Abstract
Objectives
To assess current obstetrician-gynecologist (ob-gyn) practice patterns related to the management of and barriers to smoking cessation during pregnancy and postpartum.
Methods
A smoking cessation questionnaire was mailed to 1024 American College of Obstetricians and Gynecologists Fellows in 2012. χ2 analyses were used to assess for categorical differences between groups, Pearson r was used to conduct correlational analysis, and analysis of variance was used to assess for mean differences between groups.
Results
The analyses included 252 practicing ob-gyns who see pregnant patients who returned a completed survey. Ob-gyns estimated that 23% of their patients smoke before pregnancy, 18% smoke during first trimester, 12% during second trimester, and 11% during third trimester. They approximated that 32% quit during pregnancy, but 50% return to smoking postpartum. A large majority of ob-gyns feel that it is important for pregnant and postpartum women to quit smoking, and report asking all pregnant patients about tobacco use at the initial prenatal visit. Fewer ob-gyns follow-up on tobacco use at subsequent visits when the patient has admitted to use at a prior visit. The primary barrier to intervention was reported as time limitations, though other barriers were noted that may be addressable through the provision of additional training and resources offered to physicians.
Conclusions
Compared with findings from a similar study conducted in 1998, physicians are less likely to adhere to the 5 As smoking cessation guideline at present. As we know that brief intervention is effective, it is imperative that we work toward addressing practice gaps and providing additional resources to address the important public health issue of smoking during pregnancy and postpartum.
Keywords: obstetrician-gynecologists, pregnancy, practice patterns, smoking cessation
Cigarette smoking is the primary cause of lung cancer in women, which in turn is the leading cause of female cancer death in the United States (American Cancer Society, 2010). Smoking is also the major cause of coronary heart disease and chronic obstructive pulmonary disease among women and increases a woman’s risk for esophageal, liver, colorectal, pancreas, and kidney cancers (US Department of Health and Human Services, 2001). Smoking among pregnant and postpartum women is the leading preventable cause of poor pregnancy outcomes, infant morbidity, and infant mortality. Women who smoke during pregnancy are more likely to have a wide range of negative pregnancy outcomes, including ectopic pregnancy (Coste et al., 1991), placenta previa and abruption (Handler et al., 1994), intrauterine growth restriction (Nordentoft et al., 1996), miscarriage (Armstrong et al., 1992), preterm birth (Shah and Bracken, 2000), low-birth-weight babies (US Department of Health and Human Services, 2006), and having a child die from sudden infant death syndrome (DiFranza and Lew, 1995).
Past-month cigarette use is reported by 16% of pregnant women aged 15 to 44 years (Substance Abuse and Mental Health Services Administration, 2011). Although research suggests that 20% to 40% of pregnant smokers spontaneously quit smoking before giving birth (Ockene et al., 2002; Morasco et al., 2006), rates of relapse in the postpartum period are reported to be as high as 80% among women who quit smoking during pregnancy (Fingerhut et al., 1990; Colman and Joyce, 2003; Fang et al., 2004; Centers for Disease Control and Prevention, 2007; Tong et al., 2009), with 60% relapse occurring in the first 6 months postpartum (Roske et al., 2006).
Tobacco cessation treatment for pregnant women is considered one of the most cost-saving preventive services (US Public Health Service, 2000). Clinical trials have shown that $6 is saved in health care costs for every $1 invested in smoking cessation programs for pregnant women (Marks et al., 1990). The US Preventive Services Task Force strongly recommends that clinicians ask all pregnant women about tobacco use and provide them with assistance to quit.
As obstetricians and other prenatal care clinicians are uniquely positioned to intervene during pregnancy, the American College of Obstetricians and Gynecologists (ACOG; 2000, 2010) adapted the US Public Health Service’s smoking cessation guidelines for use with pregnant women. The approach follows a manualized protocol, the 5 As, that includes scripted material and the following steps: Ask about tobacco use, advise to quit, assess willingness to make a quit attempt, assist in quit attempt, and arrange follow-up. For women who are not ready to quit smoking, the approach uses motivational interviewing to help women understand how continued smoking is related to their health problems, how continued use puts them and their unborn baby at risk, and to motivate them to quit using tobacco and to maintain their abstinence.
The suggested language can be adapted to the clinician’s personal style and the patient’s individual needs. When the 5 As is integrated into existing routines, the time commitment is usually 7 to 10 minutes (Hartmann, 2000). This low-intensity intervention achieves a modest but statistically and clinically significant effect on cessation rates, with an average risk ratio of 1.7 (Melvin et al., 2000).
Prior research (Chapin and Root, 2004) suggests that 2 key limitations of the 5 As may be that the intervention is delivered inconsistently by physicians because of their time constraints and that even when it is delivered, the women do not always recall all of the information as they get closer to birth. Fifteen years ago, a survey study of obstetrician-gynecologists (ob-gyns; Floyd et al., 2001) found that nearly all reported asking all prenatal patients about smoking status at the initial visit (97.8%), always discussing adverse effects with those who smoke (95.3%), and always advising them to stop smoking (94.9%). Fewer assisted in developing a quit plan (58.6%), provided self-help materials (37.6%), or referred to smoking cessation workshops/seminars (21.8%). These results suggest that asking and advising may have been more commonly done than assessing, assisting, and arranging follow-up.
The purpose of this study was to examine the current practice patterns and opinions of ob-gyns related to smoking cessation during pregnancy and postpartum in an effort to identify gaps that may be addressed through additional education or resources provided to them.
METHODS
Sample
In 2012, a total of 1024 ACOG Fellows were invited to participate in this research. Of them, 425 were Collaborative Ambulatory Research Network (CARN) members and 599 were non-CARN members. Members of CARN are practicing ob-gyns who have volunteered to participate in survey studies on a regular basis. The non-CARN group is composed of practicing ob-gyns who are ACOG Fellows but are not CARN members. All participants were sent an introductory letter, a questionnaire on smoking cessation, and a postage-paid return envelope. Those who did not respond after the first mailing were sent up to 3 reminder mailings. Finally, those who did not respond to the questionnaire were sent a letter with only 11 of the survey items along with a postage-paid return envelope.
