Abstract
Background
Theory-based sexual risk reduction interventions are often demonstrated effective, but few studies have examined the mechanisms that mediate their behavior changes. In addition, critical contextual factors, such as alcohol use, are often not accounted for by social cognitive theories and may add to the explanatory value of intervention effects. The purpose of this study is to examine the underlying mechanisms driving condom use following a brief sexual risk reduction intervention grounded in the Information, Motivation, Behavioral Skills (IMB) model of behavior change. We examined IMB theoretical constructs and alcohol-related contextual factors as potential mediators in separate models.
Methods
Patients (n=617) from an STI clinic in Cape Town, South Africa were randomly assigned to either a brief risk reduction intervention or an education-only control condition. We assessed information, motivation, behavioral skills, and alcohol-related variables at baseline, 3, 6, 9, and 12 months and modeled IMB constructs and alcohol-related factors as mediators of behavior change.
Results
Results of growth-curve mediational modeling showed that one year after counseling, the intervention indirectly affected sexual risk behavior through alcohol-related constructs, but not IMB constructs.
Conclusions
Alcohol use and related factors play critical roles in explaining HIV and STI risk reduction intervention effects. Interventions that directly address alcohol use as a factor in sexual risk behavior and behavior change should be the focus of future research.
Keywords: HIV/AIDS, sexual risk, condom use, mediational modeling
HIV prevention interventions that promote condom use and safer sexual risk behavior are most effective when grounded in theories of health behavior change, such as Social Cognitive Theory (Patterson et al., 2008), and the Theory of Planned Behavior (Hightow-Weidman et al., 2012). Among the most widely used conceptual frameworks in HIV prevention is the Information-Motivation-Behavioral Skills (IMB) Model (Anderson et al., 2006; Cornman, et al., 2007; Fisher et al., 1994; Fisher & Fisher, 1992; Kalichman et al., 2005; Robertson et al., 2006). The IMB model proposes that HIV prevention behaviors, particularly condom use, is determined as a function of one’s information about the behavior, one’s motivation to change the behavior, and possession of the behavioral skills necessary to engage in the behavior. In the model, information, motivation, and behavioral skills each have a direct impact on behavior. Information and motivation are also hypothesized to have an indirect impact on behavior through behavioral skills.
Beyond the intra-personal constructs of information, motivation and behavioral skills, it is widely known that contextual factors, such as self and partner alcohol use, contribute substantially to behavior and behavior change (e.g., Ewart, 1991; Rhodes, 2002). Alcohol consumption is closely associated with engaging in unprotected sexual behaviors, and places individuals at particularly high risk for sexually transmitted infection (STI), including HIV (Kalichman et al., 2007; Morojele et al., 2006; Weinhardt & Carey, 2000). Alcohol use increases sexual risks via a number of mechanisms, including reducing social and sexual inhibitions, risky alcohol-outcome expectancies, and the psychogenic effects of alcohol on decision-making (Cook & Clark, 2005). Thus, alcohol use may inhibit healthy risk behavior changes including condom use. In addition, in sociocultural contexts where alcohol use is prevalent or normative, alcohol use likely mediates risk behavior changes through mechanisms that are not accounted for in the IMB model.
South Africa is one region where there is a confluence of both prevalent HIV and hazardous alcohol use. There are 5.6 million people living with HIV in South Africa, more than any other country in the world (UNAIDS, 2011). The HIV prevalence in Cape Town, South Africa’s second largest city, is 13%. In addition, South Africa exhibits a high prevalence of hazardous drinking among men and women who consume alcohol. South African drinkers consume an average of 20 liters of alcohol per year, a rate among the highest in the world (Parry, 2005). Sexually transmitted infection (STI) clinic patients in South Africa are therefore among the highest priority populations for HIV prevention in the world.
In the current study we examine conceptual and contextual mechanisms of behavior change resulting from a theory-based sexual risk reduction intervention. We utilized data from a recent randomized clinical trial of an IMB model-based intervention designed to increase condom use among STI clinic patients (Kalichman et al., 2011). In this study men and women receiving STI clinic services were randomized to either an IMB model-based single 60-minute risk reduction counseling session or a 20-minute HIV/STI information/education session. The IMB intervention demonstrated significant increases in condom use as well as reductions in subsequent STI. However, the mechanisms that may account for safer behavior in this study have not been previously reported. For this study we tested two mediation models to examine the impact of the intervention on condom use. In one model we examined IMB constructs and in the other model we examined alcohol-related contextual factors as potential behavior change mechanisms. Our aim was to determine the theoretical and contextual factors most influential in accounting for the intervention outcomes.
Method
Participants and Setting
Participants were 414 men and 203 women receiving STI clinic services at one of the largest public STI clinics in Cape Town. The patient population is approximately 25% women and 90% indigenous (Black) Africans and approximately half of all patients have previously received STI services. The estimated HIV prevalence is 25% of clinic patients based on reactive tests among the approximately 50% of patients who accept HIV testing.
