Summary
“Epimmunome”, a term introduced recently by Swamy and colleagues, describes all molecules and pathways used by epithelial cells (ECs) to instruct immune cells. Today, we know that ECs are among the first sites within the human body to be exposed to pathogens (such as influenza viruses) and that the release of chemokine and cytokines by ECs is influenced by inhaled agents. The role of the ECs as a switchboard to initiate and regulate immune responses is altered through air pollutant exposure, such as ozone, tobacco smoke and diesel exhaust emissions. The details of the interplay between ECs and immune cells are not yet fully understood and need to be investigated further. Co-culture models, cell specific genetically-modified mice and the analysis of human biopsies provide great tools to gain knowledge about potential mechanisms. Increasing our understanding about the role of ECs in respiratory immunity may yield novel therapeutic targets to modulate downstream diseases.
Keywords: epithelial cells, immune response, influenza virus infection, air pollutant
Epithelial cells initiate and regulate immune responses
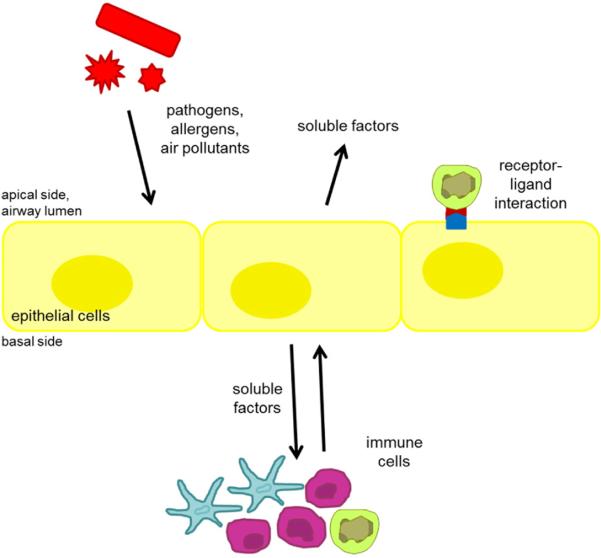
Airway epithelial cells (ECs), either nasal or pulmonary, are among the first sites within the respiratory system to be directly exposed to inhaled environmental stressors, such as air pollutants, pathogens or allergens. ECs are among 40 different cell types that have been identified in the respiratory tract [1]. Some of these cell types (such as neutrophils, dendritic cells (DCs), macrophages, lymphocytes – B cells, T cells, natural killer (NK) cells, etc.) are known to be involved in innate and/or adaptive immune responses [2]. While the importance of other cell types in the context of immune responses has been recognised for many years, only recently has the role of ECs during immune responses been discussed more intensively. Swamy et al. [3] introduced the term “epimmunome” with the goal of identifying “all molecules used by ECs to instruct immune cells” and pointed clearly to the crucial role of ECs during the initiation and regulation of an immune response. In addition, Vareille et al. [4] summarised the important roles of the airway epithelium in the fight against respiratory viruses. The function of airway ECs can be categorised on three different levels (fig. 1): First, ECs play an important barrier function. They provide a level of protection through their tightly organised cellular layer. Each EC is attached to its neighboring cells by cell-cell junctions, including tight junctions, adherens junctions and desmosomes [1, 5–7]. This allows the control of paracellular transport to maintain ionic gradients necessary for the directional secretion of different substances [1, 5–7]. Secondly, ECs are an important source for soluble factors such as chemokines and cy tokines (such as interleukin (IL)-6, IL-8, tumor necrosis factor (TNF)-α, eotaxin, RANTES (regulated on activation normal T cell expressed and secreted), monocyte chemotactic protein (MCP)-1, macrophage inflammatory protein (MIP)-1, interferon gamma-induced protein (IP)-10) [8–12] or lipid mediators (such as prostaglandins) [13] to attract, activate and regulate immune cells as well as neighboring ECs [8, 9, 14–16]. Thirdly, ECs are important during immune responses through the expression of receptors and ligands which directly interact, guide, activate, and regulate other immune cell types. One example is the interaction between ECs and NK cells. NK cells are effector lymphocytes which are important in the context of the early control of viral infections and tumour fighting [17–19]. They patrol the epithelium and kill virus infected cells or transformed tumour cells [20]. In addition to soluble mediators, the activation status of NK cells is controlled by the balance of various inhibitory and activation receptors interacting with ligands expressed on potential target cells [21, 22]. NKG2D, one of the most important activating receptor on NK cells, binds to various ligands, such as MHC class I polypeptide-related sequence (MIC) A, MICB, or UL16-binding proteins (ULBPs), which are expressed on stressed, but not normal airway ECs [23–26]. NKG2D - ligand binding interactions result in the killing of target cells, ultimately leading to the protection of the human body from infected or transformed cells [25].
Figure 1.
Interplay of airway epithelial cells and immune cells. Epithelial cells exposed to pathogens, allergens and air pollutants release soluble factors such as chemokines and cytokines addressing immune cells. Epithelial cells and immune cells also communicate via activating and inhibitory ligand-receptors interactions.
However, more knowledge about the role of ECs during immune responses, especially how they are modified by potential stressors or resident immune cells and how they in turn affect other cells, is necessary. A detailed understanding of the role of ECs could help to develop treatments which use ECs as a therapeutic target and which address diseases downstream of ECs.
