Abstract
In older adults, sedentary time is positively associated with obesity. The manner in which it is accumulated, i.e., the number of breaks in sedentary time, might be also important. We examined the cross-sectional associations of breaks in sedentary time with abdominal obesity in 301 older adults (111 men and 190 women) aged 75.0 ± 6.8 years. Sedentary time (counts min−1 < 100) and physical activity were objectively measured by accelerometry, worn during waking hours for at least three consecutive days. A break was defined as an interruption (≥100 counts min−1 < 2020) in sedentary time while performing light intensity physical activities. Sedentary time was expressed as the number of daily breaks in sedentary time or hourly breaks in sedentary time. Abdominal obesity was defined by waist circumference (men >102 cm; women >88 cm). Using binary logistic regression analyses, the odds for abdominal obesity decreased 7 % for each additional hourly break in sedentary time in women (OR = 0.93, 95 % CI: 0.87–1.00), but not men, independently of total sedentary time and moderate-to-vigorous physical activity. The odds for abdominal obesity were 3.21 times higher (p = 0.039) for women in quartile 1 (<225 breaks day−1) of daily breaks in sedentary time compared to those in quartile 4 (>353 breaks day−1) of daily breaks in sedentary time.
These findings indicate that older women who interrupt their sedentary time more frequently are less likely to present abdominal obesity. Public health recommendations regarding breaking-up sedentary time complementary to those for physical activity are likely to be relevant.
Keywords: Breaks, Sedentary time, Waist circumference, Physical activity, Older adults, Abdominal obesity
Introduction
Physical activity and sedentary behaviors are complex and distinct entities, and the lack of moderate-to-vigorous physical activity (MVPA) does not directly imply higher sedentary time. A paradigm shift proposes that inactivity physiology is qualitatively different from exercise physiology (Hamilton et al. 2007), groundbreaking a new conceptual framework based on epidemiological evidence linking sedentary behaviors directly with adverse health outcomes (Owen et al. 2014). Sedentary time’ patterns are generally represented by breaks in sedentary time considered in terms of how frequently sedentary bouts are interrupted. For example, two older adults may exhibit the same total amount of sedentary time but have different accumulation or breaking patterns during the day (Lord et al. 2011).
Geriatric population are the most sedentary group in the population—spending about 70 % (9 to 10 h day−1) of their waking hours in sedentary time (Baptista et al. 2012; Evenson et al. 2012; Healy et al. 2011a) and the least amount of time in MVPA (Baptista et al. 2012). They are also the age group that has the highest prevalence of abdominal obesity (Sardinha et al. 2012) which is associated with multiple co-morbidities (Kohrt 1998).
The associations of sedentary time with obesity have been reported for older adults independent of MVPA (Gennuso et al. 2013; Inoue et al. 2012; Swartz et al. 2012). Nevertheless, there are inconsistent findings concerning the role of sedentary time in abdominal obesity, with some studies in adults reporting no relation between overall sedentary time and abdominal fatness (McGuire and Ross 2012; Saunders et al. 2013). Disparities in associations for older adults have also been reported, with studies reporting an association of sedentary time with the presence of abdominal obesity in older women, but not in older men (Healy et al. 2011b; Scheers et al. 2012a). Understanding the pattern in which sedentary time is accumulated has been identified as a research priority and may explain these disparities in older adults (Lord et al. 2011; Swartz et al. 2012).
Recent studies using general samples of adults have found that, independent of MVPA levels and total sedentary time, more breaks in sedentary time are associated with lower adiposity (Ayabe et al. 2013; Chastin et al. 2012; Healy et al. 2011b; Oliver et al. 2012). One study has found relationships of breaks in sedentary time with overall fat mass among older adults (Chastin et al. 2012). However, no studies with older adults have examined how breaks in sedentary time are associated with being in the at-risk category for abdominal obesity. Based on this new paradigm and conceptual framework of a plausible independent role of sedentary time on adverse health outcomes, the purpose of this study was to examine the associations of total sedentary time and breaks in sedentary time with waist circumference—defined abdominal obesity in older adults.
Methods
Participants
This study included a sample of non-institutionalized Portuguese Caucasian older adults, aged 65–103 years. Participants were selected by proportionate stratified random sampling taking into account the number of people by age and gender in each region of mainland Portugal (Alentejo, Algarve, Centro, Lisboa e Norte), excluding the Madeira and Açores regions (Portuguese Archipelagos). A total of 401 participants were evaluated, of whom 301 aged 65 years or older (111 men and 190 women) had valid accelerometer data (≥ three days, including one weekend day, with ≥10 h of wear time day−1). The sample recruitment was carried out in senior universities, parish councils, city halls, day care centers, and health promotion fairs. Participants were included if they had independent physical functioning, determined by responses to the 12-item of Composite Physical Functioning Scale (Rikkli and Jones 1998), able to perform all basic and instrumental activities of daily living. All participants were informed about the possible risks of the investigation before giving their written informed consent to participate. All procedures were approved by the Ethics Committee of the Faculty of Human Kinetics, University of Lisbon, and were conducted in accordance with the Declaration of Helsinki for Human Studies (World Medical Association 2008).
