Abstract
Obstructive sleep apnea (OSA) is a common disorder associated with cardiovascular disease (CVD). One theory to explain this relationship proposes that OSA can induce systemic inflammation, thereby inducing CVD. This theory is based on the premise that obesity is a pro-inflammatory state, and that physiological derangements during sleep in subjects with OSA further aggravate inflammation. In support of this theory, some clinical studies have shown elevated inflammatory biomarkers in OSA subjects, or improvement in these markers following treatment of OSA. However, the data are inconsistent and often confounded by the effects of comorbid obesity. Animal models of OSA have been developed, which involve exposure of rodents or cells to intermittent hypoxia, a hallmark feature of OSA. Several of these experiments demonstrate that intermittent hypoxia can stimulate inflammatory pathways and lead to cardiovascular or metabolic pathology. In this review, we review relationships between OSA and inflammation, with particular attention to studies published within the last year.
Keywords: Sleep apnea, inflammation, hypoxia, metabolism
Sleep Apnea: Introduction
Obstructive sleep apnea (OSA) describes irregular breathing during sleep due to intermittent partial or complete collapse of the upper airway[1]. The prevalence of OSA in adults is 24% in men and 9% in women and increases dramatically with obesity [2]. Risk factors for OSA also include male gender, older age, and higher neck circumference[3]. The severity of OSA is usually described using the apnea hypopnea index (AHI). The AHI measures the frequency with which breathing ceases for at least 10 seconds (apnea), or decreases enough to cause hemoglobin oxygen desaturation of >3%, or an arousal from sleep (hypopnea)[4]. During an apnea or hypopnea, the sleeping subject experiences intermittent hypoxia and may also develop hypercapnia. Ineffectual efforts to breathe against the obstructed upper airway can also lead to significant autonomic activation[5] and changes in intrathoracic pressure[6]. OSA can sometimes be mitigated or completely abolished by lifestyle changes such as weight loss[7, 8]. In most cases, however, other therapies are required to improve upper airway patency. Continuous positive airway pressure (CPAP) applied to the nose and/or mouth is the most common form of treatment, and serves to splint the airway open with pressurized air. While highly efficacious, its effectiveness is limited by difficulty with adherence[9, 10]. Mandibular advancement devices, designed to lift soft tissues from the site of airway collapse, can be effective in some cases of OSA[11]. Surgery may be used to address anatomical problems (e.g., enlarged tonsils), or used as a salvage treatment for patients who are not able to use CPAP[12]. Newer treatment modalities for OSA, such as upper airway nerve stimulation are in development[13].
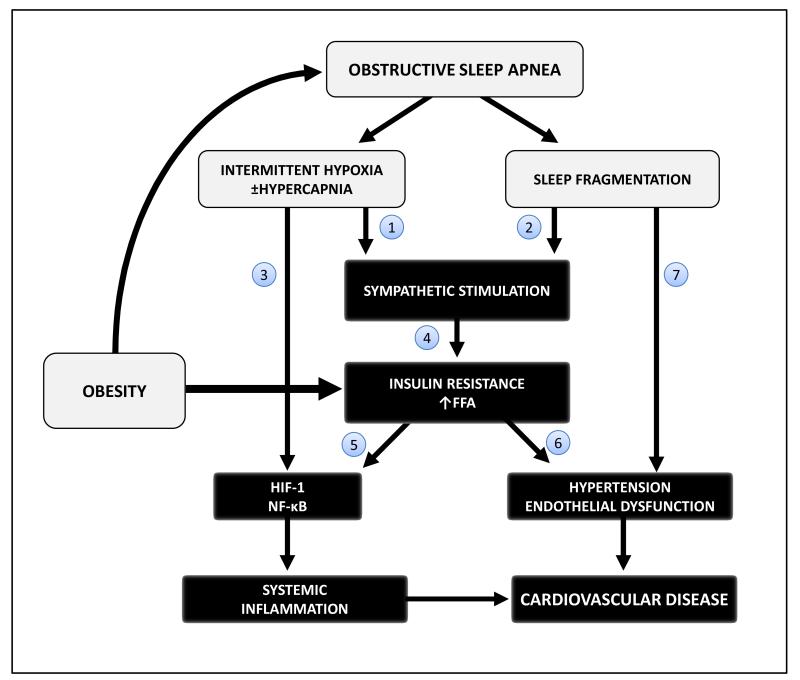
OSA was first documented as a disorder in the 1960’s, and its health impacts have since received growing attention from the public and healthcare community. The constellation of sleep fragmentation, intermittent hypoxia, hypercapnia, and ineffectual breathing efforts are believed to account for the majority of physiological derangements in OSA[14]. The prototypical symptom of OSA is excessive daytime sleepiness. Sleepiness from OSA decreases quality of life and increases hazards from activities such as driving [15]. OSA is also associated with cardiovascular disease (CVD) and chronic risk factors for CVD such as hypertension[16-18], insulin resistance[19, 20], atherosclerosis, and hyperlipidemia[21]. The Sleep Heart Health Study[22] and Wisconsin Sleep Cohort Study[23] showed an independent association between OSA and mortality. A higher incidence of CVD and cerebrovascular disease [24-26] is found in patients with OSA. Observational studies demonstrate a reduction in death and cardiovascular outcomes with CPAP use [27] [28]. However, the relationship between OSA and CVD is complex. The underlying obesity that predisposes to both OSA and CVD may account for at least some of the increased risks of CVD. In addition, OSA may itself confer risks for development of CVD. Some of the proposed pathways linking OSA to CVD include SNS activation, metabolic dysfunction, and inflammation (figure 1). In this review we will highlight studies examining the relationship between OSA and inflammation, with a focus on publications from the last year. For more comprehensive information, we refer to the reader to previous relevant reviews [29-33].
FIGURE 1.
Proposed pathways by which OSA interacts with obesity to induce inflammation and metabolic dysfunction. OSA interferes with (1) gas exchange and (2) sleep continuity. These stimuli collectively increase sympathetic nervous system outflow, which is well known to result in insulin resistance and lipolysis. In vitro data suggest that (3) IH can directly stimulate inflammation in tissues, perhaps via HIF-1 or NFκB activation. (4) Sympathetic stimulation of lipolysis with resultant increase in FFA and increased insulin also (5) stimulate the HIF-1 pathway, and (6) contribute to hypertension and endothelial function. Obesity independently contributes to OSA and to metabolic dysfunction, such that the combination of OSA and obesity may synergistically promote CVD. References supporting each of these phenomena appear below.
1: Somers et al. Sleep 1993; Somers et al. JAP 1985 [137, 138]
2. Stamatakis et al. Chest 2010; Somers et al. JCI 1995 [5, 139]
3: Ryan et al AJRCCM 2006; Ryan et al. Circulation 2005 [62, 115]
4: Barcelo et al. Eur Resp J 2011; Jun et al. Sleep 2012; Diebert et al. JCI 1980 [112, 116, 140]
5: He et al. AJP Endocrinol Metab 2011; Lee et al. Cell 2014; Halberg et al. Mol Cell Biol 2009 [108, 109, 141]
6: Chinen et al. Endocrinology 2007; Imrie et al. Biochem Biophys Acta 2010 [142, 143]
7: Couchou et al. Eur Heart J; Gottlieb et al. NEJM 2014[144] [47]
It is widely accepted that protracted vascular inflammation is responsible for the initiation and progression of atherosclerotic CVD, the leading cause of death in the Western world [34]. During initial stages of disease, vascular endothelium is injured by a variety of stressors such as reactive oxygen species (ROS), shear blood pressure forces, or circulating cholesterol or fatty acids. Endothelial injury stimulates the expression of leukocyte adhesion molecules (e.g. L- selectin, integrins) and endothelial adhesion molecules (E-selectin, P-selectin, ICAM-1, VECAM-1). Leukocytes migrate into the artery wall, through signaling by substances such as oxidized LDL-cholesterol, MCP-1 (monocyte chemoattractant protein-1), and IL-8. Small fatty streaks progress to complex atheroma via accumulation of macrophages and monocytes. Given the close relation between vascular inflammation and atherosclerosis, circulating biomarkers have been examined for their ability to predict CVD. C-reactive protein (CRP) is rapidly produced in the liver in response to macrophage release of IL-6, whereupon circulating CRP binds with bacterial polysaccharides to activate the complement cascade. Normal CRP levels are < 10 mg/L and elevations in the absence of infection may promote cancer, diabetes, and CVD [27]. In unstable angina, CRP [35] and IL-6 [36] levels predict poorer prognosis, perhaps reflecting more aggressive vascular inflammation. CRP has been shown to identify those at risk for coronary artery disease [37] [38]. High-sensitivity CRP (hsCRP) assays have better performance at relatively low levels of CRP and have also been widely used in a number of epidemiological risk studies. For example, the Physician’s Health Studydemonstrated that elevated hsCRP levels identified apparently healthy men with higher risk of developing future stroke and atherosclerotic CVD [39]. While CRP elevations carry prognostic significance, it is debated whether CRP itself is a mediator of CVD[40].
