Abstract
The American Academy of Sleep Medicine (AASM) commissioned several Workgroups to develop quality measures for the care of patients with common sleep disorders, including adults with restless legs syndrome (RLS). Using the AASM process for quality measure development, the RLS Work-group developed three target outcomes for RLS management, including improving the accuracy of diagnosis, reducing symptom severity, and minimizing treatment complications. Seven processes were developed to support these outcomes. To achieve the outcome of improving accuracy of diagnosis, the use of accepted diagnostic criteria and assessment of iron stores are recommended. To realize the outcome of decreasing symptom severity, routine assessment of severity and provision of evidence-based treatment are recommended. To support the outcome of minimizing treatment complications, counseling about potential side effects and assessing for augmentation and impulse control disorders, when indicated, are recommended. Further research is needed to validate optimal practice processes to achieve best outcomes in adult patients with RLS.
Citation:
Trotti LM, Goldstein CA, Harrod CG, Koo BB, Sharon D, Zak R, Chervin RD. Quality measures for the care of adult patients with restless legs syndrome. J Clin Sleep Med 2015;11(3):293–310.
Restless legs syndrome (RLS), also referred to as Willis-Ekbom Disease (WED), is one of the most common sleep disorders, affecting between 5% and 10% of the United States population.1,2 RLS can adversely impact quality of life, disrupt sleep, impair daytime function, and impact mood.1,3–6 The delivery of high quality care for RLS depends on correct diagnosis, work-up for known comorbid conditions, delivery of appropriate evidence-based treatment, and follow up for treatment effectiveness and complications.7 These aspects of RLS care may be subject to substantial practice variation, presenting opportunities for quality improvement.
Ensuring quality healthcare is a priority within the American medical system. The promotion of high quality sleep care is central to the mission of the AASM, which seeks to “improve sleep health and promote high quality patient-centered care through advocacy, education, strategic research, and practice standards.”8 To this end, the AASM commissioned Workgroups to develop quality care measures aimed at optimizing care for patients suffering from the most common sleep-related disorders, including adults with RLS.9 These quality care measures focus on both outcomes, that is, what happens to a patient as a result of the care received, and processes, or the steps taken by a health-care provider in the care of an individual patient. Both outcomes and processes are important in the care of the patient. Outcomes are often more directly relevant to the patient, whereas processes tend to be less influenced by factors outside an individual provider's control. All RLS outcomes and processes detailed in this report were developed by the RLS Quality Measures Workgroup and received final approval from the AASM Quality Measures Task Force and the AASM Board of Directors.
METHODS
Literature Review
A comprehensive search was conducted to identify any publications that addressed both RLS and quality care. Both “restless legs syndrome” and “Willis-Ekbom” (and associated MeSH terms) were used, in conjunction with quality terms such as quality indicators, quality measure, quality assurance, outcome measurement/assessment, process measurement/assessment, validation, performance assessment, and best practices. A total of 257 articles were identified for review. An additional search was conducted to identify clinical practice guidelines, systematic reviews, and meta-analyses published by the AASM or other organizations or groups in the National Guidelines Clearinghouse, the National Quality Measures Clearinghouse, PubMed, and the Cochrane Library pertaining to RLS (and all associated MeSH terms). Searches were limited to articles published between 2002–2013, pertaining to humans, and in English. The Work-group performed subsequent “pearling,” where references from the searched articles were examined to identify any additional relevant evidence, as well as targeted searches on individual topics (e.g., RLS and impulse control) to provide background. These additional searches identified another 58 articles. The titles and abstracts of all articles were reviewed by Workgroup members and full articles of relevant publications were obtained and reviewed to identify and provide support for quality measures. The inclusion or exclusion of supporting evidence was determined by Workgroup consensus. In general, this search strategy yielded a substantial number of society guidelines, systematic reviews, and randomized controlled trials of RLS treatments, but specific work on quality outcomes or processes was scant. The present set of RLS quality measures was derived from a combination of evidence-based studies of RLS treatment, society guidelines, expert opinion, and consensus of the RLS Workgroup. Workgroup members graded the available evidence for the strength of association between the proposed process and the desired outcome using the grading scheme shown in Table 1.
Table 1.
Strength of association between process measure and desired outcome.

Measure Selection
The RLS Workgroup members individually created lists of five outcomes and up to five associated process measures, based on their clinical and research experience with RLS. The lists were compiled into a master list, from which the Workgroup jointly selected three outcomes and associated process measures. Through review of literature and discussion among the Workgroup and consultation with a larger group of AASM Quality Measures Workgroups, the RLS Workgroup further refined the outcomes and process measures. Pilot tests in the clinics of Workgroup members and feedback from stakeholders led to further revision of the measures. Per the recommendations of the AASM Quality Measures Task Force, one of the outcomes was converted into a quantitative outcome measure, such that the outcome could be systematically evaluated and tracked. The final set of measures consists of one quantitative outcome measure, two qualitative outcomes (i.e., quality of care goals), and seven process measures (see Figure 1). The technical specifications associated with each of these quality measures can be found in the Appendix. These specifications outline how to calculate an individual provider's performance in meeting these measures using a combination of diagnostic and CPT codes and chart review.
Figure 1. RLS quality measures driver diagram.
QUALITY MEASURES
Outcome 1 – Improve the Accuracy of RLS Diagnosis
Description
Outcome 1, which is not a measured outcome but rather a broad goal of care, is improved accuracy of RLS diagnosis.
Supporting Evidence and Rationale
Both underdiagnosis and misdiagnosis of RLS remain problematic.1 Diagnostic questionnaires such as the Johns Hopkins Telephone Diagnostic Interview and structured tests such as a dopaminergic challenge or the Suggested Immobilization Test have been proposed to aid in diagnosis of RLS. However, either more conclusive data are needed, or as with Immobilization Tests, testing is cumbersome for a clinical setting. Although several bio-markers, including periodic limb movements during sleep and various single nucleotide polymorphisms, are associated with RLS, they are not sufficiently sensitive or specific to diagnose RLS. Therefore, RLS remains a clinical diagnosis, based upon symptoms reported by patients during a clinical interview, and careful attention to accurate diagnosis is critically important.
The Workgroup was in unanimous agreement that accurate diagnosis is the essential foundation for subsequent care of the RLS patient. Although accurate diagnosis is not a particularly patient-oriented outcome, the overall goal of accurate diagnosis is to allow appropriate treatment, and therefore this outcome is expected to improve more patient-oriented outcomes such as decreased symptom severity. The process measures that support this outcome are Process Measure 1 (use of accepted diagnostic criteria) and Process Measure 2 (assessment of iron stores).
Issues Addressed During Development
The diagnosis of RLS is complicated by conditions that can mimic its symptoms, including nocturnal leg cramps, positional discomfort, arthralgias/arthritis, myalgias, leg edema, peripheral neuropathy, radiculopathy, and habitual foot tapping.10 These disorders must be excluded to make an RLS diagnosis. At the same time, other medical conditions may be comorbid with RLS and cause or worsen RLS symptoms. These conditions include iron deficiency, renal disease, pregnancy, myelopathy, symptomatic venous insufficiency, peripheral artery disease, and neuropathy.11 Evaluation for these conditions is an essential component of RLS diagnosis, as the failure to do so can result in misdiagnosis and improper treatments. In early versions of these quality measures, the Workgroup attempted to develop a process measure that would monitor comprehensive evaluation for such mimics and comorbidities. However, the consensus conclusion was that extraction of requisite data from medical record systems in their current form would be too onerous. Instead, the Workgroup chose to emphasize two processes that partially address this issue: Process 1 requires use of accepted diagnostic symptom criteria, and Process 2 requires assessment of iron stores.
