ABSTRACT
Endoscopic exploration of the small bowel after pelvic radiation has limitations related to strong abdominal adhesion. It is often difficult to demonstrate the findings of radiation enteritis endoscopically, even with video capsule endoscopy (VCE) or double-balloon enteroscopy (DBE). We present our experience with three cases of radiation enteritis that were diagnosed using VCE and DBE, including their effective aspects. Radiation enteritis has not been diagnosed using conventional methods, and DBE may not accomplish deeper insertion into the ileum, although it is capable of both diagnosis and hemostasis. Therefore, VCE is thought to be the initial tool for the diagnosis of radiation enteritis when small bowel stenosis has not been previously detected and the risk of retention has been discussed.
Key Words: capsule endoscopy, double-balloon enteroscopy, mid-GI bleeding, radiation enteritis, small bowel
INTRODUCTION
Radiation enteritis (RE) usually affects the distal ileum, sigmoid colon and rectum in the field size. This chronic damage is caused by ischemia in the wall of the intestine resulting from a collagenous-vascular lesion,1) and it may sometimes appear as stenosis of the lumen and mid-GI bleeding of unknown origin despite the use of esophagogastroduodenoscopy (EGD) and colonoscopy. In such cases, even if mid-GI bleeding was suspected, endoscopic examination is often difficult because of stenosis and strong adhesion in the pelvis, as in cases of "frozen pelvis",2) which can sometimes embarrass the surgeon.
Video capsule endoscopy (VCE) and double-balloon enteroscopy (DBE) allow the evaluation of the whole small bowel and are now well-established and valuable tools in the diagnostic workup of patients with mid-GI bleeding. However, VCE can involve a major complication, i.e., the retention of the device at the site of a previously unknown small bowel stricture.3) Deep insertion into the ileum with retrograde DBE is sometimes disturbed by abdominal adhesions. In current clinical practice, the gastroenterologist may hesitate to use VCE and DBE to diagnose radiation enteritis given the abovementioned drawbacks.
We have encountered three cases with radiation enteritis that were diagnosed using VCE and DBE. In this report, we present these cases and their effective aspects.
CASE REPORTS
Case 1
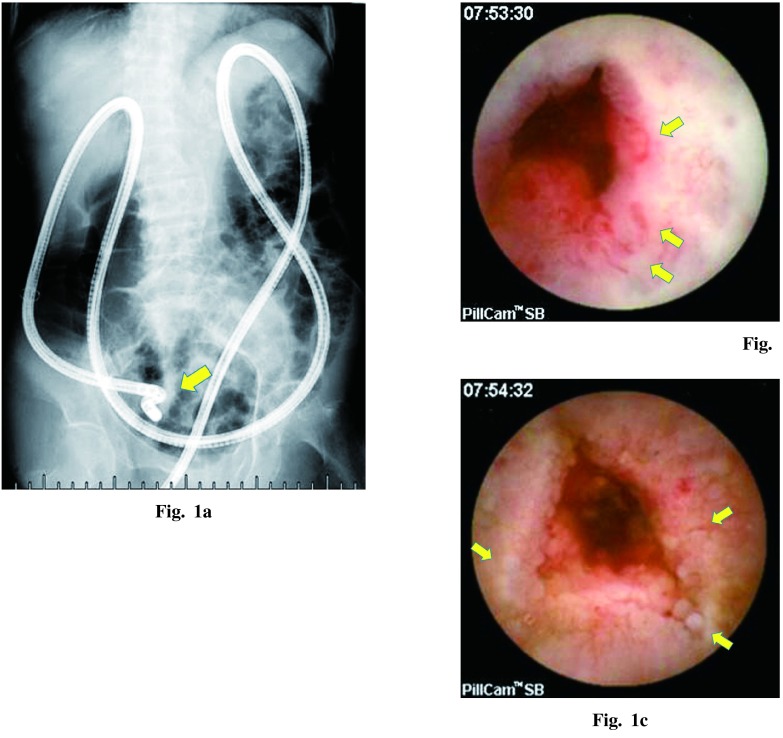
The patient was a 61-year-old woman who developed bloody stool and severe anemia while undergoing dialysis for chronic renal failure. The patient had a past history of cervical cancer of the uterus, which was treated with pelvic radiation therapy. Five years before our encounter, radiation proctitis was found and treated with repeated endoscopic coagulation, but intermittent hematochezia was subsequently observed. RE was suspected, and the patient underwent DBE using oral and anal approaches before the introduction of VCE in our hospital. However, because of strong adhesions, deep insertions were impossible (Figure 1a). Because CT, enteroclysis and DBE did not show stenosis of the small bowel and the bleeding point remained unknown, the patient subsequently underwent VCE, which revealed diffuse ileitis with multiple angioectasias (Figure 1b), circular ulceration scars and erosions based on the atrophic and irregular mucosa with scattered white villi (Figure 1c). RE was diagnosed using VCE, and the patient underwent surgical resection of 120 cm of the ileum. A surgical specimen was compatible with the diagnosis of RE based on the findings of fibrosis and inflammation.
