Key messages
The primary care practices in rural Colorado are actively implementing many aspects of the medical home.
Rural practices share PCMH aspirations including commitment to quality, safety, outcomes, cost reduction, and patient and provider satisfaction.
However, there are some aspects that may not be as relevant for some practices and communities.
The unique nature of primary care practice requires adaption and provider input into medical home implementation efforts.
Why this matters to us
The High Plains Research Network aspires to engage patients and primary care providers in all our work. The patient-centred medical home (PCMH) has become a popular model for implementing the core tenets of primary care including accessible, comprehensive, coordinated, team-based care in the context of the local community. As we visited primary care practices throughout rural eastern Colorado, we frequently heard concerns from medical providers that the required elements of the PCMH were not necessarily relevant to their patients in their community. The practices wanted to collaborate on a project to identify the most relevant and beneficial elements of the PCMH model for their community. We undertook this study as a way to add the local patient and primary care provider voice to the ongoing PCMH conversation.
Keywords: patient-centred medical home, practice-based research network, rural health
Abstract
Context The patient-centred medical home (PCMH) has become a dominant model for improving the quality and cost of primary care. Geographic isolation, small populations, privacy concerns and staffing requirements may limit implementation of the PCMH in clinical practice.
Objective To determine the primary care provider perceived benefit of PCMH for patients in rural Colorado.
Design, setting and participants The High Plains Research Network (HPRN) is a community and practice-based research network spanning 30 000 square miles in 16 counties in eastern Colorado. The HPRN consists of 58 practices, 120 primary care clinicians and 145 000 residents.
Main outcome measures Providers' perceived benefit of PCMH for individual patients.
Results Seventy-eight providers in 37 practices saw 1093 patients and completed 1016 surveys. There was wide variation among the provider-perceived benefits of PCMH elements ranging from 9% for group visits to 64% for electronic prescribing. Provider-perceived benefit was higher for patients with a chronic medical condition.
Conclusions Rural primary care providers perceived patient benefit for numerous elements of the PCMH. There is need to consider what PCMH elements may be required in practice and what components might be optional. Our findings reveal that rural practices share PCMH aspirations including commitment to quality, safety, outcomes, cost reduction, and patient and provider satisfaction. These findings support the need for ongoing conversation about how to best provide a locally relevant medical home.
Context
The patient-centred medical home (PCMH) has become a dominant model for improving the quality and cost of primary care.1–7 According to the National Committee on Quality Assurance (NCQA), the PCMH encompasses five core functions: comprehensive health care, a relationship-based whole person-centred approach, coordination of care, improved accessibility to primary care, and quality and safety.8,9 To measure practices' progress towards and achievement of these broad functions, the NCQA created six categories of PCMH standards, which are further divided into more defined, practice-level elements. These elements, which are the focus of this study, represent specific tools and resources that a practice must have in place and activities that a practice is required to perform in order to receive national certification or recognition, a frequent requirement for enhanced reimbursement.9,10 A list of the PCMH elements included in this study is given in Box 1.
Box 1. Patient-centred medical home care study elements.
Patient access to care outside normal office hours
Secure email with patients/patient remote access to health information (e.g. patient portal, personal health record, test results)
Pre-visit planning with staff (e.g. staff data gathering, ‘team huddle’)
Plan for post-visit activity/communication with patient by staff (e.g. referral and lab tracking, follow-up appointment, health maintenance)
Staff initiative and/or collaboration in patient education (in-practice or community resources)
Family involvement in care planning and/or disease management
Health assessment (e.g. prevention, health behaviours, mental health, behavioural health)
Group patient visit
Electronic health/medical record
Electronic prescribing
Medication reconciliation (e.g. EHR, sorting pill bottles, nurse review of medication list)
Tracking system for clinical information (e.g. lab, imaging, consults, discharge summaries)
Patient registry practice-wide database for patients with this/these diagnoses
Evidence-based practice protocol(s) for managing patient's diagnoses
Reminders to provider at time of visit for managing patient's care (e.g. preventive health, chronic disease management)
Safety and quality check routines in the practice
Efficient method for sharing patient information with other provider(s)/facility(ies)
Medical neighbourhood (explicit agreement with specialists/services for sharing patient care)
How are primary care providers incorporating medical home concepts and activities into their usual practice? Goldberg and Kuzel report wide practice variation in physician-reported use of PCMH elements, ranging from 87% for ‘continuity-of-care’ to just 19% for patient registries. Numerous authors have described the potential and real benefits that derive from adhering to the principles and core activities that underlie the PCMH concept.11–14 Several programmes aimed at implementing the PCMH have tested implementation strategies and patient outcomes.15–17 The American Academy of Family Physicians has implemented TransforMED, a 24-month tailored implementation of an early model of the PCMH that focused in particular on health information technology.18,19 The investigators found that practice transformation involves much more than a one-time implementation of a few new activities. Becoming a learning organisation capable of ongoing improvement and change requires motivated and engaged providers and staff, and organisational persistence.20 In their study, small improvements were found in some measures of quality of care, but no enhancement was found in patients' experience.21
Although PCMH implementation is in full swing, many practices are simultaneously attempting to implement an electronic health record (EHR). The PCMH has been actively pushed as a component of meaningful use of the EHR, and vice versa.22–25 The Health Information Technology for Economic and Clinical Health (HITECH) legislation provides financial incentives for rapid implementation of EHRs and data sharing. However, a recent Agency for Health Research and Quality (AHRQ) report stated that EHR support alone is necessary, but not sufficient, to fully implement the PCMH.26
Ultimately, if the PCMH is to improve patient outcomes and satisfaction, it must offer care that matters to patients and their providers. Although generally interested and supportive, many primary care providers in the High Plains Research Network (HPRN) voiced concerns about implementation of PCMH in their practice and community. Rural providers face a unique set of challenges to implementing some aspects of the PCMH. As the sole site of care in the community, providers already feel that they are a medical home. Geographic isolation, small populations, privacy concerns, staffing needs and limited high-speed connectivity may limit full implementation of some parts of the PCMH. Given these concerns, HPRN conducted a study to determine providers' perceived benefit of the elements of the PCMH for patients seeking care in family medicine clinics.