In order to further illustrate potential roles of ECs in respiratory immunity, we will use immune responses elicited by influenza infections, the subsequent immune cell type activation, and the roles of ECs as an example. We will provide examples of how inhaled agents alter the EC response in general and especially how factors involved in the immune responses against influenza infection are modulated by air pollutants. Later, we will provide examples of tools to study the role of ECs during respiratory immune responses.
Immune responses against influenza infections – involved cell types
Influenza virions entering the human respiratory tract infect and replicate in ECs. In turn, ECs respond to the infection by synthesising and releasing various cytokines, immunoregulatory molecules and antiviral mediators [27]. Among those, RANTES, MCP-1, IL-8, IL-6 and eotaxin released by ECs recruit and activate immune cells involved in the defense and clearance of the invading virus. Type I interferons (IFNs), produced and released by ECs, induce the synthesis and activity of mediators involved in turning off the viral replication in neighboring ECs and immune cells [10, 27–29]. IFNs produced by ECs activate the JAKSTAT pathway which induces the transcription of IFN stimulated gene (ISG) factor 3 (ISGF3). ISGF3 regulates the expression of various ISGs, such as 2’,5’-oligoadenylate synthetases (OAS), protein kinase R (PKR) and Mx proteins, which mediate viral RNA degradation and block virus replication [10, 30]. As indicated above, among the cell types recruited early during the infection in the upper airways are NK cells [31]. A subset of NK cells (cluster of differentiation (CD)56dimCD16bright cells) is considered to be more cytotoxic and releases granules containing perforin and granzymes, which induce apoptosis in influenza infected cells [32, 33]. Other subsets of NK cells (CD56brightCD16dim or CD56brightCD16-) are less cytotoxic, but secrete more cytokines, such as IFN-γ [34, 35]. However, the classification of different NK cell subsets and their functions is still being developed. Besides NK cells, macrophages and DCs have been identified in the nasal and lower respiratory submucosa [36] and are known to play important roles in the innate immune response to influenza virus infection [37]. Studies in laboratory animals have shown that macrophages are important to limit the viral spread through the phagocytosis of influenza virus-infected cells [38, 39]. Furthermore, human macrophages are known to produce cytokines which are important in the antiviral immune response and play an important role in the regulation of the adaptive immune response [40]. The professional antigen-presenting DCs – usually located underneath the airway epithelium, but above the basal membrane [41, 42] – are crucial in activating T cells. DCs present foreign antigens from infected host cells to fulfill the pivotal task of mobilising both innate and adaptive immune cells by secreting chemokines (such as chemokine (C-X-C motif) ligand (CXCL) 16, MIP-2α, MIP-2β, growth regulated oncogene (GRO) α, IP-10, RANTES) to attract neutrophils, NK cells, cytotoxic and memory T cells to the site of infection [43]. Activated DCs also up-regulate the expression of maturation receptors (such as CD80, CD86, and human leukocytes antigen (HLA)-DR) to aid in antigen presentation and provide co-stimulatory signals to T cells during influenza infection [44]. DCs migrate to peripheral lymph nodes to initiate an adaptive T cell response by activating influenza specific CD4+ and CD8+ T cell clones and supporting clonal expansion of naïve T cells via autocrine IL-2 production [45]. DCs can also enhance T cell responses through production of IFN regulated chemokines such as monokine induced by gamma interferon (MIG), IP-10, and IP-11 to drive a T helper cell type 1 CD4 T cell response and expand activated cytotoxic CD8 T cell pools [45].
EC-dependent modulations of immune cells
ECs modulate neutrophils through the release of chemokines and cytokines which act as chemo-attractants to recruit neutrophils to the airways. Important examples are RANTES, IP-10, IL-1β, IL-6 and IL-8 [10, 27, 43, 46, 47]. Different adhesion molecules expressed on the EC surface guide the neutrophils through the EC layer after they have crossed the endothelial cell layer [48]. Eosinophils are also recruited to the airways and are activated, among others, by factors released by ECs, such as RANTES, eotaxin-1 and eotaxin-2 [49]. NK cells are influenced by ECs through the release of chemokines and cytokines and through direct cell-cell interactions. ECs are a source of IL-8, IL-12, IL-15, IL-18, RANTES, IP-10, MCP-1 and eotaxin-3, which are all important for the trafficking and activation of NK cells [8, 9, 20]. Furthermore, stressed ECs express MICA/B and ULBPs which are ligands for the important activating NK receptor NKG2D [22, 25, 50, 51]. Macrophage recruitment and activation is induced by chemokines and cytokines such as IL-1β, MIP-1α, MCP-1 and TNF-α, which can all be released by ECs [46, 52, 53]. ECs and macrophages also build tight junction [5] and form tight networks together with DCs [54] which allows them to communicate via direct cell-cell interactions. Respiratory DCs lay basolaterally to respiratory ECs in the lamina propria throughout the airways [41, 42]. DCs maintain constant contact with respiratory epithelial cells, and their projections can protrude between the tight junctions of the EC barrier to directly sample the airways for pathogenic antigens [54–56]. DCs are not only influenced by direct cell-cell interactions with ECs, but also by EC-derived mediators, such as type I IFNs [28] or MIP-3α [57]. EC-derived RANTES and IP-10 not only modulate and recruit neutrophils, eosinophils and NK cells, but also T cells. T cell activity is also modulated by type I IFNs released from virus-infected ECs [28].
