ABSTRACT
With the aging of society, osteoporotic thoracolumbar compression fracture is a concern. This fracture occurs occasionally; however, some cases progress to neural compromise due to delayed vertebral body collapse requiring surgery. Surgical treatment and postoperative care are difficult because of patients’ serious comorbidities and poor bone quality, and hence, optimum treatment is not clear, even though some surgical approaches have been reported. There were 35 consecutive patients (5 males and 30 females) with osteoporotic delayed vertebral fractures and associated neurological deficit. Mean age at surgery was 70.7 years (range 60–84 years). Average postoperative follow-up was 3.8 years (range 0.6–11.3 years). All patients experienced a single vertebra collapse, except for 1 with a 2-level collapse of lumbar vertebrae. One thoracic (Th7), 19 thoracolumbar (Th12-L1), and 16 lumbar (L2-5) fractures were treated with combined posterior-anterior surgery. The American Spinal Injury Association (ASIA) impairment scale, activities of daily living (ADL) status, and local sagittal angle were evaluated both before and after surgery. Forty-six percent of all patients showed an improvement of more than 1 grade postoperatively on the ASIA impairment scale, and 74% demonstrated an improvement in ADL status. No deterioration was observed in neurological or ADL status after surgery. With regard to sagittal alignment, preoperative kyphosis of 18.4 degrees was corrected to 2.4 degrees of kyphosis postoperatively. However, 11.5 degrees loss of correction was observed at final follow-up observation. Combined posterior-anterior surgery could provide reliable improvement in both neurological and ADL status, although maintenance of postoperative alignment was difficult to achieve in some cases.
Key Words: osteoporotic vertebral fracture, combined posterior-anterior spine surgery, thoracolumbar spine, spinal instrumentation
INTRODUCTION
Osteoporotic thoracolumbar compression fracture is becoming more common with the aging of the population.1,2) Cases of osteoporotic thoracolumbar compression fracture are usually treated conservatively; however, some cases progress to neural compromise due to delayed vertebral body collapse.1,3) In such cases, surgical treatment is required for the patients to return to their daily activities. Some of the significant clinical challenges when performing surgical treatment of osteoporotic vertebral collapse with neurological deficit are as follows: vertebrae are fragile, patients are elderly, and patients often have serious comorbidities.4) The goals of operative management include performance of decompression to improve neurological deficit, correction of deformity to restore optimum alignment, and arthrodesis to obtain a stable spine. Several treatment options have been reported for treatment of patients with osteoporotic vertebral collapse and neurological deficit.4,5) However, the optimum procedure remains controversial. Some of the most promising options are anterior, posterior, or combined posterior-anterior surgery. Anterior decompression surgery has the advantage of directly decompressing neural elements but may result in further collapse of the vertebral column due to difficulty in obtaining rigid fixation.6,7) Posterior surgery has the advantage of facilitating realignment of the spinal column. However, adequate direct neural decompression cannot be achieved, and unacceptably high failure rates have been reported when traditional short-segment pedicle screw fixation is performed alone.8)
We have been performing combined posterior-anterior surgery to achieve rigid spinal stability while directly decompressing neural elements anteriorly. There are few reports related to this circumferential approach to osteoporotic vertebral collapse. This article reports surgical outcomes of 35 patients with spinal cord and/or cauda equina lesions due to osteoporotic delayed vertebral body collapse; these patients underwent combined posterior-anterior surgery.
MATERIALS AND METHODS
Thirty five consecutive patients (5 males and 30 females) with neurological deficit after osteoporotic vertebral fracture were treated with posterior fixation, followed by anterior decompression and fusion. They were analyzed retrospectively. The mean age of the patients was 70.7 years (range 60–84 years), and the average postoperative follow-up was 3.8 years (range 0.6–11.3 years). Clinical records were reviewed for demographic data, mechanism of injury, operative time, intraoperative blood loss, complications, and improvement in neurological and activities of daily living (ADL) status. Preoperative complications were as follows: rheumatoid arthritis in 6 patients, diabetes mellitus in 5 patients, Parkinson’s disease in 3 patients, brain infarction or hemorrhage in 3 patients, chronic renal failure (requiring hemodialysis) in 1 patient, and ankylosing spinal hyperostosis in 1 patient. Twenty-one patients had a history of low energy injury, 13 patients were injured by a slip, and 1 was injured by a fall from a bed. The mean duration of time from injury to surgery was 6.8 months (range 3–60 months).
