Abstract
Objective
Examine the efficacy of a personalized, modular cognitive-behavioral therapy (CBT) protocol among early adolescents with high-functioning autism spectrum disorders (ASD) and co-occurring anxiety relative to treatment as usual (TAU).
Method
Thirty-one children (11–16 years) with ASD and clinically significant anxiety were randomly assigned to receive 16 weekly CBT sessions or an equivalent duration of TAU. Participants were assessed by blinded raters at screening, post-treatment, and 1-month follow-up.
Results
Youth randomized to CBT demonstrated superior improvement across primary outcomes relative to those receiving TAU. Eleven of 16 adolescents randomized to CBT were treatment responders, versus 4/15 in the TAU condition. Gains were maintained at 1-month follow-up for CBT responders.
Conclusions
These data extend findings of the promising effects of CBT in anxious youth with ASD to early adolescents.
Clinicaltrials.gov trial reference number
NCT01563003. Internet links: http://clinicaltrials.gov/show/NCT01563003
Keywords: Autism Spectrum Disorder, Anxiety, Adolescents, Cognitive-behavioral therapy, Obsessive-compulsive disorder
Autism spectrum disorders (ASD), including Autism, Asperger’s Syndrome, and Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS), are complex neurodevelopmental disorders that occur in approximately 1 in 68 North American children.1‡ Although the hallmark features of ASD include social, communication, and cognitive impairment,2 anxiety disorders are commonly comorbid3, 4 and confer significant disability above and beyond the ASD diagnosis.5–7
Given the frequency and deleterious consequences associated with anxiety disorder comorbidity, attention has been given to developing and evaluating effective treatments. Cognitive-behavioral therapy (CBT) adapted for the clinical characteristics of youth with ASD and anxiety has demonstrated strong efficacy relative to waitlist and treatment as usual (TAU) controls in reducing anxiety symptomology in children with ASD.8–11 Relative to children with ASD and anxiety, comparatively fewer studies have examined CBT among early adolescents with ASD. Yet, adolescents present with different clinical and treatment challenges compared to children requiring the creation and evaluation of developmentally tailored interventions. For example, social functioning becomes more salient in adolescents versus children with ASD, with adolescents becoming increasingly aware of their social status and skill impairments,12 having more academic stress, and being at risk for social avoidance and peer victimization.13, 14 Clinical presentation of adolescents is characterized by increased frequency of depression and anhedonia,15 externalizing behaviors,16 and the potential for limited motivation to engage in treatment.17
Building on positive case series data,18–20 three randomized controlled trials have been reported in adolescents with ASD and comorbid anxiety. Wood et al. 21 randomized 33 adolescents (11–15 years) to 16 CBT sessions using a developmentally modified version of the Behavioral Interventions for Anxiety in Children with Autism (BIACA; see below for description)11 manual or an equivalent waitlist period. The CBT group experienced significantly greater reductions in clinician-rated anxiety severity relative to the waitlist arm (d=.74); 79% of the CBT group versus 28.6% of the waitlist group were treatment responders although no differences in rates of anxiety diagnostic remission were found. White et al. 22 randomized 30 adolescents (12–17 years) to Multimodal Anxiety and Social Skills Intervention (MASSI) or an equivalent duration waitlist control. MASSI is a modularized CBT intervention delivered in individual (up to 13 sessions), group (7 sessions) and parent education/coaching sessions (at the end of individual therapy sessions).18, 22 Modules were chosen for individual sessions based on the individual’s needs and included psychoeducation, coping and problem solving skills, and exposure therapy. Group sessions focused on structured social skills training. No significant group differences were found on anxiety outcomes with generally small effect sizes. Relative to the waitlist arm, the CBT arm demonstrated large improvements in social functioning (d=1.03). Russell et al. 23 randomized 46 adolescents and adults (14–65 years; M=26.9 years) with ASD and comorbid obsessive-compulsive disorder (OCD) to CBT or Anxiety Management (AM), which consisted of psychoeducation about mood and a healthy lifestyle, diaphragmatic breathing, progressive muscle relaxation, and problem solving training. There were no statistically significant group differences although the within-group effect size for the CBT arm was large (d=1.01 versus .6 for the AM arm) and more participants responded to CBT versus AM (45% versus 20%).
In light of the mixed findings among adolescents, the need to examine the potential of CBT relative to a control condition that allows for active intervention, and the need to determine effective treatment strategies for this cohort, we examined the relative efficacy of a modular CBT approach tailored for early adolescents with ASD and anxiety relative to TAU. Relative to TAU, we expected that the CBT group would demonstrate superior reductions in clinician-rated anxiety severity, and higher response and remission rates. A secondary aim was to examine treatment effects on youth-reported anxiety, and parent-rated youth anxiety, internalizing and externalizing symptoms, and psychosocial impairment; we expected CBT to outperform TAU on each outcome. Finally, we examined the short-term maintenance of treatment gains for CBT responders.
