Abstract
Study Objectives:
Parents of children with chronic illnesses have poorer health related quality of life (HRQoL), shorter sleep duration, and poorer sleep quality than parents of healthy children. However, night-to-night variability of sleep in parents has not previously been considered. This study compared the sleep patterns of parents of ventilator-assisted children (VENT) and healthy, typically developing children (HEALTHY), and examined the relationship between sleep variability and perceived HRQoL.
Methods:
Seventy-nine mothers and 33 fathers from 42 VENT families (n = 56) and 40 HEALTHY (n = 56) families completed the SF-36 and wore an actigraph for 2 weeks. Reported bedtime and wake time, along with actigraphic total sleep time (TST), wake after sleep onset (WASO), and sleep efficiency (SE) were examined using both average values and night-tonight instability (mean square successive differences).
Results:
VENT parents showed significantly later bedtimes, shorter TST, longer WASO, and lower SE than HEALTHY parents. VENT parents also exhibited greater instability in their reported wake time, WASO, and SE. Adjusting for family type and gender, greater instability of wake times, WASO and SE were related to poorer SF-36 subscale scores, while averaged sleep values were not.
Conclusions:
Many parents of ventilator-assisted children experience deficient sleep and show significant instability in their sleep, which was related to HRQoL. Similar to shift workers, variable sleep schedules that may result from caregiving responsibilities or stress may impact parental caregivers' health and well-being. Additional studies are needed to determine how support and other interventions can reduce sleep disruptions in parental caregivers.
Citation:
Meltzer LJ, Sanchez-Ortuno MM, Edinger JD, Avis KT. Sleep patterns, sleep instability, and health related quality of life in parents of ventilator-assisted children. J Clin Sleep Med 2015;11(3):251–258.
Keywords: parental caregivers, ventilator-assisted children, sleep, quality of life
Advances in medical technology have resulted in more ventilator-assisted children being discharged from the hospital to the home,1,2 with over 8,000 children in the United States requiring mechanical ventilation.3 Caring for a child with a chronic illness goes above and beyond normal parenting, adding frequent medical procedures, medication administration, and illness specific stressors (e.g., medical appointments, dealing with insurance). Parents of children with chronic illnesses have higher rates of depression and anxiety,4–11 poorer physical health and shorter life expectanc y,12,13 as well as significantly worse health related quality of life (HRQo L).14–17 Furthermore, shortened or disrupted sleep (from nocturnal caregiving responsibilities or stress related to the child's health) has been repor ted,16,18–21 with associations found between HRQoL and s leep.14–16 However, previous studies have not included an objective measure of sleep patterns, relying instead on subjective reports, which can be biased (caregiver reporting on their own quality of sleep and quality of life). In addition, few studies have quantitatively assessed the sleep and health of parents with ventilator-assisted children.
Unpredictable and variable nocturnal caregiving also contributes to erratic sleep patterns. For families of ventilator-assisted children, many of whom have limited (if any) night nursing su pport,19,22–24 parents may be required to be alert throughout the night on some nights, but not others.25 An association between greater night-to-night instability in sleep and poorer health outcomes has been found in shift-work nurses and patients with in somnia.26–28 Notably, a study of caregivers of dementia patients found greater objective night-to-night instability in sleep duration and quality compared to non-car egivers.29 Objective night-to-night sleep instability, however, has not been previously examined in pediatric parental caregivers.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Parental caregivers of children with chronic illnesses are known to have shorter sleep duration and poorer quality sleep, as well as poorer health related quality of life (HRQOL). However, objective sleep patterns, night-to-night variability in sleep, and the relationship between sleep and HRQOL have not been previously examined in this population.
Study Impact: This study has shown that in families with ventilator-assisted children, parent sleep is not only shorter, but more variable. Further, the instability in sleep patterns was significantly related to multiple aspects of HRQOL. Because of the high demands places on parental caregivers in terms of medical care for their children, increased support, including nursing and/or respite care, is needed to improve the quantity and quality of parent sleep.
The aim of this study was to explore differences in sleep between parents of ventilator-assisted children and parents of healthy children, as well as whether there is a relationship between objective sleep patterns (including night-to-night sleep instability) and health-related quality of life (HRQoL) in parents of children with and without ventilator-assistance. Specific study questions were: (1) Do objective sleep patterns differ between parents of ventilator-assisted children and parents of healthy, typically developing children? (2) Do parents of ventilator-assisted children show more night-to-night instability in their sleep patterns than parents of healthy, typically developing children? (3) Do parents of ventilator-assisted children have poorer HRQoL than parents of healthy, typically developing children? (4) Are objectively measured sleep patterns related to HRQoL?
METHODS
Overview
Families of children (4–17 years) were identified through multiple sources: VENT families were identified through three programs that provide medical care, case management, education, and support for families (Pennsylvania Ventilator Assisted Children's Home Program, Children's Hospital of Philadelphia Technology Dependence Center, and Children's of Alabama Home Ventilator Program); HEALTHY families were identified through peer nomination and community newspaper advertisements. Exclusion criteria were a diagnosed sleep disorder or limiting chronic health condition (e.g., chronic pain), night shift worker, non-English speaking, or a child with a diagnosed chronic illness or developmental disorder that would interfere with sleep (HEALTHY group only).
Potential participants received a letter and a telephone call to screen for eligibility. The primary caregiver was identified and invited to participate in the study. If 2 parents lived in home, both were invited (and encouraged) to participate. During a home visit, participants completed the SF-36 and were taught to use the actigraph. The actigraph was returned with a second home visit or by a pre-paid shipping package. Data were collected between October 2008 and May 2011. Data were not collected during summer months (June through August), as typical sleep patterns can change when children are not in school.30
This study was approved by the Institutional Review Board at The Children's Hospital of Philadelphia, the University of Alabama at Birmingham, and National Jewish Health.
