Abstract
The American Academy of Sleep Medicine (AASM) commissioned a Workgroup to develop quality measures for the care of patients with narcolepsy. Following a comprehensive literature search, 306 publications were found addressing quality care or measures. Strength of association was graded between proposed process measures and desired outcomes. Following the AASM process for quality measure development, we identified three outcomes (including one outcome measure) and seven process measures. The first desired outcome was to reduce excessive daytime sleepiness by employing two process measures: quantifying sleepiness and initiating treatment. The second outcome was to improve the accuracy of diagnosis by employing the two process measures: completing both a comprehensive sleep history and an objective sleep assessment. The third outcome was to reduce adverse events through three steps: ensuring treatment follow-up, documenting medical comorbidities, and documenting safety measures counseling. All narcolepsy measures described in this report were developed by the Narcolepsy Quality Measures Work-group and approved by the AASM Quality Measures Task Force and the AASM Board of Directors. The AASM recommends the use of these measures as part of quality improvement programs that will enhance the ability to improve care for patients with narcolepsy.
Citation:
Krahn LE, Hershner S, Loeding LD, Maski KP, Rifkin DI, Selim B, Watson NF. Quality measures for the care of patients with narcolepsy. J Clin Sleep Med 2015;11(3):335–355.
Narcolepsy is one of the most intriguing causes of excessive daytime sleepiness. Narcolepsy (with cataplexy) affects approximately 25–50 per 100,000 people in the US.1 The prevalence of narcolepsy without cataplexy is higher still, yet the disorder remains under-recognized and under-diagnosed. Presently, narcolepsy treatment varies due to a heterogeneous presentation of symptoms and severity of disease among patients. Although narcolepsy is uncommon compared to other sleep disorders, the American Academy of Sleep Medicine (AASM) included it in the quality measure process because it is a disorder that generally results in significant daily dysfunction when not appropriately treated. The quality measures described in this position paper include children and adolescents in the targeted patient population, as 40% to 50% of adult patients report onset of symptoms before age 15 years.2,3 However, the Workgroup notes limitations in diagnostic testing and lack of level 1 evidence-based treatment studies in the pediatric population. Because of the paucity of clinical trials and FDA-approved treatments for narcolepsy for both pediatric and adult patients, the Workgroup believed that it was imperative to include off-label options in treatment plans.
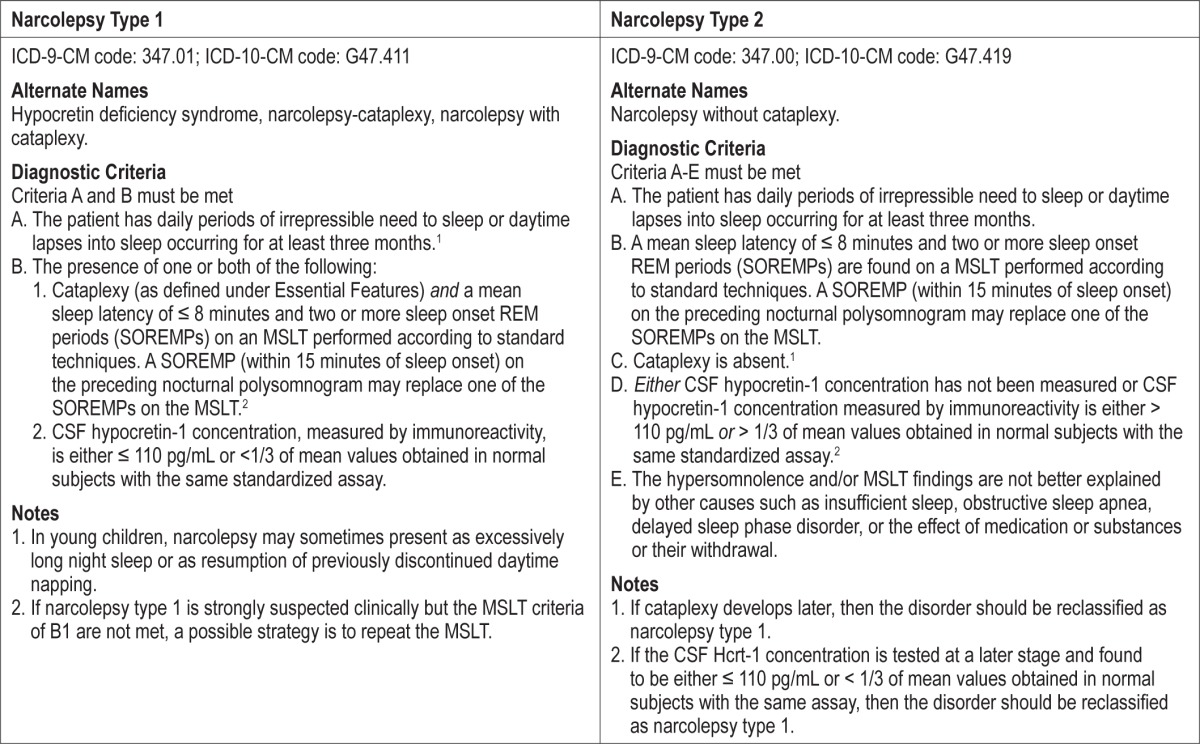