Anthropometry
Participants were weighed to the nearest 0.01 kg while wearing minimal clothes and without shoes, on an electronic scale connected to a plethysmograph computer (BOD POD®, COSMED, Rome, Italy). Height was measured to the nearest 0.1 cm with a stadiometer (Seca, Hamburg, Germany) according to the standardized procedures described elsewhere (Lohman et al. 1988). Body mass index (BMI) was calculated as body mass (kg)/height2 (m) and classified into normal (<25 kg m−2), overweight (25–29.9 kg m−2), or obesity (≥30 kg m−2) (National Institutes of Health 1998). Waist circumference was measured according to NIH procedures used in the third US National Health and Nutrition Examination Survey (NHANES III 1988–1994) protocol (National Center for Health Statistics 1996) with a flexible anthropometric tape (Seca, Hamburg, Germany) at minimal respiration and reported to the nearest 0.1 cm by positioning a tape parallel to the floor and immediately above the iliac crest. Waist circumference was then dichotomized into normal or at risk category for abdominal obesity (men > 102 cm; women > 88 cm) (National Institutes of Health 1998).
Breaks in sedentary time and physical activity
Breaks in sedentary time and physical activity were assessed by accelerometry (ActiGraph, GT1M model, Fort Walton Beach, FL). The accelerometer is a small device that measures the acceleration of normal human movements ignoring high frequency vibrations associated with mechanical equipment. All participants were asked to wear the accelerometer on the right hip, near the iliac crest for at least three consecutive days, including two weekdays and one weekend day. The devices were activated on the first morning day, and data were recorded in 15-s epochs. Apart from accelerometer non-wear time (i.e., when it was removed for sleeping or water activities), periods of at least 60 consecutive minutes of zero activity intensity counts were also considered as non-wear time. A valid day was defined as having 600 min (10 h) or more of monitor wear, and the study included the results from participants with at least three valid days (including one weekend day). Each minute during which the accelerometer counts were below 100 was considered sedentary time; total sedentary time was the sum of sedentary minutes while the accelerometer was worn. A break in sedentary time was considered as any bout of time in which the accelerometer count rose up to or above 100 counts min−1 and which stayed within the light-intensity physical activity (LIPA) range (<2020 counts min−1). Accelerometer counts ≥100 min−1 were classified as active time, with further differentiation to identify separately LIPA (100 to 2019 counts min−1) and MVPA; ≥2020 counts min−1. The difference between LIPA and the daily breaks in sedentary time variable is that whereas LIPA is the total cumulative daily time spent in LIPA per day (min day−1), breaks in sedentary time represents the number of times sedentary time was broken by LIPA (breaks day−1). Data processing also derived the following variables: bouts of at least 1, 5, and 10 min of LIPA (bouts day−1); hourly breaks in sedentary time calculated as follows (60 × daily breaks in sedentary time) / daily accelerometer wear time in minutes.
Covariates
Self-reported sociodemographics, behavioral, and medical covariates were assessed via interviewer-administered questionnaires. Employment was dichotomized as employed or unemployed (includes retired) and educational attainment was categorized as the following: (1) no education, (2) 4 years of education, (3) 9 years of education, (4) 12 years of education, and (5) higher education. Geographical location of participants according to each region of mainland Portugal (Alentejo, Algarve, Centro, Lisboa e Norte) was also introduced as a covariate. Smoking status and alcohol dependence were reported and dichotomized in two categories (no and yes). Medical history for hypertension, elevated cholesterol and glycemia, current medication, and the presence of any long-standing condition such as diabetes, asthma, cancer, or cardiac disease were also reported and classified in two categories (no or yes).
