Abstract
Objective:
To assess risk and protective factors for suicidality at 6-month follow-up in adolescent inpatients after a suicide attempt.
Methods:
One hundred seven adolescents from 5 inpatient units who had a suicide attempt were seen at 6-month follow-up. Baseline measures included sociodemographics, mood and suicidality, dependence, borderline symptomatology, temperament and character inventory (TCI), reasons for living, spirituality, and coping scores.
Results:
At 6-month follow-up, 41 (38%) subjects relapsed from suicidal behaviours. Among them, 15 (14%) had repeated a suicide attempt. Higher depression and hopelessness scores, the occurrence of a new suicide attempt, or a new hospitalization belonged to the same factorial dimension (suicidality). Derived from the best-fit structural equation modelling for suicidality as an outcome measure at 6-month follow-up, risk factors among the baseline variables included: major depressive disorder, high depression scores, and high scores for TCI self-transcendence. Only one protective factor emerged: coping–hard work and achievement.
Conclusion:
In this very high-risk population, some established risk factors (for example, a history of suicide attempts) may not predict suicidality. Our results suggest that adolescents who retain high scores for depression or hopelessness, who remain depressed, or who express a low value for life or an abnormally high connection with the universe are at higher risk for suicidality and should be targeted for more intense intervention. Improving adolescent motivation in school and in work may be protective. Given the sample size, the model should be regarded as exploratory.
Keywords: suicide, follow-up, adolescent, risk factor, protective factor, structural equation modeling
Abstract
Objectif:
Évaluer les facteurs de risque et de protection de la suicidabilité au suivi de 6 mois d’adolescents hospitalisés pour une tentative de suicide.
Méthodes:
Cent sept adolescents de 5 unités d’hospitalisation qui ont fait une tentative de suicide ont été vus à un suivi de 6 mois. Les mesures de base étaient les scores sociodémographiques, d’humeur et suicidabilité, de dépendance, de symptomatologie limite, de l’inventaire de tempérament et caractère (TCI), de raisons de vivre, de spiritualité, et d’adaptation.
Résultats:
Au suivi de 6 mois, 41 (38 %) sujets ont eu une rechute de comportement suicidaire. Parmi ceux-ci, 15 (14 %) ont répété une tentative de suicide. Des scores plus élevés de dépression et de désespoir et la survenue d’une nouvelle tentative de suicide ou d’une nouvelle hospitalisation s’inscrivaient dans la même dimension factorielle (suicidabilité). Dérivés de la modélisation par équation structurelle la mieux ajustée à la suicidabilité comme mesure de résultat au suivi de 6 mois, les facteurs de risque des variables de base étaient notamment : le trouble dépressif majeur, des scores de dépression élevés, et des scores élevés d’auto-transcendance au TCI. Un seul facteur de protection s’est dégagé : l’adaptation – travailler dur et réussir.
Conclusion:
Dans cette population à risque très élevé, certains facteurs de risque établis (par exemple, des antécédents de tentatives de suicide) peuvent ne pas prédire la suicidabilité. Nos résultats suggèrent que les adolescents qui maintiennent des scores élevés de dépression et de désespoir, qui demeurent déprimés, ou qui expriment une valeur faible pour la vie ou une connexion anormalement élevée avec l’univers sont à risque accru de suicidabilité et devraient être la cible d’interventions plus intenses. Améliorer la motivation des adolescents à l’école et au travail peut servir de protection. Étant donné la taille de l’échantillon, le modèle doit être considéré exploratoire.
Suicide is the second leading cause of death in adolescents and young adults in European countries.1 In France, recent epidemiological data showed that the suicide rate in adolescents, aged 15 to 19, was 4.1/100 000 inhabitants in 2007 (5.8 in males; 2.3 in females).2 Suicidal behaviours are also the main reason for adolescent psychiatric hospitalizations in many countries. The annual prevalence of suicidal ideation ranges from 15% to 25% in the general population,3 whereas the lifetime estimates for a suicide attempt among adolescents ranges from 1.3% to 3.8% in males and from 1.5% to 10.1% in females, with higher rates in females than in males in the older age range.4 Moreover, adolescents who die by suicide are at risk having been exposed to early life adversities, having made a prior suicide attempt, and being left without appropriate health care support within the month prior to the completion.5,6
Current models of suicide phenomena in youth have emphasized: the importance of distinguishing suicidal ideation, nonsuicidal self-harm, suicide attempt, and successful suicide7; the key role of depression in the process that transforms suicidal ideation into a suicide attempt, with depression being a strong proximal factor8; that the numerous identified risk factors do not adequately capture the outcome; and that protective factors may have to be taken into account for suicide prediction.9,10
Clinical Implications
In adolescents who attempted suicide, the maintenance of depression and hopelessness, seeking intense spiritual help, expressing a low value for life, or high connection with the universe exposed them to relapse before 6 months.
School inclusion and motivation should be promoted.
Limitations
The sample size may have limited power for some variables.
Some sites did not recruit in the same way and may have introduced biases.
Some important risk factors (for example, family history and cohesion, sexual abuse, and school bullying) were not assessed.
Compared with general population studies, fewer longitudinal studies have assessed the re-occurrence of suicide attempts in adolescents who have previously attempted suicide. Proximal risk factors include depressed mood,11–13 hopelessness,14 suicidal ideation,12,15 more severe functional impairment,11 poor family cohesion,16,17 and low peer connectedness.17 Long-lasting or distal risk factors include a previous history of suicide attempts,15–19 a lower maximum lethality for the previous suicide attempts,16 high scores for anger and hostility,19 bipolar20 or borderline personality symptomatology,21 a history of sexual abuse,16,21 a family history of suicide attempts in relatives,11 and a family history of mental health problems.11 Protective factors have been less explored in studies in very high-risk samples, with the possible exception of coping. Adolescents with previous suicide attempts show less task-oriented coping.22
Our study aimed to conduct univariate and multivariate analyses of potential risk and protective factors and to compute a model of suicidality at follow-up.23 To do so, proximal and distal risk and protective factors (sociodemographics, mood, hopelessness and suicidality, self-esteem, borderline personality symptomatology, dependence, recent life events, spirituality, reasons for living, TCI scores, and coping scores) were studied at baseline in a sample of 107 inpatient adolescents hospitalized for a suicide attempt (T1). At 6-month follow-up, we re-assessed mood, suicidality, treatment, and services given during the follow-up period and assessed T1 factors predictive of readmissions for suicidal behaviours during follow-up.
