Abstract
Background: Climate change and global warming have been reported to increase spread of foodborne pathogens. To understand these effects on Salmonella infections, modeling approaches such as regression analysis and neural network (NN) were used.
Methods: Monthly data for Salmonella outbreaks in Mississippi (MS), Tennessee (TN), and Alabama (AL) were analyzed from 2002 to 2011 using analysis of variance and time series analysis. Meteorological data were collected and the correlation with salmonellosis was examined using regression analysis and NN.
Results: A seasonal trend in Salmonella infections was observed (p<0.001). Strong positive correlation was found between high temperature and Salmonella infections in MS and for the combined states (MS, TN, AL) models (R2=0.554; R2=0.415, respectively). NN models showed a strong effect of rise in temperature on the Salmonella outbreaks. In this study, an increase of 1°F was shown to result in four cases increase of Salmonella in MS. However, no correlation between monthly average precipitation rate and Salmonella infections was observed.
Conclusion: There is consistent evidence that gastrointestinal infection with bacterial pathogens is positively correlated with ambient temperature, as warmer temperatures enable more rapid replication. Warming trends in the United States and specifically in the southern states may increase rates of Salmonella infections.
Introduction
Salmonella is an important foodborne pathogen worldwide. A recent study estimated that approximately 93.8 million human cases of gastroenteritis and 155,000 deaths occur due to Salmonella infection around the world each year (Hoelzer et al., 2011). In the United States alone, Salmonella causes an estimated 1.4 million human cases, 15,000 hospitalizations, and more than 400 deaths annually (Callaway et al., 2008). Emergence or resurgence of numerous infectious diseases are strongly influenced by environmental factors such as climate or land use change (Mills et al., 2010). Climate, weather, topology, hydrology, and other geographical characteristics of the growing site may influence the magnitude and frequency of transfer of pathogenic microorganisms from environmental sources (World Health Organization Food Safety Report, 2011).
Diseases associated with climate change are estimated already to comprise 4.6% of all environmental risks and hazards. It has been estimated that climate change in the year 2000 contributed to about 2.4% of all diarrhea outbreaks in the world, 6% of malaria outbreaks in certain developing countries, and 7% of the episodes of dengue fever in some industrial countries. In total, the estimates show that climate change related mortalities has been 0.3%, whereas the related burden of disease has been 0.4% (Kendrovski and Gjorgjev, 2012).
From 1906 to 2005, global average temperature has warmed by 0.74°C, and since 1961, sea level has risen on average by approximately 2 mm per year. Arctic sea ice extent has declined by 7.4% per decade, and snow cover and glaciers have diminished in both hemispheres (Mills et al., 2010). The rate of change in climate is faster now than in any period in the last 1000 years. According to the United Nations Intergovernmental Panel on Climate Change, in 90 years, average global temperatures will increase between 1.8°C and 4.0°C and sea level will rise between 18 and 59 cm (Patz et al., 2008; McMichael et al., 2006).
Weather, and particularly changes in expected weather patterns, can be the reason for transfer of microbial contaminants to leafy vegetables and herbs. Dry periods can cause dust storms that settle dust particles on leafy vegetables. Increased temperatures can increase the rate of microbial growth. It may also influence the population of insects and pests found in and around farms that transfer human pathogens to leafy vegetables. Relative humidity has been shown to have an effect on survival of human pathogens (Hunter et al., 2003). Climate change scenarios predict a change distribution of infectious diseases with warming and changes in outbreaks associated with weather extremes, such as flooding and droughts.
Many infectious agents, vector organisms, nonhuman reservoir species, and rate of pathogen replication are sensitive to climatic conditions. Both Salmonella and Vibrio cholerae, for example, proliferate more rapidly at higher temperatures: Salmonella in animal gut and food, V. cholerae in water. In regions where low temperature, low rainfall, or absence of vector habitat restrict transmission of vectorborne disease, climatic changes could tip the ecological balance and trigger epidemics (McMichael et al., 2006). Further, strong linear associations have been noted between temperature and notifications of Salmonellosis in European countries and Australia, and a weak seasonal relation exists for Campylobacter (McMichael et al., 2006).
The United States is likely to experience increases in extreme cold, extreme heat, hurricanes, floods, wildfires, droughts, tornadoes, and severe storms (NOAA, 2012). The health impacts of global climate change are anticipated to be widespread, geographically myriad, and profoundly influenced by preexisting social and economic disparities (Sheffield and Landrigan, 2011).
