Abstract
Background
Elevated systemic levels of myeloperoxidase (MPO) have been associated with unfavourable clinical outcomes. In the present study, we evaluate the impact of MPO, a pro-oxidant enzyme that catalyzes the initiation of lipid peroxidation and affects nitric oxide levels, on the risk of all-cause mortality in a large population of frail octogenarians and nonagenarians living in community.
Methods
We analyzed data from the Aging and Longevity Study in the Sirente Geographic Area (ilSIRENTE Study), a prospective cohort study that collected data on all individuals aged 80 years and older living in a mountain community (n = 363). The main outcome measure was the risk of death after 4 years of follow-up. Participants were divided into three groups based on MPO tertiles: lower tertile ≤ 61.5 μg/L (n = 120), intermediate tertile 61.6–140.6 μg/L (n = 120), and higher tertile ≥140.7 μg/L (n = 123).
Results
A total of 150 deaths occurred during 4-years follow-up. The mean MPO level was 170.8 ± 177.5 μg/L among those who died compared with 135.4 ± 142.4 μg/L among survivors (p = .03). Individuals in the highest MPO tertile had higher risk of mortality (40% [60/123]) compared with those in the lower tertile (26% [39/120]). After adjusting for potential confounders, compared with participants in the lower tertile, those in the higher tertile had a hazard ratio for mortality of 1.97 (95% confidence interval: 1.02–3.80).
Conclusion
Our results obtained from a representative sample of very old and frail elderly individuals expand the knowledge that low levels of MPO are associated with better survival.
Keywords: Myeloperoxidase, Mortality, Frail elderly
MYELOPEROXIDASE (MPO), a heme protein secreted by activated leukocytes, facilitates conversion of hydrogen peroxide to hypochlorous acid and generates reactive intermediates that promote lipid peroxidation (1). Previous studies reported an accumulation of lipid peroxidation products during aging (2), in agreement with other evidence suggesting that oxidative stress increases with age (3). Even though different measures of end products of lipid peroxidation have been assessed (i.e., isoprostanes, malondialdehyde [MDA], or oxidized low-density lipoprotein), MPO represents an earlier marker of oxidative damage compared with the aforementioned due to its ability to initiate lipid peroxidation process (1). Increasing evidence is indicating MPO as a contributor to several phases of atherothrombosis, from the initial insult to the vascular endothelium (4), to development of atheroma (5), to rupture of the vulnerable atherosclerotic plaque (6), and its clinical manifestation as an acute coronary syndrome (7). Moreover, the plasma concentration of MPO is increased among patients with stable coronary artery disease (8) and it has been shown to be a strong predictor of unfavorable clinical outcomes in patients with acute coronary syndrome (9,10), chronic heart failure (11), and of future coronary artery disease in healthy population (12). Furthermore, type II diabetes, a major risk factor for cardiovascular diseases and mortality, is positively associated with MPO levels (13). However, there are no studies assessing the association between MPO and all-cause mortality in frail elderly individuals. Two previous epidemiological studies (14,15) have analyzed the long-term association of MDA, a biomarker of lipid peroxidation, with risk of death in older adults, with conflicting findings. In fact, one study showed that higher MDA concentrations were not a risk factor for increased vascular or nonvascular mortality in elderly individuals (15), whereas the other documented a higher rate of mortality associated with increased plasma MDA concentrations (14).
The aim of the present study is to evaluate the impact of MPO on the risk of all-cause mortality in a large population of frail octogenarians and nonagenarians living in community, enrolled in the “Invecchiamento e Longevità nel Sirente” (Aging and longevity in the Sirente geographic area, ilSIRENTE Study) study.
METHODS
The ilSIRENTE study is a prospective cohort study performed in the mountain community living in the Sirente geographic area (L’Aquila, Abruzzo) in Central Italy. This study was designed by the Department of Gerontology, Geriatrics, and Physiatric Medicine of the Catholic University of Sacred Heart (Rome, Italy) and developed by the teaching nursing home, Opera Santa Maria della Pace (Fontecchio, L’Aquila, Italy) in a partnership with local administrators and primary care physicians of Sirente Mountain Community Municipalities. The Catholic University of Sacred Heart ethical committee ratified the entire study protocol. All the participants signed an informed consent at the baseline visit. Details of the ilSIRENTE study protocol are described in detail elsewhere (16).
Study Population
A preliminary list of all persons living in this well-defined area was obtained at the end of October 2003 from the Registry Offices of the 13 municipalities involved in the study. Everyone living in the area has to register at birth or after relocation to receive primary health care. This mandatory registration ensured a complete coverage of the population living in the area, including persons in nursing homes. From this preliminary list, potential study participants were identified by selecting all the persons living in the Sirente area who were born before January 1, 1924. Of the initial 514 individuals screened, 32 men and 53 women died or moved away from the area before the baseline assessment. Among those eligible (n = 429), prevalence of refusals was very low (16%), without significant differences across age or gender groups. As a result, the overall sample population enrolled in the ilSIRENTE study consisted of 364 participants. One patient was excluded because the blood sample for the hematological assessment was insufficient. Finally, the sample included in the present study was composed of 363 individuals.
