Abstract
Objectives:
To examine whether protective factors in the Protection for Adolescent Depression Study (PADS) moderate the impact of stressful events on depression and suicidal behaviour in the community and a clinical setting; and to study the influence of sex.
Method:
Participants were 283 adolescents from the community and 119 from a mood disorder clinic in Montreal. The participants were evaluated on 6 instruments measuring individual risk and protective factors. Descriptive analyses and univariate and multiple logistic regression models were carried out.
Results:
Risk factors predicted higher levels of depression and presence of suicidal behaviour, and protective factors predicted lower levels of depression and absence of suicidal behaviour, as expected under the vulnerability-resilience stress model. Several sex differences were observed in terms of the predictive power of risk factors (for example, hopelessness among girls and keep to themselves among boys) and protective factors (for example, focusing on the positive among girls and self-discovery among boys).
Conclusions:
Findings from the PADS suggest that protective factors moderate the impact of stress on depression and suicidal behaviour. Developing protection appears important in the presence of chronic conditions, such as depressive disorders, to reduce the likelihood of further episodes. The influence of sex makes it all the more relevant to target different factors for boys and girls to increase protection and decrease risk in prevention and intervention programs.
Keywords: protective factors, risk factors, adolescence, influence of sex, resilience, vulnerability, depression, suicidal behaviour
Abstract
Objectifs :
Dans le cadre de l’étude de protection contre la dépression chez les adolescents (PADS), examiner si les facteurs de protection modèrent l’effet des événements stressants sur la dépression et les comportements suicidaires dans la communauté et dans un contexte clinique. Étudier l’influence du sexe, et discuter des implications cliniques.
Méthode :
Les participants étaient 283 adolescents de la communauté et 119 d’une clinique des troubles de l’humeur à Montréal qui ont été évalués à l’aide de 6 instruments de mesure du risque individuel et des facteurs de protection. Des analyses descriptives et univariées, et des modèles de régression logistiques ont été effectués.
Résultats :
Les facteurs de risque prédisaient des niveaux de dépression plus élevés et la présence de comportement suicidaire, tandis que les facteurs de protection prédisaient des niveaux de dépression plus faibles et l’absence de comportement suicidaire, tel que prévu par le modèle vulnérabilité-résilience-stress. Plusieurs différences selon le sexe ont été observées relativement à l’efficacité prédictive des facteurs de risque (par exemple, le désespoir chez les filles et l’introversion chez les garçons) et des facteurs de protection (par exemple, se centrer sur le positif chez les filles et la découverte de soi chez les garçons).
Conclusions :
Les résultats de la PADS suggèrent que les facteurs de protection modèrent l’effet du stress sur la dépression et le comportement suicidaire. Il semble important de développer la protection en présence d’affections chroniques, comme les troubles dépressifs, afin de réduire la probabilité d’épisodes ultérieurs. L’influence du sexe masculin justifie d’autant plus de cibler différents facteurs pour les garçons et les filles afin d’accroître la protection et de réduire le risque dans les programmes de prévention et d’intervention.
In 2009, the suicide rate in Canada among adolescents aged 15 to 19 years was 9.0 per 100 000, reaching 12.6 for boys and 5.2 for girls. In Quebec, the overall rate was 8.1 per 100 000, reaching 11.6 and 4.5 for boys and girls, respectively.1,2 The prevalence of suicidal ideation among adolescents in developed countries has been reported within the range of 15% to 25%, whereas lifetime estimates of attempted suicide have varied from 1.3% to 3.8% for males and from 1.5% to 10.1% for females.3
Suicide is a complex public health problem involving multiple biological, psychological, family, social, and cultural determinants.3,4 Individual determinants have the highest degree of association to suicidal behaviour, with mental disorders being in the front row. Uppermost among mental disorders are mood disorders,5 with rates reaching 58% and 60% in 2 recent psychological autopsy studies of adolescents.6,7 Numerous studies in community and clinical settings have revealed an association between depressive symptoms, suicidal ideation, and attempted suicide.8
The prevalence of MDD has been estimated at 3% to 8% in adolescence and its lifetime prevalence has been reported at 15% to 20%. The rate among girls is twice that among boys.9,10 Adolescents presenting a major depressive episode have 5 to 9 other episodes in their lifetime.11 Almost 50% of adolescents who suffer from a MDD relapse within the next 5 years12 and 75% of youths with pediatric BD (mean age of 11 years) suffer from an episode of mania within the next 8 years.13 Consequently, it is legitimate to take a clinical interest in protective factors regarding youths with chronic conditions of the sort, all the more so that such an interest is respectful of their developmental potential. Such a perspective also fosters a positive perception of the initial clinical evaluation.14 Though various groups have integrated risk and protective factors in the study of psychopathology, mechanisms and interrelations remain poorly understood.15–17
Clinical Implications
Protective factors moderate the impact of stress on depression and suicidal behaviour.
Restoring protection appears important in the presence of depression to reduce the likelihood of further episodes.
Focusing on the positive represents an interesting path to pursue to increase positive thoughts and decrease dysfunctional cognitions among adolescents who are depressed and suicidal.
Limitations
Results must be interpreted within the limits of a cross-sectional study.
Self-administered instruments were used and validity of some answers can be compromised by cognitive limitations of younger participants.
Depression was assessed as a continuous variable, whereas it is assessed as a categorical one in the DSM.
Against this background, the PADS was designed during the planning phase of a mood disorder clinic. Its objectives were 3-fold: to assess the psychometric qualities of 3 measures of protective factors against depression and suicidal behaviour18; to examine the diathesis-stress model regarding these protective factors; and to study the influence of sex. Our paper focuses on the second and third of these objectives.
