Abstract
A clinician-randomized trial was conducted using the chronic care model for disease management for alcohol use problems among n=82 women served in a health care for the homeless clinic. Women with problem alcohol use received either usual care or an intervention consisting of a Primary Care Provider (PCP) brief intervention, referral to addiction services, and on-going support from a Care Manager (CM) for 6 months. Both groups significantly reduced their alcohol consumption, with a small effect size favoring intervention at 3 months, but there were no significant differences between groups in reductions in drinking or in housing stability, or mental or physical health. However, intervention women had significantly more frequent participation in substance use treatment services. Baseline differences and small sample size limit generalizability, although substantial reductions in drinking for both groups suggest screening and PCP brief treatment are promising interventions for homeless women with alcohol use problems.
Keywords: Alcohol abuse, Homeless women, Chronic care model, Primary care, Randomized trial
1. Introduction
There is a substantial prevalence of substance abuse among homeless women, including both alcohol and drug use. At the same time, there is limited gender-specific research on how to best address prevention and treatment of addiction problems among women, and especially among such high risk populations as homeless women. (National Research Council, 2010) Studies of homeless women surveyed on the street or in shelters over the past two decades have shown that between 31% and 41% have a lifetime alcohol abuse, or dependence problem, and up to 82% have a substance use disorder inclusive of both drugs and alcohol. (Bassuk, Buckner, Perloff, & Bassuk, 1998; Nyamathi, Longshore, Galaif, & Leake, 2004; Robertson, Zlotnick, & Westerfelt, 1997; Torchalla, Strehlau, Li, & Krausz, 2011; Wenzel et al., 2004; Wenzel et al., 2009) A recent study that screened 461 women receiving primary care in a health care for the homeless clinic, found 43.8% reported hazardous drinking in the last year. (Upshur, Weinreb, & Bharel, 2013). Further, studies of the homeless have found that a substance use disorder, or continued consumption of alcohol or illegal drugs, have an effect on housing stability, length of homelessness, and ability to exit homelessness. (Bassuk, et al., 1997; Bird et al., 2002; Folsom et al., 2005; Gregorie, 1996; Reardon, Burns, Preist, Sachs-Ericsson, & Lang, 2003; Sosin and Bruni, 1997; Weinreb, Rog, & Henderson, 2010; Zlotnick, Tam, & Robertson, 2003).
Despite wide recognition of substantial substance use issues in the US, access to services and engagement in addiction treatment is limited. The National Survey on Drug Use and Health in 2003–2004, for example found only 7% of the 19 million adults with a need or alcohol treatment actually received treatment. (Willenbring, 2007). However, homeless individuals may have even more barriers to accessing addiction services than other populations. For example, lack of stable housing may result in inability to use outpatient treatment (Wenzel et. al, 2001), women with social networks consisting primarily of substance users often are discouraged to engage in treatment (Kertesz et al, 2006), and high rates of co-occurring mental health problems, common in homeless populations, are associated with less use of substance abuse treatment. (Gonzalez & Rosencheck, 2002; Wenzel et al. 2001) In addition, clinicians in health care settings working with the homeless population may presume that their patients have less ability and motivation to take advantage of addiction services (Wen, Judak, & Hwang 2007). However, a recent study that examined motivation to address drug and alcohol problems among homeless women compared to low income women without a homelessness experience, found no differences in motivation to reduce alcohol or drug use between these groups of women. (Upshur, et al., 2014). Nevertheless, while specialized health care services are available for homeless individuals (Section 330 (h) of the Public Health Service Act), providers in these settings, as well as general medical care, struggle with how to best engage patients in addiction treatment.
Women seem to have particular barriers to engaging in addiction services because traditional treatment models have been male-oriented and male-dominated. (Gessler, Bormann, Kwiatkowski, Braucht, & Reichardt, 1995; National Women’s Resource Center, 1997; Zerger, 2002) On the other hand, women, including homeless women, use primary health care more frequently than men (Stein, Anderson, Koegel, & Gelberg, 2000), and women with addiction problems are more likely to follow detoxification by linking to primary care when supported to do so. (Saitz, Larson, Horton, Winter, & Samet, 2004) There is also evidence that women feel primary health care is less stigmatizing than specialty services for substance use or mental health concerns. (Green, 2006)
Health care reform in recent years has similarly moved in the direction of providing more comprehensive services for mental health and substance abuse in primary care. For example, there is current support for the importance of primary care settings to address alcohol use problems by providing screening, brief intervention, and treatment referrals. (Solberg, Maciosek, & Edwards, 2008). One model that has recently been promoted as a framework for addressing drug and alcohol problems and other health risk behaviors in primary health care settings is the collaborative care/chronic illness model (CCM). (Hung, et al., 2007; Saitz, Larson, LaBelle, Richardson, & Samet, 2008; Watkins, Pincus, Tanielian, & Lloyd, 2003) The CCM was initially focused on diseases such as diabetes, which require patient engagement in managing the condition, and frequent physician monitoring. (Wagner, Austin, & Von Korff, 1996) Watkins, et al. (2003) and Saitz et al., (2008) both point out the characteristics alcohol use disorders have in common with other chronic medical diseases to support the notion that the CCM has promise to address alcohol problems in primary health care settings. These include the long term and relapsing nature of alcohol use disorders, the unpredictable course of symptoms, complex origins, the need for patient-initiated care/collaboration, behavioral supports, and frequent monitoring. The premise is to reorganize the typical pattern of delivering acute or episodic care to individuals with chronic illnesses, by proactively managing care and engaging patients in collaboration in their health care maintenance.
The current study implemented the CCM in a small pilot, clinician randomized trial, to treat women who screened positive for hazardous drinking during a primary health care visit in a health care for the homeless clinic. To date there are limited trials of the CCM addressing alcohol use disorders in primary care, and none that address the specific needs of homeless women who have significant need for effective treatment options. The study was called Project RENEWAL: Research and Evaluation on NEW ALcohol Treatment Interventions for Homeless Women. The study hypotheses were that: 1) the CCM would significantly increase initiation, engagement, and retention in alcohol treatment for the intervention group compared to the usual care group over the 6-month follow up period; and 2) there would be significant effect sizes favoring Intervention women on drinking amounts, mental and physical health, and housing outcomes to justify further research and dissemination of this treatment intervention. All participants provided informed consent and the study was conducted in accord with the standards of the University Institutional Review Board for research on human subjects.
2. Materials and Methods
2.1 Site and recruitment methods
Project RENEWAL was conducted in a federally qualified health center in the Northeast that is one of a national network of 208 health care for the homeless grantees (Health Care for the Homeless Program, 2011). Subjects were women seeking primary health care services and who met the following study criteria: 1) screened positive for hazardous drinking using a validated alcohol use screening instrument; 2) had an assigned primary care provider (PCP) at the site or were willing to agree to receive on-going primary health care at the site; 3) were English speaking; 4) were 18 years of age or older; 5) were not receiving on-going residential or outpatient substance abuse services or HIV case management at time of study entry; and 6) were not actively psychotic at study entry.
Women with clinic appointments over a one year period were screened in the clinic waiting room using the AUDIT-C, 3-item alcohol screening instrument frequently used in primary care settings. (Bradley et al., 2007; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998; Fiellen, Reid, & O’Connell, 2007; Frank et al., 2003; Gordon et al., 2001). A one-page back to back sheet included demographic questions and the three AUDIT items on the front, along with a box to check if they were willing to discuss participation in a study and provide contact information. The back of the sheet had 11 additional questions with yes/no responses designed to establish whether their alcohol use met the DSM-IV definition of abuse or dependence (National Institute on Alcohol Abuse and Alcoholism, 2005). The AUDIT-C questions were modified in two ways: 1) the amount of drinks required to indicate binge drinking was lowered to the level hazardous for women (4 or more drinks instead of 5 or more drinks), and 2) the description of alcohol included use of substances such as cough syrup and mouthwash which are often used in the homeless population. (For more information about the screening process please see Upshur, Weinreb, and Bharel, 2013.) Clinic staff scored the responses and women whose score was 4 or greater (range was 0–12), were asked to fill out or decline the study contact information, and to complete the back of the form to assess symptoms of alcohol abuse or dependence. This score was one point above the minimum score indicating hazardous drinking in order to assure study referrals were women with significant alcohol consumption issues. All forms were then attached to the patient paperwork provided to the clinician at the health care visit.
2.2. Randomization and study enrollment
The research design was a clinician randomized design. All PCPs (MDs, PAs and NPs) who provided on-going primary care services at the clinic were randomly assigned to intervention or usual care condition by a computer program. There were 15 clinicians in the study. All patients of the clinic were routinely assigned a PCP, and therefore, the intervention status of study participants depended on their assigned clinician’s status Study enrollment occurred at a primary care visit after Project RENEWAL screening was launched in the clinic, and after a positive screen (score of 4 or more) and agreement to be contacted by the study Research Coordinator (RC). At the end of the health care visit, the PCP or nurse was asked to call the on-site research office. The RC or a volunteer would then escort the potential participant to the research office to discuss Project RENEWAL, complete informed consent, and the baseline study interview. Prior to completing the consent and interview a pre-screening process was used to verify eligibility based on all study criteria (described above). In addition, current sobriety was checked by using a salvia blood alcohol screening kit. Women who did not have time to complete study enrollment or who were intoxicated at the time (blood alcohol level >.08), were asked to return at an appointed time to complete enrollment.