Data Collection
Baseline participants’ assessments began in December 2003 and were completed in September 2004. Assessors were trained on how to perform each component of the ilSIRENTE study protocol (16). The Minimum Data Set for Home Care (MDS-HC) form was administered to all study participants following the guidelines published in the MDS-HC manual (17,18). The MDS-HC contains more than 350 data elements including sociodemographics, physical, and cognitive status variables, as well as major clinical diagnoses (19). Moreover, the MDS-HC also includes information about an extensive array of signs, symptoms, syndromes, and treatments (17,18). The MDS-HC items have shown an excellent interrater and test–retest reliability when completed by nurses performing usual assessment duties (average weighted Kappa = .8) (18,20). Additional information about family history, lifestyle, physical activity, and behavioral factors were collected using specific questionnaires shared with the “Invecchiare in Chianti Study” (21).
Functional and cognitive status measures.—
Activities of daily living (ADLs) were assessed by the assessor using the MDS-HC instrument (17,18). The ADL scale is based on seven levels of self-performance, including dressing, eating, toilet use, bathing, mobility in bed, locomotion, transfer. The Instrumental Activities of Daily Living scale is based on eight domains of function, including ability to use phone, shopping, food preparation, house keeping, laundering, mode of transportation, responsibility for own medications, ability to handle finances. Cognitive performance was assessed using a six-items seven-category scale (Cognitive Performance Scale—CPS) (15). The CPS was scored on a 7-point ordinal scale in which higher scores were associated with worse cognitive performance. The CPS considers two cognitive items (short-term memory and skills for daily decision making), one item describing communication ability (understood by others), one ADL measure (self-performance in eating), and whether in comatose status.
Blood Measurements
Venous blood samples were drawn in the morning after an overnight fast. The samples were immediately centrifuged and stored at −80°C until final analysis. Standard determinations of serum albumin, cholesterol (total and HDL), and triglycerides were performed by commercially available kits (Olympus, Milan, Italy) suitable on Olympus 2700 instrumentation.
MPO Measurements
The concentration of MPO in EDTA plasma was determined with an enzyme immunoassay (Mercodia, Uppsala, Sweden). The immunoassay is based on the sandwich technique, in which two monoclonal antibodies are directed against separate antigenic determinants on the MPO molecule. Samples were measured in duplicate after a 1 + 10 dilution with sample buffer. In this assay, the lowest detection limit is ≤3 μg/L and the measuring range is between 3 and 300 μg/L.
In the used MPO ELISA, recovery upon addition was tested by spiking four serum samples with low levels of MPO to two higher levels within the measuring range. Three identical assays were performed. The four samples were spiked separately for each assay. Recovery upon addition is 84%–98% (mean value 89%). Recovery upon dilution was tested by diluting four serum samples with high levels of MPO in five steps from 1:8 to 1:128. Three identical assays were performed. The four samples were diluted separately for each assay. Recovery upon dilution is 94%–114% (mean value 101%).
In a previous study (22) performed by using Mercodia MPO ELISA, normal MPO levels reported for healthy younger participants ranged between 44.6 and 80.9 μg/L.
The units used in the assay, μg/L, can be converted to those used on clinical practice, pmol/L, by using the conversion factor 1 μg/L = 1 ng/mL = 6.897 pmol/L based on an MPO molecular weight of 145 kDa. Moreover, R&D department of Mercodia analyzed a small subset of samples in the Prognostix CardioMPO ELISA (pmol/L) and MPO ELISA (μg/L). The sample MPO concentration in the Prognostix ELISA (after being converted from pmol/L to ng/mL) served as the observed value, and the sample MPO concentration in the Mercodia MPO ELISA (which is already expressed in ng/mL or μg/L) served as the expected value. The observed value for a sample (O) in the Prognostix test was then divided by the expected value in the Mercodia test (E), multiplied by 100, and then expressed as an O/E percentage. The mean O/E% for the small subset of samples we analyzed was 79% and the range was from 45% to 129%.
Covariates
Medical diagnoses and drugs were directly collected by general practitioners. Medical diagnoses were defined as conditions that have a relationship to the patient’s functional, cognitive, and behavioral status; medical treatment; and risk of death. The diagnoses were listed on the MDS-HC form in a check box section containing 27 specific diagnostic categories. General practitioner collected information on up to 18 different drugs received by each patient in the 7 days preceding the assessment. Body weight was measured with light clothes using a calibrated bathroom scale. Body height was measured using a standard stadiometer. Body mass index (BMI) was defined as weight (kilograms) divided by the square of height (meters). Alcohol consumption was assessed asking the participants about the number of glasses of wine drunk during a standard day. Alcohol abuse was defined as a consumption of more than half liter of wine per day.
Survival Status
Vital status was obtained from general practitioners and confirmed by the National Death Registry. Time to death was calculated from the date of baseline assessment to the date of death. All individuals were observed for 48 months.
Statistical Analysis
For the present study, from the initial sample of 364 participants, we excluded 1 participant because MPO was not determined. This selection resulted in a final sample size of 363 participants. For analytical purposes, MPO levels were categorized into three groups according to tertiles (Table 1).
Table 1.