Method
Participants
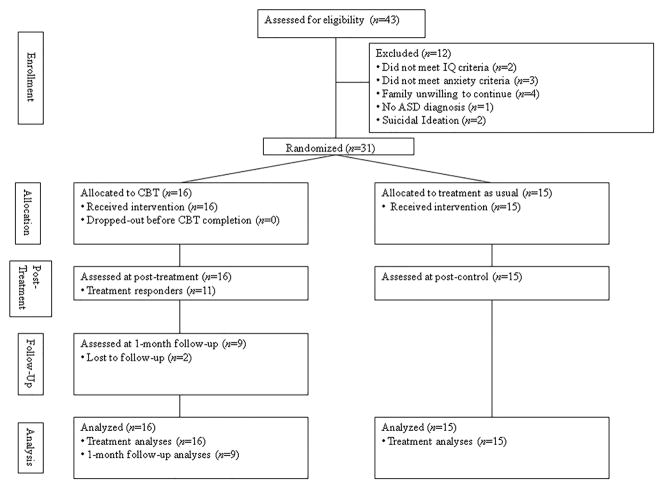
Thirty-one adolescents between the ages of 11–16 years (M=12.74, SD=1.34) participated. Youth met criteria for: 1) a diagnosis of autism, Asperger’s syndrome, or PDD-NOS; 2) a co-occurring anxiety diagnosis of separation anxiety disorder (SAD), generalized anxiety disorder (GAD), OCD, or social phobia; 3) a score ≥13 on the Pediatric Anxiety Rating Scale (PARS);24 and 4) an IQ ≥80 evaluated by the Wechsler Abbreviated Scale of Intelligence25 or review of standardized testing occurring in the prior two years. Primary anxiety diagnoses were determined using the Anxiety Diagnostic Interview Schedule-Child and Parent versions (ADIS-IV-C/P).26 At least one anxiety disorder with a Clinical Severity Rating (CSR) of ≥4 was required; the diagnosis with the highest CSR was deemed primary. Individuals randomized to CBT and who were on an established medication regime maintained their medication dosage for the duration of participation (youth randomized to TAU could make adjustments). Medications (if applicable) were stable at their present dose for 6 (antipsychotics, ADHD medications) or 8 weeks (e.g., antidepressants) prior to study enrollment for all participants, regardless of condition. Exclusion criteria included the following: 1) Initiation of new medications within 6 (antipsychotics, ADHD medications) or 12 weeks (antidepressants) before study enrollment; 2) Concurrent participation in psychotherapy, social skills training over 90 minutes per week, or other programmatic behavioral interventions (e.g., applied behavioral analysis); 3) Active suicidality; 4) Lifetime history of mania, psychosis, or substance abuse. Descriptive information is displayed in Table 1. Figure 1 displays the CONSORT diagram.
Table 1.
Demographic and clinical information as a function of treatment condition
| Measure | CBTa n=16 |
TAUa n=15 |
pb |
|---|---|---|---|
| Child sex (male) | 12 (75.0%) | 13 (86.7%) | .65 |
| Child age | 12.75 (1.24) | 12.73 (1.49) | .97 |
| Parent sex (female) | 15 (93.8%) | 15 (100.0%) | 1.00 |
| Parent graduated from college | 8 (50.0%) | 6 (40.0%) | .72 |
| Parent married | 12 (75.0%) | 12 (80.0%) | 1.00 |
| Child ethnicity/race | |||
| Caucasian | 12 (75.0%) | 14 (93.3%) | .33 |
| Asian/Pacific islander | 1 (6.3%) | 0 (0%) | 1.00 |
| Latino/a | 3 (18.8%) | 1 (6.7%) | |
| Autism spectrum disorders | |||
| Autistic disorder | 4 (25.0%) | 5 (33.3%) | .70 |
| PDD-NOS | 6 (37.5%) | 2 (13.3%) | .22 |
| Asperger’s syndrome | 6 (37.5%) | 8 (53.3%) | .48 |
| Primary anxiety disorder | |||
| Social phobia | 7 (43.8%) | 8 (53.3%) | .72 |
| SAD | 0 (0.0%) | 2 (13.3%) | .23 |
| OCD | 3 (18.8%) | 2 (13.3%) | 1.00 |
| GAD | 6 (37.5%) | 3 (20.0%) | .43 |
| Number of anxiety diagnoses | 2.75 (1.29) | 2.80 (0.77) | .90 |
| Other comorbid diagnoses | |||
| Social phobia | 6 (37.5%) | 6 (40.0%) | 1.00 |
| SAD | 3 (18.8%) | 3 (20.0%) | 1.00 |
| OCD | 3 (18.8%) | 1 (6.7%) | .60 |
| GAD | 9 (56.3%) | 9 (60.0%) | 1.00 |
| ADHD | 9 (56.3%) | 8 (53.3%) | 1.00 |
| Dysthymia/MDD | 3 (18.8%) | 4 (26.7%) | .69 |
| ODD/CD | 3 (18.8%) | 4 (26.7%) | .69 |
| Specific phobia | 6 (37.5%) | 8 (53.3%) | .48 |
| Selective mutism | 3 (18.8%) | 0 (0%) | .23 |
| Panic disorder | 1 (6.3%) | 0 (0%) | 1.00 |
| PTSD | 1 (6.3%) | 2 (13.3%) | .60 |
| Sleep terror disorder | 0 (0%) | 1 (6.7%) | .48 |
| Psychiatric medication use | |||
| SSRI | 7 (43.8%) | 6 (40.0%) | 1.00 |
| Stimulant, atomoxetine, or guanfacine | 8 (50.0%) | 9 (60.0%) | .72 |
| Atypical antipsychotic | 2 (12.5%) | 3 (20.0%) | .65 |
| Anticonvulsant | 0 (0%) | 1 (6.7%) | .48 |
| Trazodone | 0 (0%) | 1 (6.7%) | .48 |
| Benzodiazepine | 0 (0%) | 1 (6.7%) | .48 |
| Family financial statusc | |||
| Under $40,000 | 4 (25.0%) | 1 (7.7%) | .34 |
| Between $40,001-$90,000 | 6 (37.5%) | 6 (46.2%) | .72 |
| Over $90,000 | 6 (37.5%) | 6 (46.2%) | .72 |
Note. CBT=Cognitive-behavioral therapy; TAU=treatment as usual; PDD-NOS=pervasive developmental disorder not otherwise specified; SAD=separation anxiety disorder; OCD=obsessive-compulsive disorder; GAD=generalized anxiety disorder; ADHD=attention deficit hyperactivity disorder; MDD=major depressive disorder; ODD=oppositional defiant disorder; CD=conduct disorder; PTSD=posttraumatic stress disorder; SSRI=selective serotonin reuptake inhibitor.
