ABSTRACT
We sought to investigate the effects of the left internal mammary artery anastomosed to the left anterior descending artery for improving mid-term outcome in patients with severe left ventricular dysfunction. Twenty consecutive coronary artery bypass grafts performed by a single surgeon for less than 35% ejection fraction patients were reviewed retrospectively from April 2000 to November 2008. There was one perioperative death (5.0% mortality). The mean survival was 55 months with an actual 5-year survival rate of 75%. Echocardiography showed the ejection fraction improved to 10.7±0.32% (p < 0.01). The strongest correlation was observed between both the flow and the pulsatile index of the left internal mammary artery measured intraoperatively by transit time flow meter and the postoperative ejection fraction improvement (R2=0.737 and 0.639, respectively). We reappraised the mid-term beneficial effects of the internal mammary artery anastomosed to the left anterior descending artery in patients with severe left ventricular function.
Key Words: Coronary artery bypass grafting, Ventricular dysfunction, Left internal mammary artery, Left anterior descending artery
INTRODUCTION
The gold standard has been to put the left internal mammary artery (LIMA) to the left anterior descending artery (LAD) in coronary artery bypass grafting because of its excellent long-term patency rate proved by many studies.1-3) On the other hand, in patients with severe left ventricular dysfunction (SLVD) whose ejection fraction (EF) is less than 35%, the beneficial role of LIMA to LAD has not yet been clearly demonstrated. Some investigators have evaluated the results of CABG in patients with SLVD, and they indicate that angina class, coronary heart failure class, quality of life, and ventricular function do improve after CABG in patients with SLVD, but they also report a very high short-term mortality risk, as well as rather poor longer-term survival after CABG.4-6)
In the present study, we aim to study the mid-term outcome of SLVD patients undergoing CABG and roles of intraoperative characteristics of bypass conduits measured by transit time flow meter on improvement of EF and survival.
PATIENTS AND METHODS
From April 2000 to November 2008, we identified 20 patients with SLVD (EF <0.35) who were operated upon by a single surgeon (MHS) for isolated CABG. The data on these patients were retrospectively reviewed for the purpose of this study.
All patients had SLVD confirmed by echocardiography, cardiac catheterization, or nuclear scintigraphy at the time of operation before being included in this study. Improvement in EF was assessed by echocardiography twelve months after the surgery performed at our institution.
All the grafts of all the patients were verified for satisfactory patency by intraoperative transit time flow meter measurement (Medistim, Oslo, Norway) by applying our cut-off values already reported.7,8)
The survival curve was plotted using a Kaplan-Meier analysis to obtain actuarial survival using the StatView software package (Abacus Concepts, Cary, NC). The Student’s t-test for paired data was used to analyze the significance or differences between preoperative and postoperative EF and left ventricular dimensions. The sixth degree nomial distribution was used to show coefficiency.
Approval of this retrospective study was obtained from the Ethics Committee of the Gifu Prefectural Tajimi Hospital. The Committee waived individual consent for the study.
RESULTS
Patients
From April 2000 to November 2008, 20 patients with SLVD (mean EF 0.31±0.04) underwent isolated CABG. Twelve were men and eight were women ranging from 66 to 77 years old. Operative profile was shown in Table 1.
Table 1.
Operative Profile
| Arrested ONCAB | 6 |
| Beating ONCAB | 11 |
| OPCAB | 3 |
| Average graft number | 2.70 |
| LIMA | 20 |
| RA | 14 |
| SVG | 20 |
ONCAB: On Pump Coronary Artery Bypass; OPCAB: Off Pump Coronary Artery Bypass; LIMA: Left Internal Mammary Artery; RA: Radial Artery; SVG: Saphenous Vein Graft
Mortality and morbidity
Table 2 showed the postoperative mortality and morbidity. There was one death, which was due to low output syndrome three weeks after operation. One patient had ventricular dysrhythmia which was treated by amiodarone. Four patients needed prolonged mechanical ventilation of more than 72 hours. Two patients needed temporary hemodialysis.
Table 2.