Of the 475 who returned a questionnaire or a letter, 5 were retired or not practicing (3 non-CARN and 2 CARN members) and were therefore considered ineligible. The total numbers of respondents (survey and letter) were 252 CARN (60% response rate) and 218 non-CARN (37% response rate) members (n = 470).
Survey
The questionnaire was developed by the authors, along with other experts, to gather information on ob-gyn practice patterns and opinions related to patient smoking during pregnancy and postpartum. Some questions were based on previous research studies (Floyd et al., 2001). Institutional review board approval was obtained from the ACOG.
Demographics/Practice Characteristics
Demographic information collected included year of birth, graduation year, practice focus, practice location, practice setting, sex, and percentage of patients using Medicaid. Ob-gyns were asked to approximate the percentage of patients who reported smoking during pregnancy, quitting during pregnancy, and returning to smoking postpartum. For these questions, respondents were asked to provide their best estimate on the basis of what their patients report to them, rather than what their patients actually do.
Management
Ob-gyns were also asked 2 questions about screening their patients for tobacco use: one question asked about screening during the prenatal visit, and another asked how the patients were screened. These questions listed various screening behaviors, and physicians were asked to check all that apply. Information about the management of pregnancy and postpartum patients (eg, advise exercise, recommend nicotine patch, gum, etc) was obtained with 2 separate questions. Each question listed the various management behaviors, and physicians were asked to indicate how frequently they perform each behavior on a scale from 1 (never) to 5 (always). Similarly, ob-gyns indicated how often and when they communicate tobacco use during pregnancy to the newborn’s pediatrician on a scale from 1 (always) to 5 (never). To gauge interest in biochemical screening for tobacco use, ob-gyns were asked about their willingness to incorporate screening for cotinine (ie, a by-product of nicotine) into their practice (yes/no).
Barriers to Intervention
To learn about perceived barriers to providing a brief intervention to pregnant and postpartum women, a list of barriers was provided, and ob-gyns were asked to rank their top 3 barriers. Questions about how prepared ob-gyns felt to perform various screening and intervention activities were also asked. For each of the items, ob-gyns indicated being very unprepared (1), somewhat unprepared (2), somewhat prepared (3), or very prepared (4). Finally, ob-gyns indicated which resources they needed to improve smoking cessation interventions in their clinical practice. Various resources were listed, and physicians were asked to check all that apply.
The letter mailing included 10 management questions, which included 5 items about asking, advising, assessing, assisting, and arranging follow-up for pregnant women and the same 5 items for postpartum women, and one question about the percentage of patients who reported returning to smoking postpartum. The respondents to these 11 questions were compared with those who completed the entire survey to assess for differences between survey responders and nonresponders, and are not included in the main results.
Data Analyses
Differences between CARN and non-CARN members were assessed on all items, and letter and survey responders were also compared on all of the 11 items on the letter mailing (last paragraphs of Results). Only statistically significant findings are reported. We also assessed for differences based on practice focus (ob-only vs ob-gyn), percentage of Medicaid patients, and practice location on all items (screening, management, barrier, preparedness, resources, patient smoking rates, and physician smoking status), and only the statistically significant results are reported in the text or Appendix 1.
Some of the variables were grouped for χ2 analyses. Graduation year was grouped using median split, with 1962-1988 as the “older group” and 1989-2004 as the “younger group.” Practice types were grouped into “solo practice/2-clinician practice,” “hospital, clinic, community-based health center,” and “group practice/staff model HMO.” Frequency of management activities that were assessed on a 5-point scale from 1 = never to 5 = always were reduced to 3-point scales for analyses (never and rarely were combined, and usually and always were combined). Responses to questions about preparedness were grouped as “prepared” (indicated very prepared or prepared) or “unprepared (indicated very unprepared or prepared). Questions about barriers were grouped into “indicated as a top 3 barrier” or “did not indicate as a top 3 barrier.”
Responses to 4 of the management questions that had to do with advise, assist, assess, or arrange elements of a brief intervention (advise abstinence, assist in developing a quit plan and quit day, assess readiness to quit smoking, and arrange for a follow-up) were totaled for a total brief intervention management score; one score was computed for pregnant patients and one score was computed for postpartum patients. Scores could range from 4 to 20. Higher scores indicated more frequent performance of intervention management activities.
χ2 analyses were used to assess for differences between groups, Pearson r was used to assess for correlations, and analysis of variance was used to assess for mean differences between groups. Analyses were conducted using SPSS 17.0 (SPSS Inc, Chicago, Illinois), with statistical significance determined by α set at P ≤ 0.05.
RESULTS
Of the total 470 responders, 401 returned a completed survey and 69 returned a completed letter. Because the letter responses were only used for comparative analysis to determine differences in survey responders and nonresponders (see “Letter Response” hereafter), they are not included in the main results. In addition, because most survey asked about pregnant patients, responders who reported not treating pregnant patients were excluded (n = 149 survey responders and 10 letter responders). Therefore, the final sample of practicing ob-gyns who see pregnant patients included 252 survey responders and 59 letter responders.
CARN Versus Non-CARN Members
The 252 ob-gyns who responded to the survey and were used for analyses included both CARN (n = 157) CARN and non-(n = 95) ACOG Fellows. The CARN and non-CARN responders=did not differ by age (controlling for sex), sex (when controlling for age), practice location, practice type, or percentage of Medicaid patients. The CARN and non-CARN responders were found to significantly differ on 2 preparedness items; non-CARN responders were more likely to indicate that they are unprepared to educate pregnant patients about the effects of tobacco on their unborn baby (8.8% vs 2.6% of CARN, χ2 = 4.8, P = 0.028) and use resources to refer patients who need a tobacco cessation program (58.4% vs 45.2% of CARN, χ2 = 4.0, P = 0.046). Given the similarity of the data, CARN and non-CARN groups were combined for all additional analyses.
Demographics/Practice Characteristics
Demographic data for the 252 ob-gyns who were used for analyses are presented in Appendix 2. Most respondents indicated that they are white (81.7%), female (55.7%), have never smoked (78.2%), and practice obstetrics and gynecology (85.7%) in a group practice/staff model health maintenance organization (HMO) (46%) located in a suburban area (40.1%).