Developmental Psychopathology
Bridging developmental psychology and psychopathology, clinical experience and research, multilevel assessments, and interventions constitute the principles of developmental psychopathology.16,17,19,20 The priority given to high-risk environments in pioneer studies explains the emphasis on risk factors. The Kauai longitudinal study21 of 658 high-risk children born in 1955 and followed from ages 1 to 32 years and other studies of the development of children of parents with schizophrenia22 are prime examples of these. Research on children in high-risk environments has found paradoxically that some youths are able to sustain a positive outcome and develop normally despite chronic adversity.23 Such research has awakened researchers and clinicians to the value of protective factors and resilience. Hence, a conceptual model in which protective factors and resilience are integrated in evaluation and treatment would seem relevant for child psychiatry teams. Such a conceptual model would also be influential in the formulation of research questions and the selection of variables.24,25
A Vulnerability–Resilience Stress Model for Mood Disorders
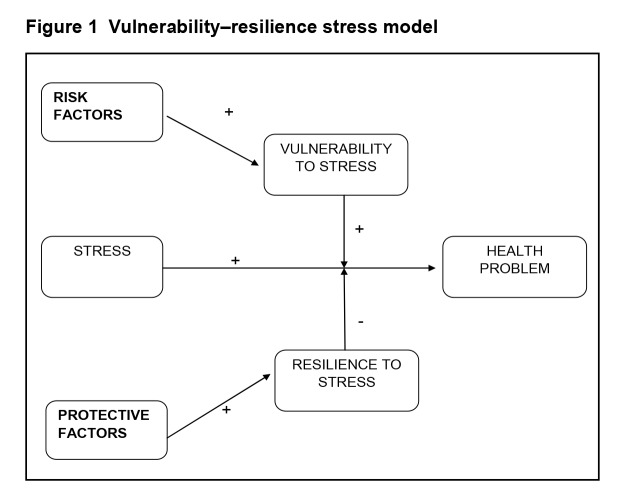
Protective and risk factors can be viewed as opposite views of the same concept. Both are factors related to stress levels, but the former have to do with resilience to stress and the latter with vulnerability to stress.15 Vulnerability influences a person’s response to stressful situations in a negative direction. Resilience, instead, influences a person’s response in a positive direction. Resilience can be defined as a dynamic process that gives rise to a positive adaptation despite an adverse experience.21,26,27 Resilience and vulnerability focus on individual features that moderate (interactive effect) the impact of stress or adversity on health outcomes. Recent findings from both animal and human studies indicate that high levels of stress can foster vulnerability whereas moderate levels can foster resilience by way of stress inoculation or a steeling effect.26,28
A vulnerability–resilience stress model based on principles of developmental psychopathology was chosen for the mood disorder clinic mentioned above. This model derives from the diathesis-stress model of depression29 and involves both resilience and vulnerability in the prediction of psychopathology. Depression results from the failure of individual adaptive mechanisms (high vulnerability and low resilience) to respond to SLEs or circumstances. Under this model, vulnerability and resilience act as moderator variables of the impact of a stressful situation (Figure 1).30,31
Figure 1.
Vulnerability–resilience stress model
In the PADS, the risk factors selected were recent SLEs for the situation at risk, as well as depression, hopelessness, and nonproductive coping for vulnerability. The protective factors were productive coping, reasons for living, and spirituality. These individual factors were selected for being proximal to suicidal behaviour, modifiable, and measurable. Protective factors against suicidal behaviour in adolescence include cognitive abilities; temperament; self-esteem; hopefulness; productive coping; defence mechanisms; self-control; spirituality and religion; reasons for living; positive attitude toward sports; caring by family, adults, and tribal leaders; parental involvement; family connectedness; school and neighbourhood safety; and pharmacotherapy (lithium for BD).32–35
Methods
Participants and Procedures
Community Sample
A convenience sample was drawn from 8 French-language secondary schools in Montreal. The size of the sample was based on the number of items subjected to factor analysis.36 The sample included 120 girls and 163 boys, of which 167 were 14 to 15 years old and 116 were 16 to 17 years old. Data collection took place from November 2006 to May 2007. The questionnaires were completed in small groups under the supervision of 2 research assistants. Consent was obtained from each adolescent and 1 parent. A procedure for providing help to youths at risk of suicidal gestures or attempts was devised and each adolescent was handed a list of resources. Approval was obtained from the research ethics committee of Rivière-des-Prairies Hospital.
Clinical Population
Adolescents were evaluated at the Mood Disorder Clinic, a specialized facility offering services at Rivière-des-Prairies Hospital to youths 6 to 17 years old with depressive disorders or BDs and associated suicidal behaviour. From 2005 to 2012, 78 girls and 41 boys 13 to 17 years old—of which 53 were 13 to 15 years old and 66 were 16 to 17 years old—were assessed. This group of 119 adolescents is smaller than in the psychometric study because only those who completed all questionnaires (risk and protection factors) were included. Adolescents and parents agreed to complete the questionnaires as part of a multidisciplinary assessment. Paper and pencil versions were used. Questions were asked by a psychologist, but some adolescents completed the questionnaires on their own with support, when needed. However, complex clinical presentations did not allow completion of all questionnaires.
Measures
Protective Factors
The ACS37 assesses specific behaviours used to deal with SLEs of daily life. It consists of 79 items (plus 1 open-ended question) that serve to rate 18 coping strategies representative of 3 coping styles: productive coping (for example, focus on solving the problem, work hard and achieve, and focus on the positive); nonproductive coping (for example, worry, tension reduction, ignore the problem, and keep to self), and reference to others (for example, seek social support and seek professional help). The RFL-A38 comprises 32 items concerning the beliefs that guide adolescents in their decision to live. The questionnaire encompasses 5 subscales: family alliance, suicide-related concerns, self-acceptance, peer acceptance and support, and future optimism. The SS39 is a 23-item self-report instrument. Four factors emerged in the PADS’s psychometric study18: spiritual beliefs, self-discovery, self-awareness and collective consciousness, and respect for others and environment.
Risk Factors
The Life Events Questionnaire40 is a 39-item instrument used to examine the past-year SLEs of adolescents aged 14 to 18 years old. The Beck Depression Inventory, Second Edition41 is a questionnaire used to assess depressive symptoms in the past 2 weeks. It comprises 21 items rated on a 4-point scale, making for a score range of 0 to 63 (0 to 13 for no depression). Item 9 was used to identify adolescents at low risk for suicide (thoughts of killing myself but would not do it) and those at high risk (would like to kill myself or would kill myself if I had a chance). The Beck Hopelessness Scale42,43 consists of 20 true or false items that serve to assess negative attitudes about the future. Its score range is 0 to 20.
