Abstract
Investigations of targeted coping skills could help guide initial treatment decisions for individuals with co-occurring posttraumatic stress disorder (PTSD) and alcohol dependence (AD) who often endorse worse coping skills than those with AD but not PTSD. Although improvement in coping skills is associated with enhanced alcohol use outcomes, no study has evaluated the utility of teaching specific coping skills in the context of comorbid PTSD/AD. We compared the effects of teaching two coping skills (cognitive restructuring [CR] and experiential acceptance [EA]) or an attention control condition on drinking and PTSD symptoms among 78 men and women with comorbid PTSD/AD during a 5-week daily follow-up assessment. Both CR and EA skills were associated with decreased drinking compared to control, and that change in drinking over time did not significantly differ between those who received CR and EA. Individuals who received CR skills, however, consumed less alcohol on a given day than those who received EA skills. Neither CR nor EA was associated with a decrease in PTSD symptom severity. These results provide preliminary support for clinicians to prioritize CR and EA skills during initial treatment sessions when working with individuals with PTSD/AD, and offer ideas for continued investigation and intervention refinement.
Keywords: Coping behavior, Posttraumatic stress disorder, Alcohol dependence, Dual diagnosis, Cognitive restructuring, Experiential acceptance
Posttraumatic stress disorder (PTSD) and alcohol use disorders frequently co-occur (Kessler et al., 1997; DSM-III-R criteria were used). Recent data from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) found that the lifetime prevalence of PTSD/AD comorbidity in the U.S. is 1.6% (Blanco et al., 2013; DSM-IV criteria were used). Compared with those with only PTSD and only AD, those with comorbid PTSD/AD report greater childhood adversity, higher rates of other Axis I and Axis II disorders, more suicide attempts, and met more diagnostic criteria for each of the two disorders (Blanco et al., 2013). Comorbid PTSD/AD individuals also report greater disability and treatment seeking than those with AD only (Blanco et al., 2013; Drapkin et al., 2011), as well as worse coping strategies (Ouimette, Brown, & Najavits, 1998). These findings highlight the need for interventions to address both PTSD and AD among these individuals.
Difficulty tolerating distress and regulating emotions has also been associated with PTSD and alcohol use disorders (McDermott, Tull, Gratz, Daughters, & Lejuez, 2009; Tull, Barrett, McMillan, Roemer, 2007). A hallmark feature of these difficulties is a lack of engagement in adaptive coping strategies when faced with distress or aversive emotional experiences. Instead, patterns of avoidant coping are often present and may be driven by the inability or unwillingness to experience negatively evaluated thoughts, feelings, sensations, and memories (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). Avoidant coping strategies have been found to play an important role in the comorbidity between PTSD and AD (Hruska, Fallon, Spoonster, Sledjeski, & Delahanty, 2011). Consistent with the self-medication hypothesis, individuals may consume alcohol as an avoidant coping strategy in response to PTSD-related distress or increased PTSD symptom severity (Kaysen et al., 2014; Simpson, Stappenbeck, Luterek, Lehevot, & Kaysen, 2014). In addition, expectations or beliefs that the effects of alcohol will relieve one’s PTSD symptoms has been associated with increased alcohol consumption and alcohol-related consequences (Vik, Islam-Zwart, & Ruge, 2008). These results highlight the importance of increasing the use of adaptive coping skills among individuals with comorbid PTSD/AD.
Overview of Psychotherapy for Comorbid PTSD and Alcohol and Drug Use Disorders
Despite the pressing need for effective interventions to address the common and debilitating comorbidity between PTSD and alcohol and drug use disorders, the current evidence base to guide optimum treatment planning for these patients is limited. Although there are three recent narrative reviews of the relevant psychotherapy literature (Berenz & Coffey, 2012; McCauley, Killeen, Gros, Brady, & Back, 2012; van Dam, Vedel, Ehring, & Emmelkamp, 2012) and a meta-analysis (Torchalla, Nosen, Rostam, & Allen, 2012), they were all published in 2012 and summarize roughly the same literature. Taken together, they indicate that non-trauma focused cognitive behavior therapy (CBT) interventions tailored to address both PTSD and substance use disorders do not confer added benefit when compared with standard substance use disorder interventions either with regard to substance use outcomes or PTSD. There was some indication across the reviews and more recent papers that trauma-focused interventions confer benefit in terms of reduced PTSD, though generally not reduced substance use behaviors, relative to control conditions (see also Foa et al., 2013; Mills et al., 2012; Sannibale et al., 2013). One challenge with these studies is that drop-out rates across interventions for those with PTSD/AD are quite high, with as many as 45% of participants dropping out of treatment in some cases (Foa et al., 2013). Thus, many patients are at risk of failing to persist in treatment long enough to be receive effective intervention elements.
In light of the high rates of early treatment drop-out among these patients (Foa et al., 2013; Mills et al., 2012; Read, Brown, & Kahler, 2004; Sannibale et al., 2013), evaluations of specific coping skills to improve PTSD or substance use outcomes early in treatment could be especially valuable. Indeed, in the larger psychotherapy literature, it is very common for adults who begin a course of psychotherapy to fail to return for a second visit (Hamilton, Moore, Crane, & Payne, 2011; Simon, Imel, Ludman, & Steinfeld, 2012; Simon & Ludman, 2010). Most of the interventions developed for those with comorbid PTSD/AD population are quite lengthy, which can be challenging with such high drop-out rates. For example, the Seeking Safety protocol (Najavits, 2004; Najavits, Weiss, Shaw, & Muenz, 1998) is comprised of 25 modules, many of which need to be delivered over two or more sessions, and a recent study by Foa and colleagues (2013) consisted of 18 sessions of Prolonged Exposure along with the same number of supportive counseling sessions that were to be attended concurrently. Given the extreme level of distress and disorganization often displayed by individuals with comorbid PTSD and substance use disorders (Drapkin et al., 2011), it could be argued that these individuals are in need of highly efficient, targeted coping skills interventions that will allow them to quickly find some relief and reduce alcohol consumption before considering lengthier treatment protocols.