Participant Recruitment and Enrollment
The sample and trial have been described elsewhere (Kalichman et al., 2011). Briefly, the criteria for referral to the study were that the patient was age 18 or older and was being seen at the clinic for STI diagnostic or treatment services. Patients who elected to enroll in the study were scheduled for a baseline assessment and counseling session in which they received informed consent, a computerized baseline assessment and a single counseling session.
Study Design and Procedures
Immediately following the baseline assessment, participants were randomly assigned to receive either: (a) the experimental 60-minute behavioral skills building HIV risk reduction counseling session; or (b) the 20-minute HIV information/educational control intervention. Participants were scheduled for follow-up assessments 3, 6, 9 and 12-months after counseling. The clinical trial is registered with ClinicalTrials.gov (NCT01242501). Both U.S. and South African institutional review boards approved all of the study procedures.
Intervention Conditions
Brief Theory-based HIV Risk Reduction Skills Counseling Intervention
The experimental intervention was grounded in the IMB model of behavior change (Fisher & Fisher, 1992). As described elsewhere (Kalichman et al., 2007), the information component of the counseling (20 minutes) reviewed facts about HIV transmission and risk behaviors; discussed the local prevalence of HIV; clarified misconceptions; dispelled myths about AIDS; and described HIV antibody testing. Once participants reviewed how people contract HIV, attention turned to their own personal risks for HIV infection. The motivation component (20 minutes) integrated motivational counseling techniques that included motivation for change and strengthening commitment to change. Addressing alcohol use as a risk factor was embedded within the motivational counseling component. The intervention included the World Health Organization’s (WHO) brief alcohol counseling model as the basis for the alcohol risk reduction (Babor et al., 1994; Hall et al., 1993). Personal risks were discussed to induce change readiness and enhance intentions to change behavior. The final component of the risk reduction counseling was behavioral self-management and sexual communication skills building (20 minutes). Counselors engaged participants in a functional analysis of their risk by having individuals discuss personal risk situations and identify cues related to their sexual risks. Behavioral rehearsal was conducted in role-plays to enhance risk reduction skills. Correct male and female condom use was also instructed and modeled allowing participants to practice condom application on wooden anatomical models with corrective feedback from the counselor. Finally, participants created personalized goals and risk reduction plans that they took with them.
HIV Information/Education-Only Control
The control condition was an HIV/STI education counseling session that consisted of the same 20 minutes that was included in the first part of the experimental intervention. This session represents a didactic educational experience similar to that used in past research (Kamb et al., 1998; Metcalf et al., 2005).
Measures
All measures were administered using computerized interviews at the baseline, 3, 6, 9, and 12-month follow-up assessments in English and Xhosa, the two languages spoken by nearly all clinic patients.
Descriptive Information
Participants reported their age, gender, education, ethnicity, marital status, and other basic demographic information.
IMB Constructs
Information
To assess HIV risk and prevention-related knowledge, we used items adapted from a measure reported by Carey and Schroder (2002) (example, “Can a person get AIDS by sharing kitchens and bathrooms with someone who has AIDS?”). Participants responded Yes, No, or Don’t Know. The test was scored for the number of correct responses, with Don’t Know responses scored incorrect, expressed as the percent correct (Kuder-Richardson 20 coefficient = .71).
Motivation
Motivation was assessed using an eight-item measure of condom use intentions (example, “I will talk with my partner about condoms”). Items were responded to on a 4-point response scale, 1 = I will definitely not do this, to 4 = I will definitely do this. Items were scored for mean responses, with higher scores indicating greater motivation (α = .82).
Behavioral Skills
Defined as the personal sense of confidence that one can perform specific behaviors under specified conditions, self-efficacy is commonly used as a proxy for behavioral skills (Bandura, 1977; 1997). The current self-efficacy scale consisted of six items (example, “I am confident about suggesting using condoms with a new sex partner”). Items were responded to on a 4-point response set, 1 = Disagree, 4 = Agree, scored for mean responses, with higher scores indicating stronger self-efficacy (α = .69).
Alcohol Use Contextual Factors
Alcohol Use
Participants also completed the AUDIT, a 10-item self-report instrument that includes quantity and frequency of alcohol use that was designed to identify individuals for whom the use of alcohol places them at risk for developing alcohol problems (Conigrave et al., 1995; De Silva et al., 2008).
Alcohol Use in Sexual Contexts/Sex with Alcohol
Participants indicated in open format the number of times that they drank alcohol, defined as beer, wine, or other alcoholic beverages before sex in the previous month.
Alcohol Outcome Expectancies
We adapted an alcohol outcome expectancy measure from items used in previous research (Aarons et al., 2003; Brown et al., 1980; 1987). The scale includes nine items that reflect expected sexual enhancement and expected loss of control following drinking (example, “I am a better sex partner after I have been drinking”), responded to on 4-point scales, 1 = Strongly disagree, to 4 = Strongly agree (α = .90).