Statistical Analyses
Descriptive analyses were carried out on recent unhappy events, risk and protective factors, and the following dependent variables: light-to-severe depression in the community, severe depression in the clinical population, suicidal ideation in the community, and suicidal intent in the clinical population. Data were analyzed using the SPSS software.44 Logistic regression models were used to predict depression and suicidal behaviour in adolescents from the community and from the clinical population. To target the moderator role of potential risk and protective factors specifically, we limited the datasets to youths with recent unhappy SLEs. This strategy was applied to avoid pitfalls associated with the modelling of interaction terms. In particular, multi-collinearity, loss of statistical power, and interpretation complexities tend to occur when multiple interaction terms share a common component. Univariate logistic models were first fit using each of the potential risk and protective factors as predictors. Sex differences were tested systematically. Afterwards, a final multiple logistic regression model was fit following a backward elimination strategy with a 0.05 significance level, starting with predictors reaching a more liberal 0.10 significance level in the univariate results. Goodness of fit was assessed for each multivariate model through the Hosmer-Lemeshow statistic.
Results
The sociodemographic characteristics of the participants are described in a companion paper.18 Among the 283 adolescents from the community, 70 (25%) were found to have light-to-severe depression and the other 213 (75%) had no depression. Among the 119 adolescents from the clinical population, 71 (60%) were found to have severe depression. In the community sample, 66 (23%) adolescents reported suicidal ideation and no one reported suicidal intent. In the clinical population, 46 (39%) adolescents reported suicidal intent, 60 (50%) reported suicidal ideation, and only 13 (11%) reported no suicidal behaviour. Finally, in the community sample, 239 (84.5%) adolescents experienced at least 1 recent SLE; all but 1 did in the clinical sample (118/119).
Univariate Analyses for Depression
Hopelessness proved a powerful risk factor in the community sample among girls. Nonproductive coping total score emerged as a powerful risk factor for being in the group with a higher level of light-to-severe depression in the community and in the group with severe depression in the clinical population (OR 4.7 and 5.2, respectively). Significant associations were observed, also, for the 8 nonproductive coping strategies in both the community and the clinical population (OR 1.5 to 3.8, respectively). Two nonproductive coping strategies, however, were significant only for girls, namely, self-blame in the community and tension reduction in the clinical population. Productive coping total score emerged as a significant predictor mainly for adolescents in the community with light-to-severe depression. The odds ratios were lower for productive coping strategies than for nonproductive coping strategies. Two productive coping strategies, namely, focusing on solving the problem and working hard to achieve, were found to be associated with higher odds of being in the group with a lower level of light-to-severe depression among girls in the community. Focusing on the positive proved a significant protective strategy for both girls and boys in the community (OR 2.6 and 1.5, respectively). RFL-A total score was a significant predictor of a lower level of depression in both community and clinical settings. The predictive power of family alliance, self-acceptance, and future optimism proved stronger for girls than for boys. Self-discovery from the SS emerged as a significant protective factor for girls and boys in the community but reached the significance level only for boys in the clinical population.
Multivariate Analyses for Depression
Hopelessness emerged as a powerful predictor of depression in the community sample, with the odds ratio much higher for girls than for boys. Indeed, the odds were 8 times as high of being in the group with a higher level of light-to-severe depression for girls who felt hopeless as for girls who felt hopeful. In the clinical population, the odds were 5 times as high of being in the severely depressed group for girls as for boys. Nonproductive coping strategies emerged as risk factors from the multivariate analyses and tension reduction proved predictive in the 2 multivariate models. Self-discovery was the only protective factor in the community. Suicide-related concerns (RFL-A subscale) and focusing on the positive were significant protective factors in the clinical population (Tables 1 and 2).
Table 1.
Univariate and multivariate logistic regression analyses predicting light-to-severe depression among youths with recent unhappy stressful life events (n = 239), community sample
| Analyses | OR | 95% CI | P |
|---|---|---|---|
| Univariatea | |||
| Risk factorsb | |||
| Hopelessness among boysc | 2.2 | 1.4 to 3.4 | <0.001 |
| Hopelessness among girlsc | 11.4 | 4.2 to 31.3 | <0.001 |
| Nonproductive coping—total scorec | 4.7 | 3.0 to 7.6 | <0.001 |
| Worry | 3.3 | 2.4 to 4.9 | <0.001 |
| Wishful thinking | 2.0 | 1.5 to 2.7 | <0.001 |
| Not coping | 2.6 | 1.9 to 3.7 | <0.001 |
| Tension reduction | 2.3 | 1.7 to 3.2 | <0.001 |
| Ignore the problem | 1.5 | 1.1 to 1.9 | 0.01 |
| Self-blame among girls | 3.1 | 1.9 to 5.0 | <0.001 |
| Keep to self | 2.8 | 2.0 to 4.0 | <0.001 |
| Seek to belong | 2.1 | 1.5 to 3.0 | <0.001 |
| Protective factorsd | |||
| Productive coping—total scorec | 2.1 | 1.2 to 2.1 | <0.001 |
| Focus on solving the problem among girls | 2.3 | 1.3 to 3.8 | 0.001 |
| Work hard and achieve among girls | 2.4 | 1.4 to 4.0 | <0.001 |
| Focus on the positive among boys | 1.5 | 0.9 to 2.3 | 0.09 |
| Focus on the positive among girls | 2.6 | 1.6 to 4.2 | <0.001 |
| Seek relaxing diversions | 1.5 | 1.1 to 2.0 | 0.006 |
| Physical recreation | 1.6 | 1.2 to 2.1 | 0.001 |
| Coping reference to othersc | |||
| Seek social support | 1.4 | 1.1 to 1.9 | 0.02 |
| Reasons for living (total score)—boysc | 1.4 | 1.0 to 2.1 | 0.05 |
| Reasons for living (total score)—girlsc | 3.3 | 1.9 to 5.7 | <0.001 |
| Family alliance among boys | 1.4 | 1.0 to 2.1 | 0.06 |
| Family alliance among girls | 3.3 | 1.9 to 5.7 | <0.001 |
| Suicide-related concerns | 1.3 | 1.0 to 1.7 | 0.07 |
| Self-acceptance among girls | 3.3 | 1.9 to 5.7 | <0.001 |
| Peer acceptance and support | 1.7 | 1.3 to 2.3 | <0.001 |
| Future optimism among girls | 2.4 | 1.4 to 3.9 | <0.001 |
| Spirituality Scalec | |||
| Self-discovery | 2.5 | 1.8 to 3.5 | <0.001 |
| Multivariate | |||
| Hopelessness among boysc | 1.7 | 1.0 to 2.9 | 0.05 |
| Hopelessness among girlsc | 8.6 | 2.9 to 25.7 | <0.001 |
| Worry | 2.5 | 1.5 to 4.0 | <0.001 |
| Tension reduction | 2.2 | 1.4 to 3.4 | <0.001 |
| Self-discovery | 2.0 | 1.3 to 3.2 | 0.002 |
Hosmer-Lemeshow test, χ2 = 4.86; df = 8, P = 0.770
Only significant univariate results are presented (P < 0.10).