Coping Skills With Potential Utility for Those With Comorbid PTSD/AD
The majority of substance abuse CBT treatment packages focus on the development of adaptive coping skills to prevent relapse in response to various types of triggers. In fact, brief 1–3 session coping skills training interventions have been investigated and found to be associated with decreased substance use among individuals with substance use disorders and no significant psychiatric comorbidities (Conrod, Castellanos-Ryan, & Strang, 2010; Monti, Rohsenow, Michalec, Martin, & Abrams, 1997; Rohsenow, Monti, Martin, Michalec, & Abrams, 2000). Further, studies that have evaluated alcohol use disorder patients’ ability to use coping skills have found that those who evidence improvements in coping skills have better alcohol use outcomes (Morgenstern & Longabaugh, 2000). Standard CBT treatment packages for AD, such as relapse prevention (Marlatt & Donovan, 2005; Marlatt & George, 1984), as well as those for individuals with comorbid PTSD/AD, such as Seeking Safety (Najavits, 2004; Najavits et al., 1998), offer a range of coping skill strategies to assist individuals successfully avoid drinking. In light of the poor treatment retention often associated with comorbid PTSD/AD and this group’s over-reliance on avoidant coping, clarifying the utility of teaching specific adaptive coping skills that significantly impact outcomes early in treatment is critical.
Two types of coping skills that are geared toward improving distress tolerance and emotion regulation include 1) cognitive restructuring, which is designed to facilitate flexible, balanced appraisal of situations, and 2) experiential acceptance, which is designed to facilitate acceptance of uncomfortable internal states and experiences without engaging in avoidant behaviors (i.e., drinking). Consistent with social learning theory (Bandura, 1969), a person’s appraisals of current situations may be influenced by their past experiences in ways that they are not consciously aware, which can lead to inflexible cognitive schemas and sub-optimal functioning. Cognitive restructuring skills, which are commonly embedded in relapse prevention treatment packages (Larimer, Palmer, & Marlatt, 1999), can help bring such biased appraisal patterns into awareness, provide strategies for challenging them, and facilitate the generation of more realistic and more balanced thoughts and beliefs, thereby reducing emotional distress (Butler, Chapman, Forman, & Beck, 2006). In the context of substance use and PTSD, if an individual strongly believes that the only way to cope effectively with increased PTSD symptoms is to consume alcohol, they are at risk for turning frequently to alcohol to ameliorate those symptoms. Cognitive restructuring techniques would, for example, guide the person to question whether this belief is always true, whether they are perhaps confusing feelings and facts, and to generate a more realistic and balanced alternative thought about their ability to cope with symptoms without using alcohol.
An experiential acceptance approach to coping with discomfort or urges to use alcohol also encourages greater awareness of one’s thoughts and feelings, but rather than challenging them (as in cognitive restructuring), the emphasis is on experiencing thoughts and feelings as passing events without judging, clinging to, or trying to change them. It is postulated that the efforts to change or suppress one’s thoughts and feelings lead to increased suffering (Bowen et al., 2009; Hayes et al., 1996; Orsillo & Batten, 2005; Witkiewitz, Bowen, Douglas, & Hsu, 2013; see also Linehan, 1993) as these efforts can actually increase thoughts about the painful stimuli (Wegner, Schneider, Carter, & White, 1987; for review, see Abramowitz, Tolin, & Street, 2001). Strategies that guide people to observe their thoughts and feelings without attachment or aversion include non-judgmentally observing how the feelings come and go from different body areas through urge surfing (another component of relapse prevention; Marlatt & Donovan, 2005; Marlatt & George, 1984), radical acceptance, and mindful breathing. In sum, an experiential acceptance approach to coping posits that it is possible to tolerate distressing thoughts and feelings without avoidance and with greater acceptance, which could result in reduced reliance on drinking and alleviated suffering.
Present Study
Evaluation of skills specifically designed to facilitate increased cognitive flexibility or increased experiential acceptance could help determine whether either or both of these standard components of relapse prevention treatment packages are helpful to individuals with comorbid PTSD/AD. The goal of the present study was to determine whether two coping skills (cognitive restructuring [CR] and experiential acceptance [EA]) reduced alcohol use or symptoms of PTSD compared to an attention control condition among individuals with current comorbid PTSD and AD. Given the high treatment dropout and the potential lack of adequate emotion regulation and distress tolerance skills among those with comorbid PTSD/AD, we hoped to determine whether these coping skills had the potential to confer initial symptom relief in a single session with additional brief telephone coaching calls to reinforce skill acquisition. As part of a larger clinical trial designed to assess mechanisms of behavior change, PTSD symptomatology and alcohol use were assessed over time via an interactive voice response (IVR) telephone system that participants accessed daily for the week prior to learning the coping skills (or nutrition control materials) and for five weeks thereafter. We hypothesized that relative to the control condition, participants who received either the CR or EA skills would report less drinking and lower PTSD symptom severity on a given day, and greater reductions in alcohol use and significantly lower PTSD symptom severity over time. Although we had no reason to expect the outcomes associated with EA and CR to differ meaningfully, we opted to compare the two active conditions using traditional between group models to provide a thorough examination of the available data.
Method
Participants and Procedure
All study procedures were approved by the VA Puget Sound Health Care System Human Subjects Division Internal Review Board. Participants who wanted to decrease their alcohol use were recruited through community newspaper advertisements and flyers and were directed to contact the research coordinator (Clinicaltrials.gov protocol #NCT00760994) to complete a brief screening assessment over the telephone. Initially eligible participants (N = 132) came to the laboratory where they provided written informed consent and completed a more thorough screening for inclusion and exclusion criteria, and were compensated $30. Inclusion criteria were: 1) age ≥ 18 years; 2) current diagnosis of AD as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association [APA], 1994) with alcohol use in the last two weeks; 3) current DSM-IV diagnosis of PTSD; 4) capacity to provide informed consent; and 5) telephone access. In addition, individuals were excluded with 1) a history of delirium tremens or seizures; 2) opiate use or treatment with any opioid-containing medications during the previous month; 3) antabuse or naltrexone treatment (because of the pharmacological impact of these medications on alcohol cravings and use); 4) symptoms of alcohol withdrawal at initial consent; 5) acute suicidality/homicidality with intent/plan; or 6) uncontrolled psychotic disorder.
Ninety two participants (50% female) remained eligible and were invited to start the daily telephone monitoring via an Interactive Voice Response (IVR) system. Our final sample is comprised of 78 (48.7% female) participants who returned for a second in-person visit approximately one week after their screening assessment and received one of three conditions (see Table 1 for participant characteristics and Figure 1 for a Consort Diagram depicting flow through the study). At the screening assessment, participants reported drinking an average of 23.8 (SD = 12.6) of the previous 42 days and consumed an average of 11.7 (SD = 8.7) standard drinks per drinking day, and had an average score of 29.8 (SD = 8.9) on the PTSD Symptom Scale-Interview Version (Foa, Riggs, Danu, & Rothbaum, 1993). Participants reported having experienced an average of 6 (SD = 2.7) different traumas and were 15.1 (SD = 10.3) years old on average at the time of their earliest trauma.