Design, setting and participants
Housed in the Department of Family Medicine at the University of Colorado Denver Anschutz Medical Campus, the HPRN is a community- and practice-based research network spanning 30 000 square miles in 16 counties in eastern Colorado. HPRN consists of 58 primary care practices, 120 primary care clinicians, 14 nursing homes, 24 behavioural health clinics, 7 public health departments and 145 000 residents. HPRN counties are considered medically underserved or health professional shortage areas. The HPRN is guided by an active Community Advisory Council (CAC) of local farmers, ranchers, schoolteachers, business owners, students and healthcare providers to assure that the research is grounded in real patient and provider experiences. While visiting practices, the HPRN staff repeatedly heard that some of the required PCMH elements would not provide benefit to their patients and that some were difficult to implement. For instance, one solo physician reported that she could not provide additional hours of access in the evening or weekends as she was the only provider available.
An observational ‘card study’ (Box 2) research project was conducted between April 2012 and January 2013.29 The card study focused on 18 of the 27 PCMH elements defined by NCQA (Box 1). The selected elements (17) were considered the most relevant to patient-specific visits, representing tools or activities a provider could employ during an individual patient visit. An 18th element, defined as medical neighbourhood, was created and added to this study to represent formal, written protocols and agreements with a wide range of healthcare facilities and community resources, beyond hospitals. Nine elements were not included in this study as they apply more closely to overall office functioning. These elements were continuity, culturally appropriate services, practice organisation and six elements pertaining to broad practice performance improvement, measurement and reporting. HPRN staff assisted with collection of the surveys to decrease the research burden on the practice.
Box 2. Card study survey methods.
Participating providers completed a survey for each patient they saw during one day of clinical care. The survey collected demographic data, whether the patient had any chronic illness and the reason for visit. The survey then asked, ‘Which components of the patient-centred medical home (PCMH) do you believe did or would have benefitted this patient?’ The provider was instructed to check all PCMH element they believed would benefit that specific patient. Providers were encouraged to complete the survey as soon as they finished seeing each patient. Completed anonymous surveys were returned at the end of the day. Practices provided the total number of patients seen by each provider on the study day.
The practice manager was interviewed to ascertain each practice's current implementation of PCMH elements. HPRN staff asked about each element of the PCMH to determine whether the practice had implemented each element, had plans to implement, was interested in implementing or had no plans for implementation. If a practice manager reported that the PCMH element had been implemented, the HPRN staff asked additional questions to provide a clear snapshot of the true extent of PCMH implementation.
We developed a PCMH score for each practice based on its level of implementation. Because no current validated rural PCMH scale exists, we used the results of our Practice PCMH Implementation Survey to determine the PCMH score. For each PCMH element, the practice was given 5 points for implementation, 2 points for planning, 1 point for interest and 0 points for no plans to implement. We weighted actual implementation heavily given the resource and time commitment necessary to truly put in place each PCMH element. Points were summed to determine the final PCMH practice score. This PCMH practice score provides a view of the variation in PCMH implementation among HPRN practices.
Main outcome measures
The main outcome measure was the primary care provider's perceived benefit of PCMH elements for individual patients seen in the participating practice.
Statistical analysis
Descriptive statistics (means, proportions, frequency distributions) were generated for patient, provider and practice characteristics as well as PCMH implementation. We compared provider perceived benefit by reason for visit and PCMH implementation status in unadjusted analyses using chi-square tests. We conducted multilevel logistic regression analysis using generalised linear mixed models (SAS Proc GLIMMIX), adjusting for clustering of patients within practices (practice included as a random intercept) in order to determine what patient (age, gender, race, chronic illness), provider (MD/DO, NP, PA), practice (PCMH score) and visit characteristics (reason for visit, problems that could not be addressed in the visit) were associated with the provider's perceived benefit for each PCMH element. Patient, provider, practice and visit level variables were included in every model. We limited practice-level variables to PCMH score because the number of practices was small (n = 37), and there was strong co-linearity between PCMH scores, practice size and FQHC status. We report P-values and 95% confidence intervals (CI) in lieu of adjusting for multiple analyses, which can result in overly stringent criteria for determining statistical significance. All statistical analysis was conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Seventy-eight providers in 37 practices saw 1093 patients and completed 1016 card study surveys (93%). Table 1 provides the demographic, basic medical history and reason for the visit for the final sample of 1016 patients for whom we have complete data. The majority of the patients were female (61%). The average age was 42 years (range, new-born to 94), 74% were white, and 20% were Hispanic. The primary reason for the visit was split with 46% for acute visit, 35% for chronic visit and 20% for a health maintenance visit. The majority of patients received care from a physician (59%), while nurse practitioners saw 19% and physician assistants saw 22%. Forty-five percent of the patients had at least one of the five common chronic conditions.