Women were younger than men (Mwomen 47.5 years, SD = 7.8, vs Mmen 55.6 years, SD = 8.9; F1,186 = 43.6, P < 0.001): 76.0% of the younger group (graduation year 1989-2004) were women compared with 36.3% of the older group (graduation year 1962-1988) (χ2 = 39.3, P < 0.001). Ob-gyns in inner-city urban areas were more likely to be practicing obstetrics only than those who were not in an inner-city urban area (36.3% vs 4.7%) (χ2 = 28.0, P < 0.001). Ob-gyns in suburban areas were more likely to be in solo (27.7% of suburban compared with 22.1% of nonsuburban) or group practice (62.8% of suburban compared with 45.1% of non-suburban) (χ2 = 16.4, P < 0.001). Ob-gyns in underserved communities were more likely to be working in a hospital or clinic than those not in an underserved community (69.2% vs 19.7%) (χ2 = 17.1, P < 0.001).
Ob-gyns estimated that 22.7% (SD = 16.7) of their patients smoke before pregnancy, 17.9% (SD = 22.6) during first trimester, 11.9% (SD = 12.6) during second trimester, and 11.0% (SD = 11.9) during third trimester. They approximated that 32.0% (SD = 31.3) of their pregnant patients report having quit smoking during pregnancy, but 49.7% (SD = 28.7) return to smoking postpartum.
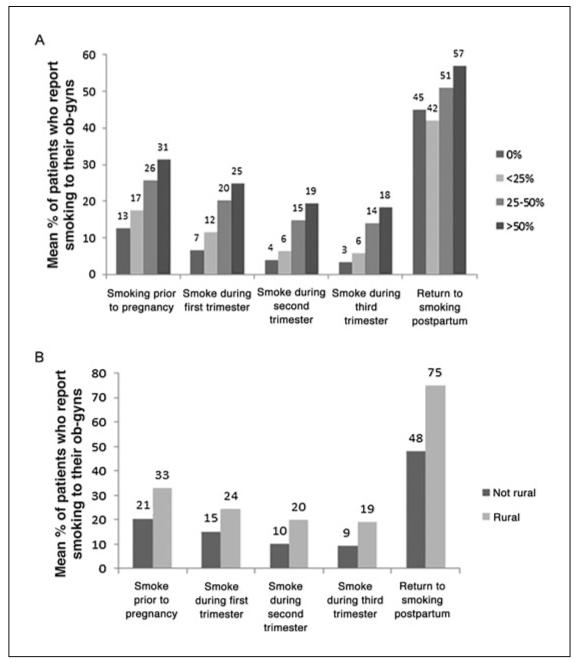
As shown in Figure 1A, ob-gyns who treat a higher percentage of Medicaid patients reported a higher percentage of patients smoking before pregnancy (F3,225 = 13.9, P < 0.001) and during first (F3,224 = 14.3, P < 0.001), second (F3,216 = 20.5, P < 0.001), and third trimesters (F3,214 = 20.7, P < 0.001). Ob-gyns with a higher percentage of Medicaid patients also reported a lower percentage of patients reporting quitting smoking during pregnancy (F3,228 = 4.4, P = 0.005), who return to smoking after postpartum (F3,194 = 2.8, P = 0.039), than those with a lower percentage of Medicaid patients. Similarly, ob-gyns in rural areas reported a higher percentage of patients smoking before pregnancy (F1,229 = 19.3, P < 0.001) and during first (F1,228 = 11.2, P = 0.001), second (F1,220 = 21.6, P < 0.001), and third trimesters (F1,218 = 23.5, P < 0.001) than those who are not in rural areas (see Fig. = 1B).
FIGURE 1.
A, The mean percentage of pregnant patients who report smoking cigarettes at each stage of pregnancy by percentage of Medicaid patients. B, The mean percentage of pregnant patients who report smoking cigarettes at each stage of pregnancy by rural versus not rural areas.
Management
Most ob-gyns reported obtaining their initial information about their patient’s tobacco use from nonphysician staff who ask the patient during an intake assessment (71.0%) and/or from asking patients themselves during an initial examination (65.9%). An additional 47.2% reported obtaining this information from patient self-report on an intake questionnaire. Only 2.0% reported biochemical verification of smoking status, and many (41%) are unwilling to incorporate cotinine screening into their practice even with minimal associated costs.
Although a large majority (88.1%) of ob-gyns reported that they ask all of their pregnant patients about tobacco use at their initial prenatal visit, fewer follow up by asking about tobacco use at subsequent visits when the patient has admitted to tobacco use at a prior visit (59.9%). If physicians suspect pregnant patients are smoking but it is not indicated on intake forms, 25% ask about tobacco use at the initial visit and approximately one third (35.4%) ask at subsequent visits. Few physicians (6.7%) ask all pregnant women about tobacco use at all subsequent visits. A total of 3.6% indicated that they do not typically ask patients about tobacco use unless they self-report tobacco use to a nurse or on intake forms.
Responses about managing pregnant patients are shown in Table 1. “Advise abstinence,” “advise reduction,” and “review reasons for quitting and benefits of quitting” were the most frequent management tasks. The least frequent were “do nothing” and “refer to group counseling” or “refer to individual counseling.” Responses about managing postpartum patients are also shown in Table 1. The most and least frequent management tasks indicated by respondents were the same as those for pregnant patients.
TABLE 1.
Obstetrician-Gynecologists’ Management of Pregnant and Postpartum Patients (n = 252)
| Management Task* | Pregnant | Postpartum |
|---|---|---|
| Advise abstinence | 4.78 (0.55) | 4.46 (0.95) |
| Advise reduction | 4.58 (0.83) | 4.31 (0.98) |
| Advise exercise | 3.79 (1.29) | 3.77 (1.29) |
| Recommend nicotine patch, gum, lozenge, inhaler, or nasal spray |
2.93 (l.25) | 3.45 (1.08) |
| Recommend varenicline or bupropion SR |
2.12 (1.12) | 2.82 (1.12) |
| Identify “trigger” situations | 3.02 (1.35) | 3.14 (1.35) |
| Identify others who smoke in the household |
3.86 (1.20) | 3.67 (1.31) |
| Review reasons for quitting and benefits of quitting |
4.57 (0.78) | 4.19 (1.10) |
| Assist in developing a quit plan and quit day |
3.27 (1.25) | 2.98 (1.36) |
| Refer to a tobacco quitline | 2.72 (1.49) | 2.54 (1.41) |
| Refer to Web sites for free materials (eg, www.smokefree.gov) |
2.39 (1.37) | 2.31 (1.34) |
| Refer to group counseling | 1.98 (1.10) | 1.93 (1.12) |
| Refer to individual counseling (not including quitlines) |
1.94 (1.15) | 1.96 (1.13) |
| Provide educational materials | 3.14 (1.36) | 2.84 (1.35) |
| Assess readiness to quit smoking |
3.87 (1.26) | 3.58 (1.27) |
| Arrange for a follow-up | 3.28 (1.48) | 2.47 (1.37) |
| Do nothing | 1.38 (0.78) | 1.66 (1.01) |
| Other (please specify) | 2.06 (1.58) | 1.87 (1.50) |
“How do you usually manage pregnant and postpartum women who report tobacco use? Check 1 per row.” Mean responses on a scale from 1 = never to 5 = always.
