Abstract
Strategies to accelerate progress of India's family planning programme are discussed and the importance of improving the quality and reach of services to address unmet contraceptive need by providing method choice is emphasized. Although there is a growing demand for both limiting and spacing births, female sterilisation, is the dominant method in the national programme and use of spacing methods remains very limited. Fertility decline has been slower in the empowered action group (EAG) States which contribute about 40 per cent of population growth to the country and also depict gloomy statistics for other socio-development indicators. It is, therefore, important to intensify efforts to reduce both fertility and mortality in these States. A rationale has been provided for implementing integrated programmes using a gender lens because the lack of women's autonomy in reproductive decision-making, compounded by poor male involvement in sexual and reproductive health matters, is a fundamental issue yet to be addressed. The need for collaboration between scientists developing contraceptive technologies and those implementing family planning services is underscored. If contraceptive technologies are developed with an understanding of the contexts in which they will be delivered and an appreciation of end-users’ needs and perspectives, they are more likely to be accepted by service providers and used by clients.
Keywords: Contraceptive choice, contraceptive technologies, quality of services, users’ needs
Introduction
The family planning programme in India has had a long and somewhat turbulent history. It has, over the years, adopted a number of different strategic approaches including a coercive target approach, a policy articulating a reproductive health and rights paradigm, contraceptive-specific incentives, and a family planning camp approach, among others1,2,3,4,5,6,7,8,9,10. Fifty years later, the impact of the programme remains uneven, and India has yet to achieve replacement level fertility. Efforts are currently underway to reconceptualise and reposition the programme so that it can be more responsive to the country's needs which differ among regions and States. There is an urgent need to re-vitalise and energise programmatic efforts in the empowered action group (EAG) states where progress has been slow. Priority programme strategies for accelerating fertility decline and improving reproductive health outcomes are discussed in this reveiew.
Operationalising the concept of informed contraceptive choice
The first, and perhaps, the most important strategy that must be underscored is the need to translate within the national programme, the fundamental concept of informed contraceptive choice which, despite much rhetoric, has remained a mirage for the people of India. It is imperative that the principle of “the rights of couples and individuals to decide freely and responsibly the number and spacing of their children and to have the information and means to do so”11, is operationalised within the national programme. The need to do so is greater now than ever before because couples in India want to both limit family size and space their births. There is, therefore, an urgent need to provide a choice of contraceptive methods to enable couples to achieve their reproductive goals. However, female sterilisation, a terminal method, has for decades, remained the mainstay of the national programme. In 2005-2006, female sterilisation accounted for 66 per cent of contraceptive use. The majority of the women (77%) who underwent sterilisation had not used any method before they were sterilised and more than half were sterilised before they reached 26 years of age12. Although reported by a negligible minority, female sterilisation was the most commonly used method even by married adolescents13. India is, perhaps, the only country where such a pattern prevails.
India's public sector programme claims to provide a “cafeteria approach” with a “basket of choices”. The method-mix in this programme includes five official methods — female sterilisation, male sterilisation, intrauterine contraceptive device (IUCD), oral contraceptives, and condoms. But modern spacing methods account for a very small fraction (10%) of contraceptive use. Between 1998-199914 and 2005-200612, there was a minimal increase (from 6.8 to 10.1%) in the proportion of couples using oral contraceptives, IUCDs, and condoms. These data indicate that the programme has not, so far, succeeded in providing contraceptives to delay the first birth and to space subsequent births12,15. Nor has it been able to reach men. Even though the non-scalpel vasectomy technique has greatly simplified the procedure for male sterilisation and condoms have been seriously promoted for the prevention of HIV and other sexually transmitted infections, men's engagement in family planning has remained minimal12,15. Thus, contraceptive choice has yet to become a reality for the people of India.
Unmet need and unplanned pregnancy
Contraceptive needs of the people have changed dramatically over the past decades. In 2005-2006, the unmet need for contraception in India was 13 per cent, of which 6 per cent was for spacing methods12. Several studies show that unmet need for family planning is greatest in the 15-19 year olds, in the less educated and in the poorest households16,17,18,19. These findings underscore the urgent need to provide information and services to these couples who want to limit their family size and/or space their births but are not using any method of contraception.
In 2005-2006, 10 per cent of all pregnancies were mistimed (wanted later) and 11 per cent were not wanted12 indicating that about 20 per cent of all pregnancies (about 5.6 million) were unwanted and/or unplanned. A significant proportion of unwanted pregnancies are aborted, more than half under unsafe conditions. Infact, abortion is perceived by many to be an extension of the government's population stabilisation programme. About 8 per cent of maternal deaths are attributed to unsafe abortion in India20. Emergency contraception, a low cost, simple and effective technology, can provide a back-up method for women to use within the first few days of unprotected intercourse to prevent unwanted pregnancy. But despite considerable evidence-based advocacy with the government to promote this method, emergency contraception pills are essentially provided by the private sector mainly in urban areas. It is time for the public sector to institute a programme for providing emergency contraception. Its strategy should be to reach poor, rural women, who do not have access to the private sector. It has been estimated that if all unwanted births were eliminated and the unmet need for contraceptives was adequately met, India's total fertility rate would drop to replacement level12.