The climate of the Southern states, including Mississippi's, has always been fluctuating and sometimes extreme. The average temperatures in Mississippi have varied substantially over the past century, with an average of 1°F increase since the late 1960s. Extreme rainfall events, primarily thunderstorms, have increased in this century. While rainfall totals have changed little, seasonal trends are apparent; summers have become slightly drier and winters slightly wetter (NOAA, 2012). On an average, 29 tornadoes are reported annually in Mississippi; the highest number was in 2008 with 109 tornadoes. In addition, during the past decade, Mississippi had experienced multiple hits by hurricanes, including the devastating Katrina (NOAA, 2012).
Climate change and global warming have contributed to the spread of several foodborne pathogens (Patz, 2008; WHO Food Safety Report, 2011). The current study was undertaken to investigate the effects of climate change on Salmonella infections and the correlation with temperature and precipitation using various modeling approaches.
Materials and Methods
Monthly data of Salmonella outbreaks from 2002 to 2011 were obtained from Mississippi State Department of Health, Department of Epidemiology; Alabama Department of Public Health; and TN Department of Health, Communicable Disease Interactive Data (available at http://health.state.tn.us/ceds/WebAim/WEBAim_criteria.aspx). In addition, meteorological data, including average air temperatures, minimum and maximum, and total precipitation for the selected station across the state and states' averages (MS, AL, and TN) were collected from the Southeast Regional Climate Center, available at: http://www.sercc.com/climateinfo/monthly_seasonal.html
Analysis of variance was performed to determine the seasonal change in Salmonella outbreaks during the study period using SAS 9.2 (SAS 9.2, Cary, NC; 2010). Time series analysis, including the Mann–Kendall test and a Seasonal trend test, was applied to quantify the relationships between the temperature and the number of notified cases of Salmonella, using the SYSTAT software package (SigmaPlot, 2009). Regression analysis was performed using SAS 9.2 where temperature and precipitation were used as independent (classification) variables and Salmonella outbreaks as dependent (response) variable.
Neural Network (NN) models for temperature effects on Salmonella outbreaks were developed using @RISK (Palisade Corporation, 2011) and NeuroShell2 (Ward Systems Group, 1993) software packages. NeuroShell2 is a program that mimics the human brain's ability to classify patterns or to make predictions or decisions based upon past experience. NeuroShell2 enables the building of sophisticated custom problem-solving applications without programming. The network is told the problem being predicted or classified, and NeuroShell2 will be able to “learn” patterns from training data and be able to make its own classifications, predictions, or decisions when presented with new data. NN models are particularly useful when there are implicit interactions and complex relationships in the data.
Monthly temperature and Salmonella data from 2002 to 2011 in MS were used to build these models. Temperature was used as an input while Salmonella outbreaks as output variables. A General Regression NN Model and Polynomial Net Models were selected from the software design architecture. Twenty percent of the data were extracted for testing, and 80% were used for training the NN models. A test data file was applied to previously saved trained NN models and thus outputs were generated. Results were exported to Excel, where graphs were created to show the association between actual data and the predicted model.
Results
To understand the effects of climate change, Salmonella association with temperature and precipitation was examined using regression analysis and NN modeling. No significant change in temperature or precipitation rates was observed during the study period (p>0.05). The highest temperature was recorded in 2007 with an average of 64.95°F, while 2009 had the highest precipitation (68.64 inches) and the lowest in 2007 (42.33 inches).