The International Classification of Sleep Disorders, Third Edition (ICSD-3) was used as the narcolepsy diagnostic reference. The ICSD-3 subdivides narcolepsy into type 1 and 2, with type 1 characterized by excessive daytime sleepiness, hypocretin deficiency syndrome, and signs of REM-sleep dissociation (e.g., cataplexy, hypnagogic and hypnopompic hallucinations, sleep paralysis) and type 2 characterized by excessive daytime sleepiness and abnormal manifestations of REM sleep on polysomnography/multiple sleep latency test (MSLT) (see Table 1).4
Table 1.
ICSD-3 diagnostic criteria for narcolepsy type 1 and 2.
The AASM commissioned Workgroups to develop quality care measures aimed at optimizing care for patients suffering from sleep-related disorders, including narcolepsy.5 These quality care measures focus on both outcomes and processes since both influence the care of the patient. Outcomes are often patient oriented, whereas processes are typically more controlled by an individual provider. The outcomes and processes detailed in this report were developed by the Narcolepsy Quality Measures Workgroup and received final approval from the AASM Quality Measures Task Force and the AASM Board of Directors.
METHODS
Literature Review
As described in the parent paper5, a comprehensive search identified publications addressing quality improvement, safety issues, and evidence-based treatment for narcolepsy. All searches were limited to articles published between 2002– 2013, pertaining to humans, and in English. Publication types such as newsletters, editorials, and case reports were excluded. A total of 306 articles were retrieved for review.
An additional search was conducted to identify clinical practice guidelines, measures, systematic reviews, meta-analyses, and consensus recommendations published by the AASM or other organizations or groups in the National Guidelines Clearinghouse, the National Quality Measures Clearinghouse, PubMed, EMBASE, PsycInfo, and the Cochrane Library pertaining to narcolepsy (and all associated MeSH terms). Searches were limited to articles published between 2002–2013, pertaining to humans with no age restriction, and in English. Other publication types noted above were excluded. Twelve additional articles were identified from this search. Workgroup members performed “pearling,” where references from full articles found through the literature search were examined to identify any additional relevant evidence, adding 9 articles.
The titles and abstracts of all articles were reviewed by two members of the Workgroup to identify papers relevant to quality improvement, safety and evidence-based treatment. Any disagreements were resolved by a third Workgroup member. Full articles of relevant publications were obtained and reviewed to identify and provide support for the quality measures.
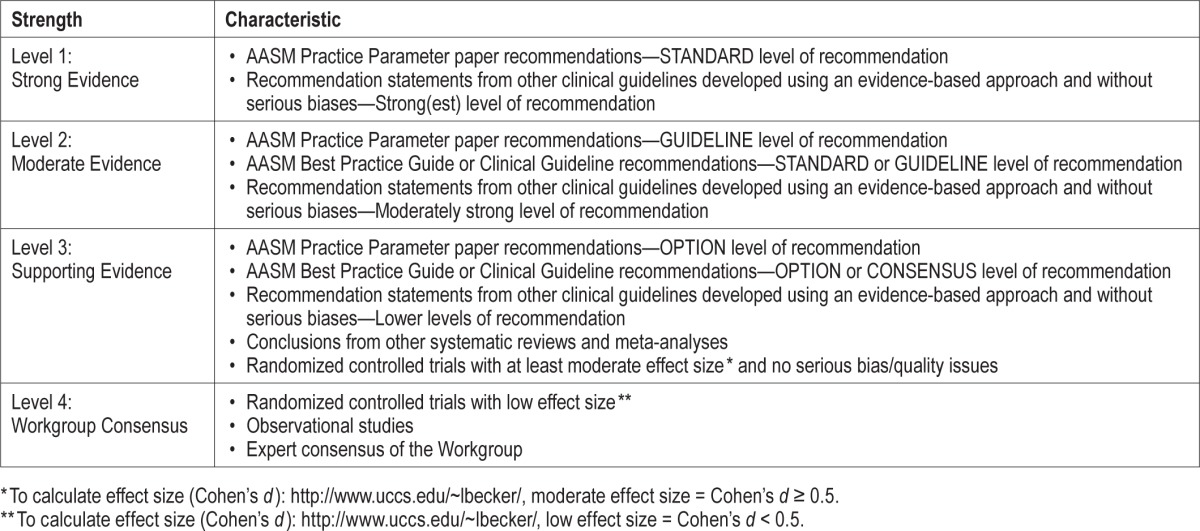
Workgroup members graded the evidence for strength of association between the proposed process and the desired outcome. For this, they used the grading scheme shown in Table 2.