Early marriage and childbearing
Early marriage continues to be the norm in India. Data from the National Family Health Survey-3 (NFHS-3)12 show that in 2005-2006, more than two-fifths of all women aged 20-24 years were married before the legal minimum age of 18 years and almost one-half of married adolescents were mothers. Less than 10 per cent of these young couples had used any contraception. A sizeable proportion of births to adolescents were unplanned, underscoring that there is a substantial unmet need for contraception in this population sub-group. Married adolescents (15-19 years) constituted the largest group with unmet contraceptive need, especially for spacing methods. Unmet need among married adolescents was 27 per cent. And, as expected, the vast majority (25%) of unmet need for this group was for spacing methods12. Fig. 1 shows that between 1988-1989 and 2005-2006, there was no decline in the unmet need for contraception among married adolescents. As adolescents face several barriers (geographic and social) in accessing family planning and other reproductive health services, it is important to design and implement programmes strategies to overcome the special barriers that they encounter13.
Fig. 1.
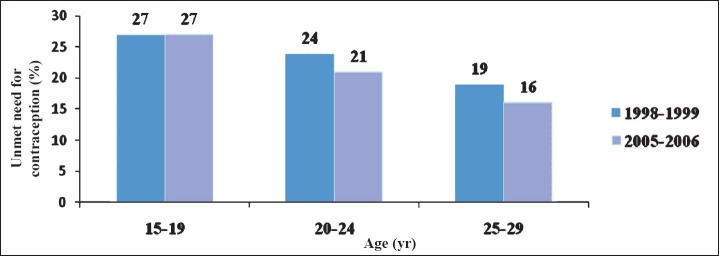
Unmet need for contraception among women in 1998-1999 and 2005-2006.
In India, childbearing is concentrated in the 20-29 year age group. Thus, in 2005-2006, women in this age group contributed over 60 per cent of total fertility; 24 per cent of these women had an unmet need for contraception of which 10 per cent was for spacing methods. These data indicate that there is an urgent need for providing these couples, with a choice of methods12.
In 2005-2006, the median interval between births for women was 31 months; 11 per cent of the births took place within 18 months and 28 per cent within 24 months. More than 60 per cent of births occurred within three years of the previous birth12. These data underscore the need for enhancing access to reversible contraceptive methods to improve birth spacing. There is ample evidence to show that adequate birth spacing has positive effects on the health of both the mother and the infant21,22,23,24,25,26. It is well documented that providing a choice of methods has multiple benefits. Method choice accelerates fertility decline and also reduces maternal, neonatal and infant mortality.
Improving quality of services to provide contraceptive choice
Data from NFHS-312 show that although the numbers are small, spacing methods are provided mainly by the private sector. Strategies to engage the private sector through social marketing and social franchising initiatives should be encouraged. But the public system, which is the major provider of family planning services, especially for the poor, must be strengthened so that a choice of methods can be provided by delivering quality services27,28,29,30,31. The need to strengthen infrastructure, human resources management, accountability and governance of the public health system has been repeatedly emphasized32 as these are major impediments to the effective delivery of health and family planning services33. Efforts to do so, however, have been uneven in the country.
It is time to focus serious attention on strengthening the health system's capacity to reach the unreached and to improve service quality. Improving the quality and reach of family planning services will not only address the issue of unmet contraceptive need and thereby accelerate fertility reduction, it will also have an impact on mortality. It is well documented that the life-time risk of maternal mortality declines with reduction in fertility because of the decrease in the number of pregnancies34. Fertility reduction can directly lower the maternal mortality ratio (MMR) by changing the age structure of the population35. Thus, reduction in fertility could bring about a decline in maternal mortality through these two mechanisms thereby, accelerating India's efforts to achieve millennium development goal (MDG 5).
Focusing on India's poorly performing States
Demographic transition is underway and fertility is declining in all the States of the country. A number of States have reached replacement level fertility. However, the pace of fertility decline has been slower in the larger, more populous EAG States (Fig. 2). These States also depict gloomy statistics for other socio-development indicators12. In these States the levels of education are lower, especially among girls, the status of women is lower, maternal and infant mortality rates are higher and poverty levels are higher. Couples also want larger families in these States. For example in 2005-2006, in Bihar and Uttar Pradesh, the contraceptive prevalence rates were 34.1 and 43.6 per cent, respectively (Fig. 3) and the total fertility rates were 4.0 and 3.8, respectively (Fig. 2)12.
Fig. 2.
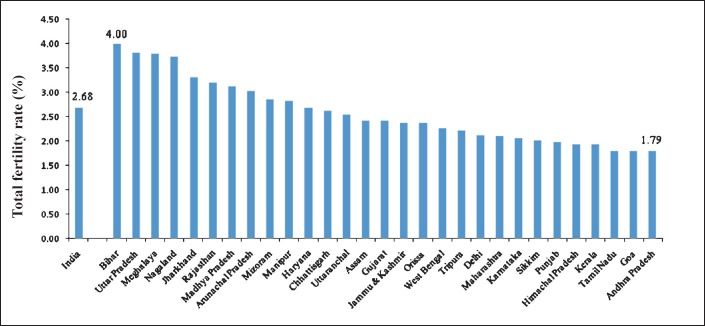
Total fertility rate by State, 2005-2006.
Source: Ref 12.
Fig. 3.
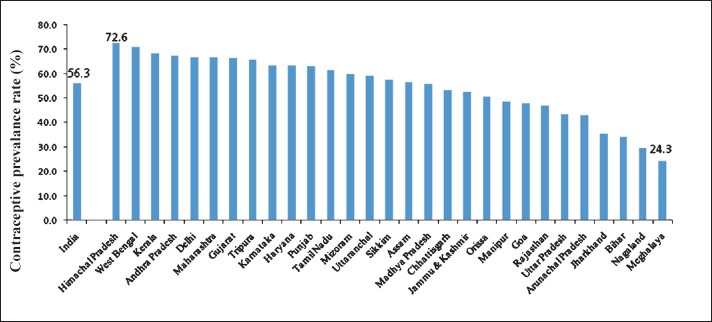
Contraceptive prevalence rate by State, 2005-2006
Source: Ref 12.