2.3 Intervention and Usual Care
The Project Renewal intervention consisted of: 1) providing evidence-based training and supports to the medical leadership and randomized intervention PCPs; 2) modifying the electronic medical record (EMR) to provide alcohol screening results and alcohol-specific notes for PCP and Care Manager (CM) visits; and 3) training a CM specifically designated to provide intervention participants with alcohol education materials, ongoing self-management support, linkage to formal addiction treatment services and self-help groups, and wellness counseling and goal setting. The study period lasted 6 months from enrollment for each participant.
The PCP training included 8 hours in 5 didactic sessions on the chronic care model, using the modified EMR module for documenting problem alcohol use and intervention strategies (e.g. brief motivational intervention, education materials, drinking reduction goal setting, wellness goals, referrals to formal substance abuse services, referrals to the clinic’s mental health services), interpreting the screening measure, completing a brief alcohol intervention as described in the NIAAA Clinician’s Guide (National Institute on Alcohol Abuse and Alcoholism, 2005), review of pharmacological treatments for alcohol addiction, motivational interviewing training, and working with the CM. A 15-page “Intervention Provider Manual” synthesized the recommended treatment steps for the PCPs and was provided to each. Two sessions were held prior to the study starting and 3 additional booster and review sessions were provided over the subsequent year.
The study was targeted to both dependent and non-dependent drinkers within an overall harm reduction approach, and use of a range of treatment approaches (self-help, specialty care, and medications) matched to the willingness of the participant to engage in care were emphasized in the clinician training. This approach, paired with supportive care management, was hypothesized to be more effective in engaging this population of women drinkers than attempting to stratify treatment approaches according to drinking severity.
Intensive CM training (20 hours) was provided based on a study-developed CM treatment manual. The Project RENEWAL CM was a bachelor’s level trained health worker who had served in previous settings as a case manager for at-risk pregnant women and those with substance use problems. The treatment manual was modified from prior work of the study team implementing the CCM in primary care for depression treatment. The training included: information on the CM role for the study; collaborating with the PCPs; using the documentation templates in the EMR; assessing baseline history and services needs; motivational interviewing techniques; delivering trauma-informed care; the patient follow-up schedule; a structured format for each follow-up visit; patient education materials on safe alcohol consumption for women, problem alcohol use consequences for women, self-management goal setting; and up-to-date lists of local addiction services and AA groups that patients could be referred to. Weekly or biweekly supervision meetings were held between the CM and site mental health staff and the study Co-Investigator to assure ongoing support and training. Part of each supervision meeting included a review of each contact with study participants since the last meeting, based on the recommended visit format and follow-up schedule in the CM manual to assure fidelity to the model.
Intervention patients received the guideline-based PCP brief intervention for problem alcohol use (National Institute on Alcohol Abuse and Alcoholims, 2005), and referral to the CM for ongoing follow-up visits for 6 months. It was expected that PCPs would provide 4–6 appointments after the brief intervention session, to encourage patient commitment to reducing or maintaining safe alcohol consumption, to encourage use of addiction medication when appropriate, and to follow-through with substance use treatments of the subject’s choice during the 6-month study follow-up. The CM was asked to complete at least 15 phone or in-person follow-up sessions in 6 months. Usual care patients did not receive referrals to, or outreach from, the study-trained CM and their PCPs were not provided any alcohol intervention training or patient materials. They delivered usual care for medical conditions, including any behavioral health or drug or alcohol use problems. All intervention and usual care participants had unrestricted access and use of all primary care and specialty care offered by the clinic, including mental health services (counseling and psychiatry); dental and vision services; laboratory and radiology; pharmacy; ob/gyn; medical respite care; hospital admissions; and general case management for benefits, employment, housing, transportation, and legal issues. Both usual care and intervention clinicians received a copy of the alcohol screening results for their patients. Both usual care and intervention participants were contacted at 3- and 6-months post-study enrollment for follow-up research interviews by the RC who was not involved with any intervention training or clinical care activities and was not aware of type of treatment received by any participants. .
2.4 Measures
Primary outcomes
Initiation, engagement and retention in treatment
The Washington Circle (McCorry, Garnick, Bartlet, Cotter & Caulk, 2000) definitions of initiation, engagement and retention in substance use treatment were used to determine use of services. All service use data were gathered from the electronic health record or the CM visit notes based on patient self-report. Initiation of treatment was defined as an inpatient hospitalization or keeping an initial alcohol use disorder (AUD) program appointment within 14 days from referral. Treatment engagement was defined as completing two additional treatment activities (e.g. group or individual sessions) during the 30 days after treatment initiation or discharge from inpatient detoxification. Treatment retention was defined as a minimum of three completed AUD services with the same AUD treatment program and/or AA or other 12-step meeting attendance in the three months after initiation. Reduction in alcohol use: The Time Line Follow Back (Sobell and Sobell 1992, Sacks, Drake, Williams, Banks, Herrell, 2003) was used to determine monthly alcohol consumption in the last three months. This is a self- report measure which reviews each day of each of the last three months using a calendar and having the respondent approximate how many drinks were consumed each day. The same procedure was used to determine the number of days in the last three months that illegal drugs were consumed. Drugs asked about included illegal prescription drugs, heroin, cocaine, marijuana, methamphetamine, hallucinogenics, and other street drugs.
Alcohol use consequences
A self-report measure developed by Weisner and Schmidt, 1995 collected information on 11 items regarding the negative consequences of alcohol use. Items are in a yes/no format and include questions about arrests, accidents, fights, and difficulties with family or employers due to alcohol use.
Mental and physical health status
General mental and physical health status was measured using the SF-8 (Ware, Kosinski, Dewey, & Gandek, 2001). The SF-8 is derived from the SF-36, one of the most widely used measures of health outcomes for clinical research. High internal reliability, and concurrent and predictive validity for health-related quality of life have been found for the physical and mental component scores (PCS and MCS). The scale provides population norming centered at 50 points indicating average health.
Housing status
The Residential Time-Line Follow Back Inventory (New Hampshire-Dartmouth Psychiatric Research Center, 1995; Cary, Carey, Maisto, Gordon & Weinhardt, 2001; Tsemberis, McHugo, Williams, Hanrahan, & Stefanic, 2007) was used to document where women were living over the past 90 days. The interviewer used a calendar and reviewed each night where the participant stayed using a large range of possible type of living situations, including own apartment, shelter, street/car/abandoned building, medical facility, family and friends, motels/hotels, and various residential programs.
Independent variables
Demographics of study sample
Information about age, ethnicity, employment status, marital and parenting status, insurance status and use of services was collected at baseline.
Co-morbid mental health conditions
Due to expected high rates of depression and Post Traumatic Stress Disorder, (PTSD), information about each was collected at baseline and follow-ups. The depression measure used was the PHQ-9 (Kroneke, Spitzer and Williams, 2001), widely used in primary care for its high sensitivity and specificity to detect major depression based on DSM criteria. The PTSD measure was the PSS (Foa, Cashman, Jaycos, & Perry, 1997; Foa. Riggs, Dancu, & Rothbaum, 1993), used to identify current symptoms subsequent to trauma.
Motivaton to change drinking
Three motivational items were asked at baseline concerning, 1) importance of changing drinking levels; 2) readiness to change drinking; and 3) confidence in success in changing drinking. These items have been used in prior work on homeless women’s motivation to change drinking (Upshur, Weinreb, Cheng, Kim, Samet, & Saitz, 2014). Each of the three items was rated on a scale of 1–10, with 1 noted as ‘not very important’ and 10 noted as ‘extremely important”.
Treatment Services
Service data were collected by getting data reports from the clinic’s EMR on all internal PCP, CM, and Behavioral Health counseling and psychiatry visits during the 6 month follow-up period after study enrollment.
Provider attitudes about treating alcohol misuse
A measure adapted from work training PCPs to treat depression was administered to clinicians at the beginning and end of the study (Upshur and Weinreb, 2008). The measure consists of 25 items tapping attitudes, skills, and practices treating alcohol use problems. The overall scale alpha reliability was .73 for this sample, with subscale reliabilities of .34, .82, and .68 respectively for clinician attitudes, clinician skills, and clinician practices.
2.5 Analysis
Data were analyzed using Stata/MP software version 12.1 (Stata Corp, 2011). Differences between usual care and intervention for various characteristics of the study sample were assessed using chi square statistics for all categorical variables with cell counts of >5 in each cell. For those items with smaller cell counts, Fisher’s exact tests were used. Differences in means of continuous outcomes were compared by a t-test when normality assumptions were met and a Wilcoxon ranksum test for outcomes with skewed distributions. Generalized estimating equation (GEE models) accounting for repeated measurements over time within study participants estimated odds ratios to compare differences in service use, motivation to change and abstinence over time between study arms.
