Abstract
Nontarget embolization is a relatively common cause of post-chemoembolization complications. Clinical presentation following nontarget embolization varies from minimal to fatal, and oftentimes relates to the vascular distribution embolized rather than the amount or type of embolic agent. Post-chemoembolization pancreatitis is an uncommon complication, but one that is known to occur. The following manuscript presents a case of post-chemoembolization pancreatitis, and suggests methods to decrease this complication as well as treatment once the complication occurs.
Keywords: interventional radiology, chemoembolization, embolization, complication, pancreatitis
Objectives: Upon completion of this article, the reader will be able to discuss the diagnosis and management of patients who develop post-TACE pancreatitis due to nontarget embolization.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Transarterial chemoembolization (TACE) is a well-established treatment modality used worldwide for unresectable hepatocellular carcinoma (HCC). Variations in medical history, tumor burden, clinical stage, and vascular anatomy result in variability in regard to risk profile and potential for complications. This case report depicts nontarget embolization with drug-eluting beads during TACE resulting in acute pancreatitis, a known but uncommon complication.
Case Report
A 59-year-old woman with a history of cirrhosis secondary to hepatitis C virus and alcohol abuse had been recently diagnosed with biopsy-proven multifocal HCC (Fig. 1). She was evaluated in the Interventional Radiology clinic and was deemed to be a good candidate for liver-directed therapy (Child-Pugh grade B, Eastern Cooperative Oncology Group performance status 1). TACE with drug-eluting beads (DEB-TACE) was performed in subselective fashion to the left lobe of the liver treating the dominant lesion in segment 3 and a smaller lesion in segment 4B without complication (Fig. 2). Follow-up imaging approximately 6 weeks later demonstrated a near-complete response to the dominant segment 3 lesion and a partial response to the segment 4B lesion (Fig. 3). The scan also revealed interval growth of a third lesion in the right hepatic lobe. The decision was made to repeat the procedure, focused on targeting the mass in segment 8 and to re-treat the lesions in the left hepatic lobe.
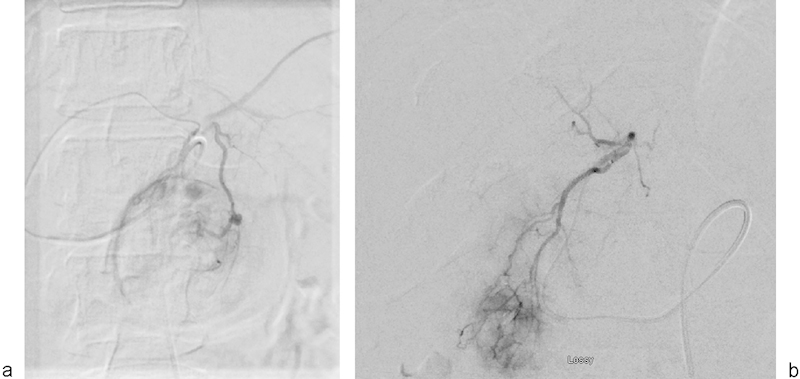
Fig. 1.

Arterial phase axial computed tomographic image through the liver demonstrates two hypervascular lesions within the left hepatic lobe (segments 3 and 4B) (arrows).
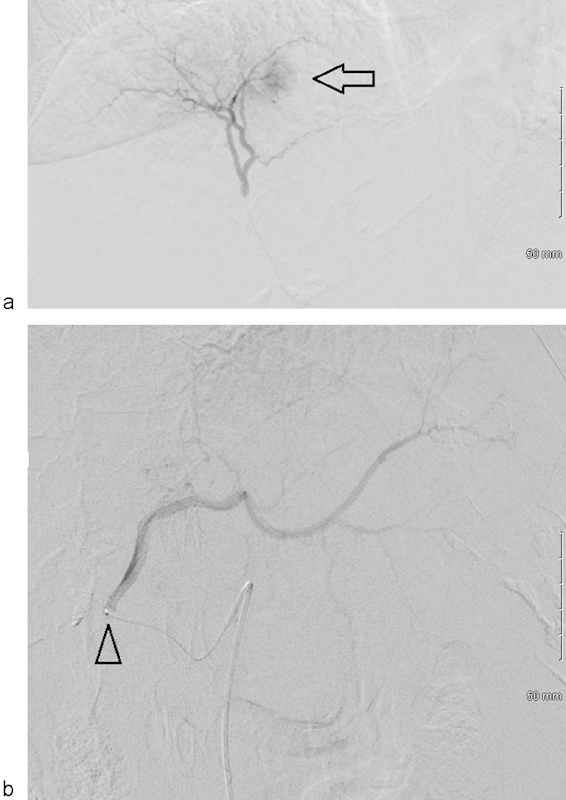
Fig. 2.