Intervention Outcomes
Sexual Behavior
Participants responded to items assessing their vaginal and anal intercourse with and without condoms in the previous month. A 30-day (one month) retrospective period was selected because previous research has shown reliable reports of numbers of partners and sexual events over this time period (Napper et al., 2010). Participants were instructed to think back over the past month and estimate the number of sex partners and number of sexual occasions in which they practiced each behavior. Responses were made using open formats to record continuous frequencies of occurrences. We also calculated the percentage of intercourse occasions protected by condoms using the ratio [condom protected vaginal + condom protected anal intercourse / total vaginal + total anal intercourse].
Data Management and Analysis
We analyzed the data in stages. First, we examined the data descriptively in SPSS. Then, models were tested in Amos Version 19 statistical software. We modeled the data using latent growth curve models because we had potential time varying constructs (i.e., the constructs were assessed at 3, 6, 9, and 12 months following the intervention) that needed to be statistically controlled. Following traditional growth curve modeling techniques, the growth curve models (GCMs) we tested included two latent variables to model the intercept and the slope for each construct. The indicators for each latent variable were the measured time varying variables from each of the four time points following baseline assessment (i.e., 3, 6, 9, and 12 months). We first modeled four independent growth curves, one for each IMB construct and the outcome: information, motivation, behavioral skills, and sexual risk behavior. This allowed us to examine intercept means and variances in the constructs at each time point, and slope means and variances across time. Given that participants received the HIV risk reduction intervention or the educational control following baseline but before 3, 6, 9, and 12 months assessments, and therefore perhaps disrupted linear growth in the constructs, we did not include baseline assessments in the independent growth curves. After testing the independent growth curves for each construct and obtaining acceptable model fit, we examined our mediational process model using 12-month data.
We examined how the intervention affected sexual risk behavior (i.e., percent protected intercourse) by conducting mediational analyses. Specifically, we examined the indirect effect of the intervention on the behavioral outcome through information, motivation, and behavioral skills. A mediational process occurs when an initial variable significantly predicts intervening, or mediating variables (i.e., mediators); this path(s) is known as the a path(s). Further, to have significant mediation the mediators must significantly predict an outcome variable; this path(s) is known as the b path(s). The resulting indirect effect is known as c’ and is the product of the a and b paths. To test for significant indirect effects we used the bootstrapping technique (Bollen & Stine, 1990; Shrout & Bolger, 2002), a nonparametric method of computing a sampling distribution by re-sampling with replacement over many trials. We bootstrapped 2,000 samples with a bias-corrected 95% confidence interval. In order to conduct bootstrapping there must be no missing data. Therefore, we imputed missing values using stochastic regression imputation.
We tested whether the intervention had an indirect effect on sexual risk behavior through information, motivation, and behavioral skills one year after the intervention. For the current research questions, we only wanted to examine relations between levels of the constructs at each time point (i.e., intercepts), and not relations between or with changes in the constructs (i.e., slopes). Therefore, we only examined associations between intercepts in our modeling and did not examine associations with or between slopes. To test for direct and indirect effects of the intervention on the behavioral outcome, we included intervention as a dichotomous exogenous variable predicting the intercepts of the proposed mediators information, motivation, and behavioral skills, and the intercept of the outcome sexual risk behavior. As per the IMB model, we also modeled direct paths from the intercepts of information, motivation, and behavioral skills to the intercept of the behavioral outcome, as well as indirect paths of the intercepts of information and motivation on behavior through behavioral skills. We allowed for correlations between the residuals of measurements taken at the same time point (3, 6, 9, and 12 months). Importantly, we controlled for baseline assessment by having baseline levels predict both the intercept and slope for each construct. Descriptive statistics for all measures are reported in Table 1.
Table 1.
Summary statistics for IMB constructs, alcohol constructs, and sexual risk behavior by time of assessment.