Inhaled agents which alter EC responses
With every breath about 500 ml air and more than one million particles are inhaled, resulting in a volume of more than 10,000 liters of air and about 300 million inhaled particles per day [58]. Inhaled particles can be grouped into pathogens, allergens and air pollutants (particulate and gaseous). All three types of inhaled agents have significant effects on ECs and also on other cell types in the respiratory mucosa. In this chapter we focus on how air pollutants change the EC responses.
(Diesel) exhaust emissions
Gowdy et al. [59] showed that exposure of mice to diesel exhaust emissions causes an up-regulation of intercellular adhesion molecule (ICAM)-1, TNF-α, MIP-2, IL-6, IFN-γ, IL-13 and an enhanced neutrophil number. Similarly, exposure of respiratory ECs (cell line A549) to diesel exhaust emissions enhances the release of IL-8 and induced cytotoxicity [60]. Exposure of ECs to diesel exhaust emissions prior to infection with influenza in vitro [61] and exposure of human volunteers prior to inoculation of live attenuated influenza virus (LAIV) in vivo enhanced markers of viral replication and IFN-γ [62]. In addition, diesel exhaust emission exposure prior to infection showed an up-regulation of viral replication and IL-6 in mice [63]. In summary, diesel exhaust emissions increase the viral replication in ECs and the release of immune response specific chemokines and cytokines.
Tobacco smoke
Numerous studies have shown that exposure to tobacco smoke modulates respiratory immune responses [64, 65], many of which are initiated and regulated by airway ECs. We have recently demonstrated that human primary nasal ECs from smokers showed increased viral shedding [66] and that viral replication was higher in volunteers exposed to cigarette smoke (both active smokers and secondhand smoke exposed) than in non-smokers [64]. A study by Horvath and colleagues comparing the immune responses elicited by inoculation with LAIV vaccine showed that smoking down-regulated LAIV-induced granzyme B levels and the number of cytotoxic NK cells in nasal lavage, but not in peripheral blood [31].
Ozone (O3)
Recent studies by Kesic et al. [67] showed enhanced viral replication in nasal ECs exposed to O3. Several human and mouse in vivo and in vitro studies have shown that O3 modifies factors involved in immune responses. Song et al. [68] showed increased pro-inflammatory markers and oxidative stress after acute exposure of ECs to O3. Other studies found an enhanced release of pro-inflammatory mediators such as IL-8, MCP-1, MCP-3, RANTES, TNF-α and granulocyte macrophage colony-stimulating factor (GMCSF) [69–73] and this effect was more pronounced in asthmatics compared to non-asthmatics [70, 71]. Interestingly, all of these chemokines are also important for the trafficking of immune cells such as NK cells [8, 9]. Exposure to hydrogen peroxide up-regulates the expression of NK cell ligands on ECs [26], suggesting that exposure to other oxidants, like O3, has the potential to interfere with the direct cell-cell interactions between ECs and NK cell by altering the expression of NK cell ligands, such as MICA/B and ULBP3.
Tools to investigate the role of ECs
In order to gain a better understanding of the role of ECs during respiratory immune responses and how ECs could be used as targets to modulate downstream diseases, various tools can be used. ECs alone in vitro (either cell lines or primary cells) provide an opportunity to estimate how ECs react to a specific inhaled agent and how these reactions can be altered. To investigate how effects on ECs modulate downstream immune responses, it is important to understand cell-cell interactions with other cell types (such as fibroblasts, endothelial cell, DCs, macrophages, NK cells, mast cells, B cells, T cells, etc). Co-culture models have been shown to be a valuable tool for understanding cell-cell interactions. Horvath et al. [74] demonstrated that antiviral defense responses in DCs are different when these cells are co-cultured with ECs from non-smokers and smokers. A study by Bleck et al. [75] investigated the impact of diesel exhaust particle (DEP)-treated ECs on DCs activity using a co-culture system. Phenotypic and functional maturation of DCs was induced by co-culturing with DEP-treated ECs but not by direct stimulation of DCs with DEP treatment of the DCs. Furthermore, conditioned media from DEP-treated ECs functionally matured the DCs [75], suggesting that EC-derived soluble mediators are enhancing DC function. Another study using triple cell co-cultures consisting of the 16HBE14o− bronchial EC line, monocyte-derived DCs, and monocyte-derived macrophages exposed to scooter exhaust emissions, demonstrated changes in immune cell function [76, 77].
In vivo exposure studies using cell type-specific genetically modified mice are another excellent tool to examine the role of ECs in respiratory immune responses. For example, Poynter et al. [78] generated airway EC-targeted transgenic mice expressing a mutant version of the inhibitory protein I-ĸBα which acts to repress the activation of the transcription factor NF-ĸB. In these genetically modified mice, stimulation with lipopolysaccharide resulted in a reduction of neutrophil influx, the secretion of neutrophilic chemokine MIP-2 and pro-inflammatory cytokine TNF-α compared to wildtype mice, suggesting that modifications at the level of epithelial cells mediated these changes.
