ABSTRACT
Various complications occur during total hip arthroplasty (THA). It is common to implement trial treatments of various implants during THA. Here we report on 2 cases in which the trial femoral head fell into the pelvis and migrated during THA. The trial head was not retrieved but left inside in one case, while the other presented the opportunity for a possible retrieval. It is important to recognize the existence of such rare complications.
Key Words: total hip arthroplasty, intraoperative Migration, intraoperative complication
INTRODUCTION
Nerve/vascular injury, bone fracture, deep venous thrombosis, etc. are known as complications during Total hip arthroplasty (THA)1-5). Concerning the installation of implants, it is common to implement trials of the femoral stem or head, and acetabular socket, before installing implants, in order to secure accuracy, and to check the degree of fixation, stress in the soft tissues, joint stability and impingement. In this paper, we describe our experience with cases in which the trial femoral head fell into the pelvis and migrated, during the intraoperative trial of the head. In the previous reports, seven cases were reported in the United States and Europe6-12), but there were only a few cases with the typical images of migrated trial head. This case is a first report in Japan with a characteristic image. In this study, we report on two cases involving migration of the trial femoral head. The patients and their families were informed that the data from the cases would be submitted for publication, and all gave their consent.
CASE 1
A 75-year-old female had been suffering from right hip pain at the age of 74, and visited our hospital as an outpatient. Bilateral osteoarthritis of the hip was found in a plane X-ray image of the hip joints (Figure 1). The plane X-ray images showed end stage of osteoarthritis with mild subluxation. Because the right-side coxalgia gradually worsened, she was admitted to our hospital. She had a total of 55 points in the Harris hip score before the surgery.
Fig. 1.

This is an anterior X-ray image of the hip joints before surgery. Narrowing of the cleft between articulations, spur formation and osteoscierosis in the acetabulum were observed, and a diagnosis of osteoarthritis was reached.
Cementless THA was performed under general anesthesia in the left lateral decubitus position. A posterior approach was used with standard skin incision. Short rotator muscles were dissected, and repaired when the wound was closed. Anterior joint capsules were resected widely. The installation angle of the acetabular cup was set, in compliance with the Pelvic Guide13), at 45° inclination, and 20° anteversion. After implementing acetabular reaming and an acetabular cup trial, an acetabular socket of φ50mm and a ceramic liner (Trident, Stryker Co. NJ, USA) were installed. Subsequently, after implementing femoral reaming and rasping, a femoral stem component (Supersecurefit, Stryker Co. NJ, USA) was installed, as is typical. Finally, the presence of stress in the soft tissues, joint instability and impingement were assessed, by using a trial femoral head of φ26mm. No dislocation occurred even at 80-degree flexion and 80-degree internal rotation. No posterior instability was found.
When an assistant, who did not have much experience in handling hip prosthesis, checked the anterior instability at external rotation in full extension, he forcibly caused an anterior dislocation. Therefore, the trial femoral head fell anteriorly and migrated within the pelvis through the site which resected anterior joint capsule. Immediately, retrieval was attempted with fingers along the interior wall of the pelvis. Not only was the retrieval unsuccessful, but the head was pushed even further inside with the fingers. The head was migrated deeper along the interior wall of the pelvis. Its location could not be confirmed with a fluoroscope.
The anterior portion of the joint capsule was opened up but we failed to find the trial head. We thought it was necessary to change the body position and requested an abdominal surgeon for help to retrieve the trial femoral head. We stopped to retrieve the trial head. It was necessary to operate on some day, if patient complaint abdominal pain or discomfort. Upon obtaining the consent from the patient’s family, the wound was closed to finish the surgery, leaving the trial femoral head inside. The X-ray image of the AP view just after the surgery showed that trial head was confirmed slightly (Figure 2). After the surgery, with CT, the trial femoral head was confirmed inside the iliac muscle, within the quadrilateral space inside the pelvis (Figure 3-A, B). Anteversion of the acetabular cup was 30 degree on CT view. It has been 3 years since the patient underwent the surgery. No clinical symptoms, such as abdominal symptoms, have been found during this period of time. The location of the trial femoral head has not changed during the past 3 years, according to the X-ray image (Figure 4). Furthermore, the current Harris hip score has improved to a total of 81 points.