Besides CRP, several other inflammatory markers have been utilized for risk stratification in primary or secondary CVD. Cytokines, which refer to signaling proteins chiefly secreted by leukocytes, also reflect activation of the immune system. Cytokines include Tumor Necrosis Factor-α (TNF-α) which is secreted from monocytes; interleukins (IL) and interferon (IFN) gamma, which are from activated leukocytes. Fibrinogen, whose synthesis increases in the liver in response to cytokines (particularly IL-6 [41]), has been shown to correlate with risks of stroke and myocardial infarction [42]. Nuclear Factor- κ β (NF-κB) is a transcription factor that regulates the immune response to infection. Known agonists of NF-κB include ROS, lipopolysaccharide, and TNF-α. Excessive activation of NF-κB can induce pathological consequences such as CVD and cancer. In turn, NF-κB potentiates the inflammatory cascade by upregulating cytokines such as TNF-α, IL-6, and IL-8. It has been challenging to determine whether OSA, obesity, or perhaps a synergistic interaction of the two states is responsible for inflammation or CVD. This inherent difficulty exists because OSA is very common in obese subjects, obesity itself is considered a pro-inflammatory state [43-46].
OSA and Inflammation – Recent Clinical Findings
Within the last year, several clinical studies have been published on the subject of OSA and inflammation, most utilizing common biomarkers such as CRP, IL-6, or TNF-α. Gottlieb et al compared the effects of 12 weeks of CPAP, oxygen, or health counseling on blood pressure in a randomized controlled trial (RCT) enrolling moderate-severe OSA [47]. They found that only CPAP effectively decreased blood pressure and lowered CRP by 20%, while oxygen or health counseling had no effect on these parameters. In the same issue of the New England Journal of Medicine, 24 weeks of medical weight loss, CPAP, or combined therapies were compared, with respect to their impact on plasma hsCRP level. CPAP alone had no effect on hsCRP, while weight loss had the anticipated CRP lowering effect [48]. Inflammatory markers were also assessed as one of the outcomes of the Multi-Center Obstructive Sleep Apnea Interventional Cardiovascular (MOSAIC) trial. MOSAIC was an RCT completed in 2012 (n=391) comparing the impact of 6 months of CPAP or usual care on sleepiness and cardiovascular risk. The primary outcome of MOSAIC was that CPAP significantly improved daytime sleepiness, but did not improve the cardiovascular risk score [49]. In a subset of MOSAIC patients (n=253), CPAP improved vascular endothelial function[50]. However, in terms of inflammatory markers, no consistent changes were observed in plasma IL-6, IL-10, CRP or TNF-α, regardless of CPAP adherence [51]. IL-6 and TNF-α levels were examined in a study of 33 OSA patients and 24 non-apneic, Body Mass Index (BMI)-matched controls as well as the impact of 3 months of CPAP therapy. At baseline, no differences in IL-6 or TNF-α were observed, nor any changes in the mean level of these cytokines with CPAP therapy [52]. Kritikou et al examined 24-hour profiles of IL-6, TNF-α receptor-1, leptin, adiponectin, hsCRP, glucose, and insulin in 77 middle-aged subjects. Men with OSA exhibited increased hsCRP, IL-6, insulin resistance, and leptin; and females had higher hsCRP than their non-apneic counterparts. However, CPAP use for 2 months had no effect on any of these outcomes [53]. Hence, most recent clinical studies have not demonstrated a change in inflammatory markers with OSA treatment.
The mixed findings above mirror a history of conflicting data concerning OSA and inflammation. For example, McNicholas et al has reviewed the inconsistent literature on OSA and its effects on CRP level. Shamsuzzaman initially reported that OSA subjects exhibited higher CRP than BMI-matched matched controls [54]. However, these findings were questioned as BMI may not adequately capture the effects of visceral adiposity[55] which is more inflammatory, and particularly prevalent in OSA. Yokoe et al showed that CPAP therapy reduced CRP and IL-6 [56]. On the other hand, four weeks of CPAP had no measureable impact on hsCRP, IL-6, or IFN-gamma in men with moderate-severe OSA [57]. Inflammatory associations with OSA were found to be governed by obesity in several other cross-sectional studies [58-60]. Adding to these complexities, one study found that mild OSA was associated with both inflammatory and anti-inflammatory cytokine profiles [61]. OSA patients exhibit increased transcription factor NF-κ β, TNF-α, and IL-8 in a manner that correlates with the extent of hypoxia during sleep [62]. Pediatric studies in OSA have showed synergistic effects of obesity and OSA on CRP [63] as well as improvements in CRP after resolution of OSA [64]. Potentially, there are patient-specific or OSA-specific factors that predispose to inflammation and the subset of individuals susceptible to inflammation in the setting of OSA has yet to be determined.
OSA and Inflammation – Novel Biomarkers
Recent publications have utilized novel biomarkers to screen for inflammation in OSA patients. In a study of 80 OSA patients and 40 BMI/age-matched controls, those with OSA exhibited higher levels of plasma hsCRP, IL-6, and TNF-α in association with increased carotid intima-media thickness, an early sign of atherosclerosis [65]. A novel biomarker, pentraxin-3 was also elevated in the OSA group. Pentraxin 3 is produced in neutrophils, macrophages, smooth muscle and endothelial cells in response to IL-1 or TNF-α signaling. It has been identified as an initiator of the complement cascade [66] and a surrogate of endothelial dysfunction [67]. A previous Japanese study reported morning pentraxin-3 levels were elevated in OSA and reduced by CPAP, a pattern not observed for hsCRP[68].
Nesfatin-1 is a molecule initially discovered for its role in central hypothalamic appetite suppression [69]. It was subsequently detected in adipocytes and up-regulated by fat ingestion [70], extending its role as an adipokine. Intriguing and diverse functions of Nesfatin-1 continue to emerge. Nesfatin-1 is present in chrondrocytes, where it augments the release of inflammatory mediators (including IL-8, IL-6, and MIP-1a) induced by IL-1. In patients with COPD, Nesfatin-1 positively correlated with serum IL-6, IL-8 and TNF-α [71], although levels of Nesfatin-1 did not change after treatment with inhaled corticosteroids. Paradoxically, Nesfatin-1 decreased inflammation in rats subjected to traumatic brain injury [72]. Thus, myriad roles of Nesfatin-1 and its implications are still being investigated. Shen et al recently examined nesfatin-1 levels in OSA patients and found them to be moderately reduced in comparison to weight-matched controls without [73].