The association of change from baseline in average number of drinks consumed in previous 3 months with intervention activities and services provided was estimated using quantile regression analysis utilizing the median of a kurtotic distribution. Multivariable models were adjusted for study arm, age, sum of all days using drugs in past 3 months, number of different housing situations, PTSD screen and baseline drinking. Total visits over the 6 month study were used. Number of visits was categorized because of small numbers of participants with greater than 1 or 2 visits. Total number of visits to current PCP, number of behavioral health visits, total number of care manager visits (for intervention women) and total number of visits to any intervention PCP (for control women) were combined to create a new variable, total number of visits to any provider/service. Associations were estimated in intervention and usual care groups separately, as well as combined. Residual analysis indicated some potential outliers. Models were run removing the outliers and results did not change, so all data are reported.. The association of patient characteristics and change from baseline in average number of drink in the previous 3 months was estimated using quartile regression as well. Multivariate models were adjusted for study arm, age, sum of all days using drugs in the last 3 months, number of different housing situations and baseline drinking.
The association of log of average number of drinks in the previous 3 months and participant characteristics was estimated using linear regression at 3- and 6-months separately. Trend in drinking over time was examined using the log of average number of drinks in the previous 3 months in an unadjusted random intercept model that included an interaction of study arm with time. Alternative outcomes, such as number of days using drugs and several different housing situations were explored using an unadjusted random intercept model. Further, effect sizes (ES) were calculated for all main outcomes. For continuous measures the ES was calculated by subtracting usual care group change from baseline from intervention group change from baseline and standardizing by the pooled standard deviation. Effect sizes for categorical measures were calculated using Cramer’s V. Finally, accounting for clustering by PCP did not substantially change estimates in the models so results reported show only data by individual subject.
3. Results
3.1 Study sample and baseline differences
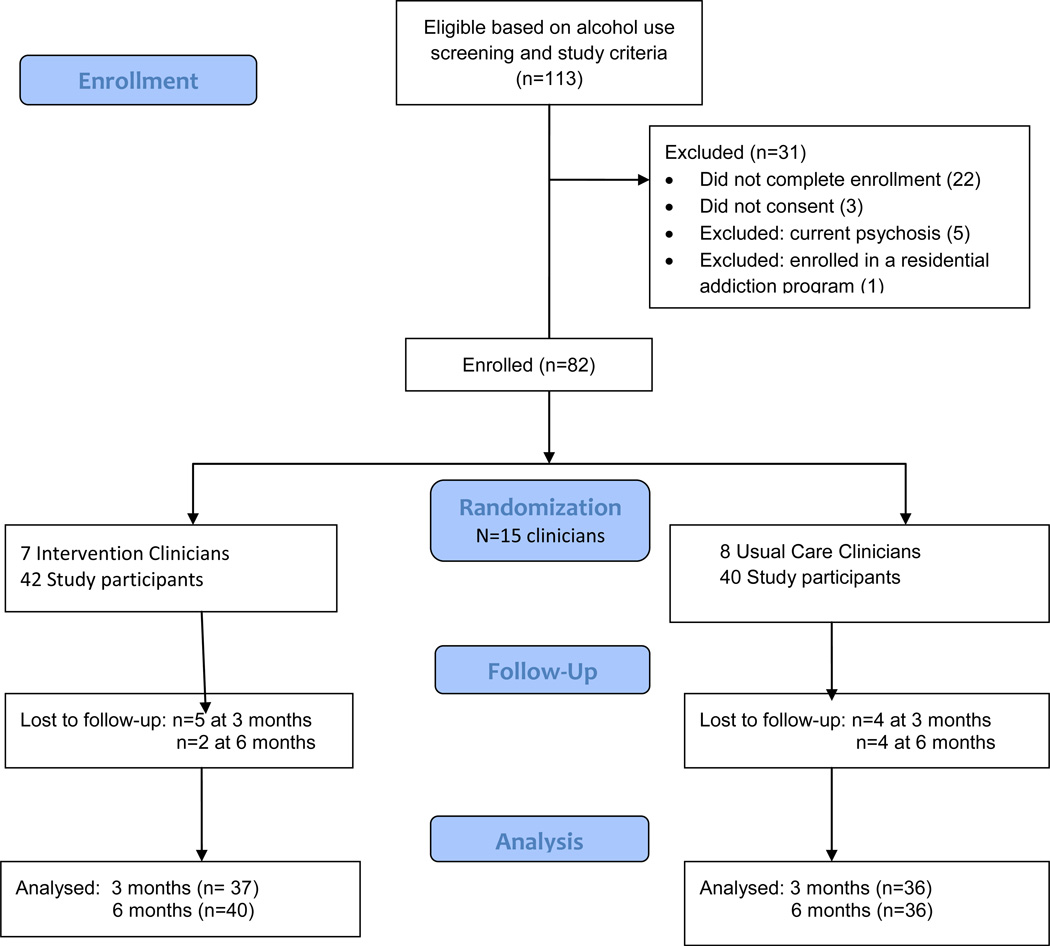
Figure 1 shows the CONSORT diagram for study recruitment, enrollment, and retention. Of n=113 women who screened positive and initially met all study criteria, only a few women were dropped from participation because of subsequent screening steps. We have little information on the 22 women who were referred to the study, but never met with the RC, other than they met the risky alcohol use score. This was because the RC only initiated a study file and recorded information for women who completed a face to face meeting. Otherwise all screening data were kept anonymous.
Figure 1.
CONSORT Study Diagram
Table 1 provides basic demographic information, baseline housing situation, baseline alcohol and drug use, and mental and physical health characteristics for both study groups. There were few significant differences except that the intervention group had significantly more days of illegal drug use at baseline compared to usual care participants, and more usual care participants had spent time on the street. Participants were on average in their mid-40s, had multiple recent housing situations including in their own apartment, on the street, in shelters, or (data not shown in table) staying with relatives or friends, in hotels/motels, detox, in jail, hospitalized for medical or mental health conditions, in medical respite care, or group homes. Women were 41% Black, and 33% white, with the remainder of multiple races, Latino, or unknown. Only one participate was Asian. Similar rates of participants in both groups had an alcohol use disorder (93.3% of Intervention participants and 83.3% of Usual Care participants) and similar magnitude of negative consequences due to their alcohol use (mean >4 of 11 items for both groups). Overall, 89% met criteria for abuse and 62% for dependence, with only 11% not meeting the criteria for either disorder. Although about 1/3 of women did not complete the alcohol use disorder checklist on the back of the screening form, mean AUDIT-C scores for women without a complete AUD checklist were high and did not differ from those who did complete the checklist. This suggests likely similar rates of substance use disorders among those for whom the AUD scores were missing.
Table 1.
Baseline Characteristics of Study Sample
| Variable | Intervention (N=42) |
Usual Care (N=40) |
P value |
|---|---|---|---|
| Age: Mean Years (SD) | 44.8 (8.4) | 46.0 (10.5) | 0.56 |
| Race: N (%) White | 18 (43.0%) | 9 (22.5%) | 0.16 |
| Black | 14 (33.3%) | 20 (50.0%) | |
| Other (Asian, Latino, mixed, or refused) | 10 (23.0%) | 11 (27.5%) | |
| Housing status last three months: N(%)1 | |||
| Any time in own apartment | 15 (35.7%) | 14 (35.2%) | 0.95 |
| Any time in shelter | 22 (52.4%) | 21 (52.5%) | 0.99 |
| Any time in street | 4 (9.5%) | 11 (27.5%) | 0.04* |
| Baseline AUDIT-C Score: Mean (SD) | 9.0 (2.3) | 7.8 (2.9) | 0.04* |
| Alcohol Use Disorder2N (%) | 28/30 (93.3%) | 20/24 (83.3%) | 0.25 |
| Alcohol Consequences: Mean (SD) | 4.6 (2.9) | 4.3 (3.0) | 0.68 |
| Avg. # drinks/month consumed last 3 months: Median (SD) | 185.0 (251.4) | 87.3 (286.1) | 0.34 |
| Motivation to change drinking (mean of 3 items) | 8.0 (2.1) | 7.0 (2.5) | 0.08 |
| No alcohol consumption last 3 months: n (%) | 9 (21.4%) | 7 (17.5%) | 0.50 |
| Avg. # days last 3 months used other drugs Mean (SD)3 | 43.3 (48.0) | 25.9 (38.2) | 0.05* |
| Overall mental health (MCS) Mean (SD) | 36.5 (10.8) | 34.8 (11.0) | 0.51 |
| Overall physical health (PHS): Mean (SD) | 41.9 (10.8) | 40.0 (9.0) | 0.43 |
| Positive for depression: N (%) | 21 (50.0%) | 23 (57.5%) | 0.50 |
| Positive for PTSD: N (%) | 32 (76.2%) | 25 (62.5%) | 0.18 |
Number and percent do not show all housing situations and most women reported several housing situations
Inclusive of abuse and dependence; missing data for n=10 Intervention and N=16 Usual Care
Inclusive of prescription and nonprescription drugs: cocaine, opioids, marijuana and 6 others
p<.05
Three women in each group reported no drinking in the last three months at initiation of the study (although significant drinking in the prior year). The rate of consumption of alcohol varied dramatically for the rest of the sample, but was on average extremely high, over 200 drinks per month on average for both groups. Median consumption was 185 drinks for the intervention group at baseline and 87 drinks for the usual care group. In addition, there was frequent use of other drugs. The most frequent drugs of use were marijuana (61% of i Intervention and 42.5% of usual care group), cocaine (45% of intervention and 37.5% of usual care group), and opioids (heroin and prescription drugs: 26% intervention and 16 % usual care).