Column values represent N (%) for categorical values and Mean (SD) for continuous variables
p-value based on independent t-test for continuous variables and Fisher’s exact test for categorical variables
Two parents in the TAU condition provided only personal financial status and did not report family financial status; the missing data rate between groups was non-significant at the p<.05 level, and only complete data were used in financial status comparisons
Figure 1.
Procedure
This study was approved by the local institutional review board. Services were provided in a university-based, multidisciplinary behavioral health clinic specializing in the treatment of pediatric anxiety in youth with and without ASD. Interested families were phone screened and those meeting initial criteria were scheduled for a screening assessment at which informed consent and assent were obtained from the legal guardian and youth. The screening assessment was completed over two days. The first visit focused on anxiety assessment (i.e., ADIS-IV-C/P, PARS), while the second visit approximately one week later included autism-specific assays. Subjects who were eligible were randomized at the end of the second visit using a computer-generated algorithm in a 1:1 ratio to receive either CBT or TAU. Therapists were assigned at random. The post-treatment assessment, identical to the anxiety-focused pre-treatment assessment, was completed after the 16th therapy session or 16th week in TAU. Responders to CBT completed a follow-up assessment one month following their post-treatment assessment. All participants completed their respective treatment arm.
Clinician-rated measures were administered by trained graduate-level independent evaluators that were blind to intervention condition. Training consisted of instructional meetings about study measures and multiple practice administrations with confederates and under observation. Blindness was maintained by verbal and written reminders to families at assessments, maintaining the IE in a separate wing of the clinic to minimize inadvertent contact with participants, and holding separate weekly supervision meetings regarding assessment and treatment. Twenty percent of audio-recorded assessments of the PARS were randomly selected and reviewed for integrity purposes by a second clinician. Inter-rater agreement was high for the PARS (intraclass correlation coefficient = .93).
Measures
Autism spectrum diagnoses were determined at screening via best estimate procedures.27 This procedure involved the administration of the Autism Diagnosis Interview–Revised (ADI-R)28 in all youth and either the Childhood Autism Rating Scale29 (n=19) or Autism Diagnosis Observation Schedule30 (n=8) by a certified doctoral-level evaluator.§ Thereafter, complete consensus between two clinicians regarding the ASD diagnosis was required for inclusion. All parent-, child-, and clinician-rated measures were completed at the pre-, post-treatment, and follow-up assessments, unless otherwise noted.
ADIS-IV-C/P26
The ADIS-IV-C/P is a psychometrically-sound semi-structured interview administered to the parent and child separately to assess the presence and severity of anxiety and comorbid disorders (e.g., attention deficit-hyperactivity disorder). The rater made the final determination regarding child diagnoses based on parent/child report and clinical judgment. The rater determines the presence of varied disorders, including a CSR, ranging from 0 to 8, for endorsed conditions.
Pediatric Anxiety Rating Scale (PARS)24
The PARS is a psychometrically sound24, 31 clinician-administered measure that assesses anxiety symptom presence and severity over the prior week. The symptom checklist assesses the presence of a variety of anxiety symptoms. The PARS severity scale ranges from 0 to 30, with scores over 12 consistent with moderate levels of anxiety and a diagnosis of an anxiety disorder.24, 32 The PARS has excellent psychometric properties in youth with ASD and anxiety.31
Clinical Global Impression-Severity and -Improvement (CGI-Severity, CGI-Improvement; Guy, 1976)
The CGI contains two single-item scales of severity and change in psychological symptoms. The CGI-Severity, ranging from 0 (“no symptoms/illness”) to 6 (“extremely severe symptoms”), reflects the overall severity of anxiety symptoms and associated interference. The CGI-Improvement, anchored by “very much worse” to “very much improved” ratings, captures improvement or worsening of anxiety symptoms. The CGI-Severity was rated at each assessment; CGI-Improvement was completed at the post-treatment and follow-up assessments.
Service Assessment for Children and Adolescents-Service Use Scale (SACA)33
The SACA is a standardized, psychometrically-sound33, 34 measure used to assess utilization history of a broad spectrum of mental health services (e.g., inpatient, outpatient, school-based, pharmacotherapy).
Columbia Impairment Scale-Parent (CIS-P)35
The CIS-P is a psychometrically-sound parent-rated questionnaire assessing parental perceptions of functional impairment experienced by the youngster across social, family, and school domains.
Child Behavior Checklist (CBCL)36
The CBCL assessed parental reports of youth internalizing and externalizing symptoms.
Multidimensional Anxiety Scale for Children–Parent (MASC-P)
The MASC-P is a 39-item parent-report measure of youth anxiety with established psychometric properties37 and treatment sensitivity in youth with ASD.11
Social Responsiveness Scale (SRS)38
The SRS is a psychometrically-sound38 parent-rated measure of social functioning in children with ASD with subdomains assessing social awareness, social information processing, capacity for reciprocal social communication, social anxiety/avoidance, and autistic preoccupations and traits.