The mean brief intervention management score (of a total of 20) was 15.2 (SD = 3.5) for pregnant women and 13.4 (SD = 3.8) for postpartum women. The brief intervention-management score for pregnant patients was significantly positively correlated with the brief intervention management scores for postpartum patients (r = 0.780, P < 0.001). Both brief intervention management scores were significantly positively correlated with the percentage of patients who report smoking before pregnancy (pregnant: r = 0.203, P = 0.004, and postpartum: r = 0.212, P = 0.003). Only brief intervention management score for pregnant patients was correlated (though weakly) with the percentage of patients who report having quit smoking during pregnancy (r = 0.163, P = 0.021), and neither brief intervention management score was correlated with percentage of pregnant patients who quit smoking during pregnancy and returned to smoking postpartum.
There was little consistency among respondents about how often they communicate information to the newborn’s pediatrician; 24.2% always, 17.5% usually, 7.1% sometimes, 12.3% rarely, and 35.7% never doing so (3.2% did not respond). The open-ended questions about when and what is communicated to the newborn’s pediatrician were analyzed among those who indicated that they always, usually, sometimes, or rarely communicate information to the newborn’s pediatrician (n = 154). When asked when they communicate to the pediatrician, 32.5% indicated doing so at delivery, 2.6% did so during third trimester, 22.1% indicated they did so via chart or problem reports (with no indication of timing), and 9.7% indicated some other time (eg, when I see him/her) (33.1% did not write in a response). When asked what they communicate to the pediatrician, 20.1% said presence of smoking, 6.5% said the amount of smoking, 1.3% said the smoking environment, 13.0% said they communicate multiple aspects (eg, presence and amount), and 9.1% indicated other (most commonly that it was communicated via chart) (50% did not write in a response).
Almost all ob-gyns indicated that it is very important or important for women to stop smoking during pregnancy (93.6%) and for women who continue to smoke during pregnancy, to stop postpartum (93.6%).
Barriers to Intervention
The most common barriers to implementing a smoking cessation intervention were time limitations, expected patient denial or resistance to treatment, and lack of referral resources for adequately dealing with prenatal tobacco use problems once identified. A total of 57.1% ranked “time limitations” as 1 of their top 3 barriers, a total of 48.8% ranked “expected patient denial or resistance to treatment” as 1 of their top 3 barriers, and a total of 42.1% ranked “lack of referral resources for adequately dealing with prenatal tobacco use problems once identified” as 1 of their top 3 barriers (see Table 2).
TABLE 2.
Percentage of Responding Obstetrician-Gynecologists Who Ranked Each Barrier at Their Number 1, Number 2, or Number 3 Barriers to Implementing Smoking Cessation Interventions
| Barrier | Ranked 1 | Ranked 2 | Ranked 3 |
|---|---|---|---|
| Time limitations | 35.3% | 9.5% | 12.3% |
| Concern about confidentiality issues (of this kind of information about the patient) |
0.0% | 0.0% | 0.8% |
| Expected patient sensitivity to this topic |
1.6% | 7.5% | 6.0% |
| Expected patient denial or resistance to treatment |
17.5% | 18.3% | 13.1% |
| Need for additional training to enhance ascertainment skills |
0.8% | 6.0% | 3.2% |
| Lack of referral resources for adequately dealing with prenatal tobacco use problems once identified |
13.9% | 15.1% | 13.1% |
| Lack of financial reimbursement for tobacco screening, assessment, and counseling |
2.8% | 8.3% | 11.1% |
| Patient inability to pay for treatment |
6.7% | 10.7% | 12.3% |
| Other | 2.0% | 0.8% | 1.6% |
Participants were given a list of potential barriers to implementing smoking cessation inventions and asked to rank their top 3 barriers.
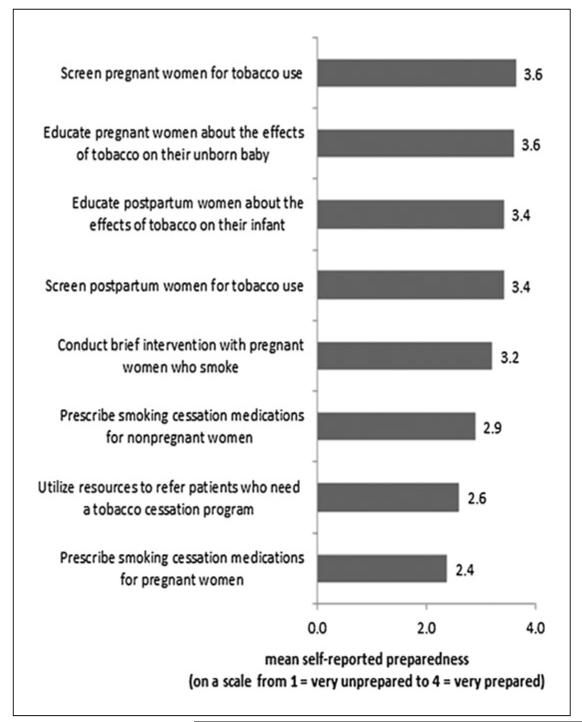
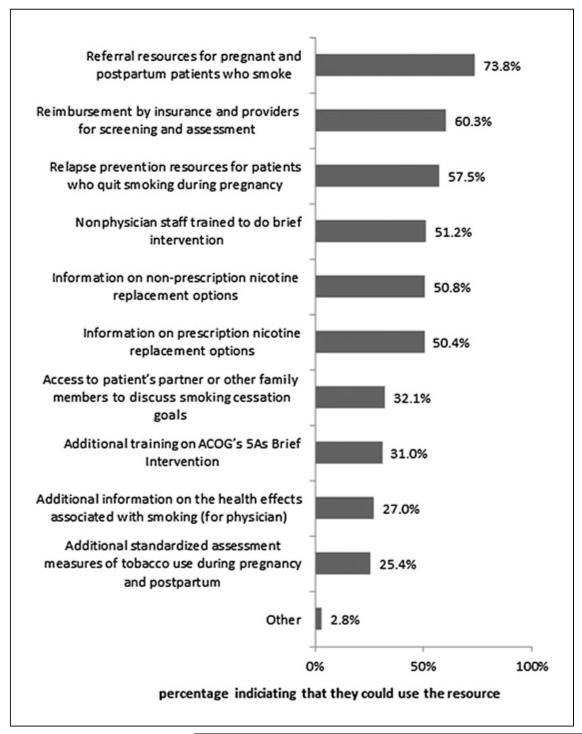
One potential barrier that we examined further was preparedness to provide smoking cessation intervention (see Fig. 2). Ob-gyns felt least prepared to prescribe smoking cessation medications to pregnant patients and to use resources to refer patients. They indicated feeling most prepared to screen and educate pregnant and postpartum women. Figure 3 shows the percentage of ob-gyns who indicated that they could use each of the resources to improve smoking cessation interventions in their clinical practice. Ob-gyns most commonly indicated that they could use resources to refer patients (74%) and resources for reimbursement by insurance and providers for screening and assessment (60%).