Both groups had substantially poorer overall mental and physical health than population norms as measure by the SF-8, and both groups had high rates of depression and PTSD symptoms. Few women were employed (only 3 in each group), and most received SSDI or SSI income and food stamps (data not shown in table). Average income primarily from these public sources was under $850 a month. Most (over 80% at enrollment) had health insurance, primarily from the state Medicaid program, and by the end of the study all but one participant reported having health insurance.
3.2 Intervention implementation and satisfaction
The average number of PCP visits during the 6- month follow-up period, for intervention participants was 4.5 (SD=4.7, range 1–27). Over one quarter (n=10) received only the one PCP visit at which alcohol use screening took place and no additional visits. PCPs indicated a mean of 1.8 visits (SD=1.3, range 0–5) where the PCP brief intervention was implemented, and M=1.5 (SD=1.2, range 0–4) where substance use treatment planning was discussed. Intervention participants (n=20 or 48%) also completed an average of 3.9 visits to behavioral health providers on site (SD=6.6, range 0–38). Usual care participants had a mean of 3.2 (SD=2.93 range 1–15) PCP visits and 2.6 (SD=3.9, range 0–17) behavioral health visits. Differences in visit frequency were not significant between the two groups for PCP or behavioral health visits, but in combination with CM visits, Intervention participants received a mean of 12.1 total visits (SD=12.9, range 1–73), while usual care participants received a mean of 6.2 (SD=6.7 range 1–32) total visits (p<.01).
To determine fidelity to the intervention activities requested of clinicians, documentation of what clinicians delivered to study participants in the intervention group was obtained through a special template created in the EMR that was not visible to control group clinicians. This implementation fidelity system required the clinician to check what 10 steps of the suggested brief intervention activities were accomplished at each visit. Monitoring of implementation was used to reinforce the requested activities during the booster training sessions. This provided a measure of how many aspects of the brief intervention were undertaken by the clinicians. While all intervention providers completed the alcohol treatment template for most of their assigned study patients, and the rate of completion did not differ across time, for 1/3 of intervention study participants, no specific alcohol intervention activities were recorded. On average, the 7 intervention clinicians delivered 72% of the planned intervention activities to those participants for whom documentation was completed (n=28), with four achieving 75% or greater implementation across study participants. More than 80% of the participants had a discussion about drinking, the risks of drinking, had their stage of motivation to change assessed, and agreed to meet with the Care Manager. Less frequently was a wellness goal set (65%), medication offered (63%), a reduction in drinking goal set (52%), a referral made to specialty care (43%) and educational handouts given (24%).
The average number of CM contacts for the intervention group was 3.6 (SD=4.7, range 0–22) while, by design, the usual care group did not receive CM services to support alcohol use treatment. About one quarter (n=10) of intervention participants received no CM contacts. The most frequent content covered in the CM visits for those who attended were provision of alcohol education materials (87%), and setting drinking goals and discussing chronic illness management (across participants an average of 78% of sessions each). On average, over half of the sessions (58%) provided to participants focused on setting a self-management goal other than for drinking. In addition, discussing the participant’s views of her drinking and conveying the excess risk of risky drinking were the focus of 44% of the sessions each. About 40% focused on housing choices. One-third of the sessions reviewed medication compliance (inclusive of any substance abuse medications prescribed and other medications), and about one-quarter of sessions included referrals for formal substance use treatment. Other topics included discussing visits with children or families (19%), help with basic needs (shelter, food, transportation, 20%), and reminders to keep medical and services appointments (21%).
As far as participant evaluation of Project RENEWAL services, most were positive about the intervention experience (data not shown in a table). Almost three-quarters reported they would definitely or probably participate again in such a program (76.3% at the 6 month follow up), and 69.2% reported they were very satisfied with the program. Almost all reported they were a little bit better or much better (92.1 %) and that the improvement in their substance use and overall health was maybe/probably/definitely related to Project RENEWAL participation (73.0%). Analyses comparing treatment satisfaction of women (n=10) who did not ever use the CM, to those who had one or more visits with the CM showed comparable satisfaction with the overall program (about three-quarters highly satisfied in both groups) however those who had one or more visits with the CM also were more satisfied with their PCP treatment of their alcohol issues (76.7% versus 44.4% very satisfied), and more felt the program met almost all their needs (46.4% vs 11.1%, p=.054).
Finally, changes in PCP attitudes, skills and willingness to address substance use issues with their patients were found(data not shown). At the beginning of the study, intervention PCPs were less positive than usual care PCPs on several items about the frequency of alcohol problems, their willingness to treat alcohol problems, and their willingness to adopt new treatment practices. At the end of the study, all intervention PCPs reported they were ‘strongly’ willing to invest in treating alcohol use problems as well as to adopt new practices to treat alcohol use problems.
3.3 Substance use treatment services initiation, engagement and retention
Our first primary outcome was to determine if the intervention improved substance use treatment initiation, engagement, or retention. Table 2 shows the rate of services use at each of these levels at baseline, and 3- and 6-month follow-up for selected services (see section 2.4 for all categories of services documented). The only significant differences between intervention and usual care participants were baseline and 3-month utilization rates of counseling sessions for substance use. At three month follow-up, while one quarter of Intervention women did not use this service, over half of usual care participants did not use this service. Further, 68% of intervention participants had used the service three or more times (defined as treatment retention) over the previous 3 months compared to 31% of usual care participants (p<.01). This difference was not significant at 6-month follow up, but 58% of Intervention participants compared to 31% of usual care participants still met the criterion for retaining in this service.
Table 2.
Selected substance use and mental health treatment services initiation, engagement, and retention at baseline and 3- and 6-month follow up.
| Intervention | Usual Care | Intervention | Usual Care | Intervention | Usual Care | |
|---|---|---|---|---|---|---|
| N (Col %) | N (Col %) | N (Col %) | N (Col %) | N (Col %) | N (Col %) | |
| Baseline | 3 Months | 6 Months | ||||
| Met criteria for spending time in drug/alcohol treatment1 | ||||||
| Did not use this service | 35 (83.3%) | 31 (77.5%) | 32 (88.9%) | 31 (86.1%) | 31 (77.5%) | 31 (86.1%) |
| Initiation | 2 (4.8%) | 1 (2.5%) | 2 (5.6%) | 2 (5.6%) | 4 (10%) | 1 (2.8%) |
| Engagement | 1 (2.4%) | 1 (2.5%) | 0 (0%) | 1 (2.8%) | 0 (0%) | 1 (2.8%) |
| Retention | 4 (9.5%) | 7 (17.5%) | 2 (5.6%) | 2 (5.6%) | 5 (12.5%) | 3 (8.3%) |
| Pearson chi: | P=0.72 | P=0.80 | P=0.38 | |||
| Met criteria for talking about substance abuse with counselor (could include Project Renewal CM) | ||||||
| Pearson chi: | P = 0.72 | P = 0.80 | P = 0.38 | |||
| Did not use this service | 10 (23.8%) | 23 (59%) | 9 (26.5%) | 19 (52.8%) | 11 (27.5%) | 18 (51.4%) |
| Initiation | 4 (9.5%) | 1 (2.6%) | 0 (0%) | 4 (11.1%) | 1 (2.5%) | 2 (5.7%) |
| Engagement | 7 (16.7%) | 2 (5.1%) | 2 (5.9%) | 2 (5.6%) | 5 (12.5%) | 4 (11.4%) |
| Retention | 21 (50%) | 13 (33.3%) | 23 (67.6%) | 11 (30.6%) | 23 (57.5%) | 11 (31.4%) |
| Pearson chi: | P = 0.01** | P = 0.01** | P = 0.11 | |||
| Met criteria for attending AA meetings | ||||||
| Did not use this service | 23 (56.1%) | 25 (62.5%) | 21 (56.8%) | 26 (72.2%) | 20 (51.3%) | 22 (61.1%) |
| Initiation | 2 (4.9%) | 1 (2.5%) | 2 (5.4%) | 0 (0%) | 2 (5.1%) | 0 (0%) |
| Engagement | 2 (4.9%) | 4 (10%) | 0 (0%) | 0 (0%) | 1 (2.6%) | 0 (0%) |
| Retention | 14 (34.1%) | 10 (25%) | 14 (37.8%) | 10 (27.8%) | 16 (41%) | 14 (38.9%) |
| Pearson chi: | P = 0.63 | P = 0.20 | P = 0.37 | |||
| Met criteria for visits to mental health provider | ||||||
| Did not use this service | 15 (36.6%) | 20 (50%) | 15 (41.7%) | 22 (61.1%) | 13 (33.3%) | 20 (57.1%) |
| Initiation | 4 (9.8%) | 4 (10%) | 5 (13.9%) | 4 (11.1%) | 3 (7.7%) | 3 (8.6%) |
| Engagement | 6 (14.6%) | 1 (2.5%) | 2 (5.6%) | 0 (0%) | 5 (12.8%) | 4 (11.4%) |
| Retention | 16 (39%) | 15 (37.5%) | 14 (38.9%) | 10 (27.8%) | 18 (46.2%) | 8 (22.9%) |
| Pearson chi: | P = 0.23 | P = 0.25 | P = 0.16 | |||
| Total contacts with any substance use service | ||||||
| Did not use any services | 5 (11.9%) | 16 (40.0%) | 6 (16.2%) | 15 (41.7%) | 6 (15.0%) | 17 (47.2%) |
| Initiation | 1 (2.4%) | 2 (5.0%) | 2 (5.4%) | 3 (8.3%) | 2 (5.0%) | 0 |
| Engagement | 4 (9.5%) | 2 (5.0%) | 1 (2.7%) | 2 (5.6%) | 2 (5.0%) | 2 (5.6%) |
| Retention | 32 (76.2%) | 20 (50.0%) | 28(75.7%) | 16 (44.4%) | 30 (75.0%) | 17 (47.2%) |
| Fischers exact | P=.01** | P=.03* | P=.005** | |||
Criterion for initiation=1 visit; Criterion for engagement is 2 visits within 3 months; Criterion for retention is 3 or more visits in 3 months.