Process Measure 1 – Use of Accepted Diagnostic Criteria
Description
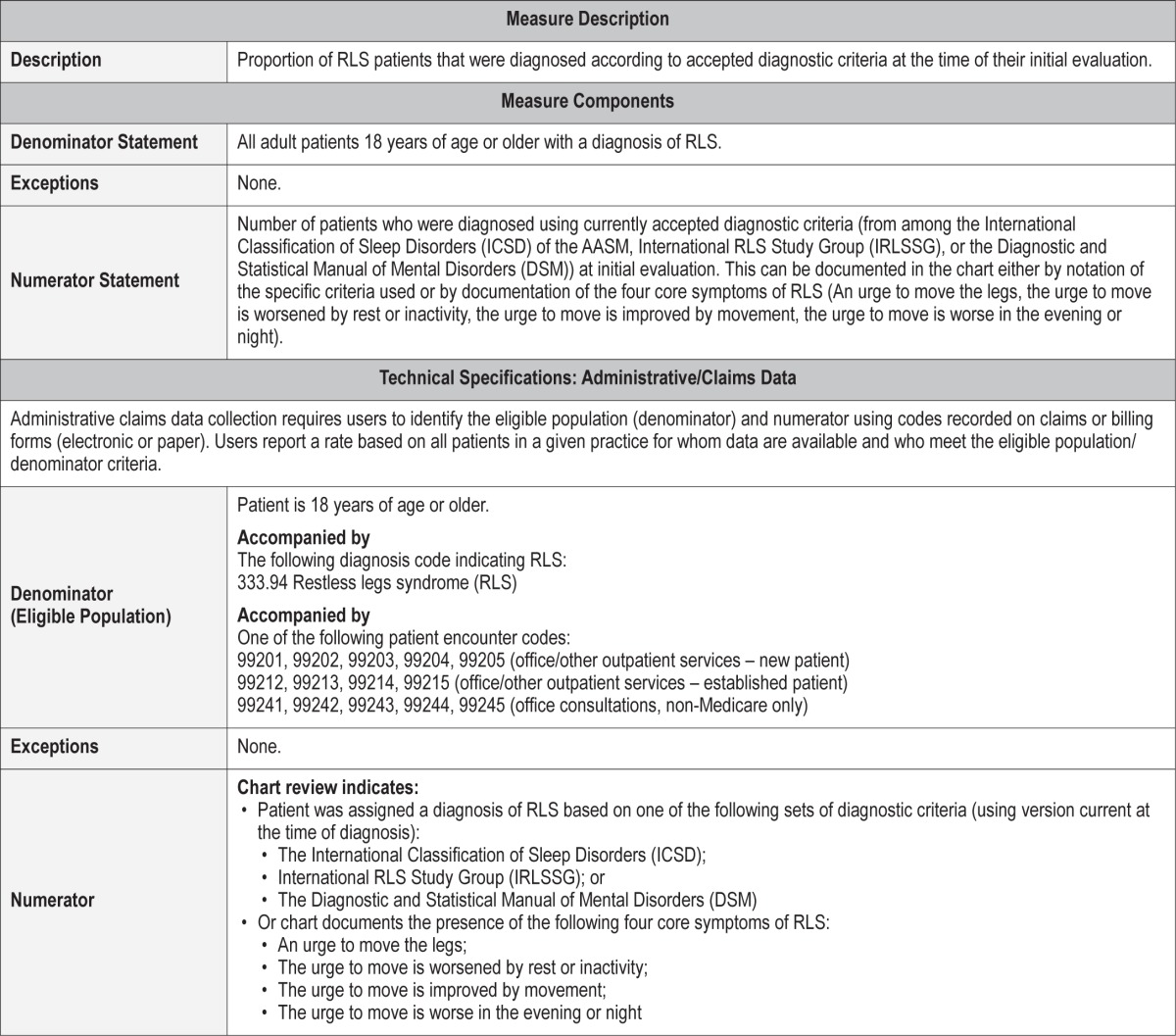
Proportion of RLS patients that were diagnosed according to accepted diagnostic criteria at the time of their initial evaluation.
Exceptions and Exception Justification
There are no exceptions for this measure.
Supporting Evidence and Rationale
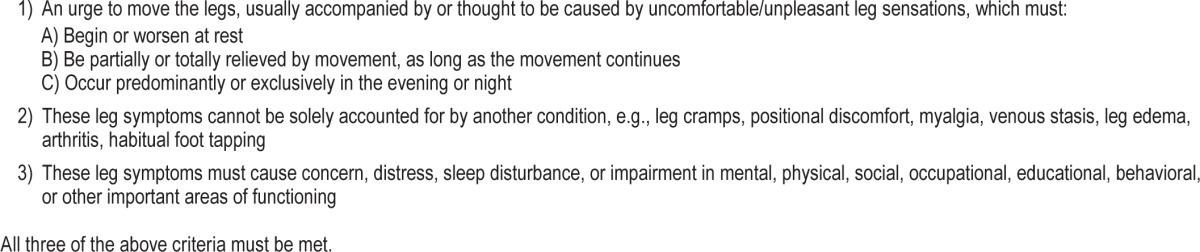
Modern diagnostic criteria for RLS were elaborated in 1995 but continue to evolve. Organizations that have RLS diagnostic criteria include the AASM (through the International Classification of Sleep Disorders), the International RLS Study Group (IRLSSG), and the American Psychiatric Association (via the Diagnostic and Statistical Manual of Mental Disorders, DSM). The core features of RLS diagnosis across the different classifications are: (1) an urge to move the legs, (2) appearance of symptoms at rest, (3) relief by movement, and (4) prominence in the evening. Diagnostic criteria from each of the groups require the exclusion of RLS mimics, but differ with regard to frequency of symptoms and disease duration. The current AASM diagnostic criteria are shown in Table 2. As multiple diagnostic criteria exist but all focus on the same key elements, use of any of the major criteria (i.e., AASM, IRLSSG, or DSM) in the most current version at the time of patient evaluation, is acceptable for this measure. The Workgroup judged the evidence supporting the relationship between this process and outcome #1 as Level 4.
Table 2.
Current International Classification of Sleep Disorders/AASM diagnostic criteria for restless legs syndrome.49
Relationship to Desired Outcome
The desired outcome (#1) is to improve the accuracy of RLS diagnosis. This process measure is a core determinant of improved diagnostic accuracy, as it requires the use of RLS criteria based upon science and expert opinion.
Opportunities for Improvement/Gaps
Awareness of RLS within the medical community is increasing. Some practitioners, however, may still have incomplete understanding of which symptoms constitute RLS. Uniform use of accepted RLS diagnostic criteria will reduce misdiagnosis of RLS.
Issues Addressed During Development
Testing of this process measure demonstrated that in many cases the specific diagnostic classification (e.g., AASM vs. IRLSSG) was not documented, even when the four core RLS features were outlined. Although RLS mimics may have been excluded by clinicians, explicit documentation of this was either absent or challenging to extract. By consensus, the Work-group therefore decided that documentation of the presence of the core features, with or without explicit comment about mimics or the set of criteria used, was sufficient to meet this process measure at the present time.
Process Measure 2 – Assessment of Iron Stores
Description
Proportion of RLS patients that had measurements of iron stores, including at least serum ferritin, performed during initial RLS evaluation.
Exceptions and Exception Justification
Medical Reasons: Patients with documented disorders of iron overload (e.g., hemochromatosis) do not need screening for iron deficiency. Although current evidence does not specify how frequently iron stores should be tested in RLS patients, the Workgroup consensus was that patients whose iron stores had been tested within the last year may not need repeat testing at the time of RLS diagnosis. The decision to repeat testing sooner than one year would depend on clinical status, with earlier assessment potentially indicated after blood loss, worsening of RLS symptoms, augmentation, or other specific situations.
Patient Reasons: Patients who decline blood draws.
System Reasons: Patients whose payers do not cover iron panel testing.