Odds ratios are based on an increase of 1 standard deviation of the dimensional variable.
Indicates scales or subscales
Odds ratios are based on a decrease of 1 standard deviation of the dimensional variable.
Table 2.
Univariate and multivariate logistic regression analyses predicting severe depression among youths with recent unhappy stressful life events (n = 118), clinical population
| Analyses | OR | 95% CI | P |
|---|---|---|---|
| Univariatea | |||
| Risk factorsb | |||
| Hopelessnessc | 2.8 | 1.8 to 4.4 | <0.001 |
| Nonproductive coping—total scorec | 5.2 | 2.7 to 9.2 | 0.002 |
| Worry | 2.4 | 1.5 to 3.8 | <0.001 |
| Wishful thinking | 1.6 | 1.1 to 2.4 | 0.01 |
| Not coping | 2.8 | 1.7 to 4.5 | <0.001 |
| Tension reduction among girls | 3.0 | 1.5 to 6.0 | <0.001 |
| Ignore the problem | 1.6 | 1.1 to 2.4 | 0.01 |
| Self-blame | 3.7 | 2.2 to 6.3 | <0.001 |
| Keep to self | 2.7 | 1.7 to 4.3 | <0.001 |
| Seek to belong | 2.9 | 1.8 to 4.7 | <0.001 |
| Protective factorsd | |||
| Productive coping—total scorec | 1.4 | 1.0 to 2.0 | 0.08 |
| Focus on the positive | 2.0 | 1.3 to 3.0 | 0.001 |
| Seek relaxing diversions among boys | 2.3 | 1.2 to 4.6 | 0.01 |
| Reasons for living (total score)c | 2.1 | 1.4 to 3.3 | <0.001 |
| Family alliance | 1.5 | 1.2 to 2.6 | 0.04 |
| Suicide-related concerns | 1.8 | 1.2 to 2.9 | 0.002 |
| Self-acceptance | 2.1 | 1.4 to 3.3 | <0.001 |
| Future optimism | 1.8 | 1.2 to 2.7 | 0.003 |
| Spirituality Scalec | |||
| Self-discovery among boys | 4.0 | 1.4 to 11.4 | 0.001 |
| Multivariate | |||
| Sex (girls, compared with boys)c | 5.0 | 1.4 to 18.5 | 0.01 |
| Tension reduction | 2.0 | 1.0 to 3.9 | 0.04 |
| Self-blame | 2.1 | 1.0 to 4.0 | 0.004 |
| Seek to belong | 2.7 | 1.3 to 5.5 | 0.03 |
| Focus on the positive | 2.4 | 1.3 to 4.5 | 0.002 |
| Suicide-related concerns | 2.5 | 1.4 to 4.7 | 0.001 |
Hosmer-Lemeshow test, χ2 = 12.044, df = 8, P = 0.149.
Only significant univariate results are presented (P < 0.10)
Odds ratios are based on an increase of 1 standard deviation of the dimensional variable.
Indicates scales or subscales
Odds ratios are based on a decrease of 1 standard deviation of the dimensional variable.
Univariate Analyses for Suicidal Behaviour
Depression and hopelessness were predictors of suicidal ideation in the community and suicidal intent in the clinical population. Nonproductive coping strategies were predictive of suicidal ideation in the community and of suicidal intent in the clinical population. Boys who keep to themselves were 6 times as likely of showing suicidal intent in the clinical population as those who did not. Productive coping strategies proved protective factors against suicidal ideation in the community but none reached the significance level in the clinical population. Physical recreation was a significant protective factor among boys but not among girls in the community. Social action stemming from coping reference to others was a predictive risk factor instead of a protective factor in the clinical population. The 5 reasons for living emerged as protective factors in both the community and the clinical population but the odds ratios were lower in the latter. Peer acceptance and support exerted greater protective power among boys than among girls in the clinical population (OR 4, compared with 1.4, respectively). Self-discovery was a significant protective factor in both the community and the clinical population, with a much higher odds ratio for boys than for girls in the clinical population.
Multivariate Analyses for Suicidal Behaviour
Only depression emerged as a significant risk factor for suicidal ideation in the community. In the clinical population, depression and keep to self were significant risk factors for suicidal intent among boys while respect for others and environment (the SS) and suicide-related concerns turned out to be protective factors (Tables 3 and 4).
Table 3.