Table 1.
PCMH card study patient demographics.*
| Variable | Number (%) |
|---|---|
| n = 1016 | |
| * Not all surveys had complete data on all elements. | |
| Gender | |
| Female | 620 (61) |
| Male | 394 (39) |
| Age | |
| < 18 | 211 (21) |
| 18–30 | 153 (15) |
| 31–64 | 411 (41) |
| > 64 | 225 (23) |
| Race/ethnicity | |
| White | 747 (74) |
| Hispanic | 207 (20) |
| Other or no answer | 62 (6) |
| Primary reason for visit | |
| Acute problem | 410 (46) |
| Chronic problem | 312 (35) |
| Health maintenance | 175 (19) |
| Provider for this visit | |
| MD/DO | 577 (59) |
| NP | 180 (18) |
| PA | 218 (23) |
| Patient medical conditions | |
| Diabetes | 131 (13) |
| Asthma/COPD | 101 (10) |
| Cardiovascular disease | 127 (13) |
| Hypertension | 241 (24) |
| Depression/anxiety | 155 (15) |
| Were there problems you were unable to address | |
| Acute problem | 89 (9) |
| Chronic problem | 142 (14) |
| Health maintenance | 152 (15) |
PCMH implementation
Table 2 provides basic practice demographics and the implementation of PCMH among participating practices. PCMH scores ranged from 27 to 87 (mean 67) representing the variation in PCMH implementation. Most practices reported implementing many of the PCMH elements with plans to implement all or most of the others. The vast majority of practices reported implementation of an EHR (81%), and all but one of the remaining practices reported plans to implement an EHR (16%). The practice that reported no plans to implement an EHR represents providers who have previously mentioned plans to retire in the next few years, thus negating EHR implementation. Although 19 practices (53%) reported implementing enhanced access outside normal office hours, 15 (41%) reported no plans to add additional access. Twenty practices reported plans to or interest in offering secure patient email, and nine practices reported current use of email. Only six practices reported offering group visits; 22 (60%) have no plans to implement group visits.
Table 2.
PCMH implementation in the High Plains Research Network.
| Variable | Number (%) | ||
|---|---|---|---|
| n = 37 | |||
| MD, medical doctor; DO, doctor of osteopathy; NP, nurse practitioner; PA, physician assistant; FTE, full-time equivalent. | |||
| Practice type | |||
| Federally qualified health centre | 10 (27) | ||
| Certified rural health clinic | 17 (46) | ||
| Private practice | 6 (16) | ||
| Other or unknown | 4 (11) | ||
| Practice staff | |||
| Total MD/DO (average) | 1.9 | ||
| leq 1 | 21 (57) | ||
| 2–3 | 10 (27) | ||
| > 3 | 6 (16) | ||
| Total NP/PA (average) | 1.4 | ||
| leq 1 | 26 (70) | ||
| 2–3 | 8 (22) | ||
| > 3 | 3 (8) | ||
| Total other staff (average) | 8.5 | ||
| leq 5 | 19 (51) | ||
| 6–10 | 10 (27) | ||
| > 10 | 8 (22) | ||
| FTE MD/DO (average) | 1.7 | ||
| FTE NP/PA (average) | 1.3 | ||
| FTE other staff (average) | 7.6 | ||
| PCMH element | Implemented (N) | Plans or interest to implement (N) | No interest to implement (N) |
| Access | 19 | 3 | 15 |
| 9 | 20 | 8 | |
| Pre-visit huddle | 26 | 4 | 7 |
| Post visit | 28 | 7 | 2 |
| Patient education | 28 | 9 | 0 |
| Family involvement | 23 | 12 | 2 |
| Health assessments | 35 | 1 | 1 |
| Group visits | 6 | 9 | 22 |
| Electronic health records | 30 | 6 | 1 |
| Electronic prescibing | 28 | 6 | 3 |
| Medication reconciliation | 32 | 1 | 4 |
| Information tracking | 32 | 4 | 1 |
| Registry | 22 | 9 | 6 |
| Protocols | 34 | 3 | 0 |
| Provider prompts/reminders | 27 | 6 | 4 |
| Safety and quality | 31 | 4 | 2 |
| Professional information sharing | 33 | 3 | 1 |
| Medical neighbourhood | 11 | 15 | 11 |
Provider perceived benefit of PCMH components
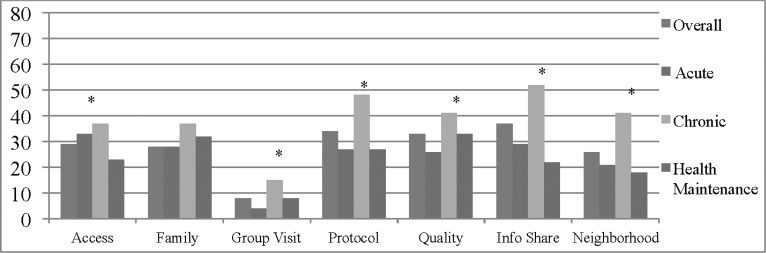
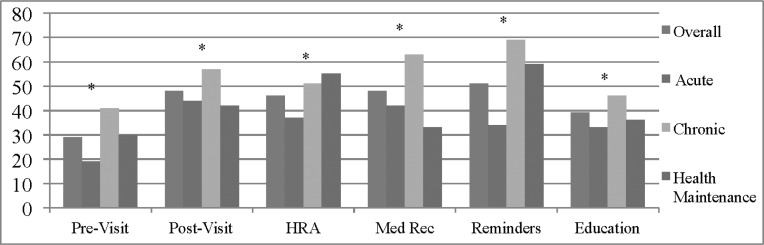
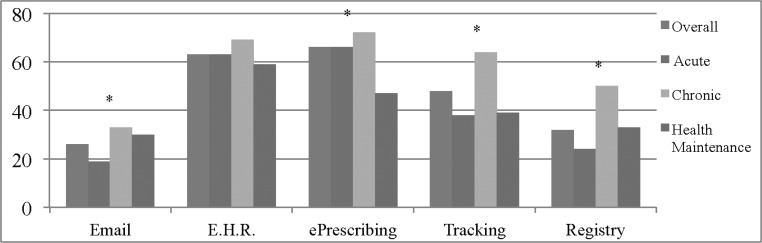