Revised Child Anxiety and Depression Scales (RCADS)
The RCADS is a psychometrically sound39, 40 47-item youth-report measure of anxiety and depressive symptoms.
Treatment
Cognitive-Behavioral Therapy
Participants received 16 weekly, individual CBT sessions according to a developmentally modified version of the BIACA treatment manual11 that was used in Wood et al. 21 In that study, revisions were made to make the materials practical for early adolescents and account for issues relevant to adolescents (e.g., social issues, motivation, comorbidity). Sessions lasted between 60–90 minutes, and were provided modularly and selected by the therapist and supervisor prior to the visit based on clinical appropriateness (see Table 2 for a listing of modules). For each child, a minimum of three sessions were spent developing coping skills (e.g., behavioral activation, cognitive restructuring) with at least eight sessions of exposure therapy. Beyond these core components (which could be used more often if appropriate), additional modules were implemented as needed to address social and adaptive skill deficits/problems, poor motivation, social/school issues, and comorbid conditions. In a slight departure from Wood et al., parents were included for the vast majority of sessions (i.e., during child and parent oriented modules) given the low treatment motivation often seen in this cohort, as well as to facilitate treatment progress and generalization (e.g., implementing exposures outside of session, scheduling peer activities, implementing reward system), promote autonomy and communication skills, and problem solve treatment barriers. For all youth, treatment was concluded with a termination module that addressed relapse prevention and continuing treatment progress.
Table 2.
Behavioral Interventions for Anxiety in Children with Autism Session Modules
| Individual Therapy Modules | |
|---|---|
| Parent | Youth |
Core Modules
|
Core Modules
|
Social Intervention Modules
|
Social Intervention Modules
|
School Module
|
OCD Focused Module
|
Support Module
|
Support Module
|
Therapy was delivered by post-doctoral fellows or doctoral students in clinical or school psychology with at least one year of experience in CBT for childhood anxiety. Clinical supervision with a doctoral-level psychologist was held weekly. To ensure treatment adherence, 20% of audio-recorded sessions were randomly selected for review. Good adherence to the treatment manual was noted for therapist competence (4.6/5.0), therapist flexibility (4.7/5.0), therapeutic alliance (4.9/5.0), and adherence to session components (4.1/5.0). Most participants randomized to CBT (15/16; 93.7%) received services in addition to study psychotherapy including psychiatric medication management (n=10; 62.5%), school counseling (n=5; 31.3%) or special education services (n=8; 50%). Regarding the number of services, 1 (6.3%) youth received no services, 9 (56.3%) youth received one service, 4 (25%) youth received two services and 2 (12.5%) youth received three services. Six out of 16 (37.5%) adolescents were not taking any psychiatric medication while 4 (25%) adolescents were taking one medication and 6 (37.5%) adolescents were taking two or more.
Treatment as Usual
If randomized to TAU, participants were able to seek any psychosocial or pharmacological treatment that they chose, or to not seek treatment, for 16 weeks. Subjects continued with preexisting medications or therapy or were able to initiate dosage changes or new medications with the prescribing provider. The research team did not influence the parents’ decision in treatment choices. Using the SACA at the post-assessment, 14 out of 15 participants randomized to TAU received psychological or psychiatric services, including medication management (n=10; 66.7%), school counseling (n=2; 13.3%), special education services (n=9; 60.0%), social skills training (n=1; 6.7%) or individual psychotherapy (n=3; 18.8%). One participant did not receive any services, 5 (33.3%) participants received one service, 7 (46.7%) participants received two services, and 2 (13.3%) participants received three or more services. A majority of youth in this arm were prescribed psychiatric medication (n=10; 66.7%) with 3 (20.0%) youth taking one medication and 7 (46.7%) youth taking two or more medications. All TAU participants were offered and accepted CBT following the post-treatment assessment.
Analytic Plan
Group differences at post-treatment for continuous outcomes were analyzed via ANCOVAs, with post-treatment scores being predicted by treatment condition while covarying for baseline scores, and via Fisher’s exact tests for dichotomous variables. Given the nascent state of this literature, as well as the a priori nature of all hypotheses, no type 1 error correction was used. At 1-month follow-up, in order to evaluate changes in symptoms for participating CBT responders (n=9; 2 were lost to follow-up), paired t-tests were conducted for continuous outcomes, and differences in categorical treatment outcomes were evaluated using binomial proportion tests. Effect sizes for continuous variables were computed and converted to Cohen’s d using formulae provided by Cooper et al., 41 where values of d of .2, .5, and .8 correspond to small, medium, and large effects respectively.42 Assuming an effect size of d=0.8 by using past CBT trials for youth with comorbid anxiety and ASD as precedent,8, 21 power to detect group differences was 0.87. Following precedent, treatment response was defined as a CGI-Improvement rating of “much improved” or “very much improved”.43 Symptom remission was classified as having a severity rating on the ADIS-IV-C/P CSR ≤3 for the primary anxiety diagnosis.
Missing data were addressed by PROC-MI in SAS 9.344 using predictive mean matching via the fully conditional specification method. Following recommendations by Graham,45 missing data was in the acceptable range for multiply-imputed models (3.5%), and auxiliary covariates were used in imputation models (a process which can take data that is not missing at random and produce estimates that are consistent with those that meet the missing at random assumption46), where covariates included all timepoints for the outcome under analysis question as well as treatment group (1-month follow-up scores were not used as a covariate in post-treatment comparisons, and treatment group was not used in follow-up analyses as all participants were randomized to CBT). Degrees of freedom for multiply imputed hypothesis-testing models were adjusted based on recommendations by Barnard and Rubin,47 and 100 imputations were employed.