p<.05
p<.01
Examining the frequency of using any of the four types of substance use services over the follow-up study period combined, however, illustrates that intervention participants maintained a high rate of treatment retention compared to usual care women. At 3 months follow-up 76% of intervention, compared to 44% of usual care participants, had three or more contacts with any substance use treatment, while only 16% had no contacts and 42% of usual care participants had no contacts (Fisher’s exact, p<.05). At 6-month follow-up 75% of intervention participants continued to report 3 or more contacts with treatment services over the last three month, while 15% had no contact, compared to 47% of usual care participants with 3 contacts, and 47% with no contact (Fisher’s exact p<.01).
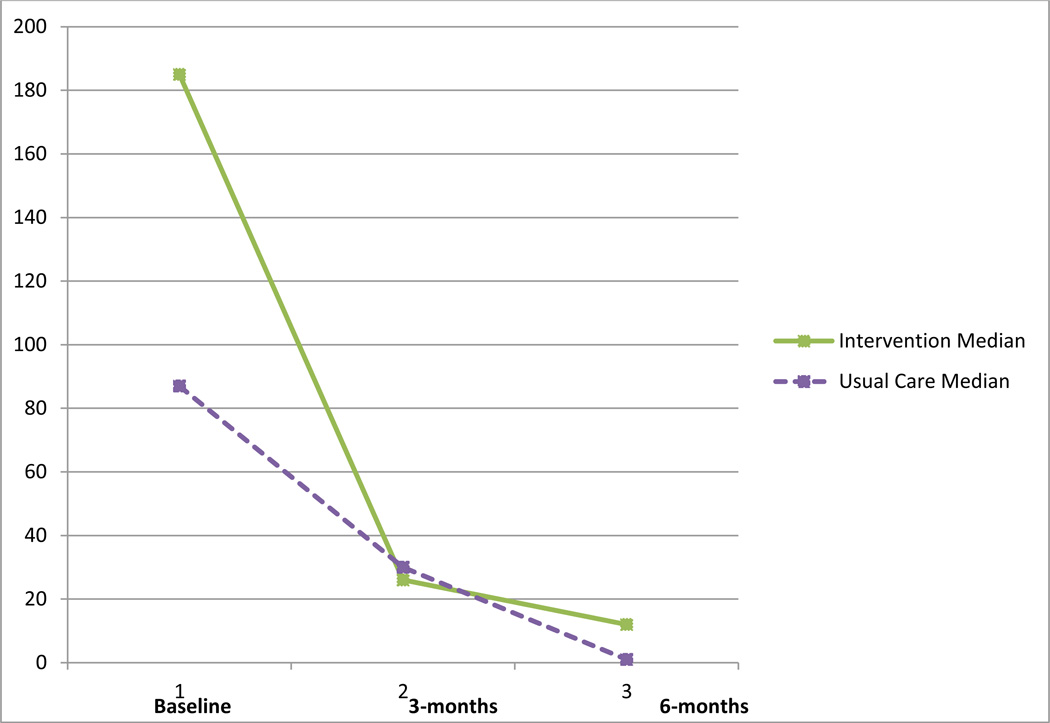
3.4 Substance use, housing, and mental and physical health outcomes
Table 3 presents 3- and 6- month study follow-up information on drinking amounts, drug use, housing status, depression, and overall physical and mental health. The rate of alcohol consumption decreased dramatically at both 3- and 6-month follow-up time points for both groups, from a median of 185 drinks/month at baseline, to 12 drinks/month for the intervention group and from a median of 87.3 drinks/month to 1.3 drinks/month for the usual care group, at 6-months. For both groups this represented a significant reduction in alcohol consumption (p=<.001), but we found no statistical differences between groups. At three months only, a small ES favored the intervention group, while by 6 months, a small ES favored the usual care group in level of alcohol consumption. In addition, a substantial proportion of both groups completely abstained from alcohol consumption in the follow-up period, representing statistically significant change from baseline to six months follow-up, but again with no significant differences between groups. The only significant differences between groups was a decrease in proportion of intervention participants meeting criteria for depression at 3-months, 32% vs. 56%, (p=<.05), and a significantly higher number of days of other drug use by intervention participants at 6-months (p=<.01). While not significant, intervention women’s reduction in alcohol use consequences and number of days using drugs, as well as their improvement in overall mental health showed small to moderate effect sizes.
Table 3.
Outcomes for substance use, housing, and mental and physical health, baseline and 3- and 6-month follow up.
| Variable | Baseline | 3-months | 6-months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Usual Care |
P value |
Intervention (N=37) |
Usual Care (N=36) |
Effect Size |
Intervention (N=40) |
Usual Care (N=36) |
Effect Size |
|
| # drinks/month last 3 months: Median (SD) | 185.0 (251.4) | 87.3 (286.1) | 0.34 | 26.0 (147.0) | 29.8 (194.9) | −0.18 | 12.0 (194.7) | 1.3 (78.7) | 0.17 |
| No alcohol consumption last 3 months: N (%) | 3 (7.1%) | 3 (7.5%) | 1.00 | 7 (18.9%) | 5 (13.9%) | 0.07 | 12 (30.0%) | 14 (38.9%) | −0.09 |
| Alcohol use consequences: Mean (SD) | 4.6 (2.9) | 4.3 (3.0) | 0.68 | 2.03 (2.1) | 2.9 (2.4) | −0.34 | 2.15 (2.7) | 1.9 (2.3) | 0.05 |
| # Days used other drugs last 3 months: Mean (SD) | 43.3 (48.0) | 25.9 (38.2) | 0.05* | 22.6 (39.7) | 21.6 (32.0) | −0.33 | 16.8 (29.4) | 3.9 (9.6) | −0.04 |
| Housing status last three months: N (%)1 | |||||||||
| Days in own apartment | 15 (35.7%) | 14 (35.2%) | 0.95 | 15 (40.5%) | 14 (38.9%) | 0.02 | 16 (40.0%) | 21 (58.3%) | 0.13 |
| Days in shelter | 22 (52.4%) | 21 (52.5%) | 0.99 | 18 (48.6%) | 18 (50.0%) | −0.01 | 12 (30.0%) | 18 (50.0%) | 0.12 |
| Days in street | 4 (9.5%) | 11 (27.5%) | 0.04* | 6 (16.2%) | 6 (16.7%) | −0 0006 | 7 (17.5%) | 4 (11.1%) | −0.13 |
| # Different housing situations last 3 months: N (%) | |||||||||
| 1 residence | 11 (26.2%) | 9 (22.5%) | 0.66 | 9 (24.3%) | 5 (13.9%) | 0.15 | 9 (22.5%) | 16 (44.4%) | 0.32 |
| 2 residences | 12 (28.6%) | 13 (32.5%) | 13 (35.1%) | 15 (41.7%) | 12 (30.0%) | 9 (25.0%) | |||
| 3 residences | 11 (26.2%) | 8 (20.0%) | 9 (24.3%) | 11 (30.6%) | 12 (30.0%) | 3 (8.3%) | |||
| 4 or more residences | 8 (19.1%) | 10 (25.0%) | 6 (16 2%) | 5 (13.9%) | 7 (17.5%) | 8 (22.2%) | |||
| Overall mental health (MCS) Mean (SD) | 35.6 (10.8) | 34.8 (11.0) | 0.51 | 38.8 (12.0) | 34.3 (11.9) | 0.21 | 39.5 (12.5) | 39.1 (10.6) | −007 |
| Overall physical health (PHS): Mean (SD) | 41.9 (10.8) | 40.0 (9.0) | 0.43 | 44.4 (10.3) | 42.3 (8.5) | 0.14 | 42.8 (11.5) | 41.0 (9.3) | −0008 |
| Positive for depression: N (%) | 32 (76.2%) | 25 (62.5%) | 0.50 | 12 (32.4%) | 20 (55.5%) | −0.23* | 16 (40.0%) | 17 (47.2%) | −007 |
Number and percent do not show all housing situations and most women reported several housing situations; p value based on total # days reported in this housing situation since last interview.
p<.05
There were no significant differences between groups at follow-up in housing status, housing stability, or overall mental or physical health. However, intervention women more than doubled the number of nights spent in their own apartment (p=<.01) at 6-months, compared to a 44% increase for usual care women (ns), although simultaneously usual care women decreased the number of nights in shelter by half (p=<.05), while intervention women’s use of shelter decreased by only 37%.
