Abstract
Background
Patient safety (PS) receives limited attention in health professional curricula. We developed and pilot tested four Objective Structured Clinical Examination (OSCE) stations intended to reflect socio-cultural dimensions in the Canadian Patient Safety Institute's Safety Competency Framework.
Setting and participants
18 third year undergraduate medical and nursing students at a Canadian University.
Methods
OSCE cases were developed by faculty with clinical and PS expertise with assistance from expert facilitators from the Medical Council of Canada. Stations reflect domains in the Safety Competency Framework (ie, managing safety risks, culture of safety, communication). Stations were assessed by two clinical faculty members. Inter-rater reliability was examined using weighted κ values. Additional aspects of reliability and OSCE performance are reported.
Results
Assessors exhibited excellent agreement (weighted κ scores ranged from 0.74 to 0.82 for the four OSCE stations). Learners’ scores varied across the four stations. Nursing students scored significantly lower (p<0.05) than medical students on three stations (nursing student mean scores=1.9, 1.9 and 2.7; medical student mean scores=2.8, 2.9 and 3.5 for stations 1, 2 and 3, respectively where 1=borderline unsatisfactory, 2=borderline satisfactory and 3=competence demonstrated). 7/18 students (39%) scored below ‘borderline satisfactory’ on one or more stations.
Conclusions
Results show (1) four OSCE stations evaluating socio-cultural dimensions of PS achieved variation in scores and (2) performance on this OSCE can be evaluated with high reliability, suggesting a single assessor per station would be sufficient. Differences between nursing and medical student performance are interesting; however, it is unclear what factors explain these differences.
Keywords: Patient safety, Health professions education, Teamwork
Background
Patient safety (PS) competency among health professionals (HPs) nearing entry to practice is an area of growing interest. There are recommendations from numerous international bodies regarding the need to restructure HP education to ensure it equips students with the knowledge, skills and attitudes necessary to function safely.1–5 Yet, PS receives limited attention in HP curricula.6 Moreover, when asked about their confidence in PS learning, new graduates in medicine, nursing and pharmacy identify a number of gaps in PS learning.7
The Canadian Patient Safety Institute (CPSI) Safety Competency Framework5 suggests six core competency domains that reflect the knowledge, skills and attitudes that enhance PS across the continuum of care (see box 1). Previously, we examined new graduates’ self-reported confidence in each of these six competency areas.7 Self-reported PS competence provides one important and cost effective source of information about the effectiveness of the HP education process,1 including aspects of an individual's PS knowledge that need attention.8 9 However, a recent systematic review concluded that physicians have a limited ability to accurately self-assess10 and this may be particularly true among the least skilled.10 11 Self-assessment alone is insufficient as it is not a stable skill (in some contexts it can be quite accurate but not in others). Instead, self-improvement is most likely to occur when a learner engages in internal reflection and also receives feedback from external sources.12
Box 1. Canadian Patient Safety Institute Safety Competencies5.
Domain 1: Contribute to a culture of patient safety—Commitment to applying core patient safety knowledge, skills and attitudes to everyday work
Domain 2: Work in teams for patient safety—Collaboration and interdependent decision-making with inter-professional teams and with patients to optimise patient safety and quality of care
Domain 3: Communicate effectively for patient safety—Promote patient safety through effective healthcare communication
Domain 4: Manage safety risks—Anticipate, recognise and manage situations that place patients at risk
Domain 5: Optimise human and environmental factors—Manage the relationship between individual and environmental characteristics to optimise patient safety
Domain 6: Recognise, respond to and disclose adverse events—Recognise the occurrence of an adverse event or close call and respond effectively to mitigate harm to the patient, ensure disclosure and prevent recurrence
Objective Structured Clinical Examinations (OSCEs) provide external assessments of knowledge, skills and behaviours in the context of a low risk simulated clinical encounter and a growing literature encourages their use to assess PS competencies.13–15 Most PS OSCE studies have focused on clinical aspects of PS, such as hand hygiene, medication labelling16 and safe performance of procedures (eg, chest tube insertion),17 or on specific quality improvement techniques, such as root cause analysis.18 19 With the exception of those that focus on error disclosure, few studies use OSCEs to assess socio-cultural aspects of PS20 21 and most are discipline-specific (ie, only for physicians or only for nurses).
