Abstract
Objective
This study evaluated the efficacy of a targeted social skills training group in school-aged children with autism spectrum disorder (ASD). The intervention, NETT (Nonverbal communication, Emotion recognition, and Theory of mind Training), is a 12-session cognitive-behavioral intervention (CBI) for verbal, school-aged children targeting ASD-specific social behavioral impairments.
Method
Sixty-nine children with ASD, 8 to 11 years of age with verbal IQs greater than 70, participated in a randomized comparative trial to examine the efficacy of NETT relative to a facilitated play group. Treatment outcomes included caregiver reports of social behavior and neuropsychological assessments of social cognition conducted by blinded raters. Outcomes were collected at baseline, endpoint, and three months posttreatment.
Results
Significant improvements were found on social behavior outcomes such as nonverbal communication, empathic responding, and social relations in the NETT condition relative to the active control at endpoint. Verbal IQ and age moderated the interaction effect on social behavior with higher verbal IQ and older age associated with improvements in the CBI condition. No significant improvements were found on social cognitive outcomes. No significant group differences were found at three-month follow-up conducted with approximately half the sample (n=34).
Conclusion
These data indicate that targeted CBI social skills groups such as NETT improve social communication deficits in verbal, school-aged children with ASD. The moderating effects of high verbal IQ suggest a need to consider participant and treatment characteristics associated with outcomes in future studies.
Keywords: social skills groups, autism, social cognition, cognitive behavioral intervention, social-communication
INTRODUCTION
Socialization groups are a widely used modality for addressing core social impairments in verbal, school-aged and older individuals with autism spectrum disorder (ASD). Socialization groups hold appeal as a cost-effective method to facilitate social contact for those at increased risk for social isolation and rejection1,2. In addition, empirical support is building for cognitive-behavioral intervention (CBI) approaches such as social skills training (SST) groups for verbally fluent, school-aged children with ASD3. Notable methodological advances are represented in a few recent studies, including use of randomized controlled trials (RCTs), manualized interventions, standardized outcomes, and fidelity checks4. However, several reviews3–5 point to methodological limitations that question recent practice recommendations, which suggest that SST groups are evidence-based interventions in ASD6,7. Specifically, existing research fails to meet core design criteria for evaluating treatment efficacy such as use of adequate sample sizes, active treatment controls, independent outcome evaluations, and data on maintenance and generalization.
The use of waitlist controls in RCTs8–13 is a particular hurdle for evaluating treatment efficacy of SST groups. Parents report high levels of satisfaction across models including interest-based social clubs, leisure activities groups, supportive play (e.g., board games), as well as CBI-based SST groups11,14. In addition to methodological and ethical concerns associated with waitlist controls, the efficacy of therapeutic SST group models must be demonstrated against less costly recreational social group models. From an implementation perspective, the use of active treatment controls will inform the selection of optimal modalities (e.g., skills-based, recreational) and providers (e.g., clinicians, paraprofessionals, peers). From a treatment development perspective, active treatment controls are needed to guide research on mechanisms and common factors associated with outcomes.
To date, three randomized comparative trials have been reported in the literature15–17. Small samples (n<14) and limited effects in two comparative trials limit interpretation due to underlying assumptions of randomization and statistical models16,17. DeRosier et al. conducted the largest comparative trial in 55 youths with ASD between the ages of 8–12 years15. The study evaluated the efficacy of S.S.GRIN, a 15-session CBI curriculum with empirical support for youth with emotional and learning disorders, relative to a modified version for children with “high-functioning autism” (S.S.GRIN-HFA). Significant group differences were found on the Social Responsiveness Scale (SRS) and measures of perceived self-efficacy. However, caregivers in the unmodified S.S.GRIN group reported an exacerbation of ASD symptoms and reduced feelings of self-efficacy, which requires further exploration given high parental satisfaction reported in other SST studies11,12.
Comparison across SST group studies in ASD is also complicated by variability in outcome measures and treatment targets. Social communication impairments in ASD are developmentally specific and may be associated with cascading effects on other social and mental health domains. Published curricula target social impairments found across social-emotional learning disabilities such as listening skills, friendship skills, and assertiveness training9,10. Other studies emphasize ASD-specific impairments in social communication and social cognition8,12–14,16–21; while still others take a broad-based approach including both general and ASD-specific impairments, like S.S.GRIN-HFA15.
Targeted interventions for core social-communication impairments are of particular interest given the dearth of treatments for core deficits in older children and individuals with ASD. Baghdadli et al. conducted a randomized comparative trial of a 20-session social cognitive intervention targeting nonverbal communication, emotion recognition, stress management, and theory of mind in 14 children with ASD17. While no differences were found in total face recognition scores on the Diagnostic Analysis of Nonverbal Accuracy 2 (DANVA2)22, the targeted social cognitive intervention was associated with improvements in identification of low-intensity (i.e. difficult to identify) adult emotions and quality of life outcomes relative to the active treatment control. However, as previously noted, small sample sizes limit interpretation of findings from this trial.
This study builds upon prior research by addressing methodological weaknesses limiting interpretation of efficacy of targeted, social cognitive skills training groups. In this study, we evaluated the efficacy of a targeted, 12-session, CBI SST group curriculum: NETT (Nonverbal communication, Emotion recognition, and Theory of mind Training). NETT utilizes targeted and top-down processing approaches characteristic of CBI similar to recently published reports of targeted social cognitive curricula12,17,20. The current study uses a randomized comparative design, manualized interventions, fidelity checks, and theoretically based outcomes to evaluate treatment efficacy. The study evaluated dual treatment targets associated with ASD and social learning, specifically, social cognition and social behavior. Treatment moderators were evaluated to help inform a more personalized approach to social skills interventions in ASD. Baseline participant characteristics including verbal abilities, age, and psychiatric comorbidities were evaluated as potential variables associated with treatment response. Moderator analyses may also inform sample selection for future studies seeking to constrain heterogeneity in this treatment area23. Given that maintenance data is rarely reported, but greatly needed4, this study includes a three-month follow-up evaluation in a subset of participants to estimate durability of treatment effects.