3.5 Association of participant characteristics and intervention services with outcomes
The change from baseline levels of drinking over the study period was modeled using quantile regression, modeling the median instead of mean drinks per month at both 3 and 6-month follow ups. Variables included Intervention status, age, days used drugs, number of different housing situations, and average number of drinks/month at baseline. In the adjusted model, for both follow-up time periods, the only two significant predictors were number of days using drugs (p=<.05 and p=<.001 at 3- and 6-months respectively), and baseline drinks/month (p=<.001 at both time points). The number of drug use days was associated with an increase in alcohol drinking rates, and the higher the baseline alcohol drinking rate, the greater the decrease in subsequent drinking. At 3-months, after adjusting for age, number of days using drugs, number of housing situations, and baseline drinking there was a non-significant reduction of −4.1 drinks/month for Intervention compared to usual care participants. At 6 months, after the same adjustments, the there was a non-significant increase in 1.4 drinks per month for intervention compared to usual care participants. In addition, motivation to change drinking was relatively high and not significantly different between groups at baseline, and was not significantly associated with changes in consumption for either intervention or control groups at either three or six month follow-up. Further, examination of alcohol consumption levels between participants classified as alcohol dependent versus nondependent revealed no significant differences at baseline, nor at 3- or 6-month follow-up.
Subsequent quantile regression models were constructed to examine 6-month outcomes for the intervention group only to see if there was an association between intensity of clinic service use and outcomes. This analysis used PCP, Behavioral Health, CM, and total health care visits over the study period. No significant associations were found overall for intervention participants in 3-month drinking levels, however, in an adjusted model (adjusted for age, days using drugs, baseline drinking level, and positive for PTSD), there was a non-significant reduction of −20.4 drinks for intervention participants who had 3 or more CM visits compared to those with 0–2 visits. Further, total contacts across all providers that were greater than 0–2 also were associated, although nonsignificantly, with reductions in drinking levels (−10.4 drinks for 3–7 contacts, −7.2 drinks for 8–13 contacts, and −14.4 drinks for 14 or more contacts).
Analyses were also conducted by stratifying the combined sample, and separately only within the intervention group, by one versus more than one PCP visit, and to examine any differences between women with no CM visits compared to those who had one or more CM visits. There were no differences in any of the outcomes associated with having more than one PCP visit versus only one. In addition, there were no differences in number of drinks per month, alcohol consequences, housing status, use of drugs, or mental or physical status scores comparing those with no CM visits versus one or more. However, at 3 month follow- up there was a non-significant trend (p=.08), and at 6-month follow-up a significant difference (p=.007), for participants with no CM visits to more often score positive for major depression.
4. Discussion
The current study tested a chronic disease care management intervention designed to improve alcohol use outcomes among women with a history of being homeless, and substance use problems, seeking health care services in a primary care clinic. Services were not targeted by drinking severity (e.g. high risk versus dependent drinkers), as in this hard-to-engage population, we hypothesized that allowing participants to choose among multiple treatment options would result in better treatment engagement overall even, though prior evidence suggests that different treatments are effective at different levels of severity of addiction.
We found that intervention women differed significantly from usual care women in their use of substance use services at each time point, including baseline. Overall they used services at a higher rate than did usual care women, and fewer intervention women had no service use in each of four categories of possible services compared to usual care women. However, participants in both groups did not use formal residential or structured outpatient substance use treatment programs very frequently (only 17.5% of usual care women and 9.5% of intervention had used a formal program in the last 3 months at baseline; these figures changed to 8.3% and 12.5% respectively at 6-month follow-up). Most used counseling and mental health services on site at the primary care clinic, or attended AA meetings. Among the 63% of the intervention group who were specifically offered addiction medication, only one accepted medication while the remainder refused. While there was not an overall significant change in increased initiation, engagement or retention in substance use services, nor uptake on medication, on the part of intervention women over time, given high baseline utilization rates, our data show that usual care women’s use of services tended to decrease over the follow up period, resulting in significantly higher overall use of services by the intervention women.
The rates of service use for substance use problems for both groups are far above those reported in other studies of homeless adults with substance use issues (Robertson, et al., 1997; Wenzel et al., 2001). This may be the result of selecting women for the study who had ongoing primary care relationships with the clinic, and therefore there were regular opportunities to link them to at least the on-site substance use counseling and mental health services. The acceptability of such services linked to primary care, rather than use of traditional off-site substance use services, is consistent with previously reported barriers for women clients to connect to programs that tend to be male oriented (Geissler et al., 1995, Zerger, 2002) While we cannot conclude that this intervention increased treatment initiation, engagement and retention, especially with specialty substance use treatment, we do conclude that the intervention may have had an effect on maintaining regular service utilization, an important dimension of ongoing chronic disease management. In examining outcomes, we found a substantial and significant decrease in alcohol consumption across both intervention and usual care groups, and no significant differences in housing type, housing stability or overall physical or mental health. The finding was surprising both in its dramatic amount of change, and in the fact that both groups of women significantly changed. Further, almost a third of the sample in both groups were abstinent from alcohol use for a full three month period at 6-month follow up, and well over half had one month of abstinence in the last three months at 6-month follow up (57.5% in intervention and 66.7% in the usual care group respectively). While the reduction in drinking across both groups could be due to regression effects given the very high baseline drinking rates, the very large changes also suggest the possibility that the observed improvement relates to the care received
We can account for the usual care group improvement in several ways. First, at baseline, PCPs assigned to the usual care condition compared to those assigned to the intervention, actually evidenced more interest and described implementing more treatment options for substance use problems in their patients. Thus usual care providers were already doing more to address substance use problems, and these positive biases in attitudes, skills and willingness meant that they may have already been delivering the type of care the intervention providers were being trained to deliver. While small numbers of providers precluded the pattern of differences from becoming significant, it appears that intervention providers increased their attitudes, skills and willingness to treat substance use problems due to the intervention training, while usual care providers were already delivering equally high quality care, thereby eliminating the expected differences in care due to the study activities. Thus patients in both groups received enhanced substance use treatment guidance from their PCP, thereby explaining the similar improvements in alcohol consumption by both groups. To address such preintervention bias, in future studies it will be necessary to determine PCP attitudes and treatment approaches prior to randominzation and stratify assignment to condition in advance.
Second, for ethical reasons, the research design called for all providers to receive a copy of the written AUDIT-C screening form at the clinic visit during which women were screened for alcohol risk in the waiting room. As a result, usual care clinicians indicated that the presence of a ‘lab report’ with an abnormal result prompted them to discuss risky drinking in the primary care visits in a different way than they might have been addressing the issue in previous encounters. Thus, while the PCPs of usual care women did not receive specific training on brief intervention for substance use, nor any of the special educational resources or referral supports received by the intervention PCPs, they still implemented a brief alcohol intervention. The power of primary care alcohol brief interventions has been demonstrated in other studies, including lower consumption and fewer drinkers consuming risky amounts (Beich, Thorsen, & Rollnick, 2003; Bertholet, Daeppen, Weitlishbach, Fleming, & Brunand, 2005; Kaner et al., 2009). The results of this study suggest that a motivated PCP implementing a brief intervention, perhaps paired with formal screening, may be enough of an intervention to make a difference in women’s substance use in a high risk population. This seems to be true whether or not women were alcohol dependent or just hazardous drinkers.
Third, while intervention intensity was estimated across participants at around 72% of all target activities, about 20% received less than 70% of the clinician intervention, and for another third we have no clinician documentation of alcohol intervention activities. Further, we did not assess quality of the intervention, nor conduct video, audio or live observations (the latter were done in role plays only in training). We also did not document what was delivered in the usual care condition, since we were concerned that providing a detailed checklist of brief intervention activities would cue the usual care clinicians even more into steps they could take with their patients who were drinking. While delivery of 50–80% of a planned intervention is considered adequate in many addiction intervention studies (Baer et al 2007), we are missing information on the intensity of the intervention for a sizeable portion of the intervention group and some portion of the group received suboptimal levels of the intervention. In part these variations can be expected in such a dynamic primary care setting with both highly transient patients as well as those with high comorbities of serious health conditions. However, further exploration of dose/response relationships was also hampered by the small sample size and large variation in drinking history among the sample. It is possible the intervention was not of sufficient intensity or fidelity, especially in comparison to usual care participants who also likely received some brief intervention activities for substance use as discussed above. Future studies addressed to improving primary care addiction interventions for homeless women will need to pay more attention to fidelity and quality documentation, as well as documenting the counterfactual condition.
The lack of other findings, such as in housing and overall physical and mental health, may be due to the short follow-up time frame of the study, and the small sample sizes given the baseline differences in the sample. Intervention women drank substantially more, were much more often poly drug users at baseline, and in fact reported significantly more days using illegal drugs at follow-up compared to usual care women. Baseline drug use was significantly associated with less reduction in alcohol consumption at follow-up. There were in addition, other limitations to teasing out the effects of the CM component of the study, since the intent-to-treat analysis resulted in about one quarter of the intervention women never receiving this component. Nevertheless, there was some evidence of a dose-response relationship, in that women who had more than three CM visits reported substantially lower numbers of drinks consumed than women with 0–2 visits. In addition, women with CM visits reported significantly less depression at 6-month follow-up.