Table 1.
Participant Characteristics
| Characteristics | Mean (SD) |
|---|---|
| Age | 44.3 (11.5) |
| N (%) | |
| Female | 38 (48.7) |
| Ethnicity/Race | |
| Caucasian | 33 (42.3) |
| African American | 34 (43.6) |
| Hispanic/Latino | 3 (3.8) |
| Native American | 2 (2.6) |
| Asian American | 1 (1.3) |
| Other | 5 (6.4) |
| Marital Status | |
| Married or partnered | 10 (12.8) |
| Divorced or separated | 27 (34.6) |
| Never married | 32 (41.0) |
| Widowed | 4 (5.1) |
| Other or missing | 5 (6.5) |
| Housing Status | |
| Living in own home | 49 (62.8) |
| Homeless | 17 (21.8) |
| Other | 12 (15.4) |
| Educational Attainment | |
| Did not graduate high school | 15 (19.2) |
| Graduated high school | 13 (16.7) |
| At least some college | 50 (64.1) |
| Employment Status | |
| Employed at least part-time | 12 (15.4) |
| Unemployed | 66 (84.6) |
| Military Status | |
| Veteran | 21 (26.9) |
| Civilian | 57 (73.1) |
| Treatment History | |
| Inpatient substance abuse | 37 (47.4) |
| Inpatient mental health | 20 (25.6) |
| Medication management | 48 (61.5) |
| Outpatient therapy | 55 (70.5) |
Figure 1.
Consort Diagram
Daily monitoring assessment
Participants completed daily assessments of alcohol use and PTSD symptoms for the previous day using IVR technology during a one-week pre-treatment baseline period and a five-week post treatment follow-up period. Due to participant scheduling, the baseline assessment period ranged from 6 to 20 days. IVR compliance was automatically tracked by the IVR system created and maintained by Database Systems Corp. To reduce the likelihood of missing data, participants who failed to call were contacted within two working days to collect the data verbally by a study staff member blind to their intervention condition; 10% of IVR assessments were collected verbally. Participants were compensated $1 for every day of completed daily monitoring, with an additional $10 for completing 7 consecutive days of monitoring or $7 for 6 days of monitoring for a maximum compensation of $102.
Randomization
Study participants were randomized by the study therapist so that the rest of the research team was blind to study condition. Randomization was stratified by gender, civilian/veteran status, and drinking frequency (<10 drinking days in the past 30 days vs. >10 drinking days in the past 30 days). Allocation to the CR, EA, or attention control condition was 1:1:3/4, respectively.
Coping Skill and Control Conditions
Overview
The same master’s level therapist administered the three conditions to study participants. The conditions were all scripted, but incorporated frequent opportunities for participant interaction. Experts in cognitive restructuring and experiential acceptance each reviewed their respective condition and their feedback was incorporated. Nutritionists with expertise in teaching the plate method of healthy eating assisted with the attention control condition materials. Participants were provided with a copy of their assigned condition script as well as a short overview statement, materials for completing homework, and a CD recording of the condition script and overview. Additionally, the study therapist attempted to provide four weekly coaching calls to assist participants as they worked to incorporate the skills in their day-to-day lives. On average, participants received 3.1 (SD = 1.2; range 0−4) calls that lasted on average 11–13 minutes each. The in-person sessions were audiotaped and a random 50% from each condition was assessed by two trained raters for fidelity to the assigned condition.
Cognitive Restructuring (CR)
The CR condition involved teaching participants how trauma exposure can lead to distorted thoughts and beliefs, which in turn can lead to negative feelings and unhealthy behaviors. They were given “A-B-C” sheets and taught how to identify the antecedent (difficult or stressful event that prompted negative thoughts/beliefs), beliefs and thoughts, and consequences (e.g., feelings, behaviors). Participants were then taught three questions selected from the Challenging Questions skill set from Cognitive Processing Therapy (Resick, Monson, & Chard, 2008) to aid them in evaluating whether a particular thought or belief is accurate; 1) “am I doing all or none thinking?” 2) “am I confusing feelings with facts?” and 3) “what is the evidence for and against this thought/belief?” The basic CR principles were illustrated first with a generic example (i.e., a friend walks past you on the street without acknowledging you) and then with a standardized drinking example (i.e., learning that a bill you thought was paid was not and drinking in response). Participants were then asked to recall a recent drinking or craving episode and the therapist guided them through the use of an A-B-C sheet to break down the components and then identify alternative, more constructive self-statements to replace the cognitive distortion. Participants were provided with A-B-C sheets and other materials germane to practicing CR at home. The CR sessions were rated by coders as all meeting minimum requirements for CR and the inter-rater agreement with regard to adherence to condition details was 90%.
Experiential Acceptance (EA)
The EA condition introduced participants to the idea that avoiding thoughts and feelings is often associated with more distress and poorer coping. Instead, accepting thoughts and feelings can enable one to make choices consistent with one’s values rather than having one’s behavior driven by distress or urges to drink. This concept was conveyed through several metaphors borrowed from Acceptance and Commitment Therapy (Hayes, Strosahl, & Wilson, 1999) including seeing the tug-of-war involved with trying to control thoughts and feelings and letting go of the proverbial rope (or letting go of the struggle to control thoughts/feelings), seeing one’s thoughts and feelings as passengers on one’s bus that can be tolerated while one “drives the bus” in valued directions, and welcoming unwanted guests at a party, just like one can cultivate a willingness to let unwanted thoughts/feelings be present so that one can go on with one’s life rather than keep tabs on them or try to bar them. In addition, participants were introduced to urge surfing (Marlatt & Donovan, 2005; Marlatt & George, 1984) and a brief mindful breathing meditation. The idea of compassion and kindness for oneself and whatever one happens to be experiencing was also introduced. Participants were assisted in identifying ways that they may avoid thoughts and feelings or try to change them, particularly those pertaining to trauma memories and alcohol craving, as well as ways that they could use the EA concepts to help them accept difficult thoughts/feelings as passing events, without judgment. EA participants were provided with a list of acceptance oriented practice activities they could try at home as well as summary materials specific to this condition. The EA sessions were rated by coders as all meeting minimum requirements for EA and the inter-rater agreement with regard to adherence to condition details was 90%.