Besides co-cultures and animal in vivo studies, human nasal or bronchial biopsies are also excellent tools to study the role of ECs and the role of specific EC factors. Hamilton and colleagues [79] used bronchial biopsies to investigate changes in tyrosine phosphorylation in the epithelium of asthmatics. They found an abnormal regulation of protein tyrosine activity in severe asthmatics and hypothesised that tyrosine kinase pathways contribute to persistent, corticosteroid-unresponsive inflammation in severe asthma. Also, several other studies used immunohisto-chemical analyses of human airway biopsies to address questions about the role of ECs in respiratory immune responses [80–83]. Biopsies can also be treated and stained for flow cytometry analysis which allows investigation of other endpoints than immunohistochemistry and can identify changes in immune cell types residing in the respiratory mucosa [84].
Conclusion
Respiratory ECs are among the first targets for inhaled, airborne environmental stressors, such as air pollutants, allergens or pathogens. During viral infections, ECs act as a switchboard to initiate and orchestrate downstream immune responses through the release of chemokines and cytokines, which in turn recruit and activate immune cells. The release of chemokines and cytokines can be changed by the concurrent or prior exposures to air pollutants thus altering immune responses. However, the current understanding about the exact roles of ECs during immune responses, how ECs are affected by inhaled agents, and how these effects in turn modulate immune responses is incomplete at best and needs to be investigated further. In particular, the interplay between ECs and respiratory or even systemic immune cells needs to be better understood so that one day we may be able to potentially use respiratory ECs as targets to modulate downstream immune responses.
Acknowledgments
Funding / potential competing interests: Loretta Müller is supported by the Swiss National Science Foundation with a personal grant. Ilona Jaspers is supported by grants from the National Institutes of Health (ES013611 and HL095163), the Flight Attendant Medical Research Institute (FAMRI), and the Environmental Protection Agency (CR83346301). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Although the research described in this article has been funded in part by the U.S. Environmental Protection Agency through cooperative agreement CR83346301 with the Center for Environmental Medicine, Asthma and Lung Biology at the University of North Carolina-Chapel Hill, it has not been subjected to the agency's required peer and policy review and therefore does not necessarily reflect the views of the agency, and no official endorsement should be inferred. Mention of trade names or commercial products does not constitute endorsement or recommendation for use.
Abbreviations
- CD
Cluster of differentiation
- CXCL
Chemokine (C-X-C motif) ligand
- DC
Dendritic cell
- DEP
Diesel exhaust particles
- EC
Epithelial cell
- GM-CSF
Granulocyte macrophage colony-stimulating factor
- GRO
Growth regulated oncogene
- HLA
Human leukocytes antigen
- ICAM
Intercellular adhesion molecule
- IFN
Interferon
- IL
Interleukin
- IP
Interferon gamma-induced protein 10
- ISG
Interferon stimulated gene
- ISGF3
Interferon stimulated gene factor 3
- LAIV
Live attenuated influenza virus
- MCP
Monocyte chemotactic protein
- MIC
MHC class I polypeptide-related sequence
- MIG
Monokine induced by gamma interferon
- MIP
Macrophage inflammatory protein
- NK
cell Natural killer cell
- O3
Ozone
- OAS
Oligoadenylate synthetases
- RANTES
Regulated on activation normal T cell expressed and secreted
- TNF
Tumor necrosis factor
- ULBP
UL16-binding proteins
References
- 1.Ochs M, Weibel ER. Functional design of the human lung for gas exchange. In: Fishman AP, et al., editors. Fishman's pulmoary diseases and disorders. Mc Graw Hill; New York, NY: 2008. pp. 23–69. [Google Scholar]
- 2.Goldsby RA, Kindt TJ, Osbonre BA, Kuby J. Immunology. 2003;5 [Google Scholar]
- 3.Swamy M, Jamora C, Havran W, Hayday A. Epithelial decision makers: in search of the 'epimmunome'. Nat Immunol. 2010;11(8):656–65. doi: 10.1038/ni.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vareille M, Kieninger E, Edwards MR, Regamey N. The airway epithelium: soldier in the fight against respiratory viruses. Clin Microbiol Rev. 2011;24(1):210–29. doi: 10.1128/CMR.00014-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lehmann AD, Blank F, Baum O, Gehr P, Rothen-Rutishauser BM. Diesel exhaust particles modulate the tight junction protein occludin in lung cells in vitro. Part Fibre Toxicol. 2009;6:26. doi: 10.1186/1743-8977-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneeberger EE, Lynch RD. Tight junctions. Their structure, composition, and function. Circ Res. 1984;55(6):723–33. doi: 10.1161/01.res.55.6.723. [DOI] [PubMed] [Google Scholar]