We developed and pilot tested a 4-station OSCE focused on the socio-cultural dimensions of the CPSI Safety Competency Framework5 that assessed both nursing and medical students at level 2 of educational outcomes, as outlined by Kirkpatrick22 and used by Barr.23 Level 2 outcomes reflect the degree to which learners acquire knowledge and skills. Using Miller's framework for clinical assessment,24 OSCEs and the use of standardised patients allow learners to demonstrate competence (knows how to do something) and performance (shows how).
Methods
OSCE development
Expert facilitators from the Medical Council of Canada led a 1.5 day case writing workshop in June 2013. Seven faculty members from nursing and medicine with content expertise in PS participated and each one submitted a case by workshop close. These cases were revised by a trained case writer in conjunction with the study authors. The revised cases were then appraised by clinicians with expertise in OSCE or PS who had not previously seen the cases. This second group assessed each case based on (1) realism and (2) suitability for both nursing and medical students. Using their feedback, four cases were selected for pilot testing. In addition to their feedback, the number of PS competencies (box 1) reflected in each case, the balance of competencies across cases and the simulation requirements for each case were taken into account. Specifically, cases requiring standardised clinicians needed to be limited as these were deemed more challenging to portray and pilot.
Setting and subjects
All third and fourth year students enrolled in an undergraduate nursing programme or undergraduate medical programme at a Canadian university were invited to participate in a ‘voluntary research study focused on PS knowledge and skills’. They were assured that their data would be anonymised and would in no way be connected to their educational record. Students were offered a $20 coffee card and dinner as a modest inducement to participate. Eighteen third year students volunteered—eight nursing students and 10 medical students. The study received approval from the relevant research ethics board at the university which took part in the pilot and from the lead author's institution.
Stations
Each station was based on one case from the workshop and reflected at least four of the competency areas in the Safety Competency Framework.5 Station 1 required learners to uncover a deep vein thrombosis (DVT) near miss and then explain the system factors that led to the near miss to the patient's spouse. Station 2 involved team dynamics and communication with a patient around a complex discharge, while station 3 required learners to persist in an interaction with a dismissive, time-pressured staff physician. Station 4 required learners to discuss an insulin overdose with the patient including how it occurred and how similar events might be prevented in the future. Learners moved through each station one at a time. Competency area 2 (work in teams for PS) was evaluated based on the learner's interaction with the standardised patient/person (SP) as well as the extent to which the learner was respectful and professional in his or her description of the role other team members (not present in the station) played in the case (eg, they did not blame others). The safety context and competency areas of each station are provided in table 1. Standardised persons were recruited and trained as per the university simulation centre's protocol. Stations were 8 min long. In stations 1–3, a 6-min buzzer was incorporated and the last 2 min were reserved for specified oral questions administered by an assessor (as described below). There were 2 min between stations for learners to read the scenario and task(s) for the following station. Learners completed all four stations in 40 min.
Table 1.
Station descriptions
| Station | Case name | Safety context | PS competency areas assessed*†‡§¶ | Standardised person |
|---|---|---|---|---|
| 1 | Jim the Roofer | Near miss (DVT)—Learner is asked to deliver a normal test result; patient's wife has received discrepant information about the test | Communication*, teamwork†, managing risk‡, R, R and disclose§, culture¶ | Patient's wife |
| 2 | Bertha's not ready to go | Complex discharge—Staff tells learner to discharge recovering stroke patient due to hospital capacity pressure; patient expresses several concerns about leaving so soon | Communication*, teamwork†, managing risk‡, culture¶ | Patient |
| 3 | Jackson is in pain | Challenging authority—Learner has concerns about a patient's pain and requests staff physician's assessment; superior is busy and dismissive | Communication*, teamwork†, managing risk‡, culture¶ | Staff physician |
| 4 | Giny's insulin | Medication error disclosure—Learner is asked to communicate an insulin overdose; patient expresses concerns and has questions | Communication*, teamwork†, R, R and disclose§, culture¶ |
Patient |
*Communicate effectively for PS.