Myeloperoxidase (MPO) Tertiles
| MPO (μg/L) | Total Sample (n = 363) |
| Lower tertile (n = 120) | |
| Cutoff | ≤61.5 |
| Median ± SD | 38.6 ± 16.5 |
| Intermediate tertile (n = 120) | |
| Cutoff | 61.6–140.6 |
| Median ± SD | 99.2 ± 23.2 |
| Higher tertile (n = 123) | |
| Cutoff | ≥ 140.7 |
| Median ± SD | 308.3 ± 184.1 |
Characteristics of the study sample were presented separately for tertiles of MPO (Table 2).
Table 2.
Characteristics of Study Population According to the Myeloperoxidase (MPO) Tertiles
| Characteristic | Total Sample (n = 363) |
|||
| MPO Tertiles* | ||||
| I (n = 120) | II (n = 120) | III (n = 123) | p for Trend | |
| Age, y | 85.3 ± 4.2 | 86.2 ± 5.0 | 85.8 ± 5.0 | .3 |
| Female | 84 (70) | 83 (69) | 76 (62) | .3 |
| Marital status | ||||
| Married | 30 (25) | 37 (31) | 34 (28) | .6 |
| Widowed | 80 (67) | 68 (57) | 76 (62) | |
| Never married | 10 (8) | 15 (12) | 13 (10) | |
| Living alone | 41 (34) | 26 (23) | 36 (31) | .1 |
| Education, y | 5.1 ± 1.4 | 5.1 ± 2.0 | 5.0 ± 1.3 | .6 |
| Activity of Daily Living Scale score† | 1.2 ± 2.3 | 1.5 ± 2.5 | 1.5 ± 2.4 | .6 |
| Instrumental Activity of Daily Living Scale score‡ | 2.7 ± 2.5 | 3.3 ± 2.5 | 3.1 ± 2.6 | .1 |
| Cognitive Performance Scale score§ | 0.7 ± 1.3 | 1.0 ± 1.7 | 0.8 ± 1.5 | .1 |
| Depression | 28 (23) | 31 (26) | 33 (27) | .8 |
| Number of diseases | 2.0 ± 1.2 | 2.3 ± 1.3 | 2.1 ± 1.3 | .4 |
| Specific disease | ||||
| Hypertension | 82 (68) | 90 (75) | 91 (74) | .4 |
| Ischemic heart disease | 18 (15) | 14 (12) | 12 (10) | .5 |
| Congestive heart failure | 5 (4) | 12 (10) | 5 (4) | .08 |
| Cancer | 5 (4) | 5 (4) | 7 (6) | .8 |
| Chronic obstructive pulmonary disease | 14 (12) | 17 (14) | 18 (15) | .7 |
| Diabetes | 34 (28) | 44 (37) | 31 (25) | .1 |
| Cerebrovascular diseases | 3 (2) | 7 (6) | 7 (6) | .4 |
| Osteoarthritis | 26 (21) | 21 (18) | 24 (20) | .7 |
| Renal disease | 1 (1) | 1 (1) | 1 (1) | 1.0 |
| Number of medications | 3.2 ± 2.3 | 3.3 ± 2.2 | 3.3 ± 2.2 | .8 |
| Body mass index, kg/m2 | 25.6 ± 4.3 | 25.3± 4.1 | 25.8± 5.0 | .6 |
| Alcohol abuse‖ | 13 (11) | 18 (15) | 14 (11) | .5 |
| Smoking habit | 2 (2) | 4 (3) | 2 (2) | .5 |
| Sensory impairment | ||||
| Hearing | 25 (21) | 34 (28) | 26 (21) | .2 |
| Vision | 28 (23) | 26 (22) | 28 (23) | .9 |
| Hematological parameters | ||||
| Albumin, g/dL | 4.2 ± 0.3 | 4.1 ± 0.2 | 4.2 ± 0.2 | .3 |
| Total cholesterol, mg/dL | 204.8 ± 43.5 | 202.4 ± 41.9 | 217.2 ± 39.3 | .01 |
| HDL cholesterol, mg/dL | 48.3 ± 14.3 | 44.6 ± 14.2 | 44.2 ± 11.4 | .04 |
| Triglycerides, mg/dL | 148.3 ± 65.2 | 148.2 ± 65.0 | 141.7 ± 56.6 | .63 |
Notes: *Data are given as number (percent) for the following variables: gender, marital status, living alone, depression, alcohol abuse, smoking habit, sensory impairment; for all the other variables, means ± SD are reported.
Activity of Daily Living Scale ranges from 0 (no functional impairment) to 7 (severe functional impairment).
Instrumental Activity of Daily Living Scale ranges from 0 (no functional impairment) to 8 (severe functional impairment).
Cognitive Performance Scale ranges from 0 (no cognitive impairment) to 6 (severe cognitive impairment).
More than half liter of wine per day.
Differences in proportions and means of covariates between different MPO tertiles were assessed using Fisher’s Exact Test and t-test statistics, respectively. A p < .05 level was chosen for statistical significance.