Results
Post-Treatment Comparisons
Descriptive and inferential statistics for baseline, post-treatment, and 1-month follow-up are in Table 3. Significant group differences at post-treatment were observed for all continuous clinician-rated measures, including the PARS (d=0.79), ADIS CSR (d=1.30), and CGI-Severity rating (d=0.94). With regard to categorical outcomes at post-treatment, 68.8% of those in the CBT group were treatment responders, compared to 26.7% of those in the TAU group (p=0.03). In considering post-treatment diagnostic status on the ADIS-C/P, 37.5% of those in the CBT condition no longer met diagnostic criteria for their primary diagnosis at post-treatment, whereas no participants in the TAU condition met criteria for diagnostic remission (p=0.02).
Table 3.
Descriptive and Inferential statistics for the CBT and TAU Conditions.
| Measure | Baseline | Post-treatment | Follow-up | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| CBT M (SD) |
TAU M (SD) |
CBT M (SD) |
TAU M (SD) |
tx | dx | CBT M (SD) |
ty | dy | tz | dz | |
| PARS | 15.81 (1.64) | 15.67 (2.50) | 10.94 (3.91) | 13.93 (3.56) | 2.21* | 0.79 | 9.78 (3.38) | −0.38 | −0.13 | 6.15** | 2.05 |
| ADIS CSRa | 5.50 (1.03) | 5.73 (0.80) | 3.69 (1.35) | 5.33 (0.90) | 3.84** | 1.30 | 2.47 (2.31) | 1.08 | 0.39 | 4.01** | 1.44 |
| CGI-Severity | 3.69 (0.60) | 3.93 (0.80) | 2.88 (0.72) | 3.67 (0.82) | 2.68* | 0.94 | 2.67 (0.50) | 0.00 | 0.00 | 5.55** | 1.85 |
| SRS | |||||||||||
| Awareness | 12.50 (3.60) | 14.47 (3.14) | 10.00 (3.29) | 13.27 (3.06) | 2.31* | 0.75 | 8.11 (2.09) | 1.81 | 0.60 | 3.90** | 1.30 |
| Cognition | 19.06 (5.87) | 20.67 (5.64) | 14.69 (5.40) | 19.80 (5.35) | 2.77** | 0.76 | 10.89 (4.43) | 4.66** | 1.55 | 8.40** | 2.80 |
| Communication | 38.06 (8.57) | 38.13 (9.44) | 27.13 (8.52) | 36.67 (9.20) | 3.75** | 1.13 | 19.78 (5.04) | 3.57** | 1.19 | 6.49** | 2.16 |
| Motivation | 18.19 (5.90) | 18.33 (5.59) | 15.13 (6.62) | 17.53 (6.60) | 1.28 | 0.35 | 10.11 (3.37) | 3.38** | 1.13 | 3.63** | 1.21 |
| Mannerisms | 18.13 (5.98) | 21.33 (6.07) | 14.00 (8.22) | 20.13 (5.99) | 1.76 | 0.52 | 7.78 (3.93) | 4.18** | 1.39 | 8.37** | 2.79 |
| Total | 105.94 (22.64) | 112.93 (24.77) | 80.94 (26.83) | 107.40 (24.53) | 2.80** | 0.84 | 56.67 (12.95) | 5.68** | 1.89 | 9.36** | 3.12 |
| RCADS | 27.94 (15.42) | 27.05 (20.86) | 23.86 (15.24) | 21.88 (17.19) | −0.30 | −0.09 | 23.12 (16.44) | −0.83 | −0.30 | 1.54 | 0.52 |
| MASC-P | 62.33 (19.99) | 64.37 (11.56) | 56.94 (17.52) | 58.62 (17.56) | 0.10 | 0.03 | 45.89 (19.69) | 1.12 | 0.44 | 1.23 | 0.44 |
| CIS-P | 23.52 (7.51) | 25.67 (7.45) | 17.24 (9.75) | 24.96 (8.91) | 2.58* | 0.59 | 18.00 (7.31) | −0.97 | −0.32 | 2.46* | 0.86 |
| CBCL | |||||||||||
| Internalizing | 28.12 (11.27) | 23.55 (8.16) | 18.79 (8.73) | 20.07 (6.89) | 1.94 | 0.48 | 17.33 (10.78) | −0.71 | −0.24 | 3.11* | 1.11 |
| Externalizing | 15.63 (10.03) | 15.70 (11.09) | 10.79 (8.48) | 15.92 (10.88) | 3.28** | 0.63 | 8.98 (6.77) | −0.98 | −0.40 | 1.48 | 0.56 |
Note.
p<.01;
p<.05
Clinical severity rating associated with principal diagnosis
Post-treatment analyses evaluated the effect of treatment condition while accounting for baseline group differences
Analyses compare 1-month follow-up to post-treatment status for treatment responders who returned for a follow-up assessment
Analyses compare 1-month follow-up to baseline status for treatment responders who returned for a follow-up assessment.
