ABSTRACT
A 67-year-old man fell from the second floor of his home and was impaled on an iron pipe used for a garden stake. The pipe was 2 cm in diameter and had entered his left buttock to his anus. A plain abdominal X-ray film showed that the tip of the pipe was located in front of the 4th lumbar vertebra, so the penetration distance was 30 cm. An emergency operation was performed for hemorrhagic shock. Laparotomy revealed massive intra-abdominal bleeding, injuries of the sigmoid and transverse mesocolon, superior rectal artery, and the first part of the duodenum. Because of suspected lower rectal injury, division of the upper rectum, closure of the rectal stump, and sigmoidostomy were performed. Gauze packing into the pelvic cavity was performed for uncontrollable bleeding. All the gauze was postoperatively removed from the drain wound without laparotomy. Six months after the operation, he underwent a second operation including anastomosis of the descending colon and lower rectum, which allowed him to live a normal daily life.
Key Words: Impalement injury, Falling accident, Massive bleeding
INTRODUCTION
Impalement injury is a specific type of trauma that is usually associated with crush injury, wound contamination, and injury to the deep organs. It is likely to result in bleeding, organ dysfunction, and infection. So its treatment has some difficulties for surgeons. This case is a successfully treated impalement injury to the buttocks with massive bleeding and duodenal perforation by a fall.
CASE REPORT
A 67-year-old man fell from the second floor of his home and was admitted our hospital after being impaled on an iron pipe that he had used for a garden stake. The pipe was 2 cm in diameter and had entered his left buttock to his anus. He was conscious, his blood pressure was 142/68, and his pulse rate was 52/min. On arrival, focused assessment with sonography for trauma as a primary survey was negative. His APACHE-II score and SOFA score were 11 points and 5 points, respectively. A plain abdominal X-ray film revealed that the tip of the pipe was located in front of the 4th lumbar vertebra, so the penetration distance was 30 cm (Fig. 1). It took 60 minutes for the primary survey. Computed tomography for the secondary survey showed that the pipe was located between the urinary bladder and the rectum (Fig. 2), with fluid and free air in the abdominal cavity. Laboratory findings were as follows: white blood cell count of 12,300/μl, hemoglobin of 11.7 g/dl, and amylase of 96 IU/L. It took about 40 minutes for the secondary survey. About 100 minutes after admission, he fell into hemorrhagic shock and an emergency operation was performed. Laparotomy showed massive bleeding in the abdominal cavity. The pipe had penetrated through the sigmoid mesocolon without causing injury to the aorta, inferior vena cava, and iliac vessels. It was carefully removed from the buttock wound (Fig. 3). We found that the superior rectal artery was torn, so it was ligated. While removing the intra-abdominal blood, careful inspection of the abdominal cavity revealed a tear of the transverse mesocolon and a 3 cm laceration of the first part of the duodenum, so the duodenal wall was sutured. According to these intraoperative findings, it was estimated that the pipe had entered the abdomen through the ischiorectal fossa between the urinary bladder and the rectum, penetrated the sigmoid and transverse mesocolon into the omental bursa, and then injured the duodenum without causing pancreatic injury (Fig. 4). Because of suspected lower rectal injury, we performed resection of the upper rectum, closure of the rectal stump, and sigmoidostomy. Four drain tubes were introduced into the omental bursa, Morrison’s pouch, and pelvic cavity (1, 1, and 2 tubes, respectively). Because it was impossible to control bleeding from the sacral surface, 20 pieces of gauze were tied together and packed into the pelvic cavity, with the ends of the tied gauzes being placed into the buttock wound along with a pelvic drain tube. Then the pelvic peritoneum was sutured to isolate the abdominal cavity from the pelvic cavity. The operating time was 195 minutes and total blood loss was 3,720 g. Intravenous dose of 1 g of cefmetazole was administered just before the surgery and the same dose was given twice a day for 5 days. His postoperative course was uneventful; hemodynamics were stable, anemia did not occur, and discharge from the drain tubes was serous or weakly bloody. Six pieces of gauze were removed from the drain wound without bleeding on the 6th postoperative day, while the other gauzes were pulled out from the pelvic cavity on the 8th and 9th postoperative days. Prolonged hospitalization was required for wound healing, and he was discharged on the 65th postoperative day. Six months after the operation, he underwent a second operation including anastomosis of the descending colon and lower rectum, which allowed him to live a normal daily life.