Fibrinogen is another biomarker that has been shown to predict CVD (Cerebrovascular Diseases) in a meta-analysis [74] [75], reflecting its role in inflammation and/or hypercoagulability. Last year, Shamsuzzaman et al examined fibrinogen levels in 36 men with OSA and 18 controls without OSA. Fibrinogen was increased in those with severe OSA compared to those with milder OSA or controls [76]. The fibrinogen level was related to the AHI, arousal index, and degree of hypoxemia. To date, the association between OSA and fibrinogen has been unclear. Basoglu et al [77] found that obese subjects with OSA had higher fibrinogen levels, as well as features of metabolic syndrome and CRP, than obese subjects without OSA. Fibrinogen and whole blood viscosity increased overnight in patients with OSA, and this phenomenon was prevented with a single night of CPAP [78]. On the other hand, several studies show less straightforward results. Morning fibrinogen was not increased in a study of children with OSA compared to those without OSA[79]. Two months of CPAP did not alter nocturnal profiles of fibrinogen [80] but interestingly decreased other clotting factors. Yet another study found no acute effect of CPAP on whole blood coagulability, but did show a chronic effect [81]. A recent study from Poland examined inflammatory markers following 6 months of mandibular advancement therapy for OSA. Authors showed an improvement in the AHI (24 to 7.05), in association with a reduction in IL-1β, D-dimer, and clotting factors [82].
YKL-40 (also referred to as human cartilage glycoprotein) is novel marker of inflammation recently examined in OSA. YKL-40 is secreted by chrondrocytes, lymphocytes, and vascular smooth muscle. It has been shown to increase in the setting of acute myocardial infarction [83], diabetes [84], rheumatoid arthritis [85], and in the serum and airways of COPD [86]. TKL-40 was increased in Chinese OSA patients compared to healthy controls [87]. The OSA group had increased blood pressure, HbA1c, lower HDL, higher LDL-C, and markedly higher YKL-40 levels. Multiple logistic regression showed that that YKL-40 strongly predicted the presence of, more so than increments of HbA1c or blood pressure. Regression analysis also showed a significant relationship between YKL-40 and AHI. Unexpectedly, the regression analysis did not identify age, male gender, smoking status, or BMI as predictors of OSA which may limit the generalizability of their findings. Another study in Chinese patients with OSA also showed increased YKL-40 levels [88] and also noted correlations between YKL-40 and BMI, HOMA-IR, CRP, and AHI.
G protein coupled receptor (GPR) 120 is a long-chain free fatty acid (FFA) receptor abundantly expressed in the intestinal tract. GPR 120 regulates the secretion of digestive hormones such as glucagon-like peptide-1. GPR 120 is also present in macrophages where it mediates ant-inflammatory effects and may protect against metabolic syndrome [89, 90]. The presence of GPR 120 on leukocytes allows for its detection in the circulation. Gozal et al examined the independent effects of obesity and OSA on monocyte GPR 120 expression, plasma GPR 120 levels, insulin resistance, lipids, and hsCRP in 226 children [91]. As expected, obesity was independently associated with a higher lipid profile, insulin resistance, and hsCRP; OSA also independently increased LDL-C and lowered HDL-C. In terms of GPR 120, there was a synergistic lowering of GPR 120 by a combination of obesity and OSA. Furthermore, GPR 120 correlated significantly with severity of OSA (AHI, SpO2 nadir, and respiratory arousal index) and strongly with insulin resistance. These findings could implicate GPR 120 as a common risk factor for metabolic syndrome and OSA, or a direct interaction between OSA and GPR 120.
Platelets are a potential source of inflammation, since they contain the enzyme cyclooxygenase (COX) which can be stimulated to synthesize prostanoids, such as pro-inflammatory thomoboxane A2 [92]. Aspirin is believed to confer vascular benefits by inhibiting platelet prostanoid release. Gauiter-Veyret et al performed studies examining the role of COX pathways in OSA. They exposed apolipoprotein E-deficient mice (a model of severe hyperlipidemia, used to show acceleration of atherosclerosis during intermittent hypoxia [93]) to 8 weeks of intermittent hypoxia (IH). IH increased atherosclerotic plaques in association with increased COX-1 and thromboxane synthesis expression, while pharmacologic blockade of COX-1 attenuated the effects of IH [94]. However, urine 11-dehydroxythromboxane (a metabolite of thromboxane A2) was not increased in patients with OSA unless they also had underlying cardiovascular risk factors; and CPAP did not affect 11-dehydroxythromboxane levels. COX-1 and COX-2 have also been examined as mediators of OSA-induced hypertension. Exposure of humans to acute IH increased arterial blood pressure ~3 mmHg, but did not significantly alter signs of COX activity. Pre-treatment with a COX-2 specific inhibitor attenuated the blood pressure increase [95].
The platelet-lymphocyte ratio (PLR) is new index being investigated for risk assessment for acute coronary syndromes [96]. The PLR is a metric that to combines the inflammatory potential of platelets, with decreased lymphocytes – a stress response that may reflect actions of cortisol[97, 98]. As platelets and lymphocytes are routinely ordered tests, the PLR is attractive for its incorporation into clinical decision making. In a recent study of 424 patients ranging from those with normal breathing to severe OSA, authors noted a dose-effect of AHI and severity of hypoxia with the PLR [99], and the prevalence of CVD increased with each quartile of the PLR.
Vitamin D is a nutrient best known for its role in calcium metabolism. Recently, vitamin D deficiency has also been proposed as a risk factor for CVD. Some of the protective roles of vitamin D have been ascribed to mechanisms including stimulation of endothelial nitric oxide production; and suppression of ROS generation, COX-1 expression, vascular adhesion molecules, and vascular smooth muscle proliferation [100]. Kheinrandish-Gozal et al compared the independent effects of obesity and OSA on plasma 25-hydroxyvitamin D, inflammatory markers, and insulin resistance in 176 children [101]. OSA was independently associated with higher hsCRP and lipids, and lower vitamin D; correlations were found between the vitamin D level and hsCRP, BMI, and insulin resistance. Multiple logistic regression identified a strong effect of African American race on lower vitamin D levels, and showed AHI and SpO2 nadir to correlate with lower vitamin D. The relation between vitamin D and OSA is complex, since low vitamin D levels are influenced by diet and ethnicity which in turn influence propensity to OSA.
In summary, clinical associations between OSA and inflammation remain ambiguous, with some studies showing elevated inflammatory markers and/or reductions of these markers after OSA treatment. However, several other studies found no association between OSA and inflammation, associations driven by overlapping effects of obesity, or lack of an anti-inflammatory effect of CPAP. Complex interactions of obesity, demographics, severity of OSA, and the homeostasis between pro/anti-inflammatory pathways may underlie these inconsistent results.
OSA and Inflammation: Animal/Cell Studies
In an effort to study the consequences of OSA in a more mechanistic fashion, animal models of OSA have been developed. Many of these models expose rodents or cells to IH simulating this aspect of OSA[30, 102] [103]. The metabolic and inflammatory consequences of IH have been reviewed in detail [30, 102] and we will focus on recent IH experiments. It should be emphasized that IH does not fully recapitulate all the effects of OSA (for example, changes in intrathoracic pressure, hypercapnia, or sleep loss). Furthermore, the hypoxia induced by such models may not reflect the actual burden of hypoxia present in human OSA[14] – a problem that has been recently recognized and addressed in some animal models of IH[104]. Nevertheless, the data generated from these IH studies may be useful in understanding effects of tissue hypoxia per se on metabolism.
Adipose tissue can become a source of inflammation in metabolic disorders, especially in the setting of hypoxia [105, 106]. To examine the role of adipose inflammation in IH-induced metabolic dysfunction, He et al exposed rats to chronic IH (8 weeks, 8 hours/day, 30 desaturations/hour). Glucose and insulin levels increased as a function of IH severity. They also exposed 3T3-L1 adipocytes cells to graded IH (6 hours a day, 8 days) and noted dose-dependent increases in HIF-1 (hypoxia inducible factor, a master regulator of cellular hypoxic responses) and Glut-1 mRNA. (Elsewhere, adipose HIF-1 has also been shown to increase in vivo with chronic IH exposure[107].) In both rat plasma and in 3T3-L1 cell extracts, TNF-α, IL-6 and leptin increased. Authors implicated NF-kB in cytokine changes and suggested that the in vitro inflammation they observed mediated the insulin resistance they observed in vivo. Recent landmark studies have demonstrated that adipose tissue HIF-1 can be potently increased by insulin [108] and acute fat ingestion, without extracellular hypoxia [109]. It is therefore possible for the inflammatory effects of HIF-1 activation in adipose tissue to arise secondary to insulin resistance or increased FFA in obesity or OSA. Other pathways for metabolic dysfunction during IH, independent of adipose inflammation, have also been recently demonstrated: Shin et al showed that glucose intolerance following chronic IH in mice was abolished by adrenal medullectomy [110] demonstrating the central role the sympathetic nervous system in altered glucose metabolism. Acutely, changes in glucose metabolism induced by IH can also be inhibited by pharmacologic blockade of alpha-adrenergic signaling[104].