†Work in teams for PS.
‡Manage safety risks.
§Recognise, respond to and disclose adverse events.
¶Contribute to a culture of safety.
DVT, deep vein thrombosis; PS, patient safety.
Assessors and scoring
Each station was scored on four or five relevant PS competency dimensions (see table 1). A single 5-point global rating scale was adopted25 and used for all: 0=COMPETENCE NOT DEMONSTRATED for a learner at this level—Skills: Clearly deficient; 1=BORDERLINE UNSATISFACTORY for a learner at this level—Skills: Somewhat deficient; 2=BORDERLINE SATISFACTORY for a learner at this level—Skills: Just adequate; 3=COMPETENCE DEMONSTRATED for a learner at this level—Skills: Good; 4=ABOVE the level expected of a learner at this level—Skills: Excellent. The decision to use rating scales alone aligns with the idea that mastery of the parts (ie, discrete skills on a checklist) does not indicate competency of the whole. While ‘global ratings provide a more faithful reflection of expertise than detailed checklists’26 and expert assessors are able to evaluate these holistic skills,27 assessors were also provided with two to three concrete behaviours per competency to look for when rating learners. The intent was to improve rater agreement by providing assessors with a common framework for each case.
Scoring in each station was done by two assessors who were both in the exam room. Each assessor was a current or retired clinical faculty member from nursing or medicine. The primary assessor also had expertise in PS science and administered the oral questions. The oral questions allowed learners to demonstrate knowledge or behaviours that may not have been elicited in their interaction with the SP. For example in station 1, regarding the DVT near miss, the oral question explicitly asked about the system issues at play (which is core PS knowledge for the ‘Contribute to a culture of patient safety’ domain) since ‘system factors’ are not something the SP spouse could realistically question. Assessors were instructed to reflect on both the learner's interaction with the SP and on the learner's response to the oral questions when rating learner's competencies.
All assessors participated in a 1-h training session to familiarise them with the OSCE goals and the rating guidelines. To promote a common understanding of the rating scale anchors and to guide assessor discrimination between rating scale options, assessors were given a ‘Guidelines to Rating Sheet’ that provided non-case-specific competency definitions, boundaries, and descriptors of COMPETENT or ABOVE performance. They also received case-specific examples for each competency dimension to guide their observations. A calibration video (of a station 3 dry run) was scored by all assessors, and then discussed so they could calibrate their ratings. Assessor dyads were asked not to discuss their ratings with one another during the OSCE. For a more detailed description of one station, including the specific behaviours tied to each of the four competency areas assessed in the case, see the online supplementary case appendix.
During the OSCE, it became clear that one assessor in station 2 was in a conflict of interest with one group of students. As a result, station 2 was rescored. The station 1 assessor dyad received refresher training and then rescored station 2 based on video recordings. Data presented here use the second set of scores for station 2 (see online supplementary technical appendix, Station 2 Reassessment for one exception).
Analysis
Reliability refers to the reproducibility of scores obtained from an assessment. We examined within-station internal consistency reliability (Cronbach's α).28 Inter-rater reliability was examined using the equivalent29 of a weighted κ.30 A weighted κ is typically used for categorical data with an ordinal structure and takes into account the magnitude of a disagreement between assessors (eg, the difference between the first and second category is less important than a difference between the first and third category; see online supplementary technical appendix, Inter-rater reliability). Two-way mixed, average-measures, agreement intraclass correlation coefficient (ICC) is also reported as it provides a measure of the score reliability. For interpretation of ICCs, including weighted κ, Cicchetti's classification (inter-rater reliability less than 0.40 is poor; 0.40–0.59 is fair; 0.60–0.74 is good; 0.75–1.00 is excellent)31 was used.