Statistical analysis
Statistical analysis was performed using SPSS Statistics for Windows version 21.0, 2012 (SPSS Inc., an IBM Company, Chicago, IL, USA). Descriptive analyses included means ± SD for all measured variables. Bivariate correlations of sedentary time, LIPA, and MVPA were performed to verify the associations between physical activity variables. Binary logistic regression analyses were performed to examine associations of MVPA, quartiles of daily breaks in sedentary time (breaks day−1), and measured hourly breaks in sedentary time (breaks h−1) with the odds for abdominal obesity (National Institutes of Health 1998), adjusting for covariates retained in backwards elimination (p < 0.1): age, accelerometer wear time, total sedentary time (min day−1), employment, educational attainment, geographical location, smoking status, alcohol dependence, medical history for chronic disease, hypertension, elevated cholesterol and glycemia, current medication status, and MVPA (min day−1) or daily breaks in sedentary time (breaks day−1). Goodness-of-fit tests including the log likelihood ratio, the Cox and Snell R Square statistic, and the Hosmer and Lemeshow Test were used as indicators of model appropriateness, and the Wald statistic was used to test the significance level of individual independent predictor variables. To examine the differences in waist circumference between quartiles of daily breaks in sedentary time (breaks day−1) and test for linear effect of the association, a one-way analysis of variance (ANOVA) was used. To examine the differences in covariates between the two women’s subgroups, t tests were used.
Results
All results are reported by gender, as a significant gender × breaks in sedentary time interaction was observed (p = 0.016). Participants’ characteristics, according to gender, are shown in Table 1. On average, men and women spent 72 and 71 % of their waking hours sedentary, 24 and 26 % in LIPA, and 3.6 and 2.6 % in MVPA, respectively. The linear correlations of breaks in sedentary time with total sedentary time, LIPA, and MVPA were (r = −0.35; r = 0.67; and r = 0.30, respectively, p ≤ 0.001) for men and (r = −0.37; r = 0.64; and r = 0.29, respectively, p ≤ 0.001), for women. Of the women, 68 % were classified as abdominally obese; 28 % of the men were abdominally obese.
Table 1.
Participants’ characteristics according to gender
| Men (n = 111) | Women (n = 190) | |
|---|---|---|
| (Mean ± SD) or % (n) | ||
| Age (years) | 74.5 ± 6.78 | 75.0 ± 7.06 |
| Employment (%) | ||
| Employed | 24 (27) | 36 (68) |
| Retired | 76 (84) | 64 (122) |
| Education (%) | ||
| None | 4.5 (5) | 6.3 (12) |
| Primary school (4 years) | 65 (72) | 67 (128) |
| Secondary school (9 years) | 13 (14) | 11 (21) |
| High school (12 years) | 6.3 (7) | 3.7 (7) |
| Higher education (>12 years) | 7.2 (8) | 3.2 (6) |
| Smoker (%) | 4.5 (5) | 1.1 (2) |
| Alcohol dependent (%) | 2.7 (3) | 0.5 (1) |
| Medical (%) | ||
| Hypertensive | 42 (47) | 53 (100) |
| Hypercholesterolemia or impaired fasting glucose | 32 (35) | 50 (95) |
| Take medication | 89 (99) | 91 (173) |
| Known chronic disease | 36 (40) | 35 (66) |
| Anthropometrics | ||
| Height (m) | 1.66 ± 0.06 | 1.53 ± 0.06 |
| Body mass (kg) | 75.2 ± 11.0 | 64.8 ± 10.0 |
| BMI (kg m−2) | 27.4 ± 3.49 | 27.7 ± 3.83 |
| Waist circumference (cm) | 97.0 ± 10.3 | 93.5 ± 10.8 |
| Accelerometer variables | ||
| Total sedentary time (min day−1) | 598 ± 114 | 583 ± 122 |
| LIPA (min day−1) | 200 ± 90 | 214 ± 95 |
| MVPA (min day−1) | 30 ± 29 | 21 ± 23 |
| Daily breaks in sedentary time (breaks day−1) | 259 ± 81 | 308 ± 91 |
| Hourly breaks in sedentary time (breaks h−1) | 19 ± 5.6 | 23 ± 6.7 |
| >1 min LIPA bouts (bouts day−1) | 83 ± 44 | 88 ± 49 |
| >5 min LIPA bouts (bouts day−1) | 3.5 ± 4.4 | 3.2 ± 4.2 |
| >10 min LIPA bouts (bouts day−1) | 0.5 ± 0.8 | 0.4 ± 0.8 |
n number of participants, SD standard deviation, BMI body mass index, LIPA light intensity physical activity, MVPA moderate-to-vigorous physical activity
The associations of total sedentary time, MVPA, and hourly breaks in sedentary time with the odds for abdominal obesity are shown in Table 2.
Table 2.