Methods
Our study, called the “Evaluation des modalités de prise en charge post hospitalière des adolescents suicidants,” is a multisite, naturalistic, prospective study on suicidal behaviours in adolescents involving 3 periods of data collection: baseline, 6-month follow-up, and 12-month follow-up. Here, we present preliminary results on the 6-month follow-up.
Participants
From January to December 2011, subjects aged 13 to 17 years were recruited from 5 pediatric departments (Rouen, Amiens, Crépy, Creil, and Meaux) in France. All adolescents who presented in the ED for a suicide attempt (according to Columbia Classification Algorithm of suicide assessment7) were invited to be hospitalized in keeping with French national clinical practice guidelines.24 The exclusion criteria included an inability to provide written informed consent (for example, moderate to severe cognitive impairment) or a current medical condition or residence outside of the geographical area of each centre to limit lost patients at follow-up. Consent for minors was obtained from each adolescent as well as from both parents. Clinical research interviews were performed by a research psychiatrist or resident. Ethics approval was obtained from the Nord-Ouest I (Centre Hospitalo–Universitaire Charles-Nicolle) Group Ethics and Medical Research Committee.
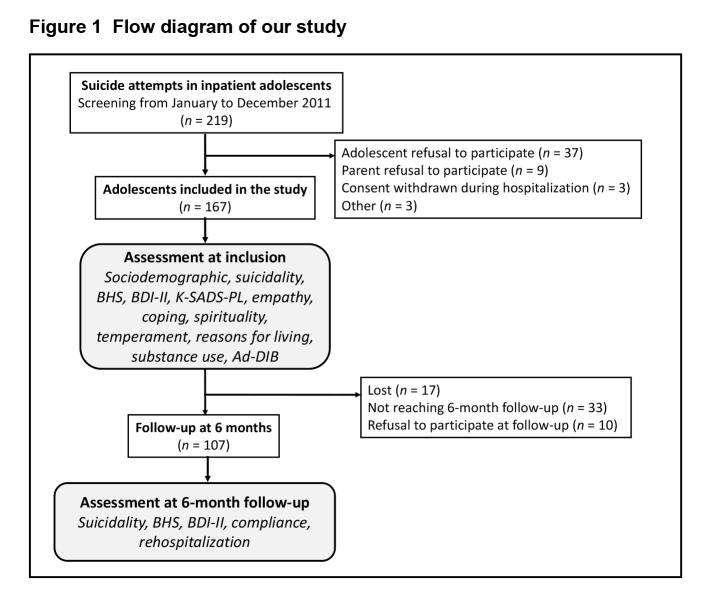
Figure 1 summarizes the flow diagram for our study. An initial 219 patients were eligible, and 167 were enrolled during their inpatient stay. The demographics of patients who refused to participate were comparable with those of the participants for average age (14.6 years for participants, compared with 15.1 years for nonparticipants) and sex (79% female participants, compared with 76% female nonparticipants). Among the 167 participants, the relative proportion of adolescents included in the study was 50% in Rouen, 24% in Amiens, 15% in Crépy, 7% in Creil, and 4% in Meaux. The centres did not differ on a subjects’ age, sex, or the presence of an internalized or externalized disorder. After discharge, treatment plans were made as usual practice in each centre except for telephone support that was systematically implemented in the Rouen site. At 6-month follow-up, 107 adolescents had a follow-up clinical assessment. There was no difference in baseline characteristics between patients assessed at follow-up and those who were not assessed for BDI-II scores, BHSs, and the number of suicide attempts (BDI-II: mean 23.5 [SD 13], compared with mean 22.1 [SD 13.8], P = 0.51; BHS: mean 8.4 [SD 5.5], compared with mean 9.3 [SD 5.6], P = 0.30; and number of suicide attempts: mean 1.6 [SD 1.5], compared with mean 1.3 [SD 0.7], P = 0.14).
Figure 1.
Flow diagram of our study
Measures
Details of the baseline measures are given in the related report by Labelle et al25 in this supplement. The baseline measures included: sociodemographic characteristics; DSM-IV Axis I main diagnoses and GAF obtained after a standardized interview, the Schedule for Mood Disorders and Schizophrenia for Children and Adolescents of School Age, Version Current and Past Episode (Kiddie-SADS-Present and Lifetime Version interview)26; depression, hopelessness and suicidality as scored with the BDI-II,27 the BHI, and the Posner Scale7, respectively, substance use and misuse as assessed with the Dependence Questionnaire for Adolescents (DEP-ADO)28; borderline personality symptomatology as scored with the Abbreviated Self-Questionnaire of the Diagnostic Interview for Borderline Personality Disorder29; and self-esteem with the Rosenberg Self-Esteem Rating Questionnaire.30
We also used the following scales as they have shown good psychometric properties and high interests in adolescent suicidal behaviours (for details, see Labelle et al25 in this supplement):
the Eysenck Questionnaire to score impulsity;
the Buss-Durke Hostility Inventory;
the TCI-56 items to score 4 temperaments (novelty seeking, harm avoidance, reward dependence, and persistence) and 3 characters (self-directedness, cooperativeness, and self-transcendence)31;
the SS to score spiritual beliefs, self-discovery, self-awareness and collective consciousness, and respect for others and environment32;
the RFL-A was used to score family alliance, suicide-related concerns, self-acceptance, peer acceptance and support, and future optimism33; and
the ACS to assess how adolescents cope with a situation or resolve a problem by scoring 3 main factors: productive coping, nonproductive coping, and reference to others.34,35 Given the key role of traumatic life, we also used the Newcomb Life Events Questionnaire for Adolescents.36
At 6-month follow-up, we explored the treatment given to participants after their stay through a standardized questionnaire querying psychotropic treatment, formal psychotherapy, family treatment, group approaches, and telephone support that was systematically implemented in the Rouen site. Suicidal ideation and suicide attempts were scored using the Posner Scale. As current depression and hopelessness are important proximal factors for suicidality, patients received the BDI-II and BHS again at 6-month follow-up. We define relapse as all patients rehospitalized for suicidal behaviours during the 6-month follow-up period (whether they had repeated a suicide attempt or not), plus all patients who reported a new suicide attempt without hospitalization. Participants are fully described in Table 1.