Measures
Sleep Patterns
All participants wore an actigraph (Motionlogger Sleep Watch, Ambulatory Monitoring Inc., Ardsley, NY) for 14 consecutive days/nights on their non-dominant wrist, pressing an event marker button at bedtime (time attempted to fall asleep) and wake time (final waking time to start the day). Participants kept a daily sleep diary used for scoring and artifact removal. Data were recorded in 1-minute epochs (Action-W software).31 Sleep variables measured were reported bedtime and wake time, total sleep time (TST, minutes scored as sleep between actigraphic sleep onset and offset), wake after sleep onset (WASO, minutes of wake after actigraphic sleep onset), and sleep efficiency (SE, time from bedtime to wake time divided by TST, reported as a percent). Approximately 9% of nights were not scored due to artifact or participants not wearing the device. There were no differences between the groups in the number of nights scored.
Health Related Quality of Life
The SF-36 is a multi-purpose, short-form health survey that assesses physical, social, and emotional well-being in 8 dimensions (physical functioning, role physical, bodily pain, general health perceptions, vitality, social functioning, role emotional, and mental health).32–34 Higher scores indicate better quality of life. The SF-36 has demonstrated adequate reliability and validity,32,34 and has been normed on large representative samples, including caregivers.35
Data Analyses
A power analysis was conducted based on our previous study of sleep in parents of children with chronic illnesses.18 Results showed that with power set at 0.80 and α = 0.01, a sample size of 35 per group was required to detect a difference in total sleep time.
Differences between the 2 family groups in sociodemo-graphic characteristics were examined using t-tests for continuous data and χ2 tests for categorical data.
We used multilevel models (MLMs) for analyzing sleep variables, accounting for multiple levels of nesting in our study design. Nightly observations of sleep were nested within individuals (parents) and parents were nested within families, with families classified into 2 groups: VENT or HEALTHY. MLMs assume that observations at the lower level are not independent (e.g. observations of sleep across nights for the same subject are not entirely independent of each other and neither are observations of sleep for members of the same family).36,37 We ran a series of 3-level models (level 1: sleep variable; level 2: individuals; level 3: family) to test differences between VENT and HEALTHY families on bedtime, wake time, TST, WASO, and SE. Data distributions for each sleep variable were inspected for normality, with transformed WASO and SE (WASO: log to the base of ten transformation of (WASO+0.5); SE: the arcsine square-root transformation) used in the MLMs. Gender was included as a covariate due to known gender differences in sleep.38,39 Analyses were conducted with the MIXED procedure in SPSS v.15.0.
To examine the night-to-night instability of each sleep variable, a series of successive differences were created by calculating differences among adjacent observations within the same subject (e.g. night 2 – night 1, night 3 – night 2, etc.).40 Since some of the successive differences were negative, these values were squared for subsequent analyses.40 The square successive differences (SSDs) can be used to compute a mean square successive difference (MSSD) as follows:
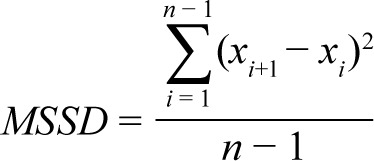 |
The MSSD is considered to be an index of variability/instability, similar to the intra-individual variance of a series of observations. However, the MSSD is considered to be more sensitive to fluctuations across successive observations.40
In order to compare differences in night-to-night instability of sleep between VENT and HEALTHY families, we used generalized MLMs (PROC GLIMMIX in SAS v.9). Since our repeated measures (the SSDs for each individual) showed a positively skewed distribution, they were modelled with a generalized MLM with a gamma error distribution and log link.40 Therefore, we conducted a series of 3-level generalized MLMs (level 1: SSDs of the sleep variable; level 2: individuals; level 3: families) to examine group differences in the instability of each sleep variable.
To explore group differences on HRQoL, we used the individuals' scores on the SF-36 (dependent variable: scores on the SF-36 dimensions; independent variable: family type). For questionnaire data that came from the same family (which may be interdependent), we considered scores from the same family as repeated observations, with gender included in the model to distinguish between the two family members (PROC MIXED in SAS v.9).41 SF-36 dimensions were not transformed to approach normality, since it has been suggested that SF-36 scores should be analyzed using straightforward parametric tests.42
Finally, the same procedure was used to explore the association between HRQoL and both the average and the MSSD of each sleep variable (data from each individual within a family were considered as repeated observations from the family unit). SF-36 dimensions were considered as the dependent variable, and each sleep variable (e.g. average SE, MSSD of SE) was the predictor, adjusting for family type and gender (PROC MIXED in SAS v.9).
Analyses were considered statistically significant if p ≤ 0.05. All statistical tests were interpreted as exploratory, rather than probative, so corrections for multiple comparisons were not employed.43,44
RESULTS
Participants
To reach our sample size of ≥ 35 families per group, a total of 172 families of children aged 4–17 years were invited to participate in the study (98 families of ventilator-assisted children [VENT] and 74 families of children without a chronic illness [HEALTHY]). Ninety families were not included (37 were never reached [27 VENT], 26 were determined to be ineligible [6 VENT], 20 declined to participate stating they were too busy [20 VENT], 2 withdrew due to the child becoming ill during the study [1 VENT], and 5 either had actigraph failures or did not wear the actigraph as instructed, resulting in < 5 nights of scorable data [2 VENT]), resulting in the final sample of 82 families (42 VENT and 40 HEALTHY; 79 mothers and 33 fathers). There were no differences in group, child age, or gender between families enrolled and not enrolled.
We obtained data from both parents in 30 families (13 VENT). In the vast majority of the remaining families (n = 52), sleep data were obtained only from the mother (94.2%). The results of generalized MLMs indicated that there were not statistically significant differences in sleep instability between families with 2 parents participating in the study and families with just one parent participating (all p > 0.05). However, with respect to mean sleep values, the results of the MLMs did show that WASO was lower in families where 2 family members participated in the study (p = 0.04).
Parents were 28 to 58 years old (mean = 42.5, SD = 7.0), 80% white, and 62% had a college or post-graduate degree (Table 1 provides complete demographic information). Children were 4 to 17 years old (mean = 10.7, SD = 4.6), 73% white, and 56% male. As can be seen in Table 1, the two family groups, VENT (n = 42) and HEALTHY (n = 40), were not significantly different on the majority of demographic variables, with the exception of education, with HEALTHY mothers having more years of education than VENT mothers, F1,77 = 10.1, p = 0.002. In addition all fathers were married (vs. 78.5% of mothers), χ2(1) = 8.4, p = 0.004, and fathers were more likely to be engaged in full-time work than mothers (84.8% of fathers vs. 35.4% of mothers), χ2(2) = 23.3, p < 0.001. For all families the mother was identified as the primary caregiver.