Supporting Evidence and Rationale
The assessment of iron stores is a recommended process in the evaluation of every RLS patient.12 Low serum iron measurements are found in up to one-third of RLS patients.13–15 Considerable physiologic, autopsy, and genetic evidence supports a contribution from iron insufficiency in RLS, and the presence of low iron stores may affect the expression of RLS symptoms. Serum ferritin levels are inversely correlated with RLS severity14,16–18 and are associated with increased rates of depression13 and augmentation18,19 in RLS patients. Randomized controlled-trials of iron therapy for RLS symptoms have yielded mixed results,20 but iron supplementation is generally considered on a case-by-case basis in RLS patients with ferritin levels below 50 or 75 mcg/L.21,22 Many clinical trials that assessed RLS treatments have excluded patients with iron deficiency anemia or low ferritin levels, raising the possibility that this subgroup of patients may need different treatment algorithms.
Common measures of iron stores include ferritin and transferrin, which together with serum iron and total iron binding capacity evaluate the peripheral iron profile. In most circumstances serum ferritin is regarded as the most sensitive and specific of these tests to diagnose iron deficiency,23 and therefore the Workgroup considers ferritin to be a minimally acceptable determination of iron stores. However, ferritin levels increase with inflammation and RLS is strongly associated with inflammatory conditions,24 which might result in elevated ferritin values in RLS patients. The Workgroup therefore recommends measurement of a full iron panel when possible. Although anemia often reflects iron deficiency, RLS may be triggered or perpetuated by iron deficiency in people without coexisting anemia,25 so a hemoglobin and hematocrit are judged insufficient to determine iron status in RLS patients.
The Workgroup judged the evidence supporting the relationship between this process and outcome #1 as Level 4.
Relationship to Desired Outcome
Outcome #1 is to improve the accuracy of RLS diagnosis. Initial assessment for iron deficiency, while not strictly necessary for diagnosis of RLS, is part of a complete diagnostic assessment in order to identify a common and clinically relevant comorbid condition.
Opportunities for Improvement/Gaps
The percent of RLS patients in whom iron stores are assessed at diagnosis is unknown, though likely affected to some degree by coverage policies of individual payers.
Issues Addressed During Development
The necessity of iron store measurement in the initial evaluation of RLS patients was accepted unanimously by the Work-group, as was the exception that the testing did not need to be repeated at RLS diagnosis if it had been done recently. The one-year time frame for the exception (i.e., not requiring re-testing of iron stores at RLS diagnosis if it had been tested within the prior one year) was chosen based on expert consensus, while considering patient comfort and resource utilization. However, the Workgroup recognizes that a variety of changes in patient condition, including but not limited to invasive procedures, blood donation, any significant blood loss, or worsening of RLS symptoms, may necessitate retesting of iron stores either at diagnosis or during subsequent care, and this measure is not meant to preclude such testing.
Outcome 2 – Decrease RLS Symptom Severity
Description
Proportion of RLS patients that showed a decrease in symptom severity within 12 months of being prescribed a new medication for RLS.
Exceptions and Exception Justifications
This measure applies to patients who are prescribed a new medication for RLS symptoms. However, the measure excludes those patients for whom new medical therapy is less likely to result in a clinically significant improvement, either for patient or medical reasons.
Medical Reasons: Patients are excluded if their symptoms have been refractory to at least 2 other medications for RLS, or they were unable to tolerate at least 2 other medications, as their improvement on second- or third-line medications may be limited. Patients are also excluded if they have mild symptoms, with little opportunity to demonstrate improvement. For identification of patients with mild symptoms, the Workgroup recommends use of an IRLSSG Rating Scale (IRLS)26 severity < 15, as this is a common exclusion criterion for RLS clinical trials, but explicit documentation of mild symptoms can substitute if the IRLS is not used. Pregnant women may sometimes be prescribed medication for RLS symptoms, but because RLS severity varies across the course of pregnancy independent of treatment, they are excluded from this measure.
Patient Reasons: Patients who are noncompliant to treatment; patients who do not return for follow-up.
System Reasons: None.
Supporting Evidence and Rationale
The negative impact of RLS on quality of life is substantial, especially when RLS symptoms are severe.27 RLS is eminently treatable with a number of different medications, many supported by Level I evidence. Because RLS symptoms may affect multiple domains (e.g., sleep disturbance, mood disturbance, daytime sleepiness, and daytime dysfunction), improvement in RLS severity may manifest differently in individual patients. Use of a validated, RLS-specific tool that addresses these multiple domains, for example the IRLS, allows these domains to be well-captured. Alternatively, combinations of validated scales might be used to assess these aspects of symptom severity. If a validated scale is not used, the clinician should document a decrease in symptom severity as reported by the patient in his or her own words. For the current iteration of quality measures, any amount of documented improvement in any aspect of severity—overall severity or a specific component symptom such as sleep quality, tiredness, sleepiness, mood, or daytime function—is considered sufficient to meet this measure. This outcome measure is supported by Process Measures 3 (assess severity at each visit) and 4 (prescribe an evidence-based treatment).
Opportunities for Improvement/Gaps
RLS is a disorder with substantial burden when untreated, and several effective, evidence-based treatments exist. Therefore, opportunity exists to reduce suffering from RLS by decreasing its severity with available treatments.
Issues Addressed During Development
The major challenge faced in the development of this measure was the decision on the best way to document symptom severity and define a clinically meaningful decrease in symptoms. These issues are discussed in detail in the Process Measure 3 section, below.
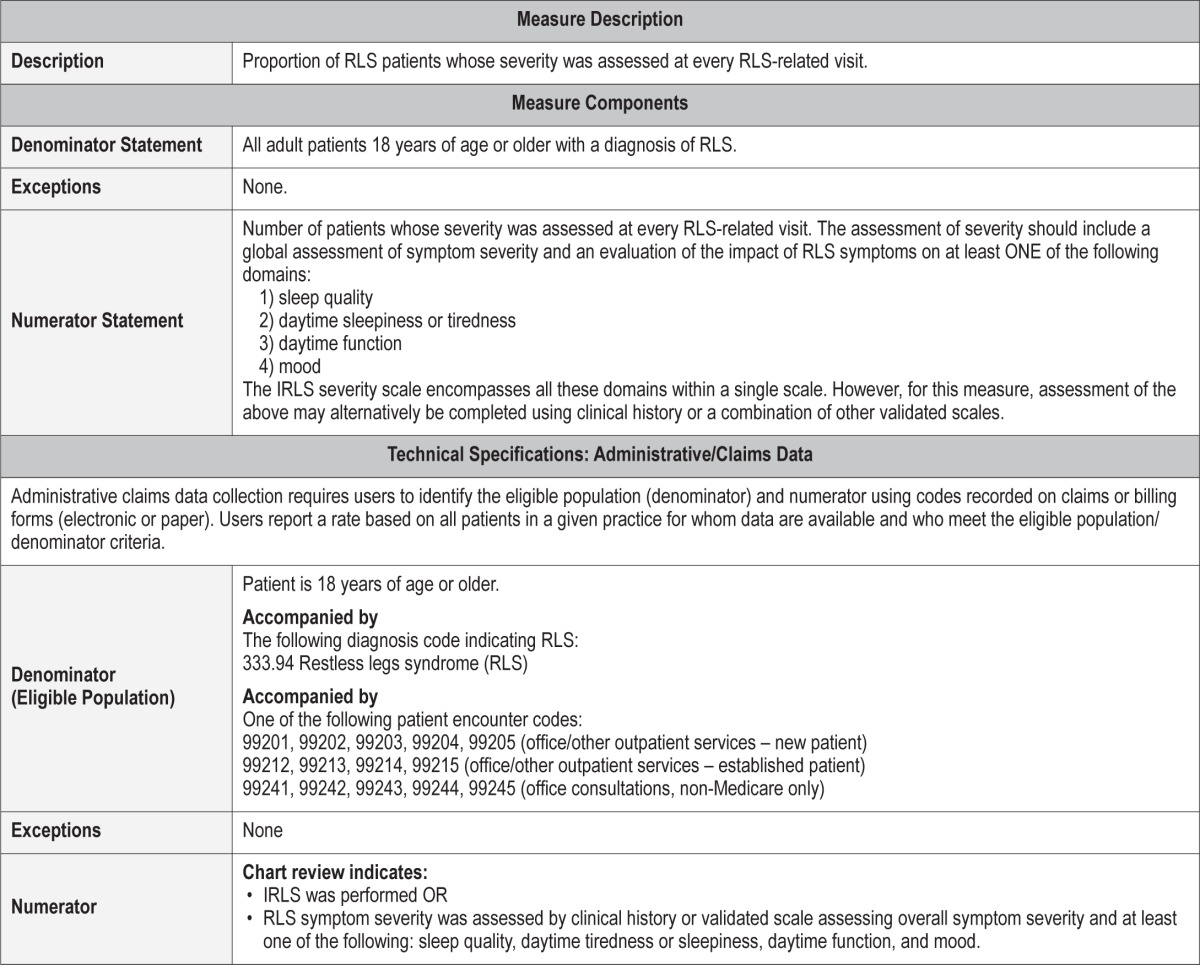
Process Measure 3 – Assessment of Symptom Severity
Description
Proportion of RLS patients whose severity was assessed at every RLS-related visit. The assessment of severity should include a global measure of severity, as well as assessment of at least one RLS-associated domain including sleep quality, daytime sleepiness/tiredness, daytime function, or mood. This may be documented with a variety of validated scales or through free-text within the medical record (e.g., “the patient reports that RLS symptoms are less severe and sleep quality has improved”).