Preference for having a son is an important reason for having a larger number of unwanted births. India's declining sex ratio provides stark evidence to show that the girl child is unwanted36,37,38,39. Declining sex ratio is ironically an outcome of the fact that although many couples desire smaller families, they want to have one or two sons. The desired family size in Bihar is 3.5 and the most commonly desired family composition is one daughter and two or three sons40. In order to achieve this family composition, couples must have four or five children. There is, therefore, a clear need to focus efforts in Bihar and other EAG States to reduce fertility. These States have both wanted and unwanted fertility. To address the issue of wanted fertility, it is important to work with couples, families and communities to generate a demand for family planning services41. Thus far, efforts to generate demand have been limited. There is a need to work creatively with civil society organisations and community-based institutions such as panchayats and self help groups to mobilise communities and generate a demand for contraception and other reproductive health services42.
The EAG States depict high level of both fertility and mortality. In these States, women and children suffer higher rates of mortality and morbidity as well as malnutrition12. There is, therefore, a need to implement an integrated approach for providing health and family planning services. Recent years have witnessed renewed efforts to revitalise and energise the National Rural Heath Mission (NRHM) especially in the less developed States. The NRHM is committed to providing integrated services to address people's multiple health needs.
Convergence of services to address multiple needs of clients
Men, women and adolescents have multiple reproductive health needs including, but not limited, to the need for contraception. It is important to ensure a convergence of services at the clients’ level to effectively address their multiple needs. Vertical programmes, funded by various donors and implemented by different departments of government, have been found to be wasteful and inefficient43,44,45. Yet, the important principle of providing integrated services to address clients’ needs has not been operationalised.
There has been a recent resurgence of interest among donors and the government to design and implement integrated programmes to address the multiple needs of individuals, families and communities. For example, efforts being led by the Bill and Melinda Gates Foundation in the State of Bihar aim at implementing integrated interventions, included under the rubric of ‘family health’, for reducing fertility as well as maternal, neonatal, infant and child mortality and for improving reproductive health and nutrition. In addition to integrating health services, laudable efforts are also underway to integrate services for water and sanitation and agriculture with health interventions46. In implementing these programmes efforts are being made to strengthen both provision of services and generation of demand for services. With diminishing donor support, it is expected that in the next few years, services for HIV and AIDS prevention, treatment, care and support will be integrated within the Reproductive and Child Health (RCH) programme under the umbrella of the National Rural Health Mission (NRHM). As these integrated programmes are planned and implemented, it will be important to undertake programmatic research to facilitate the process of systematically upscaling these best practices.
An integrated approach must, necessarily, be designed using a gender lens because the lack of women's autonomy in reproductive decision-making compounded by the lack of men's involvement and responsibility in sexual and reproductive health matters, lies at the heart of the problem47,48,49. It is obvious that men's involvement in family planning remains negligible in India. In 2005-2006, a mere 9.1 per cent of married couples used male methods or couple dependent contraceptive methods. Vasectomy was used by 1.1 per cent and condoms by 5.5 per cent men in 2005-200612. Therefore, the need to design strategies to increase male participation is obvious48,49,50,51,52,53,54,55. But success in engaging men to take responsibility for family planning has proved to be elusive so far.
There is ample evidence to show that gender disparities not only have an impact on fertility outcomes but also adversely affect mortality and morbidity as well as mental and social wellbeing. The pernicious problem of domestic violence and its adverse consequences on the physical and mental health of women and children is well documented56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72. It is, therefore, important to design and implement strategies for reducing gender disparities that prevail across caste and class, among the rich and the poor, in rural and urban populations, as well as among the educated and uneducated sections of India's patriarchal society. Both short-term and long-term, well coordinated, multisectoral approaches will be needed to address this tenacious problem.
Ensuring collaboration between scientists who develop contraceptive technologies and those who plan and implement family planning services
Several organisations including the Indian Council of Medical Research (ICMR), the Population Council, private industry, and others are making large investments to develop contraceptive technologies. It takes significant resources and a long lead-time of about 10-15 years before a new technology is ready for introduction within family planning programmes. Scientists who develop technologies and professionals who implement programmes are, however, separate constituencies who, for the most part, work in their own worlds. Until recently, there has been little or no interaction between these two groups of professionals. There has been an implicit assumption and a widely-held belief that technologies are ‘magic bullets’ that can provide a ‘quick fix’. However, experience shows that technologies alone cannot address complex health and development problems. It is now being increasingly understood and acknowledged that technologies are not a panacea. In order to be effective, they must be tailored to local needs73,74.
Historical perspective
Contraceptive technologies have had a somewhat beleaguered history globally. After having contributed to women's liberation in the 1960s, these technologies became a very contentious issue and a subject of fierce criticism during the 1980s and 1990s75. Even today this critique continues in many settings. A current example to cite is the inability to include injectable contraceptives in the national programme in India primarily because of unrelenting opposition by feminists. Injectable contraceptives are available in the private sector but not in the public sector in India.