There are also a few other limitations of the current study. One is that the health center was a well- established program with a long-standing history of serving homeless populations. Thus the clinicians were experienced in working with high risk populations, and many of the study participants had long-standing, and therefore established and trusting relationships with their PCPs that may have facilitated addressing substance use issues in ways that might not occur in newer programs. In addition, the study was conducted in an urban area with multiple resources for substance use treatment which offered a range of services to support PCP efforts to engage women in treatment that may not be available in small cities or rural areas. While most women did not use outside addiction treatment services, they were offered as options. In addition, almost all study participants had health insurance through the robust state Medicaid program, which also made access to services easier. In geographic areas where insurance coverage for homeless populations is limited, there may be many fewer mental health and addiction treatment services available.
What then are the lessons learned from this small provider randomized trial? Similar to the findings of another recent study using a chronic care model for addiction treatment in primary care (Saitz, et al. 2013), using an intent-to-treat analysis, there was no overall benefit for the intervention group compared to usual care.. Neither our study nor the Saitz et al. study found significant differences in abstinence rates, alcohol consequences, or overall physical or mental health during the study follow-up for participants receiving a chronic care model (CCM) intervention. This is despite a reasonable hypothesis that giving the chronic nature of substance abuse, ongoing monitoring and support to engage in substance use treatment might be more effective for dependent addiction than episodic and uncoordinated specialty care or medication alone. While both studies found some increase in addiction services use for the intervention group over the usual care group, other outcomes were similar for both groups and both groups evidenced some improvement over time.
Saitz et al. conclude that the CCM model may not be effective with dependent drinkers for several reasons. One is that the available treatments (psychosocial counseling, medication) for addiction are only marginally effective, and therefore merely increasing access to such treatments doesn’t change the overall pattern of addiction substantially. Further, similar to the current study, most of the patients were not seeking addiction services, and therefore, while expressing high motivation for treatment, the intervention was not powerful enough to overcome motivational and other barriers to changing substance use. This was certainly true for the current study where many woman indicated that they ‘needed’ to drink in order to tolerate life on the streets or in shelters. This leaves open the question of whether the CCM model in primary care would be helpful to less disadvantaged populations, those seeking treatment, or those with less severe addiction problems.
Nevertheless, the current study was remarkably successful in changing the alcohol consumption rates of a very high risk population of women over the short term. Thus, it appears that there may be promise in implementing screening and brief intervention (SBI) for risky drinking among women seeking primary care in homeless clinic settings, particularly if PCPs are encouraged and/or trained to act on the information. Our study suggests that PCPs who are predisposed to address substance use issues act more affirmatively to address substance use problems with their patients when presented with a ‘positive lab value’ even though they previously agreed that many of their patients have significant substance use problems. In fact, we had anecdotal stories that the positive AUDIT-C score sheet also seems to have affected some women to initiate substance use treatment on their own. Second, PCPs who are less inclined to address substance use issues changed their attitudes, willingness and actions after training and participation in the study. They became more willing to treat substance use and also more willing to adopt new practices for treating substance use in their patients. Finally, there is some evidence that frequency of contact with the CM, did result in dose-related reductions in alcohol consumption. The CM role might have also mediated the greater retention in mental health services for intervention women, and the slight increases in initiation, engagement and retention in formal substance use programs and AA attendance found at the last follow up time point.
Given that women using homeless primary care clinics are among the most at risk populations for substance use disorders, there is a great need to identify treatment approaches that can improve their AUD service utilization and outcomes. This pilot study suggests it will be beneficial to examine the various components of the intervention model more carefully in a larger scale study. Particularly important would be to compare the full chronic disease model with screening and brief intervention alone, as the implications for cost-effective reduction in risky alcohol use among these vulnerable women are significant. Further, continued research about how to efficiently and effectively integrate substance use treatment services within primary care settings will be important as the implementation of the Affordable Care Act will begin to provide better insurance access for such vulnerable populations around the country.
Figure 2.
Changes in median number of drinks consumed per month.
Highlights.
The study randomized primary care providers to implement a brief alcohol intervention
Target patients (n=82) were woman screening positive for risky drinking in a homeless clinic
In addition to a brief clinician intervention, 6-months of intensive care management was provided
Both intervention and usual care patients showed significant improvement in drinking levels
Few benefits were shown for housing status or overall mental and physical health
Acknowledgements
This study was supported by grant # R21AA018311 from the National Institute of Alcohol Abuse and Alcoholism. The authors wish to acknowledge the research and clinical staff of the Boston Health Care for the Homeless Program who participated in the study: Jim O’Connell, MD, President; Research Office: Erin Stringfellow, MSW, Julie Marston, MPH, Jess Hoy, Leah Isquith, and Stacy Swain, MHD, MDiv.; Clinical Staff: Erline Destra and Kim Herman, Care Managers; Rita Chapman, BSN,RN, LADC1, Clinic Director; Barbara Cocci, LICSW, Director and Ester Valdez, MD, Medical Director for Behavioral Health Services; Toni Abraham, NP, Assnt. Medical Director; Barry Bock, RN, Director, Clinical Operations; Pooja Bhalla, RN, Asst. Dir. Clinical Operations; Ava Cherloff and Joan Nordberg, Information Services. We also wish to thank the Project Staff from the Department of Family Medicine and Community Health, Susan Van Buskirk, MEd, and Gail Sawosik.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Carole Upshur, Department of Family Medicine and Community Health, University of Massachusetts Medical School.
Linda Weinreb, Department of Family Medicine and Community Health, University of Massachusetts Medical School.
Monica Bharel, Departments of Medicine, Boston University Medical Center and, Massachusetts General Hospital, Boston Health Care for the Homeless Program.
George Reed, Department of Quantitative Health Sciences, University of Massachusetts Medical School.
Christine Frisard, Department Medicine, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School.
References
- Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homelss and low-income housed mothers. American Journal of Psychiatry. 1998;155:1561–1564. doi: 10.1176/ajp.155.11.1561. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Buckner JC, Weinreb LF, Browne A, Bassuk SS, Dawson R, Perloff JN. Homelessness in female headed families: Childhood and adult risk and protective factors. American Journal of Public Health. 1997;87:241–248. doi: 10.2105/ajph.87.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS, Ball SA, Campbell BK, Miele GM, Schoener EP, Tracy K. Training and fidelity monitoring of behavioral interventions in multi-site addictions research: A review. Drug and Alcohol Dependence. 2007;87:107–118. doi: 10.1016/j.drugalcdep.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beich A, Thorsen T, Rollnick S. Screening in brief intervention trails targeting excessive drinkers in general practice: Systematic review and meta-analysis. British Medical Journal. 2003;327:536–542. doi: 10.1136/bmj.327.7414.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlishbach V, Fleming M, Brunand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Archives of Internal Medicine. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Bird CE, Jinnett KJ, Burnam MA, Koegel Pl, Sullivan G, Wenzel SL, Ridgely MS, Morton SC, Miu A. Predictors of contact with public service sectors among homeless adults with and without alcohol and other drug disorders. Journal of Studies on Alcohol and Drugs. 2002;63:716–725. doi: 10.15288/jsa.2002.63.716. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clinical and Experimental Research. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Cary MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behavior with the Timeline Followback (TLFB) approach: Continued development and psychometric evaluation with psychiatry patients. International Journal of STD & AIDS. 2001;12:356–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiellin DA, Reid MC, O’Connor PG. Screening for alcohol problems in primary care. A systematic review. Archives of Internal Medicine. 2000;60:1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Folsam DP, Hawthorne W, Lindamer L, Gilmer T, Bailey A, Golshan S, Jeste DV. Prevalence and risk factos for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. American Journal of Psychiaatry. 2005;162:370–376. doi: 10.1176/appi.ajp.162.2.370. [DOI] [PubMed] [Google Scholar]
- Frank D, DeBenedetti AF, Volk RJ, Williams EC, Kivlahan DR, Bradley KA. Effectiveness of the AUDIT-C as a Screening Test for Alcohol Misuse in Three Race/Ethnic Groups. Society for General Internal Medicine. 2003;23:781–787. doi: 10.1007/s11606-008-0594-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gessler LJ, Bormann CA, Kwiatkowski CF, Braucht G, Reichardt C. Women, homelessness, and substance abuse. Psychology of Women Quarterly. 1995;19:65–83. [Google Scholar]
- Gonzalez G, Rosencheck RA. Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services. 2002;53 doi: 10.1176/appi.ps.53.4.437. 737-446. [DOI] [PubMed] [Google Scholar]
- Gordon AJ, Maisto SA, McNeil M, Kraemer K, Conigliaro RL, Kelley ME, Conigliaro J. Three questions can detect hazardous drinkers. Journal of Family Practice. 2001;50:313–320. [PubMed] [Google Scholar]
- Green C. Gender and use of substance abuse treatment services. Alcohol Research and Health. 2006;29:55–62. [PMC free article] [PubMed] [Google Scholar]
- Gregorie TK. Subtypes of alcohol involvement and their relationship to exits from homelessness. Substance Use and Misuse. 1996;31:1333–1357. doi: 10.3109/10826089609063980. [DOI] [PubMed] [Google Scholar]
- Health Care for the Homeless Program. Fact Sheet. 2011 Accessed from http://www.nhchc.org/wp-content/uploads/2011/09/HCHFactSheetMay2011.pdf 12/12/13.