There was wide variation among the providers' perceived benefits of the 18 PCMH elements, ranging from just 8% of patients with provider perceived benefit for group visits to 66% of patients with perceived benefit for electronic prescribing. Figures 1–3 report provider perceived patient benefit for all 18 PCMH elements. The PCMH elements are presented in three general categories related to type of activity: practice systems, provider team activities and technology. One practice reported no benefit to any patient for any of the 18 elements, whereas nine practices reported at least occasional benefit for all 18 elements. Just 13 practices reported that even one of their patients would benefit from group visits, the least frequently reported beneficial element.
Figure 1.
Percentage of visits in which the provider reported that the individual patient would benefit, by reason for visit – practice system components. *P < 0.01 for comparison between acute, chronic and health maintenance.
Figure 2.
Percentage of visits in which the provider reported that the individual patient would benefit, by reason for visit – provider team activities. *P < 0.01 for comparison between acute, chronic and health maintenance.
Figure 3.
Percentage of visits in which the provider reported that the individual patient would benefit, by reason for visit – technology components. *P < 0.01 for comparison between acute, chronic and health maintenance.
Perceived benefit for PCMH elements varied based on the reason for visit. A pre-visit team discussion (huddle) was perceived as beneficial in 41% of patients presenting with a chronic condition, but just 19% of those presenting with an acute problem (P < 0.0001). Patient education was perceived as beneficial for 46% of patients with a chronic problem, but just 33% with an acute problem (P < 0.01). Health assessments were reported as beneficial for 55% of patients presenting for health maintenance and 51% of those with a chronic problem, but just 37% of patients with an acute problem (P < 0.0001). A majority of all patients were reported to benefit from the EHR, whereas electronic prescribing was more likely a perceived benefit for patients with a chronic problem (72% chronic, 66% acute, 47% health maintenance, P < 0.0001).
Generally, there was a strong association between provider perceived benefit and implementation status in the practice. Among patients in clinics where PCMH had been implemented, there were generally higher rates of provider perceived benefit for individual components. For instance, in practices with secure patient email, providers reported this to be a benefit for 37% of patients, compared with only 21% in practices without patient email (P < 0.0001). Table 3 provides the association between implementation and perceived benefit for all 18 PCMH elements. In practices with an EHR, providers reported this as a benefit in 69% of patient visits, compared with just 30% for practices without an EHR (P < 0.0001). However, even in practices without electronic prescribing, providers report this would be a benefit in 51% of patients.
Table 3.
Provider perceived benefit by practice implementation status.
| Provider perceived benefit of element in practices where this element | |||
|---|---|---|---|
| PCMH element | Has been implemented (% of patient encounters) | Has not been implemented (% of patient encounters) | P |
| * Perceived benefit was lower in practices with implementation of PCMH element compared to practices without the element. | |||
| Enhanced access | 45 | 17 | < 0.0001 |
| 37 | 21 | < 0.0001 | |
| Pre-visit huddle | 36 | 18 | < 0.0001 |
| Post visit | 49 | 46 | 0.50 |
| Education* | 38 | 42 | 0.25 |
| Family involvement* | 30 | 38 | < 0.01 |
| Health assessments | 47 | 17 | < 0.0001 |
| Group visits | 18 | 7 | < 0.0001 |
| Electronic health record | 69 | 30 | < 0.0001 |
| ePrescribing | 70 | 51 | < 0.0001 |
| Medication reconciliation | 49 | 44 | 0.17 |
| Tracking | 51 | 25 | < 0.0001 |
| Registry | 40 | 20 | < 0.0001 |
| Practice protocols* | 31 | 68 | < 0.0001 |
| Reminders | 52 | 46 | 0.08 |
| Quality checks | 37 | 21 | < 0.0001 |
| Sharing information | 38 | 26 | < 0.01 |
| Medical neighbourhood* | 16 | 29 | < .0001 |
Generalised linear mixed models
The results of multilevel analyses are described below. Association of perceived benefit with patient, provider, practice and visit level variables are found in Table 4.
Table 4.