Table 2.
Strength of association between process measure and desired outcome.
Measure Selection
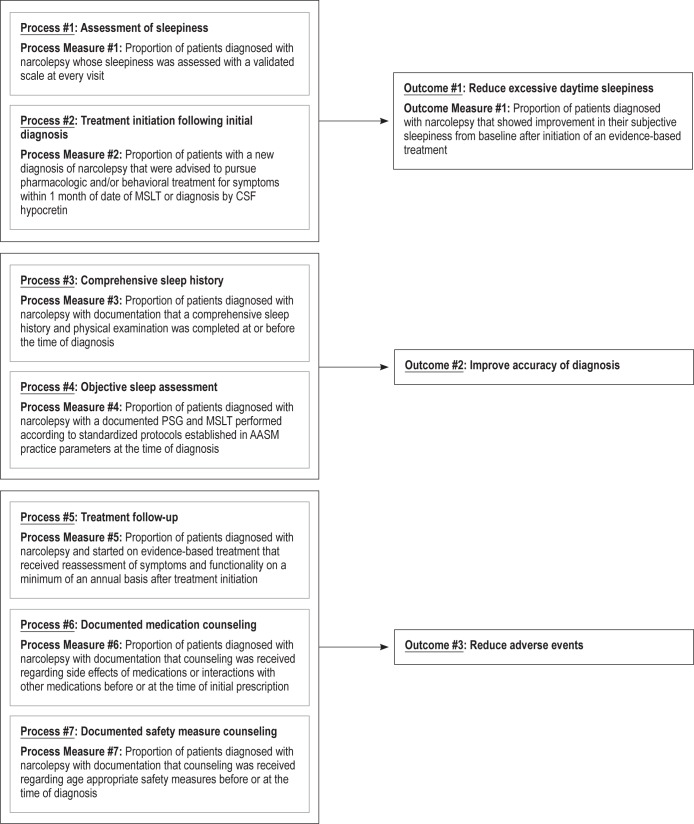
Possible outcome measures were identified using: published practice parameters, papers identified in the literature search, and Workgroup expertise. The Workgroup determined three outcomes were central to all narcolepsy patients: reduced excessive daytime sleepiness, improved accuracy of diagnosis, and avoiding adverse events (Figure 1). Other outcome measures were conceivable, for example, reducing cataplexy frequency or improving quality of life, but the Workgroup decided that they were not applicable to all patients with narcolepsy in clinical practice. The AASM Quality Measures Task Force determined that outcomes that could be tracked through a review of the medical records (reduce excessive daytime sleepiness) were designated “outcome measures,” while those that were goals but could not be quantified (improve the diagnosis of narcolepsy and reduce adverse effects) were listed simply as “outcomes.” Process measures were selected for each of the three outcomes. The technical specifications associated with each of these quality measures can be found in the Appendix. These specifications outline how to calculate an individual provider's performance in meeting these measures using a combination of diagnostic and CPT codes and chart review.
Figure 1. Narcolepsy quality measures driver diagram.
QUALITY MEASURES
Excessive daytime sleepiness is the cardinal symptom of narcolepsy and a reduction in daytime sleepiness is one of the most critical aspects in the management of narcolepsy.