Table 1.
Demographic variables for families of ventilator-assisted children (VENT) and healthy comparison children (HEALTHY).
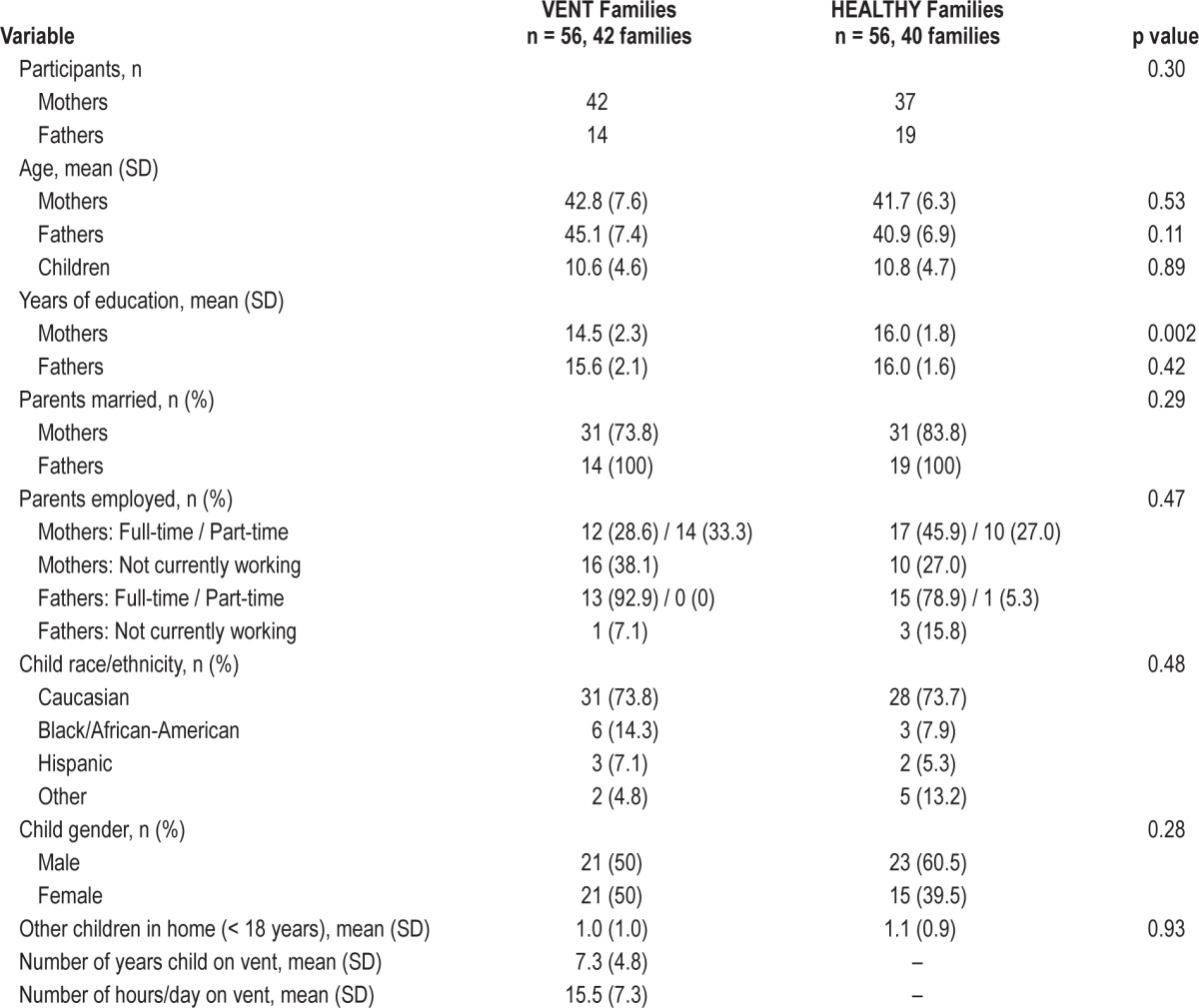
Among the VENT children, 30 were invasively ventilated while 12 were noninvasively ventilated. In terms of nursing coverage, 18 families received > 80 h/week and 24 received ≤ 80 h/week.
Question 1: Do sleep patterns differ between VENT and HEALTHY parents?
We scored 1,435 nights of data from 112 participants (mean = 12.81 nights, SD = 1.87). Means and the MSSDs of the sleep variables are presented in Table 2. VENT parents had significantly later bedtimes, significantly shorter TST, longer WASO, and lower SE than HEALTHY parents (Table 3). Gender and gender * family type were not statistically significant in any model, indicating no differences between mothers and fathers of VENT and HEALTHY children for mean sleep measures.
Table 2.
Mean values and night-to-night instability variables by family type.