In considering group differences at post-treatment for parent- and child-report measures, significant improvements in overall autism functioning were observed on the SRS (d=0.84), with significant effects detected on the awareness (d=0.75), cognition (d=0.76), and communication (d=1.13) subscales, though observed differences on the motivation (d=0.35) and mannerisms (d=0.52) subscales were non-significant. In addition, significant improvements in the CBT versus TAU arm were observed with regard to overall functional impairment (d=0.59) and externalizing child behavior (d=0.63). No other significant differences were detected on parent- or child-reported anxiety symptoms.
Maintenance of Treatment Gains for Treatment Responders at 1-Month Follow Up
No significant decline in symptoms was observed on any measure (see Table 3), and significant improvements were observed for the SRS total score (d=1.89), as well as on the cognition (d=1.55), communication (d=1.19), motivation (d=1.13), and mannerisms (d=1.39) subscales, though no further change was seen on the awareness subscale (d=0.60). No changes were observed with regard to clinician-rated status of treatment response (p=.27) or diagnostic remission (p=.79).
Discussion
We report on the efficacy of a modular CBT program for early adolescents with ASD and comorbid anxiety. Consistent with Wood et al., 21 a personalized CBT intervention significantly reduced anxiety symptoms and impairment among this population with generally large effects observed across clinician-rated anxiety outcomes. Overall, 68.8% and 37.5% of participants were classified as treatment responders or remitters, which was superior to TAU and on par with past results among youth with ASD8, 21 and those who are typically developing.48 Responders to acute treatment maintained their gains over a one-month interval. This study is the second to support the efficacy of a modularized intervention for addressing anxiety in early adolescents. Notably, treatment of adolescents with ASD and anxiety has posed a significant challenge with some CBT trials failing to demonstrate superiority relative to waitlist49 and no established efficacious pharmacotherapy options. These data suggest that a personalized CBT protocol for early adolescents with ASD and anxiety that includes a robust dose of behavioral (i.e., exposure) and cognitive (i.e., cognitive therapy) strategies holds promise.
Improvements in social awareness, cognition and communication were found in the CBT arm relative to those randomized to TAU. Different from standard CBT approaches, modules in the present treatment approach targeted social interaction skills and taught youth how to manage ASD-related mannerisms (e.g., stereotyped interests). Group differences may reflect this specific focus. A potentially complementarily interpretation is that reduction in anxiety symptoms fosters improved social functioning, which has been shown previously.8, 50 Beyond improvements in ASD symptoms, reductions in functional impairment were significant and suggest the value of CBT in improving functional outcomes beyond anxiety symptomology.
No differences in child- and parent-reported child anxiety were found. This is not completely surprising for child-reports given evidence that many youth with ASD have difficulty reporting on anxiety,51 thus contributing to measurement error variance. Non-significant findings with parents may reflect the challenges of existing measures to capture child anxiety,52 and/or difficulty in differentiating anxiety from ASD symptoms53 and understanding functional determinants of anxiety. It is also possible that parents and youth across groups perceived reductions in child anxiety. Externalizing symptoms, which may be more directly observable, demonstrated improvements in the CBT arm relative to TAU. As anxiety symptoms improved, anxious triggers that evoke disruptive responses may have correspondingly improved. As well, modules in the present CBT protocol assisted parents in managing disruptive behavior, which may have translated into benefit.
There are several study limitations. First, an active control condition (e.g., relaxation therapy, pharmacotherapy) would be preferable to TAU. Although 93% of youth received intervention in the TAU arm, treatment was not standardized and potentially not maximized for many youth. On balance, the use of TAU is an improvement relative to waitlist controls, and allowed for the possibility of patient preference in treatment selection and minimized the use of costly and non-credible control interventions. Second, although our sample was powered to detect clinically meaningful main effects, we were not powered to examine treatment mediators and moderators. Third, the sample consisted primarily of Caucasian males. Although more males than females have ASD, it would be well-advised to examine treatment efficacy and acceptability in females in a more ethno-racially diverse sample. Finally, our short follow-up interval did not allow us to evaluate long-term treatment durability.
These data add to a growing literature supporting the efficacy of CBT for anxiety in children and adolescents with ASD. At this juncture, a large scale study is needed to examine treatment outcomes relative to standard care (i.e., non-ASD specific CBT) to determine differential efficacy, as well as treatment mediators and moderators to understand the mechanisms and who benefits from which intervention. As well, dissemination of treatment protocols into real world settings is needed. Examining the effectiveness of this intervention together with varied training models will promote the use of evidence-based care, exerting a more significant impact on illness trajectory.
Acknowledgments
The authors would like to acknowledge the contributions of Erika Crawford, Anna Jones, Michael Sulkowski, Ph.D., Robert Selles, Danielle Ung, Jeffrey J. Wood, Ph.D., and Monica Wu. Mr. De Nadai is supported by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award F31 MH094095 from the National Institute of Mental Health.
Footnotes
Autism spectrum disorders as conceptualized in the Diagnostic and Statistical Manual for Mental Disorders (DSM) Fourth Edition, Text Revision included Autism, Asperger’s Syndrome, and Pervasive Developmental Disorder Not Otherwise Specified. In the DSM-5, individual diagnoses were eliminated and the rubric of autism spectrum disorder was adopted to encompass individuals characterized by deficits in both social communication/interaction and restricted repetitive behaviors, interests, and activities.
The Autism Diagnosis Observation Schedule was initially administered. To reduce subject burden while maintaining the ability to comprehensively assess youth, we switched to the Childhood Autism Rating Scale.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health.