The contribution of white adipose tissue to atherosclerosis during IH exposure was recently examined by Poulain and colleagues [111]. They exposed apolipoprotein E-deficient mice to chronic IH and reported atrophic epididymal adipose tissue with increased infiltration of macrophages. Following chronic IH, mice also developed high circulating free fatty acids (FFA), dyslipidemia and insulin resistance. Adipocytes exhibited increased IL-6 and TNF-α secretion when incubated with the lipolytic agonist isoprenaline. Surgical lipectomy of mice before exposure to chronic IH attenuated aortic atherosclerosis and hyperlipidemia. Jun et al have shown that subjects with OSA exhibit increased FFA levels during sleep [112] which might represent a human correlate of these findings. Drager et al showed that IH suppresses lipid uptake in adipose tissues in association with up-regulated angiopoetin-like protein 4 (Angptl4) levels. Angptl4 is an inhibitor of lipoprotein lipase, which is responsible for hydrolyzing lipid droplets, facilitating transfer of triglyceride and FFA from the circulation into cells. Following chronic IH, apolipoprotein E-deficient mice developed elevated lipid levels and accelerated plaque formation, but not if treated with an Angptl4 neutralizing antibody[107].
It has been suggested that the IH of OSA is more inflammatory than stable hypoxia, since cycles of hypoxia and reoxygenation bear a resemblance to ischemia-reperfusion injury which is well known to promote significant oxidative stress [31, 113, 114]. IH-induced inflammation in adipose tissues was examined in vitro by Taylor et al, who exposed primary human subcutaneous and visceral adipocytes to acute IH. IH elicited increases in NF-kB binding activity, and this activity was exponentially increased by concurrent stimulation with TNF-α. Release of IL-8, IL-6, and TNF-α was also detected in the cellular supernatant, and PCR array revealed several pro-inflammatory changes at the transcription level. By contrast, effects of IH in pulmonary endothelium and small airway epithelium were negligible. These results build upon work from the same laboratory where IH up-regulated NF-κB activity in HeLa (cervical cancer) cells [115]. The synergistic impact of IH and TNF-α at the level of adipocytes offers an interesting perspective into the interactions of OSA and obesity [116]. Collectively, these studies suggest that IH alters adipose tissue metabolism to facilitate atherosclerosis. IH may directly induce inflammation, impair the clearance of lipids from the circulation, or stimulate excessive lipolysis which promotes hyperlipidemia[117], insulin resistance and inflammation[118].
The vasculature is another alleged site of IH/OSA-induced inflammation, and several studies in the last year have addressed this phenomenon. Zhou et al showed that after chronic IH, mice exhibited increased vascular oxidative stress, inflammation and apoptosis [119]. These effects were amplified in mice lacking metallothionein, a Golgi complex molecule with anti-oxidant functions[120]. A high fat diet was also shown to amplify the endothelial dysfunction caused by chronic IH [121]. Anti-inflammatory or antioxidants have also been examined as therapies for chronic IH. Rats exposed to IH over 3 weeks developed systemic hypertension and increased markers of aortic inflammation and oxidative stress. Remarkably, the hypertension and inflammation was almost completely abolished by melatonin, and authors ascribed these findings to the possible hypoxic suppression of pineal melatonin synthesis [122] and to the anti-oxidant properties of melatonin [123]. Totoson et al examined whether cardiovascular effects of IH could be prevented by treatment with a statin, since these drugs are known to have anti-inflammatory effects. Atorvastatin attenuated increases in blood pressure, vascular elastance, carotid intima-media thickness, cardiac oxidative stress following IH exposure [124].
In the brain, IH is thought to elicit inflammation, contributing to cognitive and behavioral consequences of OSA. A recent study exposed rats to two weeks of IH and examined expression of inflammatory genes (iNOS, TNF-α, IL-1b, COX-2, IL-6) in the microglia of the cortex, medulla, and spinal cord at several time points[125]. Dynamic changes in transcription occurred, with most inflammatory markers increasing over time. Of particular interest, toll-like receptor 4 (TLR4) increased in the cortex and brainstem after chronic IH. TLR4 triggers an inflammatory cascade upon binding to lipopolysaccharide released from gram negative bacteria. In the brain, TLR4 has been implicated in several inflammatory and neurodegenerative disorders [126]. It is not clear how TLR4 is stimulated in the brain, but authors suggest a process of “sterile inflammation” citing endogenous ligands released during IH injury [127].
OSA has been proposed as an aggravator of asthma [128]. For example, treatment of OSA reduced asthma medication use in children [129]. To explore this relationship further, Broytman et al exposed rats to IH for 30 days while inducing airway inflammation using an a weekly ovalbumin challenge (an established rodent model of inducing airway hyper-responsiveness). Compared to control rats, IH-exposed animals developed reduced forced expiratory flows and increased forced vital capacity and total lung capacity, and increased airway collagen. However, no synergistic interaction of IH with ovalbumin exposure was observed, apart from a modest increase in airway monocytes. This study intriguingly suggests that IH remodels the lungs, a finding which has also been shown in another study[130]. In vitro, IH exposure of airway epithelial cell (AEC) and bronchial smooth muscle cell (BSMC) increased the expression of cytokines, growth factors, and matrix metalloproteinases (MMP)[131]. 24 hours of IH increased expression of MMP-9, MMP-2, IL-8, and pro MMP-9 activation. IH also increased platelet-derived growth factor (PDGF) expression by AECs, and VEGF expression in BSMCs. Chemotaxis by neutrophils and BSMC were also found to be increased on exposure to IH.
It is well known that male gender and post-menopausal status in women are risk factors for OSA [132, 133]. In addition, the consequences of OSA may differ by gender. OSA was identified as a risk factor for coronary disease and heart failure in middle-aged men, but not in older men or in women of any age [134]; and a Spanish study showed an increased incidence of cancer in male OSA patients, but not in females [135]. To determine whether effects of IH are modified by sex hormones, female mice were exposed to IH for 30 days after undergoing an ovariectomy or a sham surgery[136]. Following chronic IH, mice with intact ovaries exhibited increased levels of IL-6 mRNA in the brain, and both IL-6 and IL-8 in the heart. Interestingly, the increase was prevented in ovariectomized animals.
Summary and Future Directions
OSA is a common disorder that has been linked to development of CVD and metabolic dysfunction. Several theories have been proposed to explain this relationship, but they remain unproven [14]. In figure 1, we present a framework for considering the relationship between OSA, obesity, inflammation, and CVD based on current available evidence. Whether OSA is itself a cause of CVD via inflammatory pathways seems plausible and convincing from basic science studies. However, clinical trials have not been nearly as convincing. Does this inconsistent literature reflect problems of accurately translating OSA into animal/cell studies, or does it reflect challenges inherent to the complexity of OSA and its closely associated risk factors?
Further research approaches are still needed to answer this paramount question.
Acknowledgments
Dr. Vsevolod Y. Polotsky is supported by the NIH R01 HL-080105 grant and ResMed Foundation grant 90048207. Dr. Jonathan Jun is supported by the NIH grants K08 HL-109475 and Diabetes Research and Training Pilot & Feasibility Grant 114525-JHU-UMD and by American Academy of Sleep Medicine Foundation Junior Faculty Award 106-JF-14.