Time to death was calculated from the date of baseline assessment to the date of death. We examined all events that occurred during 4-years’ follow-up. Crude and adjusted hazard ratios and 95% confidence intervals (CIs) for mortality by MPO levels were calculated using Cox proportional hazard analyses. Variables considered for adjustment were age and gender in Model 1; age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, number of diseases, number of drugs, BMI, hearing impairment, and albumin in Model 2; age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, number of diseases, number of drugs, BMI, hearing impairment, albumin, total cholesterol, HDL cholesterol, and triglycerides in Model 3; age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, BMI, hearing impairment, total cholesterol, HDL cholesterol, triglycerides, albumin, and all the specific diseases resulted significantly different among deceased and alive participants (hypertension, congestive heart failure, diabetes, and cardiovascular diseases) in Model 4. In these models, age was treated as a continuous variable.
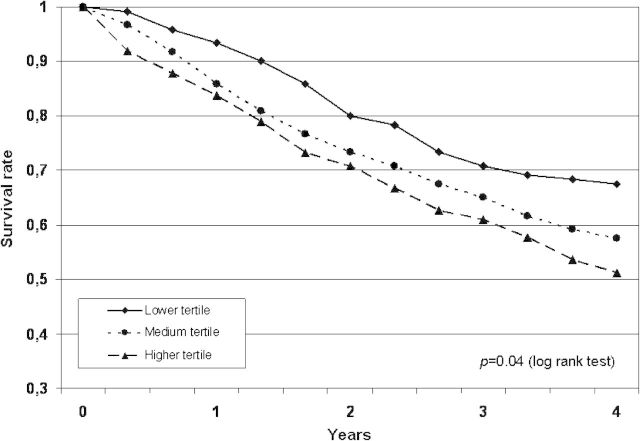
The impact of MPO levels on survival was also tested comparing the survival curves obtained with the Kaplan–Meier method (Figure 1). Differences between curves were evaluated using the log-rank test.
Figure 1.
Survival curves for patients stratified across levels of myeloperoxidase tertiles at baseline.
Statistical analysis was performed using the SPSS 10.0 package (Chicago, IL).
RESULTS
Mean age of 363 individuals participating in the study was 85.8 (SD 4.8) years and 244 (67%) were women. Characteristics of the study population according to the different levels of MPO tertiles are summarized in Table 2. Compared with participants in the first tertile of MPO, those in the third tertile had higher levels of total cholesterol (217.2 ± 39.3 vs 204.8 ± 43.5 μg/L) and lower levels of HDL cholesterol (44.2 ± 11.4 vs 48.3 ± 14.3 μg/L).
We also evaluated the baseline characteristics of the sample according to the vital status to identify potential risk factors for mortality (Table 3). Individuals showing functional and cognitive impairment had higher risk to die during 4-years’ follow-up. Similar risk was observed among individuals with higher level of comorbidity and lower BMI. In particular, the prevalence of hypertension, congestive heart failure, diabetes, and cardiovascular diseases resulted higher in deceased participants compared with those alive.
Table 3.
Characteristics of Study Population According to Death (4-years’ Follow-up)
| Characteristic | Total Sample (n = 363) |
||
| Deceased (n = 150) | Alive (n = 213) | p | |
| Age, y | 87.5 ± 5.1 | 84.6 ± 4.2 | <.001 |
| Female* | 95 (63) | 149 (70) | .2 |
| Marital status* | |||
| Married | 34 (23) | 26 (25) | |
| Widowed | 98 (65) | 127 (59) | .1 |
| Never married | 18 (12) | 20 (10) | |
| Living alone* | 29 (20) | 74 (36) | <.001 |
| Education, y | 4.9 ± 1.1 | 5.2 ± 1.8 | .09 |
| Activity of Daily Living Scale score† | 2.6 ± 2.8 | 0.5 ± 1.6 | <.001 |
| Instrumental Activity of Daily Living Scale score‡ | 4.4 ± 2.5 | 2.0 ± 2.1 | <.001 |
| Cognitive Performance Scale score§ | 1.4 ± 1.8 | 0.5 ± 1.1 | <.001 |
| Depression* | 41 (27) | 51 (24) | .4 |
| Number of diseases | 2.4 ± 1.3 | 2.0 ± 1.2 | .007 |
| Specific disease | |||
| Hypertension | 99 (66) | 164(76) | .01 |
| Ischemic heart disease | 22 (15) | 22 (10) | .1 |
| Congestive heart failure | 20 (14) | 2 (1) | <.001 |
| Cancer | 9 (6) | 8 (4) | .2 |
| Chronic obstructive pulmonary disease | 23 (15) | 26 (12) | .2 |
| Diabetes | 57 (38) | 52 (24) | .004 |
| Cerebrovascular diseases | 15 (10) | 2 (1) | <.001 |
| Osteoarthritis | 25 (17) | 46 (21) | .1 |
| Renal disease | 1 (1) | 2 (1) | .7 |
| Number of medications | 3.7 ± 2.4 | 3.0 ± 2.0 | .01 |
| Body mass index, kg/m2 | 24.5 ± 4.7 | 26.3 ± 4.2 | <.001 |
| Alcohol abuse‖* | 22 (15) | 23 (11) | .2 |
| Smoking habit* | 4 (3) | 4 (2) | .6 |
| Sensory impairment* | |||
| Hearing | 46 (31) | 37 (17) | .003 |
| Vision | 41 (27) | 45 (21) | .1 |
| Hematological parameters | 4.1 ± 0.3 | 4.2 ± 2.2 | .002 |
| Albumin, g/dL | |||
| Total cholesterol, mg/dL | 182.5 ± 42.7 | 206.6 ± 43.6 | <.001 |
| HDL cholesterol, mg/dL | 42.3 ± 13.0 | 48.0 ± 13.3 | <.001 |
| Triglycerides, mg/dL | 138.4 ± 61 | 151.5 ± 62.6 | .04 |
| MPO | 170.8 ± 177.5 | 135.4 ± 142.4 | .03 |
Notes: MPO = myeloperoxidase.