Table 1.
Adolescents who attempted suicide and successfully followed up at 6 months (n = 107): characteristics at inclusion
| Sociodemographic characteristics | |
|
| |
| Age, years, mean (SD), range | 14.91 (1.4), 12.1–17.7 |
| Sex, n (%) | |
| Female | 90 (84) |
| Male | 17 (16) |
| Number of children in the family, mean (SD), range | 2.4 (1.22), 0–6.0 |
| Significant life events, mean (SD), range | 3.85 (2.23), 0–11.0 |
| Living with both parents, n (%) | 48 (45) |
| One parent plus a step parent | 11 (10) |
| Living with one parent, n (%) | 34 (32) |
| Other (for example, foster care) | 14 (13) |
| Typical school, n (%) | 87 (83) |
| Vocational school, n (%) | 18 (17) |
| At least 1 class repeated, n (%) | |
| No | 66 (62) |
| Yes | 41 (38) |
| Suicidality characteristics | |
|
| |
| Number of suicide attempts, mean (SD), range | 1.56 (1.45), 1–10.0 |
| Posner ideation, n (%) | 29 (28) |
| No | 20 (19) |
| Passive | 53 (51) |
| Active | 2 (2) |
| Posner intentionality, n (%) | 25 (24) |
| No | 14 (13) |
| Masked | 38 (36) |
| Ambivalent | 26 (25) |
| Definitive | 2 (2) |
| Method of suicide attempt, n (%) | |
| Intoxication | 82 (84) |
| Laceration | 7 (7) |
| Precipitation | 1 (1) |
| Strangulation | 5 (5) |
| Other | 3 (3) |
| Clinical characteristics | |
|
| |
| Major depressive episode, yes, n (%) | 65 (64) |
| Borderline disorder, yes, n (%) | 70 (67) |
| BDI-II, mean (SD), range | 23.51 (12.99), 0–53.0 |
| BHS, mean (SD), range | 8.38 (5.46), 0–19.0 |
| Ab-DIB score, mean (SD), range | 17.78 (9.30), 0–40.0 |
| GAF, mean (SD), range | 68.15 (15.58), 15.0–92.0 |
| Eysenck impulsivity, mean (SD), range | 12.25 (4.77), 2.0–22.0 |
| Self-esteem, mean (SD), range | 4.54 (2.76), 0–10.0 |
| Dependence total score, mean (SD), range | 8.02 (7.07), 0–43 |
|
| |
| Dimensional characteristics | |
|
| |
| SS, mean (SD), range | |
| Spiritual beliefs | 18.6 (7.62), 4.0–38.0 |
| Self-discovery | 20.14 (4.23), 7.0–28.0 |
| Self-awareness and collective consciousness | 15.37 (4.41), 5.0–25.0 |
| Respect of others and environment | 19.22 (3.15), 7.0–24.0 |
| Total | 73.4 (14.11), 36.0–102.0 |
| RFL-A, mean (SD), range | |
| Family alliance | 4.48 (1.02), 1.0–6.0 |
| Suicide related concerns | 3.44 (1.4), 0.33–6.0 |
| Self-acceptance | 3.96 (1.12), 1.0–6.0 |
| Peer acceptance and support | 4.61 (0.98), 1.0–6.0 |
| Future optimism | 4.37 (1.0), 1.4–6.0 |
| Total | 4.19 (0.87), 1.63–6.0 |
| TCI, mean (SD), range | |
| Novelty seeking | 16.52 (4.22), 5.0–30.0 |
| Persistence | 15.47 (4.41), 4.0–26.0 |
| Harm avoidance | 17.91 (4.70), 5.0–31.0 |
| Self-directedness | 16.12 (5.29), 1.0–27.0 |
| Reward dependence | 18.88 (4.75), 8.0–29.0 |
| Cooperativeness | 18.77 (5.43), 4.0–32.0 |
| Self-transcendence | 10.16 (8.68), 0–24.0 |
| ACS, mean (SD), range | |
| Seek social support | 54.23 (18.79), 20.0–96.0 |
| Focus on solving problem | 54.25 (14.97), 16.0–96.0 |
| Work hard and achieve | 63.13 (15.53), 12.0–96.0 |
| Worry | 52.53 (16.09), 20.0–100.0 |
| Invest in close friends | 62.64 (16.45), 28.0–96.0 |
| Seek to belong | 58.06 (14.3), 24.0–88.0 |
| Wishful thinking | 49.09 (15.74), 20.0–84.0 |
| Not coping | 49.13 (17.16), 12.0–96.0 |
| Tension reduction | 52.53 (16.35), 20.0–92.0 |
| Social action | 31.12 (10.73), 20.0–70.0 |
| Ignore the problem | 48.74 (17.13), 20.0–85.0 |
| Self-blame | 58.16 (19.53), 15.0–100.0 |
| Keep to self | 62.50 (19.72), 15.0–100.0 |
| Seek spiritual support | 32.26 (19.51), 15.0–100.0 |
| Focus on the positive | 52.82 (16.32), 20.0–95.0 |
| Seek professional help | 42.14 (18.28), 20.0–85.0 |
| Seek relaxing diversions | 76.86 (18.07), 21.0–105.0 |
| Physical recreation | 63.66 (24.28), 21.0–105.0 |
Ad-DIB = Abbreviated Self-Questionnaire of the Diagnostic Interview for Borderline Personality Disorder; RFL-A = Reasons for Living Inventory for Adolescents; SS = Spirituality Scale
Statistical Analysis
All statistical analyses were performed using the R statistical package, version 2.12.2.37 The significance level alpha was set at 0.05, and all statistical tests were 2-tailed.