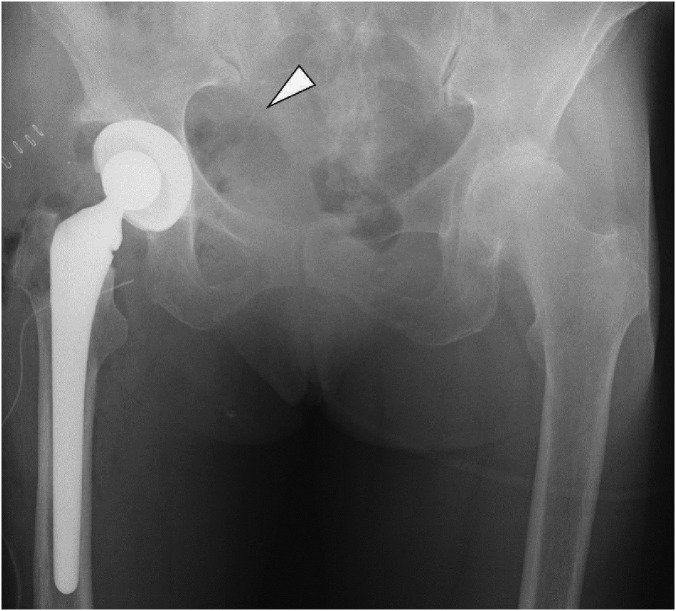
Fig. 2.
This is an anterior X-ray image of the hip joints after surgery. The trial head was faintly visible (white arrow).
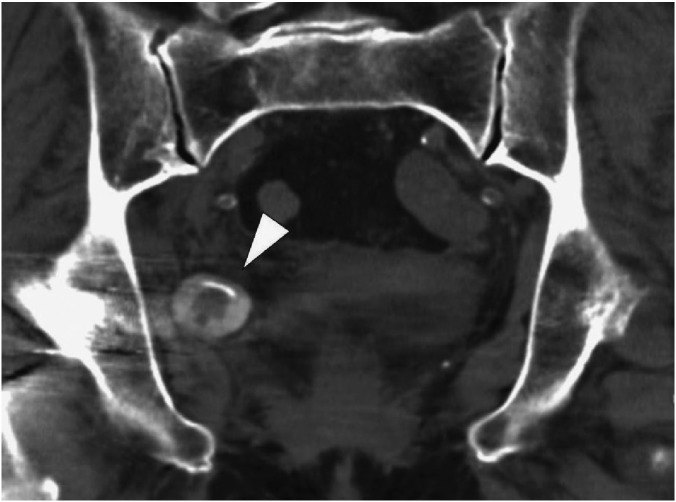
Fig. 3A.
This shows the CT after surgery. (coronal image ) The trial femoral head is observed to be inside the iliac muscle of the quadrilateral space within the pelvis. (white arrow)
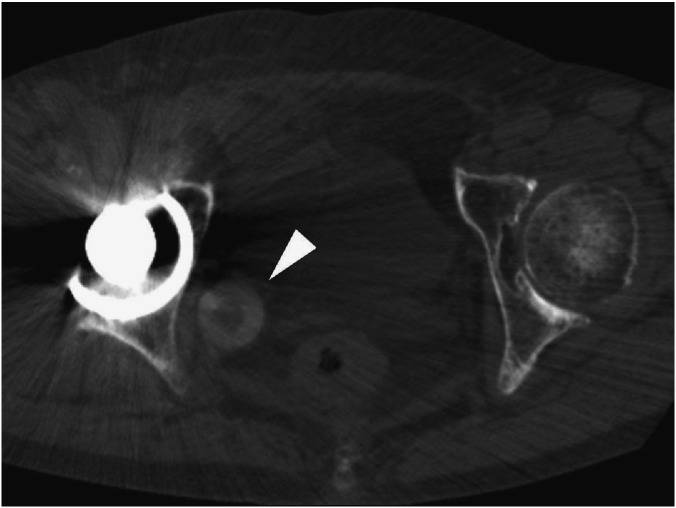
Fig. 3B.