Mortality and Morbidity
| Operative Mortality | 1 (5.00%) |
| Cardiac Complications | 1 (5.00%) |
| Neuro Complications | 0 (0%) |
| Pulmonary Complications | 4 (20.0%) |
| Infectious Complications | 0 (0%) |
| Renal Complications | 2 (10.0%) |
| Bleeding Complications | 0 (0%) |
Mid-term survival
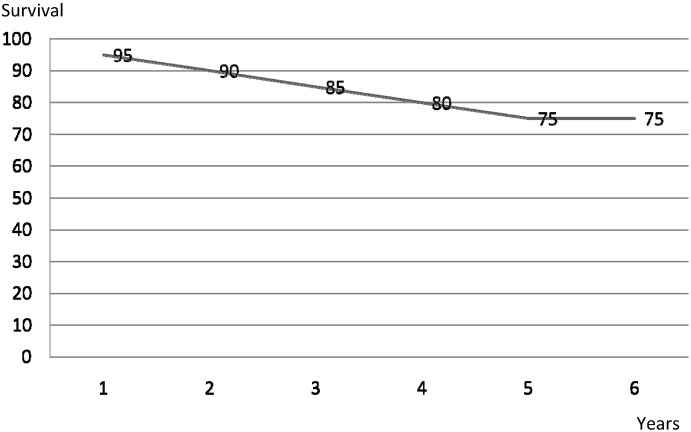
Figure 1 showed a rough survival curve. 75% actuarial survival was obtained at 5 years.
Fig. 1.
Survival Curve
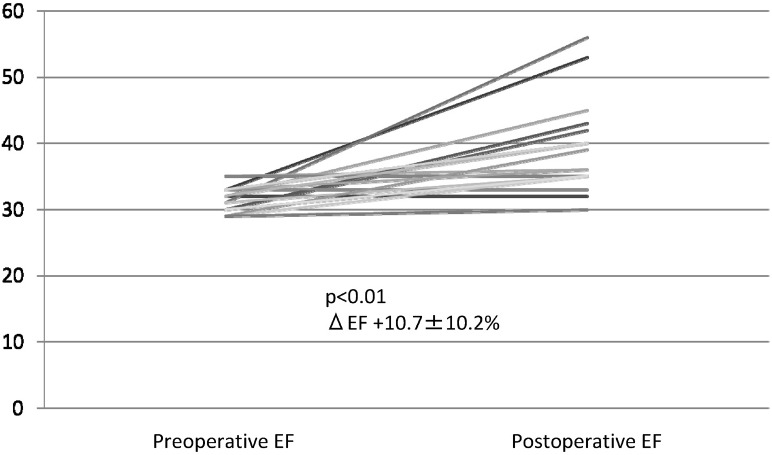
EF and left ventricular dimension improvements
Figure 2 showed EF improvements. EF increased to 10.7±10.2% postoperatively. Left ventricular end-systolic volume index (LVESVI) decreased to 21.5±10.6 postoperatively. Left ventricular end-diastolic volume index (LVEDVI) decreased to 26.3±10.2 postoperatively. Tei index9) decreases to 0.11±0.32 postoperatively. All the cardiac parameters improved significantly (p < 0.01).
Fig. 2.
EF Change
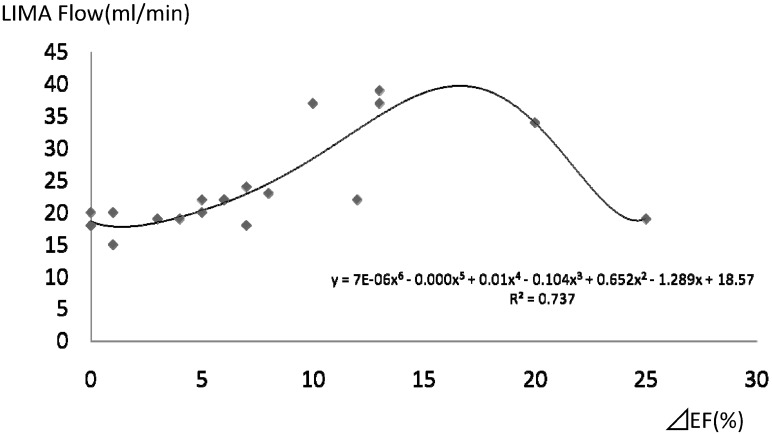
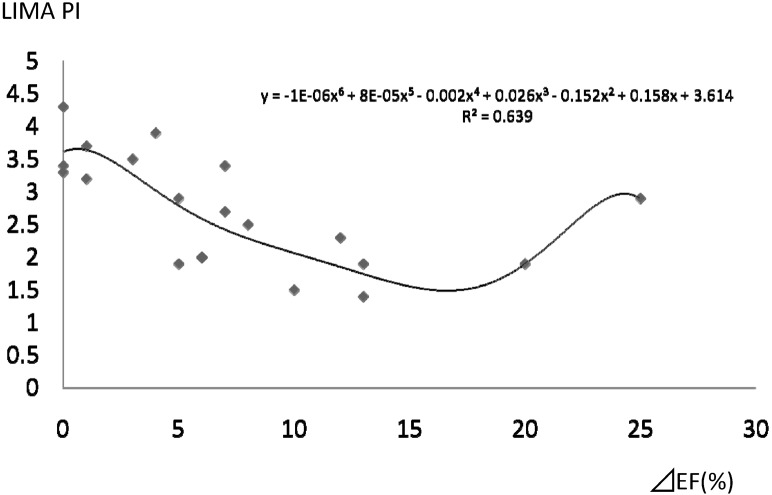
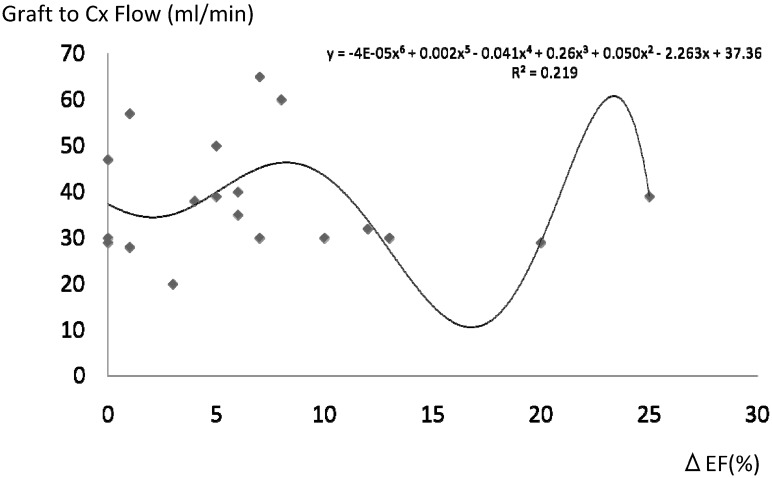
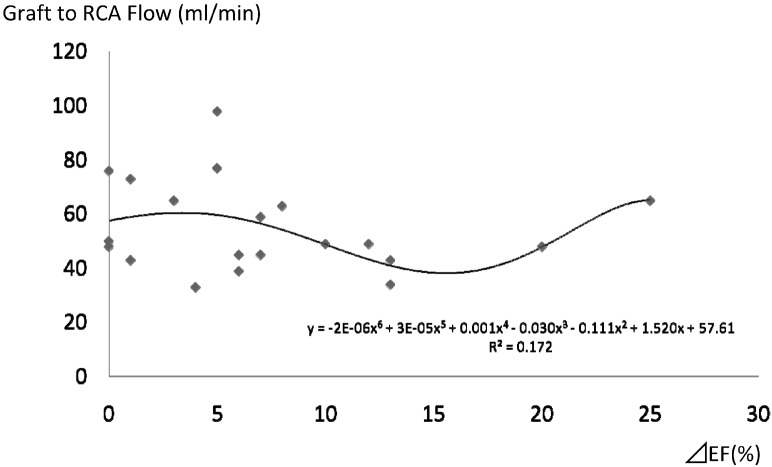
EF improvement and grafts flow characteristics
Figure 3 to 6 showed relationships between EF improvement and grafts flow characteristics. The strongest coefficient was observed between EF improvements and LIMA to LAD flow and its pulsatile index (PI) (R2=0.737 and 0.639, respectively). The