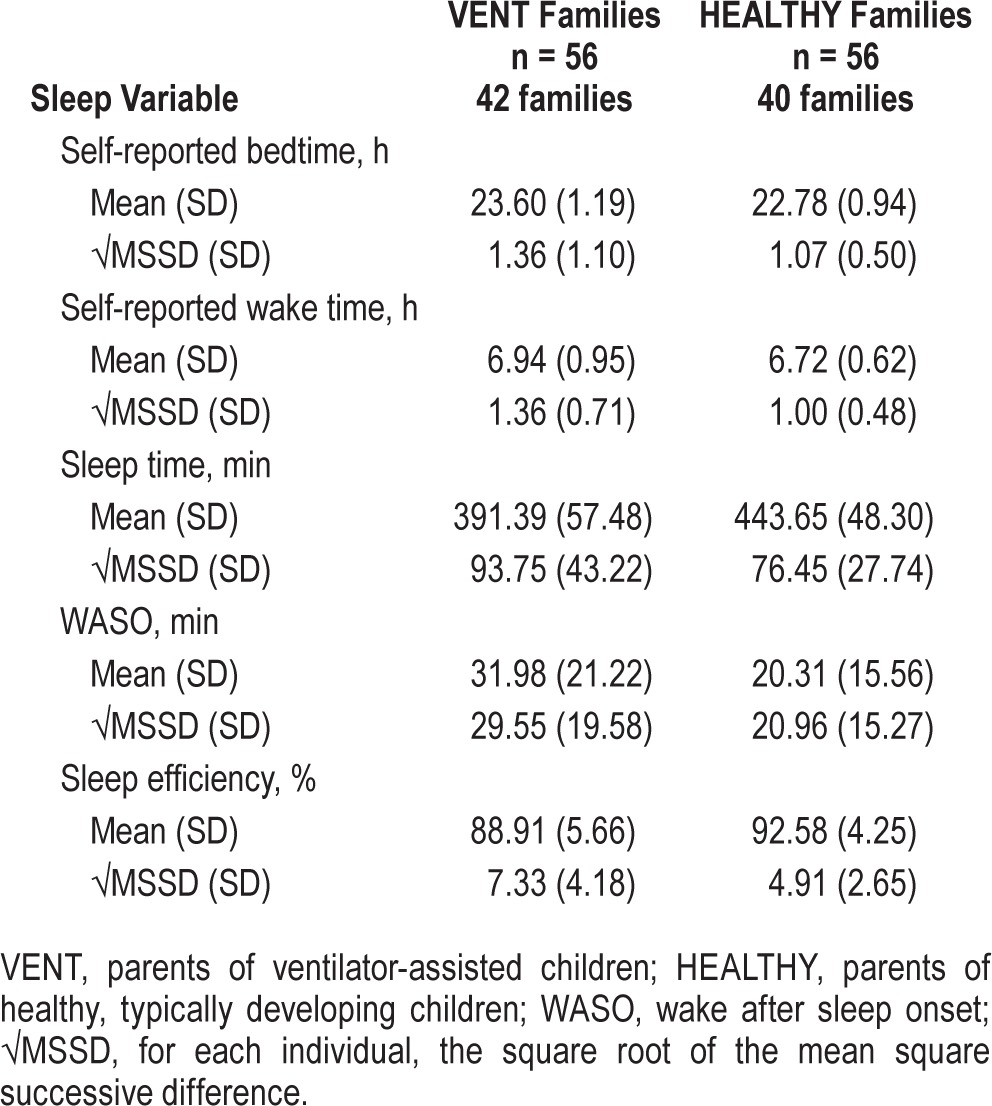
Table 3.
Multilevel models of the relationship between family type (VENT vs. HEALTHY) and sleep-related variables, adjusted for gender (n = 112).
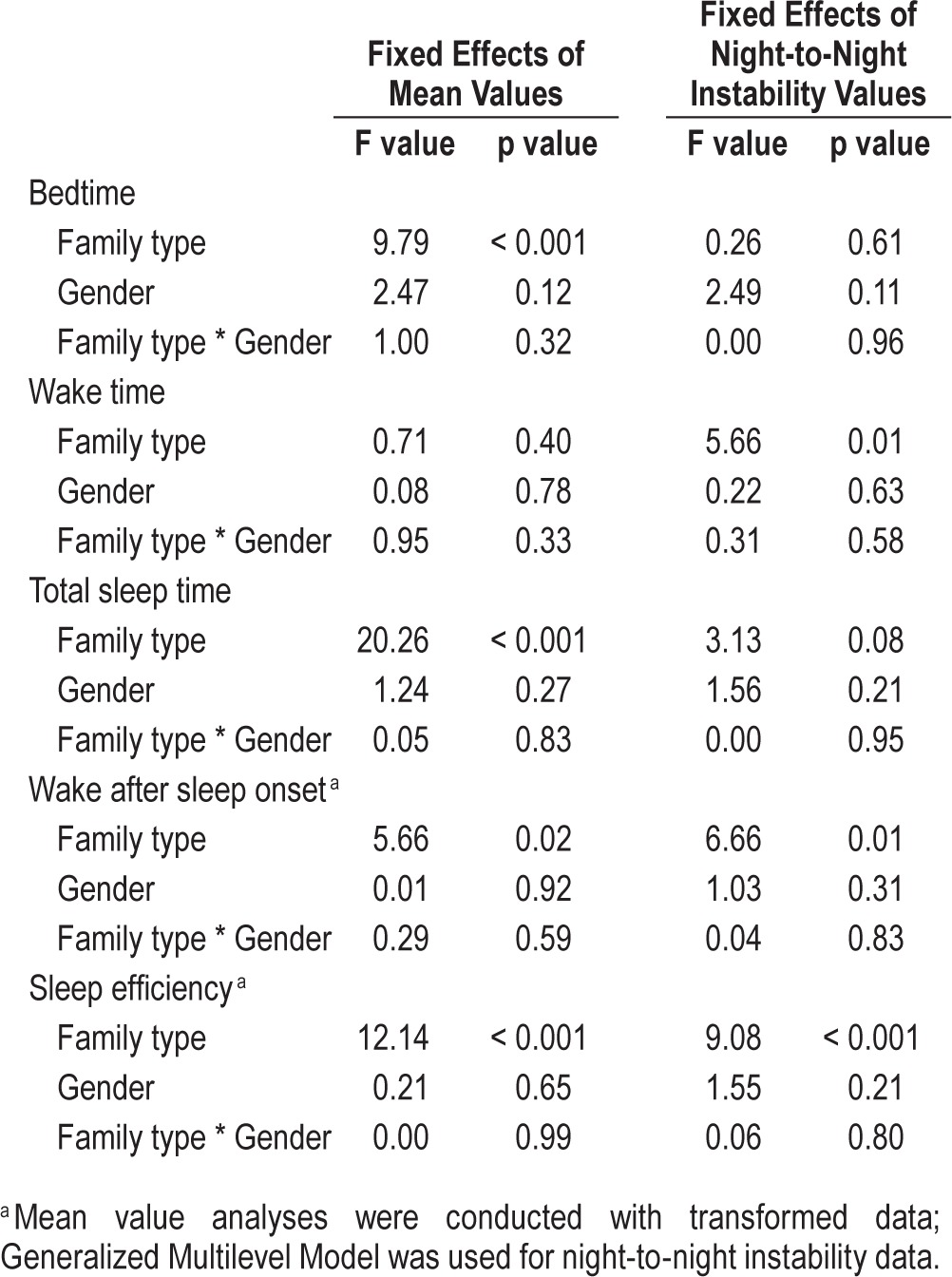
Question 2: Do VENT parents show more night-tonight instability in their sleep patterns than HEALTHY parents?
