ABSTRACT
This study demonstrates the risk adjusted cumulative sum analysis of an individual surgical learning curve for acute type A aortic dissection surgery. Thirty consecutive patients were operated by a single surgeon for acute type A aortic dissection from April 2001 to March 2008. Operative variables, mortality, and major morbidities were analyzed. The learning curve was calculated by cumulative sum analysis. The anticipated 30-day operative mortality rate was 20.2±12.7% (range, 3.3–56.7%) and the expected 30-day mortality and morbidity rate was 47.0±13.3 % (range, 21.7–70.6%) according to the Japan SCORE calculator. The observed operative and in-hospital mortality rate was 6.67% (two patients), and the observed major postoperative morbidity rate was 10.0% (three patients). Risk-adjusted cumulative sum analysis revealed that no excess deaths occurred beginning at the seventh case and thereafter. The surgeries for acute type A aortic dissection could be performed at the professionally permissive level from the beginning. Risk-adjusted cumulative sum analysis was a useful tool to monitor the performance of the surgical procedure.
Key Words: aortic dissection, surgery, learning curve, cumulative sum
INTRODUCTION
Acute type A aortic dissection (AAAD) is a highly lethal cardiovascular emergency with an incidence of 3685 new cases per year operated in Japan and had an 11.1% in-hospital mortality rate in 2010.1) A total of 586 hospitals in Japan have cardiovascular surgeons, and 1881 cardiovascular surgeons are practicing as board-certified cardiovascular surgeons.1) On an average, one hospital experiences 6.28 cases of AAAD per year and one surgeon experiences 1.96 cases of AAAD per year. Recently, there has been a high increase in the clinical audit level for cardiovascular surgery. AAAD is obviously a life threatening condition, and the available treatment alternatives do not offer encouraging results. Therefore, an emergent life-saving surgery performed by a professional expert is highly demanded. The profession itself has come to recognize clinical audit as a valuable means to improve professional standards and reduce complication rates.
The usefulness of the sequential probability cumulative sum (CUSUM) technique to analyze surgical performance has been demonstrated in recent studies.2-4) CUSUM detects changes in perioperative mortality and morbidity rate during the patient care process. Furthermore, it provides almost real-time monitoring of surgical performance if updated after each procedure. Moreover, CUSUM analysis acknowledges the importance of individual experience in monitoring performance and allows for easy charting of a learning curve with regard to the incidence of perioperative complications.
We have been working on this learning curve issue and have reported literature considering coronary artery bypass grafting5), aortic arch replacement6), and launching of a new cardiac surgery unit.7) In addition, we have shown that there is a cut-off number of cases sufficient to ensure optimal outcomes. In this study, we constructed a learning curve of AAAD surgery, which is one of the most difficult emergent cardiac surgeries in Japan.
MATERIAL AND METHODS
Thirty consecutive patients were operated for AAAD by a single surgeon (MHS) at two different hospitals from April 2001 to March 2008. At one hospital, 25 patients operated for AAAD from 2001 to 2003 and three patients among them were operated by MHS. At another hospital, 27 patients with AAAD were operated by MHS from 2004 to 2008. Clinical charts and operative records were collected for demographic data, preoperative and postoperative morbidities (including reoperation for any reasons, stroke, prolonged respiratory ventilation, hemodialysis, and sterna infection), operative variables, and short-term prognosis. Institutional Review Board approval was obtained for this clinical cardiac surgery database research. The requirement for informed consent was waived by the Institutional Review Board.