METHOD
Randomization and Study Procedures
This study employed a randomized parallel group design comparing 1) NETT and 2) facilitated play (control condition). Participants were recruited in seven phases between January 2008 and March 2012. Allocation to conditions was determined by computer-generated randomization in blocks of 10–12 for each recruitment phase. Assessments were conducted at baseline and endpoint (12 weeks). Funding to collect maintenance data was obtained during the trial and was available for participants in cycles 4–7. Behavioral outcomes included blinded neuropsychological assessments of social cognition and caregiver reports of social behavior. In addition, a subset of children also participated in secondary and exploratory outcome evaluations, including functional magnetic resonance imaging (fMRI) tasks of emotion processing and perspective taking, direct observation during unstructured playtime, and generalization probes with unfamiliar peers. These evaluations will be presented in subsequent reports.
Participants
Potential participants were recruited from community agencies, local practitioners, and advertisements. A total of 87 families signed consent between January 2008 and March 2012 to participate in the trial. Inclusion criteria were as follows: 8- to 11-year-old children with a diagnosis of ASD and a verbal IQ score of > 70. Diagnosis was established using DSM-IV24 criteria (clinical interview), Autism Diagnostic Observation Schedule (ADOS, Module 3)25, and the Autism Diagnostic Interview-Revised (ADI-R)26. A clinical history, diagnostic testing, and standardized IQ tests were undertaken at screening. Exclusion criteria were as follows: initiation of new psychiatric medication within 30 days prior to screening, known gross structural abnormalities in the brain, active seizure disorder, and aggression towards others. Of 87 families who signed consent, 18 did not get randomized for the following reasons: failure to meet study inclusion criteria, group scheduling conflicts, or inability to complete the first fMRI scan. Informed consent was obtained from all caregivers and assent was obtained from all child participants. This study was approved by the Mount Sinai Program for the Protection of Human Subjects.
Figure 1 provides a flowchart illustrating participant movement through the trial. Sixty-nine participants were randomized to one or the other intervention and 66 participants completed the intervention. From the total sample (N=69), 38 participants enrolled in cycles 4–7 were eligible for participation in the three-month maintenance evaluation and 34 participants completed the maintenance evaluation.
Figure 1.
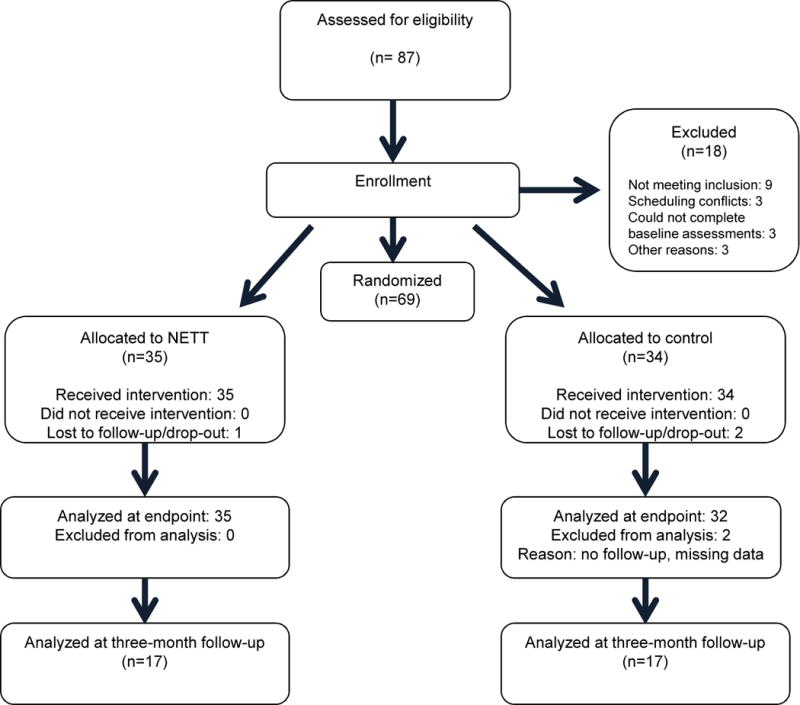
Consolidated Standards of Reporting Trials (CONSORT) diagram.
Participant characteristics are presented in Table 1. T-tests were conducted on demographic and outcome variables. There were no significant differences between treatment groups on outcome variables or moderators at baseline. Ethnicity data from caregiver reports highlight enrollment of an ethnically diverse sample: 43% White, 21% Black, 26% Hispanic, 1% Asian, and 9% Other.
Table 1.
Baseline Participant Characteristics
| Characteristic | NETT (n=35) | Facilitated Play (n=34) | p |
|---|---|---|---|
| Age in years (M, SD) | 10.05 (1.27) | 9.87 (1.32) | .57 |
| Full Scale IQ (M, SD) | 94.86 (17.34) | 93.72 (16.79) | .79 |
| Verbal IQ (M, SD) | 97.91 (16.70) | 96.44 (15.20) | .70 |
| Nonverbal IQ (M, SD) | 100.5 (18.22) | 98.97 (16.11) | .71 |
| Sex (n, % male) | 30 (85.7) | 27 (84.38) | .88 |
| Vineland Adaptive Behavior Composite (M, SD) | 80.25 (11.28) | 79.63 (9.14) | .81 |
| ADOS Module 3 Overall Total (M, SD) | 12.25 (4.36) | 10.41 (4.67) | .12 |
| SRS Total Score (M, SD) | 94.62 (24.31) | 96.41 (25.93) | .77 |
| BASC-2 Behavior Symptoms Index (M, SD) | 68.15 (9.79) | 70.90 (10.74) | .28 |
| BASC-2 Hyperactivity T-score (M, SD) | 63.85 (13.90) | 67.00 (12.21) | .34 |
| BASC-2 Anxiety T-score (M, SD) | 57.21 (10.48) | 58.74 (12.19) | .59 |
| Social cognition composite (M, SD) | 0.15 (.84) | −0.18 (.79) | .10 |
| Social behavior composite (M, SD) | −0.04(1.01) | 0.05 (.70) | .67 |
Note: ADOS = Autism Diagnostic Observation Schedule; BASC-2 = Behavior Assessment System for Children, Second Edition; NETT = Nonverbal communication, Emotion recognition, and Theory of mind Training; SRS = Social Responsiveness Scale.