FIGURE 2.
Obstetrician-gynecologists’ self-reported preparedness to provide various smoking cessation tasks (n = 252).
FIGURE 3.
Percentage of obstetrician-gynecologists who could use the resources to improve smoking cessation interventions in their clinical practice (n = 252).
Those who were more prepared to conduct a brief intervention indicated performing advise, assist, assess, and arrange management activities more frequently. Those who indicated that they were prepared to conduct a brief intervention had significantly higher brief intervention management scores for pregnant patients (M = 14.2, SD = 3.5) than those who indicated that they were unprepared (M = 10.2, SD = 3.5) (F1,198 = 39.1, P < 0.001). Those who indicated that they were prepared to conduct a brief intervention had significantly higher brief intervention management scores for postpartum women (M = 15.8, SD = 3.1) than those who indicated that they were unprepared (M = 12.3, SD = 3.4) (F1,201 = 40.2, P < 0.001).
Personal Smoking History
Men were more likely to have been smokers in the past (when controlling for age) than women (28% vs 12%). Those who had previously smoked more frequently arranged a follow-up (60% indicated usually or always) than those who had never smoked (52.6%) (χ2 = 6.0, P = 0.049). No ther significant differences were observed on the basis of personal smoking history.
Comparison With Floyd et al. (2001) Findings
A similar survey study examining ob-gyn practice relating to tobacco use during pregnancy was conducted in 1998. In an effort to compare current practice patterns with those reported 15 years ago, we evaluated responses to similar questions. Fewer physicians report asking all patients about tobacco use at the initial visit (from 98% to 88%), but substantially more are inquiring about smoking at each subsequent prenatal visit (from 11% to 60%). Fewer physicians in the current sample report always doing the following: advising pregnant patients to stop smoking (from 95% to 82%), assisting in goal setting/developing a quit plan (from 59% to 19%), providing self-help materials (from 38% to 20%), and identifying others who smoke in the home (from 56% to 38%). That said, a higher percentage recommend nicotine replacement therapy (from 7.1% to 13.9%) and arrange follow-up in the form of referrals than 15 years ago (from 21.8% to 39%).
Letter Response
A total of 69 participants returned the letter, but 10 were excluded because they do not provide obstetrics care. Although letter responders were not included in the main analyses, a comparative analysis on the 11 questions included in both the survey and the letter was conducted to determine differences in survey responders and nonresponders. Letter responders more often report assisting pregnant women in developing a quit plan (66.7% indicating always or usually) than survey responders (44.0%) (χ2 = 10.1, P = 0.006).
Additional Analyses
Appendix 1 includes the results from analyses between practice focus (ob-only vs ob-gyn), percentage of Medicaid patients, and practice location and each of the survey items (screening, management, barrier, preparedness, resources, patient smoking rates, and physician smoking status). Only the significant differences were reported. Because group sizes were small, analyses did not control for the associations between practice characteristics that were reported in the Demographics/Practice Characteristics section. Results should be interpreted with this limitation in mind.
DISCUSSION
Smoking during pregnancy is well-known to be associated with negative health consequences for both mother and unborn child. Both the US Preventive Services Task Force and ACOG strongly recommend that ob-gyns conduct smoking cessation intervention during pregnancy. Substance Abuse and Mental Health Services Administration (2009) reported that approximately 22.0% of pregnant women report past-month cigarette use in their first trimester, 14.4% in the second trimester, and 13.9% in the third trimester, suggesting that ob-gyns in our sample may be slightly underestimating the percentage of their patients who smoke during pregnancy, and the percentage who relapse in the postpartum period.
Underestimating the percentage of pregnant smokers in their practice may be related to the finding that not all physicians are asking about tobacco use throughout pregnancy. Although 88% report asking at the initial visit, fewer (60%) ask at subsequent visits, even with the knowledge that a patient is a smoker. Screening for smoking status at subsequent prenatal visits is important for several reasons: relapse to smoking is common, women may not be ready to quit until later in pregnancy, abstinence rates are highest among people exposed to repeated messages over time, and quit rates increase when prenatal care providers offer cessation advice and counseling (Floyd et al., 2001).
Compared with data collected 15 years ago from practicing ob-gyns (Floyd et al., 2001), fewer physicians report asking all patients about tobacco use at the initial visit, but more are inquiring about smoking at each subsequent prenatal visit. By increasing the number of physicians asking about smoking status at each prenatal visit, we take a step toward increasing quit rates and improving health outcomes; however, asking about use and advising cessation are only 2 of the 5 As and are done much more frequently than the assess, assist, and arrange steps despite an increase in the availability of referral resources such as Web sites and quitlines. Fewer physicians in the current sample, as compared with those in the 1988 sample, report always doing the following: advising pregnant patients to stop smoking, assisting in goal setting/developing a quit plan, providing self-help materials, and identifying others who smoke in the home. That said, a higher percentage recommend nicotine replacement therapy and arrange follow-up in the form of referrals than 15 years ago.