others were statistically insignificant. In Figure 3, it was inferred that if LIMA flow was more than 30 ml/min, anticipated improvement of EF would be more than 15%. In Figure 4, it was shown that if LIMA PI was less than 1.5, anticipated improvement of EF would be more than 15%.
Fig. 3.
LIMA Flow and EF Change
Fig. 4.
LIMA PI and EF Change
Fig. 5.
Graft to Cx Flow and EF Change
Fig. 6.
Graft to RCA Flow and EF Change
DISCUSSION
Patients with SLVD have been a challenging cohort for cardiac surgeons because of its poor operative mortality and dismal survival rate. Despite improvements of several medical and biological modalities such as cardiac resynchronization therapy10) and cell-based myocardial regeneration therapies,11,12) very sick patients are often ultimately referred for surgical myocardial revascularization or ventricular remodeling surgery by cardiologists.
Despite the ominous outlook of operative mortality and long-term survival, recent improvements of both medical optimization and surgical techniques have made it possible to attain reasonable postoperative mortality and good survival rate. Literature published since 2001 showed 4.4% to 11% mortality and 59% to 77% survival rate at 5 years in these SLVD patients who underwent CABG alone.5,6,13,14) The results of this study, i.e, 5.0% mortality and 75% survival at 5 years, were in accordance with them.