Univariate and multivariate logistic regression analyses predicting suicide ideation among youths with recent unhappy stressful life events (n = 239), community sample
| Analyses | OR | 95% CI | P |
|---|---|---|---|
| Univariatea | |||
| Risk factorsb | |||
| Depressionc | 3.4 | 2.4 to 4.9 | <0.001 |
| Hopelessnessc | 1.8 | 1.3 to 2.3 | <0.001 |
| Nonproductive coping—total scorec | 2.4 | 1.7 to 3.4 | <0.001 |
| Worry | 1.8 | 1.3 to 2.5 | <0.001 |
| Wishful thinking | 1.4 | 1.0 to 1.8 | <0.001 |
| Not coping | 2.0 | 1.5 to 2.7 | <0.001 |
| Tension reduction | 1.7 | 1.3 to 2.4 | <0.001 |
| Self-blame | 2.2 | 1.6 to 3.0 | <0.001 |
| Keep to self | 2.0 | 1.4 to 2.7 | <0.001 |
| Seek to belong | 1.7 | 1.3 to 2.4 | <0.001 |
| Protective factorsd | |||
| Productive coping—total scorec | 1.6 | 1.2 to 2.1 | 0.002 |
| Focus on the positive | 1.9 | 1.4 to 2.6 | <0.001 |
| Seek relaxing diversions | 1.3 | 1.0 to 1.7 | 0.087 |
| Physical recreation among boys | 1.6 | 1.1 to 2.6 | 0.025 |
| Reasons for living (total score)c | 1.5 | 1.1 to 2.0 | 0.003 |
| Family alliance | 1.4 | 1.0 to 1.8 | 0.025 |
| Suicide-related concerns | 1.3 | 1.0 to 1.7 | 0.073 |
| Self-acceptance | 1.5 | 1.1 to 2.0 | 0.003 |
| Peer acceptance and support | 1.4 | 1.0 to 1.8 | 0.022 |
| Future optimism | 1.3 | 1.0 to 1.7 | 0.057 |
| Spirituality Scalec | |||
| Self-discovery | 1.5 | 1.4 to 2.0 | 0.003 |
| Multivariate | |||
| Depressionc | 3.4 | 2.4 to 4.9 | <0.001 |
Hosmer-Lemeshow test χ2 = 8.696, df = 8, P = 0.369.
Only significant univariate results are presented (P < 0.10)
Odds ratios are based on an increase of 1 standard deviation of the dimensional variable.
Indicates scales or subscales
Odds ratios are based on a decrease of 1 standard deviation of the dimensional variable.
Table 4.
Univariate and multivariate logistic regression analyses predicting suicidal intent among youths with recent unhappy stressful life events (n = 118), clinical population
| Analyses | OR | 95% CI | P |
|---|---|---|---|
| Univariatea | |||
| Risk factorsb | |||
| Depressionc | 3.7 | 2.1 to 6.6 | <0.001 |
| Hopelessnessc | 2.2 | 1.4 to 3.5 | <0.001 |
| Nonproductive coping—total scorec | 1.9 | 1.2 to 2.9 | 0.002 |
| Worry | 1.5 | 1.0 to 2.2 | 0.06 |
| Not coping | 1.8 | 1.2 to 2.6 | 0.004 |
| Self-blame | 2.0 | 1.3 to 3.0 | 0.001 |
| Keep to self among boys | 5.6 | 1.7 to 18.2 | <0.001 |
| Keep to self among girls | 1.7 | 1.0 to 2.9 | 0.03 |
| Protective factorsd | |||
| Coping reference to othersc | |||
| Social action | 0.7 | 0.5 to 1.0 | 0.03 |
| Reasons for living (total score)c | 2.1 | 1.4 to 3.3 | <0.001 |
| Family alliance | 1.8 | 1.2 to 2.6 | 0.003 |
| Suicide-related concerns | 1.9 | 1.2 to 2.9 | 0.001 |
| Self-acceptance | 1.7 | 1.1 to 2.5 | 0.007 |
| Peer acceptance and support boys | 4.0 | 1.4 to 11.1 | 0.002 |
| Peer acceptance and support girls | 1.4 | 0.9 to 2.2 | 0.10 |
| Future optimism | 1.6 | 1.1 to 2.3 | 0.02 |
| Spirituality Scale (total score)c | 1.5 | 1.0 to 2.2 | 0.06 |
| Self-discovery among boys | 5.2 | 1.4 to 18.6 | 0.001 |
| Self-discovery among girls | 1.5 | 0.9 to 2.4 | 0.09 |
| Respect for others and environment | 1.4 | 0.9 to 2.0 | 0.10 |
| Multivariate | |||
| Depressionc | 4.0 | 2.0 to 7.7 | <0.001 |
| Keep to self among boys | 4.3 | 1.2 to 15.3 | 0.01 |
| Respect for others and environment | 1.7 | 1.1 to 2.8 | 0.02 |
| Suicide-related concerns | 1.7 | 1.0 to 2.8 | 0.03 |
Hosmer-Lemeshow test χ2 = 2.7144; df = 8, P = 0.951
Only significant univariate results are presented (P < 0.10)
Odds ratios are based on an increase of 1 standard deviation of the dimensional variable.
Indicates scales or subscales
Odds ratios are based on a decrease of 1 standard deviation of the dimensional variable.
Discussion
The PADS presents 3 main limitations. First, results must be interpreted within the limits of a cross-sectional study involving a large number of variables, instruments, and statistical tests with types I and II statistical errors. Second, the validity of the responses to the self-administered instruments could be undermined by the cognitive limitations of the study’s younger participants. Third, depression was assessed as a continuous variable, whereas it is treated categorically in the DSM. Our study’s strength lies in the original data collected rigorously in both community and clinical settings using validated measures.18 Our study provides support for the vulnerability–resilience stress model of depression and suicidal behaviour and clinical implications are presented.
The odds ratios of the risk factors for depression and suicidal behaviour proved higher than those for the protective factors. Such a result was expected and confirms the relevance of interventions targeting risk factors in schools and clinical settings.45,46 We should not conclude, however, that developing protective factors among youths who were depressed or suicidal is not important. Empirical studies have shown that risk factors accumulate over the years and are predictive of suicidal behaviour in youth47 and of depressiveness in adult life.48 If protective factors counterbalance the impact of vulnerability, developing such factors should lessen negative outcomes. However, it has yet to be established that doing so among adolescents who were depressed or suicidal leads to more positive outcomes over time. Only a randomized controlled study with an experimental group and a control group of participants treated as usual could shed light on the matter.
In the univariate analyses, nonproductive coping total score proved a more powerful risk factor for light-to-severe depression and severe depression than for suicidal ideation and suicidal intent (OR 4.7 and 5.2, compared with 2.4 and 1.9, respectively). Moreover, some nonproductive coping strategies were predictive of higher levels of light-to-severe and severe depression in the multivariate models. Nonproductive coping strategies were found to be predictive of intensity of depression in a comparable study in France as well.49 Depression, for its part, has been shown in other studies7,8 to be a powerful predictive factor for suicidal behaviour. The PADS findings are in line with this, as depression proved the only predictive risk factor for suicidal ideation and a significant risk factor for suicidal intent in the multivariate models. In short, targeting nonproductive coping strategies in prevention and intervention programs could be beneficial with respect to both depression and suicidal behaviour.