Given that there was strong assessor agreement, the mean of the two assessors’ scores became the station score for each candidate. Scores between nursing and medical students were compared with an independent samples t test for each station. Finally, the proportion of learners with above and below borderline competence scores for 1, 2, 3 and all 4 stations is reported.
Results
Reliability
Table 2 shows inter-rater reliability (weighted κ) and station score reliability given two assessors (average measures ICC). The weighted κ columns show that assessor agreement was good to excellent for half of the competency rating scales in all four stations. When calculated on the station scores (the mean of the competency area ratings within a station), assessor agreement was excellent for all four stations. Table 2 (average-measures ICC columns) indicates good score reliability for all four stations (Hallgren—personal communication) as all values exceed 0.8. Finally, within-station reliability was strong for all four stations (αs=0.881, 0.859, 0.893 and 0.767 for stations 1 through 4, respectively).
Table 2.
Agreement of pairs of assessors and score reliability (across competency dimensions and stations)
| Station 1 | Station 2 | Station 3 | Station 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Near miss (DVT) | Complex discharge | Challenging authority | Medication error disclosure | |||||
| PS competency area*†‡§¶ | Weighted κ | Avg measures ICC | Weighted κ | Avg measures ICC | Weighted κ | Avg measures ICC | Weighted κ | Avg measures ICC |
| Communication* | 0.517 | 0.608 | 0.660 | 0.789 | 0.717 | 0.815 | 0.432 | 0.547 |
| Teamwork† | 0.665 | 0.809 | 0.135 | 0.247 | 0.496 | 0.659 | 0.438 | 0.621 |
| Managing risk‡ | 0.794 | 0.888 | 0.637 | 0.692 | 0.869 | 0.933 | NA | NA |
| R, R and disclose§ | 0.568 | 0.716 | NA | NA | NA | NA | 0.548 | 0.714 |
| Culture¶ | 0.560 | 0.712 | 0.693 | 0.795 | 0.390 | 0.502 | 0.754 | 0.860 |
| Station score | 0.803 | 0.894 | 0.737 | 0.811 | 0.794 | 0.870 | 0.816 | 0.895 |
*Communicate effectively for PS.
†Work in teams for PS.
‡Manage safety risks.
§Recognise, respond to and disclose adverse events.
¶Contribute to a culture of safety.
DVT, deep vein thrombosis; ICC, intraclass correlation coefficient; PS, patient safety.
Station scores
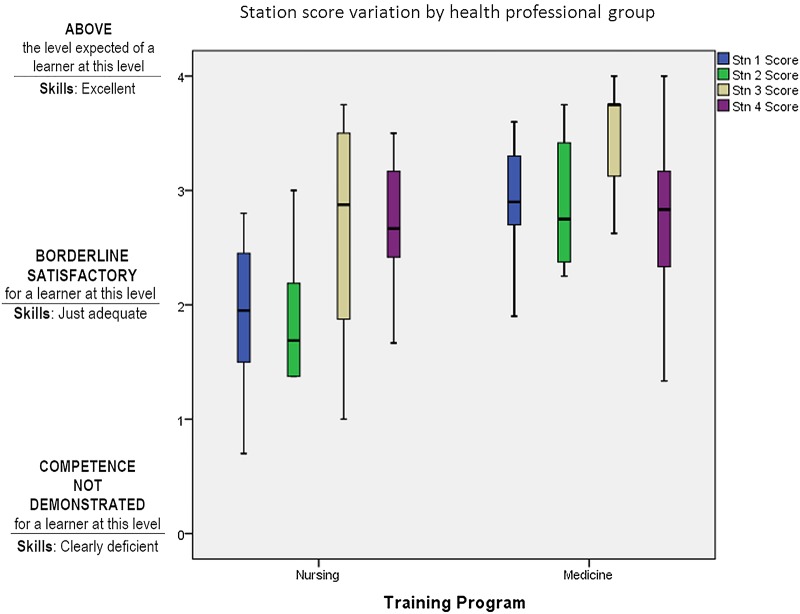
The boxplot in figure 1 shows station score variation by HP group. The whiskers show the score range for the top and bottom 25% of learners, the box shows the IQR (the middle 50% of scores for the group), and the line in the box is the median. Figure 1 shows that the proportion of learners who achieved a station score above borderline satisfactory (rating=2) varied across stations and by HP learner group.