Predictors of provider perceived benefit for PCMH element.
| PCMH element | Patient, visit, provider practice variable | Odds ratio | 95% CI | P |
|---|---|---|---|---|
| * Per 10 unit change in PCMH score. † Diagnosis of diabetes, asthma/COPD, cardiovascular disease, hypertension, depression/anxiety. | ||||
| Note: models include age, race/ethnicity, gender, provider type, chronic medical condition, reason for visit is chronic disease, problem that could not be addressed today, PCMH score. | ||||
| Access | PCMHness* | 2.7 | 1.3, 5.7 | 0.01 |
| PCMHness* | 1.5 | 1.1, 2.5 | 0.03 | |
| MD/DO | 1.9 | 1.3, 2.8 | 0.002 | |
| Chronic reason (chronic problem reason for visit) | 1.9 | 1.3, 2.9 | 0.001 | |
| Address (problems you were unable to address) | 0.6 | 0.4, 0.9 | 0.02 | |
| Pre-visit huddle | PCMHness | 2.9 | 1.6, 5.3 | 0.001 |
| MD/DO | 2.5 | 1.6, 3.9 | 0.0001 | |
| Dx medical condition{ | 1.6 | 1.03, 2.6 | 0.037 | |
| Chronic reason | 2.5 | 1.6, 3.9 | 0.0001 | |
| Post visit | PCMHness | 1.4 | 0.9, 2.3 | 0.1 |
| Male gender | 0.6 | 0.5, 0.9 | 0.006 | |
| Dx medical condition | 1.9 | 1.3, 2.8 | 0.0014 | |
| Address | 1.7 | 1.2, 2.6 | 0.007 | |
| Patient education | PCMHness | 1.7 | 1.1, 2.7 | 0.03 |
| Dx medical condition | 2.3 | 1.6, 3.4 | 0.0001 | |
| Address | 1.8 | 1.2, 2.7 | 0.004 | |
| Health assessments | PCMHness | 1.8 | 1.2, 2.7 | 0.003 |
| Dx medical condition | 1.8 | 1.2, 2.6 | 0.002 | |
| Address | 1.5 | 1.04, 2.2 | 0.03 | |
| Family involvement | PCMHness | 1.3 | 0.9, 1.8 | 0.14 |
| Dx medical condition | 2.6 | 1.8, 3.9 | 0.0001 | |
| Address | 1.5 | 1.1, 2.2 | 0.03 | |
| Group visits | PCMHness | 1.2 | 0.7, 1.9 | 0.58 |
| Male gender | 0.6 | 0.3, 0.9 | 0.03 | |
| Dx medical condition | 2.4 | 1.3, 4.6 | 0.007 | |
| Chronic reason | 2.8 | 1.6, 4.9 | 0.0003 | |
| Electronic health records | PCMHness | 2.3 | 0.9, 5.8 | 0.07 |
| MD/DO | 0.2 | 0.1, 0.4 | <.0001 | |
| Dx medical condition | 0.6 | 0.4, 0.9 | 0.04 | |
| Chronic reason | 1.9 | 1.2, 3.2 | 0.007 | |
| ePrescribing | PCMHness | 2.6 | 1.3, 5.3 | 0.01 |
| MD/DO | 0.5 | 0.3, 0.9 | 0.01 | |
| Dx medical condition | 1.6 | 1.03, 2.5 | 0.04 | |
| Medication reconciliation | PCMHness | 2.3 | 1.2, 4.3 | 0.01 |
| Male gender | 0.7 | 0.5, 0.9 | 0.02 | |
| Dx medical condition | 2.0 | 1.3, 3.1 | 0.001 | |
| Chronic reason | 1.9 | 1.2, 2.9 | 0.003 | |
| Address | 2.7 | 1.8, 4.0 | 0.0001 | |
| Info tracking | PCMHness | 1.5 | 0.9, 2.4 | 0.13 |
| Dx medical condition | 1.7 | 1.1, 2.5 | 0.01 | |
| Chronic reason | 2.1 | 1.4, 3.0 | 0.0003 | |
| Registry | PCMHness | 1.7 | 0.9, 3.1 | 0.06 |
| MD/DO | 2.1 | 1.3, 3.2 | 0.001 | |
| Dx medical condition | 1.6 | 1.03, 2.5 | 0.03 | |
| Chronic reason | 3.0 | 1.9, 4.6 | < 0.0001 | |
| Practice protocols | PCMHness | 1.8 | 0.9, 3.5 | 0.09 |
| Minority (race/ethnicity) | 1.6 | 1.1, 2.4 | 0.02 | |
| Chronic reason | 1.9 | 1.3, 2.9 | 0.001 | |
| Prompts/reminders | PCMHness | 1.6 | 1.1, 2.3 | 0.02 |
| Male gender | 0.7 | 0.5, 0.9 | 0.01 | |
| Dx medical condition | 2.2 | 1.5, 3.3 | 0.0001 | |
| Chronic reason | 2.6 | 1.8, 3.8 | 0.0001 | |
| Safety and quality | PCMHness | 1.9 | 0.9, 4.2 | 0.07 |
| MD/DO | 1.6 | 1.01, 2.4 | 0.04 | |
| Chronic reason | 1.6 | 1.0, 2.5 | 0.05 | |
| Address | 2.0 | 1.3, 3.2 | 0.003 | |
| Medical neighbourhood | PCMHness | 1.4 | 0.7, 1.0 | 0.31 |
| Chronic reason | 2.1 | 1.4, 6.4 | 0.001 | |
| Info sharing | PCMHness | 1.7 | 0.9, 3.0 | 0.09 |
| MD/DO | 2.1 | 1.3, 3.2 | 0.001 | |
| Chronic reason | 1.9 | 1.3, 2.9 | 0.002 | |
Patient characteristics
Several patient characteristics predicted provider perceived benefit from PCMH elements. Male gender was associated with lower perceived benefit for a post-visit huddle, group visit, medication reconciliation and reminders. The presence of a chronic medical condition, regardless of whether it was the primary reason for the visit, was associated with increased perceived benefit for nearly all PCMH elements except access, email, protocols, quality checks, information sharing and medical neighbourhood. Age and race/ethnicity were not predictors of perceived benefit for any PCMH elements.