Therapists and Treatment Fidelity
Intervention groups were led by licensed clinical psychologists with a minimum of three years of experience working with children with ASD. Each group also included two therapy assistants trained in the respective treatment model by lead therapists. Therapists delivered either the CBI or control treatment and were not shared between conditions. In addition, weekly supervision was provided for each treatment team led by the lead therapist. A total of three lead therapists and 16 assistant therapists provided interventions across the seven group cycles.
Treatment fidelity ratings were conducted by three, sequential, independent raters blinded to study hypotheses and not involved in treatment delivery. Treatment fidelity checklists were developed from each treatment manual. Fidelity was measured using dichotomous ratings (yes/no) reflecting implementation of critical treatment components. In addition, non-specific therapeutic factors were measured including: 1) therapist use of positive affect, 2) children’s comfort level, and 3) therapeutic alliance. Raters achieved 80% reliability prior to coding. Reliability was collected on live or videotaped sessions for approximately 40% of sessions with feedback provided to lead therapists during the intervention. Fidelity was maintained in both groups with an average of 97.4% and 97.9% of program elements followed in the NETT and control condition respectively. Ratings for non-specific or common factors ranged from 1=poor to 4=excellent. Average scores reflected good to excellent ratings on common factors (range = 3.4–3.6) and did not differ between conditions.
Interventions
Children in both groups received the same course of intervention consisting of 12 90-minute weekly sessions, which included a child therapy group and a concurrent parent group. Both child therapy groups included a 15-minute free-play/snack time, 60-minute instruction, and 15-minute wrap-up/circle time. Groups consisted of 4 to 6 children with ASD and 2 to 3 therapists to maintain a 2:1 child to therapist ratio. For both treatments, Session 1 was an introductory group (e.g. ice-breaker games, orientation to the group rules/structure) and Session 12 was a wrap-up/party. Sessions 2–11 differed based on treatment condition.
NETT
A modular CBI-based social skills curriculum for children with ASD ages 4 to 12 was developed in an outpatient autism treatment program over a five-year period. Open-label data was collected on fidelity, outcomes, and therapist satisfaction, which led to modifications of the study protocols and manuals during the development phase. Three developmentally progressive modules targeting autism-specific social cognitive impairments were selected for NETT: nonverbal communication, emotion recognition, and theory of mind. The CBI curriculum drew from a variety of sources to structure approach and activities including skillstreaming27, social skills training28, relationship development intervention,29 and thought bubbles30. Table 2 provides a detailed overview of sessions and activities outlined in the NETT treatment manual.
Table 2.
Nonverbal Communication, Emotion Recognition, and Theory of Mind Training (NETT) Curriculum Overview
| TOPIC | SESSIONS | SAMPLE STRATEGIES, GAMES, and ACTIVITIES |
|---|---|---|
| Introductions, rules, format | Session 1 | Icebreakers, introduction to schedules, token economy |
| Nonverbal Communication: “Talking without words” | Sessions 2–5 | Receptive and expressive gestural communication; Charades, Miming, “I spy,” “buddy walkers”29 |
| Emotion Identification: “Feelings” | Sessions 6–8 | Visual discrimination (pictures, videos, in vivo), Charades, intensity ratings, emotion words, role-plays (e.g. ID and reactions) |
| Theory of Mind: “I think, you think” | Sessions 9–11 | Thought bubbles,30 picture books, idioms, metaphors |
| End of group party | Session 12 | Review homework, provide summary of activities, awards ceremony, party |
Each of the three target skills (nonverbal communication, emotion recognition, and theory of mind) was described in the treatment manual with instructions for therapists, outlines for child and parent group activities, and suggestions for individualization. Instructional strategies included visual supports, didactic instruction, activities to reinforce target skills (e.g. role plays, games), weekly skills practice (2 to 3 times/week), and a token economy system to reinforce target skills and group participation. The 30-minute parent education group provided the rationale for target skills, homework review, and discussion of challenges/barriers.
Control Condition: Facilitated Play
A treatment manual for the control condition was developed to provide a supportive environment for children with ASD participating in a social group setting. The treatment manual described methods to tailor child-directed play based on the interests and abilities of group members. Therapists established “stations” to support object play (e.g., Legos, board games), motor/tactile (e.g., drawing), and dramatic play. The treatment manual also provided instruction on use of reflective statements to foster communication with the child and between peers. Each group session began with a review of a posted visual schedule, a check-in circle, activity time, and wrap-up. The 30-minute concurrent parent group was supportive in nature and facilitated by the lead therapist.
Measures
This study sought to measure effects from NETT on the dual treatment outcomes of social cognition and social behavior at study endpoint. In addition, maintenance of treatment effects was assessed in approximately half the sample at a three-month follow-up interval.