Fig. 1.
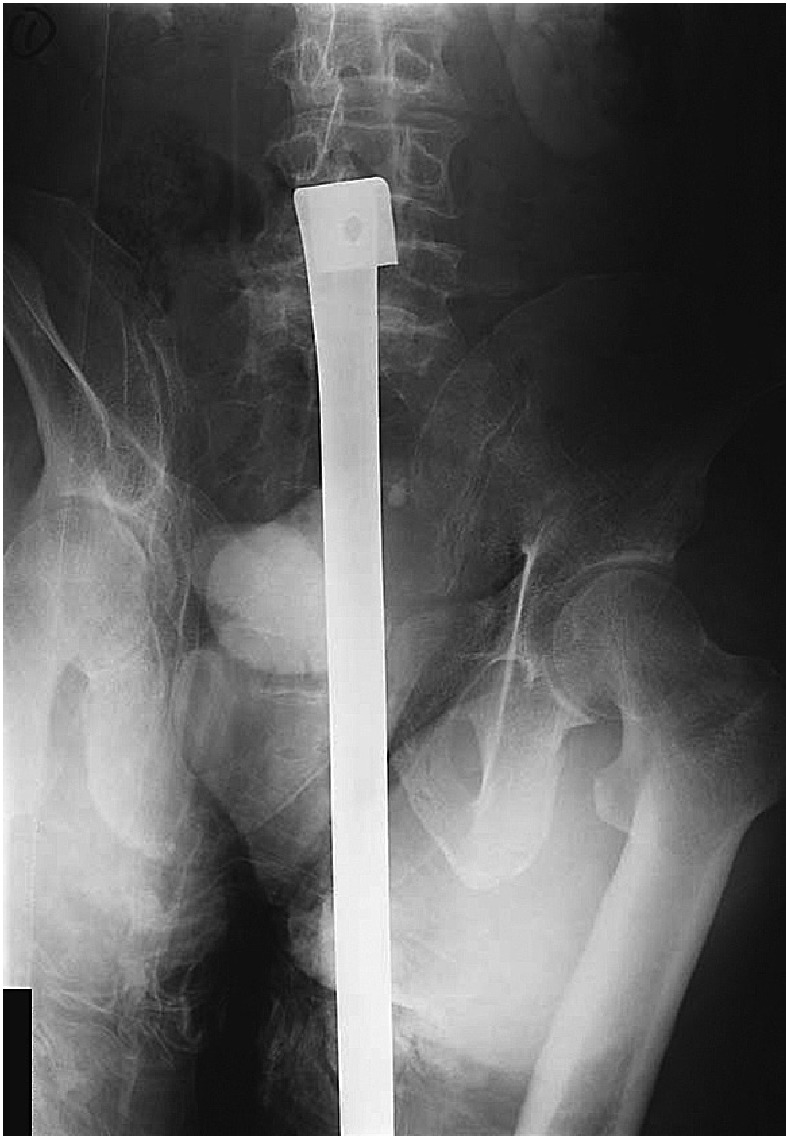
Plain abdominal X-ray film showing a metal pipe. The tip is flat and is located in front of the 4th lumbar vertebra. The length of penetration is 30 cm.
Fig. 2.
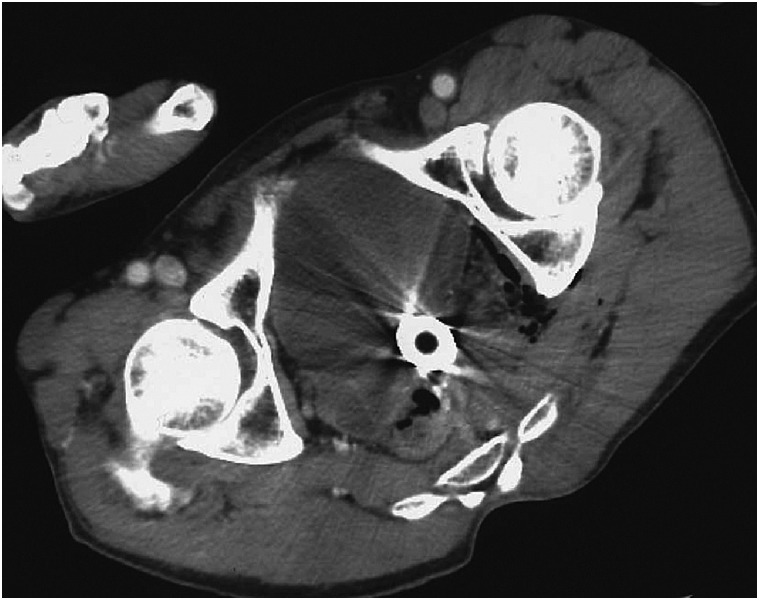
Computed tomography showing a pipe located between the urinary bladder and rectum.
