in rat islets by both glucose and αKIC, but also showed that an increase of extracellular pH up-to 7.8 can enhance insulin secretion. While the latter result appears to differ from our findings, the previous work did not show simultaneous pHi measurements. Since the strong buffering capacity of β cells prevents any significant increase of pHi until the extracellular pH is increased above 8, the reported increase of insulin release likely occurred while the intracellular pH was still within the normal range.
It is known from this and previous studies that mitochondrial fuels alone can stimulate considerable insulin secretion. The magnitude of such insulin release is less than that of glucose, suggesting that mitochondrial metabolism does not produce the full range of secretory signals generated by glucose. However, our secretion data from compounds such as leucine, αKIC and BCH show that mitochondrial activation alone is adequate to produce strong insulin secretion, as long as the pHi is maintained in the appropriate lower range. Similarly, when the mitochondrial component of glucose metabolism is eliminated with AOA and CHC (a situation which normally inhibits GSIS), glucose can still produce the full magnitude of insulin release once the pHi is decreased with DMA. Hence, an appropriate pHi can compensate for those secretory signals that are lacking in each situation, regardless of whether these signals originate in the cytosol or mitochondria. Since carboxy SNARF-AM esters localize in the cytosol with minimal compartmentalization, we expect the current pHi-measurements to principally reflect the cytosolic pH and not that of granules or other organelles. It would, however, be very interesting to see how intragranular pH and intra-mitochondrial pH affects different components of insulin secretion. Manipulating the loading conditions or using different SNARF-AM derivatives can promote compartmentalization of the dye into organelles, but more sophisticated techniques are necessary to distinguish different organelles from each other.
The mechanisms whereby a low pHi enhances or unmasks secretory signals are unclear. Since the depolarization-mediated insulin secretion by high K+ was not significantly affected by pHi-alteration, it is not likely that the distal steps of the secretory pathway are involved. The positive influence of acidification was prominent only on nutrient-derived signals, suggesting enhancement of nutrient metabolism by H+ ions, possibly by activating key metabolic enzymes. Some of the Ca2+-activated mitochondrial dehydrogenases such as α-ketoglutarate dehydrogenase and isocitrate dehydrogenase are activated by low pH [58-61]. Glutamate dehydrogenase, a key enzyme in the insulin secretion produced by BCH and leucine, is also reported to be pH-sensitive [62]. By activating these enzymes, H+ ions may enhance TCA cycle metabolism and increase the production of secretory messengers, thus enhancing the secretory capacity of mitochondrial fuels. An indirect but accurate indication as to whether low pHi enhances cellular metabolism can be obtained by measuring metabolic products such as NADH and NADPH in the presence of nutrients and acidifying agents. As shown in Fig. 8, DMA significantly increases NAD(P)H production, which leads to increased cytoplasmic NAD(P)H even in the absence of stimulatory nutrients. A role for NAD(P)H is further evidenced by the fact that DMA reverses the inhibition of GSIS by AOA and CHC (Fig. 6B), and simultaneously raises NAD(P)H (Fig. 7). However, in spite of the rise in NAD(P)H, DMA does not produce insulin secretion in the absence of a nutrient secretagogue (Fig. 4A). Hence, it is possible that this rise represents NADPH alone, which is insufficient to stimulate secretion, but prepares the cellular environment for better secretion by NADH-producing nutrients [39]. DMA-induced low pHi may either activate NADPH-producing enzymes with acidic pH-optimum, such as GDH [62], or inhibit NADPH-utilizing enzymes with alkaline pH-optimum, such as nitric oxide synthase [63-66]. As shown in previous studies with pyruvate [39], a rise in NADPH alone is not sufficient to stimulate insulin secretion, but can enhance secretion by NADH-generating nutrients. Thus, a decrease in islet pHi activates or "primes" metabolic pathways to generate extra secretory signals so that nutrients can perform their secretory function more efficiently.