Footnotes
CONFLICT OF INTEREST STATEMENT
Dr. Dileep Unnikrishnan has no conflicts of interests to declare.
REFERENCES CITED
- 1.Gastaut H, Tassinari CA, Duron B. Polygraphic study of the episodic diurnal and nocturnal (hypnic and respiratory) manifestations of the Pickwick syndrome. Brain Res. 1966;1(2):167–86. doi: 10.1016/0006-8993(66)90117-x. [DOI] [PubMed] [Google Scholar]
- 2.Young T, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N.Engl.J.Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.Peppard PE, et al. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–21. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 4.Berry RB, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi: 10.5664/jcsm.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Somers VK, et al. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96(4):1897–904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dempsey JA, et al. Pathophysiology of sleep apnea. Physiol Rev. 2010;90(1):47–112. doi: 10.1152/physrev.00043.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dempsey JA, Forster HV. Mediation of Ventilatory Adaptations. Physiol Rev. 1982;62(1):262–346. doi: 10.1152/physrev.1982.62.1.262. [DOI] [PubMed] [Google Scholar]
- 8.Smith PL, et al. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med. 1985;103(6 (Pt 1)):850–5. doi: 10.7326/0003-4819-103-6-850. [DOI] [PubMed] [Google Scholar]
- 9.Weaver TE. Adherence to positive airway pressure therapy. Curr Opin Pulm Med. 2006;12(6):409–13. doi: 10.1097/01.mcp.0000245715.97256.32. [DOI] [PubMed] [Google Scholar]
- 10.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng A, et al. Oral appliance therapy for obstructive sleep apnea. Treat Respir Med. 2005;4(6):409–22. doi: 10.2165/00151829-200504060-00005. [DOI] [PubMed] [Google Scholar]
- 12.Maurer JT. Surgical treatment of obstructive sleep apnea: standard and emerging techniques. Curr Opin Pulm Med. 2010;16(6):552–8. doi: 10.1097/MCP.0b013e32833ef7ea. [DOI] [PubMed] [Google Scholar]
- 13.Strollo PJ, Jr., et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139–49. doi: 10.1056/NEJMoa1308659. [DOI] [PubMed] [Google Scholar]
- 14.Mesarwi OA, et al. Metabolic dysfunction in obstructive sleep apnea: A critical examination of underlying mechanisms. Sleep and Biological Rhythms. 2014:n/a–n/a. doi: 10.1111/sbr.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cassel W, et al. Risk of traffic accidents in patients with sleep-disordered breathing: reduction with nasal CPAP. Eur Respir J. 1996;9(12):2606–11. doi: 10.1183/09031936.96.09122606. [DOI] [PubMed] [Google Scholar]
- 16.Montesi SB, et al. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8(5):587–96. doi: 10.5664/jcsm.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schein AS, et al. Continuous positive airway pressure reduces blood pressure in patients with obstructive sleep apnea; a systematic review and meta-analysis with 1000 patients. J Hypertens. 2014;32(9):1762–73. doi: 10.1097/HJH.0000000000000250. [DOI] [PubMed] [Google Scholar]
- 18.Fava C, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea a systematic review and meta-analysis. Chest. 2014;145(4):762–71. doi: 10.1378/chest.13-1115. [DOI] [PubMed] [Google Scholar]
- 19.Punjabi NM, et al. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am.J.Epidemiol. 2004;160(6):521–530. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 20.Babu AR, et al. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch.Intern.Med. 2005;165(4):447–452. doi: 10.1001/archinte.165.4.447. [DOI] [PubMed] [Google Scholar]
- 21.Drager LF, Jun J, Polotsky VY. Obstructive sleep apnea and dyslipidemia: implications for atherosclerosis. Curr.Opin.Endocrinol.Diabetes Obes. 2010;17(2):161–165. doi: 10.1097/MED.0b013e3283373624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Punjabi NM, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS.Med. 2009;6(8):e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Young T, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Peker Y, et al. Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med. 2002;166(2):159–65. doi: 10.1164/rccm.2105124. [DOI] [PubMed] [Google Scholar]
- 25.Hung J, et al. Association of sleep apnoea with myocardial infarction in men. Lancet. 1990;336(8710):261–4. doi: 10.1016/0140-6736(90)91799-g. [DOI] [PubMed] [Google Scholar]
- 26.Dyken ME, et al. Investigating the relationship between stroke and obstructive sleep apnea. Stroke. 1996;27(3):401–7. doi: 10.1161/01.str.27.3.401. [DOI] [PubMed] [Google Scholar]
- 27.Latina JM, Estes NA, 3rd, Garlitski AC. The Relationship between Obstructive Sleep Apnea and Atrial Fibrillation: A Complex Interplay. Pulm Med. 2013;2013:621736. doi: 10.1155/2013/621736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marin JM, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoeahypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 29.Arnaud C, et al. Obstructive sleep apnea, immuno-inflammation, and atherosclerosis. Semin.Immunopathol. 2009;31(1):113–125. doi: 10.1007/s00281-009-0148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jun J, Polotsky VY. Metabolic consequences of sleep-disordered breathing. ILAR.J. 2009;50(3):289–306. doi: 10.1093/ilar.50.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lavie L. Oxidative stress--a unifying paradigm in obstructive sleep apnea and comorbidities. Prog Cardiovasc Dis. 2009;51(4):303–12. doi: 10.1016/j.pcad.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Lavie L. Intermittent hypoxia: the culprit of oxidative stress, vascular inflammation and dyslipidemia in obstructive sleep apnea. Expert Rev Respir Med. 2008;2(1):75–84. doi: 10.1586/17476348.2.1.75. [DOI] [PubMed] [Google Scholar]
- 33.McNicholas WT. Obstructive sleep apnea and inflammation. Prog Cardiovasc Dis. 2009;51(5):392–9. doi: 10.1016/j.pcad.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 34.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–95. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 35.Liuzzo G, et al. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331(7):417–24. doi: 10.1056/NEJM199408183310701. [DOI] [PubMed] [Google Scholar]
- 36.Biasucci LM, et al. Increasing levels of interleukin (IL)-1Ra and IL-6 during the first 2 days of hospitalization in unstable angina are associated with increased risk of in-hospital coronary events. Circulation. 1999;99(16):2079–84. doi: 10.1161/01.cir.99.16.2079. [DOI] [PubMed] [Google Scholar]
- 37.Koenig W, et al. C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99(2):237–42. doi: 10.1161/01.cir.99.2.237. [DOI] [PubMed] [Google Scholar]
- 38.Haverkate F, et al. Production of C-reactive protein and risk of coronary events in stable and unstable angina. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet. 1997;349(9050):462–6. doi: 10.1016/s0140-6736(96)07591-5. [DOI] [PubMed] [Google Scholar]
- 39.Ridker PM, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336(14):973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 40.Nordestgaard BG, Zacho J. Lipids, atherosclerosis and CVD risk: is CRP an innocent bystander? Nutr Metab Cardiovasc Dis. 2009;19(8):521–4. doi: 10.1016/j.numecd.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 41.Vasse M, et al. Regulation of fibrinogen biosynthesis by cytokines, consequences on the vascular risk. Haemostasis. 1996;26(Suppl 4):331–9. doi: 10.1159/000217313. [DOI] [PubMed] [Google Scholar]