Fig. 3.

The pipe withdrawn from the buttock wound.
Fig. 4.
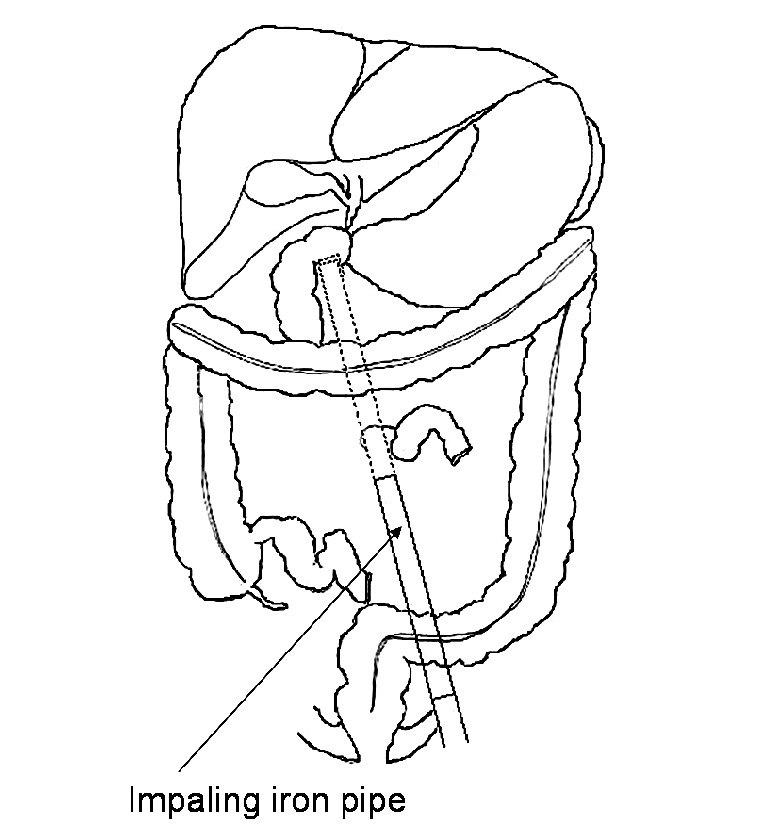
Schematic representation of the impaled pipe and intra-abdominal injury: the pipe entered the abdomen through the ischiorectal fossa between the urinary bladder and rectum, penetrated the sigmoid and transverse mesocolon into the omental bursa, and ended at the duodenum.
DISCUSSION
Impalement injury is a specific type of trauma defined as a penetrating wound caused by an object with a blunt tip and is mostly related to falls, sexual activity, and slipping with a strong external force.1,2) It is usually associated with crush injury, wound contamination, and injury to deep organs, which result in bleeding, organ dysfunction, and infection. It is important to control the bleeding, to find organ damage and evaluate its severity, to restore the function of damaged organs, and to perform adequate drainage.
To the best of our knowledge, 41 cases of impalement injury to the buttocks (excluding gunshot injury) have been reported in the English literature2-29). The mean age of the patients was 18 years (range: 3–49 years), and 26 were males. The cause was a fall (21 cases), sexual activity (11 cases), slipping (5 cases), mistakenly sitting down, and vehicle accident (2 cases each). Thirty-six cases were associated with organ injury, with the injured organs being the rectum (32 cases), urinary bladder (11 cases), duodenum, diaphragm, pancreas and lung (2 cases each), and esophagus, stomach, colon, liver, spleen, kidney, ureter and uterus (1 case each).