Only 2 productive coping strategies were shown to have a protective effect on severe depression in the univariate analyses and none demonstrated a protective effect on suicidal intent. Is this because adolescents who are severely depressed and those with suicidal intent make use of fewer productive strategies to begin with or because the influence of pre-existing productive strategies decreases over time as nonproductive ones accumulate? Both hypotheses could be true. Indeed, children living in high-risk environments have fewer protective factors at birth21 and studies of cumulative models of risk factors for depression and suicidal behaviour suggest the second hypothesis is plausible.47,48 This result underscores the relevance of fostering productive coping strategies among youths with depression and suicidal ideation as these strategies seem absent when depression intensifies and suicidal intent occurs.
One productive coping strategy, namely, focusing on the positive, emerged from the multivariate analysis as a significant protective factor against severe depression (OR 2.4). The same was noted in a study by Mirkovic et al.49 Interestingly, self-blame emerged as a significant nonproductive coping strategy in the PADS multivariate model. Self-blame can be considered as the flipside of focusing on the positive, a concept similar to positive thoughts in the field of positive psychology and psychotherapy of depression.50,51 Previous studies of girls who were depressed have reported findings along the same line.52 Findings in both Quebec and France call into question the emphasis placed on dysfunctional cognitions as risk factors in the treatment of youths with depression if positive thoughts are not fostered as a protective strategy as well.
Another productive coping coping strategy, working hard to achieve, proved protective only for girls in the univariate analyses for light-to-severe depression. It proved the only protective factor in the structural equation modelling of suicidality in a 6-month follow-up study of suicidal adolescents by our colleagues in this supplement.53 Hopelessness among girls in the community emerged from the multivariate analysis as a strong predictive risk factor for light-to-severe depression. Hopelessness is the feeling that nothing will turn out well. Interestingly, girls who focused on the positive were more protected than boys against light-to-severe depression. These differences confirm the influence of sex on coping with depressive feelings. Girls attribute greater importance to their negative thoughts than boys do.52,54 Hence, a thorough, assessment of negative thoughts should be a key step in planning interventions with depressed girls.
Boys who keep to themselves were 6 times as likely to report suicidal intent as boys who did not use this nonproductive coping strategy. This finding is important in light of the higher suicide rates among boys, as it confirms that boys are less inclined than girls to seek help.55 It is true that most youths with suicidal thoughts do not seek professional help,56 but our results confirm that sex should be taken into account when targeting barriers to consultation in prevention and intervention programs.
Recent reviews57,58 have confirmed the overall positive effects of religion and spirituality on psychological outcomes among youths, although some negative results have been reported as well. Self-discovery from the SS emerged from the multivariate analysis as a significant protective factor against light-to-severe depression. Salience of beliefs (identity, connectedness, spiritual well-being, and motivation) had the strongest inverse relation to depression in the meta-analysis by Yonker et al.58 Self-discovery appears related to salience of beliefs as it concerns positive meaning of experiences, relationships, and the ability to receive love. This might explain its protective effect on depression. Our results need to be compared with those of our colleagues in this supplement.53 In their study, seeking spiritual support (ACS) and higher self-transcendence scores (Temperament and Character Inventory) proved risk factors for suicidality. As suggested, self-transcendence might reflect a desperate quest for answers to overcome suffering when undertaken by very disturbed adolescents. Spirituality could at times be a search aimed at alleviating the burden of illness.59 Spirituality implies multiple subjective dimensions60 and the relevance of some dimensions, such as self-transcendence, must be interpreted with caution in the case of suicidal adolescents.
Studies have established that reasons for living are protective factors against suicidal behaviour.14,61 Only suicide-related concerns (fear of death or of killing oneself), however, emerged as a protective factor against severe depression and suicidal intent. Suicide-related concerns were a central protective factor in the original validation of the RFL-A.62 Promoting fear of death would be ethically questionable, but encouraging the use of media guidelines when reporting on suicide seems an effective strategy for reducing imitative suicide.63
Conclusions
The PADS findings suggest that protective factors do moderate the impact of stress on depression and suicidal behaviour. Productive coping strategies are nearly absent and nonproductive coping strategies were omnipresent when severe depression and suicidal intent occur. It is not surprising that child psychiatry professionals who assess and treat such troubled adolescents become overwhelmed by risk factors and are less inclined to consider protective factors. Cumulative models of risk factors for depression and suicidal behaviour, however, do exist. Restoring protection appears important in the presence of chronic conditions to decrease the probability of further episodes. Results regarding focusing on the positive represent an interesting path to pursue to prevent further episodes by increasing positive thoughts and decreasing dysfunctional cognitions. Finally, the influence of sex on protection and risk factors makes it all the more relevant to target different factors for girls and boys in prevention and intervention programs.
Acknowledgments
We thank Dr Silvia de Armas for her contribution to data collection and all the adolescents and their families who participated in the study. A grant was awarded to Dr Breton, Prof Labelle, and Prof Royer by the Canadian Institutes of Health Research (Gender and Health Grant No 79775) for completion of the study in the community.
None of the authors have any financial or personal conflict of interest.