Women's health advocates in India remain suspicious of all hormonal contraceptives and especially of methods that are provider-dependent. They are concerned about their potential risks and the likelihood of their misuse and even abuse in programmes that do not have trained staff to effectively deliver these methods. In their view, quality of care and informed choice are essential prerequisites for including these technologies within the national programme73.
The irony is that on the one hand, women want contraceptive choice and on the other, they oppose the introduction of technologies. Women want quality care, and service providers to treat them with respect. They want full information and supportive counselling. They want follow-up care for complications and side-effects75. Women want to be able to switch methods when problems arise. These demands are perfectly legitimate but can only be met if the quality of services is improved.
Women's health advocates call for an approach in which women's health and reproductive needs shape the health and family planning services that they receive and their confidence and ability to make reproductive decisions is enhanced. This approach recognises that there are unequal power relations between men and women, between providers and users of services and between the state and its people. Women's health advocates have critiqued the process of contraceptive development because it ignores these power differentials. They have opposed the introduction of new methods into the public sector programme because of the inadequacies of its delivery system. They argue that the process of contraceptive development must incorporate a more comprehensive analysis of the contextual factors that can affect their safety and effectiveness73,76,77. They advocate for a participatory approach in which women and men are involved in setting the parameters for developing appropriate technologies.
A number of new contraceptive technologies are currently being developed in India and elsewhere. Several innovations to make contraceptives more effective, more acceptable, easy to use, user-controlled, etc are being tried. Efforts are underway to simplify methods of delivery78 through the development of sub-dermal implants79,80,81 as well as gels82,83 and patches that can be applied to the skin84. In addition, intra-vaginal rings85,86,87,88 that can be inserted by the woman herself, long-acting methods that minimize clinic visits, postpartum contraception89,90. male contraceptives91, and immuno-contraception92,93 are being developed and tested.
As promising new contraceptive technologies are developed, a dialogue should concurrently be promoted between scientists who are developing technologies in the laboratory and those who will eventually implement them within programmes in different settings. All these stakeholders must understand the needs and perspectives of the end-users of these technologies94,95. This ‘bench-to-bedside’ paradigm should be operationalised to promote such collaboration. If contraceptive technologies are designed with an understanding of the contexts in which they will be delivered and an appreciation of the needs and perspectives of the end users, there is a higher likelihood that they will be accepted by service providers and used by clients.
Conclusion
Despite a long history, spanning some five decades, India's family planning programme has not yet achieved replacement level fertility. Efforts are, therefore, currently underway to reconceptualise the programme to design and implement priority strategies for achieving programmatic goals. Couples in India have a significant unmet need for both limiting family size and spacing births. Yet, the national programme has not, so far, been successful in providing them with a choice of contraceptive methods. To translate the fundamental concept of informed contraceptive choice, it is imperative that the quality of services is improved. Context-specific, targetted strategies are needed to provide method choice to enable clients to achieve their reproductive goals. There is an urgent need to address the problem of high unmet contraceptive need among young couples especially among married adolescents.
The pace of decline in both fertility and mortality has been slower in the empowered action group (EAG) States. It is, therefore, important to focus efforts and resources in these States. Integrated programmes, that can more effectively and efficiently address multiple reproductive health needs of the people should be implemented. Such integrated programmes must necessarily be designed using a gender lens as in India's patriarchal society son preference remains strong. Son preference results in larger families as couples try to achieve their desired family composition.
Several promising contraceptive technologies are currently in the pipeline. But for these technologies to be effectively delivered by service providers and accepted by clients, it is important that scientists developing technologies collaborate with professionals engaged with planning and implementing programmes and for all stakeholders to understand the needs and perspectives of the end-users of these technologies. Long years of experience in developing contraceptive technologies and undertaking field-based operations research on family planning programmes has provided valuable lessons. If these key principles are operationalised, it would be possible to develop appropriate contraceptive technologies that can be effectively delivered by the national programme and used by its clients.
References
- 1.New Delhi: Ministry of Health and Family Welfare; 1996. Government of India. Target-free approach in family welfare programme. [Google Scholar]
- 2.Khan ME, Townsend J. Target free approach: Emerging evidence. In: Pachauri S, Subramanian S, editors. Implementing a reproductive health agenda in India: The beginning. New Delhi: Spectra VisualWord; 1999. pp. 41–74. [Google Scholar]
- 3.Pachauri S. Moving towards reproductive health: Issues and evidence. In: Pachauri S, Subramanian S, editors. Implementing a reproductive health agenda in India: The beginning. New Delhi: Spectra VisualWord; 1999. pp. xiii–xlvii. [Google Scholar]