Association of total sedentary time, LIPA, MVPA, and hourly breaks in sedentary time with abdominal obesity, by gender
| Men (n = 111) | Women (n = 190) | |||||
|---|---|---|---|---|---|---|
| Independent variables | β (SE) | OR (95 % CI) | p | β (SE) | OR (95 % CI) | p |
| Total sedentary time (min day−1) | 0.001 (0.001) | 1.00 (0.99–1.01) | 0.251 | 0.010 (0.01) | 1.00 (0.99–1.04) | 0.297 |
| LIPA (min day−1) | −0.001 (0.001) | 1.00 (0.99–1.00) | 0.135 | −0.001 (0.001) | 1.00 (0.99–1.00) | 0.135 |
| MVPA (min day−1) | −0.040 (0.020) | 0.96 (0.92–0.99) | 0.020 | −0.020 (0.001) | 0.98 (0.97–1.00) | 0.041 |
| Hourly breaks in sedentary time (breaks h−1) | −0.120 (0.070) | 0.89 (0.78–1.01) | 0.071 | −0.070 (0.040) | 0.93 (0.87–1.00) | 0.043 |
Data are unstandardized β coefficient ± standard error (SE) or odds ratio (OR) 95 % confidence interval (CI) adjusted for age, wear time, total sedentary time, employment, educational attainment, geographical location, smoking status, alcohol dependence, medical history for chronic disease, hypertension, elevated cholesterol and glycemia, and current medication status. LIPA light intensity physical activity, MVPA moderate-to-vigorous physical activity
For each additional hourly break in sedentary time, the odds of being abdominally obese decreased by 7 % (OR = 0.93, 95 % CI: 0.87–1.00) for women but was not significant for men (Table 2). Each daily 1-min in MVPA was associated with a 4 % (OR = 0.96, 95 % CI: 0.93–0.99) and 2 % lower (OR = 0.98, 95 % CI: 0.97–1.00) odds of abdominal obesity in men and women, respectively (Table 2). There were no significant associations of sedentary time or LIPA with abdominal obesity, for both men and women (p > 0.05). Being employed was associated with an 81 % higher (OR = 2.24, 95 % CI: 1.05–4.82) odds of abdominal obesity in women, but no associations with employment were found for men. Also, no associations of total sedentary time, LIPA, MVPA, daily or hourly breaks in sedentary time with BMI were found (data not shown; p ≥ 0.05). The characteristics of the two women’s subgroups were similar for most sociodemographic and medical covariates (Table 3).
Table 3.
Women characteristics according to subgroups: abdominal obese vs no abdominal obesity
| No abdominal obese (n = 59) | Abdominal obese (n = 131) | t test | |
|---|---|---|---|
| (Mean ± SD) or % (n) | p | ||
| Age (years) | 73.8 ± 6.54 | 75.5 ± 7.49 | 0.130 |
| Employment (%) | 0.228 | ||
| Employed | 29 (17) | 37 (49) | |
| Retired | 71 (42) | 62 (81) | |
| Education (%) | 0.005 | ||
| None | 3.4 (2) | 7.6 (10) | |
| Primary school (4 years) | 63 (37) | 73 (95) | |
| Secondary school (9 years) | 17 (10) | 9.2 (12) | |
| High school (12 years) | 10 (6) | 0.8 (1) | |
| Higher education (>12 years) | 6.8 (4) | 3.1 (4) | |
| Smoker (%) | 0.00 (0) | 1.5 (2) | 0.343 |
| Alcohol dependent (%) | 0.00 (0) | 0.8 (1) | 0.508 |
| Medical (%) | |||
| Hypertensive | 42 (25) | 56 (73) | 0.089 |
| Hypercholesterolemia or impaired fasting glucose | 46 (27) | 48 (63) | 0.846 |
| Take medication | 88 (52) | 91 (119) | 0.364 |
| Known chronic disease | 19 (11) | 41 (54) | 0.001 |
| Anthropometrics | |||
| Height (m) | 1.53 ± 0.06 | 1.53 ± 0.07 | 0.780 |
| Body mass (kg) | 58.5 ± 7.86 | 68.2 ± 9.27 | <0.001 |
| BMI (kg m−2) | 24.9 ± 2.93 | 29.0 ± 3.45 | <0.001 |
| WC (cm) | 81.7 ± 5.13 | 99.1 ± 7.70 | <0.001 |
| Accelerometer variables | |||
| Total sedentary time (min day−1) | 572 ± 99.4 | 594 ± 132 | 0.258 |
| LIPA (min day−1) | 232 ± 85.0 | 203 ± 98.0 | 0.054 |
| MVPA (min day−1) | 26 ± 24 | 18 ± 20 | 0.018 |
| Daily breaks in sedentary time (breaks day−1) | 325 ± 84 | 295 ± 94 | 0.038 |
| Hourly breaks in sedentary time (breaks h−1) | 24 ± 5.9 | 22 ± 7.0 | 0.113 |
| >1 min LIPA bouts (bouts day−1) | 93 ± 46 | 84 ± 50 | 0.222 |
| >5 min LIPA bouts (bouts day−1) | 3.1 ± 3.1 | 3.0 ± 4.6 | 0.911 |
| >10 min LIPA bouts (bouts day−1) | 0.4 ± 0.7 | 0.4 ± 0.8 | 0.963 |
n number of participants, SD standard deviation, BMI body mass index, WC waist circumference, LIPA light intensity physical activity, MVPA moderate-to-vigorous physical activity
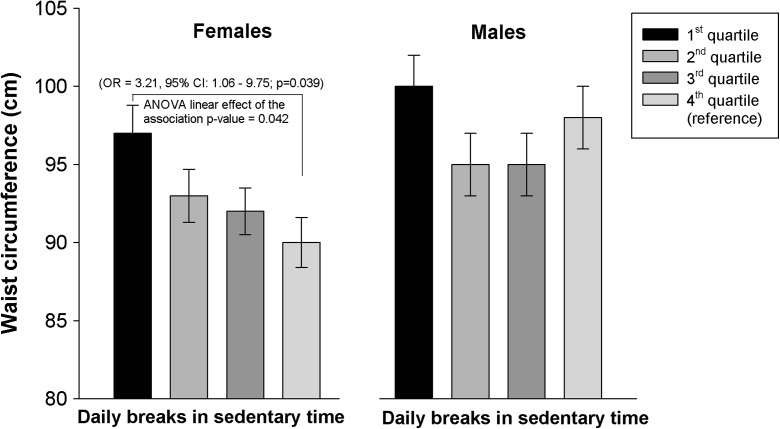