This shows the CT after surgery. (axial image) The trial femoral head is found in the quadrilateral space in the posterior inner wall of the right pelvis. (arrow head)
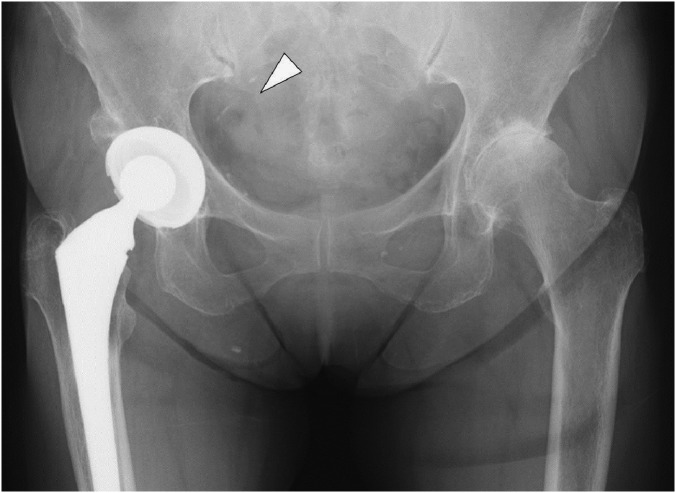
Fig. 4.
This shows an X-ray image 3 years after surgery. The trial femoral head is faintly visible inside the right pelvis. (Arrow head)
CASE 2
A 50-year-old female presented with advanced osteoarthritis of left hip secondary to acetabular dysplasia. The plane X-rays image showed grade4 by the Kellgren-Lawrence classification, and type1 by the crowe classification. Before surgery, she had a total of 54 points for the Harris hip score.
A cementless THA was performed by a procedure same as Case 1. Anterior joint capsules were resected. The installation angle of the acetabular cup was set, in compliance with the Pelvic Guide13), at 45° inclination, and 20° anteversion. After implementing acetabular reaming and an acetabular cup trial, an acetabular socket of φ48mm and a ceramic liner were installed (Trident, Stryker Co. NJ, USA). Subsequently, after implementing femoral reaming and rasping, a femoral stem component (Supersecurefit, Stryker Co. NJ, USA) was installed, as is typical. Finally, the presence of stress in the soft tissues, joint instability and impingement were assessed, by using a trial femoral head of φ28mm. No dislocation occurred up to 70-degree flexion and 90-degree internal rotation. No posterior instability was found.
When the assistant checked the anterior at external rotation in full extension, he forcibly caused anterior dislocation. At this time, the trial femoral head fell anteriorly and migrated within the pelvis through the site which resected anterior joint capsule. Because we had experienced Case 1, we did not try to retrieve it using fingers. The anterior wall of the pelvis was blocked by pressing from the surface of the skin around the groin region, and a large size Kocher was inserted in the anterior of the trial femoral head, to block any further migration in a deeper area. It was retrieved manually. When retrieving, no nerve/vascular injuries were observed. No complications were observed after 8 months of surgery, and the patient is progressing favorably.
DISCUSSION
Reports associated with the fall/ migration of a trial femoral head into the pelvis, as a complication during THA, are in existence for 7 cases, with a total of 11 examples so far6-12). However, it is believed that the frequency of occurrence is minimal. With respect to the surgical approach on the occurrence of the fall/ migration of trial femoral head into the pelvis, the Hardinge approach, anterior approach and posterior approach have been reported. In other words, it can occur with any type of approach. With respect to the occurrence situation, a slight tightness in the soft tissues was observed and no instability was mentioned. Instability of the hip joint was not observed either, in these cases. Therefore, it does not mean that a gentle stress in the hip joints or instability tends to cause the problem, but rather, it is assumed that it tends to occur when excessive tightness is observed.