| Baseline | 3 months | 6 months | 9 months | 2 months | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Range | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Information (proportion) | 0-1 | 0.77 | 0.20 | 0.85 | 0.15 | 0.85 | 0.17 | 0.85 | 0.18 | 0.84 | 0.18 |
| Motivation | 1-4 | 3.41 | 0.60 | 3.59 | 0.51 | 3.63 | 0.49 | 3.59 | 0.55 | 3.63 | 0.55 |
| Behavioral Skills | 1-6 | 3.83 | 2.14 | 4.73 | 1.93 | 4.85 | 1.83 | 4.91 | 1.81 | 4.95 | 1.79 |
| Alcohol Expectancies | 1-4 | 1.81 | 0.85 | 1.59 | 0.80 | 1.63 | 0.87 | 1.62 | 0.85 | 1.63 | 0.87 |
| Alcohol Use | 0-40 | 7.48 | 7.82 | 4.23 | 6.29 | 3.79 | 5.75 | 3.60 | 5.75 | 3.07 | 5.22 |
| Sex with Alcohol | 0- | 1.39 | 4.53 | 0.50 | 2.21 | 0.47 | 1.58 | 0.55 | 1.73 | 0.40 | 1.22 |
| Protected Intercourse (proportion) | 0-1 | 0.70 | 0.36 | 0.91 | 0.23 | 0.89 | 0.24 | 0.91 | 0.22 | 0.90 | 0.25 |
Model fit was assessed using comparative fit index (CFI; Bentler, 1990) and root-mean-square error of approximation (RMSEA; Hu & Bentler, 1999).When standardized estimates were possible we also assessed fit using the standardized root mean square residual (SRMR; Jöreskog & Sörbom, 1978). Good fit is indicated by a CFI greater than 0.95, RMSEA less than 0.05, and SRMR less than .08 (Hu & Bentler, 1999; Kline, 2010).
Results
Preliminary analyses regarding flow of participants through the trial and differences between the intervention and control group have been reported by Kalichman and colleagues (Kalichman et al., 2011). There were no differences between participants in the intervention and control group on any demographic characteristics or outcome variables assessed at baseline.
Single IMB-Construct Growth Curve Models
The growth curve model for information fit the data well, χ2 (2) = .14, p =.94, CFI=1.00, RMSEA=.00, SRMR=.00. This model showed that the slope, Ms = −.006, t = −3.81, p <.001 for information was significantly different from 0; there was a significant change in participants’ AIDS knowledge over time. Specifically, knowledge appeared to decrease slightly over time. There was also significant variance in the slope, Ds = .002, t =4.11, p <.001; there were significant differences between individuals in the change in knowledge over time.
We examined means and variances in the intercept of information at 3, 6, 9 and 12 months. As can be seen in Table 2, the means and variances in the intercept at each time point were significantly different from zero. At 3 months participants answered an average of 86% of AIDS-related knowledge questions correctly, 85% correctly at 6 and 9 months and 84% correctly at 12 months. There were individual differences in the levels of knowledge at each assessment.
Table 2.
IMB constructs and sexual risk behavior intercept means and variances at 12 months.
| Intercept Mean | Intercept Variance | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| M | t | p | D | t | p | |
| IMB Constructs | ||||||
| Information | 0.84 | 116.67 | <.001 | 0.03 | 11.82 | <.001 |
| Motivation | 3.62 | 181.96 | <.001 | 0.15 | 5.10 | <.001 |
| Behavioral Skills | 4.97 | 72.84 | <.001 | 1.77 | 4.65 | <.001 |
| Alcohol Constructs | ||||||
| Alcohol Expectancies | 1.63 | 48.19 | <.001 | 0.71 | 10.37 | <.001 |
| Alcohol Use | 3.13 | 15.59 | <.001 | 23.06 | 8.44 | <.001 |
| Sex with Alcohol | 0.41 | 8.91 | <.001 | −0.36 | −1.48 | 0.14 |
| % Protected Sex | 0.90 | 103.76 | <.001 | 0.04 | 5.39 | <.001 |
The growth curve model for motivation fit the data well, χ2 (2) = 6.37, p =.04, CFI=.99, RMSEA=.06, SRMR=.001. The slope for motivation did not differ from 0, Ms = 0.008, t =1.19, p=.23; there was no change in motivation over time. Also, there was not significant variance in the slope, Ds = −.001, t = −.08, p =.94. The means and variances in the intercept at each time point were significantly different from zero (see Table 2). At 3 months participants expressed strong motivation to use condoms (3.6 out of 4) and levels of motivation did not differ across time. There were significant between participant differences in motivation at each assessment.
The model for behavioral skills fit the data well, χ2 (2) = .67, p =.72, CFI=1.00, RMSEA=.00, SRMR=.00. The slope in behavioral skills was significantly different from zero, Ms = .07, t =2.66, p <.01; there was an increase in skills over time. There was not significant variation in the slope, Ds = 0.07, t =.98, p =.33; participants did not differ in in their individual change in behavioral skills across time. The means and variances shown in Table 2 in the intercept of behavioral skills were significantly different from zero. At 3 months, participants had moderate-high behavioral skills (average score 4.76 out of 6), at 6 months the mean in skills increased to 4.83, then 4.90 at 9 months, and at 12 months participants scored an average of 4.97 in behavioral skills. There were significant individual differences in skills at each assessment.