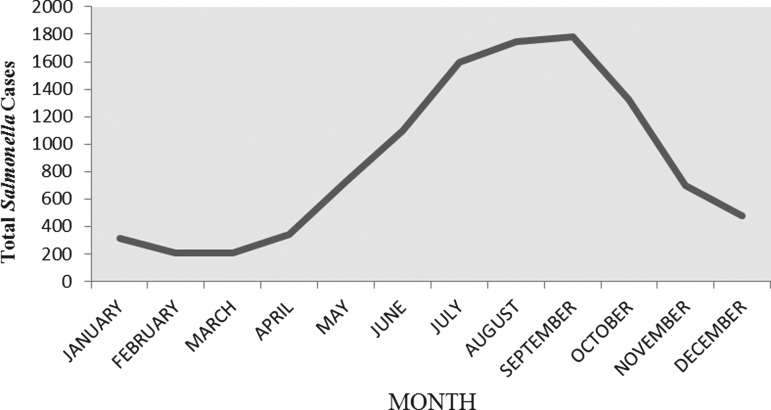
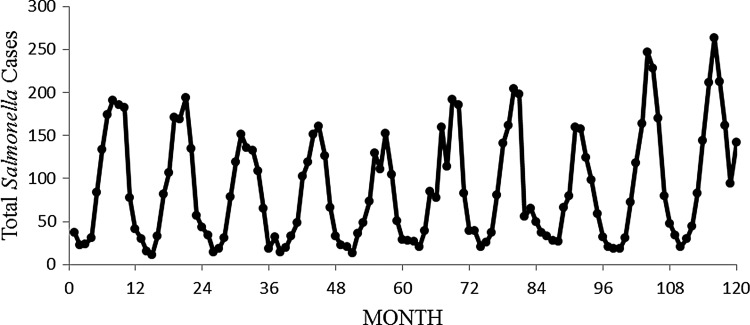
Time series analysis, including Mann–Kendall test and a Seasonal trend test, were applied to quantify the relationship between the temperature and the number of notified cases of Salmonella. A seasonal trend in Salmonella outbreaks data was observed during 2002–2011 (Fig. 1). Highest outbreaks of Salmonella were observed during the summer season with peaks during July through September. Mann–Kendall Test results are shown in Table 1 and Figure 2. Significant high infections rates were observed during the summer season (p<0.01; Kendall Tau Statistic=0.169 and Z=2.35).
FIG. 1.
Total monthly Salmonella cases in Mississippi from 2002 to 2011. Highest rates of Salmonella were observed during the summer.
Table 1.
Mann–Kendall Test Results
| Month | Number of observations | Statistic | ASE | Tau |
|---|---|---|---|---|
| January | 10 | −5 | 11.091 | −0.111 |
| February | 10 | 9 | 10.970 | 0.200 |
| March | 10 | 20 | 11.136 | 0.444 |
| April | 10 | 13 | 10.970 | 0.289 |
| May | 10 | −4 | 11.136 | −0.089 |
| June | 10 | 3 | 11.180 | 0.067 |
| July | 10 | 9 | 11.180 | 0.200 |
| August | 10 | 13 | 11.180 | 0.289 |
| September | 10 | 13 | 11.180 | 0.289 |
| October | 10 | −7 | 11.180 | −0.156 |
| November | 10 | 12 | 11.136 | 0.267 |
| December | 10 | 15 | 11.180 | 0.333 |
ASE, asymptotic standard error; Tau, the Kendall correlation coefficient; measures the strength of association.
FIG. 2.
Time series analysis for Salmonella outbreaks from January 2002 to December 2011.
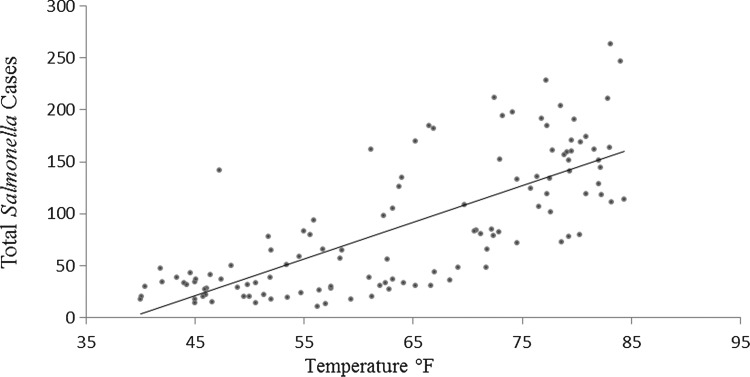
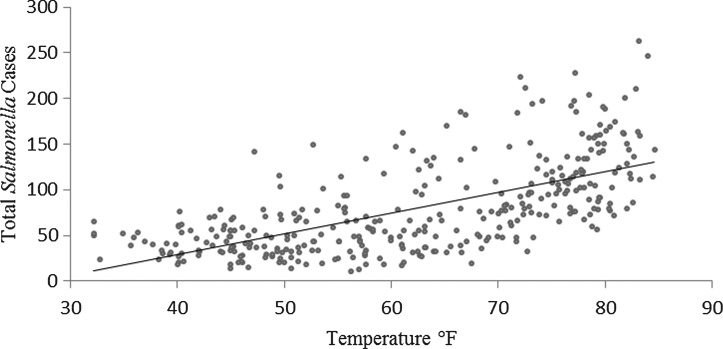
Regression analysis was performed to determine the climate effect on Salmonella. The temperature and precipitation were used as classification (independent) variables and Salmonella infections as a response (dependent) variable. Two regression analyses were performed; the first model was created using Mississippi data, and the second model was created with Mississippi, Alabama, and Tennessee data. Strong positive correlation was found between the temperature and Salmonella outbreaks in Mississippi and for the three-states model (R2=0.554, R2=0.415, respectively; p<0.01) (Figures 3 and 4). The results showed that a 1°F increase in temperature will result in an increase of four cases (3% increase of the current average) of Salmonella infections. However, no correlation was found between total precipitation and Salmonella outbreaks in MS.