- Hung DY, Rundall TG, Tallia AF, Cohen DJ, Halpin HA, Crabtree BF. Rethinking prevention in primary care: Applying the chronic care model to address health risk behaviors. The Millbank Quarterly. 2007;85:69–91. doi: 10.1111/j.1468-0009.2007.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner E, Bland M, Cassidy P, Coulton S, Deluca P, Drummond C, Gilvarry E, Shenker D. Screening and brief interventions for hazardous and harmful alcohol use in primary care: A cluster randomized controlled trial protocol. BMC Public Health. 2009;9:287. doi: 10.1186/1471-2458-9-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Larson MJ, Cheng DM, Tucker JA, Winter M, Mullins A, Saitz R, Samet JH. Need and non-need factors associated with addiction treatment utilization in a cohort of homeless and housed urban poor. Medical Care. 2006;44:225–233. doi: 10.1097/01.mlr.0000199649.19464.8f. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCorry F, Garnick D, Bartlet J, Cotter F, Chalk M. Developing performance measures for alcohol and other drug services in managed care plans. Joint Commission on Quality Improvement. 2000;26:633–643. doi: 10.1016/s1070-3241(00)26054-9. [DOI] [PubMed] [Google Scholar]
- National Research Council. Women”s Health Research: Progress, Pitfall, and Promise. Washington, DC: The National Academies Press; 2010. [Google Scholar]
- National Women’s Resource Center for the Prevention and Treatment of Alcohol, Tobacco and Other Drug Abuse and Mental Illness. Gender specific substance abuse treatment. Washington DC: 1997. CSAP Contract No. 277-94-3009. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much: A Clinician’s Guide. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, US Department of Health and Human Services; 2005. [Accessed January 6, 2011]. Available at: http://pubs.niaaa.nih.gov/publications/practioners/cliniciansguide2005/guide.pdf. [Google Scholar]
- New Hampshire-Dartmouth Psychiatric Research Center. Residential Follow-Back Calendar. Lebanon, NH: Dartmouth Medical School; 1995. [Google Scholar]
- Nyamathi A, Longshore D, Galaif ER, Leake B. Motivation to stop substance use and psychological and environmental characteristics of homeless women. Addictive Behavior. 2004;29:1839–1843. doi: 10.1016/j.addbeh.2004.03.032. [DOI] [PubMed] [Google Scholar]
- Reardon ML, Burns AB, Preist R, Sachs-Ericsson N, Lang AR. Alcohol use and other psychiatric disorders in the formerly homeless and never homeless: Prevalence, age of onset, comorbidity, temporal sequencing, and service utilization. Substance Use and Misuse. 2003;38:601–644. doi: 10.1081/ja-120017387. [DOI] [PubMed] [Google Scholar]
- Roberston JM, Zlotnick C, Westerfelt A. Drug use disorders and treatment contact among homeless adults in Alameda County, California. American Journal of Public Health. 1997;87:221–228. doi: 10.2105/ajph.87.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks JA, Drake RE, Williams VF, Banks SM, Herrell JM. Utility of the Time-Line Follow-Back to assess substance use among homeless adults. Journal of Nervous and Mental Disease. 2003;191:145–153. doi: 10.1097/01.NMD.0000054930.03048.64. [DOI] [PubMed] [Google Scholar]
- Saitz R, Cheng DM, Winter M, Kim TW, Meli SM, Allensworth-Davies D, Lloyd-Travaglini CA, Samet JH. Chronic care management for dependent alcohol and other drugs: The AHEAD randomized trial. Journal of the American Medical Association. 2013;310:1156–1167. doi: 10.1001/jama.2013.277609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Larson MJ, Horton NJ, Winter M, Samet JH. Linkage with primary medical care in a prospective cohort of adults with addictions in inpatient detoxification: Room for improvement. Health Services Research. 2004;39:587–606. doi: 10.1111/j.1475-6773.2004.00246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Larson MJ, LaBelle C, Richardson J, Samet JH. The cae for chronic disease management for addiction. Journal of Addiction Medicine. 2008;2:55–64. doi: 10.1097/ADM.0b013e318166af74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Section 330 (h) of the Public Health Service Act (42 USCS § 254b) [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: A technique for assessing self-report alcohol consumption. In: Litten R, Allen J, editors. Measuring alcohol consumption. Totowa, NJ: The Humana Press; 1992. [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: Ranking its healthimpact and cost effectiveness. American Journal of Preventive Medicine. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- Sosin MR, Bruni M. Homelessness and vulnerability among adults with and without alcohol problems. Substance Use and Misuse. 32:939–968. doi: 10.3109/10826089709055865. [DOI] [PubMed] [Google Scholar]
- StataCorp. College Station, TX. 2011 www.stata.com.
- Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: A prospective analysis. Journal of Health Care for the Poor and Underserved. 11:212–230. doi: 10.1353/hpu.2010.0675. [DOI] [PubMed] [Google Scholar]
- Stata 12,1. College Station Tx: [Google Scholar]
- Torchalla I, Strehlau V, Li K, Krausz M. Substance use and predictors of substance dependence in homeless women. Drug and Alcohol Dependence. 2011;118:173–179. doi: 10.1016/j.drugalcdep.2011.03.016. [DOI] [PubMed] [Google Scholar]
- Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefanic A. Measuring homelessness and residential stability: The Residential Time-Line Follow-Back Inventory. Journal of Community Psychology. 2007;35:29–42. [Google Scholar]
- Upshur C, Weinreb L. A survey of primary care provider (PCP) attitudes and behaviors treating adult depression: What changes after a collaborative care intervention? The Primary Care Companion to the Journal of Clinical Psychiatry. 2008;10:182–186. doi: 10.4088/pcc.v10n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upshur CC, Weinreb L, Bharel M. Homeless women and hazardous drinking: Screening results in a primary health care setting. The American Journal on Addictions. 2013 doi: 10.1111/j.1521-0391.2013.12072.x. prepublication online. [DOI] [PubMed] [Google Scholar]
- Upshur CC, Weinreb L, Cheng DM, Kim TW, Samet JH, Saitz R. Does experiencing homelessness affect women’s motivation to change alcohol or drug use? The American Journal on Addictions. 2014;23:76–83. doi: 10.1111/j.1521-0391.2013.12066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Millbank Quarterly. 74:511–544. [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Dewey JE, Gandek B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8™ Health Survey. Lincoln, RI: Quality Metric Inc; 2001. [Google Scholar]
- Watkins K, Pincus HA, Taniellian TL, Lloyd J. Using the chronic care model to improve treatment of alcohol use disorders in primary care settings. Journal of Studies on Alcohol. 2003;64:209–218. doi: 10.15288/jsa.2003.64.209. [DOI] [PubMed] [Google Scholar]
- Weinreb L, Rog D, Henderson K. Exiting shelter: An epidemiological analysis of barriers and facilitators for families. Social Services Review. 2010;84:597–614. doi: 10.1086/657108. [DOI] [PubMed] [Google Scholar]
- Weisner CM, Schmidt LA. The Community Epidemiological Laboratory: Studying alcohol problems in community and agency-based populations. Addiction. 1995;90:329–342. doi: 10.1046/j.1360-0443.1995.9033293.x. [DOI] [PubMed] [Google Scholar]
- Wen CK, Judak OL, Hwang SW. Homeless people’s perceptions of welcomeness and unwelcomeness in healthcare encounters. Journal of General Internal Medicine. 2007;22:1011–1017. doi: 10.1007/s11606-007-0183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel SL, Burnam MA, Koegel P, Morton SC, Miu A, Jinnett KJ, Sullivan JG. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Medical Care. 2001;39:1158–1169. doi: 10.1097/00005650-200111000-00003. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Tucker JS, Elliot MM, Hambarsoomians K, Perlman J, Becker K, Kollross C, Golinelli D. Prevalence anc co-occurrence of violence, substance use and disorders, and HIV risk behavior: A comparison of sheltered and low income women in Los Angeles County. Preventive Medicine. 2004;39:617–634. doi: 10.1016/j.ypmed.2004.02.027. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Green HD, Tucker JS, Golinelli D, Kennedy DP, Ryan G, Zhou A. The social context of homeless women’s alcohol and drug use. Drug and Alcohol Dependence. 2009;105:16–23. doi: 10.1016/j.drugalcdep.2009.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willenbring M. Frontlines: Linking Alcohol Services Research & Practice. Washington, DC: National Institution on Alcohol Abuse and Alcoholism, U.S. Department of Health and Human Services; 2007. Overcoming barriers: The need for full treatment integration. [Google Scholar]
- Zerger S. A Review of the Literature. Nashville TN: National Health Care for the Homeless Council; 2002. Substance Abuse Treatment: What Works for Homeless People? [Google Scholar]
- Zlotnick C, Tam T, Robertson M. Disaffiliation, substance abuse, and exiting homelessness. Substance Use and Misuse. 2003;38:577–599. doi: 10.1081/ja-120017386. [DOI] [PubMed] [Google Scholar]