Abstract
Background
Patients with coronary heart disease are recommended to use statins following hospital discharge. Acute myocardial infarction (AMI) is a common complication of hospitalization, but the use of statins following discharge among patients who were not initially hospitalized for AMI has not been assessed adequately.
Methods and Results
Using the Medicare 5% national random sample, we determined statin use among beneficiaries who were hospitalized and who had a secondary discharge diagnosis of AMI and among beneficiaries who had a primary discharge diagnosis of AMI, coronary artery bypass grafting, or percutaneous coronary intervention in 2007–2009. Statin use was defined by a pharmacy (Medicare Part D) claim within 90 days following discharge. Of 8175 Medicare beneficiaries who did not take statins prior to hospitalization, 31.2% with AMI as a secondary discharge diagnosis, 60.5% with AMI as the primary discharge diagnosis, 67.6% with coronary artery bypass grafting, and 63.9% with a percutaneous coronary intervention initiated statins. After multivariable adjustment, the risk ratio for statin initiation comparing beneficiaries with a secondary versus primary discharge diagnosis of AMI was 0.59 (95% CI 0.54 to 0.65). Among 5468 Medicare beneficiaries taking statins prior to hospitalization, statin use following discharge was lower for those with AMI as a secondary discharge diagnosis (71.8%) compared with their counterparts with AMI, coronary artery bypass grafting, and percutaneous coronary intervention (84.1%, 83.8%, and 87.3%, respectively) as the primary discharge diagnosis.
Conclusion
Medicare beneficiaries with a secondary hospital discharge diagnosis of AMI were less likely to fill statins compared with those with other coronary heart disease events.
Keywords: atherosclerosis, hospitalization, Medicare, myocardial infarction, statins
Introduction
Registries and other observational studies suggest that >80% of patients are discharged on a statin following hospitalization for a coronary heart disease (CHD) event1–2; however, most data on prescriptions for statins following CHD events are derived from patients whose primary reason for hospitalization was acute myocardial infarction (AMI) or coronary revascularization (coronary artery bypass grafting [CABG] or percutaneous coronary intervention [PCI]).3 For many hospitalizations, AMI is listed as a secondary diagnosis.4 American Heart Association (AHA) and American College of Cardiology Foundation (ACCF) guidelines recommend statins for secondary prevention for patients with AMI who do not have contraindications or documented adverse effects from statins.5–7 The guidelines do not address the issue of whether secondary prevention treatment should differ based on the precipitating cause of AMI. Patients who have an AMI during a hospitalization for another reason may have multiple competing priorities on discharge, and the provision of cardioprotective treatment may be overlooked.
The purpose of this study was to determine the proportion of patients with AMI during a hospitalization for another reason who filled a statin prescription following discharge. For our primary analyses, we assessed the proportion of Medicare beneficiaries who initiated statins within 90 days following discharge for a hospitalization with AMI as a secondary diagnosis compared with their counterparts with AMI as the primary listed diagnosis or those who underwent coronary revascularization. In a secondary analysis, we studied patients taking statins prior to their CHD hospitalization and investigated whether differences in the proportion of patients who continued taking statins following discharge differed for beneficiaries with AMI as a secondary diagnosis versus other CHD‐related hospitalizations.
Methods
Study Design and Data Sources
We conducted a retrospective cohort study of Medicare beneficiaries who experienced a hospitalization with AMI or who underwent CABG or PCI in 2007, 2008, or 2009, using a national 5% random sample from the Centers for Medicare and Medicaid Services Chronic Condition Data Warehouse. Medicare is a federal program that provides health insurance for adults aged ≥65 years, for those with disabilities, and for patients with end‐stage renal disease in the United States. We obtained demographic and insurance coverage information on individual beneficiaries from Medicare enrollment files and claims for inpatient, outpatient, skilled nursing facility, home health, durable medical equipment services, noninstitutional provider, and prescription drug files. The Centers for Medicare and Medicaid Services and the institutional review board of the University of Alabama at Birmingham approved the study.
Eligible Population
Potentially eligible beneficiaries were grouped into 1 of 4 categories based on the type of CHD event experienced: (1) hospitalization for any primary reason other than AMI but with AMI listed as a secondary inpatient discharge diagnosis (ie, concurrent event or in‐hospital complications) with or without coronary intervention; (2) hospitalization for AMI as the primary inpatient discharge diagnosis (ie, major reason for admission) with or without coronary intervention; (3) hospitalization with CABG surgery but no AMI discharge diagnosis code in any position, with or without PCI; and (4) hospitalization with a PCI procedure but no AMI discharge diagnosis code in any position and no CABG procedure code. Each hospitalization was associated with 1 primary discharge diagnosis code and up to 9 secondary diagnosis codes. AMI was defined as International Classification of Diseases, ninth revision, clinical modification (ICD‐9‐CM) discharge diagnosis code 410.xx (except 410.x2, which indicates a subsequent episode of care) in the primary or any secondary position from an inpatient record. The positive predictive value of this approach to identify AMI is >90%.8 CABG was identified using Current Procedural Terminology (CPT) codes 33510 to 33536 or ICD‐9‐CM procedure codes 36.10 to 36.19, and PCI was identified using CPT codes 92980 to 92996 or ICD‐9‐CM procedure codes 00.66, 36.01 to 36.09. Each patient contributed 1 event based on his or her first eligible AMI or hospitalization with a revascularization procedure (ie, index hospitalization).
To be eligible for this analysis, beneficiaries also had to meet the following criteria: (1) aged ≥66 years on the date of admission for the index hospitalization, (2) 365 days of continuous full coverage by Medicare prior to the index hospitalization (the baseline period) and for 90 days after the discharge date, (3) survival for at least 90 days following discharge to permit uniform observation for statin prescriptions, and (4) no evidence of CHD diagnoses or coronary revascularization procedures in the baseline period. A history of CHD was identified using ICD‐9‐CM codes for Medicare claims during the 365 days prior to the index hospitalization. Full coverage was defined as traditional Medicare fee‐for‐service (Part A coverage for inpatient care and Part B coverage for other medical services and not being enrolled in a Medicare Advantage plan) and pharmacy (Part D) Medicare coverage. To increase the homogeneity of the study cohort, we excluded patients with a length of stay for their index hospitalization of >30 days. In addition, we excluded patients for whom the treating hospital could not be identified.
Identification of Statin Use
The outcome of interest was filling a statin prescription within 90 days following hospital discharge. Statin prescription fills were identified using Medicare Part D pharmacy claims. Six types of statins (simvastatin, atorvastatin, pravastatin, rosuvastatin, lovastatin, and fluvastatin) were identified using National Drug Codes. Beneficiaries taking and not taking statins during the baseline period, identified using Part D claims, were analyzed separately.