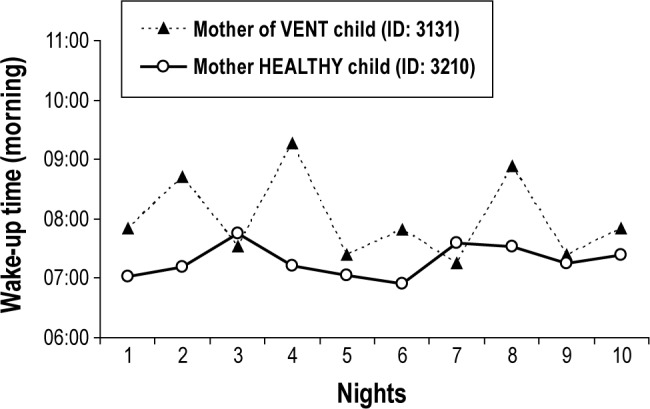
VENT parents showed significantly greater instability in their wake time, WASO, and SE across nights than did the HEALTHY parents (Tables 2 and 3). Figure 1 illustrates such a result. This figure shows the night-to-night self-reported wakeup times from a mother of a VENT child and from a mother of a HEALTHY child for the first 10 nights of recording. The 2 mothers were relatively age matched (40 and 36 years old, respectively). In both cases, the mother and the father of the family participated in the study and both families had a child younger than 12 years old. This figure shows that the mother of the VENT child exhibits more dramatic changes in her wakeup times across nights than the mother of the HEALTHY child. Gender and gender * family type were not statistically significant in any model, indicating no differences between mothers and fathers of VENT and HEALTHY children for mean sleep measures.
Figure 1. Wake-up times across nights for two age- and gender-matched parents.
To explore whether variables such as having a child who is invasively ventilated vs. noninvasively ventilated (Invasive) or the absence vs. presence of regular home nursing support (Support; i.e., ≤ 80 h vs. > 80 h/week) would contribute to the higher sleep instability seen in WASO, sleep efficiency, and wake time across time within parents of VENT children, we conducted further analyses within the VENT families group. The results of the 2 sets of generalized MLMs, using Invasive and Support as predictors of sleep instability, indicated that neither having an invasively ventilated child nor having < 80 h/week of home nursing support was significantly associated with higher instability in WASO (F = 0.10, p = 0.76; and F = 1.29, p = 0.25, respectively), sleep efficiency (F = 0.25, p = 0.62; and F = 0.05, p = 0.83, respectively), or wake time (F = 0.44, p = 0.51; and F = 0.02, p = 0.90, respectively).
Question 3: Do VENT parents have poorer HRQoL than HEALTHY parents?
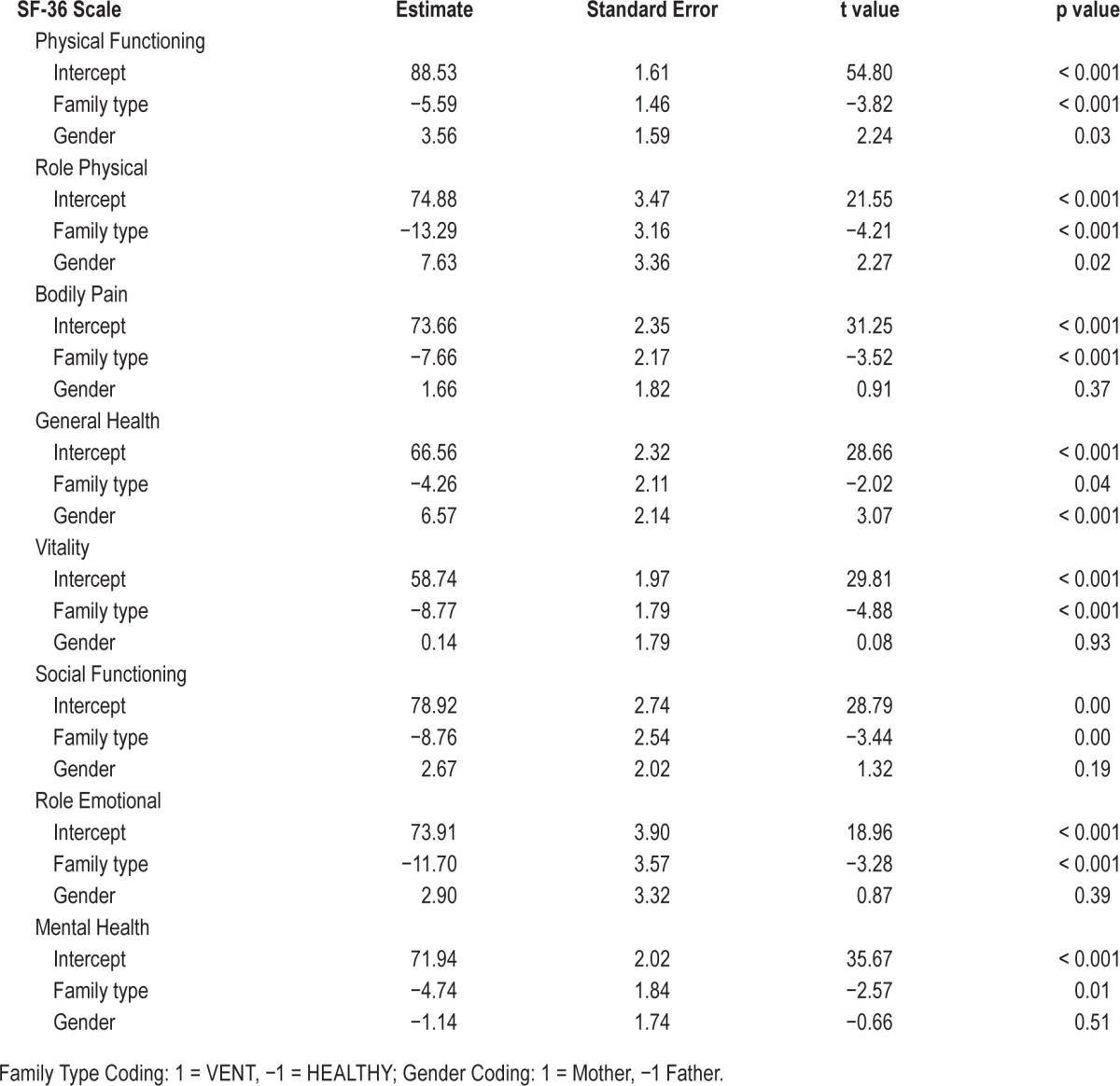
The effects of family type on the scores of the SF-36 dimensions are displayed in Table 4. Because we used effect coding for our categorical variables (family type and gender) for these analyses, the intercept in the models is the grand mean of all of the observations in the specific SF-36 dimension. The estimate for family type is equal to the difference between the mean of the group coded 1 (VENT) and the grand mean. The negative estimates for family type indicate that VENT parents had statistically significant lower scores (poorer HRQoL) than HEALTHY parents across all SF-36 dimensions.