Figure 1.
Station score variation by health professional group.
The independent samples t test comparing nursing and medical students was statistically significant for stations 1, 2 and 3 (t(16)=−3.55, p<0.01, d=1.65; t(16)=−3.83, p<0.01, d=1.81; t(16)=−2.27, p<0.05, d=1.03 for stations 1, 2 and 3, respectively). Table 3 shows that students in the nursing group scored lower than medical students on the DVT near miss (station 1), the complex discharge (station 2) and challenging authority (station 3). All of these effects exceed Cohen's (1988) convention for a large effect size (d=0.80). There was no difference in nursing and medical students’ scores on station 4—medication error (t(16)=−0.23, p=0.82, d=0.1).
Table 3.
OSCE Performance by station by learner group
| Station | Medical students station score M (SD) |
Nursing students station score M (SD) |
|---|---|---|
| 1. Near miss (DVT) | 2.90 (0.48)* | 1.91 (0.70) |
| 2. Complex discharge | 2.92 (0.57)* | 1.86 (0.60) |
| 3. Challenging authority | 3.49 (0.48)** | 2.66 (1.03) |
| 4. Medication error disclosure | 2.78 (0.77) | 2.71 (0.59) |
*p<0.01, ** p<0.05.
DVT, deep vein thrombosis; OSCE, Objective Structured Clinical Examination.
Last, overall performance across all four stations was considered. One student (6%) did not achieve a station score of 3 or higher on any of the stations (a score of 3=COMPETENCE DEMONSTRATED for a learner at this level—Skills: Good) and eight students (44%) received a station score of 3 or higher on only one station. Five students (28%) received a station score of 3 or higher on two stations, and four students (22%) received a station score of 3 or higher on three or four stations. In all, 39% of students (7/18) received an overall station score below two on at least one station (a score of 2=BORDERLINE SATISFACTORY for a learner at this level—Skills: Just adequate).
Discussion
OSCEs are a familiar, widely used method of assessing performance for HPs. Given the increasing interest in teaching PS in undergraduate HP curriculum, this study explored the use of OSCE for assessing aspects of this domain. Our results demonstrate that sufficiently reliable station scores can be achieved in OSCE stations designed to assess performance on socio-cultural aspects of PS. High levels of inter-rater reliability for the overall station scores can also be achieved, indicating a minimal amount of measurement error was introduced by independent assessors. Given this finding, future studies may only require a single assessor in each station. Although the assessors were all clinical faculty, only one assessor per dyad had PS expertise. Sometimes, the PS expert was nursing faculty, sometimes medical faculty. Our experience suggests that clinical faculty in either nursing or medicine, with as little as 1 h of training, can provide reliable assessments of HP students’ PS competence in an OSCE such as this one.
Our experience also suggests that the global ratings, although to some degree subjective, are not inherently unreliable.27 From a validity standpoint, competency assessment in the context of PS requires global ratings of holistic expertise rather than evaluation of discrete skills.27 Using an OSCE scored with global rating scales is consistent with two important trends identified by van der Vleuten and Schuwirth:27 (1) a growing emphasis on general professional competencies (such as teamwork and awareness of the roles of culture and complex systems) in HP education and (2) recognition of the value of learning skills in an integrated fashion. The OSCE described here has a veneer of required clinical skills but asks learners to demonstrate competence in more multi-faceted socio-cultural aspects of PS.