Treatment Outcomes: Social Behavior
Caregiver report measures of social behavior impairments associated with ASD were collected on the following measures: Social Responsiveness Scale (SRS)31, Griffith Empathy Measure32, and Children’s Communication Checklist-2 (CCC-2)33. Each treatment condition required caregiver participation, and thus ratings were unblinded. The Social Responsiveness Scale31 is a 65-item rating scale that is used to evaluate the presence and extent of social impairment associated with ASD. The caregiver version of the SRS was used in this study to measure the presence of social symptoms in natural settings. The Griffith Empathy Measure32 is a 23-item caregiver rating scale that assesses both affective and cognitive empathy in children and adolescents. The measure was adapted from Bryant’s Index of Empathy34 by Dadds et al. The CCC-233 is a 70-item caregiver rating scale which includes language scales (e.g., speech, syntax) and pragmatic scales (e.g., scripted language, nonverbal communication, social relations).
Treatment Outcomes: Social Cognition
Direct neuropsychological assessments of social cognition were conducted by blinded, trained raters at baseline, endpoint, and maintenance (three-month follow-up). Assessments included the Diagnostic Analysis of Nonverbal Accuracy-2 (DANVA2)22, Strange Stories Task35, and the Reading the Mind in the Eyes Test (RMET)36. The DANVA2 examines emotion recognition using both visual and auditory stimuli. Participants were administered all subtests of the DANVA2. The Strange Stories test37 is a measure of social understanding that assesses an individual’s ability to understand nonliteral statements within stories. This study utilized the revised version of the test as developed by Brent and colleagues35. The RMET36 examines an individual’s ability to determine what a person is thinking or feeling based on photographs of the eye region of male and female faces. The child and adolescent version of the Eyes Test was used in this study.
Moderators of Treatment Effects
Participant characteristics used in the moderator analysis included chronological age, verbal abilities, ASD symptoms, and comorbid mental health conditions. Verbal abilities were measured by verbal IQ composite scores, and ASD severity was measured by the SRS total. Moderating effects of anxiety and attention-deficit/hyperactivity disorder (ADHD)38 were evaluated using subscales from the Behavior Assessment System for Children, Second Edition (BASC-2)39 parent rating scales.
Social Validity
A 10-item parent satisfaction measure was developed for the study and collected on participants enrolled in cycles 4–7. The parent satisfaction measure included seven questions answered on a seven-point Likert scale with higher numbers associated with more positive ratings. Questions in the satisfaction survey probed parent/caregivers about their overall satisfaction with their child’s improvement, therapists, therapy, and research experience, as well as three open-ended questions about experiences in the intervention study.
Statistical Analysis
Principal Components Analysis: Treatment Outcome Measures
The primary aim of this study was to assess change in two targeted social learning constructs: social cognition and social behavior. Principal components analyses (PCA) was used to create composite scores for each construct and reduce the number of type-I errors associated with modeling many tests separately. In addition, composite scores provide means for reducing measurement errors related to floor/ceiling artifacts and variability in response. The analytic approach was adapted from neurocognitive research in Alzheimer’s disorder and provides a method for establishing empirically and theoretically based summary indices from multiple measures when commonly accepted measures is not available40,41. Composites were developed in a three-step process. First, missing, invalid, and/or incomplete data (i.e. more than 30% items missing when not predefined by scale) were excluded. Second, we entered raw scores for the subscales of each measure to develop empirically based groupings. Third, variables with high (>.50) and single, positive, significant loadings (i.e., >.3 on no more than one factor) were retained. The final analysis retained 99% and 93% of participants for the social cognition and social behavior composite analysis respectively.
Social Behavior Composite
The PCA for the social behavior composite included 16 scales from the SRS, CCC-2, and the Griffith Empathy Measure. Promax rotation was conducted and yielded four factors (see Supplemental Table 1, available online). Factor 1, social behavior impairments, explained 46% of the variance in scores. After omitting subscales loading onto more than one factor, the top three subscales loading on Factor 1 remained. The resulting composite included the following tests/subscales: CCC-2 social relations, CCC-2 nonverbal, and Griffith Empathy Scale total.
Social Cognition Composite
The social cognition composite included raw score totals from the DANVA2, RMET, and Strange Stories mentalizing scale. The three scales were maintained in a single factor structure, and thus no rotations were conducted. The final social cognition composite used total scores from the three scales and explained 52% of the variance.
Treatment Effects
Separate general linear mixed models (SAS/STAT software, version 9.4) were conducted on social cognition and social behavior composite scores derived from the factor analysis. Mixed models were used to examine the longitudinal effect of treatment conditions on outcome variables and the moderation analysis. Analyses included data for all participants who had at least two time points with valid data. Variables examined for moderation effects included: 1) chronological age, 2) verbal IQ, 3) SRS total, 4) BASC-2 anxiety subscale raw score and 5) BASC-2 hyperactivity subscale raw score. Each moderator was entered separately into models as a continuous variable. Evaluation of moderation effects on maintenance of treatment gains was limited because of the reduced sample size at the three-month follow-up.
RESULTS
Treatment Effects: Social Behavior and Social Cognition at Endpoint
Table 3 shows the results of the linear mixed models analysis for the outcome measures. NETT resulted in significant improvements on the social behavior composite compared to the active control condition (p=.04, see Figure 2A, Supplemental Table 2, available online). Effect size calculations indicate a large effect for NETT (Cohen’s d = .88) relative to control (Cohen’s d = .12) at week 12. However, these effect sizes should be interpreted with caution given the potential to overestimate effects in small studies with large standard errors23.
Table 3.