Operative Technique
A patient was placed in the supine position under general anesthesia. Arterial line was monitored at either of the radial artery. Near infrared ray monitoring was applied to the frontal head. We preferred to use the common femoral artery as the arterial cannulation site because it has stronger pulsation and is quick and safe. When tperfusion was inadequate, we performed apical or axillary artery cannulation. After the chest was opened, right atrial appendage was cannulated with double-borne venous drainage. Deep hypothermic circulatory arrest was attained by cooling the core done to 20 Celsius degree at the pharynx. Ascending aorta was opened and intimal tear was identified. We used retrograde cerebral perfusion via venous cannula for brain protection among the first 15 patients, and we changed it to antegrade cerebral perfusion through intraluminal cerebral perfusion balloon catheter among the last 15 patients. According to the intimal tear site, ascending or hemiarch replacement was decided, and distal anastomosis was performed first with double layer reinforcement. After performing distal anastomosis with a proper-size prosthetic graft, the graft was clamped and systemic antegrade perfusion was initiated through a side branch of the graft, and rewarming was initiated. Proximal anastomosis was performed in the same fashion as distal anastomosis with or without aortic valve procedure.
Statistical Analysis
In this study, CUSUM was defined as Sn=∑(Xi–X0), where Xi=0 for success, Xi=1 for a failure, and X0 is the reference or target value. The target value was calculated for every patient using the Japan SCORE calculator, which is an online calculator of 30-day operative and in-hospital mortality and morbidity rates (http://www.jacvsd.umin.jp).1) CUSUM curves were manually constructed for determining overall mortality rate and operative variables.8) 95% lower alarm line was defined as 95% safety of the target value for each patient.
Numerical data regarding surgery, cardiopulmonary bypass, aortic crossclamp, and deep hypothermic circulatory arrest duration were statistically analyzed by the sixth polynomial approximation coefficient.
RESULTS
This study population comprised 18 female and 12 male patients (Table 1). Their mean age was 64.1±10.8-years-old (range, 38 to 79 years). As shown in Table 2, operative and in-hospital mortality was observed in two patients (6.67%), which included rupture of the residual descending aneurysm 3 weeks after the surgery and brain infarction. Major postoperative morbidity was observed in three patients (10.0%), including one patient with a postoperative transient stroke and two patients of long respiratory ventilation and subsequent tracheostomy. The average surgery duration was 487 ±265 min (range, 240-1320 min), average cardiopulmonary duration was 260±146 min (range, 134–648 min), the average aortic crossclamp duration was 122±40.1 min (range, 63–281 min), and the average deep hypothermic circulatory arrest duration was 50.5±13.6 min (range, 18–79 min). Eight cases had surgery duration longer than the average 509.3 min. Of these eight patients, one patient was in cardiogenic shock preoperatively and one patient developed brain infarction and hemiparalysis preoperatively. Other patients showed no preoperative and intraoperative morbid risk factors.
Table 1.
Patient demographics and comorbid conditions
| Total number of patients | 30 |
| Age (years,mean±standard deviation) | 64.1±10.8 |
| Gender, female (%) | 18 (60) |
| Cardiogenic shock (%) | 5 (16.7) |
| Neurologic symptoms (%) | 3 (10.0%) |
| Chronic obstructive pulmonary disease (%) | 6 (20.0) |
| Diabetes mellitus (%) | 2 (6.67) |
| Peripheral artery disease (%) | 3 (10.0) |
| Japan SCORE mortality (%) (mean±standard deviation) | 20.2±12.7% (3.3–56.7) |
| Japan SCORE mobidity (%) (mean±standard deviation) | 47.0±13.3% (21.7–70.6) |
Table 2.