- 7.Godfrey RW. Human airway epithelial tight junctions. Microsc Res Tech. 1997;38(5):488–99. doi: 10.1002/(SICI)1097-0029(19970901)38:5<488::AID-JEMT5>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 8.Robertson MJ. Role of chemokines in the biology of natural killer cells. J Leukoc Biol. 2002;71(2):173–83. [PubMed] [Google Scholar]
- 9.Walzer T, Vivier E. G-protein-coupled receptors in control of natural killer cell migration. Trends Immunol. 2011;32(10):486–92. doi: 10.1016/j.it.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Sanders CJ, Doherty PC, Thomas PG. Respiratory epithelial cells in innate immunity to influenza virus infection. Cell Tissue Res. 2011;343(1):13–21. doi: 10.1007/s00441-010-1043-z. [DOI] [PubMed] [Google Scholar]
- 11.Brydon EW, Smith H, Sweet C. Influenza A virus-induced apoptosis in bronchiolar epithelial (NCI-H292) cells limits pro-inflammatory cytokine release. J Gen Virol. 2003;84(Pt 9):2389–400. doi: 10.1099/vir.0.18913-0. [DOI] [PubMed] [Google Scholar]
- 12.Adachi M, Matsukura S, Tokunaga H, Kokubu F. Expression of cytokines on human bronchial epithelial cells induced by influenza virus A. Int Arch Allergy Immunol. 1997;113(1–3):307–11. doi: 10.1159/000237584. [DOI] [PubMed] [Google Scholar]
- 13.Goldie RG, Fernandes LB, Farmer SG, Hay DW. Airway epithelium-derived inhibitory factor. Trends Pharmacol Sci. 1990;11(2):67–70. doi: 10.1016/0165-6147(90)90320-8. [DOI] [PubMed] [Google Scholar]
- 14.Rollins BJ. Chemokines. Blood. 1997;90(3):909–28. [PubMed] [Google Scholar]
- 15.Rossi D, Zlotnik A. The biology of chemokines and their receptors. Annual Review of Immunology. 2000;18:217–43. doi: 10.1146/annurev.immunol.18.1.217. [DOI] [PubMed] [Google Scholar]
- 16.Christopherson K, Hromas R. Chemokine regulation of normal and pathologic immune responses. Stem Cells. 2001;19(5):388–96. doi: 10.1634/stemcells.19-5-388. [DOI] [PubMed] [Google Scholar]
- 17.Vivier E, Raulet DH, Moretta A, Caligiuri MA, Zitvogel L, Lanier LL, et al. Innate or adaptive immunity? The example of natural killer cells. Science. 2011;331(6013):44–9. doi: 10.1126/science.1198687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Culley FJ. Natural killer cells in infection and inflammation of the lung. Immunology. 2009;128(2):151–63. doi: 10.1111/j.1365-2567.2009.03167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Connor GM, Hart OM, Gardiner CM. Putting the natural killer cell in its place. Immunology. 2006;117(1):1–10. doi: 10.1111/j.1365-2567.2005.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9(5):503–10. doi: 10.1038/ni1582. [DOI] [PubMed] [Google Scholar]
- 21.Vivier E, Nunes JA, Vely F. Natural killer cell signaling pathways. Science. 2004;306(5701):1517–9. doi: 10.1126/science.1103478. [DOI] [PubMed] [Google Scholar]
- 22.Bryceson YT, March ME, Ljunggren HG, Long EO. Activation, co-activation, and costimulation of resting human natural killer cells. Immunol Rev. 2006;214:73–91. doi: 10.1111/j.1600-065X.2006.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Groh V, Rhinehart R, Randolph-Habecker J, Topp MS, Riddell SR, Spies T. Costimulation of CD8alphabeta T cells by NKG2D via engagement by MIC induced on virus-infected cells. Nat Immunol. 2001;2(3):255–60. doi: 10.1038/85321. [DOI] [PubMed] [Google Scholar]
- 24.Welte SA, Sinzger C, Lutz SZ, Singh-Jasuja H, Sampaio KL, Eknigk U, et al. Selective intracellular retention of virally induced NKG2D ligands by the human cytomegalovirus UL16 glycoprotein. Eur J Immunol. 2003;33(1):194–203. doi: 10.1002/immu.200390022. [DOI] [PubMed] [Google Scholar]
- 25.Obeidy P, Sharland AF. NKG2D and its ligands. Int J Biochem Cell Biol. 2009;41(12):2364–7. doi: 10.1016/j.biocel.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Borchers MT, Harris NL, Wesselkamper SC, Vitucci M, Cosman D. NKG2D ligands are expressed on stressed human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2006;291(2):L222–31. doi: 10.1152/ajplung.00327.2005. [DOI] [PubMed] [Google Scholar]
- 27.Sladkova T, Kostolansky F. The role of cytokines in the immune response to influenza A virus infection. Acta Virol. 2006;50(3):151–62. [PubMed] [Google Scholar]
- 28.Stevens CN, Simeone AM, John S, Ahmed Z, Lucherini OM, Baldari CT, et al. T-cell receptor early signalling complex activation in response to interferon-alpha receptor stimulation. Biochem J. 2010;428(3):429–37. doi: 10.1042/BJ20091660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ciencewicki JM, Brighton LE, Jaspers I. Localization of type I interferon receptor limits interferon-induced TLR3 in epithelial cells. J.Interferon Cytokine Res. 2009;29(5):289–97. doi: 10.1089/jir.2008.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stark GR, Kerr IM, Williams BR, Silverman RH, Schreiber RD. How cells respond to interferons. Annu Rev Biochem. 1998;67:227–64. doi: 10.1146/annurev.biochem.67.1.227. [DOI] [PubMed] [Google Scholar]