The odds for being abdominally obese were significantly higher in the lowest quartile of daily breaks in sedentary time compared to the highest quartile, for women (OR = 3.21, 95 % CI: 1.06–9.75) but not for men (OR = 4.33, 95 % CI: 0.81–23.3) (Fig. 1). The ANOVA results showed significant differences in waist circumference between quartile 1 of daily breaks in sedentary time (lowest number of breaks) and quartiles 2, 3, and 4 with mean differences of 4.21 cm (p = 0.048), 4.92 cm (p = 0.015), and 4.74 cm (p = 0.018) for women but no significant differences in men (p ≥ 0.05). After adjustment for covariates, only the difference between the fourth and first quartiles (mean 7.15 cm) remained significant (p = 0.042).
Fig. 1.
Waist circumference among quartiles of daily breaks in sedentary time, by gender. Adjusted for age, total sedentary time, MVPA, total wear time, employment, educational attainment, geographical location, smoking status, alcohol dependence, medical history for the presence of chronic diseases, hypertension, elevated cholesterol and glycemia, and current medication status. MVPA moderate-to-vigorous physical activity, OR odds ratio. *Significant OR for abdominal obesity between quartiles and the differences between quartiles’ waist circumference averages using one-way analysis of variance (ANOVA) to test for linear effect of the association are presented. Quartiles of daily breaks in sedentary time: quartile 1 (<225 breaks day−1); quartile 2 (225 to 297 breaks day−1); quartile 3 (297 to 353 breaks day−1); quartile 4 (>353 breaks day−1)
Discussion
The prevalence of obesity increases with age whereas waist circumference is a good indicator of abdominal obesity. Among elderly, it has been suggested that the use of this anthropometric indicator predicts morbidity and mortality. Furthermore, abdominal obesity is strongly and inversely associated with regular physical activity. However, few studies have examined the independent associations of sedentary time and breaks in sedentary time with abdominal obesity in geriatric population. Grounded on the new paradigm of a plausible independent role of sedentary time on adverse health outcomes and consistent with the findings of previous studies on the associations of breaks in sedentary time with adiposity indices (Ayabe et al. 2013; Healy et al. 2011b; Oliver et al. 2012; Scheers et al. 2012b), we found that older women who frequently interrupted their sedentary time were less likely to be in the higher range of abdominally obesity risk category, after controlling for total sedentary time, MVPA, sociodemographic, and medical covariates. While there were non-significant associations for men, there were 7 % lower odds of having abdominal obesity for every additional hourly break in sedentary time for women. For MVPA, there were statistically significant associations with the odds for abdominal obesity, for both men and women, with each daily minute in MVPA being associated with 4 and 2 % lower odds for abdominal obesity in men and women, respectively.
The different distribution of men and women being classified as having abdominal obesity (28 % of men and 68 % of women) may in part explain why there were no significant associations for breaks in sedentary time with the odds for abdominal obesity in men. Only 28 % of men compared to 68 % of women were abdominally obese which may have weakened the associations for the breaks in sedentary time with the odds for abdominal obesity. However, similar results were reported in a previous study that examined the linear associations of breaks in sedentary time with measures of total body fat mass (Chastin et al. 2012) and found these associations to be present only in women. Therefore, a potential gender dimorphism for the associations of breaks in sedentary time with abdominal obesity risk may exist (Scheers et al. 2012a), with women benefiting the most through more breaks in sedentary time. However, considering the different distribution of men and women within the abdominal obesity categories in our sample, our study is not powered to identify whether there is or is not a significant difference in the gender response to the breaks in sedentary time. This is a limitation that should be addressed in future investigations. Regardless, the present study showed that women who broke up sedentary time no more than 17 times an hour (225 breaks day−1) had an odds of being abdominally obese of 3.21, relative to those who broke up sedentary time more than 26 times an hour (353 breaks day−1).