The current results show that intracellular pH determines the ability of nutrients to stimulate insulin secretion. This is not surprising, since most biological functions are sensitive to pH and have an optimal range of pH. However, it is remarkable that the optimal pH-range for insulin secretion is on the acidic side, and that a relatively small increase of pH above the physiological range is enough to strongly inhibit NSIS. Therefore, it is possible that a small defect in pHi regulation may cause a significant defect in insulin secretion. This is particularly relevant in NIDDM where islet pHi can decrease below the normal range due to plasma acidosis, or increase above the normal range either through overcompensation for acidosis or due to hyperglycemia. Such a mis-regulation of pHi may well contribute to the secretory defect in NIDDM. Whether or not this is the case, an experimental alteration of pHi to bring it to the optimal range should still improve insulin secretion in defective islets, and merits attention as a potential therapeutic approach.
Conclusions
This study shows that islet pHi is a critical factor that determines the presence and magnitude of different aspects of NSIS in mouse islets. The most favorable pHi for NSIS is below basal, falling between 6.4 and 6.8. Forcing islet pHi to this range a) enables glucose to induce TDP, a function normally absent in mouse islets; b) enhances direct insulin secretion by all mitochondrial secretagogues tested; and c) overcomes the inhibition of GSIS produced by mitochondrial inhibitors. These actions may be mediated through increased nutrient metabolism, as evidenced by the increase of cellular NAD(P)H levels associated with lowered pHi. The favorable effect of below-basal pHi on NSIS, particularly its ability to induce TDP, is of potential therapeutic value for correcting the secretory defect in certain cases of NIDDM.
List of abbreviations
NSIS: nutrient-stimulated insulin secretion; pHi: intracellular pH; TPEM: two-photon excitation microscopy; GSIS: glucose-stimulated insulin secretion; NIDDM: non-insulin dependent diabetes mellitus; KATP channels: ATP-dependent K+ channels; TDP: Time-dependent potentiation; KRBH: HEPES-buffered Krebs Ringer Bicarbonate solution; DMA: di-methyl amiloride; MP: methyl pyruvate; αKIC: alpha-ketoisocaproate; BCH: 2-amino-bicyclo[2,2,1]heptane-2-carboxylic acid; GDH: glutamate dehydrogenase; SNARF5: carboxy-seminaphthorhodofluor-5; CHC: α-hydroxycyanocinnamic acid; AOA: amino-oxy acetic acid.
Competing interests
None declared.
Authors' contributions
SCG designed the study and carried out the insulin secretion experiments and intracellular pH-measurements. JVR performed the NAD(P)H measurements. WSH prepared the cultured islets used in pHi and NAD(P)H measurements. DWP participated in the design and coordination of the study. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
This work was supported by the NIH grants DK42502 and DK53434. Some experiments and data analysis were performed in part through the use of the DRTC Hormone Core Resource and VUMC Cell Imaging Core Resource (supported by NIH grants CA68485, DK20593 and DK58404).
Contributor Information
Subhadra C Gunawardana, Email: subhadra.gunawardana@Vanderbilt.Edu.
Jonathan V Rocheleau, Email: Jon.Rocheleau@Vanderbilt.Edu.
W Steven Head, Email: steven.head@Vanderbilt.Edu.
David W Piston, Email: dave.piston@Vanderbilt.Edu.