Effects of Time, Group, and Participant Characteristics on Social Behavior and Social Cognition as Estimated From Mixed Models
| Social Behaviora | Social Cognitionb | |||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
| Time 1 (endpoint, N=67) | −0.05 | .11 | .62 | 0.12 | .09 | .22 |
| Group × Time 1 | −0.31 | .14 | .04* | 0.00 | .13 | .98 |
| Time 2 (three-month follow-up, n= 34) | −0.11 | .14 | .45 | .15 | .12 | .21 |
| Group × Time 2 | −0.14 | .19 | .47 | −0.17 | .17 | .31 |
| Added in separate models | ||||||
| Group × Time 1 × Verbal IQc | −0.02 | .01 | .03* | −0.00 | .01 | .82 |
| Group × Time 1 × Chronological Age | −0.22 | .11 | .05 | .03 | .10 | .73 |
| Group × Time 1 × SRS Total | −0.01 | .01 | .25 | 0.00 | .01 | .45 |
| Group × Time 1 × ADHD index | −0.01 | .03 | .60 | 0.03 | .02 | .25 |
| Group × Time 1 × Anxiety index | −0.02 | .02 | .33 | 0.03 | .02 | .21 |
Note: ADHD = attention-deficit/hyperactivity disorder; SE = standard error; SRS = Social Responsiveness Scale.
Social behavior impairment composite related to improvements in social relationships, nonverbal communication, and empathy.
Higher social cognition composite scores indicate improvement in neuropsychological assessments of emotion recognition and perspective taking.
Each moderator was entered into separate analyses.
Indicates statistically significant findings from linear mixed models (p<.05)
Figure 2.
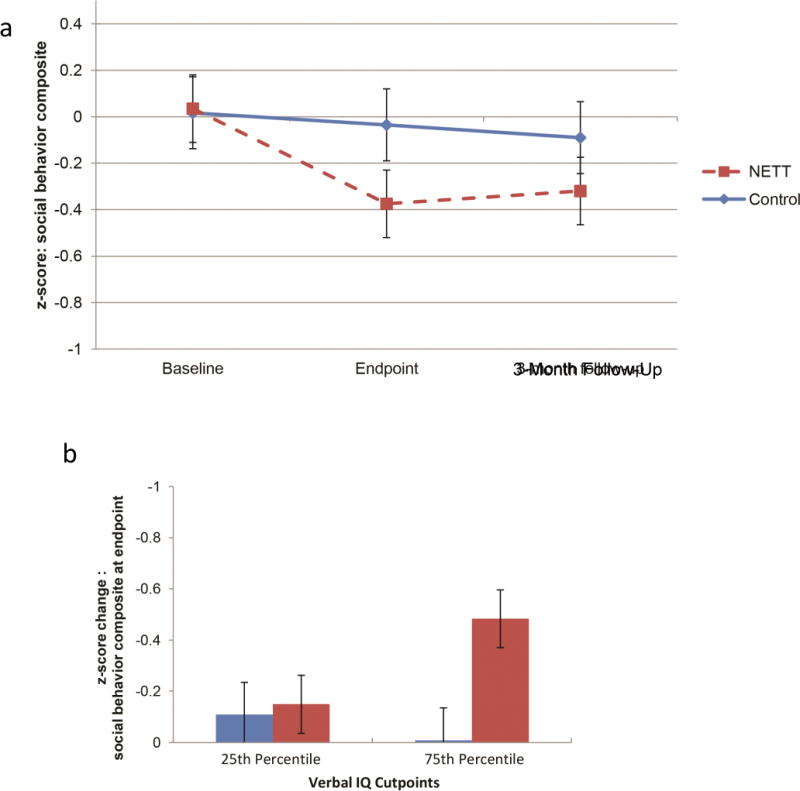
A. Improvement in social behavior impairments. Note: Interaction effect for Nonverbal communication, Emotion recognition, and Theory of mind Training (NETT) relative to active treatment control showing mean social behavior composite score and standard error (SE) at baseline, endpoint, and follow-up. B. Verbal IQ moderates improvement for NETT. Note: Change in social behavior composite (z score and SE) is shown at the 25th and 75th percentiles of verbal IQ (verbal IQ = 85 and 106, respectively).
There was no significant interaction effect on the social cognition composite at endpoint (week 12). Based on previous findings17, post hoc analyses were conducted on low-intensity (i.e., difficult) items on the DANVA2 to evaluate potential signals of effects in the social cognitive domain. Post hoc analyses suggest greater improvements for NETT compared to the comparison group across individual social cognitive measures, with significant improvements on identification of emotions on low-intensity child faces on the DANVA2 compared to controls (estimate =1.1, p<.01, Cohen’s d = .56).
Three-Month Follow-Up
Table 3 also presents data on 34 participants included in the analysis at the three-month follow-up interval. Linear mixed-model analyses indicate no significant interaction effect at the follow-up interval on social behavior (p=.38) and social cognition composites (p=.79).
Moderators of Treatment Effects
Figure 2B shows the moderating effect of verbal IQ on social behavior outcomes at endpoint (week 12). Higher verbal IQ scores were associated with greater change in social behavior composite for the NETT condition but not the control condition. Verbal IQ did not moderate group × time effects on the social cognition composite (Table 3). Age approached significance as a moderator of social behavior outcomes, with older age associated with improvement in social behavior impairments in the NETT group (p=.053). SRS total, and the anxiety and ADHD subscales from the BASC-2, were not significantly associated with change for either social cognition or social behavior composites.
Social Validity
Twenty-four parents of 38 eligible participants completed ratings on the survey measure of parental satisfaction with intervention. The mean total satisfaction rating was 5.66 (SD = 1.36, range = 2), which indicates a moderate to high level of satisfaction with allotted interventions. A t-test was conducted to evaluate group differences in overall satisfaction ratings. No group differences were found on a total satisfaction score reflecting satisfaction with improvement in social skills, therapist qualities, and research procedures (p=.163).
DISCUSSION
This study was designed to evaluate the efficacy of NETT, a targeted SST group for nonverbal communication, emotion recognition, and mentalizing impairments in verbally fluent, school-aged children with ASD. This study utilized a robust trial design with controls for non-specific therapy variables including treatment duration, intensity, therapist variables, and settings. Results supported improvements on social behavior impairments associated with ASD following the 12-session intervention.