- 31.Horvath KM, Herbst M, Zhou H, Zhang H, Noah TL, Jaspers I. Nasal lavage natural killer cell function is suppressed in smokers after live attenuated influenza virus. Respir Res. 2011;12(1):102. doi: 10.1186/1465-9921-12-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagler A, Lanier LL, Cwirla S, Phillips JH. Comparative studies of human FcRIII-positive and negative natural killer cells. J Immunol. 1989;143(10):3183–91. [PubMed] [Google Scholar]
- 33.Lanier LL, Le AM, Civin CI, Loken MR, Phillips JH. The relationship of CD16 (Leu-11) and Leu-19 (NKH-1) antigen expression on human peripheral blood NK cells and cytotoxic T lymphocytes. J Immunol. 1986;136(12):4480–6. [PubMed] [Google Scholar]
- 34.Cooper MA, Fehniger TA, Caligiuri MA. The biology of human natural killer-cell subsets. Trends Immunol. 2001;22(11):633–40. doi: 10.1016/s1471-4906(01)02060-9. [DOI] [PubMed] [Google Scholar]
- 35.Cooper MA, Fehniger TA, Turner SC, Chen KS, Ghaheri BA, Ghayur T, et al. Human natural killer cells: a unique innate immunoregulatory role for the CD56(bright) subset. Blood. 2001;97(10):3146–51. doi: 10.1182/blood.v97.10.3146. [DOI] [PubMed] [Google Scholar]
- 36.Jahnsen FL, Gran E, Haye R, Brandtzaeg P. Human nasal mucosa contains antigen-presenting cells of strikingly different functional pheno-types. Am J Respir Cell Mol Biol. 2004;30(1):31–7. doi: 10.1165/rcmb.2002-0230OC. [DOI] [PubMed] [Google Scholar]
- 37.Kreijtz JH, Fouchier RA, Rimmelzwaan GF. Immune responses to influenza virus infection. Virus Res. 2011;162(1–2):19–30. doi: 10.1016/j.virusres.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 38.Tumpey TM, Garcia-Sastre A, Taubenberger JK, Palese P, Swayne DE, Pantin-Jackwood MJ, et al. Pathogenicity of influenza viruses with genes from the 1918 pandemic virus: functional roles of alveolar macrophages and neutrophils in limiting virus replication and mortality in mice. J Virol. 2005;79(23):14933–44. doi: 10.1128/JVI.79.23.14933-14944.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim HM, Lee YW, Lee KJ, Kim HS, Cho SW, van Rooijen N, et al. Alveolar macrophages are indispensable for controlling influenza viruses in lungs of pigs. J Virol. 2008;82(9):4265–74. doi: 10.1128/JVI.02602-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Becker S, Quay J, Soukup J. Cytokine (tumor necrosis factor, IL-6, and IL-8) production by respiratory syncytial virus-infected human alveolar macrophages. J Immunol. 1991;147(12):4307–12. [PubMed] [Google Scholar]
- 41.Holt PG, Haining S, Nelson DJ, Sedgwick JD. Origin and steady-state turnover of class II MHC-bearing dendritic cells in the epithelium of the conducting airways. J Immunol. 1994;153(1):256–61. [PubMed] [Google Scholar]
- 42.Holt PG, Schon-Hegrad MA. Localization of T cells, macrophages and dendritic cells in rat respiratory tract tissue: implications for immune function studies. Immunology. 1987;62(3):349–56. [PMC free article] [PubMed] [Google Scholar]
- 43.Piqueras B, Connolly J, Freitas H, Palucka AK, Banchereau J. Upon viral exposure, myeloid and plasmacytoid dendritic cells produce 3 waves of distinct chemokines to recruit immune effectors. Blood. 2006;107(7):2613–8. doi: 10.1182/blood-2005-07-2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brimnes MK, Bonifaz L, Steinman RM, Moran TM. Influenza virus-induced dendritic cell maturation is associated with the induction of strong T cell immunity to a coadministered, normally nonimmunogenic protein. J Exp Med. 2003;198(1):133–44. doi: 10.1084/jem.20030266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grayson MH, Holtzman MJ. Emerging role of dendritic cells in respiratory viral infection. J Mol Med (Berl) 2007;85(10):1057–68. doi: 10.1007/s00109-007-0212-3. [DOI] [PubMed] [Google Scholar]
- 46.Message SD, Johnston SL. Host defense function of the airway epithelium in health and disease: clinical background. J Leukoc Biol. 2004;75(1):5–17. doi: 10.1189/jlb.0703315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qiu Y, Zhu J, Bandi V, Guntupalli KK, Jeffery PK. Bronchial mucosal inflammation and upregulation of CXC chemoattractants and receptors in severe exacerbations of asthma. Thorax. 2007;62(6):475–82. doi: 10.1136/thx.2006.066670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zemans RL, Colgan SP, Downey GP. Transepithelial migration of neutrophils: mechanisms and implications for acute lung injury. Am J Respir Cell Mol Biol. 2009;40(5):519–35. doi: 10.1165/rcmb.2008-0348TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gleich GJ. Mechanisms of eosinophil-associated inflammation. J Allergy Clin Immunol. 2000;105(4):651–63. doi: 10.1067/mai.2000.105712. [DOI] [PubMed] [Google Scholar]