When a patient has impalement injury, it is important not to remove the foreign body before the patient is admitted to hospital, because the foreign body might be controlling bleeding from injured vessels. We did not consider introducing an intra-aortic balloon catheter to control bleeding from the view point of his clinical and image findings. Application of transcatheter arterial embolization to control the bleeding was also not considered. Surgeons should investigate any organ injury in detail during the operation, because the foreign body might have been partly retracted or moved.29) In our case, the duodenal injury was found with careful intra-abdominal investigation. Recently, laparoscopic surgery of impalement injury was reported for diagnosis or removing a foreign body, however, laparoscopic approach is generally not recommended for emergent situation.30,31)
In our case, gauze packing was used to control bleeding from the sacral surface. Because the sacral venous plexus is a complex network that connects to the inferior vena cava and vertebral venous system without valves, it is often difficult to control bleeding if it is injured. When a patient with an unstable general condition suffers from massive bleeding, packing with gauze is recommended according to the principles of damage control surgery.32,33) Removal of the gauze or a second-look operation should be performed as soon as the general condition and any coagulation disorder have improved. In our case, because the pelvic cavity was isolated from the abdominal cavity by the peritoneum, the gauze could be safely removed from the hip wound without a second laparotomy.
Burch et al. have stated that the three Ds (diversion of defecation, debridement of crushed injury, and drainage) are important when treating rectal injuries.34) In our case, although we were not able to find any lower rectal injury, diversion sigmoidostomy and drainage were performed to avoid fecal contamination. Impalement injury is a specific type of trauma usually associated with bleeding, organ injury, and infection. Despite these difficulties, our case was successfully treated by precise detection and restoration of organ damage, gauze packing, and staged surgery.
REFERENCES
- 1).Boyd JS. Impalement injuries of the rectum. Ulster Med J 1955; 24: 123–128. [PMC free article] [PubMed]
- 2).Routley EF. Rectal impalement. Postgrad Med 1960; 27: 696–703. [DOI] [PubMed]
- 3).Eginton CT. Rectal impalement; report of an unusual case. Minn Med 1947; 30: 45. [PubMed]
- 4).Geer TM. Rectal wounds by gunshot and impalement. Hawaii Med J 1961; 20: 339. [PubMed]
- 5).Martin HS, Kirk RM. Perforating bladder injury by impalement. Br J Clin Pract 1966; 20: 652–653. [PubMed]
- 6).Lear GH, De KR, Birt SJ. Impalement injury by a tree branch from rectum to right nipple. Injury 1981; 12: 495–498. [DOI] [PubMed]
- 7).Datta PK. Impalement injuries of the colon and rectum. Practitioner 1982; 226: 693–696. [PubMed]
- 8).Jackson DS. Accidental impalement injuries of the intraperitoneal rectum caused by the barrel of the self loading rifle. J R Army Med Corps 1985; 131: 164–6. [DOI] [PubMed]
- 9).Busch DB, Starling JR. Rectal foreign bodies: case reports and a comprehensive review of the world’s literature. Surgery 1986; 100: 512–519. [PubMed]
- 10).Feldman MD, Butler WP, Dunmire LA. Late abscess formation after impalement injury. Del Med J 1987; 59: 725–727. [PubMed]
- 11).Grindlinger GA, Vester SR. Transvaginal injury of the duodenum, diaphragm, and lung. J Trauma 1987; 27: 575–576. [DOI] [PubMed]
- 12).Iwatt AR. Management of rectal impalement injuries. Cent Afr J Med 1988; 34: 190–195. [PubMed]