The variability in scores across stations and between HP learner groups was seen as reasonable. Participants were third year medical and nursing students in the course of their regular training programme, with no additional PS curricular material. Their overall performance levels on this OSCE suggest that socio-cultural aspects of PS in undergraduate curricula may need to be enriched.
Differences between medical and nursing student performance were relatively large on three of the four stations. However, whether these differences stem from differences in their education (eg, most third year nursing students have less OSCE experience than third year medical students) or from the type of clinical encounters they are exposed to during training (eg, nursing students are more likely to be familiar with medication errors, the one context where nursing students’ and medical students’ scores did not differ) is not clear. Relatedly, differences in nursing and medical student scores may reflect differences in how they are/have been trained to fill their professional role (eg, nurses may not be trained to question authority or to consider and communicate about system issues).
The differences between medical and nursing student performance are interesting when compared with our previous work with new graduates.7 While medical student performance was higher than nursing student performance in the current study, the pattern is reversed for self-assessed confidence on the same socio-cultural dimensions (ie, self-assessed confidence was higher for new nurses than new physicians).7 This reversal fits with Eva and Regehr12 who argue that self-assessment skills can be accurate in some contexts but not in others and therefore should be used alongside external assessments such as OSCEs.
Finally, the OSCE described here is suitable for students in nursing and medicine and may be of interest to training programmes seeking greater opportunities for inter-professional education. Our approach to station development could be relevant for other HP trainees while implementing feedback and debriefing opportunities around the OSCE would maximise the opportunity for inter-professional interactions.
Limitations/practical context for this work
With only four stations, we cannot report on the reliability of the total scores. Reliability at the OSCE level is largely a function of adequately sampling across conditions of measurement (eg, measuring the same competency in 10 or 15 different contexts (stations), with different assessors and standardised patients for each context27). A second limitation of this study pertains to the rescoring of station 2 as there is a difference in the face-to-face scoring experience and video-based scoring.
There are challenges to implementing PS OSCEs as there is little space for ‘additional material’ in existing HP curricula. However, a high stakes PS OSCE could effectively drive what is taught and what is learned. Alternatively, the PS OSCE stations described could be embedded within existing OSCEs that measure aspects of socio-cultural competence, such as communication and teamwork.
Last, these OSCE cases surfaced the kinds of intimidating and obstructive negative behaviours that trainees routinely face in the clinical training environment and which shape a hidden curriculum that can threaten PS.32 Inclusion of a debriefing session in this socio-cultural PS OSCE would give learners a rare and rich opportunity to explicitly discuss negative aspects of the hidden curriculum. Without these kinds of opportunities, structural gaps in the curriculum that limit new graduates’ capacity to improve care and prevent errors are likely to persist.33
Conclusions
The OSCE is an underexplored methodology for assessing PS competencies. In this study, the OSCE assessed socio-cultural dimensions of PS based on realistic scenarios developed and reviewed by content experts. The scenarios were mapped to PS competencies and were applicable to both nursing and medicine. The station scores were highly reliable. Further, the score variation across stations and across nursing and medical students was appropriate. Of interest and still to be explored were the differences between nursing and medical student scores as it is unclear what factors would explain these differences. This study is the foundation for further work regarding the use of OSCEs for assessing competency in important socio-cultural dimensions of PS.
Supplementary Material
Acknowledgments
We would like to acknowledge and thank our case writers, case reviewers and assessors: Ms Heather Campbell, Maryanne D'Arpino, Laura Goodfellow, Alicia Papanicolaou; Drs Sean Clarke, David Ginsburg, David Goldstein, Philip Hebert, Lindsey Patterson, and Lynfa Stroud; as well as the medical and nursing students who participated in the OSCE. We also thank Dr Nishan Sharma for observing and providing feedback and we are grateful to Dr Arthur Rothman for various suggestions pertaining to assessment and analysis.