Table 4.
Effect of family type (VENT and HEALTHY) on the 8 subscale scores of the SF-36 adjusting for gender (n = 112).
Question 4: Are sleep patterns related to HRQoL?
Adjusting for family type and gender, none of the averaged values for bedtime, wake time, TST, WASO, or SE showed a statistically significant relationship with any of the SF-36 dimensions. By contrast, higher instability in wake time across the study period was related to worse scores on Physical Functioning (b = −1.60, standard error [SE] = 0.81, t = −1.97, p = 0.05), Bodily Pain (b = −2.24, SE = 0.97, t = −2.30, p = 0.02), and General Health (b = −2.49, SE = 1.03, t = −2.41, p = 0.01). Higher instability of WASO across nights was also related to worse scores on Bodily Pain (b = −0.003, SE = 0.001, t = −2.11, p = 0.03). Higher instability of SE across nights was associated to worse scores on Role Emotional (b = −0.10, SE = 0.05, t = −2.1, p = 0.04). These negative regression coefficients in -dicate the amount of decrease in the SF-36 scores for each one point increase in the MSSD of the sleep variables.
DISCUSSION
This study is one of the first to objectively demonstrate that parents of ventilator-assisted children have shorter sleep duration and greater night-to-night instability in sleep quality and wake times compared to parents of healthy, typically developing children. To our knowledge this is also the first study to show an association between night-to-night instability of sleep and HRQoL in parental caregivers of ventilator-assisted children.
Similar to studies that only used self-reported sleep measures,15,16,18,19 VENT parents in this study averaged ∼6.5 hours of sleep, almost a full hour less than HEALTHY parents (7.4 h). Thus many VENT parents obtain deficient sleep (< 7 h sleep per night),45 which can result in poorer daytime functioning, decreased alertness, and increased negative mood.45–47 However, in our study, we did not find that shorter sleep duration was directly related to worse HRQoL.
The unpredictability of nocturnal caregiving likely contributes to caregiver stress.9,48,49 Further, nocturnal caregiving typically increases when the child is sick (also contributing to caregiver stress) or if there is intermittent or no night nursing coverage.25 Unfortunately our data did not allow for a separate examination of night nursing vs. total nursing hours, thus we were not able to examine this issue directly. However, it is likely that our findings of more variability in objective sleep measures (greater night-to-night instability in WASO and SE) and self-reported wake-up times for parents of VENT children was due to required nocturnal caregiving (which was qualitatively reported by most families). Notably, the sleep instability in parents of VENT children was significantly related to multiple dimensions of HRQoL. Thus for caregivers of children with chronic illness, inconsistent sleep patterns could play an important role in poorer health outcomes, even more so than average sleep duration over time.
The day-to-day experience of parental caregivers is not unlike that of medical professionals who may work extended or rotating shifts, including intermittent nights. In studies of both physicians and nurses, who are highly trained medical professionals, performance is negatively impacted after extended or rotating shifts,50,51 which can result in increased medical errors.52,53 Further, health outcomes have been shown to be negatively affected by night work and rotating shift work in nurses.28,54 Thus, further research is needed with parental caregivers to examine the role of variable sleep schedules and nighttime caregiving on medical decision making, fulfillment of responsibilities, and parent health outcomes.28,55–57
Notable strengths of this study compared to previous research include the relatively large sample size, the inclusion of both mothers and fathers (n = 30 families), and the use of a control group. In addition, the objective measure of sleep patterns reduces the bias inherent in self-report measures. There are also a number of limitations to this study. First, while we found a relationship between sleep and HRQoL, our study results should be considered descriptive and the cross-sectional design precludes causal conclusions. Thus to confirm these results, additional studies are needed, as well as studies that utilize a longitudinal design. Second, the study sample was heterogeneous (broad age range and variety of medical diagnoses). This limited our ability to control for either children's ages or diagnoses. Finally, ∼40% of families were not reached or declined to participate, which may limit the generalizability of the study results. However, as being too busy was the only reason given by those who declined, our study may underestimate the relationship between caregiver sleep and HRQoL, as those who were unreachable or too busy to participate might also be too busy to sleep.
CONCLUSIONS
This study highlights the importance of considering parental sleep and daytime functioning in families with ventilator-assisted children. In addition, our results suggest that consideration of sleep variability may provide new perspectives on the role of sleep in caregiver health and well-being. Because of the important service that parental caregivers provide, additional research is needed with this population to confirm these findings in larger samples, as well as further elucidate the relationship between caregiving, sleep, and health outcomes, including the role of different types of support (e.g., increased nursing, respite care) and/or interventions (e.g., cognitive-behavioral strategies to address non-caregiving sleep disturbances) for parental caregivers.