Neurological status was graded using the American Spinal Injury Association (ASIA) impairment scale. ADL was classified into the following 4 stages: stage 1, could walk by oneself; stage 2, could walk with help; stage 3, could not walk but could sit by oneself; and stage 4, could not sit by oneself. A single vertebra was collapsed in all patients except for 1 with a 2-level collapse of L1 and L4. One thoracic (Th7), 19 thoracolumbar (Th12-L1), and 16 lumbar (L2-5) fractures were noted.
For posterior internal fixation systems, Texas Scottish Rite Hospital spinal systems (Medtronic Sofamor Danek, USA) were used in all patients. The following were used for anterior reconstruction: an iliac crest graft in 1 patient, a bioactive ceramic (Apatite-wollastonite containing glass ceramic) vertebral prosthesis in 5 patients, a Pyramesh titanium mesh cage (Medtronic Sofamor Danek, USA) in 14 patients, and an expandable strut cage (Syncage-Ex, Synthes Spine) in 15 patients.
Radiographic evaluation was performed in all patients and included analysis of pre- and postoperative local sagittal alignment (LSA), postoperative arthrodesis, and postoperative complications related to instrumentation. LSA was measured from the superior endplate of the intact vertebra cephalad to the fracture and from the inferior endplate of the vertebra caudad to the fracture. Mean preoperative LSA was 18.4 degrees of kyphosis (range 50 degrees of kyphosis to 8 degrees of lordosis). Postoperative bony fusion was evaluated using computed tomography (CT) reconstruction images. Existence of a clear radiolucent zone at the border area was checked on these CT reconstruction images. Disappearance of the clear zone was interpreted as successful fusion.
Surgical procedure
Combined posterior-anterior surgery consisted of posterior fixation using a pedicle screw and hook system, followed by anterior decompression and interbody fusion in the same anesthetic setting. Posterior fixation was performed by placing 2 pedicle screws and 1 hook at 1 level above and 1 level below the injured vertebra in prone position on a Hall frame. Next, the anterior procedure was performed using the retroperitoneal or retropleural approach in the right decubitus position. Lateral and anterior aspects of the injured vertebral body were exposed. The collapsed body, including the posterior wall, was resected subtotally after removal of the discs above and below. Preservation of the endplates while removing the adjacent discs is crucial to prevent postoperative correction loss; therefore, the procedure was performed very carefully. After anterior decompression, anterior interbody fusion was performed using an anterior metal cage filled with cancellous bone chips harvested from the resected rib or iliac crest by monitoring the bone graft. Postoperative treatment An ambulation and rehabilitation program was started on the day of drain removal (usually 2–5 days after surgery). A custom-made plastic thoracolumbosacral orthosis (TLSO) was used for about 3 months. A body cast was used for 4–8 weeks postoperatively in 7 patients whose postural balance was difficult to maintain (e.g., patients with Parkinson’s disease or brain infarction).
RESULTS
The mean operative time was 235.9 min (range 170–405 min) with a mean blood loss of 684.7 mL (range 150–2400 mL). The preoperative ASIA impairment scale rating was C for 11 cases and D for 24 cases. The postoperative ASIA impairment scale rating was C for 5 cases, D for 20 cases, and E for 10 cases. Neurological deterioration was not observed after surgery or during the follow-up period. Sixteen patients (46%) showed postoperative improvement by more than 1 grade on their ASIA impairment scale. (Table 1) Preoperative ADL status was stage 2 for 9 cases, stage 3 for 16 cases, and stage 4 for 10 cases, and postoperative ADL status was stage 1 for 8 cases, stage 2 for 22 cases, stage 3 for 4 cases, and stage 4 for 1 case. Twenty-six patients (74%) showed improvement in ADL status. There was no deterioration in ADL status after surgery. (Table 2)
Table 1.