Results of this study are consistent with a growing body of literature indicating positive effects of SST groups on pro-social behavior in school-aged children with ASD. A Cochrane review3 indicates a medium effect size for SST groups compared to waitlist controls on measures of social competency (e.g., Social Skills Rating System, SRS) and small effects on emotional recognition measures. The impact of SST groups on social competency is encouraging, considering the positive associations between social competency, adjustment, and mental health in typically developing children42.
The role of developmental variables on outcomes in this trial has implications for targeting subgroups who may optimally respond to this treatment approach. Higher verbal IQ was significantly associated with improvements on social behavior impairments, and older age approached significance as a moderator of social behavior outcomes for NETT only. Study inclusion criteria limited enrollment to children with ASD and verbal IQ scores greater than 70 given the role of verbal mediation in facilitating behavior change in CBI. Results suggest a higher threshold for verbal processing skills associated with outcomes from targeted CBI-based SST groups in school-aged children with ASD. In addition, other mechanisms may also be considered, including developmental readiness (i.e., prerequisites) for target skills and aspects of pragmatic communication not captured under the gross measure of verbal abilities used in this trial.
Behavioral improvements in the absence of significant movement in cognitive targets challenge assumptions of underlying mechanisms in targeted CBI for social skills in ASD. CBIs presume a fluid relationship between the cognitive, behavioral, and environmental processes during socialization in typical development (i.e., social learning theory and reciprocal determination43). Data from this and other studies suggest a need for further research on social learning mechanisms in school-aged children with ASD. Should CBI facilitate behavioral rehearsal in the absence of cognitive effects, strategies to enhance social cognitive targets (e.g., medication augmentation or computer training program) may be investigated as a means to optimize learning and improve durability of treatment effects.
Despite non-significant effects on global social cognitive scores, post hoc analyses of difficult items suggested improvements in low-intensity child facial expressions of emotion on the DANVA2 in NETT relative to controls. Results from Baghdadli et al.17 and Thomeer et al.13 also suggest improvements in identification of subtle emotional expressions within longer-term (e.g., 6-month) social cognitive skills group models. Taken together, findings support a need to further interrogate social cognitive outcomes in targeted CBI interventions. Future research may incorporate measures with higher ceilings (e.g., dynamic faces) and/or refined social cognitive targets (e.g., reward, saliency) and help guide the treatment development pathway for this undertreated symptom domain.
This study is the largest randomized comparative trial of a social cognitive skills training group in a well-characterized, ethnically diverse sample of school-aged children with ASD. The study also contributes to data on moderators and maintenance of treatment effects from targeted CBI social skills approaches. The study evaluated two treatment targets presumed to underlie effects of CBI-based socialization interventions. Results support prior findings of effects on social behavior but not cognition. Our approach was also limited by design and measurement challenges including a potentially underpowered evaluation of maintenance (n=34), which impacts interpretation of treatment durability. Data from this study indicate approximately half the gains made in NETT were not maintained at three months post-intervention. While larger sample sizes are needed to further assess treatment durability, results support two available studies suggesting limited maintenance of SST group treatment effects after active treatment periods19,44. Outcome measures reflecting generalization and clinically significant markers of improvement (e.g. friendships, social integration) were also limited in this study. Exploratory, observational measures of generalization were collected and may provide indications of generalization in clinical settings in subsequent analyses. In addition, the reliance on unblinded parent report for measuring social behavior outcomes is a particular challenge in social skills intervention research and for this study. Parents in both conditions reported moderate to high levels of satisfaction with no detected differences in the subset of participants with social validity data. Furthermore, the trial used independent raters to evaluate fidelity and quality of both intervention conditions. Data reflected positive ratings of therapist, child, and alliance variables in both conditions. Nevertheless, unmeasured aspects of expectancy may play a role and should be mitigated in future research through exploration of objective, blinded assessments of behavioral outcomes.
The main findings from this study suggest promise for prescriptive approaches to psychosocial interventions, such as Seaver-NETT, to improve core social-communication behaviors in verbal, school-aged children with ASD. Results also provide directions for future research on targeted CBI interventions for the growing population of children with ASD without intellectual disability45. In this partial follow-up sample, group differences were no longer significant three months post-intervention and suggest reduced durability of treatment effects. Clinical best practices recommendations for educational interventions include planning for maintenance (e.g., booster sessions) and generalization (e.g., instruction in multiple settings). Our data suggest a role for planned maintenance and generalization from short-term, modular CBI interventions for persistent, core social deficits as well. Data from this trial also suggest social cognition may represent an undertreated social learning domain in available CBI-based interventions13,17. Studies designed to further interrogate treatment targets from CBI are critical to better understanding potential mechanisms and improving available treatments. If findings of reduced impact on social cognition are replicated, next-stage interventions with potential to impact multiple domains contributing to social learning may also provide a means to improve treatment durability.
Supplementary Material
Acknowledgments
The authors acknowledge Autism Speaks, the National Institute of Mental Health (NIMH, R21MH089236-01), the Brain and Behavior Research Foundation, and the Seaver Foundation for their support.
Mr. Beck served as the statistical expert for this research.
The authors wish to thank Sarah Teitelbaum, MA, at the University of Florida; Nicole Feirsen, MA, at City University of New York (CUNY)-Queens; Caroline Phillips, PhD, Lauren Stutman, PhD, Alice Brandwein, PhD, at the Child Mind Institute; Hayley Crain, MA, at the Chicago School of Professional Psychology; Lauren Donnelly, PhD, of Columbia University; Lily Schwartz, BA, at Farleigh Dickinson University; and Rachel Schmitt, PhD, at Boston Children’s Hospital, for their assistance in data collection for this trial.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical trial registration information—Neural and Behavioral Outcomes of Social Skills Groups in Children With Autism Spectrum Disorder; https://clinicaltrials.gov; NCT01190917.