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Measurement of disease severity is important at the initial evaluation to identify those patients whose symptoms may not be severe enough to warrant treatment as well as to provide a baseline for comparison after initiating treatment. Repeated measures over time allow evaluation of the success of treatment, and identification of the two major causes of treatment failure in the long-term treatment of RLS: loss of medication efficacy and augmentation.28 The Workgroup judged the evidence supporting the relationship between this process and outcome #2 as Level 4.
Relationship to Desired Outcome
Outcome measure #2 is to decrease the severity of RLS. To see a decrease in severity and to identify treatment failures that require medication changes, severity must be measured routinely.
Opportunities for Improvement/Gaps
The frequency of severity assessment at present is unknown but is likely to offer an opportunity for improvement in some practices.
Issues Addressed During Development
A major point of debate during the development of this process measure was how best to measure severity. Some members of the Workgroup, as well as some stakeholders who provided feedback, preferred to rely solely on physician history-taking in the form of free-text documentation within the medical record. In contrast, others preferred to quantify the impact of care on symptom severity, through use of a standard rating scale. Ultimately, the Workgroup decided that a requirement to use a single validated questionnaire would be premature, but that use of such scales should be encouraged to allow easier extraction of information from medical records and clearer measurement of outcomes.
Part of the challenge was the lack of a widely accepted, self-administered “gold standard” questionnaire for the assessment of RLS severity. The IRLS is widely used in clinical trials but was validated to be completed by the patient in the presence of an examiner,26 which may be too time-consuming for clinical practice. In favor of the IRLS, however, are the following: (1) it has been well validated26; (2) it correlates with the level of motor dysfunction found in RLS patients (e.g., periodic leg movement index in sleep and waking periodic leg movements during the Suggested Immobilization Test29; and (3) it assesses not only RLS severity but also the impact of RLS across multiple domains. Validation of a self-administered version of the IRLS is currently underway (D. Sharon, personal communication), and may ease current challenges with widespread clinical use of the IRLS.
As an alternative to the IRLS, the Patient Global Impression (PGI) is a more convenient and simple measure of RLS severity. This single question simply asks the patient to rate on a 7-point scale the level of illness (from “normal, not at all ill” to “extremely ill”) or the level of improvement (PGI-I) in symptoms (“very much better” to “very much worse”). This single question correlates well with the Clinical Global Impression-Improvement (CGI-I).30 However, the PGI as a single question does not address the associated features of RLS (e.g., sleep quality, daytime function, and mood) that are important aspects in many patients.
Separate from the issue of which, if any, scale should be used is the issue of what constitutes a clinically meaningful improvement. In 2007, the European RLS Study Group recommended a change in the IRLS of 6 points more than placebo as a measure of medication efficacy.31 More recent work suggests that the difference from placebo is often smaller than this (e.g., a 4.2-point improvement versus placebo for ropinirole and a 5.2-point difference for pramipexole).32 In clinical practice, the difference based on an intervention will be experienced as a change from baseline, rather than a change versus placebo, and therefore would be expected to be larger. However, this larger effect might be attenuated by the heterogenous patient population encountered in clinical practice. Such a caveat is illustrated by a recent study by Godau et al.,33 which surprisingly showed no significant improvement in IRLS after 12 months of guideline-based treatment, despite the majority of patients reporting improvement in their RLS symptoms. Thus, while the Workgroup believes that measurement of disease severity over time is an important step toward ensuring that particular interventions result in the expected decrease in symptom severity, further research is clearly needed to determine how best to measure severity and how much improvement can reasonably be expected when patients are provided quality care. In the meantime, the Workgroup chose to allow a broad range of severity measures (including free text) for this process, as well as any degree of improvement for the associated outcome measure (outcome measure #2).
Process Measure 4 – Delivery of Evidence-Based Treatment
Description
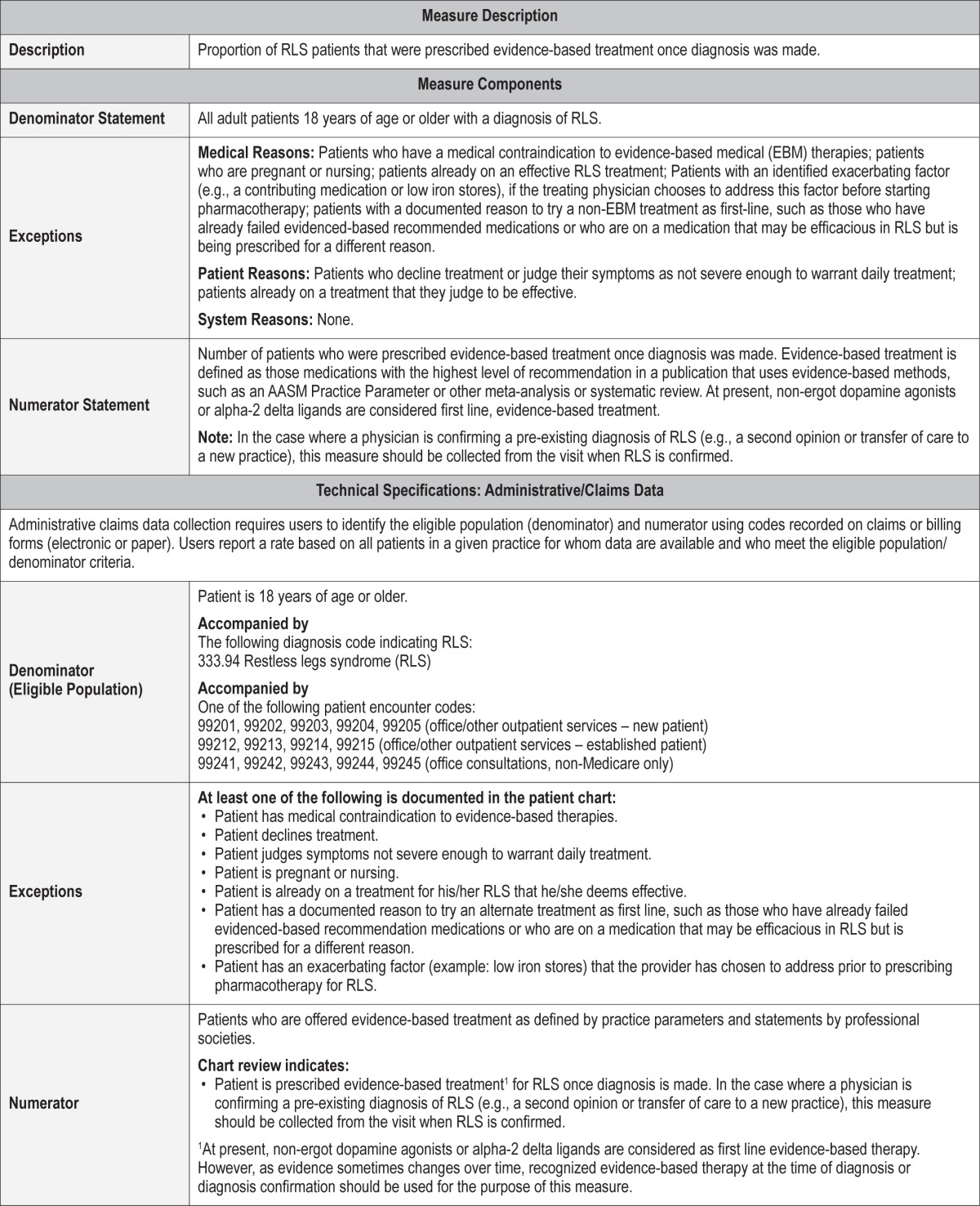
Proportion of RLS patients that were prescribed treatment consistent with available evidence-based guidelines at the time of diagnosis.