- 13).Carragher AM, Sulaiman SK, Panesar KJ. Scroto-abdominal impalement injury in a skateboard rider. J Emerg Med 1990; 8: 419–421. [DOI] [PubMed]
- 14).Kennedy D, Becher R, LaFerte R, Lee U. Transvaginal intra-abdominal impalement injury. South Med J 1992; 85: 217–218. [DOI] [PubMed]
- 15).Weber S, Mauch W, Kalayoglu M, Moon TD. Intraperitoneal and extraperitoneal bladder rupture secondary to rectal impalement. J Trauma 1995; 38: 818–819. [DOI] [PubMed]
- 16).Orr CJ, Clark MA, Hawley DA, Pless JE, Tate LR, Fardal PM. Fatal anorectal injuries: a series of four cases. J Forensic Sci 1995; 40: 219–221. [PubMed]
- 17).Juda Z. Accidental anorectal impalement in children. Pediatr Emerg Care 1997; 13: 40–43. [DOI] [PubMed]
- 18).Balier HA, Zachariou Z, Daum R. Impalement and anorectal injuries in childhood: a retrospective study of 12 cases. J Pediatr Surg 1998; 33: 1287–1291. [DOI] [PubMed]
- 19).Grisoni ER, Hahn E, Marsh E, Volsko T, Dudgeon D. Pediatric perineal impalement injuries. J Pediatr Surg 2000; 35: 702–704. [DOI] [PubMed]
- 20).Tanuma Y, Horita H, Kadono M. Extraperitoneal bladder rupture secondary to rectal impalement. Int J Urol 2001; 8: 634–636. [DOI] [PubMed]
- 21).Karger B, Teige K, Bajanowski T. Bizarre impalement fatalities--where is the implement? J Forensic Sci 2002; 47: 389–391. [PubMed]
- 22).Lederer W, Jeske HC, Gunnar K. Underestimated damage from multiple impalement injury. Med J Aust 2002; 177: 155. [DOI] [PubMed]
- 23).Soto LJ 3rd, Saltzman DA. Rectal impalement: a case review. Minn Med 2003; 86: 48–49. [PubMed]
- 24).Jang TK, Yap RL, Batler RA, Brannigan RE. Intraperitoneal bladder rupture and bowel injury from perirectal impalement. J Urol 2003; 170: 2383–2384. [DOI] [PubMed]
- 25).Kim S, Linden B, Cendron M, Puder M. Pediatric anorectal impalement with bladder rupture: case report and review of the literature. J Pediatr Surg 2006; 41: E1–3. [DOI] [PubMed]
- 26).Bronkhorst MW, Wilde JC, Hamming JF, Heij HA. Anorectal impalement in a pediatric patient with transanal evisceration of small bowel. J Pediatr Surg. 2007; 42: E23–5. [DOI] [PubMed]
- 27).Napier F, Fountain-Polley S, Kallapa C. Images in paediatrics: Ironing board impalement. Arch Dis Child 2007; 92; 758. [DOI] [PMC free article] [PubMed]
- 28).Moncure M, Konie JA, Kretzer AB, Dipasco PJ, Braxton CC. Survival Following Rectal Impalement through the Pelvic, Abdominal, and Thoracic Cavities: A Case Report. Case Report Med. Volume 2009, Article ID 361829, 4 pages. [DOI] [PMC free article] [PubMed]
- 29).Ouzonian SP, McGory ML, Chahine AA: Transperineal thoracic impalement without disphragmatic injury. J Trauma 2008; 65: 473–475. [DOI] [PubMed]
- 30).Crawford DL, McVay WB: Delayed presentation of colonic impalement injury by picture frame glass fragment treated using hand-assisted laparoscopic colectomy. Surg Laparosc Endosc Percutan Tech. 2008; 18: 619–621. [DOI] [PubMed]
- 31).Wiesel O, Makrin V, Lubezky Nir, Klausner J, Schulman CI, Soffer D: Diagnostic laparoscopy for the evaluation of abdominal impalement injuries. Isr Med Assoc J. 2008; 10: 314–315. [PubMed]
- 32).Stone HH, Strom PR, MullinsRJ: Management of the Major Coagulopathy with Onset during Laparotomy. Ann Surg. 1983; 197: 532–535. [DOI] [PMC free article] [PubMed]
- 33).Feliciano DV, Mattox KL, Jordan G: Intra-abdominal packing for control of hepatic hemorrhage: A reappraisal. J Trauma 1981; 21: 285–290. [DOI] [PubMed]
- 34).Burch JM, Feliciano DV, Mattox KL: Colostomy and drainage for civilian rectal injuries: Is that all? Ann Surg 1989; 209: 600–611. [DOI] [PMC free article] [PubMed]