DISCLOSURE STATEMENT
This study was funded by NIH K23 MH077662 (LJM) and a fellowship award from Fundación Séneca, Región de Murcia, Spain (MMSO). The authors have indicated no financial conflicts of interest. The work was performed at the Children's Hospital of Philadelphia, Children's of Alabama, and National Jewish Health.
ACKNOWLEDGMENTS
The authors thank the all of the wonderful families who took the time to participate in this study; the Pennsylvania Ventilator Assisted Children's Home Program, the Children's Hospital of Philadelphia Technology Dependence Center, and the Children's of Alabama Home Ventilator Program for their assistance with the recruitment of families of ventilator-assisted children; Devon Ambler, Jocelyn Thomas, and Kelly Ann Davis for their assistance with data collection; and Anne Kazak and Carole Marcus for their mentorship with this project.
REFERENCES
- 1.Feudtner C, Villareale NL, Morray B, et al. Technology-dependency among patients discharged from a children's hospital: a retrospective cohort study. BMC Pediatr. 2005;5:8. doi: 10.1186/1471-2431-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amin R, Sayal P, Syed F, et al. Pediatric long-term home mechanical ventilation: twenty years of follow-up from one Canadian center. Pediatr Pulmonol. 2014;49:816–24. doi: 10.1002/ppul.22868. [DOI] [PubMed] [Google Scholar]
- 3.Boroughs D, Dougherty J. Care of the ventilator-dependent child in the home: a 30-year experience. American Thoracic Society International Conference, Denver, CO. American Thoracic Society Project Committee: Pediatric Chronic Home Ventilation Guidelines Workshop.2011. [Google Scholar]
- 4.Breslau N, Staruch KS, Mortimer EA., Jr Psychological distress in mothers of disabled children. Am J Dis Child. 1982;136:682–6. doi: 10.1001/archpedi.1982.03970440026007. [DOI] [PubMed] [Google Scholar]
- 5.Silver EJ, Bauman LJ, Weiss ES. Perceived role restriction and depressive symptoms in mothers of children with chronic health conditions. J Dev Behav Pediatr. 1999;20:362–9. doi: 10.1097/00004703-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Mulhern RK, Fairclough DL, Smith B, et al. Maternal depression, assessment methods, and physical symptoms affect estimates of depressive symptomatology among children with cancer. J Pediatr Psychol. 1992;17:313–26. doi: 10.1093/jpepsy/17.3.313. [DOI] [PubMed] [Google Scholar]
- 7.Kovacs M, Iyengar S, Goldston D, et al. Psychological functioning among mothers of children with insulin-dependent diabetes mellitus: a longitudinal study. J Consult Clin Psych. 1990;58:189–95. doi: 10.1037//0022-006x.58.2.189. [DOI] [PubMed] [Google Scholar]
- 8.Jennings P. Caring for a child with a tracheostomy. Nurs Standard. 1990;4:24–6. doi: 10.7748/ns.4.30.24.s36. [DOI] [PubMed] [Google Scholar]
- 9.Kirk S. Families' experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev. 1998;24:101–14. doi: 10.1046/j.1365-2214.1998.00043.x. [DOI] [PubMed] [Google Scholar]
- 10.Toly VB, Musil CM, Carl JC. Families with children who are technology dependent: normalization and family functioning. West J Nurs Res. 2012;34:52–71. doi: 10.1177/0193945910389623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim KR, Lee E, Namkoong K, et al. Caregiver's burden and quality of life in mitochondrial disease. Pediatr Neurol. 2010;42:271–6. doi: 10.1016/j.pediatrneurol.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Brehaut JC, Kohen DE, Raina P, et al. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004;114:e182–91. doi: 10.1542/peds.114.2.e182. [DOI] [PubMed] [Google Scholar]
- 13.Raina P, O'Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115:e626–36. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- 14.Klassen AF, Klaassen R, Dix D, et al. Impact of caring for a child with cancer on parents' health-related quality of life. J Clin Oncol. 2008;26:5884–9. doi: 10.1200/JCO.2007.15.2835. [DOI] [PubMed] [Google Scholar]
- 15.Read J, Simonds A, Kinali M, et al. Sleep and well-being in young men with neuromuscular disorders receiving non-invasive ventilation and their carers. Neuromuscul Disord. 2010;20:458–63. doi: 10.1016/j.nmd.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Feeley CA, Turner-Henson A, Christian BJ, et al. Sleep quality, stress, caregiver burden, and quality of life in maternal caregivers of young children with bronchopulmonary dysplasia. J Pediatr Nurs. 2014;29:29–38. doi: 10.1016/j.pedn.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hatzmann J, Heymans HS, Carbonell A, et al. Hidden consequences of success in pediatrics: parental health-related quality of life--results from the Care Project. Pediatrics. 2008;122:e1030–8. doi: 10.1542/peds.2008-0582. [DOI] [PubMed] [Google Scholar]
- 18.Meltzer LJ, Mindell JA. Impact of a child's chronic illness on maternal sleep and daytime functioning. Arch Intern Med. 2006;166:1749–55. doi: 10.1001/archinte.166.16.1749. [DOI] [PubMed] [Google Scholar]
- 19.Heaton J, Noyes J, Sloper P, et al. The experiences of sleep disruption in families of technology-dependent children living at home. Children Soc. 2006;20:196–208. [Google Scholar]
- 20.Andrews MM, Nielson DW. Technology dependent children in the home. J Pediatr Nurs. 1988;14:111–51. [PubMed] [Google Scholar]
- 21.Kuster PA, Badr LK, Chang BL, et al. Factors influencing health promoting activities of mothers caring for ventilator-assisted children. J Pediatr Nurs. 2004;19:276–87. doi: 10.1016/j.pedn.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 22.Jardine E, O'Toole M, Paton JY, et al. Current status of long term ventilation of children in the United Kingdom: questionnaire survey. BMJ. 1999;318:295–9. doi: 10.1136/bmj.318.7179.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aday L, Wegener DH. Home care for ventilator-assisted children: implications for the children, their families, and health policy. Child Health Care. 1988;17:112–20. doi: 10.1207/s15326888chc1702_9. [DOI] [PubMed] [Google Scholar]