References
- 1.CDC. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63:1–21. [PubMed] [Google Scholar]
- 2.APA. Diagnostic and statistical manual of mental disorders. 5. Washington, D.C: American Psychiatric Association; 2013. [Google Scholar]
- 3.van Steensel FJ, Bogels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 2011;14(3):302–317. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gjevik E, Eldevik S, Fjaeran-Granum T, Sponheim E. Kiddie-SADS reveals high rates of DSM-IV disorders in children and adolescents with autism spectrum disorders. J Autism Dev Disord. 2011;41(6):761–769. doi: 10.1007/s10803-010-1095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaat AJ, Gadow KD, Lecavalier L. Psychiatric symptom impairment in children with autism spectrum disorders. J Abnorm Child Psychol. 2013;41(6):959–969. doi: 10.1007/s10802-013-9739-7. [DOI] [PubMed] [Google Scholar]
- 6.Ung DW, JJEM, Arnold E, Fujii C, Renno P, Murphy TK, Lewin A, Mutch PJ, Storch EA. Clinical characteristics of high functioning youth with autism spectrum disorders and anxiety. Neuropsychiatry. 2013;3:147–158. doi: 10.2217/npy.13.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Foc Autism Other Dev Dis. 2004;19:78–86. [Google Scholar]
- 8.Storch EA, Arnold EB, Lewin A, Nadeau J, Jones AM, de Nadai AS, Mutch PJ, Selles R, Ung D, Murphy T. The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with Autism Spectrum Disorders: A randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2013 doi: 10.1016/j.jaac.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Sofronoff K, Attwood T, Hinton S. A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. J Child Psychol Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- 10.Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: a randomized trial. J Child Psychol Psychiatry. 2012;53:410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wood JJ, Drahota A, Sze K, Har K, Chiu A, Langer DA. Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. J Child Psychol Psychiatry. 2009;50:224–234. doi: 10.1111/j.1469-7610.2008.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuusikko S, Pollock-Wurman R, Jussila K, Carter AS, Mattila ML, Ebeling H, Pauls DL, Moilanen I. Social anxiety in high-functioning children and adolescents with Autism and Asperger syndrome. J Autism Dev Disord. 2008;38(9):1697–1709. doi: 10.1007/s10803-008-0555-9. [DOI] [PubMed] [Google Scholar]
- 13.Shtayermman O. Peer victimization in adolescents and young adults diagnosed with Asperger’s syndrome: A link to depressive symptomatology, anxiety symptomatology, and suicidal ideation. Issues in Comprehensive Pediatric Nursing. 2007;30:87–107. doi: 10.1080/01460860701525089. [DOI] [PubMed] [Google Scholar]
- 14.Zablotsky B, Anderson C, Law P. The association between child autism symptomatology, maternal quality of life, and risk for depression. J Autism Dev Disord. 2013;43(8):1946–1955. doi: 10.1007/s10803-012-1745-z. [DOI] [PubMed] [Google Scholar]
- 15.Ghaziuddin M, Greden J. Depression in children with autism/pervasive developmental disorders: a case-control family history study. J Autism Dev Disord. 1998;28(2):111–115. doi: 10.1023/a:1026036514719. [DOI] [PubMed] [Google Scholar]
- 16.Green J, Gilchrist A, Burton D, Cox A. Social and psychiatric functioning in adolescents with Asperger syndrome compared with conduct disorder. J Autism Dev Disord. 2000;30(4):279–293. doi: 10.1023/a:1005523232106. [DOI] [PubMed] [Google Scholar]
- 17.Koegel RL, Mentis M. Motivation in childhood autism: can they or won’t they? J Child Psychol Psychiatry. 1985;26(2):185–191. doi: 10.1111/j.1469-7610.1985.tb02259.x. [DOI] [PubMed] [Google Scholar]
- 18.White SW, Albano AM, Johnson CR, Kasari C, Ollendick T, Klin A, Oswald D, Scahill L. Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clin Child Fam Psychol Rev. 2010;13(1):77–90. doi: 10.1007/s10567-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev. 2009;29(3):216–229. doi: 10.1016/j.cpr.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ehrenreich May J, Storch EA, Queen AH, Rodriguez JH, Ghilain CC, Alessandri M, Lewin AB, Arnold EA, Murphy TK, Lin CE, Fujii C, Renno P, Piacentini J, Laugeson EA, Wood JJ. An Open Trial of Cognitive Behavioral Therapy for Anxiety Disorders in Early Adolescents with Autism Spectrum Disorders. Focus on Autism and Other Developmental Disabilities. in press. [Google Scholar]
- 21.Wood JJ, Ehrenreich May J, Alessandri M, Fujii C, Renno P, Laugeson EA, Piacentini J, De Nadai AS, Arnold E, Lewin A, Murphy TK, Storch EA. Cognitive behavioral therapy for early adolescents with autism spectrum disorders and dlinical anxiety: A randomized, controlled trial. Behav Ther. doi: 10.1016/j.beth.2014.01.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White SW, Ollendick T, Albano AM, Oswald D, Johnson C, Southam-Gerow MA, Kim I, Scahill L. Randomized controlled trial: Multimodal Anxiety and Social Skill Intervention for adolescents with autism spectrum disorder. J Autism Dev Disord. 2013;43(2):382–394. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, Murphy DG, Mataix-Cols D. Cognitive behavior therapy for comorbid obsessive-compulsive disorder in high-functioning autism spectrum disorders: a randomized controlled trial. Depress Anxiety. 2013;30(8):697–708. doi: 10.1002/da.22053. [DOI] [PubMed] [Google Scholar]
- 24.RUPP The Pediatric Anxiety Rating Scale: development and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2002;41:1061–1069. doi: 10.1097/00004583-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Pearson; 1999. [Google Scholar]