First, we conducted several univariate analyses to explore variables measured at inclusion that were significantly associated with a new suicide attempt or a new hospitalization during the 6-month follow-up. Given the literature and the model we used to plan the study, which indicates both depression and hopelessness as key proximal risk factors for suicide attempts, we also performed univariate regression analysis to assess variables measured at inclusion that were significantly associated with BDI-II scores and BHSs at 6-month follow-up, after adjusting for the score at inclusion.
Second, to model suicidality at follow-up, we chose to use SEM, a statistical method that combines a factorial approach with regressions, in our case partial least square regression modelling. We choose this method as it is highly accurate to model prediction even when sample sizes are limited, and when several variables are strongly correlated, it allows creating a latent variable to better assess outcome.38 As suicidality is a complex variable, to model suicidality, we hypothesized a single latent variable related to relapse during the 6-month follow-up period, and related to high BDI-II scores and high BHSs at 6-month follow-up. These are all key proximal risk factors for suicidality. Before computing the model, we performed multivariate analyses to retain the most explanatory variables from the univariate analyses in a comprehensive model to predict relapse for suicidal behaviours during the 6-month follow-up and to explore the relation between variables at admission and variables at 6-month follow-up (or proxy variables). Therefore, the model included suicidality as a latent variable related to 3 dependent variables as follows: relapse during follow-up, BHS, and BDI-II scores at 6-month follow-up. Explanatory variables were those selected after a multivariate analysis exploring the 3 different variables. Several computations were made to eliminate variables that did not contribute to the final model. To check the quality of the final model, we explored whether the 3 dependent variables were included in a common dimension (which could possibly relate to our latent variable, suicidality). We also calculated several quality parameters, such as the CFI, TLI, and RMSEA.
Results
Univariate Analyses
Among the 107 adolescents with available data at 6-month follow-up, 41 (40.6%) relapsed from suicidal behaviours during the follow-up period. Among them, 15 (17%) had repeated a suicide attempt. Table 2 shows all of the variables that showed a significant association with the variables to be predicted at follow-up: relapse during 6-month follow-up, BDI-II score and BHS at 6-month follow-up. We also detailed risk and protective factors of new suicide attempts and new hospitalizations for indicative purposes as they were fused in the relapse variable.
Table 2.
Univariate analysis in adolescents hospitalized for a suicide attempt at 6-month follow-up (n = 107)
| Relapse from suicidal behaviours during the 6-month follow-up, n = 85 | No n = 51 | Yes n = 34 | t, df = 83 | P |
|
| ||||
| Major depressive disorder at first hospitalization, n = 85, (%) | 27 (53) | 25 (74) | 2.9 (1–9.4)a | 0.06 |
| BDI-II, mean (SD) | 11.5 (9.9) | 21 (14.1) | 3.21 | 0.002 |
| BHS, mean (SD) | 5 (3.4) | 8.4 (5.2) | 3.21 | 0.002 |
| ACS seek spiritual support, mean (SD) | 26.8 (11.7) | 36.5 (25.4) | 2.07 | 0.04 |
| New suicide attempt, n = 88 | No n = 63 | Yes n = 15 | t, df = 86 | P |
|
| ||||
| BDI-II, mean (SD) | 12.9 (10.5) | 20.7 (15.2) | 2.36 | 0.02 |
| SS self-awareness and collective consciousness, mean (SD) | 15.7 (4.5) | 13.0 (4.3) | 2.03 | 0.04 |
| ACS work hard and achieve, mean (SD) | 64.7 (13.4) | 51.7 (20.5) | 2.26 | 0.04 |
| ACS physical recreation, mean (SD) | 66 (24.4) | 47 (24.3) | 2.6 | 0.01 |
| New hospitalization, n = 101 | No n = 75 | Yes n = 26 | t, df = 99 | P |
|
| ||||
| BDI-II, mean (SD) | 13.9 (11.9) | 23.1 (14.8) | 2.94 | 0.004 |
| BHS, mean (SD) | 5.2 (3.9) | 9.4 (5.3) | 3.93 | <0.001 |
| Number of suicide attempts at first hospitalization, mean (SD) | 1.3 (0.8) | 2.4 (2.4) | 2.23 | 0.03 |
| ACS seek social support, mean (SD) | 56.9 (18.5) | 46.6 (18.3) | 2.42 | 0.02 |
| GAF at first hospitalization, mean (SD) | 70.8 (13.9) | 63.2 (18.5) | 2.11 | 0.03 |
| Self-esteem, mean (SD) | 4.1 (2.8) | 5.5 (2.7) | 2.03 | 0.05 |
| Hopelessness (BHS), n = 107b | Estimate | Standard error | t, df = 105 | P |
|
| ||||
| Ab-DIB score | 0.16 | 0.05 | 3.37 | 0.001 |
| BDI-II at first hospitalization | 0.15 | 0.039 | 3.76 | <0.001 |
| BDI-II | 0.22 | 0.026 | 8.58 | <0.001 |
| TCI cooperativeness | −0.18 | 0.07 | 2.57 | 0.01 |
| ACS work hard and achieve | −0.06 | 0.029 | 2.08 | 0.04 |
| ACS seek relaxing diversion | 0.06 | 0.024 | 2.5 | 0.01 |
| Eysenck impulsivity | 0.29 | 0.09 | 3.17 | 0.002 |
| Depression (BDI-II score), n = 107b | Estimate | Standard error | t, df = 105 | P |
|
| ||||
| Ab-DIB score | 0.32 | 0.14 | 2.21 | 0.03 |
| BHS | 1.6 | 0.24 | 6.55 | <0.001 |
| Spirituality–spiritual beliefs | 0.33 | 0.13 | 2.4 | 0.02 |
| TCI harm avoidance | −0.55 | 0.27 | 2.07 | 0.04 |
| TCI self-transcendence | 0.62 | 0.18 | 3.41 | <0.001 |
| ACS seek social support | 0.12 | 0.05 | 2.12 | 0.03 |
| GAF at first hospitalization | 0.15 | 0.07 | 1.94 | 0.06 |
OR (95% CI);
Adjusted on score at inclusion (first hospitalization)
Ad-DIB = Abbreviated Self-Questionnaire of the Diagnostic Interview for Borderline Personality Disorder
Higher BHS and BDI-II scores at 6-month follow-up and higher scores for the ACS seek spiritual support were significant risk factors for relapse from suicidal behaviours at 6-month follow-up. Higher BDI-II scores at 6-month follow-up were the only risk factor for new suicide attempts at 6-month follow-up. Three protective factors emerged from the variables assessed at inclusion as follows: the ACS hard work and achievement, physical recreation and spirituality self-awareness, and collective consciousness. Several variables were significantly associated with risk for a new hospitalization during 6-month follow-up: higher BHS and BDI-II scores at 6-month follow-up, the number of suicide attempts at inclusion, and the severity at inclusion. The ACS seeking social support was the only protective factor that emerged from the variables assessed at inclusion.