Covariates
We assessed covariates using claims and enrollment information from the 365‐day period before the index hospitalization. In addition to the categories of CHD event experienced, potential predictors measured during the baseline period included age, sex, race or ethnicity, socioeconomic status (defined as receipt of the low‐income subsidy for Part D premiums or dual Medicare or Medicaid eligibility), comorbid medical conditions (history of hyperlipidemia, diabetes, stroke, renal disease, and depression), Charlson comorbidity index,9–10 hospitalization and skilled nursing facility admission in the year prior to the index hospitalization, residency in a nursing home,11 cardiologist care in the year prior to the index hospitalization, use of nonstatin lipid‐lowering medications (ezetimibe, bile acid sequestrants, fibrates, and niacin), and total number of medications taken (defined by their unique generic names). Other variables assessed were calendar year of the index hospitalization; rehospitalization within 90 days after discharge; and duration of the hospitalization for the index CHD event, categorized as 1 to 7, 8 to 14, and 15 to 30 days.
Statistical Analysis
For patients who did not fill a statin prior to their index hospitalization, characteristics were stratified by category of CHD event (secondary discharge diagnosis of AMI, primary discharge diagnosis of AMI, CABG, and PCI). Because all patients were required to have survived and to have had Medicare coverage for 90 days following discharge, no patients were censored. For each CHD category, we used the Kaplan‐Meier method to calculate the proportion of beneficiaries initiating statins during the first 90 days following hospital discharge. We calculated the risk ratio for statin initiation using generalized estimating equation models with a binomial distribution and log link function, accounting for the clustering of patients within hospitals. After calculating crude risk ratios, 2 levels of adjustment were performed. Initial adjustment included age, sex, race or ethnicity, and calendar year of the CHD event to account for demographic differences between patients included in each of the CHD event categories. Subsequent adjustment also included the factors measured during the baseline period prior to the CHD event (socioeconomic status, comorbid medical conditions, the Charlson comorbidity index, all‐cause hospitalization, long‐term nursing home residency, skilled nursing facility admission, cardiologist care, total number of medications taken, use of nonstatin lipid‐lowering medications), duration of the index CHD hospitalization, and rehospitalization within 90 days after discharge to further account for differences in health status and treatments between the CHD categories. Among patients with AMI as a secondary discharge diagnosis, we determined the distribution of primary discharge diagnoses (grouped into ICD‐9‐CM 3‐digit categories) and the proportion initiating statins for each primary diagnosis group within 90 days after discharge. Because some patients may have paid for their medications through a mechanism that did not result in a Part D claim, we conducted a sensitivity analysis limited to patients who had at least 1 Medicare claim for any medication during the 90 days following discharge. Patients who did not initiate statins following a CHD event may have had a history of intolerance. In an attempt to identify a population that was less likely to have statin contraindications or intolerance, we conducted 3 sensitivity analyses excluding patients (1) who filled any nonstatin lipid‐lowering medications during baseline; (2) who had a history of CHD prior to the index hospitalization, using all available Medicare claims including those >365 days prior to the index hospitalization; and (3) who had no medication fills, who had cardiologist care, and who had a prescription filled for a nonstatin lipid‐lowering drug during baseline. Finally, we repeated our main analyses among patients who filled a statin in the baseline period (ie, prevalent statin users). All statistical analyses were carried out using SAS statistical software version 9.2 (SAS Institute Inc).
Results
During 2007–2009, 109 799 Medicare beneficiaries experienced a hospitalization for CHD, based on the 5% national random sample. After applying the exclusion criteria, our final study cohort consisted of 13 643 beneficiaries of whom 65.9% filled a statin prescription within 90 days following discharge. A flowchart of the exclusion criteria is presented in Figure 1.
Figure 1.
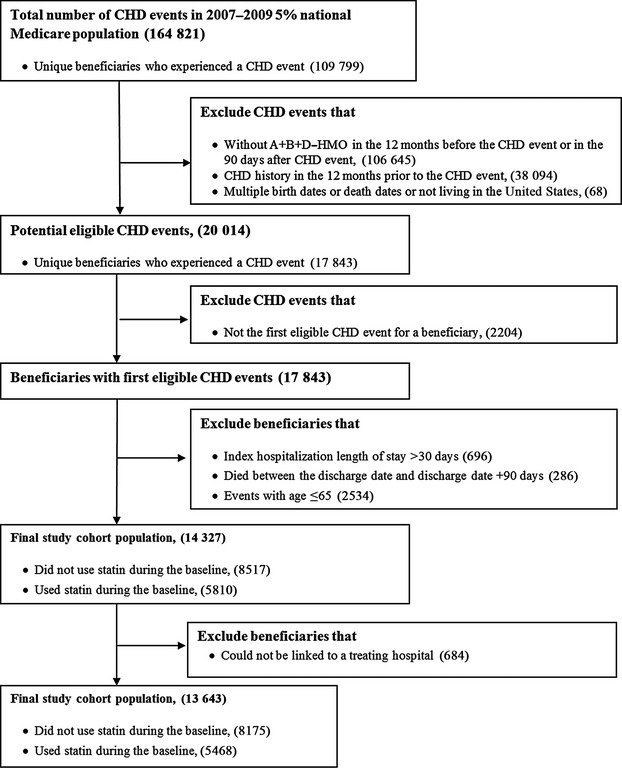
Selection of the study cohort. CHD indicates coronary heart disease. HMO indicates health maintenance organization.
Nonusers of Statins Prior to Index Hospitalization
Of the 13 643 patients, 8175 had not filled a statin during the 365 days prior to their index CHD hospitalization. Of this group, 4407 (54%) were categorized as AMI as primary discharge diagnosis, 1852 (23%) had AMI as a secondary discharge diagnosis, 1314 (16%) were in the PCI category, and 602 (7%) were in the CABG category (Table 1). Patients with an AMI as primary or secondary discharge diagnosis were older and were less likely to be men compared with those in the PCI or CABG categories. Compared with patients with PCI, CABG, or AMI as a primary discharge diagnosis, those with AMI as a secondary discharge diagnosis were more likely to have received a low‐income subsidy for Medicare Part D, to be eligible for Medicaid, to have been hospitalized during the year prior to the index CHD hospitalization, to have depression, to have a higher Charlson comorbidity index, to be a nursing home resident, to take more medications, and to have a longer index hospitalization.
Table 1.