In addition to revealing general trends in smoking cessation intervention, results also indicate variability in intervention by population. Ob-gyns more frequently offer smoking cessation intervention to pregnant patients than to postpartum patients. Specifically, ob-gyns more frequently review the reasons for quitting smoking and benefits of quitting, assist in developing a quit plan and quit day, provide educational materials, and arrange for follow-up for pregnant patients than for postpartum patients. Conversely, ob-gyns more frequently recommend the nicotine patch, gum, lozenge, inhaler, or nasal spray and varenicline or bupropion SR to postpartum patients than to pregnant patients.
Despite recognizing smoking cessation intervention as equally important for both pregnant and postpartum patients, there is a significant difference in how these patients are assessed and managed. The implications of this may negatively impact mother and newborn. A nursing mother who smokes transmits nicotine to her infant through her breast milk in concentrations between 1.5 and 3 times the simultaneous concentration she is experiencing (Steldinger et al., 1988). Smoking in the household during the postpartum period also exposes infants to the negative health effects of environmental tobacco smoke, which include acute lower respiratory tract infections such as bronchitis and pneumonia, more frequent and severe asthma attacks, respiratory symptoms such as coughing and breathlessness, and increased ear infections (US Department of Health and Human Services, 2006). Additional focus on postpartum continuing care with smoking cessation is necessary to provide the best quality care for a mother and her newborn, particularly given the high relapse rates to smoking among those who are able to quit during pregnancy (Coleman-Cowger, 2012).
An encouraging finding from our results is that ob-gyns who treat higher-risk populations (ie, populations reporting having a greater percentage of smokers throughout pregnancy) report conducting some management tasks more frequently than ob-gyns who work with populations that are not necessarily at higher risk. Those who practice in rural areas are more likely to identify others who smoke and arrange a follow-up. This is promising in that those who are most in need may be more likely to receive intervention from their physician.
Although ob-gyns recognize the importance of smoking cessation during pregnancy, time constraints are reported as the number 1 barrier to providing smoking cessation intervention, as has also been suggested by prior research (Chapin and Root, 2004). Although this is a very real barrier that is difficult to address, other barriers listed by physicians in this study may be addressable. For instance, patient resistance to treatment is common, yet may be overcome with the motivational interviewing approach of the 5 Rs as described in the 5 As protocol (see Appendix 3).
Another common barrier noted by survey respondents was lack of financial reimbursement for tobacco screening, assessment, and counseling. The Patient Protection and Affordable Care Act section 4107 (aka health care reform) now requires Medicaid coverage for pregnant women to access tobacco cessation drugs and counseling as of October 1, 2010; thus, it is likely that this barrier will be at least partially overcome.
A significant percentage of ob-gyns feel the need for additional training on smoking cessation, particularly in the areas of identifying local resources for referrals and prescribing drugs for smoking cessation during pregnancy. Some resources are listed in Appendix 3, but there are many more resources available to pregnant smokers now than ever before, and it is important that physicians are aware of these and can refer their patients to those they believe will be best for them. Relapse prevention resources are also needed, and ob-gyns may benefit from additional information on postpartum continuing care for smoking cessation (see Coleman-Cowger, 2012).
Although this study adds significantly to our knowledge of current ob-gyn practice patterns as they relate to smoking cessation during pregnancy and postpartum, and identifies the needs of physicians to better conduct smoking cessation interventions, it is not without limitations. First, data were based on physician self-report; thus, it is possible that respondents over- or underestimated actual practice; however, the data we have obtained are important in that they provide a sense of how many smokers physicians believe they treat, which may be an underestimate of how many smokers they actually treat. Second, the moderate response rate may also be a limitation of this study; however, the response rate in this study is similar to other studies conducted with CARN and non-CARN samples (eg, Perkins et al., 2013 and Vink et al., 2013). It is possible that the responders have greater interest in the topic area than nonresponders and were more willing to complete a survey on smoking cessation. If this was indeed the case, the number of ob-gyns conducting smoking cessation interventions may actually be lower in the general ob-gyn population than that reported here.
CONCLUSIONS
Ob-gyns recognize the importance of smoking cessation during pregnancy and postpartum but may not be intervening with the 5 As because of various barriers, some of which may be overcome through the provision of additional resources. Although a large majority of ob-gyns screen for tobacco use at the initial prenatal visit, fewer report doing this than ob-gyns sampled 15 years ago. Several practice gaps were identified by this study, including the need for follow-up with smokers after the initial determination of smoking status and the need for greater focus on postpartum relapse prevention. Ob-gyns face significant time limitations that may prohibit them from intervening fully with their smoking patients; thus, it is important to also address gaps such as identifying appropriate local resources for referral. Smoking rates during pregnancy and postpartum can be impacted by the provision of brief intervention, and as such, we must do all we can to ensure that the barriers to providing these brief interventions are overcome through the provision of additional resources.
Acknowledgments
Supported by grant, UA6MC19010, through the US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program. Additional support was provided by the National Institute on Drug Abuse of the National Institutes of Health under grant number 1R34DA032683.
Appendix
APPENDIX 1.