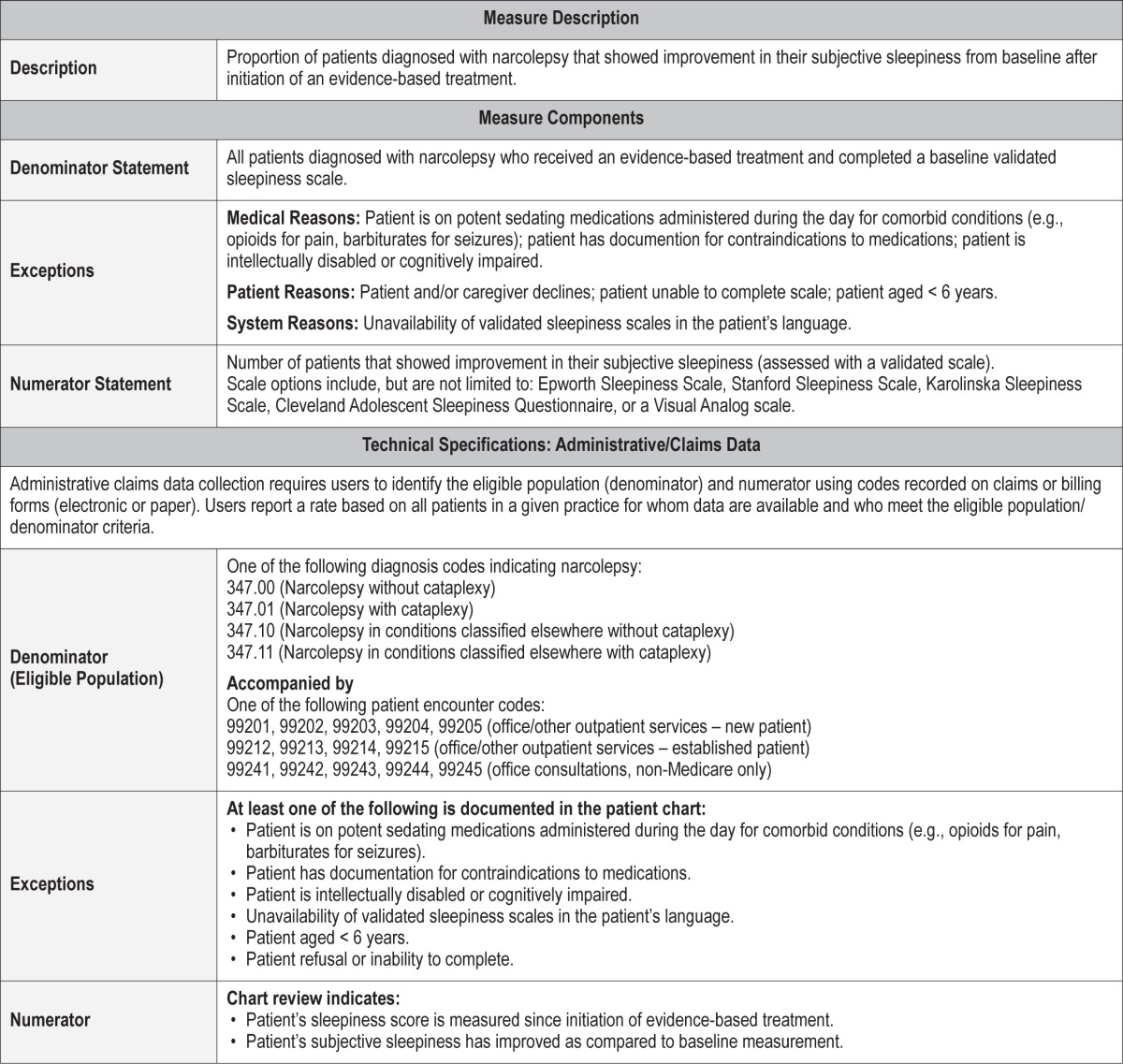
Outcome Measure 1 – Reduce Excessive Daytime Sleepiness
Description
Proportion of patients diagnosed with narcolepsy that showed improvement in their subjective sleepiness from baseline after initiation of an evidence-based treatment. This outcome measure is highly patient centered, given the implications for an individual of excessive daytime sleepiness for functioning and quality of life.
Excessive daytime sleepiness must be measured with a validated scale including, but not limited to, the Epworth Sleepiness Scale, Stanford Sleepiness Scale, Karolinska Sleepiness Scale, Cleveland Adolescent Sleepiness Questionnaire, or a Visual Analog Scale.
Exceptions and Exception Justifications
Medical Reasons: Patients on potent sedating medications administered during the day for comorbid conditions; patients documented for contraindications to medications; patients who are intellectually disabled or cognitively impaired.