Finally, the model for percent of intercourse occasions protected by condoms fit the data well, χ2 (2) = 5.57, p =.99, CFI=1.00, RMSEA=.05, SRMR=.001. The model showed that the slope did not differ significantly from zero, Ms = .00, t =.89, p =.89; there was no change in percent protected intercourse over time. There was not significant variation between individuals in the slope, Ds = .002, t =1.85, p =.07. The means and variances in the intercept of percent protected intercourse were significantly different from zero at all time points (see Table 2). At 3 months, participants reported an average of 91% condom protected sex acts, and this did not change significantly over time. There were also significant between participant differences for percent protected intercourse at each assessment. In sum, we were able to examine associations between the intercepts for the IMB constructs and risk behavior intercourse at all time points.
IMB Mechanisms of Behavior Change
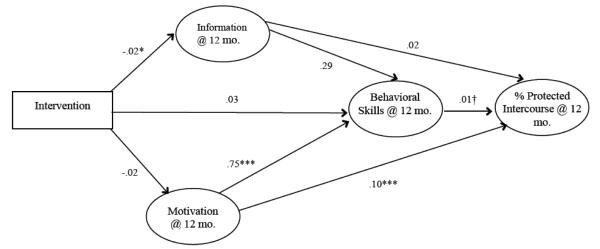
Based on the acceptable model fits for the individual constructs, we proceeded to examine an IMB mediational process model for data at 12 months (Figure 1). The model fit the data well (χ2 (177) = 227.83, p <.001, CFI =.98, RMSEA =.03). The intervention significantly predicted information. The direction of the intervention effect was opposite of what we would have predicted, but consistent with findings from the main outcome analyses (Kalichman et al., 2011). Participants who received the HIV risk reduction intervention reported less AIDS-related knowledge than participants in the education-only control group. Apart from an effect on information, the intervention did not significantly predict the intercepts in motivation, behavioral skills, or the behavioral outcome percent protected intercourse. Also, information did not significantly predict behavioral skills nor the behavioral outcome. Therefore, the results showed that there was a significant a path from the intervention to the intercept of information, but there was a non-significant b path from information to the behavioral outcome. This precludes any examination of a mediating effect of the intervention on percent protected intercourse through information. The results also showed that there were non-significant a paths from the intervention to motivation and behavioral skills. Thus, this precludes any examination of mediating effects of motivation and behavioral skills of the intervention on the behavioral outcome. We did however find associations between motivation, behavioral skills, and behavior.
Figure 1.
IMB mechanisms at 12 months.
Motivation positively predicted behavioral skills, indicating that those with higher levels of motivation also had more behavioral skills. In addition, motivation and behavioral skills both positively predicted the behavioral outcome, although the effect of behavioral skills on risk reducing behavior was marginally significant (p <.10). Participants with higher levels of motivation and behavioral skills also had a higher percentage of condom-protected intercourse. There was a marginal indirect effect of motivation on percent protected intercourse through behavioral skills, Estimate= .008, SE=.006, 95% CI= −.001 to .02, p = .07. The squared multiple correlation was .06. Therefore, the model accounted for a range of 6% one year after counseling.
Single Alcohol-Construct Growth Curve Models
The growth curve model for alcohol expectancies fit the data well, χ2 (2) = .95, p =.62, CFI=1.00, RMSEA=.00, SRMR=.00. The slope in alcohol expectancies was not significantly different from zero, Ms = .01, t =1.40, p = .16; there was not a change in expectancies across all participants on average over time. There was significant variation in the slope, Ds = 0.02, t =2.13, p <. 05; participants differed in their individual change in alcohol expectancies across time.
As shown in Table 2, the means and variances in the intercept of alcohol expectancies were significantly different from zero. At 3 months, participants had low alcohol expectancies (average score 1.60 out of 4), and on average this level of expectancies did not change over time. There were significant individual differences in alcohol expectancies at each assessment.
The growth curve model for alcohol use fit the data well, χ2 (2) = 1.22, p =.54, CFI=1.00, RMSEA=.00, SRMR=.00. The slope in alcohol use was significantly different from zero, Ms = −.37, t = −6.36, p <.001; average alcohol use decreased over time. There was not significant variation in the slope, Ds = 0.39, t =0.75, p =.45; participants did not differ in their individual change in alcohol use across time. The means and variances in the intercept of alcohol use were significantly different from zero at all time points (see Table 2). At 3 months, on average participants engaged in a low amount of alcohol use (average score 4.24 out of 40), at 6 months the mean was 3.87, at 9 months the mean was 3.50, and at 12 months the mean of alcohol use across participants was 3.13. There were significant individual differences in levels of alcohol use at each assessment.
The growth curve model for alcohol in sexual contexts fit the data well, χ2 (2) = 3.74, p =.15, CFI=1.00, RMSEA=.04, SRMR=.00. The slope in sex with alcohol was significantly different from zero, Ms = −.04, t = −2.10, p <.05; average alcohol use in sexual contexts decreased over time. There was also significant variation in the slope, Ds = −0.37, t =-5.56, p < .001; participants differed in their individual change in alcohol use in sexual contexts across time.