Characteristics of Patients Not Taking Statins Prior to Having a Coronary Heart Disease Event
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=4407) | AMI, Secondary Discharge Diagnosis (n=1852) | PCI (n=1314) | CABG (n=602) | |
| Calendar year of index event | ||||
| 2007 | 32.6 | 28.9 | 37.2 | 27.7 |
| 2008 | 35.3 | 35.5 | 35.6 | 38.2 |
| 2009 | 32.0 | 35.6 | 27.2 | 34.1 |
| Age group, y | ||||
| 66 to 69 | 14.6 | 9.8 | 22.2 | 23.1 |
| 70 to 74 | 16.7 | 13.6 | 23.7 | 28.1 |
| 75 to 79 | 18.3 | 17.3 | 25.8 | 26.1 |
| 80 to 84 | 19.3 | 20.3 | 17.2 | 16.0 |
| ≥85 | 31.1 | 39.0 | 11.1 | 6.8 |
| Men | 34.1 | 26.4 | 42.7 | 56.8 |
| Race or ethnicity | ||||
| Black | 7.7 | 8.9 | 5.9 | 4.0 |
| White | 87.6 | 85.0 | 90.3 | 91.7 |
| Other | 4.7 | 6.1 | 3.9 | 4.3 |
| Socioeconomic status | ||||
| Low‐income subsidy for Medicare Part D premiums | 41.5 | 54.3 | 32.7 | 25.6 |
| Medicaid eligibility | 26.9 | 33.6 | 19.5 | 15.3 |
| Comorbidities | ||||
| History of hyperlipidemia | 30.1 | 25.3 | 51.6 | 56.8 |
| History of diabetes | 26.1 | 28.0 | 29.1 | 29.2 |
| History of stroke | 2.0 | 4.0 | 2.1 | 2.7 |
| History of renal disease | 9.2 | 12.4 | 11.7 | 10.8 |
| History of depression | 13.0 | 20.1 | 10.4 | 8.5 |
| Charlson comorbidity index | ||||
| 0 | 36.4 | 24.5 | 28.3 | 22.3 |
| 1 to 3 | 38.2 | 37.2 | 41.6 | 46.7 |
| ≥4 | 25.4 | 38.3 | 30.1 | 31.1 |
| Hospitalization for any cause during baseline | 27.9 | 43.2 | 63.2 | 83.4 |
| Nursing home residence | 11.7 | 21.3 | 2.8 | –* |
| Skilled nursing facility stay | 9.9 | 18.5 | 3.9 | –* |
| Most recent cardiologist care | ||||
| None | 87.0 | 84.7 | 60.4 | 46.7 |
| <31 days of index event | 3.6 | 3.6 | 27.9 | 41.5 |
| 31 to 365 days of index event | 9.4 | 11.8 | 11.6 | 11.8 |
| Number of medications during baseline* | ||||
| 0 | 8.3 | 6.1 | 5.9 | 7.5 |
| 1 to 5 | 27.3 | 19.7 | 26.3 | 30.4 |
| 6 to 10 | 31.8 | 28.2 | 34.8 | 35.6 |
| >10 | 32.6 | 46.0 | 33.0 | 26.6 |
| Filled nonstatin lipid‐lowering medications | 6.5 | 6.5 | 10.0 | 8.3 |
| Duration of hospitalization for the index CHD event, days | ||||
| 0 to 7 | 68.9 | 41.3 | 94.8 | 47.3 |
| 8 to 14 | 23.9 | 39.3 | 3.9 | 37.2 |
| 15 to 30 | 7.2 | 19.4 | 1.3 | 15.5 |
| Hospitalization during 90 days following discharge | 30.0 | 36.3 | 30.7 | 23.9 |
Data are shown as percentages. All variables except duration of hospitalization for the index CHD event and hospitalization during the 90 days following discharge are derived using data from the 365 days prior to the index CHD event. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Calculated as number of medications distinguished by unique generic drug names during the year prior to the index event.
Centers for Medicare and Medicaid Services policy requires suppression of cell sizes <11.
The proportion of patients who filled a statin gradually increased over the 90 days after discharge; however, the majority of patients who initiated statins did so within 10 days following discharge (Figure 2). Overall, 54.9% of patients who were not taking statins prior to their CHD event filled a statin within 90 days of discharge. At 90 days after discharge, 60.5% of those with AMI as their primary discharge diagnosis, 63.9% with PCI, and 67.6% with CABG filled a statin prescription. In contrast, only 31.2% of patients with a secondary discharge diagnosis for AMI filled a statin prescription within 90 days of discharge. In unadjusted and adjusted models, patients with a secondary discharge diagnosis of AMI were less likely than their counterparts with a primary discharge diagnosis of AMI to initiate statins (Table 2). Results were similar in sensitivity analyses limited to patients who filled a prescription for at least 1 medication of any type during the 90 days following discharge (Table 3) after excluding patients who were treated with nonstatin lipid‐lowering medications (Table 4); who had a documented history of CHD within or >365 days prior to the index hospitalization (Table 5); and who had no medication fills, who had cardiologist care, or who used nonstatin lipid‐lowering therapies only during the 365‐day baseline period (Table 6).
Figure 2.
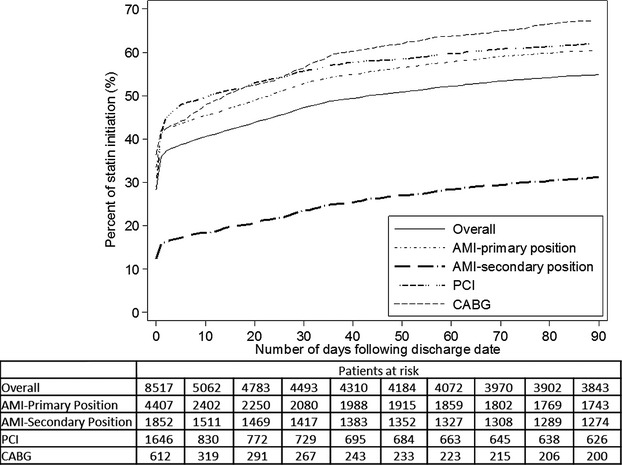
Percent of patients initiating statins following a coronary heart disease event. AMI indicates acute myocardial infarction; CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
Table 2.
Percentages and Risk Ratios for Initiating Statins Within 90 Days of a Coronary Heart Disease Event Associated With Category of Event Experienced
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=4407) | AMI, Secondary Discharge Diagnosis (n=1852) | PCI (n=1314) | CABG (n=602) | |
| Statin initiation, % | 60.5 | 31.2 | 63.9 | 67.6 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.52 (0.47 to 0.56) | 1.03 (0.95 to 1.11) | 1.12 (1.01 to 1.24) |
| Model 1 | 1 (ref) | 0.54 (0.49 to 0.59) | 0.98 (0.90 to 1.06) | 1.00 (0.90 to 1.12) |
| Model 2 | 1 (ref) | 0.59 (0.54 to 0.65) | 1.00 (0.91 to 1.09) | 1.08 (0.95 to 1.23) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering medications, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Table 3.
Risk Ratios for Initiating Statins Within 90 Days of a Coronary Heart Disease Event Associated With Category of Coronary Heart Disease Event Experienced Among Patients Who Filled at Least 1 Medication During the 90‐Day Follow‐up
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=4188) | AMI, Secondary Discharge Diagnosis (n=1675) | PCI (n=1266) | CABG (n=578) | |
| Statin initiation, % | 63.6 | 34.5 | 66.4 | 70.4 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.54 (0.50 to 0.59) | 1.05 (0.97 to 1.14) | 1.11 (1.00 to 1.23) |
| Model 1 | 1 (ref) | 0.56 (0.51 to 0.61) | 0.97 (0.90 to 1.05) | 1.00 (0.90 to 1.11) |
| Model 2 | 1 (ref) | 0.61 (0.56 to 0.67) | 1.01 (0.92 to 1.10) | 1.08 (0.95 to 1.22) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering medications, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Table 4.