Provider Characteristics
Provider type (MD/DO) was associated with higher perceived benefit for email, pre-visit huddles, disease registry, quality checks, and information sharing, but lower perceived benefit from EHR and electronic prescribing.
Practice characteristics
The practice-level PCMH implementation score (PCMHness) was significantly associated with greater perceived benefit for enhanced access, email, pre-visit huddle, patient education, health assessments, electronic prescribing, medication reconciliation and reminders.
Visit characteristics
Having a chronic illness as the reason for a visit was associated with increased odds of provider perceived benefit for secure email, pre-visit huddle, group visits, EHR, medication reconciliation, tracking, registry, practice protocols, reminders, information sharing, quality checks and medical neighbourhood. Being unable to address a health problem at this visit was associated with increased odds of perceived benefit for post-visit huddle, patient education, health assessments, family involvement, medication reconciliation and quality checks.
Discussion
Primary care providers believe that the comprehensive, connected and person-centred values of the PCMH are essential elements of high-quality medical care. Their practices aspire to deliver the philosophical components of the medical home whether they are formally implementing the PMCH or not. Although the academic discussion on the value of the PCMH may appear settled in the published literature, it remains unclear how patients, primary care providers, and healthcare policy makers embrace the benefit of the PCMH.27,28
Does the PCMH, as Chana and Ahluwalia state, ‘enable the delivery of what matters to people?’ (see article in this issue). Using a card study methodology, we examined to what extent, in the course of over 1000 individual patient encounters, primary care providers perceived the patient benefit for common elements of the medical home. Although several other authors have reported variable attitudes and the use of PCMH elements, most of those studies were conducted using general surveys of provider and practice knowledge, attitudes and experiences with PCMH. This is the first study we know of that determined the primary care provider perception of benefit for each element at the individual patient level. Our data were gathered in the midst of a big push in the region by multiple organisations for medical practices to become medical homes, which means that most providers and staff had some familiarity with the concept of the PCMH. Not surprisingly, the providers who participated in this study assigned quite a range of perceived benefit to the individual elements of a medical home.
Providers reported patient benefit to many aspects of the medical home. Higher rates of perceived benefits were reported for patients presenting with a chronic condition compared with an acute problem. The electronic health record and electronic prescribing were among the elements with the highest frequency of perceived benefit. Because we frequently heard about the barriers and dilemmas associated with EHR implementation, we were surprised that providers reported such high levels of patient benefit from the EHR. Both of these elements had much higher rates of perceived benefit among providers in practices that had already implemented an EHR. These positive results may be because providers and practices with a less positive impression of the value of an EHR are less likely to implement one. Or, perhaps the use of an EHR provides evidence of the patient benefit derived from the EHR. It is not possible to determine whether perceived benefit leads to implementation or availability of the element leads to perceived benefit to patients. Although closely associated in a number of the PCMH elements that we measured, the direction in which this perceived benefit acts is unclear.
Several elements of the PCMH were not perceived as a benefit to patients. Although practices may complete the required training and basic paperwork to accomplish formal PCMH recognition, they may not actually use all elements of the PCMH. For example, providers rarely reported that their patient would benefit from a group visit (9%). This number jumped to 15% of those with a chronic condition. Interestingly, in practices that had implemented group visits (13 of 37), providers reported that just 17% of their patients would benefit from this PCMH element. There are many reasons why the group visit may not have been perceived as beneficial. Issues of privacy, the prevalence of other group activities and clubs in rural communities, and fewer numbers of patients with specific conditions may make group visits less attractive.
As expected, the presence of a chronic illness was a strong predictor for perceived benefit from PCMH activities. The PCMH has been designed primarily for chronic disease management and was uniformly associated with the perceived benefit of systems-, provider/staff activities- and technologically based components of the PCMH, as shown in Figures 1–3. This comes as no surprise given that 35% of the patient visits were for chronic illness management, and providers reported that in 14% of the visits, chronic care management was not adequately addressed. This provides internal validity to the study by demonstrating that many elements of the PCMH do, in fact, benefit chronic care management and the extension of care beyond the current visit. The inability to address all the patient's problems at the current visit was a strong predictor of perceived benefit from the PCMH, consistent with the broader view of the medical home as a team concept that includes care outside the exam room.
Primary care practice includes acute illness and injury care, chronic disease management and preventive health maintenance encounters. How does the medical home support all aspects of primary care? Chronic disease was the primary reason for a visit in just one-third of cases, and a co-morbid chronic illness was only present in 45% of the encounters. Several elements, such as health assessment screens and reminders, appeared to be beneficial for health maintenance visits. PCMH elements were not perceived as being as beneficial in acute care management as in chronic care management. Surprisingly, increased access to care was not perceived by the provider as being beneficial in acute care. Perhaps this does not take into account patient preferences as it was the provider who completed the survey. The benefits from the medical home model for patients with an acute problem or health maintenance visit may need to be made more explicit or included in implementation strategies. The medical home may need additional components specifically related to patients with an acute problem.