Fig. 1a Fluoroscopic image during retrograde DBE. The endoscope was crooked and was not inserted into the deeper ileum because of pelvic adhesion.
Fig. 1b Multiple angiectasias and fresh blood visualized with VCE.
Fig. 1c VCE indicated rough mucosa, which consisted of atrophic, irregular or scattered white villi.
Case 2
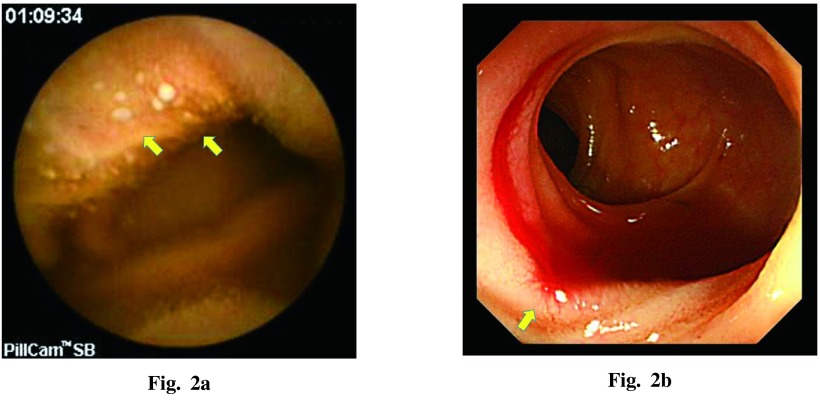
The patient was a 65-year-old woman who was admitted to our hospital for intermittent hematochezia of unknown origin following severe anemia. Although the patient had a history of pelvic radiation therapy, small bowel stenosis was not revealed in previous examinations. She subsequently underwent VCE, which showed multiple angioectasias, based on the atrophic and irregular mucosa with scattered white villi caused by RE (Figure 2a). For rapid treatment, retrograde DBE was performed, but the endoscope could not reach the lesion because of the pelvic adhesion. The subsequent intraoperative endoscopy detected the bleeding vessel in the rough mucosa (Figure 2b), and surgical resection was performed. A surgical specimen was compatible with the diagnosis of RE based on the findings of fibrosis and inflammation.
Fig. 2a VCE indicated scattered white villi.
Fig. 2b The bleeding vessel in the rough mucosa was found using intraoperative endoscopy.
Case 3
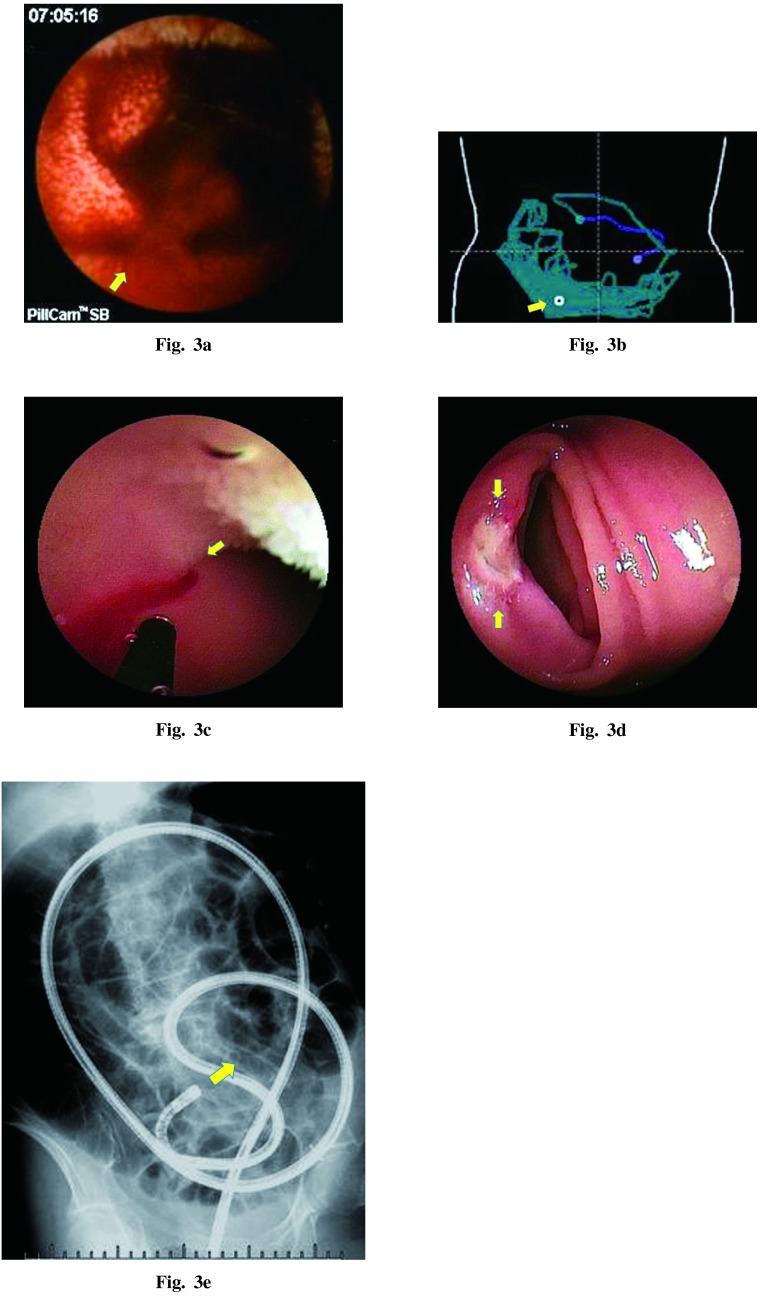
This 74-year-old woman started oral chemotherapy for cervical cancer after undergoing pelvic radiation therapy. One-half year later, she was evaluated for hematochezia and iron deficiency anemia, with an Hb of 5.6 g/dL (reference range 11–16 g/dL). Her EGD results were normal. A colonoscopy showed fresh blood from the oral side in the terminal ileum. Mid-GI bleeding was suspected, and VCE was subsequently performed. VCE revealed fresh blood (Figure 3a b) based on the atrophic and irregular mucosa with scattered white villi in the distal ileum. Subsequent DBE demonstrated active bleeding from the vessel in the distal ileum, and we performed endoscopic heat coagulation (Figure 3c, d, e). Since that treatment, hematochezia has not been seen.
Fig. 3a VCE detected a spouting hemorrhage in the distal ileum.
Fig. 3b The localization map of the bleeding point in the VCE reading software.
Fig. 3c Retrograde DBE accessed the bleeding point that VCE indicated and attempted hemostasis using the heat coagulation device.