Abbreviations
- ACS
Adolescent Coping Scale
- BD
bipolar disorder
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- MDD
major depressive disorder
- PADS
Protection for Adolescent Depression Study
- RFL-A
Reasons for Living Inventory for Adolescents
- SLE
stressful life event
- SS
Spirituality Scale
References
- 1.Légaré G, Gagné M, St-Laurent D, et al. Mise à jour 2013. Institut national de la santé publique et Bureau du coroner. Montreal (QC): Gouvernement du Québec; 2013. La mortalité par suicide au Québec: 1981–2010. [Google Scholar]
- 2.Statistics Canada, Government of Canada . Suicides et taux de suicide selon le sexe et l’âge [Internet] Ottawa (ON): Statistics Canada; 2014. [cited 2013 Jul 4] Available from: http://www.statcan.gc.ca/tables-tableaux/sum-som/102/cst01/hlth66a-fra.htm. [Google Scholar]
- 3.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 4.Consoli A, Peyre H, Speranza M, et al. Suicidal behaviors in depressed adolescents: role of perceived relationships in the family. Child Adolesc Psychiatry Ment Health. 2013;7(1):8. doi: 10.1186/1753-2000-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaffer D, Gould MS, Fisher P, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53(4):339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- 6.Portzky G, Audenaert K, van Heeringen K. Suicide among adolescents: a psychological autopsy study of psychiatric, psychosocial and personality-related risk factors. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):922–930. doi: 10.1007/s00127-005-0977-x. [DOI] [PubMed] [Google Scholar]
- 7.Renaud J, Berlim MT, McGirr A, et al. Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: a case–control study. J Affect Disord. 2008;105(1–3):221–228. doi: 10.1016/j.jad.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 8.Labelle R, Breton JJ, Pouliot L, et al. Cognitive correlates of serious suicidal ideation in a community sample of adolescents. J Affect Disord. 2013;145(3):370–377. doi: 10.1016/j.jad.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 9.Birmaher B, Ryan ND, Williamson DE, et al. Childhood and adolescent depression: a review of the past 10 years. Part II. J Am Acad Child Adolesc Psychiatry. 1996;35(12):1575–1583. doi: 10.1097/00004583-199612000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Zalsman G, Brent DA, Weersing VR. Depressive disorders in childhood and adolescence: an overview: epidemiology, clinical manifestation and risk factors. Child Adolesc Psychiatr Clin N Am. 2006;15(4):827–841. doi: 10.1016/j.chc.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27(8):959–985. doi: 10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao U, Hammen CL, Poland RE. Longitudinal course of adolescent depression: neuroendocrine and psychosocial predictors. J Am Acad Child Adolesc Psychiatry. 2010;49(2):141–151. doi: 10.1097/00004583-201002000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geller B, Tillman R, Bolhofner K, et al. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65(10):1125–1133. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gutierrez PM, Osman A. Adolescent suicide: an integrated approach to the assessment of risk and protective factors. DeKalb (IL): Northern Illinois University Press; 2008. [Google Scholar]
- 15.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry. 1987;57(3):316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 16.Masten AS. Developmental psychopathology: pathways to the future. Int J Behav Dev. 2004;30(1):47–54. [Google Scholar]
- 17.Toth SL, Cicchetti D. The historical origins and developmental pathways of the discipline of developmental psychopathology. Isr J Psychiatry Relat Sci. 2010;47(2):95–104. [PubMed] [Google Scholar]
- 18.Labelle R, Breton JJ, Berthiaume C, et al. Psychometic properties of three measures of protective factors for depression and suicidal behavior among adolescents. Can J Psychiatry. 2015;60(2 Suppl 1):S16–S26. [PMC free article] [PubMed] [Google Scholar]
- 19.Sroufe AL, Rutter M. The domain of developmental psychopathology. Child Dev. 1984;55:1184–1199. [PubMed] [Google Scholar]
- 20.Sameroff AJ, Chandler MJ. Reproductive risk and the continuum of caretaking casualty. In: Horowitz FD, Hetherington M, Scarr-Salapalck S, et al., editors. Review of child development research. Vol. 4. Chicago (IL): Chicago University Press; 1975. pp. 187–244. [Google Scholar]
- 21.Werner EE. Vulnerable but invincible: high-risk children from birth to adulthood. Acta Paediatr Suppl. 1997;422:103–105. doi: 10.1111/j.1651-2227.1997.tb18356.x. [DOI] [PubMed] [Google Scholar]
- 22.Sameroff A, Seifer R, Zax M, et al. Early indicators of developmental risk: Rochester Longitudinal Study. Schizophr Bull. 1987;13(3):383–394. doi: 10.1093/schbul/13.3.383. [DOI] [PubMed] [Google Scholar]
- 23.Richters J, Weintraub S. Beyond diathesis: toward an understanding of high-risk environments. In: Rolf J, Masten AS, Cicchetti D, et al., editors. Risk and protective factors in the development of psychopathology. Cambridge (GB): Cambridge University Press; 1990. pp. 67–96. [Google Scholar]
- 24.Breton JJ, Boyer R, Bilodeau H, et al. Is evaluative research on youth suicide programs theory-driven? The Canadian experience. Suicide Life Threat Behav. 2002;32(2):176–190. doi: 10.1521/suli.32.2.176.24397. [DOI] [PubMed] [Google Scholar]
- 25.Sroufe AL. Psychopathology as an outcome of development. Dev Psychopathol. 1997;9:251–268. doi: 10.1017/s0954579497002046. [DOI] [PubMed] [Google Scholar]
- 26.Kim-Cohen J, Turkewitz R. Resilience and measured gene-environment interactions. Dev Psychopathol. 2012;24(4):1297–1306. doi: 10.1017/S0954579412000715. [DOI] [PubMed] [Google Scholar]
- 27.Ionescu S, Blanchet A. Psychologie clinique, psychopathologie et psychothérapie. Paris (FR): Presses Universitaires de France; 2006. [Google Scholar]
- 28.Rutter M. Resilience as a dynamic concept. Dev Psychopathol. 2012;24(2):335–344. doi: 10.1017/S0954579412000028. [DOI] [PubMed] [Google Scholar]
- 29.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 30.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 31.Kraemer HC, Stice E, Kazdin A, et al. How do risk factors work together? Mediators, moderators and independent, overlapping and proxy risk factors. Am J Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 32.Beautrais AL, Collings SCD, Ehrhardt P, et al. Suicide prevention: a review of evidence of risk and protective factors and points of effective intervention. Wellington (NZ): Ministry of Health; 2005. [Google Scholar]