A residual decrease in daytime alertness is not unexpected for patients on potent sedating medications, causing the Workgroup to identify this condition as an exception. For example, patients with narcolepsy on potent sedating medications (e.g. opioid for pain, barbiturate for seizures) administered during the day for comorbid conditions would not be included in this measure. Other exceptions would include documented contraindications for pharmacologic treatment for excessive daytime sleepiness.
Patient Reasons: Patient and/or caregiver declines; patient unable to complete scale; patients aged less than six years when children may still need daytime naps.
System Reasons: Unavailability of validated sleepiness scales in the patient's language.
Supporting Evidence and Rationale
Treatment objectives should include control of sleepiness and other sleep related symptoms when present. (Standard)6 [Level 1]
“It has been previously recommended that a major objective of treatment of narcolepsy should be to alleviate daytime sleepiness. The goal should be to produce the fullest possible return of normal function for patients at work, at school, at home, and socially.”6
Opportunities for Improvement/Gaps
Poor communication and fragmented health care systems interfere with the patient learning of their diagnosis and treatment options. Narcolepsy patients with comorbid conditions should be treated without using medications that could exacerbate excessive daytime sleepiness.
Issues Addressed During Development
Consensus was reached without difficulty that reduction of excessive daytime sleepiness was a pivotal outcome for all patients with narcolepsy. Thus debate centered more on the process measures such as patient self-reports versus physiological tools like the Maintenance of Wakefulness Test. The Workgroup also discussed whether to exclude any subgroups such as patients requiring sedating medications for a comorbid condition. Children were not excluded as accurate information on excessive daytime sleepiness can be obtained from parents, caregivers, and/or teachers. Outcome limitations were discussed including poor correlation between objective and subjective changes in excessive daytime sleepiness, and a lack of consensus regarding degree in scale's change considered a successful improvement. The Workgroup agreed that a reduction in excessive daytime sleepiness was acceptable (e.g., a declining Epworth Sleepiness Scale score) without specifying the necessary amount of improvement.
The variety of acceptable assessment tools, their methodological limitations, and each patient's individual experience makes it challenging to mandate the degree of improvement.
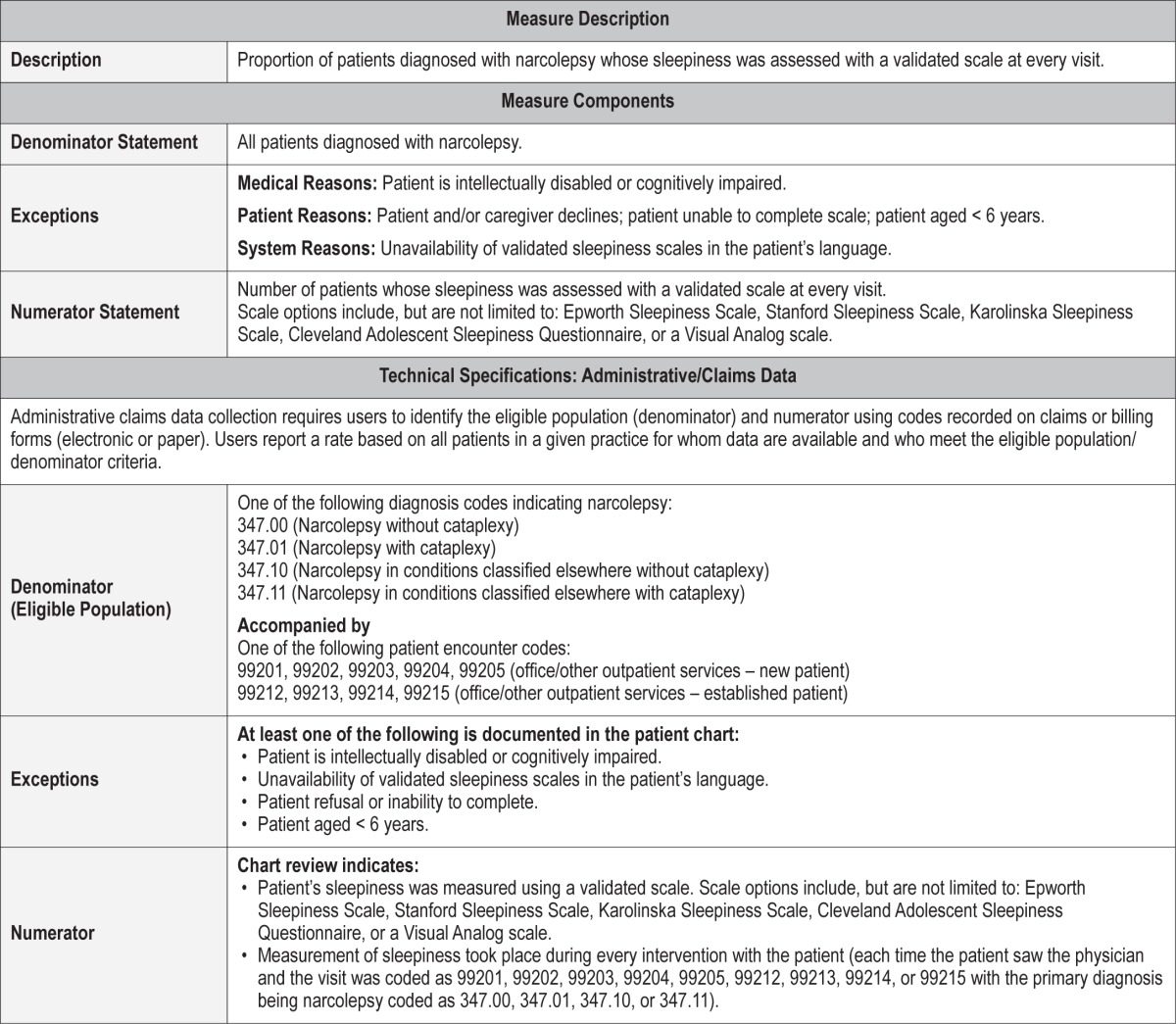
Process Measure 1 – Assessment of Sleepiness
Description
Proportion of patients diagnosed with narcolepsy whose sleepiness was assessed with a validated scale at every visit.