Fig. 3d The bleeding was stopped with endoscopic coagulation alone.
Fig. 3e Fluoroscopic image during retrograde DBE. The endoscope was smoothly inserted into the deeper ileum.
DISCUSSION
Endoscopic exploration of the small bowel after pelvic radiation is limited by strong abdominal adhesion, and it is often difficult to demonstrate the findings of RE endoscopically. There have been several reports of successful diagnosis with VCE or DBE,4-7) but this is the first report in which both VCE and DBE were performed without complication and the features of each modality were evident in the RE diagnosis. VCE is able to demonstrate the specific finding of RE but has a high risk of retention when the other examination detects the small bowel stenosis. A patency capsule is recommended to prevent retention in such cases. In comparison, DBE sometimes has the complication of deep insertion in the ileum after pelvic radiation; therefore, the bleeding lesion is not detected, as in our first two cases.
Regarding the histopathological diagnosis of RE, the presence of the characteristic telangiectasias in the intestinal mucosa strongly suggests a possible diagnosis.6) In the present report, VCE revealed angioectasia, redness, erosion and edematous mucosa. Moreover, the most characteristic finding was atrophic and irregular mucosa with scattered white villi. Because VCE can be used to closely observe the mucosa of the small bowel under physiological conditions, it catches abnormalities of the villi more easily and in greater detail compared with DBE, which pushes the villi down with air pressure. In the first two patients, VCE could reveal the central lesion of the injured area, which DBE could not. In addition, VCE could show the location of the lesion using the localization map provided with the software. Although DBE is said to be the gold standard method for small bowel management7) and can be used to discover important small bowel lesions that VCE could miss, we think that RE is among the few disorders (along with small angioectasia) for which VCE may have a greater diagnostic value compared with DBE.8) VCE is feasible for the initial examination of RE because it can prove the presence of the injury itself in a non-invasive manner and suggests the route selection for DBE, showing the location of the lesion. During the course of management, VCE can be performed repeatedly.