Exceptions and Exception Justifications
Medical Reasons: Patients who have a medical contraindication to evidence-based treatment; patients who are pregnant or nursing women; patients with an explicitly identified exacerbating factor that the physician chooses to address prior to instituting additional therapy; patients who have an explicitly documented reason to try a non-EBM based treatment (e.g., having already failed other EBM recommendations or having a comorbidity that could be addressed along with RLS by a single medication) are excluded from this measure. Given the complexity of these exceptions, the reason for any departure from evidence-based medicine should be clearly stated within the medical record.
Patient Reasons: Patients who decline treatment or judge their symptoms not severe enough to warrant daily treatment and patients already on a treatment that they judge to be effective regardless of the published level of evidence are excluded from this measure.
System Reasons: None.
Supporting Evidence and Rationale
Multiple recent systematic reviews have demonstrated the efficacy of several medications for RLS symptoms.22,28,31,34–36 The current AASM practice parameter recommends treatment with a non-ergotamine dopamine agonist (pramipexole or ropinirole) as a standard, with the use of the calcium channel alpha-2-delta ligand gabapentin enacarbil (and other medications, including opiates) as a guideline.22 Reviews by other RLS stakeholder groups have led to similar but not identical recommendations; some have reported equivalent high level recommendations for both the non-ergotamine dopamine agonists (including rotigotine) and the three calcium channel alpha-2-delta ligands (gabapentin enacarbil, gabapentin, and pregabalin).34,36 Both the IRLSSG and the WED Foundation Medical Advisory Board recommend either non-ergotamine dopamine agonists or alpha-2-delta ligands as first line therapy for RLS.12,28 The Workgroup judged the evidence supporting the relationship between this process and outcome #2 as Level 1.
Relationship to Desired Outcome
Delivery of evidence-based medical therapy has been well-documented to decrease symptom severity and is therefore expected to promote outcome #2.
Opportunities for Improvement/Gaps
The current rate of use of evidence-based medication for RLS is unknown, but epidemiologic data from several years ago suggest that RLS is under-treated among patients who desire treatment.27
Issues Addressed During Development
The Workgroup acknowledges that current best evidence is a target that changes over time. At present, published evidence-based guidelines support non-ergot dopamine agonists and alpha-2-delta ligands as first-line RLS treatment. However, as further treatment evidence accumulates, these recommendations may change. As a result, adherence to this process measure requires following the evidence-based guidelines that are current when care is delivered, rather than following guidelines that are active at the time of publication of this manuscript. This issue is well illustrated by the publication of a large, placebo-controlled study of opiates for RLS37 during the development of these measures. Opiates are currently recommended by the AASM at a guideline level.22
Outcome 3 – Minimize Treatment Complications
Description
Outcome 3, which is not a measured outcome but rather a broad goal of care, is minimizing treatment complications.
Supporting Evidence and Rationale
There are multiple medication side effects from the commonly used RLS medications. Because side effects can affect medication compliance and efficacy, minimization of treatment complications is an important goal of RLS management. In RLS patients, adverse medication reactions result in discontinuation of therapy in about 10% to 20% of patients on dopa-mine agonist therapy, 10% of patients on gabapentin enacarbil, and up to 30% of patients prescribed opioids.22,28 This outcome is supported by process measures 5 (counseling about medication side effects), 6 (assessment of impulse control disorders), and 7 (assessment of augmentation).
The frequency at which RLS treatment complications are evaluated and therapy adjusted accordingly is unknown. In other chronic illnesses, patient satisfaction with treatment is associated with greater medication adherence, increased likelihood of therapy continuation, and improved outcomes.38 By increasing the recognition of treatment complications and the need to ameliorate these side effects, RLS symptom control may be optimized while improving patient quality of life and safety.
Issues Addressed During Development
This outcome measure specifically addresses the safety and patient-centered domains set forth by the Institute of Medicine (IOM) for quality assessment.39 The Workgroup agreed unanimously on its inclusion as an outcome measure.