Change in the ASIA impairment scale: preoperative to postoperative
| Preoperative | Postoperative | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| A | |||||
| B | |||||
| C | 5 | 6 | |||
| D | 14 | 10 | |||
| E | |||||
Table 2.
Change in the ADL stage: preoperative to postoperative
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | |
| Stage 1 | ||||
| Stage 2 | 3 | 6 | ||
| Stage 3 | 2 | 12 | 2 | |
| Stage 4 | 3 | 4 | 2 | 1 |
Mean LSA was 18.4 degrees of kyphosis before surgery, 2.4 degrees of kyphosis immediately after surgery, and 13.5 degrees of kyphosis at final follow-up. At final follow-up, there was 4.9 degrees correction in kyphosis compared to the situation before surgery and 11.5 degrees loss of correction compared to the situation during initial postoperative radiograph. There were no neurological or vascular complications.
Postoperative atelectasis occurred in 5 patients, postoperative pneumonia in 2 patients, postoperative delirium in 2 patients, and upper gastrointestinal hemorrhage in 1 patient. There was deep wound infection in 2 patients and superficial infection of the left iliac crest in 1 patient. One patient’s deep wound infection was surgical site infection; the other patient’s was caused by a bedsore. The patients with deep wound infections required instrumentation removal and revision surgery. One patient underwent revision surgery 3 months after initial surgery because the anterior metal cage was sinking. At final follow-up, solid bone fusion was observed in 34 patients (fusion could not be achieved in a patient on hemodialysis). Sinking of the cage (>5 mm) and screw loosening were detected in 9 and 7 patients, respectively. Subsequent compression fracture after surgery was observed in 9 patients; however, no further surgical treatment was needed, except external fixation with TLSO.
Illustrative case
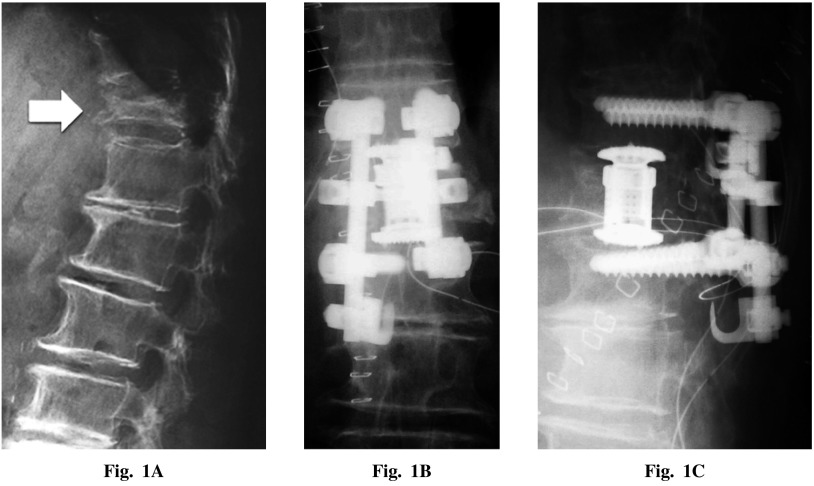
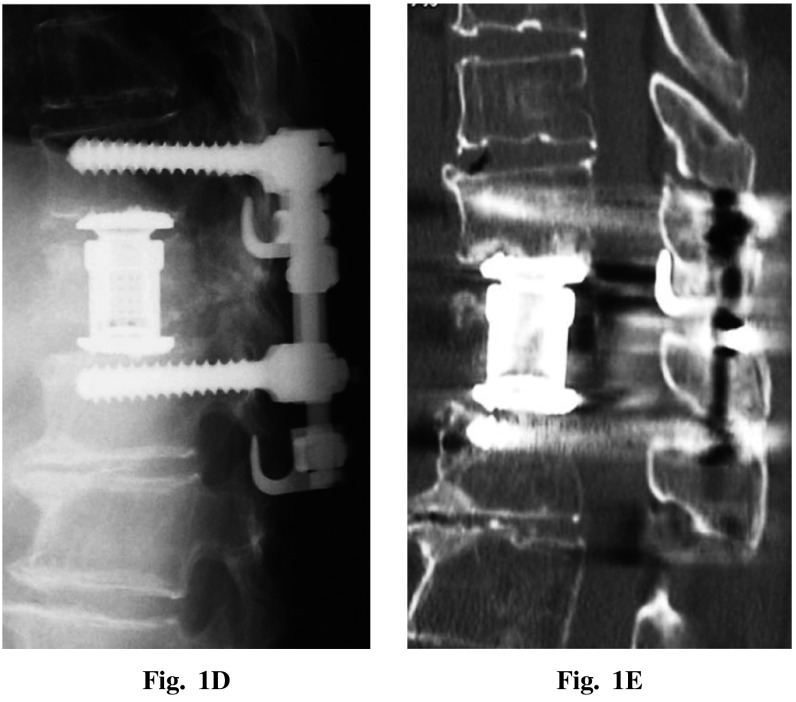
A 74-year-old female sustained a Th12 compression fracture after a fall. She was treated conservatively but she experienced severe backache and bilateral foot drop (MMT 2) 4 months later. Her preoperative ADL status was stage 3. A preoperative radiograph showed comminuted burst fracture of the Th12 vertebra, and the Th11-L1 LSA was 21 degrees of kyphosis. She underwent combined posterior-anterior surgery with an operative time of 221 min and estimated blood loss of 670 mL. Her postoperative LSA was 8 degrees of kyphosis. Three days after surgery, she was ambulatory, wore a hard brace, and returned to her usual daily activities. One-year post surgery, her LSA was 10 degrees of kyphosis and her foot drop improved to MMT 4. She could walk by herself with a cane; her postoperative ADL status improved to stage 2 (Figures 1).
Fig. 1.