References
- Straub SG, Sharp GW. Glucose-stimulated signaling pathways in biphasic insulin secretion. Diabetes Metab Res Rev. 2002;18:451–463. doi: 10.1002/dmrr.329. [DOI] [PubMed] [Google Scholar]
- Nesher R, Cerasi E. Modeling phasic insulin release: immediate and time-dependent effects of glucose. Diabetes. 2002;51:S53–S59. doi: 10.2337/diabetes.51.2007.s53. [DOI] [PubMed] [Google Scholar]
- Henquin JC, Ishiyama N, Nenquin M, Ravier MA, Jonas JC. Signals and pools underlying biphasic insulin secretion. Diabetes. 2002;51:S60–S67. doi: 10.2337/diabetes.51.2007.s60. [DOI] [PubMed] [Google Scholar]
- Nesher R, Cerasi E. Biphasic insulin release as the expression of combined inhibitory and potentiating effects of glucose. Endocrinology. 1987;121:1017–1024. doi: 10.1210/endo-121-3-1017. [DOI] [PubMed] [Google Scholar]
- Cerasi E. Potentiation of insulin release by glucose in man. II. Role of the insulin response, and enhancement of stimuli other than glucose. Acta Endocrinologica. 1975;79:502–510. [PubMed] [Google Scholar]
- Grill V, Rundfeldt M. Effects of priming with D-glucose on insulin secretion from rat pancreatic islets: Increased responsiveness to other secretagogues. Endocrinology. 1979;105:980–987. doi: 10.1210/endo-105-4-980. [DOI] [PubMed] [Google Scholar]
- Gembal M, Gilon P, Henquin JC. Evidence that glucose can control insulin release independently from its action on ATP-sensitive K+ channels in mouse B cells. J Clin Invest. 1992;89:1288–1295. doi: 10.1172/JCI115714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato Y, Aizawa T, Komatsu M, Okada N, Yamada T. Dual functional role of membrane depolarization/Ca2+ influx in rat pancreatic B-cell. Diabetes. 1992;41:438–443. doi: 10.2337/diab.41.4.438. [DOI] [PubMed] [Google Scholar]
- Taguchi N, Aizawa T, Sato Y, Ishihara F, Hashizume K. Mechanism of glucose-induced biphasic insulin release: physiological role of adenosine triphosphate-sensitive K+ channel-independent glucose action. Endocrinology. 1995;136:3942–3948. doi: 10.1210/en.136.9.3942. [DOI] [PubMed] [Google Scholar]
- Komatsu M, Schermerhorn T, Aizawa T, Sharp GWG. Glucose stimulation of insulin release in the absence of extracellular Ca2+ and in the absence of any increase in intracellular Ca2+ in rat pancreatic islets. Proc Natl Acad Sci, USA. 1995;92:10728–10732. doi: 10.1073/pnas.92.23.10728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komatsu M, Schermerhorn T, Noda M, Straub SG, Aizawa T, Sharp GWG. Augmentation of insulin release by glucose in the absence of extracellular Ca2+: New insights into stimulus-secretion coupling. Diabetes. 1997;46:1928–1938. doi: 10.2337/diab.46.12.1928. [DOI] [PubMed] [Google Scholar]
- Gunawardana SC, Sharp GW. Intracellular pH plays a critical role in glucose-induced time-dependent potentiation of insulin release in rat islets. Diabetes. 2002;51:105–113. doi: 10.2337/diabetes.51.1.105. [DOI] [PubMed] [Google Scholar]
- Yamada S, Komatsu M, Aizawa T, Sato Y, Yajima H, Yada T, Hashiguchi S, Yamauchi K, Hashizume K. Time-dependent potentiation of the beta-cell is a Ca2+-independent phenomenon. J Endocrinol. 2002;172:345–354. doi: 10.1677/joe.0.1720345. [DOI] [PubMed] [Google Scholar]