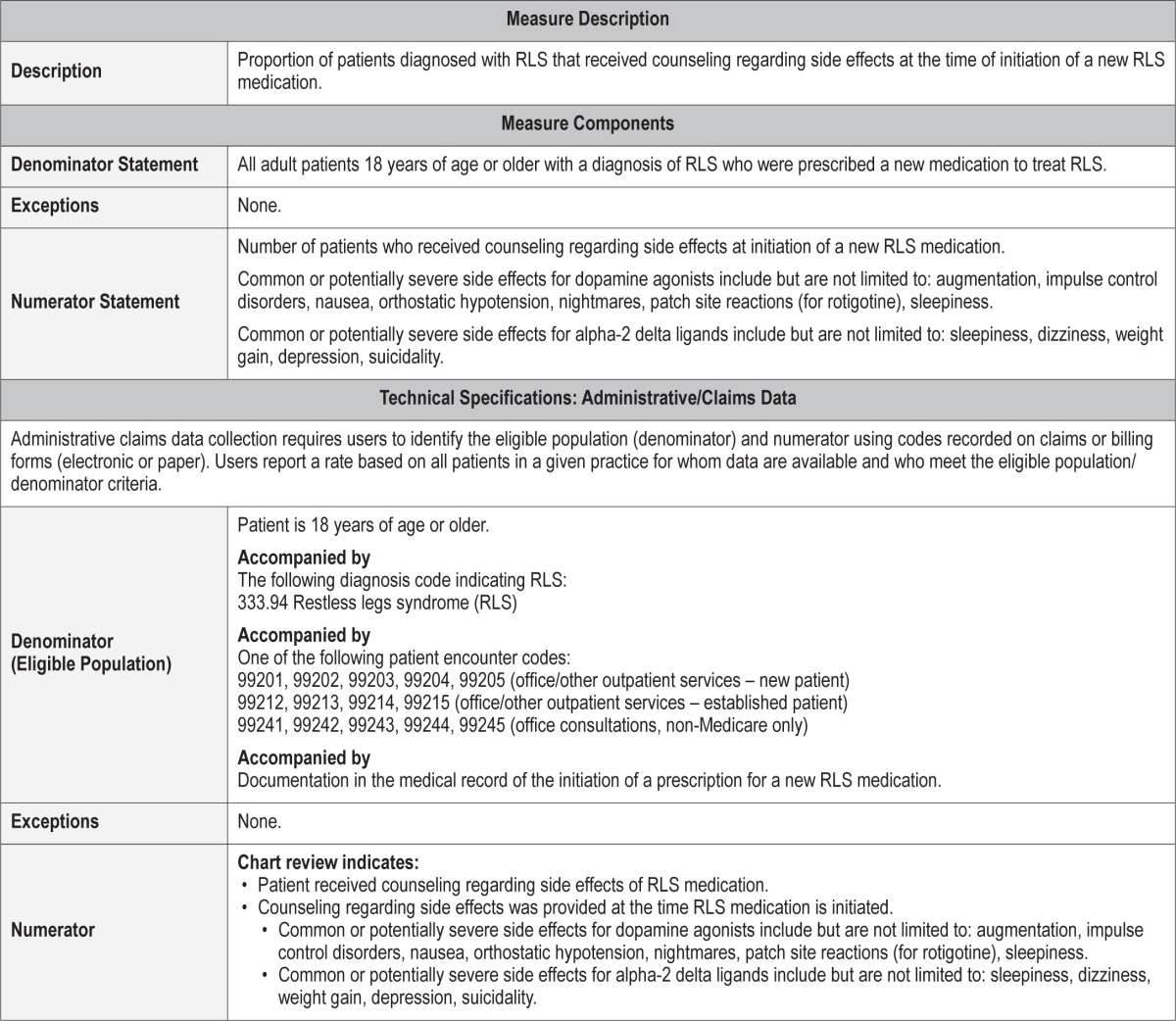
Process Measure 5 – Counseling About Medication Side Effects
Description
Proportion of patients diagnosed with RLS who receive counseling regarding side effects at the time of initiation of a new RLS medication.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Ample evidence demonstrates that side effects are common in patients undergoing treatment for RLS with pharmacotherapy. Patients receiving dopamine agonists can experience side effects including, but not limited to, impulse control disorders, augmentation, nausea, vomiting, headaches, dizziness, fatigue, somnolence, insomnia, hallucinations, and application site reactions (the latter for rotigotine only).22,28,34 Side effects experienced on alpha-2-delta ligand medication include, but are not limited to, swelling, imbalance, change in cognition, dizziness, weight gain, suicidality, dry mouth, and somnolence.22,28,34 Opioid medications are associated with worsening of sleep disordered breathing, change in mood, sedation, constipation, and potential for abuse, among others.22,28 Iron supplementation is sometimes associated with nausea, vomiting, diarrhea, constipation, and dark colored stools.34 When clinicians counsel patients about potential medication side effects, adverse drug events are significantly reduced.40 In its most recent clinical summary, the Agency for Healthcare Research and Quality recommended that clinicians discuss “the available evidence for the harms of the various treatments for RLS” with patients and their caregivers.41 Therefore, the Workgroup developed this process measure to minimize treatment complications by the promotion of counseling regarding side effects of medication. This counseling should be performed at initiation of any new RLS medication. The Workgroup judged the evidence supporting the relationship between this process and outcome #3 as Level 4.
Relationship to Desired Outcome
This process measure is related to outcome measure 3 (minimize treatment complications). To our knowledge, no literature links counseling on medication side effects to a reduction in side effects among patients with RLS. However, in other patient groups, medication counseling reduces adverse drug events significantly.40 Increased awareness of potential adverse reactions may increase the likelihood that patients report medication side effects to their physicians. This, in turn, could lead to changes in therapy, fewer treatment complications, and better treatment efficacy.
Opportunities for Improvement/Gaps
The rate at which physicians counsel patients about potential RLS medication side effects is unknown.
Issues Addressed During Development
Conversations between physicians and patients regarding medication safety may occur more often than they are documented within the medical record, and adoption of this process measure will require explicit documentation of such conversations. However, because of the importance of side effect counseling, the Workgroup decided that the minimal added documentation burden was outweighed by the potential benefits of more widespread side effect counseling.
Process Measure 6 – Assessment for Impulse Control Disorders
Description
Proportion of RLS patients treated with a dopamine agonist or levodopa that were assessed for impulse control disorders at every RLS visit. Assessment of impulse control disorders may be performed either by history or a validated scale.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Impulse control disorders or behaviors, including pathologic gambling, excessive shopping, hypersexuality, and punding, have been reported to occur in patients with RLS who are treated with dopamine agonists or levodopa.21,28,42,43 The exact frequency of such behaviors and their relationship to dopaminergic medications is an area of ongoing investigation. Questionnaire-based assessments have suggested a prevalence between 6% and 17% in treated RLS patients.21 People with RLS, whether treated or not, appear to have an increase in impulsivity.42 An increase in impulsivity in patients treated with dopamine agonists was reported by some,28,43 but not all.42
Current consensus treatment guidelines highlight impulse control disorders as a serious treatment complication in RLS. Both the International RLS Study Group28 and the Willis Ekbom Disease Foundation12 recommend that RLS patients treated with dopaminergic agents be screened for impulse control disorders at every follow-up visit. The recommendation to screen at every visit likely reflects the potential seriousness of this complication, which can have profound psychosocial consequences.44 The development of impulse control disorders may be a delayed side effect (starting an average of 9 months after beginning dopamine agonist therapy), so ongoing screening for this complication is needed.12 The Workgroup judged the evidence supporting the relationship between this process and outcome #3 as Level 4.
Relationship to Desired Outcome
This process measure will minimize treatment complications by helping to ensure that the onset of an impulse control disorder is identified early, so that treatment can be modified as necessary.
Opportunities for Improvement/Gaps
The frequency with which patients treated with dopaminergic therapy for RLS are assessed for impulse control disorders is unknown. However, as this potential complication was first reported in RLS patients relatively recently,45 physician awareness may still be limited.
Issues Addressed During Development
At this time, no impulse control disorder assessment tool exists that is universally recommended for RLS patients. Therefore, the Workgroup agreed that documentation of the presence or absence of this syndrome was sufficient for this measure.
Process Measure 7 – Assessment for Augmentation
Description
Proportion of RLS patients treated with a dopamine agonist or levodopa that were assessed for augmentation at every RLS visit.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Clinical experience, longitudinal open-label studies, and expert consensus all identify augmentation as a common and problematic treatment complication of dopaminergic therapy for RLS, despite a relative paucity of data from placebo-controlled trials on the frequency and timing of this complication.35 Current expert consensus guidelines recommend that patients be asked about symptoms of augmentation at every visit41 or that augmentation be “carefully assessed.28 Augmentation should be defined based on currently accepted criteria. At present the Max Planck diagnostic criteria46 include the following:
Symptoms occurring at least four hours earlier in the day than previously experienced, or
Symptoms occurring two to four hours earlier, along with at least one of the following: (a) additional body parts, such as the arms, becoming affected by RLS sensations; (b) faster symptom onset upon resting; (c) more intense symptom character; (d) shorter duration of response to treatment; or
A persistent paradoxical response to treatment defined as worsening after dose increase and improving after dose decrease.
The Workgroup judged the evidence supporting the relationship between this process and outcome #3 as Level 4.
Relationship to Desired Outcome
Augmentation is judged by some experts as “the most meaningful and clinically relevant adverse event” related to dopaminergic treatment of RLS,35 and therefore detection of augmentation is necessary to allow appropriate management that minimizes adverse impact on patients.
Opportunities for Improvement/Gaps
The frequency with which augmentation is assessed during follow-up treatment is unknown.