We observed a significant inverse association of breaks in sedentary time with the odds of being in the abdominal obesity risk category. This finding is consistent with a previous study that examined linear associations of breaks in sedentary time with continuous measures of waist circumference, which also had a similar number of daily breaks in sedentary time (current study: 288 ± 88; (Henson et al. 2013): 273 ± 60). The odds for abdominal obesity were significantly lower in the highest quartile compared to the first quartile. The differences in waist circumference between daily breaks in sedentary time quartile 1 (lowest number of breaks) and quartiles 2, 3, and 4 (4.2, 4.9, and 4.7 cm lower waist circumference, respectively) are supported by a previous study in adults that found a similar trend (quartiles 2, 3, and 4 were all significantly different from quartile 1) (Healy et al. 2011b).
Similar to previous studies of older adults (Henson et al. 2013; Santos et al. 2012), lower MVPA but not total sedentary time or LIPA were associated with higher odds of abdominal obesity for both men and women. Moreover, the inverse association of MVPA with abdominal obesity was stronger in men compared to women, which in addition to the weaker associations of breaks in sedentary time with abdominal obesity in men, seemed to indicate that MVPA, rather than breaks in sedentary time may be of greater importance for controlling abdominal obesity in men. Since both the quartile categories of daily breaks in sedentary time and the continuous measures of breaks in sedentary time were associated with the odds for abdominal obesity, breaks in sedentary time, rather than total sedentary time or total LIPA, may be more relevant for abdominal obesity risk (Ando et al. 2013; Chastin et al. 2012). These cross-sectional findings together with findings on the metabolic syndrome (Bankoski et al. 2011) provide preliminary evidence that breaking up sedentary time may be important to target in the prevention of abdominal obesity in a geriatric population, especially for women (Chastin et al. 2012). These results should be confirmed in future prospective studies.
Findings from a small intervention study support this possibility, suggesting that regular variations in posture allocation may be an influential factor in the regulation of energy homeostasis (Swartz et al. 2011), a key factor in the development of obesity. Previous findings have demonstrated that sedentary time can be reduced by following a brief intervention based on goal setting and behavioral self-monitoring in older adults (Gardiner et al. 2011).
A randomized controlled trial (Ando et al. 2013) also found that breaking sedentary time more often may lead to efficient utilization of ingested fat by preventing decreased fat oxidation and as a result reduces fat deposition. Decreased fat oxidation with prolonged sedentary time has been observed in rats as a result of decreased heparin-releasable lipoprotein lipase activity, which directs consumed fat toward muscle (Zderic and Hamilton 2006). Recent human studies have been found that regular walking breaks of light intensity activities were more effective than continuous physical activity at decreasing postprandial glycemia and insulinemia in healthy, normal-weight adults (Dunstan et al. 2012; Peddie et al. 2013). Another study found that alternating standing and sitting in 30 min bouts results in modest beneficial effects on postprandial glucose responses in overweight/obese adults (Scheers et al. 2012a). Lower postprandial glycemia is indicative of a more efficient response to glucose ingestion and has been shown to be inversely associated with abdominal fat deposition (Khoury et al. 2010; Nakatsuji et al. 2010). These physiological changes may be underlying the associations of breaks in sedentary time with abdominal obesity and should be addressed in future investigations.
An important strength of our study is that sedentary time was objectively measured by accelerometry, but still, there is some limitation as accelerometers are not sensitive to detect all activities such as biking, standing, and upper body movement. Although the criteria that we considered to validate accelerometer data (≥3 days, including one weekend day, with ≥10 h of wear time day−1) has been used in large scale studies, this criteria may be less reliable than a 7-day period and therefore must be presented as a limitation. The cross-sectional design of this study limits inference about the direction of causality between the breaks in sedentary time and abdominal obesity. We cannot rule out the possibility that more breaks in sedentary time result from lower levels of adiposity. Moreover, based on the cutoffs for waist circumference (men > 102 cm; women > 88 cm), on average women were abdominally obese while men were in the normal category. The fact that men had lower levels of abdominal obesity may underlie the lack of significant associations of breaks in sedentary time with abdominal obesity in men.