Risk Ratios for Initiating Statins Within 90 Days of a Coronary Heart Disease Event Associated With Category of Coronary Heart Disease Event Experienced Excluding Patients Who Filled Any Nonstatin Lipid‐Lowering Medications During Baseline
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=4119) | AMI, Secondary Discharge Diagnosis (n=1732) | PCI (n=1182) | CABG (n=552) | |
| Statin initiation, % | 60.8 | 31.1 | 65.4 | 69.0 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.51 (0.47 to 0.56) | 1.08 (1.00 to 1.17) | 1.14 (1.02 to 1.27) |
| Model 1 | 1 (ref) | 0.53 (0.49 to 0.58) | 0.99 (0.91 to 1.07) | 1.02 (0.91 to 1.13) |
| Model 2 | 1 (ref) | 0.59 (0.53 to 0.65) | 1.00 (0.91 to 1.11) | 1.09 (0.96 to 1.25) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering medications, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Table 5.
Risk Ratios for Initiating Statins Within 90 Days of a Coronary Heart Disease Event Excluding Patients Who Had a History of Coronary Heart Disease Event Prior to the Index Hospitalization Using All Available Data
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=3932) | AMI, Secondary Discharge Diagnosis (n=1654) | PCI (n=1066) | CABG (n=507) | |
| Statin initiation, % | 61.6 | 31.9 | 66.9 | 71.4 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.52 (0.47 to 0.57) | 1.09 (1.00 to 1.18) | 1.16 (1.04 to 1.29) |
| Model 1 | 1 (ref) | 0.54 (0.49 to 0.59) | 1.00 (0.92 to 1.09) | 1.03 (0.92 to 1.16) |
| Model 2 | 1 (ref) | 0.59 (0.54 to 0.65) | 1.00 (0.91 to 1.11) | 1.09 (0.95 to 1.25) |
All available data include claims >365 days prior to admission for the CHD‐related hospitalization. Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering medications, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Table 6.
Risk Ratios for Initiating Statins Within 90 Days of a Coronary Heart Disease Event Associated Excluding Patients Who Had No Medication Fills, Who Had Cardiology Care, and Who Filled Nonstatin Lipid‐Lowering Therapies During the 365‐Day Baseline Period
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=3254) | AMI, Secondary Discharge Diagnosis (n=1361) | PCI (n=608) | CABG (n=218) | |
| Statin initiation, % | 60.8 | 31.1 | 65.4 | 69.0 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.51 (0.46 to 0.57) | 1.12 (1.01 to 1.25) | 1.24 (1.06 to 1.45) |
| Model 1 | 1 (ref) | 0.53 (0.48 to 0.59) | 1.03 (0.92 to 1.14) | 1.09 (0.93 to 1.28) |
| Model 2 | 1 (ref) | 0.59 (0.53 to 0.66) | 1.02 (0.90 to 1.15) | 1.13 (0.94 to 1.34) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering drugs, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Risk ratios for statin initiation associated with the predictors included in the multivariable model are shown in Table 7. In a model adjusted for age, sex, race, and calendar year, patients were less likely to initiate statins if they were older; received a low‐income subsidy for Medicare Part D premiums; were dual Medicare or Medicaid eligible; had diabetes, strokes, renal disease, depression, or a higher Charlson comorbidity index; were hospitalized for any cause during baseline; were nursing home residents; had a skilled nursing home stay; had cardiologist care 31 to 365 days prior to the index event; took nonstatin lipid‐lowering medications; or had an index hospitalization of >7 days. After full multivariable adjustment, patients were less likely to initiate statins within 90 days of discharge if they were aged >85 years, had a higher Charlson comorbidity index, were nursing home residents, had cardiologist care 31 to 365 days prior to the index event, did not use any medication during baseline, or took nonstatin lipid‐lowering medications.
Table 7.
Factors Associated With Initiation Of Statins Within 90 Days of Hospital Discharge for Coronary Heart Disease Events Among Patients on Medicare
| Statin Initiation, % | Risk Ratio (95% CI) | ||
|---|---|---|---|
| Model 1 | Model 2 | ||
| Event category | |||
| AMI, primary | 60.5 | Ref | Ref |
| AMI, secondary | 31.2 | 0.54 (0.49 to 0.59) | 0.59 (0.54 to 0.65) |
| PCI | 64.0 | 0.98 (0.91 to 1.07) | 1.00 (0.91 to 1.10) |
| CABG | 67.6 | 1.04 (0.93 to 1.16) | 1.12 (0.98 to 1.27) |
| Calendar year | |||
| 2007 | 54.8 | Ref | Ref |
| 2008 | 53.8 | 1.00 (0.93 to 1.07) | 0.99 (0.92 to 1.07) |
| 2009 | 56.3 | 1.05 (0.98 to 1.13) | 1.04 (0.97 to 1.12) |
| Age group, y | |||
| 66 to 69 | 69.2 | Ref | Ref |
| 70 to 74 | 64.3 | 0.95 (0.86 to 1.04) | 0.96 (0.88 to 1.06) |
| 75 to 79 | 58.8 | 0.88 (0.80 to 0.96) | 0.91 (0.82 to 0.99) |
| 80 to 84 | 54.8 | 0.84 (0.76 to 0.92) | 0.89 (0.81 to 0.98) |
| ≥85 | 38.4 | 0.61 (0.55 to 0.67) | 0.68 (0.60 to 0.74) |
| Sex | |||
| Female | 51.5 | Ref | Ref |
| Male | 61.1 | 1.03 (0.96 to 1.09) | 1.01 (0.95 to 1.08) |
| Race or ethnicity | |||
| White | 55.2 | Ref | Ref |
| Black | 49.3 | 0.90 (0.80 to 1.02) | 0.98 (0.87 to 1.11) |
| Asian | 59.7 | 1.10 (0.86 to 1.40) | 1.12 (0.88 to 1.43) |
| Hispanic | 56.3 | 1.06 (0.85 to 1.32) | 1.12 (0.89 to 1.40) |
| Other | 56.8 | 1.05 (0.84 to 1.32) | 1.05 (0.84 to 1.32) |
| Socioeconomic status | |||
| Low‐income subsidy for Medicare Part D premiums | 48.8 | 0.84 (0.78 to 0.89) | 0.92 (0.84 to 1.01) |
| Medicaid eligibility | 49.8 | 0.89 (0.83 to 0.96) | 1.07 (0.97 to 1.19) |
| Comorbidities | |||
| History of hyperlipidemia | 58.8 | 1.05 (0.98 to 1.11) | 1.03 (0.97 to 1.11) |
| History of diabetes | 51.1 | 0.88 (0.82 to 0.94) | 0.98 (0.91 to 1.06) |
| History of stroke | 42.8 | 0.81 (0.65 to 1.00) | 1.00 (0.81 to 1.25) |
| Renal disease | 42.3 | 0.76 (0.68 to 0.85) | 0.94 (0.83 to 1.06) |
| Depression | 43.8 | 0.80 (0.72 to 0.87) | 0.98 (0.89 to 1.08) |
| Charlson comorbidity index | |||
| 0 | 65.6 | Ref | Ref |
| 1 to 3 | 56.4 | 0.87 (0.82 to 0.93) | 0.91 (0.84 to 0.98) |
| ≥4 | 41.7 | 0.67 (0.61 to 0.72) | 0.80 (0.72 to 0.88) |
| Hospitalization for any cause during baseline | 49.7 | 0.85 (0.80 to 0.90) | 0.96 (0.88 to 1.03) |
| Nursing home residence | 27.2 | 0.53 (0.47 to 0.60) | 0.65 (0.57 to 0.75) |
| Skilled nursing facility stay | 32.1 | 0.62 (0.55 to 0.70) | 0.89 (0.77 to 1.02) |
| Most recent cardiologist care | |||
| None | 55.7 | Ref | Ref |
| <31 days of index event | 59.5 | 1.02 (0.93 to 1.12) | 0.91 (0.82 to 1.01) |
| 31 to 365 days of index event | 44.6 | 0.82 (0.74 to 0.91) | 0.83 (0.74 to 0.92) |
| Number of medications | |||
| 0 | 54.9 | 1.07 (0.94 to 1.21) | 0.82 (0.72 to 0.94) |
| 1 to 5 | 64.7 | 1.33 (1.23 to 1.44) | 1.02 (0.94 to 1.12) |
| 6 to 10 | 56.2 | 1.20 (1.11 to 1.29) | 1.00 (0.93 to 1.09) |
| >10 | 46.7 | Ref | Ref |
| Filled nonstatin lipid‐lowering medications | 49.7 | 0.84 (0.75 to 0.95) | 0.84 (0.74 to 0.95) |
| Hospitalization days for the index CHD event | |||
| 0 to 7 | 59.7 | Ref | Ref |
| 8 to 14 | 48.2 | 0.84 (0.78 to 0.91) | 0.95 (0.88 to 1.02) |
| 15 to 30 | 46.9 | 0.80 (0.72 to 0.89) | 0.95 (0.85 to 1.07) |
| Hospitalized during 90 days following discharge | 52.3 | 0.94 (0.88 to 1.01) | 1.03 (0.96 to 1.10) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 includes all variables in the table and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Of beneficiaries with AMI as a secondary discharge diagnosis, almost 50% had a primary discharge diagnosis for diseases of the circulatory system or diseases of the respiratory system (Table 8).