- 50.Cosman D, Mullberg J, Sutherland CL, Chin W, Armitage R, Fanslow W, et al. ULBPs, novel MHC class I-related molecules, bind to CMV glycoprotein UL16 and stimulate NK cytotoxicity through the NKG2D receptor. Immunity. 2001;14(2):123–33. doi: 10.1016/s1074-7613(01)00095-4. [DOI] [PubMed] [Google Scholar]
- 51.Biron CA, Nguyen KB, Pien GC, Cousens LP, Salazar-Mather TP. Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu Rev Immunol. 1999;17:189–220. doi: 10.1146/annurev.immunol.17.1.189. [DOI] [PubMed] [Google Scholar]
- 52.See H, Wark P. Innate immune response to viral infection of the lungs. Paediatr Respir Rev. 2008;9(4):243–50. doi: 10.1016/j.prrv.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tao F, Kobzik L. Lung macrophage-epithelial cell interactions amplify particle-mediated cytokine release. American Journal of Respiratory Cell and Molecular Biology. 2002;26(4):499–505. doi: 10.1165/ajrcmb.26.4.4749. [DOI] [PubMed] [Google Scholar]
- 54.Blank F, Rothen-Rutishauser B, Gehr P. Dendritic cells and macrophages form a transepithelial network against foreign particulate antigens. American Journal of Respiratory Cell and Molecular Biology. 2007;36(6):669–77. doi: 10.1165/rcmb.2006-0234OC. [DOI] [PubMed] [Google Scholar]
- 55.Rothen-Rutishauser BM, Kiama SG, Gehr P. A three-dimensional cellular model of the human respiratory tract to study the interaction with particles. Am J Respir Cell Mol Biol. 2005;32(4):281–9. doi: 10.1165/rcmb.2004-0187OC. [DOI] [PubMed] [Google Scholar]
- 56.Jahnsen FL, Strickland DH, Thomas JA, Tobagus IT, Napoli S, Zosky GR, et al. Accelerated antigen sampling and transport by airway mucosal dendritic cells following inhalation of a bacterial stimulus. J Immunol. 2006;177(9):5861–7. doi: 10.4049/jimmunol.177.9.5861. [DOI] [PubMed] [Google Scholar]
- 57.Reibman J, Hsu Y, Chen LC, Bleck B, Gordon T. Airway epithelial cells release MIP-3alpha/CCL20 in response to cytokines and ambient particulate matter. Am J Respir Cell Mol Biol. 2003;28(6):648–54. doi: 10.1165/rcmb.2002-0095OC. [DOI] [PubMed] [Google Scholar]
- 58.Gehr P, Mühlfeld C, Rothen-Rutishauser B, Blank F. Particle-Lung Interactions. In: Gehr P, et al., editors. Lung Biology in Health and Disease. Second Edition. Informa Health; 2010. [Google Scholar]
- 59.Gowdy K, Krantz QT, Daniels M, Linak WP, Jaspers I, Gilmour MI. Modulation of pulmonary inflammatory responses and antimicrobial defenses in mice exposed to diesel exhaust. Toxicol Appl.Pharmacol. 2008;229(3):310–9. doi: 10.1016/j.taap.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 60.de Bruijne K, Ebersviller S, Sexton KG, Lake S, Leith D, Goodman R, et al. Design and testing of Electrostatic Aerosol in Vitro Exposure System (EAVES): an alternative exposure system for particles. Inhal Toxicol. 2009;21(2):91–101. doi: 10.1080/08958370802166035. [DOI] [PubMed] [Google Scholar]
- 61.Jaspers I, Ciencewicki JM, Zhang W, Brighton LE, Carson JL, Beck MA, et al. Diesel exhaust enhances influenza virus infections in respiratory epithelial cells. Toxicol Sci. 2005;85(2):990–1002. doi: 10.1093/toxsci/kfi141. [DOI] [PubMed] [Google Scholar]
- 62.Noah TL, Zhou H, Zhang H, Horvath K, Robinette C, Kesic M, et al. Diesel exhaust exposure and nasal response to attenuated influenza in normal and allergic volunteers. Am J Respir Crit Care Med. 2012;185(2):179–85. doi: 10.1164/rccm.201103-0465OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ciencewicki J, Gowdy K, Krantz QT, Linak WP, Brighton L, Gilmour MI, et al. Diesel exhaust enhanced susceptibility to influenza infection is associated with decreased surfactant protein expression. Inhal Toxicol. 2007;19(14):1121–33. doi: 10.1080/08958370701665426. [DOI] [PubMed] [Google Scholar]
- 64.Noah TL, Zhou H, Jaspers I. Alteration of the nasal responses to influenza virus by tobacco smoke. Curr Opin Allergy Clin Immunol. 2012;12(1):24–31. doi: 10.1097/ACI.0b013e32834ecc80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Arcavi L, Benowitz NL. Cigarette smoking and infection. Arch Intern Med. 2004;164(20):2206–16. doi: 10.1001/archinte.164.20.2206. [DOI] [PubMed] [Google Scholar]
- 66.Jaspers I, Horvath KM, Zhang W, Brighton LE, Carson JL, Noah TL. Reduced expression of IRF7 in nasal epithelial cells from smokers after infection with influenza. Am J Respir Cell Mol Biol. 2010;43(3):368–75. doi: 10.1165/rcmb.2009-0254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kesic MJ, Meyer M, Bauer R, I J. Exposure to ozone modulates human airway protease/antiprotease balance contributing to increased influenza A infection. PLoS ONE. 2012;7(4):e35108. doi: 10.1371/journal.pone.0035108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Song H, Tan W, Zhang X. Ozone induces inflammation in bronchial epithelial cells. J Asthma. 2011;48(1):79–83. doi: 10.3109/02770903.2010.529224. [DOI] [PubMed] [Google Scholar]