FIG. 3.
Mississippi regression analysis between temperature and Salmonella. y=3.5252x – 137.65; R2=0.554.
FIG. 4.
Regression analysis between temperature and Salmonella in Mississippi, Tennessee, and Alabama. y=2.2769x – 62.171; R2=0.4154.
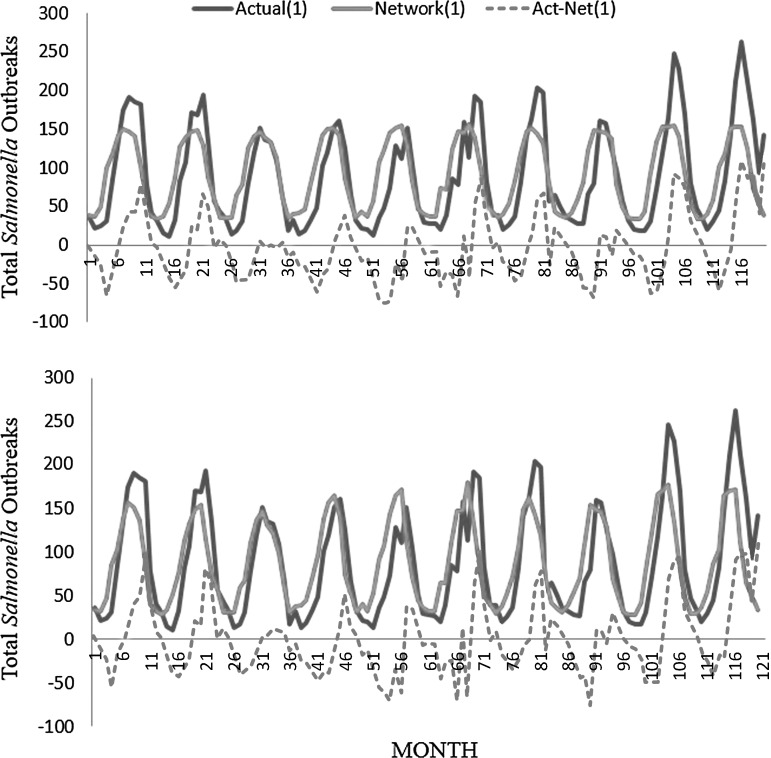
NN models for detecting temperature effect on Salmonella outbreaks were developed. Monthly temperature and Salmonella data, from 2002 to 2011 in MS, were used to build the models. Temperature was used as an input variable while Salmonella outbreaks were used as output variable for the model. A General Regression NN Model and Polynomial Net Models were selected from design architecture. Results of the two models (Table 2) showed that coefficient of determination R2 was 0.567 and 0.582, respectively, when exposed to test data. The correlation coefficients for the models were 0.757 and 0.763, respectively, which shows a strong correlation between the outcomes and the predicted values. NN models showed a strong effect of rise in temperature on the Salmonella outbreaks, as shown in Figure 5.
Table 2.
Results of Two Neural Network Models: Effects of Temperature on Salmonella
| Results | GRNN | GMDH |
|---|---|---|
| R2 | 0.567 | 0.582 |
| r2 | 0.573 | 0.582 |
| Mean squared error | 1745 | 1688 |
| Mean absolute error | 32.82 | 31.62 |
| Min. absolute error | 0.085 | 0.0383 |
| Max. absolute error | 109 | 108 |
| Correlation coefficient r | 0.757 | 0.763 |
GRNN, General Regression Neural Network; GMDH, Group Method of Data Handling, Polynomial Net.
FIG. 5.
General Regression NN and Polynomial Net (Group Method of Data Handling, Polynomial Net) Models to forecast the Salmonella outbreak from January 2002 through December 2011.