Attention Control Condition
The plate method of good nutrition was designed to engage control participants in a comparable length interaction with the therapist that involved learning something germane to health but not specifically relevant to either PTSD or problematic alcohol use. Participants were asked to assess their current eating habits, instructed in the basics of the plate method of nutrition including proper portion sizes, and assisted in identifying ways that they could bring their diet in alignment with the plate method recommendations. Information on how to shop on a budget and how to eat out were also covered. The control sessions were rated by coders as all meeting minimum requirements for teaching the plate method and the inter-rater agreement with regard to adherence to condition details was 84%.
Measures
Screening assessment
Alcohol-related medical history and safety
Exclusion criteria were assessed using a structured interview. Suicidality was assessed with the suicide section of the Hamilton Depression Inventory (HAM-D; Hamilton, 1960).
Mental health diagnoses
The “Substance Use Disorder” and “Psychotic and Associated Symptoms” sections of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-1; First, Gibbon, Spitzer, & Williams, 1995) were administered to assess diagnoses of alcohol dependence, opioid abuse or dependence, schizophrenia, schizoaffective, or schizophreniform disorder. The SCID-1 is a widely used structured interview that assesses psychiatric history with good psychometric properties. To assess for past-month PTSD diagnostic status, we administered the PTSD Symptom Scale-Interview Version (PSS-I; Foa et al., 1993), which has demonstrated good reliability and internal consistency. The Traumatic Life Events Questionnaire (Kubany et al., 2000), a 23 item self-report measure that assesses exposure to potentially traumatic events using behaviorally descriptive terms, was used to assess trauma exposure in participants’ lifetime.
Substance use
The Form-42 was adapted from the Form-90 (Miller & Del Boca, 1994) to assess alcohol use and treatment for 6-weeks prior to baseline. It was used to characterize the sample and ensure that participants had used alcohol in the previous two weeks. The Form-42 was also administered at the end of the 5-week follow-up period. Percent days abstinent was calculated for the pre-treatment as well as post-treatment assessment periods.
Daily monitoring assessment
Alcohol use
Participants indicated the number of standard drinks of beer, wine, and liquor (defined for the participant as 12 oz. beer, 5 oz. wine, and 1.5 oz liquor) consumed, each queried separately and then summed for the total number of standard drinks per day.
PTSD symptoms
Twelve items were adapted from the PTSD Checklist-Civilian Version (PCL-C; Weathers & Ford, 1996). Items that were likely to vary daily and that were the strongest predictors of PTSD clusters in factor analytic studies of PTSD (e.g., King, Leskin, King, & Weathers, 1998; Krause, Kaltman, Goodman, & Dutton, 2007; Palmieri, Weathers, Difede, & King, 2007) were selected for inclusion. Items included three re-experiencing symptoms, two avoidance symptoms, three emotional numbing symptoms, and four hyperarousal symptoms. Participants indicated how bothered they were during the previous day by each symptom on 9-point scales ranging from 0 = not at all to 8 = all the time. Items were averaged to create an overall daily severity score. The internal reliability was examined for the current sample using within person averages of the daily responses to each item (α = .94).
Data Analytic Strategy
Our primary analytic goal was to examine differences between individuals in the coping skill conditions (CR or EA) compared to those in the control condition on their daily alcohol use and PTSD symptom severity, as well as their change in alcohol use and PTSD symptom severity over the course of the 5-week follow-up IVR assessment period. To do this, we used generalized estimating equation (GEE; Hardin & Hilbe, 2003) models to account for the nested nature of our data (i.e., repeated daily assessments of alcohol use and PTSD symptoms within individuals). Participants provided IVR data for an average of 7.2 (SD = 2.3; range 3–14) days during the baseline IVR assessment period, which was 97.4% of all possible days (i.e., 2.6% of baseline days were missing). Participants provided an average of 30.6 (SD = 7.3; range 5–35) days of IVR data during the follow-up IVR assessment period. Data were collected on 2,387 (87.4%) days of the possible 2,730 follow-up monitoring days (12.6% of follow-up days were missing). If a participant provided data on a given day, less than 1% of the possible responses were missing. Because of this low percentage of missing data, and because missing days may have been due to variables already included in the model (e.g., alcohol use, PTSD symptoms), the maximum likelihood estimation procedures used were likely sufficient to handle potential problems related to missing data (Allison, 2009).
To examine the impact of the CR and EA skills on alcohol use and PTSD symptom severity, four GEE models were tested. First, we included two dummy coded condition variables with the control condition as the reference to examine differences between both the CR and EA conditions and the control separately for alcohol use and PTSD symptoms. The next two models included two dummy coded condition variables with EA as the reference to examine differences between having received the CR versus EA condition. Because alcohol use was a positively skewed count variable, models predicting alcohol use were estimated using a negative binomial distribution with a log link function. GEEs with a negative binomial distribution provide incidence rate ratios (IRRs), which serve as a standardized effect size. In the case of a main effect of the CR condition compared to control, the IRRs would reflect the percentage increase or decrease in the rate of drinking as a function of the CR condition compared to control while holding all other variables constant. A normal distribution with an identity link function was used for models predicting PTSD symptoms.
In addition to the condition variables, all models included covariates to control for baseline alcohol use and PTSD symptom severity centered at the grand mean, a variable for gender to account for differences in drinking amounts between men and women (0 = male and 1 = female), an indicator variable for weekend versus weekday (0 = weekday and 1 = weekend), a grand-mean centered variable for the number of coaching calls the participants received, a person-mean centered follow-up IVR monitoring day variable, and interaction terms between the condition variables and follow-up monitoring day to test for changes in alcohol use or PTSD symptoms associated with a condition across the assessment period. We also examined whether other demographic variables were associated with alcohol use or PTSD symptoms during the follow-up IVR assessment period for inclusion in the models as covariates. For alcohol use, older age (b = .01, p < .01) and being single (b = .90, p < .001) were associated with greater alcohol consumption. Race/ethnicity and employment status were not significantly associated with alcohol use (p’s > .17). Participants who were older (b = .02, p < .05), White (b = .41, p < .05), and unemployed (b = .74, p < .01) had greater PTSD symptom severity during the follow-up assessment period. Marital status was not significantly associated with PTSD symptom severity (b = .37, p = .22). The significant covariates were included in the respective alcohol use or PTSD models. Analyses were conducted in Stata 11.2 (StataCorp, 2009).