Footnotes
Contributors: LRG designed the study (including data collection tools and methods), monitored data collection, cleaned and analysed the data, and drafted and revised the paper. She is the guarantor. DT and PGN contributed to overall study design, data collection as well as revising and approving the manuscript. SS and IdV contributed to OSCE design and analysis, revising and approving the manuscript. SSS contributed to assessment and analysis, revising and approving the manuscript. EGV, ML-F and JM contributed to overall study design, revising and approving the manuscript.
Funding: This study was funded by a research grant from the Canadian Patient Safety Institute (CPSI), RFA09-1181-ON. CPSI did not play a role in the design, analysis, interpretation or write-up of the study.
Competing interests: None.
Ethics approval: The study received approval from the Human Participants Review Committee in the Office of Research Ethics at York University in Toronto and at Queen's University in Kingston (Health Sciences Research Ethics Board).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lucian Leape Institute. Unmet needs: teaching physicians to provide safe patient care. Boston: National Patient Safety Foundation, 2010. [Google Scholar]
- 2.Department of Health. Modernising medical careers. The new curriculum for the foundation years in postgraduate education and training. London, UK: Department of Health, 2007. [Google Scholar]
- 3.American Association of Colleges of Nursing. Hallmarks of quality and patient safety: recommended baccalaureate competencies and curricular guidelines to ensure high-quality and safe patient care. J Prof Nurs 2006;22:329–30. 10.1016/j.profnurs.2006.10.005 [DOI] [PubMed] [Google Scholar]
- 4.Cronenwett L, Sherwood G, Barnsteiner J, et al. Quality and safety education for nurses. Nurs Outlook 2007;55:122–31. 10.1016/j.outlook.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 5.Frank JR, Brien S; on behalf of The Safety Competencies Steering Committee. The safety competencies: enhancing patient safety across the health professions. Ottawa, ON: Canadian Patient Safety Institute, 2008. [Google Scholar]
- 6.Wong BM, Etchells EE, Kuper A, et al. Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med 2010;85:1425–39. 10.1097/ACM.0b013e3181e2d0c6 [DOI] [PubMed] [Google Scholar]
- 7.Ginsburg LR, Tregunno D, Norton PG. Self-reported patient safety competence among new graduates in medicine, nursing and pharmacy. BMJ Qual Saf 2013;22:147–54. 10.1136/bmjqs-2012-001308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ginsburg L, Castel E, Tregunno D, et al. The H-PEPSS: an instrument to measure health professionals’ perceptions of patient safety competence at entry into practice. BMJ Qual Saf 2012;21:676–84. 10.1136/bmjqs-2011-000601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Regehr G, Hodges B, Tiberius R, et al. Measuring self-assessment skills: an innovative relative ranking model. Acad Med 1996;71(10 Suppl):S52–4. 10.1097/00001888-199610000-00043 [DOI] [PubMed] [Google Scholar]
- 10.Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 2006;296:1094–102. 10.1001/jama.296.9.1094 [DOI] [PubMed] [Google Scholar]
- 11.Hodges B, Regehr G, Martin D. Difficulties in recognizing one's own incompetence: novice physicians who are unskilled and unaware of it. Acad Med 2001;76(10 Suppl):S87–9. 10.1097/00001888-200110001-00029 [DOI] [PubMed] [Google Scholar]
- 12.Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and research agenda. Acad Med 2005;80(10 Suppl):S46–54. 10.1097/00001888-200510001-00015 [DOI] [PubMed] [Google Scholar]