Excessive daytime sleepiness must be measured with a validated scale including, but not limited to, the Epworth Sleepiness Scale, Stanford Sleepiness Scale, Karolinska Sleepiness Scale, Cleveland Adolescent Sleepiness Questionnaire, or a Visual Analog Scale. Though not formally validated, the modified Epworth Sleepiness Scale has been used in a number of clinical research studies as well as in clinical practice to assess sleepiness in children ages 6–16 years of age, thus demonstrating adequate construct validity. Clinically relevant measures, such as the Clinical Global Impression of Change (CGI-c) used in many clinical trials of therapeutic agents may also be used.7
Exceptions and Exception Justifications
Medical Reasons: Patients who are intellectually disabled or cognitively impaired.
Patient Reasons: Patient and/or caregiver declines; patient unable to complete scale; patients aged less than six years when children may still need daytime naps.
System Reasons: Unavailability of validated sleepiness scales in the patient's language.
Supporting Evidence and Rationale
The AASM Practice Parameter for the treatment of narcolepsy discusses “control of sleepiness” but a process for measuring excessive daytime sleepiness (EDS) is not specified. Treatment objectives should include control of sleepiness and other sleep related symptoms when present. (Standard)6 [Level 1]
The Epworth Sleepiness Scale (ESS) is used to assess the extent to which sleepiness interferes with daily activities. The ESS is a self-administered instrument that assesses the likelihood of dozing or falling asleep during 8 situations of daily life (e.g., watching TV; in a car, while stopped for a few minutes in traffic), rated on a scale of 0 to 3, with 3 indicating a high chance of dozing. The total score is the sum of scores for the 8 items. An improvement in wakefulness corresponds to a reduction in the ESS total score; a score ≥ 10 was used to define excessive sleepiness.8 [Level 4]
Relationship to Desired Outcome
Using a clinically relevant tool to assess sleepiness in addition to a thorough clinical history is essential to ensuring a more accurate assessment of sleepiness in determining whether the therapy has been successful.
Opportunities for Improvement/Gaps
Future work could focus on developing additional tools for measuring excessive daytime sleepiness.
Issues Addressed During Development
The Workgroup discussed at length the limitations of validated subjective sleepiness scales and specifically the use of validated scales in the clinical forum, but concluded that these tools were the best options available to clinicians. In the years to come new assessment scales, and hopefully scales to address the sleepiness inherent in narcolepsy, may be developed and validated, making a comprehensive list of all appropriate tools impractical. The aim was to promote process measures that do not create an undue burden. Objective measures like the maintenance of wakefulness test are therefore not appropriate as process measures in routine clinical practice. There was recognition that self-report measures and objective tools do not correlate well and may assess different dimensions of excessive daytime sleepiness.