Operative Data and Postoperative Results
| Operation time, minutes | 487±265 |
| CPB time, minutes | 260±146 |
| ACC time, minutes | 122±40.1 |
| DHCA time, minutes | 50.5±13.6 |
| Ascending replacement (%) | 25 (83.3) |
| Hemiarch replacement (%) | 5 (16.7) |
| Concomitant AVR (%) | 3 (10.0) |
| Aortic valve suspension(%) | 5 (16.7) |
| Concomitant CABG (%) | 5 (16.7) |
| Concomitant Bentall (%) | 2 (6.67) |
| 30-day mortality (%) | 2 (6.67) |
| 30-day morbidity (%) | 3 (10.0) |
CPB: Cardiopulmonary Bypass, ACC: Aortic Cross Clamp, DHCA: Deep Hypothermic Circulatory Arrest, AVR: Aortic Valve Replacement, CABG: Coronary Artery Bypass Grafting
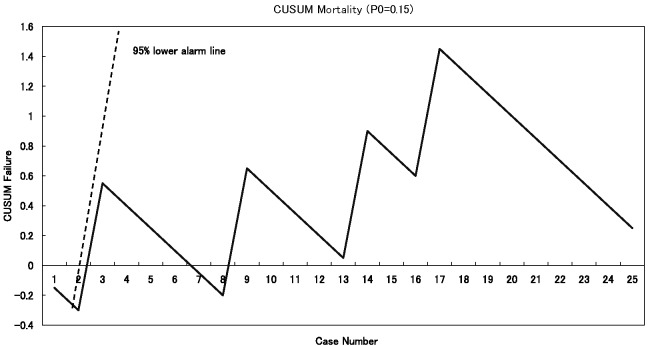
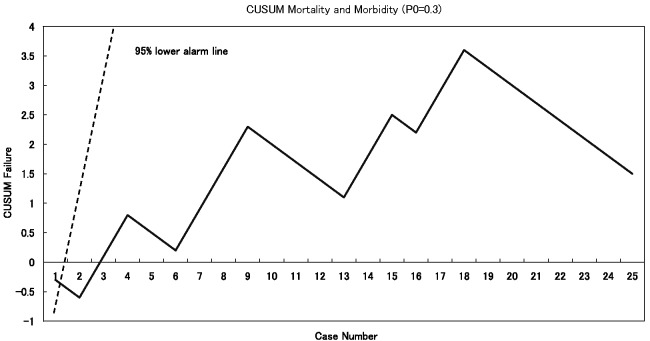
Figure 1 shows CUSUM learning curve of mortality and Figure 2 shows CUSUM learning curve of mortality and morbidity. In both figures, the learning curves did not transgress the 95% lower alarm line.
Fig. 1.
Risk Adjusted Cumulative Sum Analysis of Mortality. Horizontal axis denotes the number of cases and vertical axis denotes cumulative deaths.
95% upper alarm, 80% upper alert, and 80% lower alert lines are not shown in this figure because they were located beyond the height of the graph.
Fig. 2.
Risk Adjusted Cumulative Sum Analysis of Mortality and Morbidity. Horizontal axis denotes the number of cases and vertical axis denotes cumulative morbidity.
95% upper alarm, 80% upper alert, and 80% lower alert lines are not shown in this figure because they were located beyond the height of the graph.
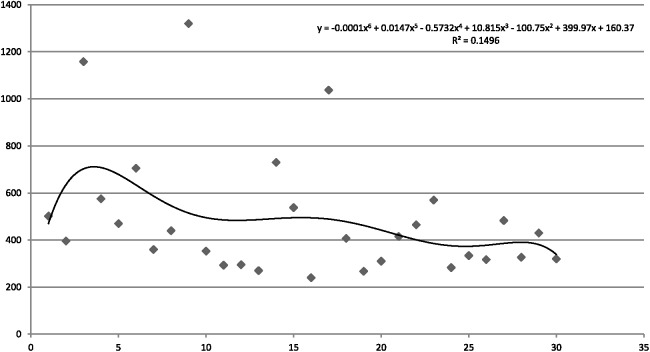
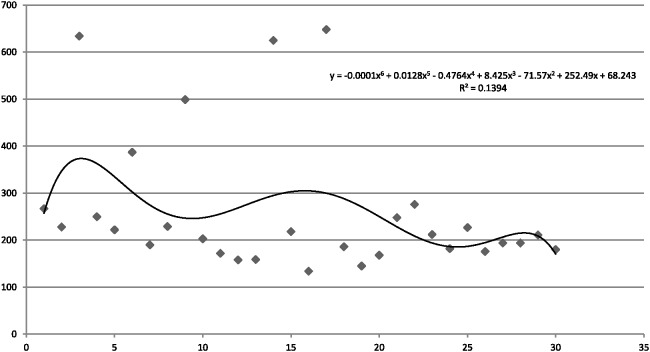
Scattered graphs regarding surgery and cardiopulmonary bypass duration are shown in Figure 3 and 4. A negative and downward correlation was observed for surgery duration and cardiopulmonary bypass duration with R2 values by the sixth polynomial approximation coefficient analysis of 0.149 and 139, respectively, which were not statistically significant.