- 33.Breton JJ. Suicide in adolescents: toward a model including risk and protective factors. Oral presentation at: International Association of Child and Adolescent Psychiatry and Allied Professions; 2012 July 21 25; Paris (FR). [Google Scholar]
- 34.Halfon N, Labelle R, Cohen D, et al. Juvenile bipolar disorder and suicidality: a review of the last ten years of literature. Eur Child Adolesc Psychiatr. 2012;22(3):139–151. doi: 10.1007/s00787-012-0328-z. [DOI] [PubMed] [Google Scholar]
- 35.Knafo A, Mirkovic B, Belloncle V, et al. L’énigme du suicide à l’adolescence. Paris (FR): Bibliothèque Sigmund Freud; 2012. Nouveaux regards sur l’évaluation du risque suicidaire à l’adolescence: les facteurs de protection; pp. 71–99. [Google Scholar]
- 36.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. London (GB): Pearson Education Inc; 2007. [Google Scholar]
- 37.Frydenberg E, Lewis R. The Adolescent Coping Scale, administrator’s manual. Melbourne (AU): The Australian Council for Education Research; 1993. [Google Scholar]
- 38.Osman A, Downs WR, Kopper BA, et al. The reasons for living inventory for adolescents (RFL-A): development and psychometric properties. J Clin Psychol. 1998;54(8):1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 39.Delaney C. The Spirituality Scale: development and psychometric testing of a holistic instrument to assess the human spiritual dimension. J Holist Nurs. 2005;23(2):145–167. doi: 10.1177/0898010105276180. [DOI] [PubMed] [Google Scholar]
- 40.Newcomb MD, Huba GJ, Bentler PM. A multidimensional assessment of stressful life events among adolescents: derivation and correlates. J Health Soc Behav. 1981;22:400–415. [Google Scholar]
- 41.Beck AT, Steer R, Brown GK. Manual of the BDI-II. San Antonio (TX): The Psychological Corporation; 1994. [Google Scholar]
- 42.Beck AT, Weissman A, Lester D, et al. The measurement of pessimism: the Hopelessness Scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 43.Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio (TX): Psychological Corporation; 1996. [Google Scholar]
- 44.IBM Corporation . IBM SPSS statistics for Windows. Armonk (NY): IBM Corporation; 2012. version 21.0. [Google Scholar]
- 45.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pössel P, Martin NC, Garber J, et al. A randomized controlled trial of a cognitive-behavioral program for the prevention of depression in adolescents compared with nonspecific and no-intervention control conditions. J Couns Psychol. 2013;60(3):432–438. doi: 10.1037/a0032308. [DOI] [PubMed] [Google Scholar]
- 47.Fergusson DM, Beautrais AL, Horwood LJ. Vulnerability and resiliency to suicidal behaviours in young people. Psychol Med. 2003;33(1):61–73. doi: 10.1017/s0033291702006748. [DOI] [PubMed] [Google Scholar]
- 48.Korkeila K, Korkeila J, Vahtera J, et al. Childhood adversities, adult risk factors and depressiveness: a population study. Soc Psychiatry Psychiatr Epidemiol. 2005;40(9):700–706. doi: 10.1007/s00127-005-0969-x. [DOI] [PubMed] [Google Scholar]
- 49.Mirkovic B, Labelle R, Guilé JM, et al. Coping skills among adolescent suicide attempters: results of a multisite study. Can J Psychiatry. 2015;60(2 Suppl 2):S37–S45. [PMC free article] [PubMed] [Google Scholar]
- 50.Kobau R, Seligman MEP, Peterson C, et al. Mental health promotion in public health: perspectives and strategies from positive psychology. Am J Public Health. 2011;101(8):e1–e9. doi: 10.2105/AJPH.2010.300083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seligman ME, Rashid T, Parks AC. Positive psychotherapy. Am Psychol. 2006;61(8):774–788. doi: 10.1037/0003-066X.61.8.774. [DOI] [PubMed] [Google Scholar]
- 52.Nolen-Hoeksema S, Stice E, Wade E, et al. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. J Abnorm Psychol. 2007;116(1):198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- 53.Consoli A, Cohen D, Bodeau N, et al. Risk and protective factors for suicidality at 6-month follow-up in adolescent inpatients who attempted suicide: an exploratory model. Can J Psychiatry. 2015;60(2 Suppl 2):S27–S36. [PMC free article] [PubMed] [Google Scholar]
- 54.Nolen-Hoeksema S. Emotion regulation and psychopathology: the role of gender. Annu Rev Clin Psychol. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. Epub 2011 Oct 24. [DOI] [PubMed] [Google Scholar]
- 55.Mariu KR, Merry SN, Robinson EM, et al. Seeking professional help for mental health problems among New Zealand secondary school students. Clin Child Psychol Psychiatry. 2012;17(2):284–297. doi: 10.1177/1359104511404176. [DOI] [PubMed] [Google Scholar]
- 56.Michelmore L, Hindley P. Help-seeking for suicidal thoughts and self-harm in young people: a systematic review. Suicide Life Threat Behav. 2012;42(5):507–524. doi: 10.1111/j.1943-278X.2012.00108.x. [DOI] [PubMed] [Google Scholar]
- 57.King PE, Carr D, Boitor C. Religion, spirituality, positive youth development, and thriving. Adv Child Dev Behav. 2011;41:161–195. doi: 10.1016/b978-0-12-386492-5.00007-5. [DOI] [PubMed] [Google Scholar]
- 58.Yonker JE, Schnabelrauch CA, Dehaan LG. The relationship between spirituality and religiosity on psychological outcomes in adolescents and emerging adults: a meta-analytic review. J Adolesc. 2012;35(2):299–314. doi: 10.1016/j.adolescence.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 59.Baetz M, Bowen R, Jones G, et al. How spiritual values and worship attendance relate to psychiatric disorders in the Canadian population. Can J Psychiatry. 2006;51(10):654–661. doi: 10.1177/070674370605101005. [DOI] [PubMed] [Google Scholar]
- 60.Royer C, Pronovost G, Charbonneau S. Valeurs sociales fondamentales de jeunes québécoises et québécois : ce qui compte pour eux. In: Pronovost G, Royer C, editors. Les valeurs des jeunes. Quebec City (QC): Presses de l’Université du Québec;; 2004. pp. 49–69. [Google Scholar]
- 61.Goldston DB, Daniel SS, Reboussin BA, et al. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study. J Am Acad Child Adolesc Psychiatry. 2001;40(1):91–99. doi: 10.1097/00004583-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 62.Gutierrez PM, Osman A, Kopper BA, et al. Why young people do not kill themselves: the reasons for living inventory for adolescents. J Clin Child Psychol. 2000;29(2):177–187. doi: 10.1207/S15374424jccp2902_4. [DOI] [PubMed] [Google Scholar]
- 63.Bohanna I, Wang X. Media guidelines for the responsible reporting of suicide: a review of effectiveness. Crisis. 2012;33(4):190–198. doi: 10.1027/0227-5910/a000137. [DOI] [PubMed] [Google Scholar]