In these case, when posterior impingement or anterior instability is assessed with external rotation in full extension, migration occurred because the assistant forcibly caused anterior dislocation. It was believed that the trial femoral head was flipped and migrated deeper in the pelvis, because of the additional excessive stress on the hip joint. In addition, the possibility was that it was easy to be dislocated forward because the anteversion of the acetabular cup of case1 was moderately excessive. Batouk at al. reported that the region in which the trial femoral head fell and migrated was the anterior of the sacroiliac joint6), while Alfonso et al. reported it was inside the retroperitoneum of the exterior of ilioposoas muscle9), Callaghan et al. reported that it was the inside surface of the psoas tendon8) and Wes et al. reported it was inside the psoas bursa7). In the present case, the trial femoral head was confirmed to be in the quadrilateral space within the pelvis, in an area lower than previous reports. It is believed that this was because the trial femoral head was flicked into the lower area, due to the dislocation in a high extension position, and furthermore because the surgeon pushed further with his fingers.
According to the previous report, there were only 3 examples in which trial femoral heads were left behind without being retrieved, while they were retrieved in 8 samples. With respect to the retrieval method, it has been reported that aortic cross-clamping was used for retrieval7), or an ilio-inguinal approach was developed for retrieval8), or when it migrated to the retroperitoneum, it was retrieved under laparoscopic vision9). How to handle retrieval of a trial femoral head is not difficult if it is retrieved in a calm manner. However, in case 1, because the surgeon tried to retrieve it with fingers from the very beginning, he was unable to grasp it properly and it slipped, resulting in further dislocation into a deep area of the pelvis. Retrieval from the original surgical wound was not possible. Because the corrosion of the trial head and the further movement were possible, it was sure that the retrieval was desirable. However, upon obtaining informed consent from the patient and her family, further efforts at retrieval were not attempted. It is recommended that a retrieval operation from the anterior be implemented together with an abdominal surgeon and vascular surgeon.
With regard to case 2, retrieval was possible by blocking the anterior, based on the experience in case 1. As shown in the above, when a trial femoral head is migrated into the pelvis, the retrieval becomes difficult. The hip joint of the patients receiving THA often showed significant contracture. Anterior joint capsule was usually reinforced by an iliofemoral ligament and a pubofemoral ligament. When we enlarge the surgical site, we must resect anterior joint capsule to obtain the better visual field and to release the hip contracture. If anterior joint capsule was completely resected, a trial head will easily migrate to the anterior space under the rectus femoris muscle (Figure5). Because we recommend that the anterior joint capsule resection should be a minimum. The extension and abduction test of the hip carried out because we should confirm anterior instability and posterior impingement. We suggest to have put gauze through the neck to control a stem because dislocation with the force prevented. We should operate it to avoid nerves, vascular injury if we perform grasp of a trial head with forceps as far as we can look it in the face.
Fig. 5.
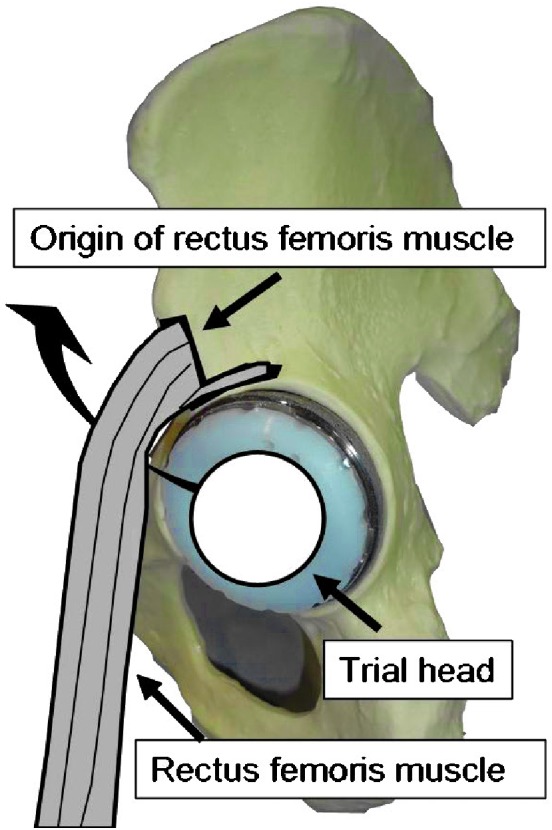
When anterior joint capsule was resected, the trial head arrived at the pelvic medial wall through the inside of the rectus femoris muscle.