Results
Participant background characteristics are presented in Table 1. Compared to participants in the CR or EA conditions, those in the control condition were less likely to have had inpatient mental health treatment, χ2 (2) = 6.27, p < .05. Participants did not differ on any of the other background characteristics across intervention conditions (all p’s > .11). Average baseline and follow-up alcohol use and PTSD symptom severity by conditions are shown in Table 2. There were no statistically significant differences in drinking (F[2,75] = 2.16, p = .12, η2p = .06) or average PTSD symptoms (F[2,75] = 2.03, p = .14, η2p = .05) during the baseline IVR period across conditions.
Table 2.
Means (and Standard Deviations) of Alcohol Consumption and PTSD Symptom Severity by Condition
| Conditions |
||||
|---|---|---|---|---|
| EA (n=27) |
CR (n=31) |
Control (n=20) |
Total Sample (N=78) |
|
| Average IVR drinks per day | ||||
| Baseline | 5.2 (5.9) | 2.7 (3.5) | 4.6 (4.7) | 4.0 (4.8) |
| Follow-up | 3.6 (5.0) | 1.8 (2.5) | 3.1 (3.7) | 2.8 (3.8) |
| Average IVR PTSD symptoms | ||||
| Baseline | 3.2 (1.6) | 3.9 (1.6) | 4.0 (1.4) | 3.7 (1.6) |
| Follow-up | 2.7 (1.4) | 3.1 (1.8) | 3.4 (1.3) | 3.0 (1.5) |
Note. EA = experiential acceptance; CR = cognitive restructuring; PTSD = posttraumatic stress disorder; IVR = interactive voice response. IVR PTSD symptom range 0–8.
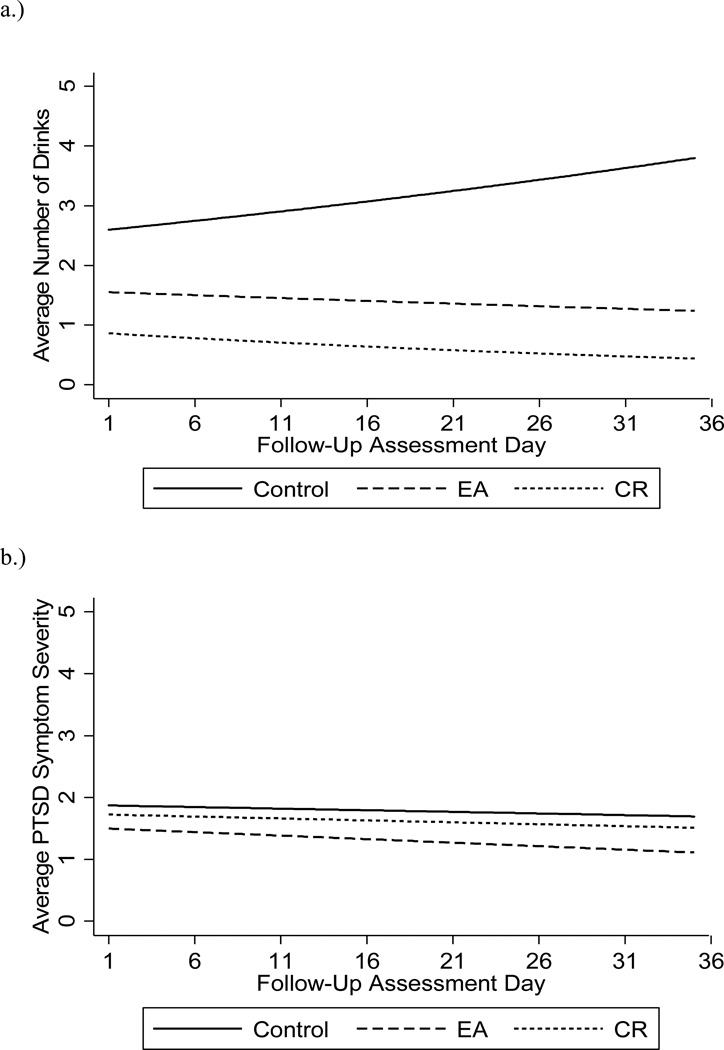
Results of the GEE model for alcohol use indicate that alcohol consumption was greater for men, those older in age, and on weekends compared to weekdays (Table 3). Heavier baseline drinking was associated with more drinking on a given day during the follow-up assessment period and having completed more coaching calls was associated with less drinking on a given day during the follow-up period. There was a significant main effect of CR condition compared to control that was superseded by a significant interaction between CR condition (compared to control) and follow-up day (i.e., time). There was also a significant interaction between EA condition (compared to control) and follow-up day. Individuals in the CR condition had a 2% decrease in drinking per day across the follow-up assessment period compared to control, whereas those in the EA condition had a 1% decrease in drinking per day during the follow-up period compared to control (Figure 2a). Specifically, that would mean that an individual who consumed 10 drinks the day after receiving the CR intervention would have consumed 5 drinks during the final day of the follow-up period, whereas an individual who consumed 10 drinks the day after receiving the EA intervention would have consumed 7.1 drinks during the final day of the follow-up period. In a second GEE model that compared CR with EA, those in the CR condition reported consuming significantly fewer drinks on a given day compared to those in the EA condition (b = −0.34, p < .001, IRR = 0.71, 95% C.I.: 0.59, 0.85); however, the change in drinking across the follow-up assessment period (i.e., the slope of the lines) did not significantly differ between those in the CR and EA conditions (b = −0.01, p = .12, IRR = 0.99, 95% C.I.: 0.97, 1.00).
Table 3.
Daily model predicting alcohol consumption on a given day and change across the follow-up assessment period by condition
| b | IRR [95% CI] | |
|---|---|---|
| Female gender | −0.18* | 0.84 [0.71, 0.97] |
| Age | 0.01* | 1.01 [1.00, 1.02] |
| Married | 0.24 | 1.27 [0.998, 1.62] |
| Inpatient mental health treatment | −0.09 | 0.92 [0.76, 1.10] |
| Weekend | 0.23*** | 1.26 [1.13, 1.41] |
| follow-up day | 0.01 | 1.01 [0.998, 1.02] |
| Baseline IVR drinking | 0.16*** | 1.17 [1.15, 1.19] |
| Baseline IVR PTSD severity | 0.05 | 1.05 [0.998, 1.11] |
| Number coaching calls | −0.17*** | 0.85 [0.78, 0.91] |
| CR condition | −0.53*** | 0.59 [0.47, 0.73] |
| EA condition | −0.19 | 0.83 [0.69, 1.00] |
| CR condition x follow-up day | −0.03** | 0.97 [0.95, 0.99] |
| EA condition x follow-up day | −0.02* | 0.98 [0.97, 0.999] |
Note. IRR = incidence rate ratio; CI = confidence interval; IVR = interactive voice response; PTSD = posttraumatic stress disorders; CR = cognitive restructuring; EA = experiential acceptance.
p < .05.
p < .01.
p < .001.