In the three patients whose cases are described in this paper, prior examinations did not detect small bowel stenosis, and VCE retention did not occur. However, previous reports indicated VCE retention, and the other examinations did not show small bowel stenosis.9) The wide lumen or thick wall in the local site of the ileum may suggest possible VCE retention, but the risk of retention is often difficult to predict; moreover, it is thought that retention is not related to the treatment period or the interval of radiation therapy according to previous reports.9,10) Thus, in cases in which RE is suspected as the cause of mid-GI bleeding, VCE should be performed, given its effectiveness and the risk of retention using CT or enteroclysis.
In the chronic form of the disease, medical treatment is often ineffective, and surgery is ultimately required to treat complications. Moreover, surgeons have difficulty dealing with the pelvic organs after radiation treatment. Of our three cases that were diagnosed with VCE, two were treated surgically because DBE could not accomplish deep insertion. In our experience, the bleeding from the mucosa that was injured by radiation was not oozing from the entire injured mucosa; rather, it was small arterial bleeding from the small exposed vessels within the mucosa. To treat such bleeding, retrograde DBE should be conducted initially and followed by intraoperative endoscopy when active bleeding from RE is diagnosed with prior VCE, CT or scintigraphy because DBE can complete the hemostasis using a clip or coagulation without laparotomy after pelvic radiation. If vital signs are unstable, angiography is suggested.
In conclusion, RE has not been diagnosed using conventional methods, and DBE may not accomplish deeper insertion into the ileum, although it is capable of both diagnosis and hemostasis. Therefore, VCE is recommended as the initial tool for diagnosing radiation enteritis when small bowel stenosis has not been previously detected and the risk of retention has been discussed.
Abbreviations
- radiation enteritis
(RE)
- esophagogastroduodenoscopy
(EGD)
- video capsule endoscopy
(VCE)
- double-balloon enteroscopy
(DBE)
Footnotes
None of the authors have any financial relationships to disclose that are relevant to this publication.
REFERENCES
- 1).Nguyen NP, Antoine JE. Radiation enteritis. In: Feldman M, Friedman LS, Sleisenger MH, eds. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. Philadelphia: Saunders, 2002. p.1998.
- 2).Mohiuddin M, Marks G. High dose preoperative irradiation for cancer of the rectum, 1976–1988. Int J Radiat Oncol Biol Phys 1991; 20: 37–43. [DOI] [PubMed]
- 3).Cave D, Legnani P, de Franchis R, Lewis BS. ICCE consensus for capsule retention. Endoscopy 2005; 37: 1065–1067. [DOI] [PubMed]
- 4).Kopelman Y, Groissman G, Fireman Z. Radiation enteritis diagnosed by capsule endoscopy. Gastrointest Endosc 2007; 66: 599. [DOI] [PubMed]
- 5).Pasha SF, Harrison ME, Leighton JA. Obscure GI bleeding secondary to radiation enteritis diagnosed and successfully treated with retrograde double-balloon enteroscopy. Gastrointest Endosc 2007; 65: 552–554. [DOI] [PubMed]
- 6).Martínez Ares D, González Conde B, Souto Ruzo J, Vázquez Millán MA, Estévez Prieto E, Alonso Aguirre P, Vázquez Iglesias JL. Obscure gastrointestinal bleeding: a complication of radiation enteritis diagnosed by wireless capsule endoscopy. Rev Esp Enferm Dig 2004; 96: 132–137. [DOI] [PubMed]
- 7).Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A, Ajibe H, Ido K, Sugano K. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol 2004; 2: 1010–1016. [DOI] [PubMed]
- 8).Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small bowel bleeding. Endoscopy 2006; 38: 59–66. [DOI] [PubMed]
- 9).Rogers AM, Kuperman E, Puleo FJ, Shope TR. Intestinal obstruction by capsule endoscopy in a patient with radiation enteritis. JSLS 2008; 12: 85–87. [PMC free article] [PubMed]
- 10).Lee DW, Poon AO, Chan AC. Diagnosis of small bowel radiation enteritis by capsule endoscopy. Hong Kong Med J 2004; 10: 419–421. [PubMed]