- 4.Washington D.C., USA: World Bank; 1995. World Bank. India's family welfare programme: Towards a reproductive and child health approach. Population and Human Resources Division, South Asia Country Department II, Report No. 14644 – IN. [Google Scholar]
- 5.Pachauri S. India's family welfare program: Towards a reproductive and child health approach. Population and Human Resources, Operations Division. The World Bank, South Asia Country Department (India, Nepal and Bhutan) Washington D.C., USA: World Bank; 1996. Reproductive and child health services; pp. 46–52. [Google Scholar]
- 6.Pachauri S. A shift from family planning to reproductive health: New challenges. In: Srinivasan K, editor. Population policy and reproductive health. New Delhi: Population Foundation of India; 1996. [Google Scholar]
- 7.Rao M. Family planning programme: Paradigm shift in strategy. Econ Polit Weekly. 2000;35:4317–22. [Google Scholar]
- 8.Germaine A, Nowrojee S, Pyne HH. Setting a new agenda: Sexual and reproductive health and rights. In: Sen G, Germaine A, Chen LC, editors. Population policies reconsidered: Health, empowerment and rights. Harvard Series on Population and International Health. Boston: Harvard University Press; 1994. pp. 27–46. [Google Scholar]
- 9.Jain A, Bruce J. A reproductive health approach to the objectives and assessment of family planning programs. In: Sen G, Germaine A, Chen LC, editors. Population policies reconsidered: Health empowerment and rights. Boston: Harvard University Press; 1994. pp. 192–211. [Google Scholar]
- 10.New Delhi: MOHFW, Government of India, 2000; 2000. Ministry of Health and Family Welfare (MOHFW). National Population Policy. [Google Scholar]
- 11.New York: United Nation; 1994. [accessed on September 16, 2014]. United Nations. International conference on population and development. Available from: http://www.un.org/popin/icpd/conference/offeng/poa.html . [Google Scholar]
- 12.I. India, Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06. [Google Scholar]
- 13.Mumbai: IIPS; 2010. International Institute for Population Sciences, Population Council. Youth in India: Situation and needs 2006-2007, Executive Summary. [Google Scholar]
- 14.I. Mumbai: IIPS; 2001. International Institute for population Sciences (IIPS) and Macro International. National Family Health Servery (NFHS-2) 1998-99. [Google Scholar]
- 15.Pachauri S. Expanding contraceptive choice in India: Issues and evidence. J Fam Welfare. 2004;50:13–25. [Google Scholar]
- 16.Ganatra B, Hirve SS. Induced abortions among adolescent women in rural Maharashtra. Reprod Health Matter. 2002;10:76–85. doi: 10.1016/s0968-8080(02)00016-2. [DOI] [PubMed] [Google Scholar]
- 17.Pachauri S, Santhya KG. Socio-demographic and reproductive health profile of adolescents in India: A review. Demography India. 2002;31:163–78. [Google Scholar]
- 18.Pachauri S, Santhya KG. Reproductive choices for Asian adolescents: A focus on contraceptive behaviour. Int Fam Plann Perspect. 2002;28:186–95. [Google Scholar]
- 19.Santhya KG, Jejeebhoy SJ. Sexual and reproductive health needs of married adolescent girls. Econ Polit Weekly. 2003;38:4370–7. [Google Scholar]
- 20.New Delhi: Registrar General of India; 2001-2003. Registrar General of India. Sample registration system statistical report 2001-2003. [Google Scholar]
- 21.Conde-Agudelo A, Anyeli Rosas-Bermúdez, Ana Cecilia Kafury-Goeta. Birth spacing and the risk of adverse perinatal outcomes: A meta-analysis. JAMA. 2006;295:1809–23. doi: 10.1001/jama.295.15.1809. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad P, Khan AZ, Hasan B, Sinha SN. Morbidity pattern in relation to birth interval and birth order in children. Indian J Pediatr. 1982;49:689–93. doi: 10.1007/BF02752655. [DOI] [PubMed] [Google Scholar]
- 23.Cleland JG, Zeba AS. The effect of birth spacing on childhood mortality in Pakistan. Popul Stud. 1984;38:401–18. doi: 10.1080/00324728.1984.10410300. [DOI] [PubMed] [Google Scholar]
- 24.Conde-Agudelo A, Rosas-Bermudez A, Castano F, Norton HM. Effects of birth spacing on maternal, perinatal, infant, and child health: A systematic review of causal mechanisms. Stud Fam Plann. 2012;43:93–114. doi: 10.1111/j.1728-4465.2012.00308.x. [DOI] [PubMed] [Google Scholar]
- 25.Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC. Effects of birth spacing on maternal health: A systematic review. Am J Obstet Gynecol. 2007;196:297–308. doi: 10.1016/j.ajog.2006.05.055. [DOI] [PubMed] [Google Scholar]
- 26.Dewey KG, Cohen RJ. Does birth spacing affect maternal or child nutritional status? A systematic literature review. Matern Child Nutr. 2007;3:151–73. doi: 10.1111/j.1740-8709.2007.00092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pachauri S. Washington D.C., USA: World Bank; 1995. Defining an essential package of reproductive and child health services. In: India's family welfare program: Towards a reproductive and child health approach. Population and Human Resources, Operations Division, The World Bank, South Asia Country Department (India, Nepal and Bhutan) [Google Scholar]
- 28.Narang R. Measuring perceived quality of health care services in India. Int J Health Care Qual Assur. 2010;23:171–86. doi: 10.1108/09526861011017094. [DOI] [PubMed] [Google Scholar]
- 29.Rama Rao S, Lacuesta M, Costello M, Pangolibay B, Jones H. The link between quality of care and contraceptive use. Int Fam Plann Perspect. 2003;29:76–83. doi: 10.1363/ifpp.29.076.03. [DOI] [PubMed] [Google Scholar]
- 30.Khan ME, Gupta RB, Patel BC. The quality and coverage of family planning services in Uttar Pradesh: Client perspectives. In: Koenig MA, Khan ME, editors. Improving quality of care in India's family welfare programme: The challenge ahead. New York: Population Council; 1999. [Google Scholar]
- 31.Koenig MA, Foo GHC, Joshi K. Quality of care within the Indian family welfare programme: A review of recent evidence. Stud Fam Plann. 2000;31:1–18. doi: 10.1111/j.1728-4465.2000.00001.x. [DOI] [PubMed] [Google Scholar]
- 32.Pachauri S. Editorial. Sexual and reproductive health services: Priorities for South and East Asia. Indian J Community Med. 2011;36:83–4. doi: 10.4103/0970-0218.84116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.United Nations Development Programme (UNDP), Achieving MDGs in India. [accessed on September 16, 2014]. Available from: http://www.in.undp.org/content/india/en/home/mdgoverview .