Discussion
In the current study, the effects of climate variation on Salmonella infections in MS were examined. Results indicated an increase in temperature is positively correlated with Salmonella infections. A seasonal trend was also observed in this study, with the highest outbreaks during the summer to early fall. The positive relationship between temperature and Salmonella infections, observed in this study, using regression and neural network models, was similar to recent findings from Australia, Europe, North America, and Asia with similar trends (D'Souza et al., 2005; Taylor et al., 2009; Zhang et al., 2010). Endemic regions for Salmonella outbreaks include developing countries in South Central and Southeast Asia, and many parts of Africa, the Middle East, and Latin America. In countries such as sub-Saharan Africa, nontyphoidal salmonellae are consistently the most common bacterial bloodstream isolates in both adults and children presenting with fever and are associated with a case fatality of 20–25% (Feasey et al., 2012). It is worth noting, however, that the foodborne outbreak surveillance systems in developing countries cover <1% of the actual outbreaks (Tajkarimia et al., 2013).
In the current study, an increase of 1°F was shown to result in four new cases of Salmonella in MS. Other studies also found that weekly counts of enteric bacterial disease cases generally increased with weekly temperature after adjusting for seasonal and long-term trends (Fleury et al., 2006). Zhang et al. (2010) had suggested that a potential 1°C rise in mean weekly maximum temperature may be related to an 8.8% increase in the weekly number of cases, and a 1°C rise in mean weekly minimum temperature may lead to a 5.8% increase in the weekly number of cases.
During the current study period, there was no significant change in Salmonella cases in MS; however, a seasonal trend was observed. Any such increase in Salmonella outbreaks could be attributed to the implementation of better surveillance systems, such as PulseNet, which allows Salmonella cases to be grouped into an outbreak that otherwise would have been considered as sporadic cases (Zhang et al., 2011). Since we did not observe any such increase during our study period, it remains a mere speculative assumption.
The southern states climate is generally warm and wet, with mild and humid winters. Since 1970, average annual temperatures in the region have increased by about 2°F, and the average annual temperatures in the region are projected to increase by 4 to 9°F by 2080 (Karl et al., 2009). Climate change and extreme events may increase the spread of foodborne illnesses in this region, particularly in disadvantaged states such as Mississippi.
Better growth of Salmonella at higher temperatures leads to higher concentration of Salmonella in the food supply in the warmer months. Inadequate cooking practices are also more common during these months (picnics, barbecues, etc.). Temperature may affect the transmission of Salmonella infections via several causal pathways, such as direct effects on bacterial proliferation and indirect effects on eating habits during hot days. The optimum temperature for the growth of Salmonellae is between 35°C and 37°C. The growth is greatly reduced at <15°C. Ambient temperature influences the development of Salmonella at various stages in the food chain, including bacterial loads on raw food production, transport, and inappropriate storage (Juneja, 2007; Zhang et al., 2010).
There is consistent evidence that gastrointestinal infection with bacterial pathogens is positively correlated with ambient temperature, as warmer temperatures enable more rapid replication. Annually, Salmonella notifications peak in summer and the rate of notifications has been shown to be positively and linearly correlated with the mean temperature of the previous month or week (Bambrick et al., 2008; Russell et al., 2010). Although some of the increase in summer months may be due to changed eating behaviors (more “eating out” while on holidays and attending outdoor functions such as barbecues), ambient temperatures contribute directly to pathogen multiplication in foods and thus likelihood of infection. Furthermore, it was noted that enteric diseases in temperate latitudes have a seasonal pattern, with the highest incidence of illnesses during the summer months. A study of foodborne illnesses in the United Kingdom found a relationship between the incidence of disease and the temperature in the month preceding the illness (Bentham and Langford, 2001). It is believed that the survival and growth of certain enteric pathogens are, within limits, positively correlated with ambient temperature (Fleury et al., 2006).