- 13.Battles JB, Wilkinson SL, Lee SJ. Using standardised patients in an objective structured clinical examination as a patient safety tool. Qual Saf Health Care 2004;13(Suppl 1):i46–50. 10.1136/qshc.2004.009803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salas E, Wilson KA, Burke CS, et al. Using simulation-based training to improve patient safety: what does it take?. Jt Comm J Qual Patient Saf 2005;31:363–71. [DOI] [PubMed] [Google Scholar]
- 15.Varkey P, Natt N. The objective structured clinical examination as an educational tool in patient safety. Jt Comm J Qual Patient Saf 2007;33:48–53. [DOI] [PubMed] [Google Scholar]
- 16.Pernar LI, Shaw TJ, Pozner CN, et al. Using an objective structured clinical examination to test adherence to Joint Commission National Patient Safety Goal--associated behaviors. Jt Comm J Qual Patient Saf 2012;38:414–18. [DOI] [PubMed] [Google Scholar]
- 17.Wagner DP, Hoppe RB, Lee CP. The patient safety OSCE for PGY-1 residents: a centralized response to the challenge of culture change. Teach Learn Med 2009;21:8–14. 10.1080/10401330802573837 [DOI] [PubMed] [Google Scholar]
- 18.Gupta P, Varkey P. Developing a tool for assessing competency in root cause analysis. Jt Comm J Qual Patient Saf 2009;35:36–42. [DOI] [PubMed] [Google Scholar]
- 19.Varkey P, Natt N, Lesnick T, et al. Validity evidence for an OSCE to assess competency in systems-based practice and practice-based learning and improvement: a preliminary investigation. Acad Med 2008;83:775–80. 10.1097/ACM.0b013e31817ec873 [DOI] [PubMed] [Google Scholar]
- 20.Daud-Gallotti RM, Morinaga CV, Arlindo-Rodrigues M, et al. A new method for the assessment of patient safety competencies during a medical school clerkship using an objective structured clinical examination. Clinics (Sao Paulo) 2011;66:1209–15. 10.1590/S1807-59322011000700015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh R, Singh A, Fish R, et al. A patient safety objective structured clinical examination. J Patient Saf 2009;5:55–60. 10.1097/PTS.0b013e31819d65c2 [DOI] [PubMed] [Google Scholar]
- 22.Kirkpatrick DL. Evaluation of training. In: Craig R, Bittel L, eds. Training and development handbook. New York: McGraw Hill, 1967:87–112. [Google Scholar]
- 23.Barr H. Competent to collaborate: towards a competency-based model for interprofessional education. J Interprof Care 1998;12:181–7. 10.3109/13561829809014104 [DOI] [Google Scholar]
- 24.Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65(9 Suppl):S63–7. 10.1097/00001888-199009000-00045 [DOI] [PubMed] [Google Scholar]
- 25.National Assessment Collaboration (NAC). http://mcc.ca/examinations/nac-overview/ (accessed 13 May 2014).
- 26.Regehr G, MacRae H, Reznick RK, et al. Comparing the psychometric properties of checklists and global rating scales for assessing performance on an OSCE-format examination. Acad Med 1998;73:993–7. 10.1097/00001888-199809000-00020 [DOI] [PubMed] [Google Scholar]
- 27.van der Vleuten CP, Schuwirth LW. Assessing professional competence: from methods to programmes. Med Educ 2005;39:309–17. 10.1111/j.1365-2929.2005.02094.x [DOI] [PubMed] [Google Scholar]
- 28.Brannick MT, Erol-Korkmaz HT, Prewett M. A systematic review of the reliability of objective structured clinical examination scores. Med Educ 2011;45:1181–9. 10.1111/j.1365-2923.2011.04075.x [DOI] [PubMed] [Google Scholar]
- 29.Hallgren KA. Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol 2012;8:23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213–20. 10.1037/h0026256 [DOI] [PubMed] [Google Scholar]
- 31.Cicchetti D. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 1994;6:284–90. 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- 32.Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med 1998;73:403–7. 10.1097/00001888-199804000-00013 [DOI] [PubMed] [Google Scholar]
- 33.Aron DC, Headrick LA. Educating physicians prepared to improve care and safety is no accident: it requires a systematic approach. Qual Saf Health Care 2002;11:168–73. 10.1136/qhc.11.2.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.