Higher hopelessness (BHS) at 6-month follow-up was significantly associated with higher borderline personality, impulsivity, and the ACS seeking relaxing diversion scores at inclusion and BDI-II scores at 6-month follow-up. Higher TCI cooperativeness and ACS hard work and achievement scores predicted lower BHS at 6-month follow-up.
Higher depression (BDI-II) scores at 6-month follow-up were significantly associated with higher borderline personality, severity (GAF), spiritual beliefs, TCI self-transcendence, and higher ACS seeking social support scores at inclusion and higher BHS at 6-month follow-up. Higher TCI harm avoidance scores predicted lower BDI-II scores at 6-month follow-up.
Modelling Suicidality at 6-Month Follow-Up
As suicidality is a complex variable, to model suicidality, we hypothesized it could be a latent variable related to relapse from suicidal behaviours during follow-up and to high BDI-II and BHS at 6-month follow-up. These are the key proximal risk factors for suicidality. To enter fewer potential explanatory variables into the model, we also conducted multivariate regression based on previous univariate analyses to select the most robust variables that predicted BHS and BDI-II scores at 6-month follow-up. We also performed new analyses to explore relapse from suicidal behaviours.
Using multivariate regression, higher BDI-II (estimate = 0.1, SE = 0.04, t = 2.57, df = 81, P = 0.01), and impulsivity (estimate = 0.2, SE = 0.09, t = 2.21, df = 81, P = 0.03) scores at inclusion predicted higher hopelessness (BHS) at 6-month follow-up. Also, higher ACS hard work and achievement scores at inclusion predicted lower BHS at 6-month follow-up. Finally, higher TCI self-transcendence (estimate = 0.62, SE = 0.18, t = 3.41, df = 87, P < 0.001) and BDI-II scores at inclusion (estimate = 0.58, SE = 0.077, t = 7.43, df = 87, P < 0.001) predicted higher depression (BDI-II) scores at 6-month follow-up.
Multivariate analysis showed that risk factors for relapse from suicidal behaviours included the existence of a MDE (OR 3.25; 95% CI 1.17 to 10.2, P = 0.03) and a higher ACS seeking spiritual support score at inclusion (OR 1.03; 95% CI 1.005 to 1.064, P = 0.03); this means that an ACS seeking spiritual support score increase of 20 points increased the odds ratio for relapse by a factor of 1.8 (e20 × 0.03). No protective factors were found.
The first SEM model included suicidality as a latent variable related to 3 dependent variables as follows: relapse from suicidal behaviors during the follow-up period, as well as BHS and BDI-II scores at 6-month. Explanatory variables were impulsivity, BDI, TCI self-transcendence, ACS seeking spiritual support, ACS hard work and achievement scores, and the existence of a MDE at inclusion. Impulsivity and ACS seeking spiritual support score did not reach statistical significance.
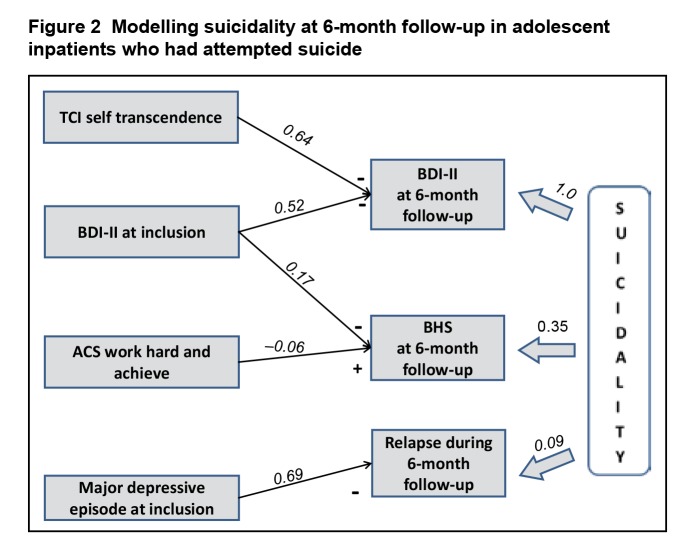
The final SEM model is summarized in Figure 2 and shows excellent quality parameters. First, the 3 dependent variables (relapse, BHS, and BDI-II scores at 6-month follow-up) did, indeed, belong to a common dimension, for example, a common latent variable (suicidality), as they were significantly associated (BDI-II as baseline: estimate = 0.347, SE = 0.11, P = 0.002; for BHS: estimate = 0.088, SE = 0.025, P = 0.001 for relapse). Second, model quality parameters were excellent: the CFI and the TLI were close to 1 as expected (CFI = 0.96 and TLI = 0.92). The RMSEA was close to 0 as expected (RMSEA = 0.08; 90% CI 0.00 to 0.17). Statistical links between variables in the model are indicated in Figure 2. Risk factors included higher BDI-II and TCI self-transcendence scores and the existence of a MDE at inclusion. We found only 1 significant protective factor: higher ACS hard work and achievement scores at inclusion.