Table 8.
Primary Discharge Diagnoses and Percentage Initiating Statins for Patients With Acute Myocardial Infarction in a Secondary Position
| Primary Discharge Diagnosis (ICD‐9‐CM codes) | n | % | Statin Initiation, % |
|---|---|---|---|
| Diseases of the circulatory system (390 to 459) | 536 | 28.9 | 38.8 |
| Diseases of the respiratory system (460 to 519) | 382 | 20.6 | 29.8 |
| Infectious and parasitic diseases (001 to 139) | 280 | 15.1 | 25.4 |
| Injury and poisoning (800 to 999) | 205 | 11.1 | 29.3 |
| Diseases of the digestive system (520 to 579) | 144 | 7.8 | 27.8 |
| Diseases of the genitourinary system (580 to 629) | 69 | 3.7 | 23.2 |
| Diseases of musculoskeletal system and connective tissue (710 to 739) | 58 | 3.1 | 27.6 |
| Endocrine, nutritional, metabolic, and immunity disorders (240 to 279) | 45 | 2.4 | 28.9 |
| Neoplasms (140 to 239) | 37 | 2.0 | 35.1 |
| Other* | 96 | 5.2 | 27.5 |
ICD‐9‐CM indicates International Classification of Diseases, Ninth Revision, Clinical Modification.
Includes clinical classification categories with <20 patients.
Prevalent Statin Users
Of the population eligible for the current study, 5810 had filled a statin prescription during the 365 days prior to the index CHD hospitalization and were considered prevalent statin users. Table 9 shows the characteristics of prevalent statin users. Overall, 82.2% of prevalent statin users filled a statin prescription within 90 days of hospital discharge. The percentage of prevalent statin users who filled a statin prescription within 90 days of discharge was lower for those with AMI as a secondary discharge diagnosis (71.8%) compared with those with AMI as the primary discharge diagnosis (84.1%) or those with PCI (87.3%) or CABG (83.8%) (Table 10). After multivariable adjustment and compared with beneficiaries who had a primary discharge diagnosis of AMI, those with a secondary discharge diagnosis of AMI were 11% less likely to fill a statin prescription within 90 days of hospital discharge (risk ratio 0.89; 95% CI 0.82 to 0.97). Among prevalent statin users, no difference in filling a statin prescription was present between patients with AMI as the primary discharge diagnosis and those with PCI (risk ratio 1.01; 95% CI 0.93 to 1.10) or CABG (risk ratio 0.99; 95% CI 0.88 to 1.11) after multivariable adjustment.
Table 9.
Characteristics of 5468 Patients Taking Statins Prior to Their Coronary Heart Disease Events (Prevalent Statin Users)
| Categories of CHD Event | ||||
|---|---|---|---|---|
| AMI, Primary Discharge Diagnosis (n=2460) | AMI, Secondary Discharge Diagnosis (n=1140) | PCI (n=1264) | CABG (n=604) | |
| Calendar year | ||||
| 2007 | 31.8 | 26.8 | 32.8 | 31.6 |
| 2008 | 35.9 | 36.1 | 36.5 | 33.1 |
| 2009 | 32.2 | 37.1 | 30.8 | 35.3 |
| Age group, y | ||||
| 66 to 69 | 16.9 | 13.0 | 26.5 | 27.8 |
| 70 to 74 | 19.9 | 16.9 | 26.9 | 28.5 |
| 75 to 79 | 22.9 | 19.4 | 22.1 | 25.8 |
| 80 to 84 | 19.8 | 24.3 | 16.3 | 14.2 |
| ≥85 | 20.5 | 26.4 | 8.2 | 3.6 |
| Men | 31.5 | 27.5 | 38.6 | 48.2 |
| Race or ethnicity | ||||
| Black | 9.6 | 11.8 | 8.5 | 5.1 |
| White | 84.3 | 80.2 | 84.9 | 89.9 |
| Other | 6.1 | 8.0 | 6.6 | 5.0 |
| Socioeconomic status | ||||
| Low‐income subsidy for Medicare Part D premiums | 46.7 | 52.9 | 39.7 | 28.8 |
| Medicaid eligibility | 31.0 | 38.0 | 28.4 | 20.9 |
| Comorbidities | ||||
| History of hyperlipidemia | 71.2 | 69.0 | 81.0 | 87.8 |
| History of diabetes | 42.4 | 20.6 | 49.1 | 40.9 |
| History of stroke | 4.5 | 5.2 | 3.8 | 2.5 |
| History of renal disease | 14.3 | 20.3 | 13.8 | 12.1 |
| History of depression | 13.7 | 20.4 | 14.3 | 11.6 |
| Charlson comorbidity index | ||||
| 0 | 20.7 | 13.8 | 19.9 | 16.6 |
| 1 to 3 | 43.5 | 39.1 | 43.1 | 50.0 |
| ≥4 | 35.7 | 47.1 | 37.0 | 33.4 |
| Hospitalization for any cause during baseline | 33.1 | 47.6 | 58.9 | 82.5 |
| Nursing home residence | 10.1 | 19.2 | 3.5 | –* |
| Skilled nursing facility stay | 9.8 | 18.4 | 4.8 | 2.3 |
| Most recent cardiologist care | ||||
| None | 81.9 | 79.5 | 53.6 | 43.1 |
| <31 days of index event | 4.0 | 5.5 | 33.3 | 41.4 |
| ≥31 to 365 days of index event | 14.1 | 15.0 | 13.1 | 15.6 |
| Number of medications* | ||||
| 0 | n/a | n/a | n/a | n/a |
| 1 to 5 | 11.5 | 8.0 | 10.1 | 16.1 |
| 6 to 10 | 32.8 | 26.4 | 34.3 | 38.6 |
| >10 | 55.7 | 65.6 | 55.6 | 45.4 |
| Filled nonstatin lipid‐lowering drugs | 19.2 | 15.9 | 22.2 | 20.7 |
| Duration of hospitalization for the index CHD event, days | ||||
| 0 to 7 | 66.4 | 39.2 | 94.2 | 46.9 |
| 8 to 14 | 25.4 | 39.4 | 4.5 | 40.7 |
| 15 to 30 | 8.3 | 21.4 | 1.3 | 12.4 |
| Hospitalization during 90 days following discharge | 31.4 | 36.3 | 30.7 | 26.7 |
Data are shown as percentages. All variables except duration of hospitalization for the index CHD event and hospitalization during 90 days following discharge are derived using data from the 365 days prior to the index CHD event. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; n/a, not available; PCI, percutaneous coronary intervention.