There may be PCMH elements that are not universally relevant for all practices and patients. Some parts of the medical home may be elective or ancillary. Certainly, a provider who perceives no benefit to a PCMH element is unlikely to incorporate it into their usual patient care. If providers remain unconvinced that some elements will benefit their patients, neither the accrediting agency nor any other organisation will likely extract much more than paper compliance, having little to no effect on actual patient care. If, however, some of these items are considered to be crucial elements of the primary care medical home, new strategies will be needed to bring the providers and their practices on-board. Improving the local implementation of many of the PCMH elements may provide more benefit or perceived benefit for patients. As found in several large studies, successful implementation requires a local practice champion, long-term support, and the commitment of providers and administrators.5,12,20 Identifying the sine qua non medical home elements that primary care should make available to all patients is a worthy conversation and in need of additional input from providers, patients and policy makers.
Limitations
At the time of our research, PCMH implementation was being encouraged and supported by multiple community-based organisations throughout Colorado. Several practices in the HPRN were actively pursuing formal PCMH accreditation and many others were preparing for implementation. The strength of PCMH implementation work in Colorado may have impacted our findings. However, given the uncertain benefit of PCMH and the immense work of implementation, it is unclear whether the ongoing PCMH work throughout Colorado would have increased or decreased providers' perceptions. Our anecdotal conversations with primary care providers offered evidence of both.
Although our PCMH practice score (PCMHness) is not a validated outcome measure, it provided us with a method for differentiating practices based on their experience with and interest in PCMH activities. Our method of arriving at these scores might serve as a reference point for developing a more precise and useful way to quantify the patient-centredness of a practice with, for example, differential weighting of the various components and more patient input.27
Practice reported implementation of PCMH elements and our interviews attempted to determine the level of implementation. However, whether reported implementation translated into actual routine use for specific activities is still unclear. For instance, although 21 practices (58%) reported implementing a patient registry, it was reported as beneficial in just 32% of patient encounters. One possibility is that our implementation interview overestimated the degree that PCMH elements were implemented into usual practice and routine care. It is clear that most of the practices and providers in this study aspire to include the PCMH elements in their day-to-day patient care.
Conclusions
Linguists and anthropologists have long known that, just as smaller more isolated animal populations generate greater diversity of species, the variety of local languages and cultures varies directly with remoteness and inversely with population size.30–32 This same scaling principle holds true for medical practices. The more rural and remote, the more practices tend to vary from each other and from a norm weighted toward larger population centres. The team of primary care providers and researchers undertook this project with an understanding that rural communities and medical practices are different and individual. PCMH requirements and implementation strategies may need to be uniquely tailored for individual practices. The development of a PCMH scale that can quantify the level of PCMH implementation for a national standard and is also locally relevant and recognises the unique nature of primary care practices could help guide future implementation. There is need for further study of PCMH in varying contexts, with an eye toward adapting the structure and requirements of the medical home to each practice, while not forsaking the PCMH aspirations that contribute to quality, safety, clinical outcomes, cost reduction and patient and provider satisfaction.
ACKNOWLEDGEMENTS
Thank you to the Community Advisory Council of the High Plains Research Network for helping guide the research implementation and interpretation of results. Thanks also to the primary care practices, providers, and staff that participated in this research study.
Contributor Information
Susan Gale, High Plains Research Network, Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO, USA.
Tony Gerk, Northeast Colorado Family Medicine, Sterling, CO, USA.
Sergio Sanchez, High Plains Research Network, Community Advisory Council, USA.
Perry Dickinson, High Plains Research Network, Department of Family Medicine, University of Colorado School of Medicine, Aurora, CO, USA.
ETHICAL APPROVAL
This study was approved by the Colorado Multiple Institutional Review Board.
CONFLICTS OF INTEREST
None.
REFERENCES
- 1.American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA) (2007) Joint Principles of the Patient-Centered Medical Home. www.aafp.org/online/etc/medialib/aafp_org/documents/policy/fed/jointprinciplespcmh0207.Par.0001.File.tmp/022107medicalhome.pdf (accessed 17/07/11).
- 2.Rosenthal TC. (2008) The medical home: growing evidence to support a new approach to primary care. Journal of the American Board of Family Medicine 21:427–40. [DOI] [PubMed] [Google Scholar]
- 3.Stange KC, Nutting PA, Miller WL. et al. (2010) Defining and measuring the patient-centered medical home. Journal of General Internal Medicine 25:601–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stange KC, Miller WL, Nutting PA, Crabtree BF, Stewart EE, Jaen CR. (2010) Context for understanding the National Demonstration Project and the patient-centered medical home. Annals of Family Medicine 8(Suppl_1):S2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaen CR. (2010) Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Annals of Family Medicine 8(Suppl_1):S45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pugno PA. (Year) One giant leap for family medicine: preparing the 21st-century physician to practice patient-centered, high-performance family medicine. Journal of the American Board of Family Medicine 23 Suppl 1:S23–27. [DOI] [PubMed] [Google Scholar]
- 7.Berwick DM. (2009) What ‘patient-centered’ should mean: confessions of an extremist. Health Affairs (Millwood) 28:w555–65. [DOI] [PubMed] [Google Scholar]
- 8.National Committee for Quality Assurance (2010) A Companion Guide to NCQA's PPC–PCMH Standards. www.ncqa.org/tabid/1034/Default.aspx
- 9.National Committee for Quality Assurance (2013) Patient-Centered Medical Home: Recognition Programs. www.ncqa.org/Programs/Recognition/PatientCenteredMedicalHomePCMH.aspx
- 10.National Committee for Quality Assurance (Year) Physician Practice Connections–Patient-Centered MedicalHome™. www.ncqa.org/tabid/631/Default.aspx (accessed 21/08/08).