Table 2 shows the means and variances in the intercept of alcohol use in sexual contexts at each time point. At 3, 6, 9, and 12 months, the means in the intercepts significantly differed from zero. At 3 months, participants had an average of less than one episode of alcohol use in a sexual context (M=.54), at 6 months the mean for sex with alcohol was 0.50, 0.45 at 9 months, and 0.41 at 12 months. At 3 and 12 months, the variance in the intercept of sex with alcohol did not significantly differ from zero. That is, we only found significant individual differences in levels of alcohol use in sexual contexts at 6 and 9 months. Therefore, we were able to examine associations with the intercept of sex with alcohol only at these time points.
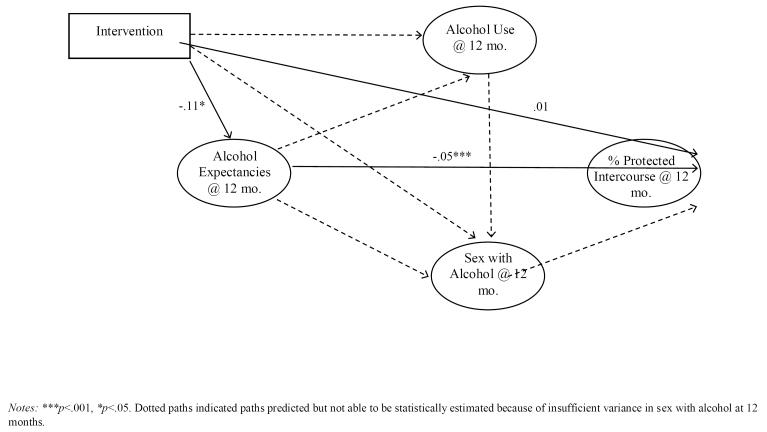
Alcohol Mechanisms of Behavior Change
We found acceptable model fits for the individual alcohol constructs and proceeded to examine an alcohol expectancies and alcohol use mediational process model (Figure 2). We had hypothesized that the intervention had an indirect effect on percent protected intercourse through alcohol expectancies, alcohol use, and alcohol use in sexual contexts. However, there was no variance across participants in alcohol use in sexual contexts at 12 months, therefore we could not examine this variable in the model. Further, preliminary analyses showed that the intervention did not significantly affect alcohol use. Thus, the model we tested was one in which the intervention had a direct effect on percent condom use and an indirect intervention effect through alcohol expectancies. This model fit the data well, χ2 (149) = 633.58, p <.001, CFI =.93, RMSEA = .07. The intervention had a significant effect on alcohol expectancies; participants who received the HIV risk reduction intervention had significantly less risky alcohol expectancies than participants in the control group. Participants who had more risky expectancies from drinking reported a lower percentage protected intercourse. We assessed the indirect effect of the intervention on sexual risk behavior through alcohol expectancies. Indeed, there was a significant indirect effect, Estimate= .006, SE=.003, 95% CI= .001 to .012, p = .016 indicating that at 12 months, the intervention still affected alcohol expectancies, which in turn influenced sexual risk reduction behavior.
Figure 2.
Alcohol mechanisms at 12 months.
Discussion
The purpose of this study was to examine the underlying mechanisms driving protective sexual behaviors following a theory-based sexual reduction counseling intervention among STI patients in Cape Town, South Africa. We first examined IMB constructs as mechanisms of sexual risk behavior change and found that the IMB constructs did not significantly mediate the intervention effects. Growth curve modeling allowed us to examine changes in IMB constructs over the course of the study. We found that information/knowledge slightly reduced whereas behavioral skills increased over time across all participants. It is possible that recall of the didactic information on HIV/AIDS taught to participants diminished over the year, while participants improved in skills as they continued to practice safer behavior. We also found that the intervention did not have the predicted effects on information, motivation, or behavioral skills; thus, these constructs could not account for the significant effect on condom-protected intercourse. Instead, we found that the intervention indirectly affected sexual risk behavior through alcohol-related contextual factors. Thus, while the IMB model provides a useful framework for designing behavior change interventions, there is limited evidence that IMB constructs account for observed behavior changes. Our results also support previous studies that identified alcohol use as a significant factor in sexual risk behaviors, and have suggested alcohol use supersedes social cognitive constructs in explaining behavior change (Weinhardt & Carey, 2000). These findings have important implications for future HIV prevention interventions.
The IMB model-based intervention we examined significantly reduced risky alcohol-outcome expectancies relative to the control condition. In turn, less risky expectancies predicted less alcohol use in sexual contexts, as well as more condom use. The fact that alcohol-related variables were more useful in explaining our intervention effect on sexual risk behavior than IMB constructs has implications for HIV risk reduction counseling. Whereas alcohol use is known to be a robust correlate and predictor of sexual risk behavior, particularly in South Africa (Kalichman et al., 2007; Weinhardt & Carey, 2000). Thus, our study suggests that HIV prevention should directly address alcohol expectancies in relation to sexual contexts.