Digital subtraction angiography demonstrates tumor hypervascularity in segment 3 (a) and 4B (b).
Fig. 3.

Arterial phase axial computed tomographic images performed 6 weeks after transarterial chemoembolization demonstrate near-complete resolution of the segment 3 lesion (arrow) and persistent peripheral nodular enhancement of the segment 4B lesion (arrowhead).
During the second treatment session, the segment 8 lesion was treated subselectively. The two lesions in the left hepatic lobe were treated nonselectively with the tip of the catheter in the left main hepatic artery, and approximately 50 mg doxorubicin loaded on 100 to 300 micron LC beads (BTG International Ltd., London, United Kingdom) was instilled (Fig. 4). At the authors' institution, all patients are admitted after TACE for observation. This patient was admitted and oral narcotic pain medication and antiemetics were initiated. Overnight the patient developed worsening abdominal pain with increased nausea and vomiting. Physical exam revealed new abdominal distention, decreased bowel sounds, and severe epigastric pain with palpation.
Fig. 4.
Digital subtraction angiographic images taken during second session with DEB-TACE demonstrate tumor vascularity in segment 8 (arrow) (a). (b) Left main hepatic artery angiogram taken before the administration of drug-eluting beads (note the microcatheter position in proximal portion of the artery) (arrowhead).
Given concern for an acute surgical abdomen, laboratory tests were ordered and an abdomen/pelvis CT was performed that revealed findings consistent with acute pancreatitis (Fig. 5). The patient was treated with bowel rest and intravenous hydration and narcotics; she was discharged home in 72 hours without further adverse sequela.
Fig. 5.
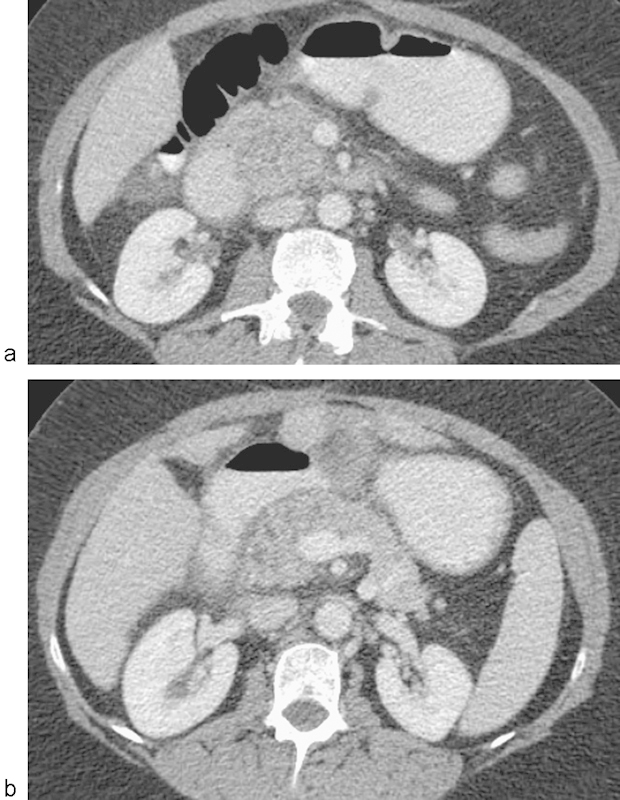
(a, b) Portal venous phase axial CT images through the pancreas demonstrate findings consistent with acute pancreatitis including focal enlargement and hypoattenuation of the pancreatic uncinate/head (edema), indistinct margins (inflammation), and surrounding retroperitoneal stranding.