Figure 2.
Predicted average daily alcohol consumption (2a) and PTSD symptom severity (2b) by condition as a function of time. Estimates are shown for men.
To follow-up on the significant changes in alcohol consumption for those in the CR and EA conditions, we compared the percent days abstinent from screening to follow-up. For those in the CR condition, there was a significant increase in percent days abstinent from screening (M = 53.0, SD = 33.2) to follow-up (M = 78.3, SD = 31.7), t(30) = 5.66, p < .001, d = .78. For those in the EA condition, there was also a significant increase in percent days abstinent from screening (M = 37.0, SD = 35.9) to follow-up (M = 60.8, SD = 43.5), t(26) = 3.09, p < .01, d = .60.
As shown in Table 4, results of the GEE model for PTSD symptom severity revealed that individuals who were older and of White ethnicity reported greater PTSD symptom severity on a given day during the follow-up period. Higher rates of baseline drinking and baseline PTSD symptom severity predicted greater PTSD symptom severity on a given day during the follow-up period. There were no differences in PTSD symptom severity between those assigned to the CR or EA conditions compared to control on a given day or over the assessment period (Figure 2b). Additionally, in a separate GEE model comparing CR to EA, there were no differences between those in the CR and EA conditions on their PTSD symptom severity on a given day (b = 0.13, p = .39, 95% C.I.: −0.17, 0.44) or across the follow-up assessment period (b = 0.01, p = .69, 95% C.I.: −0.02, 0.03).
Table 4.
Daily model predicting PTSD symptom severity on a given day and change across the follow-up assessment period by condition
| b | 95% CI | |
|---|---|---|
| Female gender | −0.05 | −0.32, 0.21 |
| Age | 0.03*** | 0.01, 0.04 |
| White | 0.54*** | 0.27, 0.82 |
| Employed | −0.21 | −0.61, 0.19 |
| Inpatient mental health treatment | −0.08 | −0.39, 0.23 |
| Weekend | 0.02 | −0.06, 0.11 |
| follow-up monitoring day | −0.01 | −0.03, 0.02 |
| Baseline IVR drinking | 0.06*** | 0.03, 0.09 |
| Baseline IVR PTSD severity | 0.61*** | 0.52, 0.69 |
| Number coaching calls | −0.07 | −0.19, 0.06 |
| CR condition | −0.13 | −0.47, 0.22 |
| EA condition | −0.26 | −0.59, 0.07 |
| CR condition x follow-up day | 0.00 | −0.03, 0.03 |
| EA condition x follow-up day | −0.01 | −0.03, 0.02 |
Note. CI = confidence interval; IVR = interactive voice response; PTSD = posttraumatic stress disorders; CR = cognitive restructuring; EA = experiential acceptance.
p < .001.
Discussion
The present study assessed the efficacy of teaching either CR or EA coping skills to decrease alcohol use and PTSD symptom severity in an effort to guide decisions about which skills to prioritize during initial treatment sessions with individuals with this common comorbidity. The results indicate that both skill sets were associated with a decrease in drinking compared to a nutrition education control, and that change in drinking over time did not significantly differ between those who received one of the two active coping skill conditions. However, individuals who were taught CR skills consumed less alcohol on a given day than those who received the EA skills even after controlling for their alcohol consumption during the baseline assessment period. Neither CR nor EA skills were associated with a decrease in PTSD symptom severity. Because individuals with comorbid PTSD and AD often have difficulty engaging in and adhering to lengthy treatment regimens, our results provide initial support for providing brief CR or EA skills during the initial phase of treatment to reduce alcohol consumption.
It is noteworthy that both the CR and EA skills were associated with decreased drinking over the 5-week follow-up assessment period with such brief interventions (i.e., a single session plus up to four coaching calls). Further, both groups had significant increases in their percent days abstinent from baseline to the final visit and for both groups, these changes were associated with medium to large effect sizes. Individuals in both active conditions increased their percent days abstinent by approximately 50%. Percent days abstinent is a commonly used metric to assess substance use treatment outcomes. Individuals with improvements in percent days abstinent typically experience reduced problems associated with alcohol as well as improved overall functioning (e.g., Hester, Delaney, & Campbell, 2011). These findings, therefore, provide further support for the clinical utility of delivering focused coping skills interventions early in treatment for those with PTSD/AD. This is particularly remarkable given that the participants had relatively severe and chronic problems with PTSD and AD as evidenced by their high rates of prior inpatient and outpatient treatment. Additionally, at baseline, participants reported consuming an average of 11.7 drinks per drinking day and had experienced an average of 6 traumas in their lifetime, the earliest of which occurred an average of 29 years prior to assessment. This sample was also unstable in that 22% were homeless and 85% were unemployed at the time of the baseline assessment. Despite this high level of distress and instability, a large percentage of these individuals returned for their second laboratory visit and received a coping skills therapy session (84.8%) and 88.5% of those who received this session finished the study (75.0% of the original 92 eligible participants completed the study). Additionally, the active coping skill conditions were associated with reduced drinking compared to control. Together, these results lend further support to the potential effectiveness, feasibility, and clinical utility of targeted coping skill interventions for individuals with comorbid PTSD/AD for alcohol use outcomes.
This study is the first to directly compare CR and EA skills to reduce alcohol use and PTSD symptom severity among a population with comorbid PTSD/AD. Results suggest that although both CR and EA skills can be helpful in bringing about a decrease in drinking at least in the short-term, CR appears to be associated with less drinking overall than EA. This may be due to potential differences in the ease with which participants can learn the CR versus EA skills in a single session and implement them with relatively little assistance. CR skills are somewhat more tangible and may be easier to implement after only a single session, with CBT treatment packages typically covering CR skills in only a session or two (e.g., Lewinsohn, Steinmetz, Antonuccio, & Teri, 1984; Marlatt & Donovan, 2005; Monti, Kadden, Rohsenow, Cooney, & Abrams, 2002). It is also possible that increasing cognitive flexibility and engaging in more balanced thinking is especially helpful in tempering impulsive behavior, as it may lead to the recognition of options other than drinking in situations historically associated with drinking. On the other hand, EA skills such as acceptance and mindfulness may take more time to effectively learn and implement, with mindfulness-based interventions often devoting many sessions (as many as 8 2-hour sessions) teaching and practicing mindfulness skills (Baer, 2003; Bowen et al., 2009; Williams, Duggan, Crane, & Fennell, 2006). It may be beneficial for future studies to examine the relationship between coping skill acquisition and alcohol use outcome measures. Our results suggest, however, that although it may be helpful to provide patients with comorbid PTSD/AD with a range of skills from which to choose when managing symptoms, CR skills should be prioritized and presented early in the treatment process in order to help reduce problematic drinking.