The results of this study should be interpreted in light of its limitations. Relative to other cities in southern Africa, Cape Town is better resourced. Also, the trial was conducted in one STI clinic a Cape Town. Therefore, the generalizability of the current findings may be limited. The study findings are also limited by relying on self-reported sexual and alcohol use behaviors, which are sensitive to socially desirable responding. The rates of sexual risk and alcohol use behaviors in this study may therefore have been suppressed and should be considered lower-bounds. Also, we used self-efficacy as a proxy for behavioral skills rather than a direct assessment of skills. With these constraints in mind, we believe that brief HIV risk reduction counseling for STI patients has the potential to prevent HIV infections and can be maximized by directly addressing alcohol-associated contextual and cognitive factors.
The results of the current study contribute to the growing literature on effectiveness single session brief interventions to reduce HIV risk (Eaton et al., 2012). Thus, brief interventions should potentially be scaled-up, particularly in resource poor settings and areas where HIV prevalence is high, like South Africa. Importantly, our results also show that the effectiveness of this brief risk reduction counseling intervention may have been driven by alcohol-related contextual and cognitive factors. Based on our results, as well as others’, we believe that HIV prevention interventions may limit AIDS-related information/education and concentrate on motivation and factors related to motivation. This study further suggests that interventions focused primarily on motivation may be useful only after directly intervening on risk-related alcohol use. Theoretical frameworks that encompass contextual/environmental as well as cognitive and behavioral factors, such as Ewart’s (1991) Social Action Theory and Bandura’s (1997) Social Cognitive Theory, may prove more useful in accounting for sexual risk behavior change. With very limited resources in poor community clinics, time must be prioritized to address the most critical correlates of risk reduction behaviors, like risky alcohol outcome expectancies and alcohol use in sexual contexts.
Acknowledgments
National Institutes of Health grant R01-MH074371-04 supported this research. Preparation of this manuscript was supported by a National Institute on Drug Abuse K01 Mentored Career Development Award (K01 DA036447-01) awarded to the first author.
Footnotes
Conflict of Interest Statement All of the authors (EVP, SCK, RG, DC, LAE, & LCS) declare that they have no conflicts of interest.
References
- Aarons GA, Goldman MS, Greenbaum PE, Coovert MD. Alcohol expectancies: integrating cognitive science and psychometric approaches. Addictive Behaviors. 2003;28(5):947–961. doi: 10.1016/s0306-4603(01)00282-9. [DOI] [PubMed] [Google Scholar]
- Anderson ES, Wagstaff DA, Heckman TG, Winett RA, Roffman RA, Solomon LJ, Sikkema KJ. Information-Motivation-Behavioral Skills (IMB) Model: testing direct and mediated treatment effects on condom use among women in low-income housing. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 2006;31(1):70–79. doi: 10.1207/s15324796abm3101_11. doi:10.1207/s15324796abm3101_11. [DOI] [PubMed] [Google Scholar]
- Babor TF, Grant M, Acuda W, Burns FH, Campillo C, Del Boca FK, Machona M. A randomized clinical trial of brief interventions in primary care: summary of a WHO project. Addiction (Abingdon, England) 1994;89(6):657–660. doi: 10.1111/j.1360-0443.1994.tb00944.x. discussion 660–678. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura Albert. Self-Efficacy: The Exercise of Control. 1st ed Worth Publishers; 1997. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Stine R. Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological methodology. 1990;20(1):15–140. [Google Scholar]
- Brown SA, Christiansen BA, Goldman MS. The Alcohol Expectancy Questionnaire: an instrument for the assessment of adolescent and adult alcohol expectancies. Journal of Studies on Alcohol. 1987;48(5):483–491. doi: 10.15288/jsa.1987.48.483. [DOI] [PubMed] [Google Scholar]
- Brown SA, Goldman MS, Inn A, Anderson LR. Expectations of reinforcement from alcohol: their domain and relation to drinking patterns. Journal of Consulting and Clinical Psychology. 1980;48(4):419–426. doi: 10.1037//0022-006x.48.4.419. [DOI] [PubMed] [Google Scholar]
- Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2002;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conigrave KM, Hall WD, Saunders JB. The AUDIT questionnaire: choosing a cut-off score. Addiction. 1995;90(10):1349–1356. doi: 10.1046/j.1360-0443.1995.901013496.x. [DOI] [PubMed] [Google Scholar]
- Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sexually Transmitted Diseases. 2005;32(3):156–164. doi: 10.1097/01.olq.0000151418.03899.97. [DOI] [PubMed] [Google Scholar]