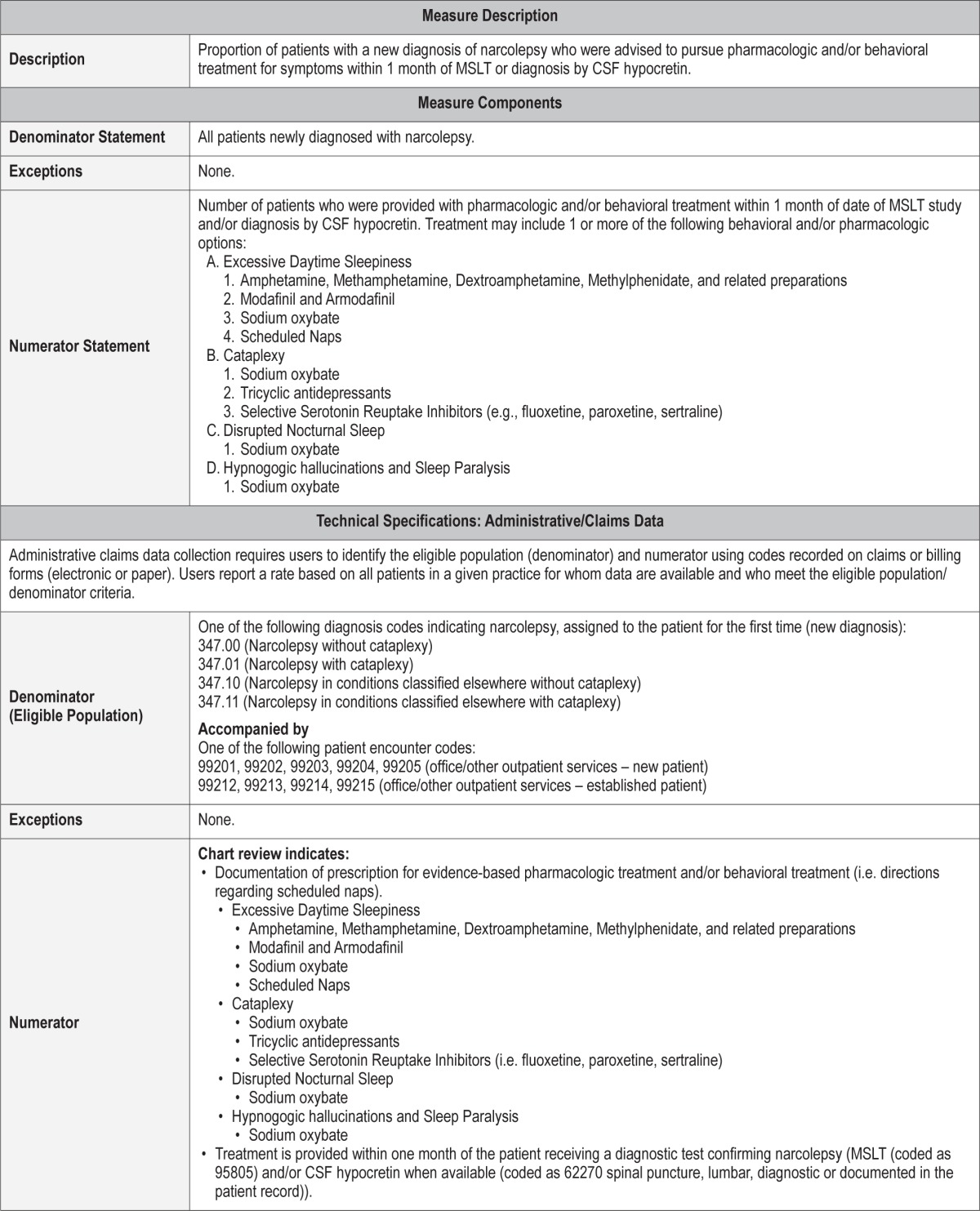
Process Measure 2 – Treatment Initiation Following Initial Diagnosis
Description
Proportion of patients with a new diagnosis of narcolepsy that were advised to pursue pharmacologic and/or behavioral treatment for symptoms within 1 month of MSLT or diagnosis by CSF hypocretin.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Treatment objectives should include control of sleepiness and other sleep related symptoms when present. (Standard)6 [Level 1]
Treatment should alleviate daytime sleepiness in order to optimize patients' daily functioning at work, school, home, and personal life. The practice parameter regarding treatment of narcolepsy also specifies that treatment goals should control nocturnal symptoms of disrupted sleep, cataplexy, hypnagogic hallucinations, and sleep paralysis, when present and troublesome to patients with narcolepsy.6
The following are treatment options for narcolepsy:
Modafinil is effective for treatment of daytime sleepiness due to narcolepsy [4.1.1.2]. (Standard)6 [Level 1] Armodafinil is the R-enantiomer of modafinil and has differing pharmacokinetics than modafinil. It also has been shown to be effective for the treatment of excessive daytime sleepiness in patients with narcolepsy. [Level 4]9,10
Sodium oxybate is effective for treatment of cataplexy, daytime sleepiness, and disrupted sleep due to narcolepsy [4.2.1, 4.1.1.3, 4.3.1]. (Standard)6 [Level 1] Sodium oxybate may be effective for treatment of hypnagogic hallucinations and sleep paralysis [4.4.1]. (Option)6 [Level 3]
Amphetamine, methamphetamine, dextroamphetamine, and methylphenidate are effective for treatment of daytime sleepiness due to narcolepsy [4.1.1.1]. (Guideline)6 [Level 2]
Selegiline may be an effective treatment for cataplexy and daytime sleepiness [4.1.1.4]. (Option)6 [Level 3]
Ritanserin may be effective treatment of daytime sleepiness due to narcolepsy [4.1.1.6]. (Option)6 [Level 3]
Scheduled naps can be beneficial to combat sleepiness but seldom suffice as primary therapy for narcolepsy [4.1.2]. (Guideline)6 [Level 2]
Tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), venlafaxine, and reboxetine may be effective treatment for cataplexy [4.2.2]. (Guideline)6 [Level 2]
Tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs), and venlafaxine may be effective treatment for treatment of sleep paralysis and hypnagogic hallucinations [4.4.2]. (Option)6 [Level 3]
Effective treatment of excessive daytime sleepiness has been shown to improve patient functional status.11 [Level 4] and quality of life.12 [Level 4] There is limited level 1 evidence to advise on specific treatment of special populations such as children, pregnant women and breastfeeding mothers. New treatments for narcolepsy may be developed in the future, and over time this measure will need to be updated as new treatments become available.
Relationship to Desired Outcome