Despite the promising results for the skills to reduce alcohol use in this comorbid PTSD/AD sample, neither the CR nor the EA skills were associated with decreased PTSD symptom severity. One possible explanation for this is that the examples worked through during the therapy session (especially in the CR condition) and coaching calls were largely alcohol focused rather than trauma focused. As avoidance is a key feature of PTSD and is thought to maintain PTSD symptoms (Foa & Kozak, 1986), it is plausible that without focused assistance from the therapist in learning to use CR or EA to specifically address trauma-related symptoms, individuals in our study were unlikely to spontaneously use the skills to address trauma-related symptoms or cognitions. Thus, it is possible that patients would have benefited from spending more time directly discussing the ways in which the CR and EA skills could be applied to their PTSD symptoms. Further, models of PTSD/AD comorbidity posit alcohol use functions to self- medicate symptoms of PTSD (Khatzian, 2003; Ouimette, Read, Wade, & Tirone, 2010; Simpson et al., 2014; Wolitzky-Taylor, Bobova, Zinbarg, Mineka, & Craske, 2012). It is possible that reduced drinking meant that PTSD symptoms were not being self-medicated and were thus elevated in the short-term. If so, with continued practice of the CR and EA skills and a longer follow-up we might have observed a subsequent decrease in PTSD symptoms. Future studies should consider how best to deliver brief coping skill interventions to reduce both alcohol use and PTSD symptoms. A longer follow-up period would also allow for the examination of a possible sleeper effect with regard to PTSD symptoms and to determine whether the reduction in alcohol consumption is maintained.
Limitations of the present study include a relatively short follow-up assessment period of only 5-weeks; however, the collection of daily data provides valuable information about the incremental changes in symptomatology over time. Also, we did not assess all PTSD symptoms during the follow-up IVR assessment. Although we only excluded the symptoms that seemed unlikely to vary from day-to-day (e.g., foreshortened sense of the future) and were therefore not necessary to track on a daily basis, these symptoms could have changed over time as a result of skill acquisition in ways which we were not able to capture. Lastly, the act of recalling and reporting drinking on a daily basis may have enhanced the interventions by prompting participants to use their CR or EA skills, which could have contributed to the decrease in drinking over time associated with both of these conditions. However, given that those in the attention control condition also monitored their drinking daily and did not show marked decreases in their drinking argues that measurement reactivity was likely not a strong factor in our results. Future studies should examine whether the same decrease in alcohol use is observed if the CR or EA skills are administered without a subsequent daily monitoring assessment period or if the monitoring contributed significantly to the success of the interventions.
In conclusion, the present study provides an initial step toward addressing the benefit of targeted coping skills interventions in reducing alcohol use among individuals with comorbid PTSD/AD. Both CR and EA skills significantly reduced drinking over the 5-week follow-up assessment period compared to control; however, individuals who received the CR skills drank less alcohol on a given day than those who received EA. Future research should consider ways to strengthen the presentation and acquisition of the coping skills to more directly impact PTSD outcomes, and evaluate whether the changes in alcohol use are maintained over a longer period of time. Despite the study’s limitations, it is promising that a brief presentation of CR and EA coping skills was associated with reduced drinking among a highly distressed sample of individuals with comorbid PTSD/AD.
Highlights.
Cognitive restructuring (CR) and experiential acceptance (EA) coping skills were examined in a sample with comorbid PTSD/AD
CR and EA coping skills were associated with decreased daily drinking compared to control across a 5-week follow-up period
Individuals who were taught CR skills consumed less alcohol on a given day than those who were taught EA skills
Neither CR nor EA skills were associated with a decrease in PTSD symptom severity across the 5-week follow-up period
Results support prioritizing CR and EA skills during initial treatment sessions with individuals with comorbid PTSD/AD
Acknowledgements
This study was supported in part by a grant from NIH/NIAAA (R21AA17130; PI: Simpson) as well as by resources from the Center of Excellence in Substance Abuse Treatment and Education (CESATE) at the VA Puget Sound Health Care System.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- Abramowitz JS, Tolin DF, Street GP. Paradoxical effects of thought suppression: A meta-analysis of controlled studies. Clinical Psychology Review. 2001;21:683–703. doi: 10.1016/s0272-7358(00)00057-x. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data. In: Millsap RE, Maydeu-Olivares A, editors. The SAGE Handbook of Quantitative Methods in Psychology. Thousand Oaks, CA: SAGE Publications Inc; 2009. pp. 72–89. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Ed. Washington DC: Author; 1994. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. [Google Scholar]
- Bandura A. Social learning of moral judgments. Journal of Personality and Social Psychology. 1969;11:275–279. doi: 10.1037/h0026998. [DOI] [PubMed] [Google Scholar]
- Berenz EC, Coffey SF. Treatment of co-occurring posttraumatic stress disorder and substance use disorders. Current Psychiatry Reports. 2012;14:469–477. doi: 10.1007/s11920-012-0300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Perez-Fuentes G, Okuda M, Wang S. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2013;132:630–638. doi: 10.1016/j.drugalcdep.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins S, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer M, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Archives of General Psychiatry. 2010;67:85–93. doi: 10.1001/archgenpsychiatry.2009.173. [DOI] [PubMed] [Google Scholar]