- Grill V, Adamson U, Cerasi E. Immediate and time-dependent effects of glucose on insulin release from rat pancreatic tissue: Evidence for different mechanisms of action. J Clin Invest. 1978;61:1034–1043. doi: 10.1172/JCI109002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zawalich WS, Zawalich KC. Species differences in the induction of time-dependent potentiation of insulin secretion. Endocrinology. 1996;137:1664–1669. doi: 10.1210/en.137.5.1664. [DOI] [PubMed] [Google Scholar]
- Berglund O. Lack of glucose-induced priming of insulin release in the perfused mouse pancreas. J Endocrinol. 1987;114:185–189. doi: 10.1677/joe.0.1140185. [DOI] [PubMed] [Google Scholar]
- Berglund O. Different dynamics of insulin secretion in the perfused pancreas of mouse and rat. Acta Endocrinol. 1980;93:54–60. doi: 10.1530/acta.0.0930054. [DOI] [PubMed] [Google Scholar]
- Cerasi E. Potentiation of insulin release by glucose in man. III. Normal recognition of glucose as a potentiator in subjects with low insulin response and in mild diabetics. Acta Endocrinologica. 1975;79:511–534. doi: 10.1530/acta.0.0790511. [DOI] [PubMed] [Google Scholar]
- Nesher R, Abramovitch E, Cerasi E. Correction of diabetic pattern of insulin release from islets of the spiny mouse (Acomys cahirinus) by glucose priming in vivo. Diabetologia. 1985;28:233–236. doi: 10.1007/BF00282239. [DOI] [PubMed] [Google Scholar]
- Grill V, Efendic S. Loss of priming effect of glucose on A and D cell secretion in perfused pancreas from alloxan-diabetic rats: role of insulin and alloxan. Diabetologia. 1983;24:47–51. doi: 10.1007/BF00275947. [DOI] [PubMed] [Google Scholar]
- Grill V, Rundfeldt M. Abnormalities of insulin responses after ambient and previous exposure to glucose in streptozotocin-diabetic and dexamethazone-treated rats. Role of hyperglycemia and increased B-cell demands. Diabetes. 1986;35:44–51. doi: 10.2337/diab.35.1.44. [DOI] [PubMed] [Google Scholar]
- Nadi AB, Malaisse WJ. Altered metabolic priming by D-glucose in pancreatic islets from Goto-Kakizaki rats. Int J Mol Med. 2000;5:625–629. doi: 10.3892/ijmm.5.6.625. [DOI] [PubMed] [Google Scholar]
- Pace CS. Role of pH as a transduction device in triggering electrical and secretory responses in islet B cells. Federation Proceedings. 1984;43:2379–2384. [PubMed] [Google Scholar]
- Smith JS, Pace CS. Modification of glucose-induced insulin release by alteration of pH. Diabetes. 1983;2:61–66. doi: 10.2337/diab.32.1.61. [DOI] [PubMed] [Google Scholar]
- Pace CS, Tarvin JT, Smith JS. Stimulus-secretion coupling in beta-cells: modulation by pH. Am J Physiol. 1983;244:E3–E18. doi: 10.1152/ajpendo.1983.244.1.E3. [DOI] [PubMed] [Google Scholar]
- Best L, Bone EA, Meats JE, Tomlinson S. Is intracellular pH a coupling factor in nutrient-stimulated pancreatic islets? J Mol Endocrinol. 1988;1:33–38. doi: 10.1677/jme.0.0010033. [DOI] [PubMed] [Google Scholar]
- Best L, Yates AP, Gordon C, Tomlinson S. Modulation by cytosolic pH of calcium and rubidium fluxes in rat pancreatic islets. Biochem Pharmacol. 1988;37:4611–4615. doi: 10.1016/0006-2952(88)90328-0. [DOI] [PubMed] [Google Scholar]