A: Preoperative lateral radiograph showed osteoporotic compression fracture at Th12 (white arrow). Postoperative posteroanterior (B) and lateral (C) radiographs. D: Postoperative lateral radiograph taken 1 year post surgery showing no loss of correction. E: Postoperative CT scan taken 1 year post surgery.
DISCUSSION
The purpose of this study was to evaluate the surgical outcome of osteoporotic delayed vertebral fractures with neurological deficit treated with combined posterior-anterior surgery. Results of this study demonstrated that this surgery provided good neurological recovery and improvement of ADL status in most patients postoperatively. However, although we adopted a circumferential approach incorporating various ideas related to surgical technique and implant selection, postoperative loss of sagittal alignment was observed in some cases.
Osteoporotic delayed vertebral collapse has 2 main problems in terms of the surgical procedure: instability of the anterior spinal column and neural compression at the anterior pillar of the spinal column.5) For this reason, anterior decompression and fusion is one of the ideal choices.5) Kaneda et al. developed their original device for anterior stabilization and reported preferable short-term results after surgery in patients with osteoporotic vertebral fracture.5) However, in other reports, it has been recommended that anterior decompression and fusion should not be used alone because of the difficulty in obtaining rigid fixation.6,7,9) In patients with osteoporosis, an anterior vertebral body screw would be insufficient for initial stability because of the fragility of the vertebra.7)
The posterior approach is another major approach. However, in the conventional posterior procedure, it is difficult to achieve complete decompression of the spinal canal.10-12) Moreover, stability of posterior correction and instrumentation is the second major problem. There is evidence that initial correction of the traumatic sagittal plane deformity deteriorates over time in spite of solid posterolateral fusion.8)
Minimally invasive surgeries (i.e., vertebroplasty or kyphoplasty) have recently been of interest for anterior column support. Use of these procedures in combination with posterior short-segment pedicle screw fixation in treatment of acute thoracolumbar fractures has been reported to provide successful outcomes.9,13-15) However, in cases with osteoporosis, it was reported that initial rigid stability could not be achieved and postoperative kyphosis subsequently progressed.16-18) Furthermore, inadequate decompression was possible in patients with neurological deficit, and there was potential for neurological complications due to graft misplacement.19) Thus, the validity of this approach as a surgical treatment option for osteoporotic vertebral fracture has not been established.