- 24.Gowans M, Keenan HT, Bratton SL. The population prevalence of children receiving invasive home ventilation in Utah. Pediatr Pulmonol. 2007;42:231–6. doi: 10.1002/ppul.20558. [DOI] [PubMed] [Google Scholar]
- 25.Meltzer LJ, Boroughs DS, Downes JJ. The relationship between home nursing coverage, sleep, and daytime functioning in parents of ventilator-assisted children. J Pediatr Nurs. 2010;25:250–7. doi: 10.1016/j.pedn.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kay DB, Dzierzewski JM, Rowe M, et al. Greater night-to-night variability in sleep discrepancy among older adults with a sleep complaint compared to noncomplaining older adults. Behav Sleep Med. 2013;11:76–90. doi: 10.1080/15402002.2011.602775. [DOI] [PubMed] [Google Scholar]
- 27.Suh S, Nowakowski S, Bernert RA, et al. Clinical significance of night-to-night sleep variability in insomnia. Sleep Med. 2012;13:469–75. doi: 10.1016/j.sleep.2011.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asaoka S, Aritake S, Komada Y, et al. Factors associated with shift work disorder in nurses working with rapid-rotation schedules in Japan: the nurses' sleep health project. Chronobiol Int. 2013;30:628–36. doi: 10.3109/07420528.2012.762010. [DOI] [PubMed] [Google Scholar]
- 29.Rowe MA, McCrae CS, Campbell JM, et al. Sleep pattern differences between older adult dementia caregivers and older adult noncaregivers using objective and subjective measures. J Clin Sleep Med. 2008;4:362–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Nixon GM, Thompson JM, Han DY, et al. Short sleep duration in middle childhood: risk factors and consequences. Sleep. 2008;31:71–8. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–7. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 33.McHorney CA, Ware JE, Jr, Lu JF, et al. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Ware JE., Jr SF-36 health survey update. Spine. 2000;25:3130–9. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 35.Rodrigue JR, Kanasky WF, Marhefka SL, et al. A psychometric normative database for pre-lung transplantation evaluations. J Clin Psychol Med S. 2001;8:229–36. [Google Scholar]
- 36.Peugh JL, DiLillo D, Panuzio J. Analyzing mixed-dyadic data using structural equation models. Struct Equ Modeling. 2013;20:314–37. [Google Scholar]
- 37.Atkins DC. Using multilevel models to analyze couple and family treatment data: basic and advanced issues. J Fam Psychol. 2005;19:98–110. doi: 10.1037/0893-3200.19.1.98. [DOI] [PubMed] [Google Scholar]
- 38.Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 39.Baker FC, O'Brien LM, Armitage R. Sex differences and menstrual-related changes in sleep and circadian rhythms. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia: Elsevier Saunders; 2005. [Google Scholar]
- 40.Jahng S, Wood PK, Trull TJ. Analysis of affective instability in ecological momentary assessment: indices using successive difference and group comparison via multilevel modeling. Psychol Methods. 2008;13:354–75. doi: 10.1037/a0014173. [DOI] [PubMed] [Google Scholar]
- 41.Campbell L, Kashy DA. Estimating actor, partner and interaction effects for dyadic data using PROC MIXED and HLM: a user-friendly guide. Pers Relatshp. 2002;9:327–42. [Google Scholar]
- 42.Torrance N, Smith BH, Lee AJ, et al. Analysing the SF-36 in population-based research. A comparison of methods of statistical approaches using chronic pain as an example. J Eval Clin Pract. 2009;15:328–34. doi: 10.1111/j.1365-2753.2008.01006.x. [DOI] [PubMed] [Google Scholar]
- 43.Proschan MA, Waclawiw MA. Practical guidelines for multiplicity adjustment in clinical trials. Control Clin Trials. 2000;21:527–39. doi: 10.1016/s0197-2456(00)00106-9. [DOI] [PubMed] [Google Scholar]
- 44.Bender R, Lange S. Adjusting for multiple testing--when and how? J Clin Epidemiol. 2001;54:343–9. doi: 10.1016/s0895-4356(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 45.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 46.Van Dongen HP, Maislin G, Mullington JM, et al. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 47.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 48.Meltzer LJ. Mothers of children with chronic illnesses: a caregiver burden model and summer camp as respite care. Dissertation Abstracts International: Section B: The Sciences and Engineering 63[10B], 4915. 2003 [Google Scholar]
- 49.Heaton J, Noyes J, Sloper P, et al. Families' experiences of caring for technology-dependent children: a temporal perspective. Health Soc Care Comm. 2005;13:441–50. doi: 10.1111/j.1365-2524.2005.00571.x. [DOI] [PubMed] [Google Scholar]
- 50.Arnedt JT, Owens J, Crouch M, et al. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294:1025–33. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 51.Rosenbluth G, Landrigan CP. Sleep science, schedules, and safety in hospitals: challenges and solutions for pediatric providers. Pediatr Clin North Am. 2012;59:1317–28. doi: 10.1016/j.pcl.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 52.Dorrian J, Lamond N, van den Heuvel C, et al. A pilot study of the safety implications of Australian nurses' sleep and work hours. Chronobiol Int. 2006;23:1149–63. doi: 10.1080/07420520601059615. [DOI] [PubMed] [Google Scholar]
- 53.Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3:e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liang G, Schernhammer E, Qi L, et al. Associations between rotating night shifts, sleep duration, and telomere length in women. PLoS One. 2011;6:e23462. doi: 10.1371/journal.pone.0023462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 56.Dorrian J, Lamond N, van den Heuvel C, et al. A pilot study of the safety implications of Australian nurses' sleep and work hours. Chronobiol Int. 2006;23:1149–63. doi: 10.1080/07420520601059615. [DOI] [PubMed] [Google Scholar]
- 57.Rosenbluth G, Landrigan CP. Sleep science, schedules, and safety in hospitals: challenges and solutions for pediatric providers. Pediatr Clin North Am. 2012;59:1317–28. doi: 10.1016/j.pcl.2012.09.001. [DOI] [PubMed] [Google Scholar]