Discussion
Acute pancreatitis is a known complication of TACE. Khan et al demonstrated up to 40% incidence of elevated serum pancreatic enzymes after nonselective (lobar) treatment of HCC with conventional TACE; however, none were symptomatic.1 The incidence of symptomatic acute pancreatitis after TACE is estimated at 2 to 4%,2 3 though the true incidence may be underestimated since mild acute pancreatitis could easily be misdiagnosed as postembolization syndrome given the overlap of symptoms between the two conditions. While most reported cases of acute pancreatitis after TACE resolve with medical management, fatalities have been reported.4 5 6 7 This underscores the importance of taking appropriate measures to avoid this complication, and to consider the diagnosis in a patient with abdominal pain after TACE.
Acute pancreatitis after chemoembolization is thought to result from pancreatic ischemia due to reflux of embolic material into pancreatic arterial branches. To avoid this complication, embolization should be performed with the catheter positioned as far distally into the branches supplying the tumor as possible, such that any refluxed embolic material is likely to end up in other hepatic arterial branches (which is generally well tolerated). In certain circumstances, however, it may be more appropriate to perform TACE from a lobar artery. In the case presented here, the patient experienced only a modest response to initial selective treatment of the segment 4B tumor; one possible explanation for the suboptimal response was that there were other branches supplying the tumor that were too small to catheterize, a problem that might be overcome by treating from the lobar artery. Additional advantages of a lobar approach to treatment in this case include simultaneous coverage of the other left lobe tumor, and reduction in fluoroscopy time and contrast in a patient who was already undergoing treatment of a right lobe tumor during the same session.
In patients with a long proper hepatic artery, reflux of embolic material from one lobar hepatic artery is most likely to embolize to the other lobar hepatic artery. However, in this case the patient's common hepatic artery essentially trifurcates into right and left hepatic arteries, and the gastroduodenal artery (Figs. 6 and 7); such anatomy makes refluxed embolic material from the left hepatic artery equally likely to end up in the right hepatic artery and the gastroduodenal artery. Thus, this patient's anatomy put her at particularly high risk for the development of acute pancreatitis after TACE due to inline flow from the common hepatic artery to the gastroduodenal artery to the superior pancreaticoduodenal artery. Having made the decision to perform left lobar TACE, the catheter should have been positioned further into the left hepatic artery, and given the risk of reflux into the gastroduodenal artery, embolization should have been meticulously monitored under fluoroscopy to ensure that reflux was detected as early as possible. The most conservative approach, which may have been reasonable in this particular instance, would have been to empirically embolize the gastroduodenal artery near its origin prior to performing left lobar TACE.
Fig. 6.
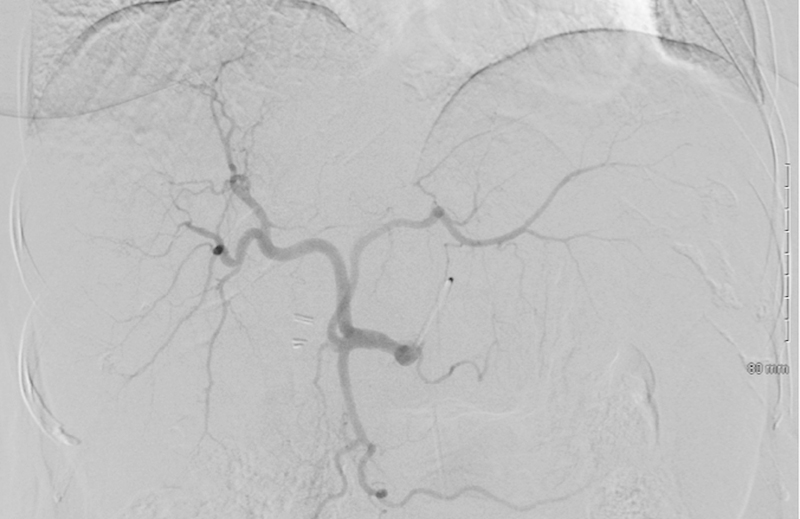
Common hepatic arteriogram demonstrating trifurcation into left hepatic, right hepatic, and gastroduodenal arteries. This anatomy puts patient at high risk for reflux from the left hepatic artery into the pancreatic arterial supply.