Figure 2.
Modelling suicidality at 6-month follow-up in adolescent inpatients who had attempted suicide
Discussion
Summarizing Current Data
In adolescents hospitalized for a suicide attempt, the risk of relapse for suicidal behaviours is very high (40.6% in our sample). Among these relapses, re-occurrence of active suicidal behaviours (suicide attempt) is also high (17%). These rates are in line with those found in previous similar studies16,21 conducted in inpatients that range between 19% to 26% for new suicidal events and 12% to 19% for new suicide attempts during the first 6-month follow-up and confirm that adolescent inpatients who experienced a suicide attempt should be regarded as very high risk subjects.The best fitting SEM did confirm that high depression and hopelessness scores at 6-month follow-up and the occurrence of relapses for suicidal behaviours belonged to the same factorial dimension. Risk factors among the baseline variables included a diagnosis of MDD, high depression scores, and high scores for TCI self-transcendence; only 1 protective factor emerged, ACS hard work and achievement.
Limitations and Strengths
Although our study has some strengths (multisite, prospective, context of free access to care, and hypotheses driven), the exploratory model should be interpreted within the study limitations. First, the sample size may have limited power for some variables (for example, the borderline dimension, impulsivity, and the 1-point data for 6-month follow-up) and did not permit the inclusion of treatment moderators in the model. We are hoping to include these measures in further research as the study is still ongoing. Second, the 6-month follow-up was short, and we expect more suicidal events to occur during the next 6 months.15 Third, some sites did not recruit in the same way and may have introduced biases despite the absence of any site effects in the analysis. Fourth, some important risk factors were not assessed: history of suicide attempts in relatives,11 family history of mental health problems,11 poor family cohesion,16,17 parental relationship,39 sexual abuse, and school bullying.40,41 Finally, the sampling only captured a part of the adolescents who died by suicide (Berkson bias) as many completers may not be hospitalized or experience a previous suicide attempt.5
Comments on Positive Results
Regarding the clinical risk factors found here, we are not surprised that we again found that MDD, high depression scores at baseline, and at 6-month follow-up are significant risk factors. Both a diagnosis of MDD and the severity of the depression are associated with higher risk for re-occurrence of suicide attempts in adolescent inpatients.16,21 More striking are the findings from the coping and temperament instruments that we used to examine spirituality.
Spiritual and religious behaviours have always been part of the human experience; however, much controversy remains as to how we should define them. Historically, religiosity and spirituality were well-defined constructs. Based on qualitative analyses of various definitions, Shek42 reported that the conceptions were distributed over several content areas as connectedness or relationships (horizontality), processes contributing to a higher level of connectedness (verticality), reactions to sacred things, and personal transcendence. Today, spirituality often refers to an individualistic, open-ended, freeing, and ultimately subjective quest, whereas religiosity has been gradually moving toward a more narrow characterization that represents doctrinal and ritual aspects.43 Adolescence and young adulthood appear to be key developmental periods for the settlement of one’s spirituality. Research on the impact of spirituality on adolescent developmental outcomes suggests that high spirituality is associated with overall better youth development.44 In at-risk children (for example, children of a depressed mother), family agreement and the practice of a religious denomination may be a protective factor, independent of the effects of maternal depression.45
In our study, we used several instruments that referred to spirituality: the SS and some factors from the TCI, ACS, and RFL-A. The Delaney Scale did not appear to influence outcomes. The formulation of the questions is always positive, and the scale does not explore how the adolescent uses spirituality to adapt or cope with life experiences. Here, we found that higher TCI self-transcendence scores at baseline were risk factors for suicidality at 6-month follow-up. TCI self-transcendence refers to questions indicating that the adolescent identifies him- or herself as part of the universe (for example, “I have sometimes the feeling I belong to something that has no limit in time nor space”) or has already be involved in an unusual experience (for example, “I think I already experienced once an extra sensorial perception”). In other words, in the context of adolescents who have attempted suicide, those expressing a low value for their life or perceiving themselves as part of a greater universe should be targeted more carefully during treatment. Do these findings mean that, in some cases, the positive support structure commonly present through spirituality is not functioning, as it typically is in general population samples?21 Alternatively, do these findings instead mean that the adolescent is desperately seeking outside or magical forces to overcome their suffering? Or does it mean that in some way these adolescents experienced brief psychotic moments?
Only 1 protective factor emerged from the ACS: hard work and achievement. These strategies suggest that the adolescent is conscientious about work or school, works hard and tries to achieve high standards. Stated as a reverse proposition, it also suggests that poor school achievement and school withdrawal are risk factors for suicide attempts in adolescents.39 As for clinical implications, it suggests that every effort should be made to promote school success and to include in the therapeutic process a discussion of the adolescent’s life goals, especially those that also refer to school and education.
Comments on Negative Predictions
In this very high-risk sample, we found that neither a previous history of suicide attempts at baseline nor the number of suicide attempts prior to hospitalization predicted the re-occurrence of suicidality during the follow-up period in the multivariate analyses. This is contrary to expectations and to other similar studies.15–17,19,46 In our sample, only 5% of the adolescents had not experienced a past suicide attempt; thus, it can be argued that there was not enough variability to assess the prediction. Yen et al21 reported a similar finding and proposed that a past history of suicide attempts might be a more reliable predictor of subsequent suicidality in less acute settings (for example, community, school, or primary care samples).
Borderline personality disorder or traits were the second predictors that were significant in univariate analysis but were not significant in the multivariate model. Greenfield et al46 reported on a 6-month outcome study a large group of adolescents admitted at ED for suicidal behaviours. Borderline personality disorder was associated with subsequent suicidality together with substance use and female sex.46 However, our findings are similar to those of Yen et al.21 As we used a dimensional approach and a borderline construct that included symptoms of impulsivity, depressed mood with suicidality and self-injurious behaviours, and psychosis, it may be possible that the construct was too diffuse to adequately represent as a single independent variable. Although controversial, we recommend the assessment of borderline symptomatology in high-risk adolescents.