- 34.Wilmoth J. The lifetime risk of maternal mortality: Concept and measurement. Bull World Health Organ. 2009;87:256–62. doi: 10.2471/BLT.07.048280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jain A. Measuring the effect of fertility decline on the maternal mortality ratio. Stud Fam Plann. 2011;42:247–60. doi: 10.1111/j.1728-4465.2011.00288.x. [DOI] [PubMed] [Google Scholar]
- 36.New Delhi: United Nations Population Fund; 2001. United Nations Population Fund. Sex-selective abortions and fertility decline: The case of Haryana and Punjab. [Google Scholar]
- 37.Kaur R. Khap panchayats, sex ratio and female agency. Econ Polit Weekly. 2010 Jun 5;45:14–6. [Google Scholar]
- 38.Kaur R, John M, Palriwala R, Raju S, Sagar A. Bangalore, India: ActionAid and IDRC, Books for Change; 2008. Planning families, planning gender: The adverse child sex ratio in selected districts of Madhya Pradesh, Rajasthan, Himachal Pradesh, Haryana and Punjab. [Google Scholar]
- 39.New Delhi: Ministry of Health & Family Welfare; 2003. Ministry of Health and Family Welfare, Office of the Registrar General and Census Commissioner, India United Nations Population Fund (UNFPA). Missing.... Mapping the adverse child sex ratio in India. [Google Scholar]
- 40.Bhatnagar I, Khan ME, Hazra A. New Delhi: Population Council; 2011. Increasing acceptance of spacing methods in rural Bihar: Implications for behaviour change communication. Policy Brief No. 5. [Google Scholar]
- 41.Darmstadt GL, Tarigopula UK. Behavior change communication as an intervention to improve family health outcomes. J Fam Welfare. 2010;56:1–8. [Google Scholar]
- 42.Pachauri S. New Delhi: Program for Appropriate Technology in Health (PATH), National Working Group Meeting on Convergence; 2009. Options and challenges for converging health and other social services. [Google Scholar]
- 43.Pachauri S. Sexual and reproductive health services: Priorities for South and East Asia. Indian J Community Med. 2011;36:83–4. doi: 10.4103/0970-0218.84116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pachauri S. Relationship between AIDS and family planning programmes: A rationale for developing integrated reproductive health services. HTR. 1994;4(Supp):321–47. [PubMed] [Google Scholar]
- 45.Ringheim K, Yeakey M, Gribble J, Sines E, Stepahin S. Policy Brief. Washington, D.C: Population Reference Bureau; 2009. Supporting the integration of family planning and HIV services. [Google Scholar]
- 46.Bill and Melinda Gates Foundation. [accessed on September 16, 2014]. Available from: www.gatesfoundation.org .
- 47.Murthi M, Guio AC, Dreze J. Mortality, fertility and gender bias in India: A district-level analysis. Popul Dev Rev. 1995;21:745–82. [Google Scholar]
- 48.Raju S, Leonard A, editors. New Delhi: Population Council; 2000. Men as supportive partners in reproductive health: Moving from rhetoric to reality. [Google Scholar]
- 49.Karra MV, Stark NN, Wolf J. Male involvement in family planning: A case study spanning five generations of a South Indian family. Stud Fam Plann. 1997;28:24–34. [PubMed] [Google Scholar]
- 50.Pachauri S. Special Article. Male involvement in reproductive health care. J Indian Med Assoc. 2001;99:138–41. [PubMed] [Google Scholar]
- 51.Barua A, Pande RP, MacQuarrie K, Walia S. Caring men? Husbands’ involvement in maternal care of young wives. Econ Polit Weekly. 2004;39:5661–8. [Google Scholar]
- 52.Greene ME, Barker G. Masculinity and its public health implications for sexual and reproductive health and HIV prevention. In: Parker R, Sommer M, editors. Handbook of global public health. London: Routledge; 2011. [Google Scholar]
- 53.Piet-Pelon NJ, Rob U, Khan ME, editors. New Delhi: Hindustan Publishing Corporation; 1999. Men in Bangladesh, India and Pakistan: Reproductive health issues. [Google Scholar]
- 54.Raju S. Men as supportive partners in reproductive health: NGOs pave the way. In: Pachauri S, Subramanian S, editors. Implementing a reproductive health agenda in India: The beginning. New Delhi, India: Spectra VisualWord; 1999. pp. 303–24. [Google Scholar]
- 55.Verma RK, Pulerwitz J, Mahendra VS, Khandekar S, Barker G, Fulpagare P, Singh SK. Challenging and changing gender attitudes among young men in India. Reprod Health Matter. 2006;14:1–10. doi: 10.1016/S0968-8080(06)28261-2. [DOI] [PubMed] [Google Scholar]