- Drapkin ML, Yusko D, Yasinski C, Oslin D, Hembree EA, Foa EB. Baseline functioning among individuals with PTSD and alcohol dependence. Journal of Substance Abuse Treatment. 2011;41:186–192. doi: 10.1016/j.jsat.2011.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. Structured clinical interview for DSM-IV (SCID) New York, NY: New York State Psychiatric Institute; 1995. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: exposure of corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Yusko DA, McLean CP, Suvak MK, Bux DA, Jr, Oslin D, O’Brien CP, Imms P, Riggs DS, Volpicelli J. Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: a randomized clinical trial. Journal of the American Medical Association. 2013;310:488–495. doi: 10.1001/jama.2013.8268. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton S, Moore AM, Crane DR, Payne SH. Psychotherapy dropouts: Differences by modality, license, and DSM-IV diagnosis. Journal of Marital and Family Therapy. 2011;37:333–343. doi: 10.1111/j.1752-0606.2010.00204.x. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized Estimating Equations. Chapman & Hall/CRC: Boca Raton, FL; 2003. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Hester RK, Delaney HD, Campbell W. ModerateDrinking.com and moderation management: Outcomes of a randomized clinical trial with non-dependent problem drinkers. Journal of Consulting and Clinical Psychology. 2011;79:214–224. doi: 10.1037/a0022487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruska B, Fallon W, Spponster E, Sledjeski EM, Delahanty DL. Alcohol use disorder history moderates the relationship between avoidance coping and posttraumatic stress symptoms. Psychology of Addictive Behaviors. 2011;25:405–414. doi: 10.1037/a0022439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins D, Simpson T, Stappenbeck CA, Blayney J, Lee CM, Larimer ME. Proximal relationships between PTSD symptoms and drinking among female college students: Results from a Daily Monitoring Study. Psychology of Addictive Behaviors. 2014;28:62–73. doi: 10.1037/a0033588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10(9):47–54. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence of the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton M. Longitudinal factor structure of posttraumatic stress symptoms related to intimate partner violence. Psychological Assessment. 2007;19(2):165–175. doi: 10.1037/1040-3590.19.2.165. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse Prevention: An overview of Marlatt’s cognitive-behavioral model. Alcohol, Research, & Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Steinmetz JL, Antonuccio D, Teri L. Group therapy for depression: The Coping with Depression course. International Journal of Mental Health. 1984;13:8–33. [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment for Borderline Personality Disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Marlatt GA, Donovan DM. Relapse Prevention, Second Edition, Maintenance Strategies in the Treatment of Addictive Behaviors. New York, NY: Guilford Press; 2007. [Google Scholar]
- Marlatt GA, George WH. Relapse prevention: Introduction and overview of the model. British Journal of Addiction. 1984;79:261–273. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- McCauley JL, Killeen T, Gros DF, Brady KT, Back SE. Posttraumatic stress disorder and co-occurring substance use disorders: Advances in assessment and treatment. Clinical Psychology: Science and Practice. 2012;19:283–304. doi: 10.1111/cpsp.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott MJ, Tull MT, Gratz KL, Daughters SB, Lejuez CW. The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. Journal of Anxiety Disorders. 2009;23:591–599. doi: 10.1016/j.janxdis.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Back SE, Brady KT, Baker AL, Hopwood S, …Ewer PL. Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence. Journal of the American Medical Association. 2012;308:690–699. doi: 10.1001/jama.2012.9071. [DOI] [PubMed] [Google Scholar]
- Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams DB. Treating Alcohol Dependence: A Coping Skills Training Guide. 2 nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- Monti PM, Rohsenow DJ, Michalec E, Martin RA, Abrams DB. Brief coping skills treatment for cocaine abuse: Substance use outcomes at three months. Addiction. 1997;92:1717–1728. [PubMed] [Google Scholar]
- Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: A review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95:1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Treatment of Posttraumatic Stress Disorder and Substance Abuse: Clinical guidelines for implementing the Seeking Safety therapy. Alcoholism Treatment Quarterly. 2004;22(1):43–62. [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking Safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11:437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Batten SV. Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification. 2005;29:95–129. doi: 10.1177/0145445504270876. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addictive Behaviors. 1998;23:785–795. doi: 10.1016/s0306-4603(98)00064-1. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Read JP, Wade M, Tirone V. Modeling associations between posttraumatic stress symptoms and substance use. Addictive Behaviors. 2010;35(1):64–67. doi: 10.1016/j.addbeh.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center ground zero. Journal of Abnormal Psychology. 2007;116:329–341. doi: 10.1037/0021-843X.116.2.329. [DOI] [PubMed] [Google Scholar]
- Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy: Veteran/military version. Washington, DC: Department of Veterans’ Affairs; 2008. [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. Journal of Consulting and Clinical Psychology. 2000;68:515–520. doi: 10.1037//0022-006x.68.3.515. [DOI] [PubMed] [Google Scholar]
- Sannibale C, Teesson M, Creamer M, Sitharthan T, Bryant RA, Sutherland K, Taylor K, Bostock-Matusko D, Visser A, Peek-O”Leary M. Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction. 2013;108:1397–1410. doi: 10.1111/add.12167. [DOI] [PubMed] [Google Scholar]
- Simon GE, Imel ZE, Ludman EJ, Steinfeld BJ. Is dropout after a first psychotherapy visit always a bad outcome? Psychiatric Services. 2012;63(7):705–707. doi: 10.1176/appi.ps.201100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ. Predictors of early dropout from psychotherapy for depression in community practice. Psychiatric Services. 2010;61:684–689. doi: 10.1176/ps.2010.61.7.684. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, Kaysen D. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123:237–247. doi: 10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Torchalla I, Nosen L, Rostam H, Allen P. Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment. 2012;42:65–77. doi: 10.1016/j.jsat.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- van Dam D, Vedel E, Ehring T, Emmelkamp PMG. Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: A systematic review. Clinical Psychology Review. 2012;32:202–214. doi: 10.1016/j.cpr.2012.01.004. [DOI] [PubMed] [Google Scholar]
- Vik PW, Islam-Zwart KA, Ruge LN. Application of the PTSD-alcohol expectancy questionnaire (P-AEQ) to sexually assaulted college women. Addiction Research and Theory. 2008;16:585–594. [Google Scholar]
- Weathers F, Ford J. Psychometric properties of the PTSD checklist (PCL-C, PCL-S, PCLM, PCL-PR) In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. [Google Scholar]
- Wegner DM, Schneider DJ, Carter SR, White TL. Paradoxical effects of thought suppression. Journal of Personality and Social Psychology. 1987;53:5–13. doi: 10.1037//0022-3514.53.1.5. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Duggan DS, Crane C, Fennell MJV. Mindfulness-based cognitive therapy for prevention of recurrence of suicidal behavior. Journal of Clinical Psychology: In Session. 2006;62:201–210. doi: 10.1002/jclp.20223. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, Hsu SH. Mindfulness-based relapse prevention for substance craving. Addictive Behaviors. 2013;38:1563–1572. doi: 10.1016/j.addbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors. 2012;37:982–985. doi: 10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]