Comparisons Based on Practice Characteristics
| Survey Item | Practice Characteristic | Mean (SD) or % Indicating |
P |
|---|---|---|---|
| Estimated percentage of patients who report smoking before pregnancy |
Non–inner-city urban | 19.3 (SD = 11.8) | 0.038 |
| Not non–inner-city urban | 24.3 (SD = 18.6) | ||
| Estimated percentage of patients who report smoking during the third trimester |
Suburban areas | 9.14 (SD = 9.5) | 0.044 |
| Not suburban areas | 12.4 (SD = 13) | ||
| Physician personally asks prenatal patients about tobacco use at initial examination |
>50% Medicaid patients | 82.8% | 0.003 |
| 25%-50% Medicaid patients | 64.4% | ||
| <25% Medicaid patients | 73.2% | ||
| 0% Medicaid patients | 46.9% | ||
| Ask prenatal patients they suspect might be smoking at the initial visit |
Non–inner-city urban | 16.0% | 0.029 |
| Not non–inner-city urban | 29.2% | ||
| Suburban areas | 33.7% | 0.010 | |
| Not in suburban areas | 18.8% | ||
| Ask prenatal patients about tobacco use at all subsequent visits |
Rural areas | 20.5% | <0.001 |
| Not rural areas | 4.8% | ||
| Underserved communities | 25.0% | 0.004 | |
| Not in underserved communities |
5.9% | ||
| Only ask prenatal patients about tobacco use if women self-report use on intake form |
Suburban areas | 7.2% | 0.023 |
| Not in suburban areas | 1.4% | ||
| Identify others who smoke in household with pregnant patients |
Rural areas | 88.1% | 0.004 |
| Not in rural areas | 62.2% | ||
| Non-inner-city urban | 54.8% | 0.024 | |
| Not non–inner-city urban | 72.1% | ||
| Arrange follow-up with pregnant patients | Rural areas | 75.7% | 0.014 |
| Non-rural areas | 49.4% | ||
| Non-inner-city urban | 40.6% | 0.034 | |
| Not in non–inner-city urban | 60.1% | ||
| Refer pregnant patients to a tobacco quitline | Rural areas | 29.3% | 0.040 |
| Nonrural areas | 34.7% | ||
| Provide educational materials to pregnant patients |
Underserved communities | 73.3% | 0.043 |
| Not in underserved communities |
41.1% | ||
| Refer postpartum patients to group counseling |
Non–inner-city urban | 4.1% | 0.015 |
| Not in non–inner-city urban | 12.3% | ||
| Assess postpartum patients’ readiness to quit smoking |
Non–inner-city urban | 45.1% | 0.033 |
| Not in non–inner-city urban | 63.1% | ||
| Always or usually communicate to pediatricians |
Urban inner city | 72.8% | 0.014 |
| Not in urban inner city | 41.2% | ||
| Feel very or somewhat prepared to conduct brief intervention with pregnant patients who smoke |
Non–inner-city urban | 72.4% | 0.016 |
| Not in non–inner-city urban | 85.4% | ||
| Rural areas | 92.5% | 0.046 | |
| Not rural areas | 79.0% | ||
| Underserved communities | 100% | 0.047 | |
| Not in underserved communities |
79.9% | ||
| Feel prepared to prescribe smoking cessation medications to nonpregnant patients |
Ob-only practice | 83.3% | 0.003 |
| Obstetrician-gynecologist practice |
43.0% | ||
| Other practice | 25.0% | ||
| Need nonphysician staff trained to do brief intervention |
> 50% Medicaid patients | 70.2% | 0.047 |
| 25%-50% Medicaid patients | 49.3% | ||
| <25% Medicaid patients | 47.2% | ||
| 0% Medicaid patients | 55.2% | ||
| Urban inner city | 78.3% | 0.017 | |
| Not urban inner city | 52.2% | ||
| Need reimbursement for screening and assessment |
Non–inner-city urban | 54.9% | 0.040 |
| Not non–inner-city urban | 68.9% | ||
| Suburban areas | 73.7% | 0.013 | |
| Not suburban areas | 57.9% |
APPENDIX 2.
Demographic Characteristics (n = 252)
| Mean year completed obstetrician-gynecologist residency | 1992 (SD = 9.3) |
| Mean year of graduation from medical school | 1987 (SD = 9.7) |
| Mean age, yr | 51 (SD = 9.2) |
| Sex, % | |
| Male | 42.5 |
| Female | 55.6 |
| Missing | 2.0 |
| Practice focus, % | |
| Obstetrics only | 7.1 |
| Obstetrics and gynecology | 85.7 |
| Other | 3.2 |
| Missing | 4.0 |
| Practice type, % | |
| Solo practice/2-clinician practice | 21.0 |
| Hospital or clinic | 15.9 |
| Group practice/staff model HMO | 46.0 |
| Community-based health center | 3.6 |
| Medical school or parent university | 8.7 |
| Other | 2.8 |
| Missing | 2.0 |
| Provide comprehensive primary care, % | |
| Yes | 30.6 |
| No | 66.7 |
| Missing | 2.8 |
| Racial group most identified with, % | |
| White | 81.7 |
| Black or African American | 6.0 |
| Asian | 7.9 |
| American Indian or Alaskan Native | 0.0 |
| Native Hawaiian or Pacific Islander | 0.0 |
| Hispanic or Latino | 3.2 |
| Not Hispanic or Latino | 92.5 |
| Percentage of patients on Medicaid | |
| 0% | 12.7 |
| <25% | 29.0 |
| 25%-50% | 30.2 |
| >50% | 24.2 |
| Missing | 4.0 |
| Practice location,* % | |
| Urban, inner city | 9.5 |
| Urban, not inner city | 30.6 |
| Suburban | 40.1 |
| Rural | 16.7 |
| Underserved communities | 6.3 |
| Smoking status, % | |
| Have never smoked regularly | 78.2 |
| Currently smoke, but am trying to quit | 0.8 |
| Used to smoke regularly, but I will quit | 15.5 |
| Currently smoke and am not trying to quit | 1.6 |
| Missing | 3.6 |
Respondents were allowed to indicate more than 1.
APPENDIX 3.
Smoking Cessation Resources
| Refresher course on the 5 As (developed by the Centers for Disease Control and Prevention, ACOG, and the Prevention Research Center at Dartmouth University) |
www.smokingcessationandpregnancy.org |
| Clinician s guide to helping pregnant women quit smoking (developed by ACOG) |
http://www.acog.org/~/media/Departments/Tobacco%20Alcohol%20and%20Substance%20Abuse/SCDP.pdf?dmc=1&ts=20130313T1336097771 |
| Smoking cessation quitline (example) | 1-800-QUIT-NOW |
| Smoking cessation Web site (example) | http://www.becomeanex.org/pregnant-smokers.php# |
Footnotes
The authors declare no conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Health and Human Services or the National Institutes of Health.