Issues Addressed During Development
Whether patients with well controlled RLS symptoms should be excluded from this measure was considered. However, due to the importance of recognizing augmentation, the Workgroup decided that no patients on levodopa or dopamine agonists should be excluded from this measure. By definition, patients who report effective control of RLS symptoms do not meet criteria for augmentation. Therefore, documentation of well-controlled symptoms, which is extracted from the medical record, is sufficient for the evaluation of augmentation for the purpose of this measure. Additional documentation of assessment for augmentation would be required if RLS symptoms are not well controlled.
IMPLEMENTATION STRATEGIES AND FUTURE DIRECTIONS
The RLS literature is rich with high-grade research evidence on treatment and pathophysiology, but research into quality measures and processes is in its infancy. For the most part, the processes recommended in this document are based on Level 4 evidence. It is vital that research be performed to delineate which processes truly result in meaningful, patient-oriented improvements in outcome. We consider these measures to be an early step in an ongoing process of improving care of the patient with RLS, rather than the final word.
To our knowledge, this is the first published set of quality measures for RLS. Implementation of these measures, therefore, may be best managed using a gradual phase-in period. For example, a short period of baseline data collection may be needed to determine how well measures are already met, followed by a focused period of time for implementation of strategies to meet these measures. Finally, a reassessment of implementation success is needed. Some of these processes are likely already performed, just not routinely documented; implementation of recommended measures may require changes to physician documentation in addition to practice itself. The development of local quality measure teams, to oversee implementation, may be helpful.
Documenting completion of the majority of these measures will require review of individual clinic notes. This process is likely to require time and expertise. Clearly, a need exists for better, easier, and more routine methods to document the quality of physician care. Laborious review of individual notes has the potential to redirect resources that would otherwise be devoted to the provision of quality care. The Workgroup weighed the advantages of easily-extractable process measures against those that required chart review yet may be more likely to improve outcomes. The Workgroup concluded, in most cases, that the priority must be quality measures—processes and outcomes—that truly matter. Development of electronic medical record fields that can incorporate these measures on the front end, rather than relying on a review of notes after the fact, is urgently needed to streamline the implementation of these and other quality measures.
In the development of these measures, the Workgroup identified a number of issues of substantial importance to RLS quality care which we decided to defer until a future version of quality measures. In particular, the current measures are all geared toward adult patients with RLS. Although RLS can be problematic in childhood, diagnostic criteria and treatment strategies may differ in adult and pediatric RLS patients, and separate or modified quality measures are likely to be needed for children. Many of the current adult measures are specific to the initial diagnosis and management of RLS, yet RLS is a disorder that can present unique challenges over the long term course of management.28 Future adult quality indicators may additionally focus on such issues, including management of augmentation, especially when sufficient trial data are available regarding optimal management. Similarly, quality care of RLS patients may need specific modifications in certain clinical populations, such as pregnant women and patients with end-stage renal disease. Treatment guidelines are beginning to emerge for these specific populations.47,48 Finally, the Workgroup recognizes that improvement in patient compliance with treatment plans is an important aspect of quality care, over which the provider has some influence. Future measures may incorporate measures of physician attempts to improve patient compliance.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Chervin has consulted for MC3 and Zansors, has received royalties from UpToDate and Cambridge University Press, and is a current member of the American Academy of Sleep Medicine Board of Directors. Mr. Harrod is an employee of the American Academy of Sleep Medicine. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The American Academy of Sleep Medicine would like to thank the following parties for their review of these measures, and for providing feedback and suggestions to improve the relevancy and utility of these measures in their field of practice: Ruth Boland, RN; Belen Esparis, MD; Anthony Masi, MD; Margaret Moen, MD; Bonnie Norris, RN; Michael Rack, MD; Tilak Verma, MD; American Academy of Family Physicians (AAFP); the International Parkinson and Movement Disorder Society (MDS); Willis-Ekbom Disease (WED) Foundation. The AASM did not seek or receive endorsement of these measures from any of the reviewers and respective organizations who provided feedback. The authors carefully considered all feedback provided, and implemented as many suggestions as were feasible in the refining of these measures. We would also like to thank Carolyn Winter-Rosenberg, AASM Director of Coding and Compliance, for guidance in compiling the technical specifications associated with these quality measures.
APPENDIX
The following are the technical specifications for the restless legs syndrome quality measures, which can be used to calculate an individual provider's performance in meeting these measures. Tracking and periodically reviewing this performance data will help providers identify opportunities for improvement within their own practices.
 |
Process Measure #1: Use of accepted diagnostic criteria
Process Measure #2: Assessment of iron stores

Outcome #2: Decrease RLS symptom severity

Process Measure #3: Assessment of symptom severity
Process Measure #4: Delivery of evidence-based treatment
Process Measure #5: Medication side effects
Process Measure #6: Assessment for impulse control disorders

Process Measure #7: Assessment for augmentation

REFERENCES
- 1.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–92. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 2.Winkelman JW, Finn L, Young T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin Sleep Cohort. Sleep Med. 2006;7:545–52. doi: 10.1016/j.sleep.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lesperance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov Disord. 1997;12:61–5. doi: 10.1002/mds.870120111. [DOI] [PubMed] [Google Scholar]
- 4.Phillips B, Hening W, Britz P, Mannino D. Prevalence and correlates of restless legs syndrome: results from the 2005 National Sleep Foundation Poll. Chest. 2006;129:76–80. doi: 10.1378/chest.129.1.76. [DOI] [PubMed] [Google Scholar]
- 5.Lee HB, Hening WA, Allen RP, et al. Restless legs syndrome is associated with DSM-IV major depressive disorder and panic disorder in the community. J Neuropsychiatry Clin Neurosci. 2008;20:101–5. doi: 10.1176/jnp.2008.20.1.101. [DOI] [PubMed] [Google Scholar]
- 6.Hening WA, Allen RP, Chaudhuri KR, et al. Clinical significance of RLS. Mov Disord. 2007;22(Suppl 18):S395–400. doi: 10.1002/mds.21665. [DOI] [PubMed] [Google Scholar]
- 7.Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol Clin. 2012;30:1137–66. doi: 10.1016/j.ncl.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 8.American Academy of Sleep Medicine. 2014. http://www.aasmnet.org/aboutaasm.aspx.