Studies also predicted that notification rates of Salmonella infection are expected to increase in future as climate change causes ambient temperatures to rise above the previous average, contributing to around 1000 extra cases annually. This relates to an annual difference of approximately 1200 lost workdays and $120,000 in the cost of health care and surveillance by 2050 (Bambrick et al., 2008). By considering a suite of future climate scenarios, the Intergovernmental Panel on Climate Change projected global surface temperature increases between 1.1 and 6.4°C over the next century. Studies had shown that the main health risks caused by climate change include health impacts of weather disasters; health impacts of temperature extremes, including heat waves; mosquito-borne infectious diseases; foodborne infectious diseases (including those due to Salmonella, Campylobacter, and many other microbes); waterborne infectious diseases, and other health risks from poor water quality; diminished food availability (yields, costs/affordability); nutritional consequences, increases in urban air pollution (e.g., ozone), and the interaction of this environmental health hazard with meteorological conditions; changes in aeroallergens (spores, pollens), potentially exacerbating asthma and other allergic respiratory diseases; and mental health consequences of social, economic, and demographic dislocations (e.g., in parts of rural Australia, and via disruptions to traditional ways of living in remote indigenous communities) (Bambrick et al., 2008; Semenza and Menne, 2009; Petrescue et al., 2011).
On the other hand, no correlation between monthly average precipitation rate and Salmonella was observed in this study. A better association with Salmonella outbreaks was observed in studies using daily or weekly rates of precipitation. In addition, no significant change in precipitation rates was observed during the study period. Other studies, however, indicated that maximum and minimum temperatures, relative humidity, and rainfall were all positively correlated with the number of cases of Salmonella, with the lag values of the effects being between 2 weeks and 2 months. They reported that rainfall, especially heavy rainfall events, may affect the frequency and level of contamination of drinking water, and hence enteric infection. A strong association between drinking water quality, precipitation, and gastroenteritis was reported (Zhang et al., 2008).
Climatic changes can also impact the emergence or re-emergence of infectious disease agents. There are some general principles of pathogen emergence, which are associated with changes in ecology and agriculture, technology and industry, globalization, human behavior and demographics, epidemiological surveillance, and microbial adaptation (Tauxe, 2002; Rose et al., 2001). It is important to recognize that pathogen emergence usually occurs as a consequence of a combination of two or more specific factors (Jaykus et al., 2011).
NN modeling of Salmonella and temperature
Over the last few years, artificial neural networks, as nonlinear modeling techniques, had been proposed for use in predictive microbiology (Ibarra and Yang, 1999; McKee et al., 2000; Jacoboni et al., 2001; Garcíaa-Gimeno et al., 2003; Hervas et al., 2007; Valero et al., 2007; Khanzadi et al., 2010). In the current study, two neural network models—General Regression NN Model and Polynomial Net Model—were used to predict the effects of temperature on Salmonella outbreaks in MS. Several architectures of neural network models were developed to determine the best-fitting models. Both of the reported models showed a significant correlation between temperature and Salmonella outbreak. Previous studies had used a general regression neural network and Monte Carlo simulation models for predicting survival and growth of Salmonella on raw chicken skin as a function of serotype, temperature, and time (Oscar, 2004).
Statistical methodologies and modeling were shown to be useful tools to recognize the impact of fluctuating weather on human health. Despite its connection to seasonal changes in temperature, Salmonella infections have declined in Europe and other parts of the world in the last decade, likely in part due to ramped-up public health efforts (Zhang et al., 2010). The decline raises hope that any effects of climate change on foodborne illness might be counteracted with carefully implemented health promotion and food safety policies.
Conclusions
Climate changes are likely to increase the severity, frequency, timing, and duration of extreme weather events in the United States, which in turn will increase health risks. The transmission of Salmonella to humans is a complex ecological process; warmer temperatures, in combination with differences in eating behavior, may contribute to enteric infections including Salmonella infection. Regression and neural network models were used to determine the correlation between increase in temperature and increase in Salmonella outbreaks. Both models showed strong positive correlation between increase in temperature and Salmonella infections. However, considering the seasonal variation, neural network models turned out to be better predictor models.
Acknowledgments
The project described was supported by Grant Number G12RR013459 from the National Center of Research Resources, G12MD007581 from National Institutes of Health(NIH)/National Institute on Minority Health and Health Disparities (NIMHD), and PGA-P210944 from the U.S. Department of State.
Disclosure Statement
No competing financial interests exist.