- Best L, Elliot AC. Changes in 2',7'-bis(carboxyethyl) 5'(6')-carboxyflurescein, fura-2 and autofluorescence in intact rat pancreatic islets in response to nutrients and non-nutrients. Mol Cell Endocrinol. 1995;111:191–198. doi: 10.1016/0303-7207(95)03568-R. [DOI] [PubMed] [Google Scholar]
- Sener A, Hutton JC, Kawazu S, Boschero AC, Somers G, Devis G, Herchuelz A, Malaisse WJ. The stimulus-secretion coupling of glucose-induced insulin release; Metabolic and functional effects of NH4+ in rat islets. J Clin Invest. 1978;62:868–878. doi: 10.1172/JCI109199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrun P, Van Ganse E, Juvent M, Deleers M, Herchelz A. Na+-H+ exchange in the process of glucose-induced insulin release from the pancreatic B-cell. Effects of amiloride on 86Rb, 45Ca fluxes and insulin release. Biochim Biophys Acta. 1982;886:448–456. doi: 10.1016/0167-4889(86)90181-3. [DOI] [PubMed] [Google Scholar]
- Lynch AM, Meats JE, Best L, Tomlinson S. Effects of nutrient and non-nutrient stimuli on cytosolic pH in cultured insulinoma (HIT-T15) cells. Biochim Biophys Acta. 1989;1012:166–170. doi: 10.1016/0167-4889(89)90091-8. [DOI] [PubMed] [Google Scholar]
- Hutton JC, Sener A, Herchuelz A, Valverde I, Boschero AC, Malaisse WJ. The stimulus-secretion coupling of glucose-induced insulin release. XLII. Effects of extracellular pH on insulin release: their dependency on nutrient concentration. Horm Metab Res. 1980;12:294–299. doi: 10.1055/s-2007-996274. [DOI] [PubMed] [Google Scholar]
- Lindstrom P, Sehlin J. Effect of intracellular alkalinization on pancreatic islet calcium uptake and insulin secretion. Biochem J. 1986;239:199–204. doi: 10.1042/bj2390199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom P, Sehlin J. Effect of glucose on the intracellular pH of pancreatic islet cells. Biochem J. 1984;218:887–892. doi: 10.1042/bj2180887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Diwu Z, Leung WY. Synthesis and photophysical properties of new fluorinated benzo(c)xanthene dyes as intracellular pH indicators. Bioorg Med Chem Let. 2001;11:2903–2905. doi: 10.1016/S0960-894X(01)00595-9. [DOI] [PubMed] [Google Scholar]
- Sener A, Malaisse WJ. L-leucine and a nonmetabolized analogue activate pancreatic islet glutamate dehydrogenase. Nature (London) 1980;288:187–189. doi: 10.1038/288187a0. [DOI] [PubMed] [Google Scholar]
- Liu Y-J, Cheng H, Drought H, MacDonald MJ, Sharp GWG, Straub SG. Activation of the KATP channel-independent signaling pathway by the non-hydrolysable analog of leucine, BCH. Am J Physiol. 2003;285:E380–E389. doi: 10.1152/ajpendo.00008.2003. [DOI] [PubMed] [Google Scholar]
- Gylfe E. Comparison of the effects of leucines, non-metabolizable leucine analogues and other insulin secretagogues on the activity of glutamate dehydrogenase. Acta diabet Lat. 1976;13:20–24. doi: 10.1007/BF02591577. [DOI] [PubMed] [Google Scholar]
- Rocheleau JV, Head WS, Nicholson WE, Powers AC, Piston DW. Pancreatic islet beta-cells transiently metabolize pyruvate. J Biol Chem. 2002;277:30914–30920. doi: 10.1074/jbc.M202314200. [DOI] [PubMed] [Google Scholar]
- Lacy PE, Kostianovsky M. Method for the isolation of intact islets of Langerhans from the rat pancreas. Diabetes. 1967;16:35–39. doi: 10.2337/diab.16.1.35. [DOI] [PubMed] [Google Scholar]