*Data are given as number (percent) for the following variables: gender, marital status, living alone, depression, alcohol abuse, smoking habit, sensory impairment; for all the other variables, means ± SD are reported.
Activity of Daily Living Scale ranges from 0 (no functional impairment) to 7 (severe functional impairment).
Instrumental Activity of Daily Living Scale ranges from 0 (no functional impairment) to 8 (severe functional impairment).
Cognitive Performance Scale ranges from 0 (no cognitive impairment) to 6 (severe cognitive impairment).
More than half liter of wine per day.
A total of 150 deaths (55 men and 95 women) occurred during 4-years’ follow-up. The mean MPO level was 170.8 ± 177.5 μg/L among those who died compared with 135.4 ± 142.4 μg/L among survivors (p = .03). There was a direct association between mortality and MPO levels (Table 4). Rate of mortality was 26% among participants in the lower tertile, 34% among those in the intermediate tertile, and 40% among those in the higher tertile. In the unadjusted model, there was a significant and progressive increment in mortality as MPO levels increased. Adjusting for potential confounders, including age, gender, and markers of frailty, the strength of the association between MPO level and mortality remained significant (Table 4). When total cholesterol, HDL cholesterol, and triglycerides were added to the Cox proportional hazard model, the direct association between MPO level and mortality persisted: Compared with participants in the lower tertile, those in the higher tertile had a hazard ratio for mortality of 1.64 (95% CI: 1.04–2.58). In the full-adjusted model (Model 4), the participants in the higher MPO tertile had the highest hazard ratio for mortality, 1.97 (95% CI: 1.02–3.80).
Table 4.
Association Between Myeloperoxidase (MPO) Levels and All-Cause Mortality After Adjustment for Various Confounders
| MPO Tertiles | Mortality During 4-Years’ Follow-up | Unadjusted | Model 1* | Model 2† | Model 3‡ | Model 4§ |
| Number (%) | HR (95% CI) | |||||
| All participants (n = 363) | ||||||
| Lower | 39 (26) | — | — | — | — | |
| Medium | 51 (34) | 1.39 (0.92–2.12) | 1.32 (0.87–2.02) | 1.26 (0.79–2.01) | 1.19 (0.74–1.90) | 0.98 (0.48–1.95) |
| Higher | 60 (40) | 1.67 (1.11–2.50) | 1.67 (1.11–2.50) | 1.87 (1.20–2.92) | 1.64 (1.04–2.58) | 1.97 (1.02–3.80) |
Notes: ADL = activity of daily living; BMI = body mass index; CI = confidence interval; CPS = Cognitive Performance Scale; HR = hazard ratio.
In Model 1, we adjusted for age and gender.
In Model 2, we adjusted for age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, number of diseases, number of drugs, BMI, hearing impairment, and albumin.
In Model 3, we adjusted for age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, number of diseases, number of drugs, BMI, hearing impairment, albumin, total cholesterol, HDL-cholesterol, triglycerides. In all models, age was treated as a continuous variable.
In Model 4, we adjusted for age, gender, living alone, functional impairment (ADL scale score), cognitive impairment (CPS scale score), depression, BMI, hearing impairment, albumin, total cholesterol, HDL-cholesterol, triglycerides, hypertension, congestive heart failure, diabetes, cerebrovascular diseases.
The impact of MPO levels on 4-years’ survival was also tested comparing the survival curves obtained with the Kaplan–Meier method. Survival curves for different MPO tertiles are shown in Figure 1.
DISCUSSION
In the present study, we explored the association of baseline MPO plasma concentrations with 4-year mortality in a sample of community-dwelling older persons aged 80 years and older. Our findings show that plasma levels of MPO were positively associated with all-cause death in frail and very old persons living in the community, independently of age, gender, and other clinical and functional variables. In particular, after adjusting for several clinical correlates of mortality risk, such as cognitive, sensory and functional impairments, BMI, comorbidity, and number of drugs, baseline MPO plasma concentration emerged as an independent predictor of mortality.
The octogenarians and nonagenarians enrolled in this study represent an interesting and new model to investigate the biological and nonbiological determinants of aging and longevity, as well as their interactions. Furthermore, studies performed in specific and well-defined geographic region—such as the Sirente Mountain Community—can be particularly useful in interpreting and disentangling all the complex interactions involved in the development of disability status and longevity (16).