Fig. 7.
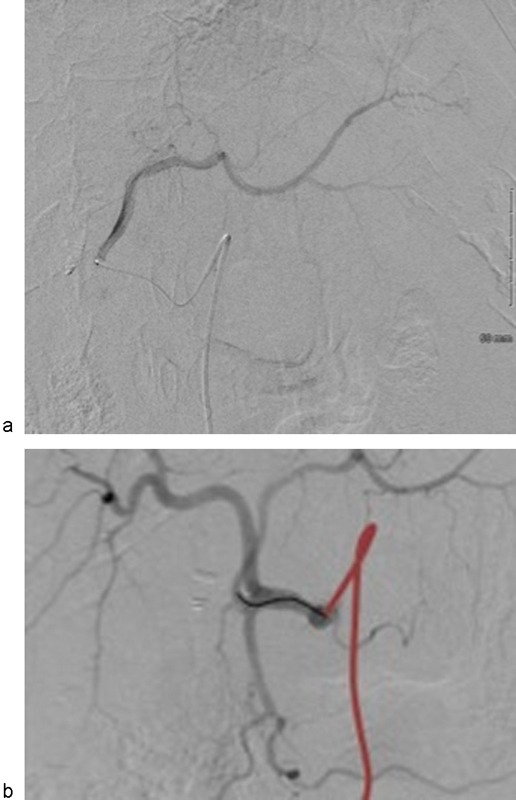
(a) Left hepatic arteriogram prior to TACE from the left hepatic artery. (b) Common hepatic arteriogram with red marking position of base catheter and black marking position of microcatheter during chemoembolization of the left hepatic lobe.
Fortunately, this case of acute pancreatitis complicating DEB-TACE was mild and self-limited. However, it serves as a reminder of this uncommon but potentially life-threatening complication of TACE, which should be kept in mind when planning the procedure and when following patients postprocedure.
References
- 1.Khan K N, Nakata K, Shima M. et al. Pancreatic tissue damage by transcatheter arterial embolization for hepatoma. Dig Dis Sci. 1993;38(1):65–70. doi: 10.1007/BF01296775. [DOI] [PubMed] [Google Scholar]
- 2.López-Benítez R, Radeleff B A, Barragán-Campos H M. et al. Acute pancreatitis after embolization of liver tumors: frequency and associated risk factors. Pancreatology. 2007;7(1):53–62. doi: 10.1159/000101878. [DOI] [PubMed] [Google Scholar]
- 3.Ozçinar B, Güven K, Poyanli A, Özden I. Necrotizing pancreatitis after transcatheter arterial chemoembolization for hepatocellular carcinoma. Diagn Interv Radiol. 2009;15(1):36–38. [PubMed] [Google Scholar]
- 4.Komekado H, Kokuryu H, Kimura T. et al. Two cases of acute necrotizing pancreatitis complicating after transcatheter arterial embolization for hepatocellular carcinoma. J Gastroenterol. 2005;40(1):107–108. doi: 10.1007/s00535-004-1503-x. [DOI] [PubMed] [Google Scholar]
- 5.Rodríguez-Grau M C, Jusué V, Fiera A, Castaño C, García-Buey L C. Acute pancreatitis as fatal complication after chemoembolization of hepatocellular carcinoma. Rev Esp Enferm Dig. 2014;106(2):146–147. doi: 10.4321/s1130-01082014000200013. [DOI] [PubMed] [Google Scholar]
- 6.Addario L, Di Costanzo G G, Tritto G, Cavaglià E, Angrisani B, Ascione A. Fatal ischemic acute pancreatitis complicating trans-catheter arterial embolization of small hepatocellular carcinoma: do the risks outweigh the benefits? J Hepatol. 2008;49(1):149–152. doi: 10.1016/j.jhep.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 7.Nawawi O, Hazman M, Abdullah B. et al. Transarterial embolisation of hepatocellular carcinoma with doxorubicin-eluting beads: single centre early experience. Biomed Imaging Interv J. 2010;6(1):e7. doi: 10.2349/biij.6.1.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]