Calculated as number of medications distinguished by unique generic drug names during the year prior to the index event.
Centers for Medicare and Medicaid Services policy requires suppression of cell sizes <11.
Table 10.
Percentages and Risk Ratios Filling a Statin Within 90 Days of a Coronary Heart Disease Event by Event Category Among Patients Taking Statins During the Year Prior to the Index Event
| AMI, Primary Discharge Diagnosis (n=2460) | AMI, Secondary Discharge Diagnosis (n=1140) | PCI (n=1264) | CABG (n=604) | |
|---|---|---|---|---|
| Statin initiation, % | 84.1 | 71.8 | 87.3 | 83.8 |
| Risk ratio (95% CI) for initiating statins | ||||
| Unadjusted | 1 (ref) | 0.85 (0.79 to 0.93) | 1.04 (0.97 to 1.12) | 1.00 (0.90 to 1.10) |
| Model 1 | 1 (ref) | 0.86 (0.79 to 0.93) | 1.03 (0.95 to 1.11) | 0.99 (0.90 to 1.11) |
| Model 2 | 1 (ref) | 0.89 (0.82 to 0.97) | 1.01 (0.93 to 1.10) | 0.99 (0.88 to 1.11) |
Model 1 is adjusted for age, race, sex, and calendar year and accounted for clustering by hospital. Model 2 is adjusted for age, race, sex, calendar year, socioeconomic status, comorbidities (history of hyperlipidemia, history of diabetes, history of stroke, history of renal disease, history of depression, Charlson comorbidity index, all‐cause hospitalization), skilled nursing facility stay, nursing home residence, most recent cardiologist care, number of medications, filled nonstatin lipid‐lowering medications, duration of hospitalization for the index CHD event, and hospitalization during the 90 days following discharge and accounted for clustering by hospital. AMI indicates acute myocardial infarction; CABG, coronary artery bypass grafting; CHD, coronary heart disease; PCI, percutaneous coronary intervention.
Discussion
In this observational study, we found that a substantial proportion of Medicare beneficiaries who had a CHD event did not fill prescriptions for statins within 90 days of discharge. Although 60% to 70% of patients with AMI as the primary reason for their hospitalization or with a revascularization procedure initiated statin use, only 31% of patients having AMI during hospitalization for another reason initiated statin use within 90 days of discharge. More than 80% of patients who were taking statins prior to their CHD event filled a statin prescription within 90 days of hospital discharge; however, among those taking statins prior to their index event, only 72% who had AMI during hospitalization for another reason filled a statin prescription following discharge. Among Medicare beneficiaries with AMI during hospitalization for another reason, the lower use of statins remained after adjustment for potential confounding factors. The low proportion of statin use among patients with AMI as a secondary diagnosis may represent a missed opportunity to prevent subsequent CHD events.
Statins delay mortality and reduce the risk for recurrent cardiovascular events in patients with established CHD.12–16 Using data from 90 056 participants in 14 randomized trials of statins, the Cholesterol Treatment Trialists’ Collaboration conducted a prospective patient‐level meta‐analysis to investigate the effects of statins on major coronary events, strokes, or coronary revascularizations. This meta‐analysis revealed that statin treatment can reduce the overall incidence of major coronary events among patients with previous history of CHD, regardless of the patient's initial lipid profile or other presenting characteristics.16 Consistent with this finding, current guidelines recommend that all patients be discharged on a statin following a CHD event unless a compelling contraindication is present6; however, the guidelines do not specifically address the group of patients with AMI that occurred as a complication of or concurrently with another reason for hospitalization.
Despite the significant CHD risk reduction associated with statin use and AHA and ACCF guidelines recommending their use,6 several studies have reported suboptimal statin use among people with established CHD. Using Medicare data from the New Jersey Pharmaceutical Assistance for the Aged and Disabled program and the Pennsylvania Pharmaceutical Assistance Contract for the Elderly program, Setoguchi et al assessed temporal trends in the use of statins among patients hospitalized for AMI in any position who survived at least 90 days after discharge. This study reported that 11% used statins in 1995, whereas 61% used statins in 2004.17 The latter number is similar to the results of our current national study of Medicare beneficiaries in 2007–2009. Although some registry studies have reported that a much higher percentage of patients are discharged with prescriptions for statins,1,18–19 a recent study using the National Cardiovascular Data Practice Innovation and Clinical Excellence PINNACLE Registry reported that only 68% to 72% of eligible patients with coronary artery disease received statin prescriptions in the outpatient setting.20 The lower prevalence of statin prescriptions in the PINNACLE Registry may be due to statin intolerance, incomplete documentation, or inclusion of a more heterogeneous patient and practice population than inpatient registries and randomized trials.20 In addition, patients may not fill prescribed medications because of inadequate health literacy, dislike of taking medications, and fears of side effects.21
We found that characteristics of patients with AMI occurring during a hospitalization for another reason were different from those of patients with AMI as the primary listed diagnosis or with coronary revascularization. In addition to being older and having higher Charlson comorbidity index scores, patients with AMI as a secondary diagnosis were more likely to be nursing home residents and to be eligible for a low‐income subsidy for Part D prescription drug coverage premiums. These findings are in agreement with previous studies reporting that patients who had AMI during hospitalization for another reason were more likely to have a history of diabetes and other comorbidities than patients who presented to the hospital with AMI.22–23 Although a study of the Veteran's Health Administration system showed that patients with in‐hospital AMIs were less likely to have intensive treatment or to take statins prior to their hospitalization than patients presenting with AMI,23 these studies did not report the proportion of patients initiating statins after discharge for an in‐hospital AMI compared with an out‐of‐hospital AMI.