Evidence available so far regarding the specific impact of MPO as a novel inflammatory marker on survival are primarily obtained on patients presenting symptoms of acute coronary syndrome and are not unanimous. In fact, although some studies have indicated MPO as a prognostic marker of early (7,9) and delayed (23) adverse cardiac events in patients with chest pain and other clinical features of acute coronary syndrome, one study reported no significant differences in all-cause mortality rates in patients with symptoms suggestive of acute coronary syndrome and increased MPO concentrations (24). It has also been reported that plasma MPO does not predict mortality independent of other cardiovascular risk factors in patients with clinical and angiographic confirmation of stable coronary artery disease (22). More consistent are the reports regarding the unfavorable prognostic value of MPO concentration after ST-Segment elevation myocardial infarction (10,25,26).
Moreover, elevated plasma MPO levels are reported to be predictive of increased adverse clinical outcomes even in chronic cardiovascular diseases as in heart failure (11), and it has been recently demonstrated that elevated serum MPO levels are associated with an increased risk of developing incident heart failure in healthy elderly individuals (27).
Several mechanisms support a role of MPO in the onset and progression of endothelial dysfunction and atherosclerosis (28–30), pathological processes tightly linked to the genesis of cardiovascular diseases, one of the leading causes of death and disability in older people. In fact, MPO-derived reactive oxidant can reduce nitric oxide bioavailability in endothelial cells (28), modulate the generation of proatherogenic oxidized low-density lipoprotein (30), and promote metalloproteinase activation thereby weakening the fibrous cap of atherosclerotic plaques and propagating plaque rupture (29).
In our study, MPO predicts all-cause mortality in older adults aged 80 years or more even after the correction for lipid profile, the only cardiovascular risk factor that resulted significantly different among the three MPO tertiles. This could be particularly interesting in the light of the documented role for MPO in the oxidative modification of HDL in vivo (31,32), with consequent functional inactivation. The reduction in plasma HDL can clearly lead to diminished reverse cholesterol transport (33) and thereby promote atherosclerosis. In addition, HDL serves as a potent antioxidant, anti-inflammatory, and antithrombotic factor (34) and it has been documented in chronic kidney disease that HDL deficiency is compounded by impaired HDL antioxidant activity (35), which are events that again can contribute to accelerated atherosclerosis. So one of the mechanism by which MPO can increase mortality in elderly individuals could be the reduction of HDL cholesterol plasma levels that have been demonstrated to be a reliable marker of frailty and poor prognosis among the oldest elderly individuals (34).
At this point, it should be noted a constraint regarding the specificity of oxidative stress biomarkers in relation to aging and disease (36). In fact, it is difficult to discriminate if the oxidative damage is due to the aging process or is diseased-related. Considering that most oxidative stress indices, such as MPO, cannot differentiate between free-radical species produced as a result of senescence or induced by comorbidities (37); we cannot exclude that the measured MPO might be, at least in part, a consequence of pathological processes. However, the association between plasma MPO baseline concentration with 4-year mortality in our analysis remained significant even after adjusting for comorbidities and drug use.
Some methodological issues may have influenced our results. As in all cohort studies, selective survival before entry into the cohort has to be taken into consideration. Furthermore, in this longitudinal observational study, results may be confounded by unmeasured factors. In the absence of randomization, it is likely that there are significant, not considered, differences between the evaluation groups that may have biased the study results and conclusions. Another limitation of the present study is determined by the lack of any documentation concerning the cause of death. However, we were interested in characterizing the impact of MPO plasma concentration itself on all-cause mortality. Finally, the ilSIRENTE sample population was composed of persons aged 80 years or older, so our results may not be applicable to other age groups.
In conclusion, we showed that in a representative sample of very old and frail elderly individuals, risk of death is directly associated with MPO, an early marker of lipid peroxidation. Our findings support the hypothesis of a strong implication of oxidative stress in the process of living an extremely long life. The potential utility of plasma MPO for predicting risk of mortality in the elderly individuals needs further investigation.
Acknowledgments
The “Invecchiamento e Longevità nel Sirente” (ilSIRENTE) study was supported by the “Comunità Montana Sirentina” (Secinaro, L’Aquila, Italy). We thank all the participants for their enthusiasm in participating in the project and their patience during the assessments. We are grateful to all the persons working as volunteers in the “Protezione Civile” and in the Italian Red Cross of Abruzzo Region for their support. We sincerely thank the “Comunità Montana Sirentina” and, in particular, its President who promoted and strongly supported the development of the project. The ilSIRENTE Study group is composed as follows: Steering Committee: R. Bernabei, F. Landi; Coordination: A. Russo, M. Valeri, G. Venta; Writing Panel: C. Barillaro, M. Cesari, P. Danese, L. Ferrucci, G. Onder, M. Pahor, V. Zamboni, E. Capoluongo; Participants: Comune di Fontecchio: P. Melonio, G. Bernabei, A. Benedetti; Comune di Fagnano: N. Scarsella, A. Fattore, M. Fattore; Comune di Tione: M. Gizzi; Comune di Ovindoli: S. Angelosante, E. Chiuchiarelli; Comune di Rocca di Mezzo: S. Pescatore; Comune di Rocca di Cambio: G. Scoccia; Comune di Secinaro: G. Pizzocchia; Comune di Molina Aterno: P. Di Fiore; Comune di Castelvecchio: A. Leone; Comune di Gagliano Aterno: A. Petriglia; Comune di Acciano: A. Di Benedetto; Comune di Goriano Sicoli: N. Colella; Comune di Castel di Ieri: S. Battista; RSA Opera Santa Maria della Pace: A. De Santis, G. Filieri, C. Gobbi, G. Gorga, F. Cocco, P. Graziani.