- 42.Wilhelmsen L, et al. Fibrinogen as a risk factor for stroke and myocardial infarction. N Engl J Med. 1984;311(8):501–5. doi: 10.1056/NEJM198408233110804. [DOI] [PubMed] [Google Scholar]
- 43.Gerner RR, et al. Metabolic inflammation: role of cytokines in the crosstalk between adipose tissue and liver. Can J Physiol Pharmacol. 2013;91(11):867–72. doi: 10.1139/cjpp-2013-0050. [DOI] [PubMed] [Google Scholar]
- 44.Arner P. The adipocyte in insulin resistance: key molecules and the impact of the thiazolidinediones. Trends Endocrinol Metab. 2003;14(3):137–45. doi: 10.1016/s1043-2760(03)00024-9. [DOI] [PubMed] [Google Scholar]
- 45.Yudkin JS, et al. Low-grade inflammation may play a role in the etiology of the metabolic syndrome in patients with coronary heart disease: the HIFMECH study. Metabolism. 2004;53(7):852–7. doi: 10.1016/j.metabol.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 46.Visser M, et al. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282(22):2131–5. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- 47.Gottlieb DJ, et al. CPAP versus oxygen in obstructive sleep apnea. N Engl J Med. 2014;370(24):2276–85. doi: 10.1056/NEJMoa1306766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chirinos JA, et al. CPAP, weight loss, or both for obstructive sleep apnea. N Engl J Med. 2014;370(24):2265–75. doi: 10.1056/NEJMoa1306187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Craig SE, et al. Continuous positive airway pressure improves sleepiness but not calculated vascular risk in patients with minimally symptomatic obstructive sleep apnoea: the MOSAIC randomised controlled trial. Thorax. 2012;67(12):1090–6. doi: 10.1136/thoraxjnl-2012-202178. [DOI] [PubMed] [Google Scholar]
- 50.Kohler M, et al. CPAP improves endothelial function in patients with minimally symptomatic OSA: results from a subset study of the MOSAIC trial. Chest. 2013;144(3):896–902. doi: 10.1378/chest.13-0179. [DOI] [PubMed] [Google Scholar]
- 51.Stradling JR, et al. Markers of inflammation: data from the MOSAIC randomised trial of CPAP for minimally symptomatic OSA. Thorax. 2014 doi: 10.1136/thoraxjnl-2014-205958. [DOI] [PubMed] [Google Scholar]
- 52.Unuvar Dogan F, et al. Relationships between Obstructive Sleep Apnea Syndrome, Continuous Positive Airway Pressure Treatment, and Inflammatory Cytokines. Sleep Disord. 2014;2014:518920. doi: 10.1155/2014/518920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kritikou I, et al. Sleep apnoea, sleepiness, inflammation and insulin resistance in middle-aged males and females. Eur Respir J. 2014;43(1):145–55. doi: 10.1183/09031936.00126712. [DOI] [PubMed] [Google Scholar]
- 54.Shamsuzzaman AS, et al. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002;105(21):2462–4. doi: 10.1161/01.cir.0000018948.95175.03. [DOI] [PubMed] [Google Scholar]
- 55.Cheng TO. Could elevated C-reactive protein in patients with obstructive sleep apnea be due to obesity per se? Circulation. 2003;107(1):e9. doi: 10.1161/01.cir.0000046771.12875.6c. author reply e9. [DOI] [PubMed] [Google Scholar]
- 56.Yokoe T, et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. 2003;107(8):1129–34. doi: 10.1161/01.cir.0000052627.99976.18. [DOI] [PubMed] [Google Scholar]
- 57.Kohler M, et al. Effects of continuous positive airway pressure on systemic inflammation in patients with moderate to severe obstructive sleep apnoea: a randomised controlled trial. Thorax. 2009;64(1):67–73. doi: 10.1136/thx.2008.097931. [DOI] [PubMed] [Google Scholar]
- 58.Guilleminault C, Kirisoglu C, Ohayon MM. C-reactive protein and sleep-disordered breathing. Sleep. 2004;27(8):1507–11. doi: 10.1093/sleep/27.8.1507. [DOI] [PubMed] [Google Scholar]
- 59.Barcelo A, et al. Effects of obesity on C-reactive protein level and metabolic disturbances in male patients with obstructive sleep apnea. Am J Med. 2004;117(2):118–21. doi: 10.1016/j.amjmed.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 60.Ryan S, et al. Cardiovascular risk markers in obstructive sleep apnoea syndrome and correlation with obesity. Thorax. 2007;62(6):509–14. doi: 10.1136/thx.2006.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sahlman J, et al. The activation of the inflammatory cytokines in overweight patients with mild obstructive sleep apnoea. J Sleep Res. 2010;19(2):341–8. doi: 10.1111/j.1365-2869.2009.00787.x. [DOI] [PubMed] [Google Scholar]
- 62.Ryan S, Taylor CT, McNicholas WT. Predictors of elevated nuclear factor-kappaB-dependent genes in obstructive sleep apnea syndrome. Am.J.Respir.Crit Care Med. 2006;174(7):824–830. doi: 10.1164/rccm.200601-066OC. [DOI] [PubMed] [Google Scholar]
- 63.Gozal D, et al. C-reactive protein and obstructive sleep apnea syndrome in children. Front Biosci (Elite Ed) 2012;4:2410–22. doi: 10.2741/e553. [DOI] [PubMed] [Google Scholar]
- 64.Kheirandish-Gozal L, et al. Plasma C-reactive protein in nonobese children with obstructive sleep apnea before and after adenotonsillectomy. J Clin Sleep Med. 2006;2(3):301–4. [PMC free article] [PubMed] [Google Scholar]
- 65.Ciccone MM, et al. Correlation between inflammatory markers of atherosclerosis and carotid intima-media thickness in Obstructive Sleep Apnea. Molecules. 2014;19(2):1651–62. doi: 10.3390/molecules19021651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bottazzi B, et al. An integrated view of humoral innate immunity: pentraxins as a paradigm. Annu Rev Immunol. 2010;28:157–83. doi: 10.1146/annurev-immunol-030409-101305. [DOI] [PubMed] [Google Scholar]
- 67.Yasunaga T, et al. Plasma pentraxin 3 is a more potent predictor of endothelial dysfunction than high-sensitive C-reactive protein. Int Heart J. 2014;55(2):160–4. doi: 10.1536/ihj.13-253. [DOI] [PubMed] [Google Scholar]
- 68.Kobukai Y, et al. Morning Pentraxin3 Levels Reflect Obstructive Sleep Apnea-Related Acute Inflammation. J Appl Physiol (1985) 2014 doi: 10.1152/japplphysiol.00237.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oh IS, et al. Identification of nesfatin-1 as a satiety molecule in the hypothalamus. Nature. 2006;443(7112):709–12. doi: 10.1038/nature05162. [DOI] [PubMed] [Google Scholar]
- 70.Ramanjaneya M, et al. Identification of nesfatin-1 in human and murine adipose tissue: a novel depot-specific adipokine with increased levels in obesity. Endocrinology. 2010;151(7):3169–80. doi: 10.1210/en.2009-1358. [DOI] [PubMed] [Google Scholar]
- 71.Leivo-Korpela S, et al. Adipokines NUCB2/nesfatin-1 and visfatin as novel inflammatory factors in chronic obstructive pulmonary disease. Mediators Inflamm. 2014;2014:232167. doi: 10.1155/2014/232167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang CH, et al. The anti-inflammatory and anti-apoptotic effects of nesfatin-1 in the traumatic rat brain. Peptides. 2012;36(1):39–45. doi: 10.1016/j.peptides.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 73.Shen P, et al. Decreased levels of serum nesfatin-1 in patients with obstructive sleep apnea syndrome. Sleep Breath. 2014 doi: 10.1007/s11325-014-1039-0. [DOI] [PubMed] [Google Scholar]
- 74.Emerging Risk Factors, C. et al. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310–20. doi: 10.1056/NEJMoa1107477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fibrinogen Studies, C. et al. Associations of plasma fibrinogen levels with established cardiovascular disease risk factors, inflammatory markers, and other characteristics: individual participant meta-analysis of 154,211 adults in 31 prospective studies: the fibrinogen studies collaboration. Am J Epidemiol. 2007;166(8):867–79. doi: 10.1093/aje/kwm191. [DOI] [PubMed] [Google Scholar]