- Cornman DH, Schmiege SJ, Bryan A, Joseph Benziger T, Fisher JD. An information-motivation-behavioral skills (IMB) model-based HIV prevention intervention for truck drivers in India. Social Science & Medicine. 2007;64(8):1572–1584. doi: 10.1016/j.socscimed.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva P, Jayawardana P, Pathmeswaran A. Concurrent validity of the alcohol use disorders identification test (AUDIT) Alcohol and Alcoholism (Oxford, Oxfordshire) 2008;43(1):49–50. doi: 10.1093/alcalc/agm061. doi:10.1093/alcalc/agm061. [DOI] [PubMed] [Google Scholar]
- Eaton LA, Huedo-Medina TB, Kalichman SC, Pellowski JA, Sagherian MJ, Warren M, Johnson BT. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: implications for bundling prevention packages. American journal of public health. 2012;102(11):e34–44. doi: 10.2105/AJPH.2012.300968. doi:10.2105/AJPH.2012.300968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewart CK. Social action theory for a public health psychology. American Psychologist. 1991;46(9):931–946. doi: 10.1037//0003-066x.46.9.931. doi:10.1037/0003-066X.46.9.931. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13(3):238. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Fisher Jeffrey D., Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. doi:10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Hall W, Saunders JB, Babor TF, Aasland OG, Amundsen A, Hodgson R, Grant M. The structure and correlates of alcohol dependence: WHO collaborative project on the early detection of persons with harmful alcohol consumption--III. Addiction (Abingdon, England) 1993;88(12):1627–1636. doi: 10.1111/j.1360-0443.1993.tb02037.x. [DOI] [PubMed] [Google Scholar]
- Hightow-Weidman LB, Pike E, Fowler B, Matthews DM, Kibe J, McCoy R, Adimora AA. HealthMpowerment.org: Feasibility and acceptability of delivering an Internet intervention to young Black men who have sex with men. AIDS Care. 2012;24(7):910–920. doi: 10.1080/09540121.2011.647677. doi:10.1080/09540121.2011.647677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL IV: Analysis of linear structural relationships by the method of maximum likelihood. International Educational Services; 1978. [Google Scholar]
- Kalichman SC, Cain D, Eaton L, Jooste S, Simbayi LC. Randomized clinical trial of brief risk reduction counseling for sexually transmitted infection clinic patients in Cape Town, South Africa. American Journal of Public Health. 2011;101(9):e9–e17. doi: 10.2105/AJPH.2011.300236. doi:10.2105/AJPH.2011.300236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prevention Science: The Official Journal of the Society for Prevention Research. 2007;8(2):141–151. doi: 10.1007/s11121-006-0061-2. doi:10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndromes (1999) 2007;44(5):594–600. doi: 10.1097/QAI.0b013e3180415e07. doi:10.1097/QAI.0b013e3180415e07. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Malow R, Dévieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: Test of the information-motivation-behavior skills (IMB) model. Community mental health journal. 2005;41(3):277–290. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamb ML, Fishbein M, Douglas JM, Jr, Rhodes F, Rogers J, Bolan G, Peterman TA. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA: The Journal of the American Medical Association. 1998;280(13):1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. The Guilford Press; 2010. [Google Scholar]
- Metcalf CA, Douglas JM, Jr, Malotte CK, Cross H, Dillon BA, Paul SM, Peterman TA. Relative efficacy of prevention counseling with rapid and standard HIV testing: a randomized, controlled trial (RESPECT-2) Sexually Transmitted Diseases. 2005;32(2):130–138. doi: 10.1097/01.olq.0000151421.97004.c0. [DOI] [PubMed] [Google Scholar]
- Morojele NK, Kachieng’a MA, Mokoko E, Nkoko MA, Parry CDH, Nkowane AM, Saxena S. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Social Science & Medicine (1982) 2006;62(1):217–227. doi: 10.1016/j.socscimed.2005.05.031. doi:10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV Risk Behavior Self-Report Reliability at Different Recall Periods. AIDS and Behavior. 2010;14(1):152–161. doi: 10.1007/s10461-009-9575-5. doi:10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry CDH. South Africa: alcohol today. Addiction (Abingdon, England) 2005;100(4):426–429. doi: 10.1111/j.1360-0443.2005.01015.x. doi:10.1111/j.1360-0443.2005.01015.x. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, Strathdee SA. Efficacy of a Brief Behavioral Intervention to Promote Condom Use Among Female Sex Workers in Tijuana and Ciudad Juarez, Mexico. American Journal of Public Health. 2008;98(11):2051–2057. doi: 10.2105/AJPH.2007.130096. doi:10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T. The [] risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. [Google Scholar]
- Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: testing the Information-Motivation-Behavior Skills (IMB) model. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2006;38(1):18–25. doi: 10.1016/j.jadohealth.2004.08.013. doi:10.1016/j.jadohealth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological methods. 2002;7(4):422. [PubMed] [Google Scholar]
- Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research. 2000;11:125–157. [PMC free article] [PubMed] [Google Scholar]