- Arkhammar POG, Terry BR, Kofod H, Thastrup O. Pancreatic islets cultured on extracellular matrix: An excellent preparation for microfluorometry. Methods Cell Sci. 1998;19:255–268. doi: 10.1023/A:1009712630494. [DOI] [Google Scholar]
- Patterson GH, Knobel SM, Arkhammar P, Thastrup O, Piston DW. Separation of the glucose-stimulated cytoplasmic and mitochondrial NAD(P)H responses in pancreatic islet beta cells. Proc Natl Acad Sci USA. 2000;97:5203–5207. doi: 10.1073/pnas.090098797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett BD, Jetton TL, Ying G, Magnuson MA, Piston DW. Quantitative subcellular imaging of glucose metabolism within intact pancreatic islets. J Biol Chem. 1996;271:3647–3651. doi: 10.1074/jbc.271.7.3647. [DOI] [PubMed] [Google Scholar]
- Piston DW, Knobel SM. Quantitative imaging of metabolism by two-photon excitation microscopy. Methods Enzymol. 1999;307:351–368. doi: 10.1016/S0076-6879(99)07023-8. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Piston DW, Goodman RH. Regulation of corepressor function by nuclear NADH. Science. 2002;295:1895–1897. doi: 10.1126/science.1069300. [DOI] [PubMed] [Google Scholar]
- Sener A, Kawazu S, Hutton JC, Boschero AC, Devis G, Somers G, Herchuelz A, Malaisse WJ. The stimulus-secretion coupling of glucose-induced insulin release. Effect of exogenous pyruvate on islet function. Biochem J. 1978;176:217–232. doi: 10.1042/bj1760217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzen S. Effects of alpha-ketocarboxylic acids and 4-pentenoic acid on insulin secretion from the perfused rat pancreas. Biochem Pharmacol. 1978;27:1321–1324. doi: 10.1016/0006-2952(78)90114-4. [DOI] [PubMed] [Google Scholar]
- Leclercq-Meyer V, Garcia-Martinez JA, Villanueva-Penacarrillo ML, Valverde I, Malaisse WJ. In vitro and in vivo insulinotropic action of methyl pyruvate. Horm Metab Res. 1995;27:477–481. doi: 10.1055/s-2007-980006. [DOI] [PubMed] [Google Scholar]
- Bakkali Nadi A, Zhang TM, Malaisse WJ. Effects of the methyl esters of pyruvate, succinate and glutamate on the secretory response to meglitinide analogues in rat pancreatic islets. Pharmacol Res. 1996;33:191–194. doi: 10.1006/phrs.1996.0026. [DOI] [PubMed] [Google Scholar]
- Malaisse WJ, Jijakli H, Ulusoy S, Cook L, Best L, Vinambres C, Villanueva-Penacarrillo ML, Valverde I, Sener A. Insulinotropic action of methyl pyruvate: secretory, cationic, and biosynthetic aspects. Arch Biochem Biophys. 1996;335:229–244. doi: 10.1006/abbi.1996.0504. [DOI] [PubMed] [Google Scholar]
- Jijakli H, Nadi AB, Cook L, Best L, Sener A, Malaisse WJ. Insulinotropic action of methyl pyruvate: enzymatic and metabolic aspects. Arch Biochem Biophys. 1996;335:245–257. doi: 10.1006/abbi.1996.0505. [DOI] [PubMed] [Google Scholar]
- Muller-Borer BJ, Yang H, Marzouk SAM, Lemasters JJ, Cascio WE. pHi and pHo at different depths in perfused myocardium measured by confocal fluorescence microscopy. Am J Physiol. 1998;275:H1937–H1947. doi: 10.1152/ajpheart.1998.275.6.H1937. [DOI] [PubMed] [Google Scholar]
- Haugland RP. Molecular Probes, Eugene, OR. 5. 1992. Molecular Probes Handbook of Fluorescent Probes and Research Chemicals 1992–1994; p. 129. [Google Scholar]