It is recommended, as a means of preventing migration, that an anterior block be implemented with gauze packing10), if stress in the joint is strong, or a "necklace" be used, threading the trial femoral head9).
In conclusion we have experienced 2 cases in which migration of the trial femoral head into the pelvis during THA was observed, both of which were intraoperative complications. Attention is necessary for anterior dislocations when implementing the head trial. If the trial femoral head migrated, retrieve the trial head in a calm manner so that it will not further migrate into a deep area. It is necessary to recognize this as an intraoperative complication of THA.
Conflict of interest
The authors have declared no conflicts of interest.
REFERENCES
- 1).Bergqvist D, Carlsson AS, Ericsson BF. Vascular complications after total hip arthroplasty. Acta Orthop Scand, 1983 Apr; 54(2): 157–163. [DOI] [PubMed]
- 2).Pekkarinen J, Alho A, Puusa A, Paavilainen T. Recovery of sciatic nerve injuries in association with total hip arthroplasty in 27 patients. J Arthroplasty, 1999 Apr; 14(3): 305–311. [DOI] [PubMed]
- 3).Thillemann TM, Pedersen AB, Johnsen SP, Søballe K. Inferior outcome after intraoperative femoral fracture in total hip arthroplasty: outcome in 519 patients from the Danish Hip Arthroplasty Registry. Acta Orthop, 2008 Jun; 79(3): 327–334. [DOI] [PubMed]
- 4).Molli RG, Lombardi AV Jr, Berend KR, Adams JB, Sneller MA. A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res, 2012 Feb; 470(2): 450–461. [DOI] [PMC free article] [PubMed]
- 5).Mont MA, Jacobs JJ, Boggio LN, Bozic KJ, Della Valle CJ, Goodman SB, Lewis CG, Yates AJ Jr, Watters WC 3rd, Turkelson CM, Wies JL, Donnelly P, Patel N, Sluka P; AAOS. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg, 2011 Dec; 19(12): 768–776. [DOI] [PubMed]
- 6).Batouk O, Gilbart M, Jain R. Intraoperative dislocation of the trial femoral head into the pelvis during total hip arthroplasty: a case report. J Bone Joint Surg Am, 2001; 83–A: 1549–1551. [DOI] [PubMed]
- 7).Wes Y. Madsen, Bryan S. Mitchell, Stephen L. Kates. Successful intraoperative retrieval of dislocated femoral trial head during total hip arthroplasty. J Arthroplasty, 2012; 25(5): 820.e9–11. [DOI] [PubMed]
- 8).Callaghan JJ, McAndrew C, Boese CK, Forest E. Intrapelvic migration of the trial femoral head during total hip arthroplasty: is retrieval necessary? A report of four cases. Iowa Orthop J, 2006; 26: 60–62. [PMC free article] [PubMed]
- 9).Alfonso D, Idjadi J, Lamont JG. Retrieval of a trial femoral head that displaces into the periacetabular soft tissue during mini-incision total hip arthroplasty. A case report. J Bone Joint Surg Am, 2006; 88: 866–868. [DOI] [PubMed]
- 10).Princep A. Intraoperative migration of the trial femoral head into the pelvis during total hip arthroplasty: prevention and retrieval. J Bone Joint Surg Am, 2002; 84-A: 880–881. [DOI] [PubMed]
- 11).Ziv YB, Backstein D, Safir O, Kosashvili Y. Intraoperative dislocation of a trial femoral head into the pelvis during total hip arthroplasty. Can J Surg, 2008; 51: E73–74. [PMC free article] [PubMed]
- 12).Vertelis A, Vertelis L, Tarasevicius S. Trial femoral head loss in to the soft tissues of pelvis during primary total hip replacement: a case report. Cases J, 2008 Sep 12; 1(1): 151. [DOI] [PMC free article] [PubMed]
- 13).Kanoh T, Hasegawa Y, Masui T, Yamaguchi J, Kawabe K, Ishiguro N. Accurate acetabular component orientation after total hip arthroplasty using an acetabular alignment guide. J Arthroplasty, 2010 Jan; 25(1): 81–86. [DOI] [PubMed]