- 76.Shamsuzzaman A, et al. Severity of obstructive sleep apnea is associated with elevated plasma fibrinogen in otherwise healthy patients. Sleep Breath. 2014 doi: 10.1007/s11325-014-0938-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Basoglu OK, et al. Metabolic syndrome, insulin resistance, fibrinogen, homocysteine, leptin, and C-reactive protein in obese patients with obstructive sleep apnea syndrome. Ann Thorac Med. 2011;6(3):120–5. doi: 10.4103/1817-1737.82440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chin K, et al. Effects of NCPAP therapy on fibrinogen levels in obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 1996;153(6 Pt 1):1972–6. doi: 10.1164/ajrccm.153.6.8665063. [DOI] [PubMed] [Google Scholar]
- 79.Kaditis AG, et al. Morning levels of fibrinogen in children with sleep-disordered breathing. Eur Respir J. 2004;24(5):790–7. doi: 10.1183/09031936.04.00009804. [DOI] [PubMed] [Google Scholar]
- 80.Phillips CL, et al. Effects of continuous positive airway pressure on coagulability in obstructive sleep apnoea: a randomised, placebo-controlled crossover study. Thorax. 2012;67(7):639–44. doi: 10.1136/thoraxjnl-2011-200874. [DOI] [PubMed] [Google Scholar]
- 81.Guardiola JJ, et al. Hypercoagulability in patients with obstructive sleep apnea. Sleep Med. 2001;2(6):517–23. doi: 10.1016/s1389-9457(01)00088-0. [DOI] [PubMed] [Google Scholar]
- 82.Nizankowska-Jedrzejczyk A, et al. Modulation of inflammatory and hemostatic markers in obstructive sleep apnea patients treated with mandibular advancement splints: a parallel, controlled trial. J Clin Sleep Med. 2014;10(3):255–62. doi: 10.5664/jcsm.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nojgaard C, et al. Serum levels of YKL-40 increases in patients with acute myocardial infarction. Coron Artery Dis. 2008;19(4):257–63. doi: 10.1097/MCA.0b013e3282f40dd5. [DOI] [PubMed] [Google Scholar]
- 84.Nielsen AR, et al. Plasma YKL-40: a BMI-independent marker of type 2 diabetes. Diabetes. 2008;57(11):3078–82. doi: 10.2337/db08-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kazakova M, et al. Relationship between sonographic parameters and YKL-40 levels in rheumatoid arthritis. Rheumatol Int. 2013;33(2):341–6. doi: 10.1007/s00296-012-2387-3. [DOI] [PubMed] [Google Scholar]
- 86.Letuve S, et al. YKL-40 is elevated in patients with chronic obstructive pulmonary disease and activates alveolar macrophages. J Immunol. 2008;181(7):5167–73. doi: 10.4049/jimmunol.181.7.5167. [DOI] [PubMed] [Google Scholar]
- 87.Wang X, Xing GH. Serum YKL-40 concentrations are elevated and correlated with disease severity in patients with obstructive sleep apnea syndrome. Scand J Clin Lab Invest. 2014;74(1):74–8. doi: 10.3109/00365513.2013.859726. [DOI] [PubMed] [Google Scholar]
- 88.Li W, Yu Z, Jiang C. Association of Serum YKL-40 With the Presence and Severity of Obstructive Sleep Apnea Syndrome. Lab Med. 2014;45(3):220–5. doi: 10.1309/LMS98AKCXRSL2XOR. [DOI] [PubMed] [Google Scholar]
- 89.Oh DY, et al. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell. 2010;142(5):687–98. doi: 10.1016/j.cell.2010.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ichimura A, et al. Dysfunction of lipid sensor GPR120 leads to obesity in both mouse and human. Nature. 2012;483(7389):350–4. doi: 10.1038/nature10798. [DOI] [PubMed] [Google Scholar]
- 91.Gozal D, et al. Obstructive sleep apnea and obesity are associated with reduced GPR 120 plasma levels in children. Sleep. 2014;37(5):935–41. doi: 10.5665/sleep.3664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dovizio M, et al. Role of platelets in inflammation and cancer: novel therapeutic strategies. Basic Clin Pharmacol Toxicol. 2014;114(1):118–27. doi: 10.1111/bcpt.12156. [DOI] [PubMed] [Google Scholar]
- 93.Jun J, et al. Effect of intermittent hypoxia on atherosclerosis in apolipoprotein E-deficient mice. Atherosclerosis. 2010;209(2):381–386. doi: 10.1016/j.atherosclerosis.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gautier-Veyret E, et al. Intermittent hypoxia-activated cyclooxygenase pathway: role in atherosclerosis. Eur Respir J. 2013;42(2):404–13. doi: 10.1183/09031936.00096512. [DOI] [PubMed] [Google Scholar]
- 95.Beaudin AE, et al. Cyclooxygenases 1 and 2 differentially regulate blood pressure and cerebrovascular responses to acute and chronic intermittent hypoxia: implications for sleep apnea. J Am Heart Assoc. 2014;3(3):e000875. doi: 10.1161/JAHA.114.000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Akkaya E, Gul M, Ugur M. Platelet to lymphocyte ratio: A simple and valuable prognostic marker for acute coronary syndrome. Int J Cardiol. 2014 doi: 10.1016/j.ijcard.2014.08.143. [DOI] [PubMed] [Google Scholar]
- 97.Thomson SP, McMahon LJ, Nugent CA. Endogenous cortisol: a regulator of the number of lymphocytes in peripheral blood. Clin Immunol Immunopathol. 1980;17(4):506–14. doi: 10.1016/0090-1229(80)90146-4. [DOI] [PubMed] [Google Scholar]
- 98.Nelson DH, et al. Blood levels of 17-hydroxycorticosteroids following the administration of adrenal steroids and their relation to levels of circulating leukocytes. J Clin Invest. 1952;31(9):843–9. doi: 10.1172/JCI102671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Koseoglu HI, et al. Platelet-lymphocyte ratio is an independent predictor for cardiovascular disease in obstructive sleep apnea syndrome. J Thromb Thrombolysis. 2014 doi: 10.1007/s11239-014-1103-4. [DOI] [PubMed] [Google Scholar]
- 100.Kassi E, et al. Role of vitamin D in atherosclerosis. Circulation. 2013;128(23):2517–31. doi: 10.1161/CIRCULATIONAHA.113.002654. [DOI] [PubMed] [Google Scholar]
- 101.Kheirandish-Gozal L, Peris E, Gozal D. Vitamin D levels and obstructive sleep apnoea in children. Sleep Med. 2014;15(4):459–63. doi: 10.1016/j.sleep.2013.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Drager LF, Jun JC, Polotsky VY. Metabolic consequences of intermittent hypoxia: relevance to obstructive sleep apnea. Best.Pract.Res.Clin.Endocrinol.Metab. 2010;24(5):843–851. doi: 10.1016/j.beem.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jun J, Polotsky VY. Sleep Disordered Breathing And Metabolic Effects: Evidence From Animal Models. Sleep Med.Clin. 2007;2(2):263–277. doi: 10.1016/j.jsmc.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jun JC, et al. Intermittent Hypoxia-Induced Glucose Intolerance is Abolished by Alpha-Adrenergic Blockade or Adrenal Medullectomy. Am J Physiol Endocrinol Metab. 2014 doi: 10.1152/ajpendo.00373.2014. p. ajpendo 00373 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Regazzetti C, et al. Hypoxia decreases insulin signaling pathways in adipocytes. Diabetes. 2009;58(1):95–103. doi: 10.2337/db08-0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Trayhurn P, Wang B, Wood IS. Hypoxia in adipose tissue: a basis for the dysregulation of tissue function in obesity? Br J Nutr. 2008;100(2):227–35. doi: 10.1017/S0007114508971282. [DOI] [PubMed] [Google Scholar]