- 56.Jejeebhoy SJ. Associations between wife-beating and foetal and infant death: Impressions from a survey in rural India. Stud Fam Plann. 1998;29:300–8. [PubMed] [Google Scholar]
- 57.Verma RK, Collumbien M. Wife beating and the link with poor sexual health and risk behaviour among men in urban slums in India. J Com Fam Stud. 2003;34:61–74. [Google Scholar]
- 58.Kumar S, Jeyaseelan L, Suresh S, Ahuja RC. Domestic violence and its mental health correlates in Indian women. Br J Psychiat. 2005;187:62–7. doi: 10.1192/bjp.187.1.62. [DOI] [PubMed] [Google Scholar]
- 59.Chowdhary N, Patel V. The effect of spousal violence on women's health: Findings from the Stree Arogya Shodh in Goa, India. J Postgrad Med. 2008;54:306–12. doi: 10.4103/0022-3859.43514. [DOI] [PubMed] [Google Scholar]
- 60.Singh A, Mahapatra B, Dutta S. Spousal abuse and infant and child mortality in India. Asia Pac Popul J. 2008;23:33–54. [Google Scholar]
- 61.Stephenson R, Koenig MA, Acharya R, Roy TK. Domestic violence, contraceptive use and unwanted pregnancy in rural India. Stud Fam Plann. 2008;39:177–86. doi: 10.1111/j.1728-4465.2008.165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Koenig M, Stephenson R, Acharya R, Barrick L, Ahmed S, Hindin M. Domestic violence and early childhood mortality in rural India: Evidence from prospective data. Int J Epidemiol. 2010;39:825–33. doi: 10.1093/ije/dyq066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ackerson LK, Subramanian SV. Intimate partner violence and death among infants and children in India. Pediatrics. 2009;124:e878–89. doi: 10.1542/peds.2009-0524. [DOI] [PubMed] [Google Scholar]
- 64.Chhabra S. Sexual violence among pregnant women in India. J Obstet Gynaecol. 2008;34:238–41. doi: 10.1111/j.1447-0756.2008.00761.x. [DOI] [PubMed] [Google Scholar]
- 65.Stephenson R, Koenig MA, Ahmed S. Domestic violence and symptoms of gynaecologic morbidity among women in North India. Int Fam Plan Perspect. 2006;32:201–8. doi: 10.1363/3220106. [DOI] [PubMed] [Google Scholar]
- 66.Duvvury N, Nayak M, Allendorf K. Washington, DC: International Centre for Research on Women; 2002. Links between masculinity and violence: Aggregate analysis. Domestic Violence in India: Exploring strategies, promoting dialogue. Men masculinity and domestic violence in India: Summary report of four studies; pp. 52–70. [Google Scholar]
- 67.Shagun S, McCormick MC, Subramanian SV, Silverman JG. Son preference and intimate partner violence victimization in India: Examining the role of actual and desired family composition. J Biosoc Sci. 2012;44:43–56. doi: 10.1017/S002193201100037X. [DOI] [PubMed] [Google Scholar]
- 68.Martin S, Kilgallen B, Tsui AO, Maitra K, Singh KK, Kupper LL. Sexual behaviors and reproductive health outcomes: Associations with wife abuse in India. JAMA. 1999;282:1967–72. doi: 10.1001/jama.282.20.1967. [DOI] [PubMed] [Google Scholar]
- 69.Raj A, Saggurti N, Lawrence D, Balaiah D, Silverman JG. Association between adolescent marriage and marital violence among young adult women in India. Int J Gynaecol Obstet. 2010;110:35–9. doi: 10.1016/j.ijgo.2010.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Santhya KG, Ram U, Acharya R, Jejeebhoy SJ, Ram F, Singh A. Associations between early marriage and young women's marital and reproductive health outcomes: Evidence from India. Int Perspect Sex Reprod Health. 2010;36:132–9. doi: 10.1363/ipsrh.36.132.10. [DOI] [PubMed] [Google Scholar]
- 71.Jejeebhoy SJ, Santhya KG, Acharya R. New Delhi: Population Council and UNFPA; 2010. Health and social consequences of marital violence: A synthesis of evidence from India. [Google Scholar]
- 72.Silverman JG, Decker MR, Cheng DM, Wirth K, Saggurti N, McCauley HL, et al. Gender-based disparities in infant and child mortality based on maternal exposure to spousal violence: The heavy burden borne by Indian girls. Arch Pediatr Adolesc Mede. 2011;165:22–7. doi: 10.1001/archpediatrics.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Salhan S, Tripathi V. Factors influencing discontinuation of intrauterine contraceptive devices: an assessment in the Indian context. Eur J Contracept Reprod Health Care. 2004;9:245–59. doi: 10.1080/13625180400017495. [DOI] [PubMed] [Google Scholar]
- 74.Mallik R. Beyond the magic bullet: Introduction of emergency contraceptive pills in India. Centre for Health and Gender Equity. 2003. [accessed on September 16, 2014]. Available from: https://nwhn.org/emergencycontraceptives-india-beyond-magic-bullet .