In this study we focused on the roles of graft conduits in improving EF because such studies were few. Luciani et al concluded that use of the left internal thoracic artery was inversely associated with return of congestive heart failure with an odds ratio 0.84 and p value < 0.03 [15]. We found that only LIMA flow and PI had the statistically strongest coefficient power on improvement of EF with R2 of 0.737 and 0.639, respectively. Since we reported that mean LIMA flow of 15 ml/min and PI of 5.1 were the good cutoff criteria for a functioning graft,7,8) this study showed that mean LIMA flow of 30 ml/min and PI of 1.5 were good predictors for improvement of EF. As shown in Figure 3 and 4, EF improvement was not linear to flow and PI. This was thought to be due to different LAD region, LAD viability, and coronary flow reserve.
Limitations included that a sample size of 20 patients was too small sample size to draw significant conclusions and this study was retrospective. On the other hand, even with a sample size of 20 patients, the polynomial coefficient curve could be constructed with statistically meaningful significance, and that this study was not biased.
In conclusion, we reappraised the mid-term beneficial effects of the internal mammary artery anastomosed to the left anterior descending artery in patients with severe left ventricular function.
REFERENCES
- 1).Lytle BW, Loop FD, Cosgrove DM, Ratliff NB, Easley K, Taylor PC. Long-term (5–12 years) serial studies of internal mammary artery and saphenous vein coronary bypass grafts. J Thorac Cardiovasc Surg 1985; 89: 248–58. [PubMed]
- 2).Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC. Influence of internal mammary artery graft on 10-year survival and other cardiac events. N Engl J Med 1986; 314: 1–6. [DOI] [PubMed]
- 3).Cameron AA, Green GE, Brogno DA, Thornton J. Internal thoracic artery grafts: 20-year clinical follow-up. J Am Coll Cardiol 1995; 25: 188–92. [DOI] [PubMed]
- 4).Shapira I, Isakov, Yakirevich V, Topilsky M. Long-term results of coronary artery bypass surgery in patients with severely depressed left ventricular function. Chest 1995; 108: 1546–1550. [DOI] [PubMed]
- 5).Carr JA, Haithcock BE, Paone G, Bernabei AF, Silverman NA. Long-term outcome after coronary artery bypass grafting in patients with severe left ventricular dysfunction. Ann Thorac Surg 200; 74: 1531–1536. [DOI] [PubMed]
- 6).Appoo J, Norris C, Merali S, Graham MM, Koshal A, Knudtson ML, Ghali WA. Long-term outcome of isolated coronary artery bypass surgery in patients with severe left ventricular dysfunction. Circulation 2004; 110 [suppl II]: II-13–II-17. [DOI] [PubMed]
- 7).Tokuda Y, Song MH, Ueda Y, Usui A, Akita T. Predicting early coronary artery bypass graft failure by intraoperative transit time flow measurement. Ann Thorac Surg 2007; 84: 1928–34. [DOI] [PubMed]
- 8).Tokuda Y, Song MH, Oshima H, Usui A, Ueda Y. Predicting midterm coronary artery bypass graft failure by intraoperative transit time flow measurement. Ann Thorac Surg 2008; 86: 532–6. [DOI] [PubMed]
- 9).Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol 1995; 26: 135–136. [PubMed]
- 10).Linde C, Abraham WT, Gold MR, St John Sutton M, Ghio S, Daubert C; REVERSE Study Group. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and precious heart failure symptoms. J Am Coll Cardiol 2008; 52: 1834–43. [DOI] [PubMed]
- 11).Lee MS, Makkar RR. Stem-cell transplantation in myocardial infarction: a status of report. Ann Intern Med 2004; 140: 729–737. [DOI] [PubMed]
- 12).Heilmann CA, Attmann T, Thiem A, Haffner E, Beyersdorf F, Lutter G. Gene therapy in cardiac surgery: intramyocardial injection of naked plasmid DNA for chronic myocardial ischemia. Eur J Cardiothorac Surg 2003; 24: 785–793. [DOI] [PubMed]
- 13).Lorusso R, La Canna G, Ceconi C, Borghetti V, Totaro P, Parrinello G, Coletti G, Minzioni G. Long-term results of coronary artery bypass grafting procedure in the presence of left ventricular dysfunction and hibernating myocardium. Eur J Cardiothorac Surg 2001; 20: 937–948. [DOI] [PubMed]
- 14).Hills GS, Zehr KJ, Williams AW, Schaff HV, Orzulak TA, Daly RC, Mullany CJ, Rodeheffer RJ, Oh JK. Outcome of patients with low ejection fraction undergoing coronary artery bypass grafting: Renal function and mortality after 3.8 years. Circulation 2006; 114 [suppl I]: I-414–I-419. [DOI] [PubMed]
- 15).Luciani GB, Montalbano G, Casali G, Mazzucco A. Predicting long-term functional results after myocardial revascularization in ischemic cardiomyopathy. J Thorac Cardiovasc Surg 2000; 120: 478–89. [DOI] [PubMed]