- 9.Morgenthaler TI, Aronsky AJ, Carden KA, Chervin RD, Thomas SM, Watson NF. Measurement of quality to improve care in sleep medicine. J Clin Sleep Med. 2015;11:279–91. doi: 10.5664/jcsm.4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benes H, Walters AS, Allen RP, Hening WA, Kohnen R. Definition of restless legs syndrome, how to diagnose it, and how to differentiate it from RLS mimics. Mov Disord. 2007;22(Suppl 18):S401–8. doi: 10.1002/mds.21604. [DOI] [PubMed] [Google Scholar]
- 11.Ondo WG. Common comorbidities and differential diagnosis of restless legs syndrome. J Clin Psychiatry. 2014;75:e06. doi: 10.4088/JCP.12074nr2c. [DOI] [PubMed] [Google Scholar]
- 12.Silber MH, Becker PM, Earley C, Garcia-Borreguero D, Ondo WG. Willis-Ekbom Disease Foundation revised consensus statement on the management of restless legs syndrome. Mayo Clin Proc. 2013;88:977–86. doi: 10.1016/j.mayocp.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 13.Cuellar NG, Hanlon A, Ratcliffe SJ. The relationship with iron and health outcomes in persons with restless legs syndrome. Clin Nurs Res. 2011;20:144–61. doi: 10.1177/1054773810388557. [DOI] [PubMed] [Google Scholar]
- 14.O'Keeffe ST, Noel J, Lavan JN. Restless legs syndrome in the elderly. Postgrad Med J. 1993;69:701–3. doi: 10.1136/pgmj.69.815.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohayon MM, O'Hara R, Vitiello MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev. 2012;16:283–95. doi: 10.1016/j.smrv.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curgunlu A, Doventas A, Karadeniz D, et al. Prevalence and characteristics of restless legs syndrome (RLS) in the elderly and the relation of serum ferritin levels with disease severity: hospital-based study from Istanbul, Turkey. Arch Gerontol Geriatr. 2012;55:73–6. doi: 10.1016/j.archger.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Sun ER, Chen CA, Ho G, Earley CJ, Allen RP. Iron and the restless legs syndrome. Sleep. 1998;21:371–7. [PubMed] [Google Scholar]
- 18.Frauscher B, Gschliesser V, Brandauer E, et al. The severity range of restless legs syndrome (RLS) and augmentation in a prospective patient cohort: association with ferritin levels. Sleep Med. 2009;10:611–5. doi: 10.1016/j.sleep.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Hogl B, Oertel WH, Stiasny-Kolster K, et al. Treatment of moderate to severe restless legs syndrome: 2-year safety and efficacy of rotigotine transdermal patch. BMC Neurol. 2010;10:86. doi: 10.1186/1471-2377-10-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trotti LM, Bhadriraju S, Becker LA. Iron for restless legs syndrome. Cochrane Database Syst Rev. 2012;5:CD007834. doi: 10.1002/14651858.CD007834.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silber MH. Sleep-related movement disorders. Continuum. 2013;19:170–84. doi: 10.1212/01.CON.0000427207.13553.68. [DOI] [PubMed] [Google Scholar]
- 22.Aurora RN, Kristo DA, Bista SR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults-an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses: an American Academy of Sleep Medicine Clinical Practice Guideline. Sleep. 2012;35:1039–62. doi: 10.5665/sleep.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM. Ferritin for the clinician. Blood Rev. 2009;23:95–104. doi: 10.1016/j.blre.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weinstock LB, Walters AS, Paueksakon P. Restless legs syndrome--theoretical roles of inflammatory and immune mechanisms. Sleep Med Rev. 2012;16:341–54. doi: 10.1016/j.smrv.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Silber MH, Richardson JW. Multiple blood donations associated with iron deficiency in patients with restless legs syndrome. Mayo Clinic Proc. 2003;78:52–4. doi: 10.4065/78.1.52. [DOI] [PubMed] [Google Scholar]
- 26.Walters AS, LeBrocq C, Dhar A, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4:121–32. doi: 10.1016/s1389-9457(02)00258-7. [DOI] [PubMed] [Google Scholar]
- 27.Hening W, Walters AS, Allen RP, Montplaisir J, Myers A, Ferini-Strambi L. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med. 2004;5:237–46. doi: 10.1016/j.sleep.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14:675–84. doi: 10.1016/j.sleep.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Borreguero D, Larrosa O, de la Llave Y, Granizo JJ, Allen R. Correlation between rating scales and sleep laboratory measurements in restless legs syndrome. Sleep Med. 2004;5:561–5. doi: 10.1016/j.sleep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Hogl B, Gschliesser V, Poewe W. Assessing treatment outcome in RLS trials and clinical care: CGI-I, PGI, or VAS? Sleep Med. 2013;14:125–6. doi: 10.1016/j.sleep.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Trenkwalder C, Kohnen R, Allen RP, et al. Clinical trials in restless legs syndrome--recommendations of the European RLS Study Group (EURLSSG) Mov Disord. 2007;22(Suppl 18):S495–504. doi: 10.1002/mds.21538. [DOI] [PubMed] [Google Scholar]
- 32.Scholz H, Trenkwalder C, Kohnen R, Riemann D, Kriston L, Hornyak M. Dopamine agonists for restless legs syndrome. Cochrane Database Syst Rev. 2011:CD006009. doi: 10.1002/14651858.CD006009.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Godau J, Spinnler N, Wevers AK, Trenkwalder C, Berg D. Poor effect of guideline based treatment of restless legs syndrome in clinical practice. J Neurol Neurosurg Psychiatry. 2010;81:1390–5. doi: 10.1136/jnnp.2010.211417. [DOI] [PubMed] [Google Scholar]
- 34.Wilt TJ, MacDonald R, Ouellette J, et al. Treatment for restless legs syndrome. comparative effectiveness review No. 86. AHRQ Publication. 2012;12(13) [Google Scholar]
- 35.Hornyak M, Scholz H, Kohnen R, Bengel J, Kassubek J, Trenkwalder C. What treatment works best for restless legs syndrome? Meta-analyses of dopaminergic and non-dopaminergic medications. Sleep Med Rev. 2014;18:153–64. doi: 10.1016/j.smrv.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Borreguero D, Ferini-Strambi L, Kohnen R, et al. European guidelines on management of restless legs syndrome: report of a joint task force by the European Federation of Neurological Societies, the European Neurological Society and the European Sleep Research Society. Eur J Neurol. 2012;19:1385–96. doi: 10.1111/j.1468-1331.2012.03853.x. [DOI] [PubMed] [Google Scholar]
- 37.Trenkwalder C, Benes H, Grote L, et al. Prolonged release oxycodonenaloxone for treatment of severe restless legs syndrome after failure of previous treatment: a double-blind, randomised, placebo-controlled trial with an open-label extension. Lancet Neurol. 2013;12:1141–50. doi: 10.1016/S1474-4422(13)70239-4. [DOI] [PubMed] [Google Scholar]
- 38.Atkinson MJ, Sinha A, Hass SL, et al. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12. doi: 10.1186/1477-7525-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 40.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166:565–71. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 41.Agency for Healthcare Research and Quality. Treatment for restless legs syndrome: clinician research summary. AHRQ Publication. 2013;12:EHC147–3. [Google Scholar]
- 42.Bayard S, Langenier MC, Dauvilliers Y. Decision-making, reward-seeking behaviors and dopamine agonist therapy in restless legs syndrome. Sleep. 2013;36:1501–7. doi: 10.5665/sleep.3044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cornelius JR, Tippmann-Peikert M, Slocumb NL, Frerichs CF, Silber MH. Impulse control disorders with the use of dopaminergic agents in restless legs syndrome: a case-control study. Sleep. 2010;33:81–7. [PMC free article] [PubMed] [Google Scholar]
- 44.Voon V, Potenza MN, Thomsen T. Medication-related impulse control and repetitive behaviors in Parkinson's disease. Curr Opin Neurol. 2007;20:484–92. doi: 10.1097/WCO.0b013e32826fbc8f. [DOI] [PubMed] [Google Scholar]
- 45.Evans AH, Butzkueven H. Dopamine agonist-induced pathological gambling in restless legs syndrome due to multiple sclerosis. Mov Disord. 2007;22:590–1. doi: 10.1002/mds.21303. [DOI] [PubMed] [Google Scholar]
- 46.Garcia-Borreguero D, Allen RP, Kohnen R, et al. Diagnostic standards for dopaminergic augmentation of restless legs syndrome: report from a World Association of Sleep Medicine-International Restless Legs Syndrome Study Group consensus conference at the Max Planck Institute. Sleep Med. 2007;8:520–30. doi: 10.1016/j.sleep.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 47.de Oliveira MM, Conti CF, Valbuza JS, de Carvalho LB, do Prado GF. The pharmacological treatment for uremic restless legs syndrome: evidence-based review. Mov Disord. 2010;25:1335–42. doi: 10.1002/mds.22955. [DOI] [PubMed] [Google Scholar]
- 48.Picchietti DL, Hensley JG, Bainbridge JL, et al. Consensus clinical practice guidelines for the diagnosis and treatment of restless legs syndrome/Willis-Ekbom disease during pregnancy and lactation. Sleep Med Rev. 2014 Nov 4; doi: 10.1016/j.smrv.2014.10.009. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 49.American Academy of Sleep Medicine. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. International classification of sleep disorders. [Google Scholar]