The third negative finding was the lack of prediction of substance use in our study. This could be because of the young age of our sample and the middle-town areas for recruitment.
The last negative finding was the lack of prediction of traumatic life events, both recent (<1 year) and lifetime, despite several studies reporting the importance of a history of child sexual abuse.16,21 The Newcomb Inventory includes the probing of 11 events that have occurred in family members and 9 events that were experienced directly by the adolescent. None directly assess a history of child sexual abuse.
Conclusion
In this very high-risk population, the re-occurrence of a suicide attempt during adolescence is a frequent and major public health concern. Risk factors for future suicide attempts in this population are more difficult to ascertain as some established risk factors may not predict suicidality in adolescents. Our results suggest that adolescents who retain high scores for depression or hopelessness, who seek intense spiritual help, or who express a low value for life through being part of the universe are at higher risk of suicidality and should be targeted with more intense intervention. Developing abilities to improve adolescent motivation in school and work may be protective. Given the sample size, the model should be regarded as exploratory.
Acknowledgments
We thank all of the adolescents and their families who participated in our study, as well as the staff from the pediatric EDs of the University Hospitals of Amiens and Rouen, and the General Hospitals of Creil and Meaux. We are also grateful to the Centre Hospitalier Spécialisé du Rouvray, which promoted the study. We also thank the Fondation Pfizer and the Fondation de France for granting the study. None of the sponsors or the promoters interfered with the study design, interpretation of the data, or writing of the draft.
Abbreviations
- ACS
Adolescent Coping Scale
- BDI-II
Beck Depression Inventory, Second Edition
- BHI
Beck Hopelessness Inventory
- BHS
Beck Hopelessness Score
- CFI
Comparative Fit Index
- ED
emergency department
- GAF
Global Assessment of Functioning
- MDD
major depressive disorder
- MDE
major depressive episode
- RFL-A
Reasons for Living Inventory for Adolescent
- RMSEA
root mean square error of approximation
- SE
standard error
- SEM
structural equation modelling
- SS
Spirituality Scale
- TCI
Temperament and Character Inventory
- TLI
Tucker-Lewis Index
References
- 1.European Commission Eurostat . Eurostat [Website] Brussels (BE): Eurostat; 2008. Available from: http://epp.eurostat.ec.europa.eu. [Google Scholar]
- 2.de Tournemire R. Teenagers’ suicides and suicide attempts: finding one’s way in epidemiologic data. Arch Pediatr. 2010;17(8):1202–1209. doi: 10.1016/j.arcped.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Flament MF, Cohen D, Choquet M, et al. Phenomenology, psychosocial correlates and treatment seeking in major depression and dysthymia in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40:1070–1078. doi: 10.1097/00004583-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 5.Renaud J, Berlim MT, Séguin M, et al. Recent and lifetime utilization of health care services by children and adolescent suicide victims: a case–control study. J Affect Disord. 2009;117(3):168–173. doi: 10.1016/j.jad.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Séguin M, Renaud J, Lesage A, et al. Youth and young adult suicide: a study of life trajectory. J Psychiatr Res. 2011;45(7):863–870. doi: 10.1016/j.jpsychires.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Posner K, Oquendo MA, Gould M, et al. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–1043. doi: 10.1176/appi.ajp.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foley DL, Goldston DB, Costello EJ, et al. Proximal psychiatric risk factors for suicidality in youth: the Great Smoky Mountains Study. Arch Gen Psychiatry. 2006;63(9):1017–1024. doi: 10.1001/archpsyc.63.9.1017. [DOI] [PubMed] [Google Scholar]
- 9.Beautrais AL, Collings SCD, Ehrhardt P, et al. Suicide prevention: a review of evidence of risk and protective factors, and points of effective intervention. Wellington (NZ): Ministry of Health; 2005. [Google Scholar]
- 10.Breton JJ, Labelle R, Berthiaume C, et al. Protective factors against depression and suicidal behaviour in adolescence. Can J Psychiatry. 2015;60(2 Supp 1):S5–S15. [PMC free article] [PubMed] [Google Scholar]
- 11.King CA, Kerr DC, Passarelli MN, et al. One-year follow-up of suicidal adolescents: parental history of mental health problems and time to post-hospitalization attempt. J Youth Adolesc. 2010;39(3):219–232. doi: 10.1007/s10964-009-9480-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miranda R, Scott M, Hicks R, et al. Suicide attempt characteristics, diagnoses, and future attempts: comparing multiple attempters to single attempters and ideators. J Am Acad Child Adolesc Psychiatry. 2008;47(1):32–40. doi: 10.1097/chi.0b013e31815a56cb. [DOI] [PubMed] [Google Scholar]
- 13.Spirito A, Valeri S, Boergers J, et al. Predictors of continued suicidal behavior in adolescents following a suicide attempt. J Clin Child Adolesc Psychol. 2003;32(2):284–289. doi: 10.1207/S15374424JCCP3202_14. [DOI] [PubMed] [Google Scholar]
- 14.Aglan A, Kerfoot M, Pickles A. Pathways from adolescent deliberate self-poisoning to early adult outcomes: a six-year follow-up. J Child Psychol Psychiatry. 2008;49(5):508–515. doi: 10.1111/j.1469-7610.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- 15.Prinstein MJ, Nock MK, Simon V, et al. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psychol. 2008;76(1):92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brent DA, Greenhill LL, Compton S, et al. The Treatment of Adolescent Suicide Attempters study (TASA): predictors of suicidal events in an open treatment trial. J Am Acad Child Adolesc Psychiatry. 2009;48(10):987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Czyz EK, Liu Z, King CA. Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. J Clin Child Adolesc Psychol. 2012;41(2):214–226. doi: 10.1080/15374416.2012.651998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gehin A, Kabuth B, Pichene C, et al. Ten year follow-up study of 65 suicidal adolescents. J Can Acad Child Adolesc Psychiatry. 2009;18(2):117–125. [PMC free article] [PubMed] [Google Scholar]