References
- Bambrick H, Dear K, Woodruff R, Hanigan I, McMichael A. The impacts of climate change on three health outcomes: Temperature-related mortality and hospitalizations, salmonellosis and other bacterial gastroenteritis, and population at risk from dengue. Garnaut Climate Change Rev 2008. Available at http://garnautreview.org.au/CA25734E0016A131/WebObj/03-AThreehealthoutcomes/$File/03-A%20Three%20health%20outcomes.pdf
- Bentham G, Langford IH. Environmental temperatures and the incidence of food poisoning in England and Wales. Int J Biometeorol 2001;45:22–26 [DOI] [PubMed] [Google Scholar]
- Callaway TR, Edrington TS, Anderson RC, Byrd JA, Nisbet DJ. Gastrointestinal microbial ecology and the safety of our food supply as related to Salmonella. J Anim Sci 2008;86(Suppl):E163–E172 [DOI] [PubMed] [Google Scholar]
- D'Souza RM. Climatic factors association with hospitalization and emergency room presentations of diarrhea. Epidemiology 2005;16:S60 [Google Scholar]
- Feasey NA, Dougan G, Kingsley RA, Heyderman RS, Gordon MA. Invasive non-typhoidal Salmonella disease: An emerging and neglected tropical disease in Africa. Lancet 2012;379:2489–2499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleury M, Charron DF, Holt JD, Allen OB, Maarouf AR. A time series analysis of the relationship of ambient temperature and common bacterial enteric infections in two Canadian provinces. Int J Biometeor 2006;50:385–391 [DOI] [PubMed] [Google Scholar]
- Garcíaa-Gimeno RM, Hervás-Martíanez C, Barco-Alcalá E, Zurera-Cosano G, Sanz-Tapi E. An artificial neural network approach to Escherichia coli O157:H7 growth estimation. J Food Sci 2003;68:639–645 [Google Scholar]
- Hervás C, Martínez JA, Zurera G, García RM, Martínez JA. Optimization of computational neural network for its application in the prediction of microbial growth in food. Food Sci Technol Int 2007;7:159 [Google Scholar]
- Hoelzer K, Isabel A, Switt M, Wiedmann M. Animal contact as a source of human non-typhoidal salmonellosis. Vet Res 2011;42:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter PR. Climate change and waterborne and vector-borne disease. J Appl Microbiol 2003;94(Suppl):37S–46S [DOI] [PubMed] [Google Scholar]
- Ibarra JG, Yang T. Estimation of internal temperature in chicken meat by means of mid-infrared imaging and neural networks. Precision Agric Biol Qual 1999;24. doi: 10.1117/12.336903 [DOI] [Google Scholar]
- Jacoboni I, Martelli PL, Fariselli P, De Pinto V, Casadio R. Prediction of the transmembrane regions of β-barrel membrane proteins with a neural network-based predictor. Protein Sci 2001;10:779–787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaykus L-A, Woolridge M, Frank JM, Miraglia M, McQuatters-Gollop A, Tirado C, Clarke R, Friel M. Climate change: Implications for food safety. FAO Rep 2011. Available at ftp://ftp.fao.org/docrep/fao/010/i0195e/i0195e00.pdf
- Juneja VK, Valenzuela Melendres M, Huang L, Gumudavelli V, Subbiah J, Thippareddi H. Modeling the effect of temperature on growth of Salmonella in chicken. Food Microbiol 2007;24:328–335 [DOI] [PubMed] [Google Scholar]
- Karl TR, Melillo JM, Peterson TC. (eds.). Global Climate Change Impacts in the United States. United States Global Change Research Program. New York: Cambridge University Press, 2009 [Google Scholar]
- Kendrovski V, Gjorgjev D. Climate change: Implication for food-borne diseases (Salmonella and food poisoning among humans in R. Macedonia). In: Structure and Function of Food Engineering. Rijeka, Croatia: INTECH, 2012, pp. 151–170 [Google Scholar]
- Khanzadi S, Gharibzadeh S, Raoufy RM, Razavilar V, Khaksar R, Radmehr B. Application of artificial neural networks to predict Clostridium botulinum growth as a function of Zataria multiflora essential oil, pH, NaCl, and temperature. J Food Safety 2010;30:490–505 [Google Scholar]
- McKee KT, Shields TM, Jenkins PR, Zenilman JM, Glass GE. Application of a geographic information system to the tracking and control of an outbreak of shigellosis. Clin Infect Dis 2000;31:728–733 [DOI] [PubMed] [Google Scholar]
- McMichael AJ, Woodruff RE, Hales S. Climate change and human health: Present and future risks. Lancet 2006;367:859–869 [DOI] [PubMed] [Google Scholar]