- Blank PS, Silverman HS, Chung OY, Hogue BA, Stern MD, Hansford RG, Lakatta EG, Capogrossi MC. Cytosolic pH measurements in single cardiac myocytes using carboxy-seminaphthorhodafluor-1. Am J Physiol. 1992;263:H276–H284. doi: 10.1152/ajpheart.1992.263.1.H276. [DOI] [PubMed] [Google Scholar]
- Slayman CL, Moussatos VV, Webb WW. Endosomal accumulation of pH indicator dyes delivered as acetoxymethyl esters. J Exp Biol. 1994;196:419–438. doi: 10.1242/jeb.196.1.419. [DOI] [PubMed] [Google Scholar]
- Wieder ED, Hang H, Fox MH. Measurement of intracellular pH using flow cytometry with carboxy-SNARF-1. Cytometry. 1993;14:916–921. doi: 10.1002/cyto.990140810. [DOI] [PubMed] [Google Scholar]
- Zawalich WS, Zawalich KC, Ganesan S, Calle R, Rasmussen H. Effects of the phorbol ester phorbol 12-myristate 13-acetate on islet-cell responsiveness. Biochem J. 1991;278:49–56. doi: 10.1042/bj2780049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton RM, McCormack JG. The calcium sensitive dehydrogenases of vertebrate mitochondria. Cell Calcium. 1986;7:377–386. doi: 10.1016/0143-4160(86)90040-0. [DOI] [PubMed] [Google Scholar]
- Nichols BJ, Rigoulet M, Denton RM. Comparison of the effects of Ca2+, adenine nucleotides and pH on the kinetic properties of mitochondrial NAD(+)-isocitrate dehydrogenase and oxoglutarate dehydrogenase from the yeast Saccharomyces cerevisiae and rat heart. Biochem J. 1994;303:461–465. doi: 10.1042/bj3030461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YO, Koh HJ, Kim SH, Jo SH, Huh JW, Jeong KS, Lee IJ, Song BJ, Huh TL. Identification and functional characterization of a novel, tissue-specific NAD(+)-dependent isocitrate dehydrogenase beta subunit isoform. J Biol Chem. 1999;274:36866–36875. doi: 10.1074/jbc.274.52.36866. [DOI] [PubMed] [Google Scholar]
- Lowry M, Ross D. Activation of oxoglutarate dehydrogenase in the kidney in response to acute acidosis. Biochem J. 1980;190:771–780. doi: 10.1042/bj1900771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nissim I. Newer aspects of glutamine/glutamate metabolism: the role of acute pH changes. Am J Physiol. 1999;277:F493–F497. doi: 10.1152/ajprenal.1999.277.4.F493. [DOI] [PubMed] [Google Scholar]
- Nakada S, Ishikawa T, Yamamoto Y, Kaneko Y, Nakayama K. Constitutive nitric oxide synthases in rat pancreatic islets: direct imaging of glucose-induced nitric oxide production in beta-cells. Pflugers Arch. 2003;447:305–311. doi: 10.1007/s00424-003-1176-y. [DOI] [PubMed] [Google Scholar]
- Lajoix AD, Reggio H, Chardes T, Peraldi-Roux S, Tribillac F, Roye M, Dietz S, Broca C, Manteghetti M, Ribes G, Wollheim CB, Gross R. A neuronal isoform of nitric oxide synthase expressed in pancreatic beta-cells controls insulin secretion. Diabetes. 2001;50:1311–1323. doi: 10.2337/diabetes.50.6.1311. [DOI] [PubMed] [Google Scholar]
- Yaqoob M, Edelstein CL, Wieder ED, Alkhunaizi AM, Gengaro PE, Nemenoff RA, Schrier RW. Nitric oxide kinetics during hypoxia in proximal tubules: effects of acidosis and glycine. Kidney Int. 1996;49:1314–1319. doi: 10.1038/ki.1996.187. [DOI] [PubMed] [Google Scholar]
- Fleming I, Hecker M, Busse R. Intracellular alkalinization induced by bradykinin sustains activation of the constitutive nitric oxide synthase in endothelial cells. Circ Res. 1994;74:1220–1226. doi: 10.1161/01.res.74.6.1220. [DOI] [PubMed] [Google Scholar]