REFERENCES
- American Cancer Society . Cancer Facts & Figures 2010. American Cancer Society; Atlanta, GA: 2010. [Google Scholar]
- American College of Obstetricians and Gynecologists . Smoking Cessation During Pregnancy. American College of Obstetricians and Gynecologists; Washington, DC: 2000. ACOG Education Bulletin Number 260. [Google Scholar]
- American College of Obstetricians and Gynecologists Smoking cessation during pregnancy (committee opinion no. 471) Obstet Gynecol. 2010;116:1241–1244. doi: 10.1097/AOG.0b013e3182004fcd. [DOI] [PubMed] [Google Scholar]
- Armstrong BG, McDonald AD, Sloan M. Cigarette, alcohol, and coffee consumption and spontaneous abortion. Am J Public Health. 1992;82:85–87. doi: 10.2105/ajph.82.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Preventing Smoking and Exposure to Secondhand Smoke Before, During, and After Pregnancy. Centers for Disease Control and Prevention; Atlanta, GA: [Accessed on March 12, 2013]. 2007. Available at: http://www.cdc.gov/nccdphp/publications/factsheets/Prevention/pdf/smoking.pdf. [Google Scholar]
- Chapin J, Root W. Improving obstetrician-gynecologist implementation of smoking cessation guidelines for pregnant women: an interim report of the American College of Obstetricians and Gynecologists. Nicotine Tob Res. 2004;6:S253–S257. doi: 10.1080/14622200410001669123. [DOI] [PubMed] [Google Scholar]
- Coleman-Cowger VH. Smoking cessation intervention for pregnant women: a call for extension to the postpartum period. Matern Child Health J. 2012;16:937–940. doi: 10.1007/s10995-011-0837-2. [DOI] [PubMed] [Google Scholar]
- Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. Am J Prev Med. 2003;24:29–35. doi: 10.1016/s0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- Coste J, Job-Spira N, Fernandez H. Increased risk of ectopic pregnancy with maternal cigarette smoking. Am J Public Health. 1991;81:199–201. doi: 10.2105/ajph.81.2.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Lew RA. Effect of maternal cigarette smoking on pregnancy complications and sudden infant death syndrome. J Fam Pract. 1995;40:385–394. [PubMed] [Google Scholar]
- Fang WL, Goldstein AO, Butzen AY, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. J Am Board Fam Med. 2004;17:264–275. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- Fingerhut LA, Kleinman JC, Kendrick JS. Smoking before, during, and after pregnancy. Am J Public Health. 1990;80:541–544. doi: 10.2105/ajph.80.5.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd RL, Belodoff B, Sidhu J, et al. A survey of obstetrician-gynecologists on their patients’ use of tobacco and other drugs during pregnancy. Prenat Neonatal Med. 2001;6:201–207. [Google Scholar]
- Handler AS, Mason ED, Rosenberg DL, et al. The relationship between exposure during pregnancy to cigarette smoking and cocaine use and placenta previa. Am J Obstet Gynecol. 1994;170:884–889. doi: 10.1016/s0002-9378(94)70303-5. [DOI] [PubMed] [Google Scholar]
- Hartmann KE. Clear and concise interventions for smoking cessation. Hosp Phys. 2000;36:19–27. [Google Scholar]
- Marks JS, Koplan JP, Hogue CJ, et al. A cost-benefit/cost-effectiveness analysis of smoking cessation for pregnant women. Am J Prev Med. 1990;6:282–289. [PubMed] [Google Scholar]
- Melvin CL, Dolan-Mullen P, Windsor RA, et al. Recommended cessation counseling for pregnant women who smoke: a review of the evidence. Tob Control. 2000;9:iii80–iii84. doi: 10.1136/tc.9.suppl_3.iii80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morasco BJ, Dornelas EA, Fischer EH, et al. Spontaneous smoking cessation during pregnancy among ethnic minority women: a preliminary investigation. Addict Behav. 2006;31:203–210. doi: 10.1016/j.addbeh.2005.04.022. [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Lou HC, Hansen D, et al. Intrauterine growth retardation and premature delivery: the influence of maternal smoking and psychosocial factors. Am J Public Health. 1996;86:347–354. doi: 10.2105/ajph.86.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ockene JK, Ma Y, Zapka JG, et al. Spontaneous cessation of smoking and alcohol use among low-income pregnant women. Am J Prev Med. 2002;23:150–159. doi: 10.1016/s0749-3797(02)00492-0. [DOI] [PubMed] [Google Scholar]
- Perkins RB, Anderson BL, Sheinfeld Gorn S, et al. Challenges in cervical cancer prevention: a survey of obstetrician-gynecologists. Am J Prev Med. 2013;45:175–181. doi: 10.1016/j.amepre.2013.03.019. [DOI] [PubMed] [Google Scholar]
- Roske K, Hannover W, Grempler J, et al. Post-partum intention to resume smoking. Health Educ Res. 2006;21:386–392. doi: 10.1093/her/cyh069. [DOI] [PubMed] [Google Scholar]
- Shah NR, Bracken MB. A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. Am J Obstet Gynecol. 2000;182:465–472. doi: 10.1016/s0002-9378(00)70240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steldinger R, Luck W, Nau H. Half lives of nicotine in milk of smoking mothers: implications for nursing. J Perinat Med. 1988;16:261–262. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . The NSDUH Report: Substance Use Among Women During Pregnancy and Following Childbirth. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2009. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results From the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. NSDUH Series H-41. HHS Publication No. (SMA) 11-4658. [Google Scholar]
- Tong VT, Jones JR, Dietz PM, et al. Trends in smoking before, during and after pregnancy—Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 31 sites, 2000-2005. Morb Mortal Wkly Rep. 2009;58:1–31. [PubMed] [Google Scholar]
- US Department of Health and Human Services . Women and Smoking: A Report of the Surgeon General. Centers for Disease Control and Prevention; Atlanta, GA: [Accessed March 12, 2013]. 2001. Health consequences of tobacco use among women; pp. 177–450. Available at: http://www.ncbi.nlm.nih.gov/books/NBK44303/ [Google Scholar]
- US Department of Health and Human Services . The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2006. [Google Scholar]
- US Public Health Service . Treating Tobacco Use and Dependence: A Systems Approach. US Public Health Service; Rockville, MD: 2000. [Google Scholar]
- Vink J, Anderson BL, Fuchs K, et al. Opinions and practice patterns of obstetricians-gynecologists in the United States regarding amniocentesis in twins. Prenat Diag. 2013;33:899–903. doi: 10.1002/pd.4164. [DOI] [PubMed] [Google Scholar]