Disclosure: Dr. Soorya has received research funding from Autism Speaks, the Brain and Behavior Research Foundation, and the Brinson Foundation. She has served as a consultant to University of North Carolina-Chapel Hill, the Mount Sinai School of Medicine, and Coronado Biosciences. She has received royalties from Hogrefe Publishing. Dr. Weinger has received research funding from Autism Speaks. Dr. Gorenstein has received funding from the UJA Federation of New York. Dr. Halpern has received funding from the UJA Federation of New York. Dr. Kolevzon has received research funding from the National Institutes of Health, Autism Science Foundation, Seaver Foundation, Hoffman-La Roche, Neuren Pharmaceuticals, and Synapdx. Dr. Buxbaum has received research funding from NIMH, the National Institute on Aging, and Sage Bionetworks. He has served as an advisory board member for the Brain and Behavior Research Foundation, the Hussman Foundation, the Phelan-McDermid Syndrome Foundation, and the Autism Science Foundation. He is an editor for Molecular Autism and receives royalties from the Biomed Central Publishing Group. He is also an editor for Elsevier, The Neuroscience of Autism Spectrum Disorders, and Oxford University Press, Neurobiology of Mental Illness. He retains intellectual property rights for IGF1 in Shank3 IP, PTSD Risk Assessment, and Autism Genetics/Treatment. Dr. Wang has received research funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Mr. Beck and Ms. Soffes report no biomedical financial interests or potential conflicts of interest.
Supplemental materials cited in this article is available online.
References
- 1.Bauminger N, Shulman C, Agam G. Peer interaction and loneliness in high-functioning children with autism. Journal of autism and developmental disorders. 2003;33(5):489–507. doi: 10.1023/a:1025827427901. [DOI] [PubMed] [Google Scholar]
- 2.Rotheram-Fuller E, Kasari C, Chamberlain B, Locke J. Social involvement of children with autism spectrum disorders in elementary school classrooms. Journal of child psychology and psychiatry, and allied disciplines. 2010;51(11):1227–1234. doi: 10.1111/j.1469-7610.2010.02289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reichow B, Steiner AM, Volkmar F. Social skills groups for people aged 6 to 21 with autism spectrum disorders (ASD) The Cochrane database of systematic reviews. 2012;7:Cd008511. doi: 10.1002/14651858.CD008511.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaat AJ, Lecavalier L. Group-based social skills treatment: A methodological review. Research in Autism Spectrum Disorders. 2014;8(1):15–24. [Google Scholar]
- 5.Kasari C, Patterson S. Interventions addressing social impairment in autism. Current psychiatry reports. 2012;14(6):713–725. doi: 10.1007/s11920-012-0317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reichow B, Volkmar FR. Social skills interventions for individuals with autism: evaluation for evidence-based practices within a best evidence synthesis framework. Journal of autism and developmental disorders. 2010;40(2):149–166. doi: 10.1007/s10803-009-0842-0. [DOI] [PubMed] [Google Scholar]
- 7.Williams White S, Keonig K, Scahill L. Social Skills Development in Children with Autism Spectrum Disorders: A Review of the Intervention Research. Journal of autism and developmental disorders. 2006 Dec 29; doi: 10.1007/s10803-006-0320-x. [DOI] [PubMed] [Google Scholar]
- 8.Beaumont R, Sofronoff K. A multi-component social skills intervention for children with Asperger syndrome: the Junior Detective Training Program. Journal of child psychology and psychiatry, and allied disciplines. 2008;49(7):743–753. doi: 10.1111/j.1469-7610.2008.01920.x. [DOI] [PubMed] [Google Scholar]
- 9.Frankel F, Myatt R, Sugar C, Whitham C, Gorospe CM, Laugeson E. A randomized controlled study of parent-assisted Children’s Friendship Training with children having autism spectrum disorders. Journal of autism and developmental disorders. 2010;40(7):827–842. doi: 10.1007/s10803-009-0932-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laugeson EA, Frankel F, Gantman A, Dillon AR, Mogil C. Evidence-based social skills training for adolescents with autism spectrum disorders: the UCLA PEERS program. Journal of autism and developmental disorders. 2012;42(6):1025–1036. doi: 10.1007/s10803-011-1339-1. [DOI] [PubMed] [Google Scholar]
- 11.Koenig K, White SW, Pachler M, et al. Promoting social skill development in children with pervasive developmental disorders: a feasibility and efficacy study. Journal of autism and developmental disorders. 2010;40(10):1209–1218. doi: 10.1007/s10803-010-0979-x. [DOI] [PubMed] [Google Scholar]
- 12.Lopata C, Thomeer ML, Volker MA, et al. RCT of a manualized social treatment for high-functioning autism spectrum disorders. Journal of autism and developmental disorders. 2010;40(11):1297–1310. doi: 10.1007/s10803-010-0989-8. [DOI] [PubMed] [Google Scholar]
- 13.Thomeer ML, Lopata C, Volker MA, et al. Randomized Clinical Trial Replication of a Psychosocial Treatment for Children with High-Functioning Autism Spectrum Disorders. Psychology in the Schools. 2012;49(10):942–954. [Google Scholar]
- 14.McMahon CM, Lerner MD, Britton N. Group-based social skills interventions for adolescents with higher-functioning autism spectrum disorder: a review and looking to the future. Adolescent health, medicine and therapeutics. 2013;2013(4):23–28. doi: 10.2147/AHMT.S25402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeRosier ME, Swick DC, Davis NO, McMillen JS, Matthews R. The efficacy of a Social Skills Group Intervention for improving social behaviors in children with High Functioning Autism Spectrum disorders. Journal of autism and developmental disorders. 2011;41(8):1033–1043. doi: 10.1007/s10803-010-1128-2. [DOI] [PubMed] [Google Scholar]