Low statin use among Medicare beneficiaries with AMI as a secondary discharge diagnosis observed in this study might in part reflect physicians’ evaluations of the benefit–harm tradeoff for patients with multiple comorbidities or a history of statin intolerance.24–25 Although statin therapy would not benefit patients who were already dying from another cause, not prescribing treatment for many patients with AMI listed as a secondary diagnosis may not be appropriate. Among patients with CVD, statin use has been shown to benefit older patients (Pravastatin or Atorvastatin Evaluation and Infection Therapy Thrombolysis in Myocardial Infarction 22 trial), patients with chronic kidney disease (Treating to New Targets trial), and patients with prior stroke (Stroke Prevention by Aggressive Reduction in Cholesterol Levels trial), and current guidelines recommend secondary prevention for all AMIs.7,25–29 Our findings are consistent with prior reports that older patients and those with history of hypertension, stroke, and renal dysfunction are less likely to receive statin prescriptions after AMI.26 Although statins generally have a good safety profile, many patients report side effects.30 Statin intolerance is not directly captured in Medicare data. Excluding beneficiaries who used nonstatin lipid‐lowering therapy or who had prior cardiologist care but who did not fill a prescription for statins did not affect our results. Additional studies are necessary to identify the reasons for the lower levels of statin treatment in these high‐risk populations.
The current study has several strengths including a large sample of people having CHD events; the ability to evaluate information from patients before and after their CHD events; and the use of the Medicare 5% national sample, providing a high degree of generalizability to US adults aged ≥65 years. We acknowledge a number of limitations of this study. We were unable to validate AMI in the secondary discharge diagnosis position, although the available evidence supports the validity of the diagnosis.8 Using a sample of Medicare beneficiaries from Pennsylvania, Kiyota and colleagues evaluated several Medicare claims–based definitions of AMI and found that AMI defined using the primary diagnosis alone (ICD‐9‐CM codes 410.xx, except 410.x2) had a positive predictive value of 94.1%, and AMI defined using codes in any position had a positive predictive value of 92.3%.8 Using Medicare‐linked records for participants aged ≥65 years in the Women's Health Initiative, a recent study reported that 138 of 431 women (32%) who had an adjudicated AMI had a Medicare claim for hospitalization with a secondary diagnosis of AMI but no primary diagnosis of AMI.31 These studies indirectly support the accuracy of identifying patients with AMI by using primary and secondary discharge diagnosis codes.
Medicare data do not include information on whether a statin prescription was written, only whether it was filled. Furthermore, some patients may have filled their statin prescriptions without submitting a claim to Medicare. Although it is not known what percentage of Medicare beneficiaries with prescription drug coverage who fill statin prescriptions do not submit claims for reimbursement, a recent study using the osteoporosis drug alendronate as an example estimated that this may occur for up to of 15% of generic prescriptions available through low‐cost pharmacy programs.32 We conducted a sensitivity analysis limited to patients who filled any prescription medications within 90 days of discharge, and the results were similar. Furthermore, Medicare lacks data on history of statin intolerance and contraindications. We used claims data to assess information on comorbidities and other patient characteristics. A necessary assumption of this approach is that the lack of claims for a condition (eg, diabetes) implies that the patient does not have it. Finally, Medicare data do not include laboratory values, thus we did not have information on beneficiaries’ low‐density lipoprotein cholesterol levels; however, all patients experiencing a CHD event have an indication for the use of statins regardless of cholesterol level.6
In conclusion, <60% of Medicare beneficiaries not taking statins at the time of a CHD hospitalization initiated statin use within 90 days of discharge. Of particular importance, <1 in 3 patients experiencing an AMI during hospitalization for another primary condition initiated statins within 90 days of discharge. Even among patients taking statins prior to their CHD hospitalization, those having an AMI during hospitalization for another reason were less likely to fill a statin prescription within 90 days of discharge. These data highlight the need for additional efforts to increase the appropriate use of evidence‐based lipid‐lowering therapy following the occurrence of a CHD event.
Sources of Funding
This research, including design and conduct of the study, analysis and interpretation of the data, and preparation of the manuscript, was supported through an academic collaboration between University of Alabama at Birmingham, Icahn School of Medicine at Mount Sinai and Amgen Inc. The academic authors conducted all analyses and maintained the rights to publish this manuscript.
Disclosures
Dr Yun reports research support from Amgen. Dr Safford reports consulting fees, and salary support from diaDexus; research support from Amgen. Dr Farkouh reports research support from Amgen. Dr Kent reports research support from Amgen. Sharma reports support from Amgen. Dr Kilgore reports research support from Amgen. Dr Bittner reports research support from Amgen. Dr Rosenson has served on Advisory Boards and reports research support from Amgen. Dr Delzell reports research support from Amgen. Dr Muntner is advisory board member and grant recipient of Amgen, he reports consultant fees from Amgen; Dr Levitan reports research support from Amgen.
References
- Peterson ED, Roe MT, Chen AY, Fonarow GC, Lytle BL, Cannon CP, Rumsfeld JS. The NCDR Action Registry‐GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 2010; 96:1798-1802. [DOI] [PubMed] [Google Scholar]
- Guzman LA, Li S, Wang TY, Daviglus ML, Exaire J, Rodriguez CJ, Torres VI, Funk M, Saucedo J, Granger C, Pina IL, Cohen MG. Differences in treatment patterns and outcomes between hispanics and non‐hispanic whites treated for ST‐segment elevation myocardial infarction: results from the NCDR ACTION Registry‐GWTG. J Am Coll Cardiol. 2012; 59:630-631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradiso‐Hardy FL, Gordon WL, Jackevicius CA, Kertland HR, Pearson GJ, Pickering JL, Poirier L, Semchuk BM, Verret L. The importance of in‐hospital statin therapy for patients with acute coronary syndromes. Pharmacotherapy. 2003; 23:506-513. [DOI] [PubMed] [Google Scholar]
- Rosamond WD, Chambless LE, Sorlie PD, Bell EM, Weitzman S, Smith JC, Folsom AR. Trends in the sensitivity, positive predictive value, false‐positive rate, and comparability ratio of hospital discharge diagnosis codes for acute myocardial infarction in four US communities, 1987–2000. Am J Epidemiol. 2004; 160:1137-1146. [DOI] [PubMed] [Google Scholar]
- Smith SC, Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, Grundy SM, Hiratzka L, Jones D, Krumholz HM, Mosca L, Pasternak RC, Pearson T, Pfeffer MA, Taubert KAAHA/ACC; National Heart, Lung, and Blood Institute. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006; 113:2363-2372. [DOI] [PubMed] [Google Scholar]
- Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd‐Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KAWorld Heart Federation and the Preventive Cardiovascular Nurses Association. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124:2458-2473. [DOI] [PubMed] [Google Scholar]
- Smith SC, Jr, Blair SN, Bonow RO, Brass LM, Cerqueira MD, Dracup K, Fuster V, Gotto A, Grundy SM, Miller NH, Jacobs A, Jones D, Krauss RM, Mosca L, Ockene I, Pasternak RC, Pearson T, Pfeffer MA, Starke RD, Taubert KA. AHA/ACC scientific statement: AHA/ACC guidelines for preventing heart attack and death in patients with atherosclerotic cardiovascular disease: 2001 update: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation. 2001; 104:1577-1579. [DOI] [PubMed] [Google Scholar]
- Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of medicare claims‐based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004; 148:99-104. [DOI] [PubMed] [Google Scholar]
- Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD‐9‐CM administrative data: differing perspectives. J Clin Epidemiol. 1993; 46:1075-1079. [DOI] [PubMed] [Google Scholar]
- Schneeweiss S, Maclure M. Use of comorbidity scores for control of confounding in studies using administrative databases. Int J Epidemiol. 2000; 29:891-898. [DOI] [PubMed] [Google Scholar]
- Yun H, Kilgore M, Curtis JR, Delzell E, Gary LC, Saag K, Morrisey MA, Becker D, Matthews R, Smith W, Locher JL. Identifying types of nursing facility stays using medicare claims data: an algorithm and validation. Health Serv Outcomes Res Method. 2010; 10:100-110. [Google Scholar]
- Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994; 344:1383-1389. [PubMed] [Google Scholar]
- Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial Investigators. N Engl J Med. 1996; 335:1001-1009. [DOI] [PubMed] [Google Scholar]
- Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The long‐term intervention with pravastatin in ischaemic disease (lipid) study groupN Engl J Med. 1998; 339:1349-1357. [DOI] [PubMed] [Google Scholar]
- Robinson JG, Maheshwari N. A “poly‐portfolio” for secondary prevention: a strategy to reduce subsequent events by up to 97% over five years. Am J Cardiol. 2005; 95:373-378. [DOI] [PubMed] [Google Scholar]
- Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes RCholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol‐lowering treatment: Prospective meta‐analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267-1278. [DOI] [PubMed] [Google Scholar]
- Setoguchi S, Glynn RJ, Avorn J, Mittleman MA, Levin R, Winkelmayer WC. Improvements in long‐term mortality after myocardial infarction and increased use of cardiovascular drugs after discharge: a 10‐year trend analysis. J Am Coll Cardiol. 2008; 51:1247-1254. [DOI] [PubMed] [Google Scholar]
- Diercks DB, Owen KP, Kontos MC, Blomkalns A, Chen AY, Miller C, Wiviott S, Peterson ED. Gender differences in time to presentation for myocardial infarction before and after a national women's cardiovascular awareness campaign: a temporal analysis from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress ADverse Outcomes with Early Implementation (CRUSADE) and the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network‐Get with the Guidelines (NCDR ACTION Registry‐GWTG). Am Heart J. 2010; 160:80-87. [DOI] [PubMed] [Google Scholar]
- Chan PS, Oetgen WJ, Buchanan D, Mitchell K, Fiocchi FF, Tang F, Jones PG, Breeding T, Thrutchley D, Rumsfeld JS, Spertus JA. Cardiac performance measure compliance in outpatients: the American College of Cardiology and National Cardiovascular Data Registry's PINNACLE (Practice Innovation And Clinical Excellence) program. J Am Coll Cardiol. 2010; 56:8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddox TM, Chan PS, Spertus JA, Tang F, Jones P, Ho PM, Bradley SM, Tsai TT, Bhatt DL, Peterson PN. Variations in coronary artery disease secondary prevention prescriptions among outpatient cardiology practices: insights from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol. 2014; 63:539-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison TN, Derose SF, Cheetham TC, Chiu V, Vansomphone SS, Green K, Tunceli K, Scott RD, Marrett E, Reynolds K. Primary nonadherence to statin therapy: patients’ perceptions. Am J Manag Care. 2013; 19:e133-e139. [PubMed] [Google Scholar]
- Zahn R, Schiele R, Seidl K, Kapp T, Glunz HG, Jagodzinski E, Voigtlander T, Gottwik M, Berg G, Thomas H, Senges J. Acute myocardial infarction occurring in versus out of the hospital: patient characteristics and clinical outcome. Maximal Individual TheRapy in Acute Myocardial Infarction (MITRA) Study Group. J Am Coll Cardiol. 2000; 35:1820-1826. [DOI] [PubMed] [Google Scholar]
- Maynard C, Lowy E, Rumsfeld J, Sales AE, Sun H, Kopjar B, Fleming B, Jesse RL, Rusch R, Fihn SD. The prevalence and outcomes of in‐hospital acute myocardial infarction in the department of veterans affairs health system. Arch Intern Med. 2006; 166:1410-1416. [DOI] [PubMed] [Google Scholar]
- Ko DT, Mamdani M, Alter DA. Lipid‐lowering therapy with statins in high‐risk elderly patients: the treatment‐risk paradox. JAMA. 2004; 291:1864-1870. [DOI] [PubMed] [Google Scholar]
- Alonzo CB. Myths and facts concerning the use of statins in very old patients. Cardiovasc Hematol Disord Drug Targets. 2011; 11:17-23. [DOI] [PubMed] [Google Scholar]
- Albert NM, Birtcher KK, Cannon CP, Goff DC, Jr, Mulgund J, Liang L, Fonarow GC. Factors associated with discharge lipid‐lowering drug prescription in patients hospitalized for coronary artery disease (from the Get With the Guidelines database). Am J Cardiol. 2008; 101:1242-1246. [DOI] [PubMed] [Google Scholar]
- Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RGPROSPER study group. PROspective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): A randomised controlled trial. Lancet. 2002; 360:1623-1630. [DOI] [PubMed] [Google Scholar]
- Sever PS, Dahlof B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren JASCOT Investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower‐than‐average cholesterol concentrations, in the Anglo‐Scandinavian Cardiac Outcomes Trial‐Lipid Lowering Arm (ASCOT‐LLA): a multicentre randomised controlled trial. Lancet. 2003; 361:1149-1158. [DOI] [PubMed] [Google Scholar]
- Ray KK, Bach RG, Cannon CP, Cairns R, Kirtane AJ, Wiviott SD, McCabe CH, Braunwald E, Gibson CM, Investigators PI‐T. Benefits of achieving the NCEP optional LDL‐C goal among elderly patients with ACS. Eur Heart J. 2006; 27:2310-2316. [DOI] [PubMed] [Google Scholar]
- Cohen JD, Brinton EA, Ito MK, Jacobson TA. Understanding Statin Use in America and Gaps in Patient Education (USAGE): an internet‐based survey of 10,138 current and former statin users. J Clin Lipidol. 2012; 6:208-215. [DOI] [PubMed] [Google Scholar]
- Hlatky MA, Ray RM, Burwen DR, Margolis KL, Johnson KC, Kucharska‐Newton A, Manson JE, Robinson JG, Safford MM, Allison M, Assimes TL, Bavry AA, Berger J, Cooper‐DeHoff RM, Heckbert SR, Li W, Liu S, Martin LW, Perez MV, Tindle HA, Winkelmayer WC, Stefanick ML. Use of Medicare data to identify coronary heart disease outcomes in the Women's Health Initiative. Circ Cardiovasc Qual Outcomes. 2014; 7:157-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun H, Curtis JR, Saag K, Kilgore M, Muntner P, Smith W, Matthews R, Wright N, Morrisey MA, Delzell E. Generic alendronate use among Medicare beneficiaries: are part D data complete? Pharmacoepidemiol Drug Saf. 2013; 22:55-63. [DOI] [PMC free article] [PubMed] [Google Scholar]