Fig. 3.
Operation Duration and Case Loads. Horizontal axis denotes the number of cases and vertical axis denotes surgery duration in minutes.
Fig. 4.
Cardiopulmonary Bypass Duration and Case Loads. Horizontal axis denotes the number of cases and vertical axis denotes cardiopulmonary bypass duration in minutes.
All patients needed blood transfusion, including packed blood cell, fresh frozen plasma, or platelet concentrate.
DISCUSSION
Unlike the frequency and stable surgical results of patients with a type B aortic dissection9),10), patients with AAAD very infrequently visit board-certified cardiac surgeons in Japan. Kazui et al. recently reported that 435 hospitals treated 9556 patients of AAAD in five years with a 13.2% mortality rate and four hospitals, which treated more than 20 patients, showed a 7.90% mortality in Japan.11) These results are very much superior to those of Europe and the US that reported 26% operative and in-hospital mortality.12,13)
The correlation between quantity and quality of a surgical procedure has been recently investigated intensively. Although some groups reported data that strongly support the positive relationship between the number (quantity) of cases and operative results (quality) in coronary artery bypass grafting,14),15) other groups have questioned the relationship.16),17) In a large study on AAAD with 3013 patients, the mortality rate was 23%, which was not significantly different from that reported by the IRAD consortium, which is thought to be representative of high-volume aortic surgery centers. They argued that operative repair of AAAD may have a constant minimum force of mortality, which only heightens the importance of identifying and treating patients at risk for dissection.3),13)
This study inferred two facts. First, an independent cardiac surgeon could launch into AAAD surgery with safe results, which was shown as below 95% lower alarm line performance in the CUSUM analysis. Second, the surgery, cardiopulmonary bypass, aortic crossclamp, and deep hypothermic circulatory arrest duration did not change significantly throughout the study period.
The first observation may be because of the excellent mentoring of the cardiac surgeon and uniform operative techniques at teaching hospitals. In addition, we provide careful and meticulous postoperative care to prevent patient death even in patients complicated with stroke. Surgery in the first three cases were performed under strict supervision of the senior attending-consultant surgeon, and the remaining cases were performed by a surgeon undertaking the study. The nursing staff changed in turns; however, perfusionists who operated the pumps were highly experienced personnel. The second observation was in accordance with the quantity-quality relationship. It may also be explained by the finding that preoperative morbid status of patients with AAAD varies widely and differently influences the surgery duration. Furthermore, preoperative neurological and circulatory status, the extent of dissection and the quality of the aortic wall, and coagulapathic status differ among patients. These complex factors reflect the fact that the surgery duration differed among patients.
A potential limitation of this study is that the study population 30 cases of AAAD is too small to draw definite conclusions. Furthermore, the limited amount of literature dealing directly with the relationship between the number of cases (quantity) and learning curve in AAAD surgery was also a limitation. As mentioned, patients with AAAD rarely consult cardiac surgeons in Japan. CUSUM analysis used in this study was not dependent on the number of cases and was statistically significant. Another limitation is the criticism that this CUSUM analysis provides information that could not be generalized and did not consider other patient care-related issues or variables. Moreover, it is logically impossible to generalize the result of different surgeons because each surgeon has a different surgical training background. This study is intended to be considered not as a generalization but as an example. In addition, the operative background of the study patients was different, and the adjuncts were changed on the basis of the study. The study period spanned eight years during which skills of surgeons could have improved.