References
- 1.Zhang R, Brennan ML, Shen Z, et al. Myeloperoxidase functions as a major enzymatic catalyst for initiation of lipid peroxidation at sites of inflammation. J Biol Chem. 2002;277:46116–46122. doi: 10.1074/jbc.M209124200. [DOI] [PubMed] [Google Scholar]
- 2.Miquel J, Ramirez-Bosca A, Soler A, et al. Increase with age of serum lipid peroxides: implications for the prevention of atherosclerosis. Mech Ageing Dev. 1998;100:17–24. doi: 10.1016/s0047-6374(97)00118-8. [DOI] [PubMed] [Google Scholar]
- 3.Sohal RS, Weindruch R. Oxidative stress, caloric restriction, and aging. Science. 1996;273:59–63. doi: 10.1126/science.273.5271.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vita JA, Brennan ML, Gokce N, et al. Serum myeloperoxidase levels independently predict endothelial dysfunction in humans. Circulation. 2004;110:1134–1139. doi: 10.1161/01.CIR.0000140262.20831.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazen SL, Gaut JP, Crowley JR, Hsu FF, Heinecke JW. Elevated levels of protein-bound p-hydroxyphenylacetaldehyde, an amino-acid-derived aldehyde generated by myeloperoxidase, are present in human fatty streaks, intermediate lesions and advanced atherosclerotic lesions. Biochem J. 2000;352(pt 3):693–699. [PMC free article] [PubMed] [Google Scholar]
- 6.Sugiyama S, Kugiyama K, Aikawa M, Nakamura S, Ogawa H, Libby P. Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidase-mediated oxidant in plaque erosion and thrombogenesis. Arterioscler Thromb Vasc Biol. 2004;24:1309–1314. doi: 10.1161/01.ATV.0000131784.50633.4f. [DOI] [PubMed] [Google Scholar]
- 7.Brennan ML, Penn MS, Van LF, et al. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med. 2003;349:1595–1604. doi: 10.1056/NEJMoa035003. [DOI] [PubMed] [Google Scholar]
- 8.Zhang R, Brennan ML, Fu X, et al. Association between myeloperoxidase levels and risk of coronary artery disease. JAMA. 2001;286:2136–2142. doi: 10.1001/jama.286.17.2136. [DOI] [PubMed] [Google Scholar]
- 9.Baldus S, Heeschen C, Meinertz T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003;108:1440–1445. doi: 10.1161/01.CIR.0000090690.67322.51. [DOI] [PubMed] [Google Scholar]
- 10.Mocatta TJ, Pilbrow AP, Cameron VA, et al. Plasma concentrations of myeloperoxidase predict mortality after myocardial infarction. J Am Coll Cardiol. 2007;49:1993–2000. doi: 10.1016/j.jacc.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 11.Tang WH, Tong W, Troughton RW, et al. Prognostic value and echocardiographic determinants of plasma myeloperoxidase levels in chronic heart failure. J Am Coll Cardiol. 2007;49:2364–2370. doi: 10.1016/j.jacc.2007.02.053. [DOI] [PubMed] [Google Scholar]
- 12.Meuwese MC, Stroes ES, Hazen SL, et al. Serum myeloperoxidase levels are associated with the future risk of coronary artery disease in apparently healthy individuals: the EPIC-Norfolk Prospective Population Study. J Am Coll Cardiol. 2007;50:159–165. doi: 10.1016/j.jacc.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 13.Wiersma JJ, Meuwese MC, van Miert JN, et al. Diabetes mellitus type 2 is associated with higher levels of myeloperoxidase. Med Sci Monit. 2008;14:CR406–CR410. [PubMed] [Google Scholar]
- 14.Huerta JM, Gonzalez S, Fernandez S, Patterson AM, Lasheras C. Lipid peroxidation, antioxidant status and survival in institutionalised elderly: a five-year longitudinal study. Free Radic Res. 2006;40:571–578. doi: 10.1080/10715760600580470. [DOI] [PubMed] [Google Scholar]
- 15.Marniemi J, Jarvisalo J, Toikka T, Raiha I, Ahotupa M, Sourander L. Blood vitamins, mineral elements and inflammation markers as risk factors of vascular and non-vascular disease mortality in an elderly population. Int J Epidemiol. 1998;27:799–807. doi: 10.1093/ije/27.5.799. [DOI] [PubMed] [Google Scholar]
- 16.Landi F, Russo A, Cesari M, et al. The ilSIRENTE study: a prospective cohort study on persons aged 80 years and older living in a mountain community of Central Italy. Aging Clin Exp Res. 2005;17:486–493. doi: 10.1007/BF03327416. [DOI] [PubMed] [Google Scholar]
- 17.Morris JN, Fries BE, Bernabei R, et al. RAI—Home Care Assessment Manual. Washington, DC: InterRAI Coporation; 1996. [Google Scholar]
- 18.Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 19.Morris JN, Fries BE, Steel K, et al. Comprehensive clinical assessment in community setting: applicability of the MDS-HC. J Am Geriatr Soc. 1997;45:1017–1024. doi: 10.1111/j.1532-5415.1997.tb02975.x. [DOI] [PubMed] [Google Scholar]