- Mills JN, Gage KL, Khan AS. Potential influence of climate change on vector-borne and zoonotic diseases: A review and proposed research plan. Int J Health Geogr 2010;9:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [NOAA] National Oceanic and Atmospheric Administration. U.S. Climate Extremes Index. 2012. Available at: http://www.ncdc.noaa.gov/extremes/cei/, accessed April20, 2012
- NOAA National Weather Service Weather Forecast General Tornado Statistics for Mississippi 1950–2013. Available at: http://www.srh.noaa.gov/jan/?n=gen_tor_stats, accessed April28, 2013
- Oscar TP. A Quantitative risk assessment model for Salmonella and whole chickens. Int J Food Microbiol 2004;93:231–247 [DOI] [PubMed] [Google Scholar]
- Palisade Corporation. @Risk 4.0: A New Standard in Risk Analysis. Ithaca, NY: Palisade Corporation, 2011. Available at: http://www.palisade.com/risk [Google Scholar]
- Patz JA, Olson SH, Uejio CK, Gibbs HK. Disease emergence from global climate and land use change. Med Clin N Am 2008;92:1473–1491 [DOI] [PubMed] [Google Scholar]
- Petrescu C, Suciu O, Ionovici R, Herbarth O, Franck U, Schlink U. Respiratory health effects of air pollution with particles and modification due to climate parameters in an exposed population: Long and short term study. Int J Energy Environ 2011;1:102–112 [Google Scholar]
- Rose JB, Epstein PR, Lipp EK, Sherman BH, Bernard SM, Patz JA. Climate variability and change in the United States: Potential impacts on water and foodborne diseases caused by microbiologic agents. Environ Health Perspect 2001;109(Suppl 2):211–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell R, Paterson M, Lima N. How will climate change affect mycotoxins in food? Food Res Int 2010;43:1902–1914 [Google Scholar]
- SAS Institute Inc. SAS User's Guide: Statistics Version 9.2 ed. Cary, NC: SAS Institute Inc., 2010 [Google Scholar]
- Semenza JC, Menne B. Climate change and infectious diseases in Europe. Lancet Infect Dis 2009;9:365–375 [DOI] [PubMed] [Google Scholar]
- Sheffield PE, Landrigan PJ. Global climate change and children's health: Threats and strategies for prevention. Environ Health Perspect 2011;119:291–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SigmaPlot; version 13. Chicago: SYSTAT Software, Inc., 2009 [Google Scholar]
- Southeast Regional Climate Center. Available at: http://www.sercc.com/climateinfo/monthly_seasonal.html, accessed March15, 2012
- Tajkarimia M, Ibrahimb SA, Fraserc AM. Food safety challenges associated with traditional foods in Arabic speaking countries of the Middle East. Trends Food Sci Technol 2013;29:116–123 [Google Scholar]
- Tauxe RV. Emerging foodborne pathogens. Int J Food Microbiol 2002;78:31–41 [DOI] [PubMed] [Google Scholar]
- Taylor E, Kastner J, Renter D. Challenges involved in the Salmonella Saintpaul outbreak and lessons learned. 2009. Available at: http://krex.k-state.edu, accessed May2013 [DOI] [PubMed] [Google Scholar]
- Tennessee Department of Health, Communicable Disease Interactive Data. Available at: http://health.state.tn.us/ceds/WebAim/WEBAim_criteria.aspx, accessed March6, 2012
- Valero A, Hervás C, García-Gimeno RM, Zurera G. Product unit neural network models for predicting the growth limits of Listeria monocytogenes. Food Microbiol 2007;24:452– 464 [DOI] [PubMed] [Google Scholar]
- Ward Systems Group. 1993 NeuroShell 2 User's Manual. Frederick, MD: Ward Systems Group, Inc., 1993. [Google Scholar]
- [WHO] World Health Organization—Food Safety Report. 2011. Available at: http://www.who.int/foodsafety/en/, accessed January25, 2014 [Google Scholar]
- Zhang G, Brown EW González-Escalona N. Comparison of real-time PCR, reverse transcriptase real-time PCR, loop-mediated isothermal amplification, and the FDA conventional microbiological method for the detection of Salmonella spp. in produce. Appl Environ Microbiol 2011;77:6495–6501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Bi P, Hiller J. Climate variations and salmonellosis transmission in Adelaide, South Australia: A comparison between regression models. Int J Biometeorol 2008;52:179–187 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Peng B, Hiller JE. Climate variations and Salmonella infection in Australian subtropical and tropical regions. Sci Total Environ 2010;408:524–530 [DOI] [PubMed] [Google Scholar]