Conflict of Interest
None
REFERENCES
- 1).Kuwano H, Amano J, Yokomise H. Thoracic and cardiovascular surgery in Japan during 2010 : annual report by The Japanese Association for Thoracic Surgery. Gen Thorac Cardiovasc Surg 2012; 60: 680–708. [DOI] [PubMed]
- 2).Holzhey DM, Jacobs S, Walther T, Mochalski M, Mohr FW, Falk V. Cumulative sum failure analysis for eight surgeons performing minimally invasive direct coronary artery bypass. J Thorac Cardiovasc Surg 2007; 134; 663–669. [DOI] [PubMed]
- 3).Novick RJ, Fox SA, Stitt LW, Kiaii BB, Swinamer SA, Rayman R, et al. Assessing the learning curve in off-pump coronary artery surgery via CUSUM failure analysis. Ann Thorac Surg 2002; 73: 358–362. [DOI] [PubMed]
- 4).Rogers CA, Reeves BC, Caputo M, Ganesh JS, Bonser RS, Angelini GD. Control chart methods for monitoring cardiac surgical performance and their interpretation. J Thorac Cardiovasc Surg 2004; 128: 811–819. [DOI] [PubMed]
- 5).Song MH, Tajima K, Watanabe T, Ito T. Learning curve of coronary surgery by a cardiac surgeon in Japan with the use of cumulative sum analysis. Jpn J Thorac Cardiovasc Surg 2005; 53: 551–556. [DOI] [PubMed]
- 6).Song MH, Tokuda Y, Hirai M, Ueda Y. Learning curve of arch-first technique analyzed by cumulative sum. Asian Cardiovasc Thoracic Ann 2007; 15: 507–510. [DOI] [PubMed]
- 7).Song MH, Tokuda Y, Nakayama T, Hattori K, Hirai M. Safe launching of a newly appointed cardiac surgery unit at a low-volume hospital with the use of cumulative sum analysis. Circ J 2008; 72: 437–440. [DOI] [PubMed]
- 8).Novick RJ, Stitt LW. The learning curve of an academic cardiac surgeon:Use of the CUSUM method. J Card Surg 1999; 14: 312–22. [DOI] [PubMed]
- 9).Sakakura K, Kubo N, Ako J, Ikeda N, Funayama H, Hirahata T, et al. Determinants of in-hospital death and rupture in patients with a Stanford B aortic dissection. Circ J 2007; 71: 1521–4. [DOI] [PubMed]
- 10).Hata M, Sezai A, Niino T, Yoda M, Wakui S, Unosawa S, et al. Prognosis for patients with type B acute aortic dissection: risk analysis of early death and requirement for elective surgery. Circ J 2007; 71: 1279–82. [DOI] [PubMed]
- 11).Kazui T, Osada H, Fuijta H. An attempt to analyze the relation between hospital surgical volume and clinical outcome. Gen Thorac Cardiovasc Surg 2007; 55: 483–492. [DOI] [PubMed]
- 12).Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): New Insights into an Old Disease. JAMA 2000; 283: 897–903. [DOI] [PubMed]
- 13).Knipp BS, Deeb M, Prager RL, Williams CY, Upchurch, Jr GR, Patel HJ. A contemporary analysis of outcomes for operative repair of type A aortic dissection in the United States. Surgery 2007; 142: 524–528. [DOI] [PubMed]
- 14).Hannan EL, Wu C, Ryan TJ, Bennet E, Culliford AT, Gold JP, et al. Do hospitals and surgeons with higher coronary artery bypass graft surgery volumes still have lower risk-adjusted mortality rates? Circulation 2003; 108: 795–801. [DOI] [PubMed]
- 15).Shahian DM, Normand SL. The volume-outcome relationship: from Luft to Leapfrog. Ann Thorac Surg 2003; 75: 1048–58. [DOI] [PubMed]
- 16).Welke KF, Barnett MJ, Sarrazin MS, Rosenthal GE. Limitations of hospital volume as a measure of quality of care for coronary artery bypass graft surgery. Ann Thorac Surg 2005; 80: 2114–9. [DOI] [PubMed]
- 17).Rathore SS, Epstein AJ, Volpp KG, Krumholz HM. Hospital coronary artery bypass graft surgery volume and patient mortality, 1998–2000. Ann Surg 2004; 239: 110–7. [DOI] [PMC free article] [PubMed]