- 11.Fernald DH, Deaner N, O'Neill C, Jortberg BT, Degruy FV, 3rd, Dickinson WP. (Year) Overcoming early barriers to PCMH practice improvement in family medicine residencies. Family Medicine 43:503–9. [PubMed] [Google Scholar]
- 12.Grumbach K, Grundy P. (2010) Outcomes of Implementing Patient Centered Medical Home Interventions: a review of the evidence from prospective evaluation studies in the United States. Patient-centered Primary Care Collaborative; Washington, DC: www.pcpcc.net/files/evidence_outcomes_in_pcmh.pdf (accessed 27/02/12). [Google Scholar]
- 13.Rittenhouse DR, Thom DH, Schmittdiel JA. (Year) Developing a policy-relevant research agenda for the patient-centered medical home: a focus on outcomes. Journal of General Internal Medicine 25:593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carney PA, Eiff MP, Saultz JW. et al. (2009) Aspects of the patient-centered medical home currently in place: initial findings from preparing the personal physician for practice. Family Medicine 41:632–9. [PubMed] [Google Scholar]
- 15.Stewart EE, Nutting PA, Crabtree BF, Stange KC, Miller WL, Jaen CR. (2010) Implementing the patient-centered medical home: observation and description of the National Demonstration Project. Annals of Family Medicine 8(Suppl_1):S21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.David A, Baxley L. (Year) Education of students and residents in patient centered medical home (PCMH): preparing the way. Annals of Family Medicine 9:274–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rogers J, Juliao TR. (Year) Innovation and creativity in education curricula for the medical home. Family Medicine 43:693–5. [PubMed] [Google Scholar]
- 18.Jaen CR, Crabtree BF, Palmer RF. et al. (2010) Methods for evaluating practice change toward a patient-centered medical home. Annals of Family Medicine 8(Suppl_1): S9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nutting PA, Crabtree BF, Stewart EE. et al. (2010) Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Annals of Family Medicine 8(Suppl_1): S33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crabtree BF, Nutting PA, Miller WL, Stange KC, Stewart EE, Jaen CR. (2010) Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Annals of Family Medicine 8(Suppl_1):S80–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaen CR, Ferrer RL, Miller WL. et al. (2010) Patient outcomes at 26 months in the patient-centered medical home National Demonstration Project. Annals of Family Medicine 8(Suppl_1):S57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright A, Henkin S, Feblowitz J, McCoy AB, Bates DW, Sittig DF. (2013) Early results of the meaningful use program for electronic health records. New England Journal of Medicine 368:779–80. [DOI] [PubMed] [Google Scholar]
- 23.Adler-Milstein J, Green CE, Bates DW. (2013) A survey analysis suggests that electronic health records will yield revenue gains for some practices and losses for many. Health Affairs (Millwood) 32:562–70. [DOI] [PubMed] [Google Scholar]
- 24.Bates DW, Bitton A. (Year) The future of health information technology in the patient-centered medical home. Health Affairs (Millwood) 29:614–21. [DOI] [PubMed] [Google Scholar]
- 25.Ralston JD, Coleman K, Reid RJ, Handley MR, Larson EB. (Year) Patient experience should be part of meaningful-use criteria. Health Affairs (Millwood) 29:607–13. [DOI] [PubMed] [Google Scholar]
- 26.Moreno L, Peikes D, Krilla A. (2010) Necessary But Not Suffcient: The HITECH Act and health information technology's potential to build medical homes (Prepared by Mathematica Policy Research under Contract No. HHSA290200900019I TO2). AHRQ Publication No. 10–0080-EF Agency for Healthcare Research and Quality: Rockville, MD. [Google Scholar]
- 27.Cooley WC, McAllister JW, Sherrieb K, Clark RE. (2003) The Medical Home Index: development and validation of a new practice-level measure of implementation of the medical home model. Ambulatory Pediatrics 3(4):173–80. [DOI] [PubMed] [Google Scholar]
- 28.Goldberg DG, Kuzel AJ. (2009) Elements of the patient-centered medical home in family practices in Virginia. Annals of Family Medicine 7:301–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Westfall JM, Zittleman L, Staton EW. et al. (2011) Card studies for observational research in practice. Annals of Family Medicine 9:63–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dalby A. (2003) Language in Danger: the loss of linguistic diversity and the threat to our future. Columbia University Press: New York. [Google Scholar]
- 31.Lupyan G, Dale R. (2010) Language structure is partly determined by social structure. PLoS One 5: e8559 dx.doi.org/10.1371%2Fjournal.pone.0008559 (accessed 12/04/13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nettle D. (1998) Explaining global patterns of language diversity. Journal of Anthropological Archaeology 17(4):21. [Google Scholar]