- 26.Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions. San Antonio, TX: Graywinds Publications; 1996. [Google Scholar]
- 27.Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry. 1982;39(8):879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 28.Rutter M, LeCouteur A, Lord C. Autism Diagnostic Interview, Revised. Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- 29.Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS) J Autism Dev Disord. 1980;10(1):91–103. doi: 10.1007/BF02408436. [DOI] [PubMed] [Google Scholar]
- 30.Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 1999. [Google Scholar]
- 31.Storch EA, Wood JJ, Ehrenreich-May J, Jones AM, Park JM, Lewin A, Murphy TK. Convergent and discriminant validity and reliability of the Pediatric Anxiety Rating Scale in youth with autism spectrum disorders [published online ahead of print March 2012] J Autism Dev Disord. 2012 doi: 10.1007/s10803-012-1489-9. [DOI] [PubMed] [Google Scholar]
- 32.Ginsburg GS, Keeton C, Drazdowski TK, Riddle M. The utility of clinician ratings of anxiety using the Pediatric Anxiety Rating Scale. Child Youth Care Forum. 2011;40:93–105. [Google Scholar]
- 33.Horwitz S, Hoagwood K, Stiffman AR, Summerfield T, Weisz JR, Costello J, et al. Measuring youth’s use of mental health services: reliability of the SACA-Services Assessment for Children and Adolescents. Psychiatric Services. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- 34.Hoagwood K, Horwitz SM, Stiffman AR. Concordance between parent reports of children’s mental health services and services records: The Services Assessment for Children & Adolescents. J Child Fam Stud. 2000;9:315–331. [Google Scholar]
- 35.Bird H, Andrews H, Schwab-Stone M, Goodman S, Dulcan M, Richters J, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research. 1996;6:295–307. [Google Scholar]
- 36.Achenbach TM. Manual for the ASEBA School-Age Forms and Profiles. Burlington: University of Vermont; 2001. [Google Scholar]
- 37.Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Clin Child Adolesc Psychol. 2002;31(3):335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- 38.Constantino J. The Social Responsiveness Scale. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- 39.Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther. 2005;43(3):309–322. doi: 10.1016/j.brat.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Sterling L, Renno P, Storch EA, Ehrenreich-May J, Lewin AB, Arnold E, Lin E, Wood J. Validity of the Revised Children’s Anxiety and Depression Scale for youth with autism spectrum disorders. Autism. 2014 doi: 10.1177/1362361313510066. [DOI] [PubMed] [Google Scholar]
- 41.Cooper H, Hedges LV, Valentine JC, editors. The Handbook of Research Synthesis and Meta-Analysis. New York: Russell Sage Foundation; 2009. [Google Scholar]
- 42.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 43.Storch EA, Lewin AB, De Nadai AS, Murphy TK. Defining treatment response and remission in obsessive-compulsive disorder: a signal detection analysis of the Children’s Yale-Brown Obsessive Compulsive Scale. J Am Acad Child Adolesc Psychiatry. 2010;49(7):708–717. doi: 10.1016/j.jaac.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 44.Institute S. SAS/STAT User’s Guide (version 9.3) Cary, NC: SAS Institute, Inc; 2011. [Google Scholar]
- 45.Graham JW. Missing data analysis: Making it work in the real world. Annual Rev Psychol. 2009 doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 46.Donaldson GW, Moinpour CM. Learning to live with missing quality-of-life data in advanced-stage disease trials. J Clin Oncol. 2005;23(30):7380–7384. doi: 10.1200/JCO.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 47.Barnard J, Rubin DB. Miscellanea: Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- 48.Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Ginsburg GS, Rynn MA, McCracken J, Waslick B, Iyengar S, March JS, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pugliese CE, White BA, White SW, Ollendick TH. Social anxiety predicts aggression in children with ASD: clinical comparisons with socially anxious and oppositional youth. J Autism Dev Disord. 2013;43(5):1205–1213. doi: 10.1007/s10803-012-1666-x. [DOI] [PubMed] [Google Scholar]
- 50.Wood JJ, Drahota A, Sze K, Van Dyke M, Decker K, Fujii C, Bahng C, Renno P, Hwang WC, Spiker M. Effects of cognitive behavioral therapy on parent-reported autism symptoms in school-age children with high-functioning autism. J Autism Dev Disord. 2009;39:1608–1612. doi: 10.1007/s10803-009-0791-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Storch EA, Ehrenreich May J, Wood JJ, Jones AM, de Nadai AS, Lewin A, Arnold EB, Murphy TK. Multiple informant agreement on the Anxiety Disorders Interview Schedule in youth with autism spectrum disorders. J Child Adolesc Psychopharmacol. 2012;22:292–299. doi: 10.1089/cap.2011.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lecavalier L, Wood JJ, Halladay AK, Jones NE, Aman MG, Cook EH, Handen BL, King BH, Pearson DA, Hallett V, Sullivan KA, Grondhuis S, Bishop SL, Horrigan JP, Dawson G, Scahill L. Measuring anxiety as a treatment endpoint in youth with autism spectrum disorder. J Autism Dev Disord. 2014;44(5):1128–1143. doi: 10.1007/s10803-013-1974-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.White SW, Schry AR, Maddox BB. The assessment of anxiety in high-functioning adolescents with autism spectrum disorder. J Autism Dev Disord. 2012;42:1138–1145. doi: 10.1007/s10803-011-1353-3. [DOI] [PubMed] [Google Scholar]