To achieve rigid stability in using our combined posterior-anterior surgery approach, several factors were considered when choosing the stabilization technique. With regard to stabilization of posterior elements, pedicle screw pullout strength was highly correlated with bone mineral density,20) and combination of pedicle screw and laminar hooks was considered important to obtain initial rigid stability.21,22) With regard to stabilization of the anterior part, using only iliac crest autograft for anterior column reconstruction might not be sufficient in osteoporosis patients. A titanium cage was used in most cases based on reports indicating that a titanium cage would give more rigid initial stability.23,24) Therefore, a posterior-anterior approach using the pedicle screw and laminar hook combination with a titanium cage theoretically could be an ideal operative strategy for achieving initial fixation stability. However, with this approach, loss of correction by more than 10° was observed postoperatively, and maintenance of postoperative alignment was not achieved in all cases. Notably, loss of correction was large in patients with severe comorbities such as Parkinson’s disease or rheumatoid arthritis.25) Moreover, loss of correction tended to be greater in patients requiring a larger correction angle, such as patients with severe preoperative local kyphosis or vertebral collapse in a lumbar lesion. Because this combined posterior-anterior approach involves short segment fusion, a very large correction angle is not feasible. Thus, an appropriate correction angle could not be achieved using only this approach in those cases. To obtain a larger correction angle, osteotomy or longer fusion is needed. However, these procedures can be more burdensome in older patients due to their invasiveness. Therefore, the necessity of osteotomy or longer fusion must be carefully considered in those severe cases. The operative time and intraoperative blood loss of this combined posterior-anterior surgery were similar to those reported previously for anterior surgery,5,9) and we could use this combined approach even in older patients if the fusion area was sufficiently small. The present study did not compare this approach to other surgical approaches in patients with the same background, and further studies are needed to validate this approach.
CONCLUSION
The combined posterior-anterior surgical approach could provide reliable improvement in both neurological and ADL status in patients with osteoporotic delayed vertebral fracture, and thus, this surgical strategy may be useful for treating these fractures.
Conflict of Interest
Nil
REFERENCES
- 1).Frost H. Clinical management of the symptomatic osteoporotic patient. The Orthopedic clinics of North America, 1981; 12: 671–681. [PubMed]
- 2).Lee Y, Yip KM. The osteoporotic spine. Clinical orthopaedics and related research, 1996; 323: 91–97. [DOI] [PubMed]
- 3).Salomon C, Chopin D, Benoist M. Spinal cord compression: an exceptional complication of spinal osteoporosis. Spine, 1988; 13: 222–224. [PubMed]
- 4).Uchida K, Kobayashi S, Matsuzaki M, Nakajima H, Shimada S, Yayama T, Sato R, Baba H. Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. European Spine Journal, 2006; 15: 1759–1767. [DOI] [PubMed]
- 5).Kaneda K, Asano S, Hashimoto T, Satoh S, Fujiya M. The treatment of osteoporotic-posttraumatic vertebral collapse using the Kaneda device and a bioactive ceramic vertebral prosthesis. Spine, 1992; 17: 295–303. [DOI] [PubMed]
- 6).Starr JK, Hanley Jr EN. Junctional burst fractures. Spine, 1992; 17: 551–557. [DOI] [PubMed]
- 7).Eysel P, Schwitalle M, Oberstein A, Rompe JD, Hopf C, Küllmer K. Preoperative estimation of screw fixation strength in vertebral bodies. Spine, 1998; 23: 174–180. [DOI] [PubMed]