- 107.Drager LF, et al. Chronic intermittent hypoxia induces atherosclerosis via activation of adipose angiopoietin-like 4. Am J Respir Crit Care Med. 2013;188(2):240–8. doi: 10.1164/rccm.201209-1688OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.He Q, et al. Regulation of HIF-1{alpha} activity in adipose tissue by obesity-associated factors: adipogenesis, insulin, and hypoxia. Am J Physiol Endocrinol Metab. 2011;300(5):E877–85. doi: 10.1152/ajpendo.00626.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lee YS, et al. Increased adipocyte O2 consumption triggers HIF-1alpha, causing inflammation and insulin resistance in obesity. Cell. 2014;157(6):1339–52. doi: 10.1016/j.cell.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shin MK, et al. The effect of adrenal medullectomy on metabolic responses to chronic intermittent hypoxia. Respir Physiol Neurobiol. 2014;203C:60–67. doi: 10.1016/j.resp.2014.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Poulain L, et al. Visceral white fat remodelling contributes to intermittent hypoxia-induced atherogenesis. Eur Respir J. 2014;43(2):513–22. doi: 10.1183/09031936.00019913. [DOI] [PubMed] [Google Scholar]
- 112.Barcelo A, et al. Free fatty acids and the metabolic syndrome in patients with obstructive sleep apnoea. Eur Respir J. 2011;37(6):1418–23. doi: 10.1183/09031936.00050410. [DOI] [PubMed] [Google Scholar]
- 113.Jun J, et al. Intermittent hypoxia has organ-specific effects on oxidative stress. Am.J.Physiol Regul.Integr.Comp Physiol. 2008;295(4):R1274–R1281. doi: 10.1152/ajpregu.90346.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kanagy NL. Vascular effects of intermittent hypoxia. ILAR.J. 2009;50(3):282–288. doi: 10.1093/ilar.50.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112(17):2660–7. doi: 10.1161/CIRCULATIONAHA.105.556746. [DOI] [PubMed] [Google Scholar]
- 116.Jun JC, et al. Effects of sleep apnea on nocturnal free fatty acids in subjects with heart failure. Sleep. 2011;34(9):1207–1213. doi: 10.5665/SLEEP.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sniderman AD, Cianflone K. Substrate delivery as a determinant of hepatic apoB secretion. Arterioscler.Thromb. 1993;13(5):629–636. doi: 10.1161/01.atv.13.5.629. [DOI] [PubMed] [Google Scholar]
- 118.Schaffer JE. Lipotoxicity: when tissues overeat. Curr.Opin.Lipidol. 2003;14(3):281–287. doi: 10.1097/00041433-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 119.Zhou S, et al. Deletion of metallothionein exacerbates intermittent hypoxia-induced oxidative and inflammatory injury in aorta. Oxid Med Cell Longev. 2014;2014:141053. doi: 10.1155/2014/141053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cai L, et al. Metallothionein in radiation exposure: its induction and protective role. Toxicology. 1999;132(2-3):85–98. doi: 10.1016/s0300-483x(98)00150-4. [DOI] [PubMed] [Google Scholar]
- 121.Badran M, et al. Chronic intermittent hypoxia causes endothelial dysfunction in a mouse model of diet-induced obesity. Sleep Med. 2014;15(5):596–602. doi: 10.1016/j.sleep.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 122.Kaur C, et al. Increased vascular permeability and nitric oxide production in response to hypoxia in the pineal gland. J Pineal Res. 2007;42(4):338–49. doi: 10.1111/j.1600-079X.2007.00424.x. [DOI] [PubMed] [Google Scholar]
- 123.Hung MW, et al. Melatonin ameliorates endothelial dysfunction, vascular inflammation, and systemic hypertension in rats with chronic intermittent hypoxia. J Pineal Res. 2013;55(3):247–56. doi: 10.1111/jpi.12067. [DOI] [PubMed] [Google Scholar]
- 124.Totoson P, et al. Atorvastatin protects against deleterious cardiovascular consequences induced by chronic intermittent hypoxia. Exp Biol Med (Maywood) 2013;238(2):223–32. doi: 10.1177/1535370212473696. [DOI] [PubMed] [Google Scholar]
- 125.Smith SM, Friedle SA, Watters JJ. Chronic intermittent hypoxia exerts CNS region-specific effects on rat microglial inflammatory and TLR4 gene expression. PLoS One. 2013;8(12):e81584. doi: 10.1371/journal.pone.0081584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Trotta T, et al. Biological role of Toll-like receptor-4 in the brain. J Neuroimmunol. 2014;268(1-2):1–12. doi: 10.1016/j.jneuroim.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 127.Gozal E, et al. Proteomic analysis of CA1 and CA3 regions of rat hippocampus and differential susceptibility to intermittent hypoxia. J Neurochem. 2002;83(2):331–45. doi: 10.1046/j.1471-4159.2002.01134.x. [DOI] [PubMed] [Google Scholar]
- 128.Guven SF, et al. The prevalence of obstructive sleep apnea in patients with difficult-to-treat asthma. Asian Pac J Allergy Immunol. 2014;32(2):153–9. doi: 10.12932/AP0360.32.2.2013. [DOI] [PubMed] [Google Scholar]
- 129.Lu Y, et al. [Treatment of obstructive sleep apnea-hypopnea syndrome for children refractory asthma] Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2014;49(6):462–7. [PubMed] [Google Scholar]
- 130.Reinke C, et al. Chronic intermittent hypoxia induces lung growth in adult mice. Am J Physiol Lung Cell Mol Physiol. 2011;300(2):L266–73. doi: 10.1152/ajplung.00239.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Philippe C, et al. Airway cell involvement in intermittent hypoxia-induced airway inflammation. Sleep Breath. 2014 doi: 10.1007/s11325-014-1019-4. [DOI] [PubMed] [Google Scholar]
- 132.Dancey DR, et al. Impact of menopause on the prevalence and severity of sleep apnea. Chest. 2001;120(1):151–5. doi: 10.1378/chest.120.1.151. [DOI] [PubMed] [Google Scholar]
- 133.Bixler EO, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163(3 Pt 1):608–13. doi: 10.1164/ajrccm.163.3.9911064. [DOI] [PubMed] [Google Scholar]
- 134.Gottlieb DJ, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Campos-Rodriguez F, et al. Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am J Respir Crit Care Med. 2013;187(1):99–105. doi: 10.1164/rccm.201209-1671OC. [DOI] [PubMed] [Google Scholar]
- 136.Torres M, et al. Effect of ovariectomy on inflammation induced by intermittent hypoxia in a mouse model of sleep apnea. Respir Physiol Neurobiol. 2014;202:71–4. doi: 10.1016/j.resp.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 137.Somers VK, Abboud FM. Chemoreflexes--responses, interactions and implications for sleep apnea. Sleep. 1993;16(8 Suppl):S30–S33. [PubMed] [Google Scholar]
- 138.Somers VK, et al. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J Appl Physiol (1985) 1989;67(5):2101–6. doi: 10.1152/jappl.1989.67.5.2101. [DOI] [PubMed] [Google Scholar]
- 139.Stamatakis KA, Punjabi NM. Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest. 2010;137(1):95–101. doi: 10.1378/chest.09-0791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Deibert DC, Defronzo RA. Epinephrine-induced insulin resistance in man. J.Clin.Invest. 1980;65(3):717–721. doi: 10.1172/JCI109718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Halberg N, et al. Hypoxia-inducible factor 1alpha induces fibrosis and insulin resistance in white adipose tissue. Mol Cell Biol. 2009;29(16):4467–83. doi: 10.1128/MCB.00192-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Chinen I, et al. Vascular lipotoxicity: endothelial dysfunction via fatty-acid-induced reactive oxygen species overproduction in obese Zucker diabetic fatty rats. Endocrinology. 2007;148(1):160–165. doi: 10.1210/en.2006-1132. [DOI] [PubMed] [Google Scholar]
- 143.Imrie H, Abbas A, Kearney M. Insulin resistance, lipotoxicity and endothelial dysfunction. Biochim.Biophys.Acta. 2010;1801(3):320–326. doi: 10.1016/j.bbalip.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 144.Chouchou F, et al. Sympathetic overactivity due to sleep fragmentation is associated with elevated diurnal systolic blood pressure in healthy elderly subjects: the PROOF-SYNAPSE study. Eur Heart J. 2013;34(28):2122–31. 2131a. doi: 10.1093/eurheartj/eht208. [DOI] [PubMed] [Google Scholar]