- 20.Landi F, Tua E, Onder G, et al. Minimum data set for home care: a valid instrument to assess frail older people living in the community. Med Care. 2000;38:1184–1190. doi: 10.1097/00005650-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48:1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 22.Stefanescu A, Braun S, Ndrepepa G, et al. Prognostic value of plasma myeloperoxidase concentration in patients with stable coronary artery disease. Am Heart J. 2008;155:356–360. doi: 10.1016/j.ahj.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 23.Cavusoglu E, Ruwende C, Eng C, et al. Usefulness of baseline plasma myeloperoxidase levels as an independent predictor of myocardial infarction at two years in patients presenting with acute coronary syndrome. Am J Cardiol. 2007;99:1364–1368. doi: 10.1016/j.amjcard.2006.12.060. [DOI] [PubMed] [Google Scholar]
- 24.Apple FS, Pearce LA, Chung A, Ler R, Murakami MM. Multiple biomarker use for detection of adverse events in patients presenting with symptoms suggestive of acute coronary syndrome. Clin Chem. 2007;53:874–881. doi: 10.1373/clinchem.2006.080192. [DOI] [PubMed] [Google Scholar]
- 25.Dominguez-Rodriguez A, Samimi-Fard S, Abreu-Gonzalez P, Garcia-Gonzalez MJ, Kaski JC. Prognostic value of admission myeloperoxidase levels in patients with ST-segment elevation myocardial infarction and cardiogenic shock. Am J Cardiol. 2008;101:1537–1540. doi: 10.1016/j.amjcard.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 26.Khan SQ, Kelly D, Quinn P, Davies JE, Ng LL. Myeloperoxidase aids prognostication together with N-terminal pro-B-type natriuretic peptide in high-risk patients with acute ST elevation myocardial infarction. Heart. 2007;93:826–831. doi: 10.1136/hrt.2006.091041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang WH, Katz R, Brennan ML, et al. Usefulnessof myeloperoxidase levels in healthy elderly subjects to predict risk for developing heart failure. Am J Cardiol. doi: 10.1016/j.amjcard.2009.01.026. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abu-Soud HM, Hazen SL. Nitric oxide is a physiological substrate for mammalian peroxidases. J Biol Chem. 2000;275:37524–37532. doi: 10.1074/jbc.275.48.37524. [DOI] [PubMed] [Google Scholar]
- 29.Fu X, Kassim SY, Parks WC, Heinecke JW. Hypochlorous acid oxygenates the cysteine switch domain of pro-matrilysin (MMP-7). A mechanism for matrix metalloproteinase activation and atherosclerotic plaque rupture by myeloperoxidase. J Biol Chem. 2001;276:41279–41287. doi: 10.1074/jbc.M106958200. [DOI] [PubMed] [Google Scholar]
- 30.Hazen SL, Heinecke JW. 3-Chlorotyrosine, a specific marker of myeloperoxidase-catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. J Clin Invest. 1997;99:2075–2081. doi: 10.1172/JCI119379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng L, Nukuna B, Brennan ML, et al. Apolipoprotein A-I is a selective target for myeloperoxidase-catalyzed oxidation and functional impairment in subjects with cardiovascular disease. J Clin Invest. 2004;114:529–541. doi: 10.1172/JCI21109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng L, Settle M, Brubaker G, et al. Localization of nitration and chlorination sites on apolipoprotein A-I catalyzed by myeloperoxidase in human atheroma and associated oxidative impairment in ABCA1-dependent cholesterol efflux from macrophages. J Biol Chem. 2005;280:38–47. doi: 10.1074/jbc.M407019200. [DOI] [PubMed] [Google Scholar]
- 33.Marsche G, Hammer A, Oskolkova O, Kozarsky KF, Sattler W, Malle E. Hypochlorite-modified high density lipoprotein, a high affinity ligand to scavenger receptor class B, type I, impairs high density lipoprotein-dependent selective lipid uptake and reverse cholesterol transport. J Biol Chem. 2002;277:32172–32179. doi: 10.1074/jbc.M200503200. [DOI] [PubMed] [Google Scholar]
- 34.Zuliani G, Romagnoni F, Bollini C, Leoci V, Soattin L, Fellin R. Low levels of high-density lipoprotein cholesterol are a marker of disability in the elderly. Gerontology. 1999;45:317–322. doi: 10.1159/000022112. [DOI] [PubMed] [Google Scholar]
- 35.Moradi H, Pahl MV, Elahimehr R, Vaziri ND. Impaired antioxidant activity of high-density lipoprotein in chronic kidney disease. Transl Res. 2009;153:77–85. doi: 10.1016/j.trsl.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 36.Dotan Y, Lichtenberg D, Pinchuk I. Lipid peroxidation cannot be used as a universal criterion of oxidative stress. Prog Lipid Res. 2004;43:200–227. doi: 10.1016/j.plipres.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 37.Rowe JW. The new gerontology. Science. 1997;278:367. doi: 10.1126/science.278.5337.367. [DOI] [PubMed] [Google Scholar]