- 19.Goldston DB, Daniel SS, Reboussin DM, et al. Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiatry. 1999;38(6):660–671. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Halfon N, Labelle R, Cohen D, et al. Juvenile bipolar disorder and suicidality: a review of the last 10 years of literature. Eur Child Adolesc Psychiatry. 2013;22(3):139–151. doi: 10.1007/s00787-012-0328-z. [DOI] [PubMed] [Google Scholar]
- 21.Yen S, Weinstock LM, Andover MS, et al. Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychol Med. 2013;43(5):983–993. doi: 10.1017/S0033291712001912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nrugham L, Holen A, Sund AM. Suicide attempters and repeaters: depression and coping: a prospective study of early adolescents followed up as young adults. J Nerv Ment Dis. 2012;200(3):197–203. doi: 10.1097/NMD.0b013e318247c914. [DOI] [PubMed] [Google Scholar]
- 23.Breton JJ, Boyer R, Bilodeau H, et al. Is evaluative research on youth suicide programs theory-driven? The Canadian experience. Suicide Life Threat Behav. 2002;32(2):176–190. doi: 10.1521/suli.32.2.176.24397. [DOI] [PubMed] [Google Scholar]
- 24.Agence nationale d’accréditation et d’evaluation en santé (ANAES) Prise en charge hospitalière des adolescents après une tentative de suicide [Internet] Saint-Denis (FR): ANAES; 1998. Available from: http://www.has-sante.fr/portail/upload/docs/application/pdf/suicidecourt.pdf. [Google Scholar]
- 25.Labelle R, Breton JJ, Berthiaume C, et al. Psychometric properties of three measures of protective factors for depression and suicidal behaviour among adolescents. Can J Psychiatry. 2015;60(2 Suppl 1):S16–S26. [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients journal. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 28.Landry M, Trembaly J, Guyon L, et al. DEP-ADO Grille de dépistage de consommation problématique d’alcool et de drogues chez les adolescents et les adolescentes. Drogues, Santé et Sociétés. 2004;3(1):19–37. [Google Scholar]
- 29.Guilé JM, Greenfield B, Berthiaume C, et al. Reliability and diagnostic efficiency of the abbreviated-diagnostic interview for borderlines in an adolescent clinical population. Eur Child Adolesc Psychiatry. 2009;18(9):575–581. doi: 10.1007/s00787-009-0015-x. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg M. Society and adolescent self-image. Princeton (NJ): Princeton University Press; 1965. [Google Scholar]
- 31.Rigozzi C, Rossier J. Validation d’une version abrégée du TCI (TCI-56) sur un échantillon de jeunes fumeurs. Annales médicopsychologiques. 2004;162:541–548. [Google Scholar]
- 32.Delaney C. The Spirituality Scale: development and psychometric testing of a holistic instrument to assess the human spiritual dimension. J Holist Nurs. 2005;23(2):145–167. doi: 10.1177/0898010105276180. discussion 168–171. [DOI] [PubMed] [Google Scholar]
- 33.Osman A, Downs WR, Kopper BA, et al. The Reasons for Living Inventory for Adolescents (RFL-A): development and psychometric properties. J Clin Psychol. 1998;54(8):1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 34.Frydenberg E, Lewis R. The Adolescent Coping Scale. Melbourne (AU): Australian Council for Educational Research; 1993. [Google Scholar]
- 35.Leclerc D, Pronovost J, Dumont M. Echelle de coping pour adolescent : validation canadienne-française de l’Adolescent Coping Scale de Frydenberg et Lewis (1993) Revue québécoise de psychologie. 2009;30(1):177–196. [Google Scholar]
- 36.Newcomb MD, Huber GJ, Bentler PM. A multidimensional assessement of stressful life events among adolescents. J Health Social Behav. 1981;22:400–415. [Google Scholar]
- 37.R statistical package. The R project for statistical computing. Version 2.12.2 [Website]. Available from: http://www.r-project.org.
- 38.Pearl J. Causality: models, reasoning and inference. Cambridge (GB): Cambridge University Press; 2000. [Google Scholar]
- 39.Consoli A, Peyre H, Speranza M, et al. Suicidal behaviors in depressed adolescents: role of perceived relationships in the family. Child Adolesc Psychiatry Ment Health. 2013;7(1):8. doi: 10.1186/1753-2000-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.King CA, Merchant CR. Social and interpersonal factors relating to adolescent suicidality: a review of the literature. Arch Suicide Res. 2008;12(3):181–196. doi: 10.1080/13811110802101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seidowsky E, Deniau E, Brunelle J, et al. Une prévention des passages à l’acte hétéro-agressifs graves en milieu scolair est-elle possible? Etude de la littérature sur les tueries scolaires et discussion de deux observations cliniques. Neuropsychiatrie de l’enfance et de l’adolescence. 2011;59:393–403. [Google Scholar]
- 42.Shek DT. Spirituality as a positive youth development construct: a conceptual review. Scientific World Journal. 2012;458953 doi: 10.1100/2012/458953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koenig HG, McCullough ME, Larson DB. Handbook of religion and health. London (GB): Oxford University Press; 2001. [Google Scholar]
- 44.Yonker JE, Schnabelrauch CA, Dehaan LG. The relationship between spirituality and religiosity on psychological outcomes in adolescents and emerging adults: a meta-analytic review. J Adolesc. 2012;35(2):299–314. doi: 10.1016/j.adolescence.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 45.Jacobs M, Miller L, Wickramaratne P, et al. Family religion and psychopathology in children of depressed mothers: ten-year follow-up. J Affect Disord. 2012;136(3):320–327. doi: 10.1016/j.jad.2011.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Greenfield B, Henry M, Weiss M, et al. Previously suicidal adolescents: predictors of six-month outcome. J Can Acad Child Adolesc Psychiatry. 2008;17(4):197–201. [PMC free article] [PubMed] [Google Scholar]