- 75.Prakasamma M. Jaipur: Health Watch Trust; 1999. Community need-based reproductive and child health in India: Progress and constraints; pp. 18–31. [Google Scholar]
- 76.Pachauri S. Coerced contraception? Moral and policy challenges of long-acting birth control. Stud Fam Plann. 1997;28:166–7. [Google Scholar]
- 77.Sundari TK, Berer M, Cottingham J, editors. Geneva: World Health Organization; 1997. Beyond acceptability: User's perspectives on contraception. [Reprod Health Matter] [Google Scholar]
- 78.Sitruk-Ware R. Delivery options for contraceptives. Drug Discov Today. 2005;10:977–85. doi: 10.1016/S1359-6446(05)03499-9. [DOI] [PubMed] [Google Scholar]
- 79.Diaz S, Peralta O, Juez G, Herreros C, Casado ME, Salvatierra AM, et al. Fertility regulation in nursing women. Contraceptive effectiveness of a subdermal progesterone implant. Contraception. 1984;30:311–25. doi: 10.1016/s0010-7824(84)80023-2. [DOI] [PubMed] [Google Scholar]
- 80.Croxatto HB, Diaz S. Subdermal progesterone implants for fertility regulation in nursing women. In: Zatuchni GI, Goldsmith A, Shelton JD, Sciara JJ, editors. Long-acting contraceptive delivery systems. Philadelphia: Harper & Row; 1984. pp. 311–25. [Google Scholar]
- 81.Diaz S, Zepeda A, Maturana X, Reyes MV, Miranda P, Casado ME, et al. Fertility regulation in nursing women. Contraceptive performance, duration of lactation infant growth, and bleeding patterns during use of progesterone vaginal rings, progestin-only pills, Norplant implants, and Copper T 380-A intrauterine devices. Contraception. 1997;56:223–32. doi: 10.1016/s0010-7824(97)00135-2. [DOI] [PubMed] [Google Scholar]
- 82.Mahabadi V, Amory JK, Swerdloff RS, Bremner WJ, Page ST, Sitruk-Ware R, et al. Combined transdermal testosterone gel and the progestin Nestorone suppresses serum gonadotropins in men. J Clin Endocrinol Metab. 2009;94:2313–20. doi: 10.1210/jc.2008-2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brache V, Croxatto HB, Kumar N, Sitruk-Ware R, Cochón L, Schiappacasse V, et al. Effect of sexual intercourse on the absorption of levonorgestrel after vaginal administration of 0.75mg in Carraguard® gel: A randomized, cross-over, pharmacokinetic study. Contraception. 2009;79:150–4. doi: 10.1016/j.contraception.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fraser IS, Weisberg E, Kumar N, Kumar S, Humberstone AJ, McCrossin L, et al. An initial pharmacokinetic study with a Metered Dose Transdermal System® for delivery of the progestogen Nestorone® as a possible future contraceptive. Contraception. 2007;76:432–8. doi: 10.1016/j.contraception.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 85.Brache V, Sitruk-Ware R, Williams A, Blithe D, Croxatto H, Kumar N, et al. Effects of a novel estrogen-free, progesterone receptor modulator-contraceptive vaginal ring on inhibition of ovulation, bleeding patterns and endometrium in normal women. Contraception. 2012;85:480–8. doi: 10.1016/j.contraception.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nath A, Sitruk-Ware R. Progesterone vaginal ring for contraceptive use during lactation. Contraception. 2010;82:428–34. doi: 10.1016/j.contraception.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 87.Croxatto HB, Dıaz S. Progesterone vaginal rings for contraception during breastfeeding. In: Runnebaum B, Rabe T, Kiesel L, editors. Advances in gynecological and obstetric research series. Female contraception and male fertility regulation. II. New Jersey: The Parthenon Publishing Group; 1991. pp. 135–42. [Google Scholar]
- 88.Sivin I, Diaz S, Croxatto HB, Miranda P, Shaaban M, Sayed EH, et al. Contraceptives for lactating women: A comparative trial of a progesterone-releasing vaginal ring and the copper T 380A IUD. Contraception. 1997;55:225–32. doi: 10.1016/s0010-7824(97)00008-5. [DOI] [PubMed] [Google Scholar]
- 89.Eroglu K, Akkuzu G, Vural G, Dilbaz B, Akin A, Taskin L, et al. Comparison of efficacy and complications of IUD insertion in immediate postplacental/early postpartum period with interval period: 1 year follow-up. Contraception. 2006;74:376–81. doi: 10.1016/j.contraception.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 90.Lara RR, Menocal TG, Ramos PC, Velazquez RN. Random comparative study between intrauterine device Multiload Cu375 and TCu 380A inserted in the postpartum period. Ginecol Obstet Mex. 2006;74:306–11. [PubMed] [Google Scholar]
- 91.Liu PY, Swerdloff RS, Anawalt BD, Anderson RA, Bremner WJ, Elliesen J, et al. Determinants of the rate and extent of spermatogenic suppression during hormonal male contraception: An integrated analysis. J Clin Endocrinol Metab. 2008;93:1774–83. doi: 10.1210/jc.2007-2768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Talwar GP. Fertility regulating and immunotherapeutic vaccines reaching human trials stage. Hum Reprod Update. 1997;3:301–10. doi: 10.1093/humupd/3.4.301. [DOI] [PubMed] [Google Scholar]
- 93.Talwar GP, Hingorani V, Kumar S, Roy S, Banerjee A, Shahani SM, et al. Phase I clinical trials with three formulations of anti-human chorionic gonadotropin vaccine. Contraception. 1990;41:301–16. doi: 10.1016/0010-7824(90)90071-3. [DOI] [PubMed] [Google Scholar]
- 94.Sanchez S, Araya C, Tijero M, Diaz S. Women's perceptions and experience with the progesterone vaginal ring for contraception during breastfeeding. Beyond acceptability: User's perspectives on contraception Reprod Health Matter. 1997. [accessed on September 16, 2014]. pp. 49–57. Available from: http://www.rhmjournal.org.uk/publications/beyond-acceptability/049_Sanchez.pdf .
- 95.Gilliam M, Holmquist S, Berlin A. Factors associated with willingness to use the contraceptive vaginal ring. Contraception. 2007;76:30–4. doi: 10.1016/j.contraception.2007.03.009. [DOI] [PubMed] [Google Scholar]