- 8).McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. The Journal of Bone & Joint Surgery, 1993; 75: 162–167. [DOI] [PubMed]
- 9).Sudo H, Ito M, Kaneda K, Abumi K, Kotani Y, Nagahama K, Minami A, Iwasaki N. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. The Spine Journal, 2013. [DOI] [PubMed]
- 10).Hashimoto T, Kaneda K, Abumi K. Relationship between traumatic spinal canal stenosis and neurologic deficits in thoracolumbar burst fractures. Spine, 1988; 13: 1268–1272. [DOI] [PubMed]
- 11).Kostuik JP. Anterior fixation for burst fractures of the thoracic and lumbar spine with or without neurological involvement. Spine, 1988; 13: 286–293. [DOI] [PubMed]
- 12).Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior Decompression and Stabilization with the Kaneda Device for Thoracolumbar Burst Fractures Associated with Neurological Deficits*†. The Journal of Bone & Joint Surgery, 1997; 79: 69–83. [DOI] [PubMed]
- 13).Toyone T, Tanaka T, Kato D, Kaneyama R, Otsuka M. The treatment of acute thoracolumbar burst fractures with transpedicular intracorporeal hydroxyapatite grafting following indirect reduction and pedicle screw fixation: a prospective study. Spine, 2006; 31: E208-E214. [DOI] [PubMed]
- 14).Korovessis P, Hadjipavlou A, Repantis T. Minimal invasive short posterior instrumentation plus balloon kyphoplasty with calcium phosphate for burst and severe compression lumbar fractures. Spine, 2008; 33: 658–667. [DOI] [PubMed]
- 15).Uchida K, Nakajima H, Yayama T, Miyazaki T, Hirai T, Kobayashi S, Chen K, Guerrero AR, Baba H. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery: Clinical article. Journal of Neurosurgery: Spine, 2010; 13: 612–621. [DOI] [PubMed]
- 16).Matsuyama Y, Goto M, Yoshihara H, Tsuji T, Sakai Y, Nakamura H, Sato K, Kamiya M, Ishiguro N. Vertebral reconstruction with biodegradable calcium phosphate cement in the treatment of osteoporotic vertebral compression fracture using instrumentation. Journal of spinal disorders & techniques, 2004; 17: 291–296. [DOI] [PubMed]
- 17).Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine, 1991; 16: 1335–1341. [DOI] [PubMed]
- 18).Lotz JC, Hu SS, Chiu DF, Yu M, Colliou O, Poser RD. Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine, 1997; 22: 2716–2723. [DOI] [PubMed]
- 19).Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine, 2001; 26: 88–99. [DOI] [PubMed]
- 20).Halvorson TL, Kelley LA, Thomas KA, Whitecloud III TS, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine, 1994; 19: 2415–2420. [DOI] [PubMed]
- 21).Hasegawa K, Takahashi HE, Uchiyama S, Hirano T, Hara T, Washio T, Sugiura T, Youkaichiya M, Ikeda M. An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine, 1997; 22: 958–962. [DOI] [PubMed]
- 22).Chiba M, McLain RF, Yerby SA, Moseley TA, Smith TS, Benson DR. Short-segment pedicle instrumentation: biomechanical analysis of supplemental hook fixation. Spine, 1996; 21: 288–294. [DOI] [PubMed]
- 23).Hoshijima K, Nightingale RW, Jim RY, Richardson WJ, Harper KD, Yamamoto H, Myers BS. Strength and stability of posterior lumbar interbody fusion: Comparison of titanium fiber mesh implant and tricortical bone graft. Spine, 1997; 22: 1181–1188. [DOI] [PubMed]
- 24).Hasegawa K, Abe M, Washio T, Hara T. An experimental study on the interface strength between titanium mesh cage and vertebra in reference to vertebral bone mineral density. Spine, 2001; 26: 957–963. [DOI] [PubMed]
- 25).Nakashima H, Yukawa Y, Ito K, Horie Y, Machino M, Kato F. Combined posteroanterior surgery for osteoporotic delayed vertebral fracture and neural deficit in patients with Parkinson’s disease. Orthopedics, 2009; 32. [DOI] [PubMed]