- 69.Jaspers I, Flescher E, Chen LC. Ozone-induced IL-8 expression and transcription factor binding in respiratory epithelial cells. Am J Physiol. 1997;272(3 Pt 1):L504–11. doi: 10.1152/ajplung.1997.272.3.L504. [DOI] [PubMed] [Google Scholar]
- 70.Bayram H, Sapsford RJ, Abdelaziz MM, Khair OA. Effect of ozone and nitrogen dioxide on the release of proinflammatory mediators from bronchial epithelial cells of nonatopic nonasthmatic subjects and atopic asthmatic patients in vitro. J Allergy Clin Immunol. 2001;107(2):287–94. doi: 10.1067/mai.2001.111141. [DOI] [PubMed] [Google Scholar]
- 71.Bosson J, Stenfors N, Bucht A, Helleday R, Pourazar J, Holgate ST, et al. Ozone-induced bronchial epithelial cytokine expression differs between healthy and asthmatic subjects. Clin Exp Allergy. 2003;33(6):777–82. doi: 10.1046/j.1365-2222.2003.01662.x. [DOI] [PubMed] [Google Scholar]
- 72.Michalec L, Choudhury BK, Postlethwait E, Wild JS, Alam R, Lett-Brown M, et al. CCL7 and CXCL10 orchestrate oxidative stress-in duced neutrophilic lung inflammation. J Immunol. 2002;168(2):846–52. doi: 10.4049/jimmunol.168.2.846. [DOI] [PubMed] [Google Scholar]
- 73.Nichols BG, Woods JS, Luchtel DL, Corral J, Koenig JQ. Effects of ozone exposure on nuclear factor-kappaB activation and tumor necrosis factor-alpha expression in human nasal epithelial cells. Toxicol Sci. 2001;60(2):356–62. doi: 10.1093/toxsci/60.2.356. [DOI] [PubMed] [Google Scholar]
- 74.Horvath KM, Brighton LE, Zhang W, Carson JL, Jaspers I. Epithelial cells from smokers modify dendritic cell responses in the context of influenza infection 1. American Journal of Respiratory Cell and Molecular Biology. 2010 doi: 10.1165/rcmb.2010-0190OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bleck B, Tse DB, Jaspers I, Curotto de Lafaille MA, Reibman J. Diesel exhaust particle-exposed human bronchial epithelial cells induce dendritic cell maturation. J Immunol. 2006;176(12):7431–7. doi: 10.4049/jimmunol.176.12.7431. [DOI] [PubMed] [Google Scholar]
- 76.Muller L, Comte P, Czerwinski J, Kasper M, Mayer AC, Gehr P, et al. New exposure system to evaluate the toxicity of (scooter) exhaust emissions in lung cells in vitro. Environ Sci Technol. 2010;44(7):2632–8. doi: 10.1021/es903146g. [DOI] [PubMed] [Google Scholar]
- 77.Muller L, Comte P, Czerwinski J, Kasper M, Mayer ACR, Schmid A, et al. Investigating the potential for different scooter and car exhaust emissions to cause cytotoxic and (pro-)inflammatory responses to a 3D in vitro model of the human epithelial airway. Toxicological and Environmental Chemistry. 2012;94(1):164–80. [Google Scholar]
- 78.Poynter ME, Irvin CG, Janssen-Heininger YM. A prominent role for airway epithelial NF-kappa B activation in lipopolysaccharide-induced airway inflammation. J Immunol. 2003;170(12):6257–65. doi: 10.4049/jimmunol.170.12.6257. [DOI] [PubMed] [Google Scholar]
- 79.Hamilton LM, Puddicombe SM, Dearman RJ, Kimber I, Sandstrom T, Wallin A, et al. Altered protein tyrosine phosphorylation in asthmatic bronchial epithelium. Eur Respir J. 2005;25(6):978–85. doi: 10.1183/09031936.05.00098604. [DOI] [PubMed] [Google Scholar]
- 80.Krishna MT, Madden J, Teran LM, Biscione GL, Lau LC, Withers NJ, et al. Effects of 0.2 ppm ozone on biomarkers of inflammation in bronchoalveolar lavage fluid and bronchial mucosa of healthy subjects. Eur Respir J. 1998;11(6):1294–300. doi: 10.1183/09031936.98.11061294. [DOI] [PubMed] [Google Scholar]
- 81.Aris RM, Christian D, Hearne PQ, Kerr K, Finkbeiner WE, Balmes JR. Ozone-induced airway inflammation in human subjects as determined by airway lavage and biopsy. Am Rev Respir Dis. 1993;148(5):1363–72. doi: 10.1164/ajrccm/148.5.1363. [DOI] [PubMed] [Google Scholar]
- 82.Roos-Engstrand E, Wallin A, Bucht A, Pourazar J, Sandstrom T, Blomberg A. Increased expression of p38 MAPK in human bronchial epithelium after lipopolysaccharide exposure. Eur Respir J. 2005;25(5):797–80. doi: 10.1183/09031936.05.00078804. [DOI] [PubMed] [Google Scholar]
- 83.Wilson SJ, Wallin A, Della-Cioppa G, Sandstrom T, Holgate ST. Effects of budesonide and formoterol on NF-kappaB, adhesion molecules, and cytokines in asthma. Am J Respir Crit Care Med. 2001;164(6):1047–52. doi: 10.1164/ajrccm.164.6.2010045. [DOI] [PubMed] [Google Scholar]
- 84.Horvath KM, Brighton LE, Herbst M, Noah TL, Jaspers I. Live Attenuated Influenza Virus (LAIV) induces different mucosal T cell function in nonsmokers and smokers. Clin Immunol. 2012;42(3):232–6. doi: 10.1016/j.clim.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]