- 16.Lerner MD, Mikami AY. A Preliminary Randomized Controlled Trial of Two Social Skills Interventions for Youth With High-Functioning Autism Spectrum Disorders. Focus on Autism and Other Developmental Disabilities. 2012;27(3):147–157. [Google Scholar]
- 17.Baghdadli A, Brisot J, Henry V, et al. Social skills improvement in children with high-functioning autism: a pilot randomized controlled trial. European child and adolescent psychiatry. 2013;22(7):433–442. doi: 10.1007/s00787-013-0388-8. [DOI] [PubMed] [Google Scholar]
- 18.Solomon M, Goodlin-Jones BL, Anders TF. A social adjustment enhancement intervention for high functioning autism, Asperger’s syndrome, and pervasive developmental disorder NOS. Journal of autism and developmental disorders. 2004;34(6):649–668. doi: 10.1007/s10803-004-5286-y. [DOI] [PubMed] [Google Scholar]
- 19.Bauminger N. Brief report: individual social-multi-modal intervention for HFASD. Journal of autism and developmental disorders. 2007;37(8):1593–1604. doi: 10.1007/s10803-006-0245-4. [DOI] [PubMed] [Google Scholar]
- 20.Begeer S, Gevers C, Clifford P, et al. Theory of Mind training in children with autism: a randomized controlled trial. Journal of autism and developmental disorders. 2011;41(8):997–1006. doi: 10.1007/s10803-010-1121-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology and Psychiatry. 2009;50(3):224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nowicki S, Jr, Duke MP. Manual for the Receptive Tests of the Diagnostic Analysis of Nonverbal Accuracy 2. Atlanta: Emory University; 2003. [Google Scholar]
- 23.Kraemer H, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of general psychiatry. 2006;63(5):484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 25.Lord C, Risi S, Lambrecht L, et al. The Autism Diagnostic Observation Schedule–Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- 26.Rutter M, Le Couteur A, Lord C. ADI-R Autism Diagnostic Interview – Revised. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- 27.McGinnes E, Goldstein AP. Skillstreaming the Elementary School Child: New Strategies and Perspectives for Teaching Prosocial Skills. Campaign, Illinois: Research Press; 1997. [Google Scholar]
- 28.Baker J. Shawnee Mission. Kansas: Autism Asperger Publishing Company; 2003. Social Skills Training: For Children and Adolescents with Asperger Syndrome and Social-Communication Problems. [Google Scholar]
- 29.Gutstein S, Sheely R. Relationship Development Intervention Activities for Children, Adolescents and Adults. London: Jessica Kingsley Publications; 2002. [Google Scholar]
- 30.Wellman HM, Baron-Cohen S, Caswell R, et al. Thought-bubbles help children with autism acquire an alternative to a theory of mind. Autism: the international journal of research and practice. 2002;6(4):343–363. doi: 10.1177/1362361302006004003. [DOI] [PubMed] [Google Scholar]
- 31.Constantino J. Social Responsiveness Scale (SRS) Los Angeles: Western Psychological Services; 2005. [Google Scholar]
- 32.Dadds MR, Hunter K, Hawes DJ, et al. A measure of cognitive and affective empathy in children using parent ratings. Child psychiatry and human development. 2008;39(2):111–122. doi: 10.1007/s10578-007-0075-4. [DOI] [PubMed] [Google Scholar]
- 33.Bishop D. Children’s Communication Checklist Version 2 (CCC-2) London: Psychological Corporation; 2003. [Google Scholar]
- 34.Bryant BK. An Index of Empathy for Children and Adolescents. Child development. 1982;53(2):413–425. [Google Scholar]
- 35.Brent E, Rios P, Happe F, Charman T. Performance of children with autism spectrum disorder on advanced theory of mind tasks. Autism: the international journal of research and practice. 2004;8(3):283–299. doi: 10.1177/1362361304045217. [DOI] [PubMed] [Google Scholar]
- 36.Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. Journal of Child Psychology and Psychiatry. 2001;42(2):241–251. [PubMed] [Google Scholar]
- 37.Happe FGE. An advanced test of theory of mind: understanding of story characters’ thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. Journal of Autism and Developmental Disorders. 1994;24(2):129–154. doi: 10.1007/BF02172093. [DOI] [PubMed] [Google Scholar]
- 38.Antshel KM, Polacek C, McMahon M, et al. Comorbid ADHD and anxiety affect social skills group intervention treatment efficacy in children with autism spectrum disorders. Journal of developmental and behavioral pediatrics: JDBP. 2011;32(6):439–446. doi: 10.1097/DBP.0b013e318222355d. [DOI] [PubMed] [Google Scholar]
- 39.Reynolds C, Kamphaus R. Behavior Assessment System for Children – Second Edition (BASC-2) Circle Pines, MN: AGS Publishing; 2004. [Google Scholar]
- 40.Wilson RS, Beckett LA, Barnes LL, et al. Individual differences in rates of change in cognitive abilities of older persons. Psychology and Aging. 2002;17(2):179–193. [PubMed] [Google Scholar]
- 41.Wilson RS, Schneider JA, Arnold SE, Bienias JL, Bennett DA. Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Archives of general psychiatry. 2007;64(10):1204–1212. doi: 10.1001/archpsyc.64.10.1204. [DOI] [PubMed] [Google Scholar]
- 42.Denham SA, Blair KA, DeMulder E, et al. Preschool Emotional Competence: Pathway to Social Competence? Child development. 2003;74(1):238–256. doi: 10.1111/1467-8624.00533. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Social learning theory. Oxford, England: Prentice-Hall; 1977. [Google Scholar]
- 44.Bauminger N. Brief report: group social-multimodal intervention for HFASD. Journal of autism and developmental disorders. 2007;37(8):1605–1615. doi: 10.1007/s10803-006-0246-3. [DOI] [PubMed] [Google Scholar]
- 45.Center for Disease Control and Prevention. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years — Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2010. Morbidity and Mortality Weekly Report (MMWR) 2014:1–21. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