The majority of participants in our study was retired and had no specific work context. Women who were employed had 81 % higher odds of being abdominal obese, compared with the retired women. We hypothesized that women who were retired may have more free time and therefore more opportunities to be physically active and break sedentary time more often. Also, the fact that women usually do more housework may justify why retired women present less odds for abdominal obesity compared with employed women.
The lack of association between employment and the odds for abdominal obesity in men may be explained by a lower contribution in housework, and therefore, a similar pattern can be found in both work and leisure time settings.
Another potential limitation is that considering only 36 % of our sample had medical problems like diabetes, asthma, cancer, or cardiac disease, our results cannot be generalized to people who have health problems. We also cannot rule out the possible residual confounding from potentially important unmeasured covariates like diet. Future studies would benefit from prospective designs to examine the association of breaks in sedentary time with abdominal obesity in both men and women.
These findings might have potential implications for the prevention of abdominal obesity in older adults. Our findings provide objective evidence that in older women, total sedentary time may not be the most important determinant for abdominal obesity but that additional to time spent in MVPA, the fragmentation of sedentary time may attenuate the development of abdominal obesity, especially in women. As such, programs engaged exclusively on MVPA may overlook an area that is of also of importance to obesity control. Along with messages related to accumulating at least 150 min week−1 of MVPA, older adults could also be encouraged to sit less and stand/walk more often, even with light intensity levels.
Conclusion
The present findings revealed an inverse association for the breaks in sedentary time with abdominal obesity in older women, using cross-sectional data. Therefore, older women that interrupted sedentary time more often were less likely to be abdominal obese independently of total sedentary time itself and MVPA levels.
Acknowledgments
Conflict of interest
There was no financial or any other kind of personal conflict of interest.
Author contributions
All authors meet the criteria for authorship stated in the Uniform Requirements Submitted to Biomedical Journals. PBJ, AMS, and LBS devised the idea for the study, and PBJ was responsible for the statistical analysis. All authors including DAS and FB were involved in interpreting the results of the analysis and critically reviewed the manuscript. All authors approved the final version.
Sponsor’s role
Júdice is supported by the Portuguese Foundation for Science and Technology (SFRH/BD/81403/2011). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
References
- Ando T, et al. Effects of intermittent physical activity on fat utilization over a whole day. Med Sci Sports Exerc. 2013;45:1410–1418. doi: 10.1249/MSS.0b013e3182885e4b. [DOI] [PubMed] [Google Scholar]
- Ayabe M, Kumahara H, Morimura K, Sakane N, Ishii K, Tanaka H. Accumulation of short bouts of non-exercise daily physical activity is associated with lower visceral fat in Japanese female adults. Int J Sports Med. 2013;34:62–67. doi: 10.1055/s-0032-1314814. [DOI] [PubMed] [Google Scholar]
- Bankoski A, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011;34:497–503. doi: 10.2337/dc10-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baptista F, et al. Prevalence of the Portuguese population attaining sufficient physical activity. Med Sci Sports Exerc. 2012;44:466–473. doi: 10.1249/MSS.0b013e318230e441. [DOI] [PubMed] [Google Scholar]
- Chastin SF, Ferriolli E, Stephens NA, Fearon KC, Greig C. Relationship between sedentary behaviour, physical activity, muscle quality and body composition in healthy older adults. Age Ageing. 2012;41:111–114. doi: 10.1093/ageing/afr075. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenson KR, Buchner DM, Morland KB (2012) Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Preventing chronic disease 9:E26. doi:E26 [pii] [PMC free article] [PubMed]
- Gardiner PA, Eakin EG, Healy GN, Owen N (2011) Feasibility of reducing older adults’ sedentary time. Am J Prev Med 41:174-177. doi:10.1016/j.amepre.2011.03.020S0749-3797(11)00266-2 [pii] [DOI] [PubMed]
- Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013 doi: 10.1249/MSS.0b013e318288a1e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- Healy GN, Clark BK, Winkler EA, Gardiner PA, Brown WJ, Matthews CE. Measurement of adults’ sedentary time in population-based studies. Am J Prev Med. 2011;41:216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32:590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson J, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56:1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- Inoue S, Sugiyama T, Takamiya T, Oka K, Owen N, Shimomitsu T. Television viewing time is associated with overweight/obesity among older adults, independent of meeting physical activity and health guidelines. J Epidemiol / Japan Epidemiol Assoc. 2012;22:50–56. doi: 10.2188/jea.JE20110054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury DE, Hwalla N, Frochot V, Lacorte JM, Chabert M, Kalopissis AD. Postprandial metabolic and hormonal responses of obese dyslipidemic subjects with metabolic syndrome to test meals, rich in carbohydrate, fat or protein. Atherosclerosis. 2010;210:307–313. doi: 10.1016/j.atherosclerosis.2009.11.017. [DOI] [PubMed] [Google Scholar]
- Kohrt WM. Abdominal obesity and associated cardiovascular comorbidities in the elderly. Coron Artery Dis. 1998;9:489–494. doi: 10.1097/00019501-199809080-00004. [DOI] [PubMed] [Google Scholar]
- Lohman TG, Roche AS, Martorell R. Anthropometric standardization reference manual. Champaign: Human Kinetics; 1988. [Google Scholar]
- Lord S, Chastin SF, McInnes L, Little L, Briggs P, Rochester L. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing. 2011;40:205–210. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- McGuire KA, Ross R. Incidental physical activity and sedentary behavior are not associated with abdominal adipose tissue in inactive adults. Obesity (Silver Spring) 2012;20:576–582. doi: 10.1038/oby.2011.278. [DOI] [PubMed] [Google Scholar]
- Nakatsuji H, Kishida K, Kitamura T, Nakajima C, Funahashi T, Shimomura I. Dysregulation of glucose, insulin, triglyceride, blood pressure, and oxidative stress after an oral glucose tolerance test in men with abdominal obesity. Metab Clin Exp. 2010;59:520–526. doi: 10.1016/j.metabol.2009.08.013. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics N . NHANES III anthropometric procedures video. Washington, DC: U.S. Government Printing Office; 1996. [Google Scholar]
- National Institutes of Health Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults–the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- Oliver M, Schluter PJ, Healy GN, Tautolo ES, Schofield G, Rush E (2012) Breaks in sedentary time—associations with body size in pacific mothers and their children: findings from the Pacific Islands Families Study. J Phys Act Health [DOI] [PubMed]
- Owen N, Salmon J, Koohsari MJ, Turrell G, Giles-Corti B. Sedentary behaviour and health: mapping environmental and social contexts to underpin chronic disease prevention. Br J Sports Med. 2014;48:174–177. doi: 10.1136/bjsports-2013-093107. [DOI] [PubMed] [Google Scholar]
- Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr. 2013 doi: 10.3945/ajcn.112.051763. [DOI] [PubMed] [Google Scholar]
- Rikkli RE, Jones CJ. The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults. J Aging Phys Activ. 1998;6:363–375. [Google Scholar]
- Santos DA, Silva AM, Baptista F, Santos R, Gobbo LA, Mota J, Sardinha LB. Are cardiorespiratory fitness and moderate-to-vigorous physical activity independently associated to overweight, obesity, and abdominal obesity in elderly? Am J Hum Biol. 2012;24:28–34. doi: 10.1002/ajhb.21231. [DOI] [PubMed] [Google Scholar]
- Sardinha LB, et al. Prevalence of overweight, obesity, and abdominal obesity in a representative sample of Portuguese adults. PLoS One. 2012;7:e47883. doi: 10.1371/journal.pone.0047883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders TJ, Tremblay MS, Despres JP, Bouchard C, Tremblay A, Chaput JP. Sedentary behaviour, visceral fat accumulation and cardiometabolic risk in adults: a 6-year longitudinal study from the Quebec Family Study. PLoS One. 2013;8:e54225. doi: 10.1371/journal.pone.0054225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheers T, Philippaerts R, Lefevre J. Patterns of physical activity and sedentary behavior in normal-weight, overweight and obese adults, as measured with a portable armband device and an electronic diary. Clin Nutri (Edinburgh, Scotland) 2012;31:756–764. doi: 10.1016/j.clnu.2012.04.011. [DOI] [PubMed] [Google Scholar]
- Scheers T, Philippaerts R, Lefevre J. SenseWear-determined physical activity and sedentary behavior and metabolic syndrome. Med Sci Sports Exerc. 2012 doi: 10.1249/MSS.0b013e31827563ba. [DOI] [PubMed] [Google Scholar]
- Swartz AM, Squires L, Strath SJ. Energy expenditure of interruptions to sedentary behavior. Int J Behav Nutr Phys Activ. 2011;8:69. doi: 10.1186/1479-5868-8-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz AM, Tarima S, Miller NE, Hart TL, Grimm EK, Rote AE, Strath SJ. Prediction of body fat in older adults by time spent in sedentary behavior. J Aging Phys Act. 2012;20:332–344. doi: 10.1123/japa.20.3.332. [DOI] [PubMed] [Google Scholar]
- World Medical Association Declaration of Helsinki—ethical principles for medical research involving human subjects. WMJ. 2008;54:122–125. [Google Scholar]
- Zderic TW, Hamilton MT. Physical inactivity amplifies the sensitivity of skeletal muscle to the lipid-induced downregulation of lipoprotein lipase activity. J Appl Physiol. 2006;100:249–257. doi: 10.1152/japplphysiol.00925.2005. [DOI] [PubMed] [Google Scholar]