Excessive daytime sleepiness has a significant detrimental impact on psychological, social, academic, and vocational function and personal safety.6 Starting treatment within 1 month of the date of the MSLT study or diagnosis by CSF hypocretin should reduce excessive daytime sleepiness.
Opportunities for Improvement/Gaps
Research regarding timelines for treatment of narcolepsy is lacking.
Issues Addressed During Development
The decision to recommend treatment initiation within a 1-month time period was based on discussion of Workgroup members and their expert consensus, as there is no relevant literature to inform a more evidence-based time frame. The Workgroup notes that treatment initiation should be as soon as possible after a confirmed diagnosis but attempts to set a baseline for acceptable clinical practice. However, the Workgroup recognizes that a 1-month follow-up visit after diagnostic testing may not be feasible in all practice types. In such cases, the Workgroup recommends practitioner's document a phone call or correspondence with the patient informing them of their diagnosis and recommended treatment plan.
The Workgroup recognizes that improvement in symptoms such as excessive daytime sleepiness will not necessarily translate into improved quality of life. In one study, subjective sleepiness decreased significantly after treatment of narcolepsy, but scores on many quality of life domains did not significantly differ between treatment and drug-naive patients.13 In contrast, other double-blind controlled studies have shown more robust changes in quality of life measures in response to treatment.11,12
Furthermore, treatment may improve, but not eliminate, symptoms such as excessive daytime sleepiness.14 Additional counseling on residual symptoms and symptom management in work, school, or driving setting may be necessary at the time of treatment initiation.
Outcome 2 – Improve Accuracy of Diagnosis
Description
Outcome 2, which is not a measured outcome but rather a broad goal of care, is improved accuracy of narcolepsy diagnosis. Clearly, diagnostic accuracy is a critical aspect of narcolepsy management. Misdiagnosis of narcolepsy may occur for multiple reasons with substantial consequences for patients.
Supporting Evidence and Rationale
Appropriate and accurate diagnostic testing culminating in a diagnosis of narcolepsy is the best guidance for counseling, management, and the development of long-term treatment plans. An erroneous diagnosis of narcolepsy can occur for multiple reasons and can result in a lost opportunity to treat the causative etiology of a patient's excessive daytime sleepiness.
Issues Addressed During Development
The Workgroup felt strongly that improving the accuracy of diagnosis for narcolepsy is an important outcome; however, it was recognized that directly measuring and tracking this outcome would be challenging and burdensome beyond the control of a physician or reporting facility.
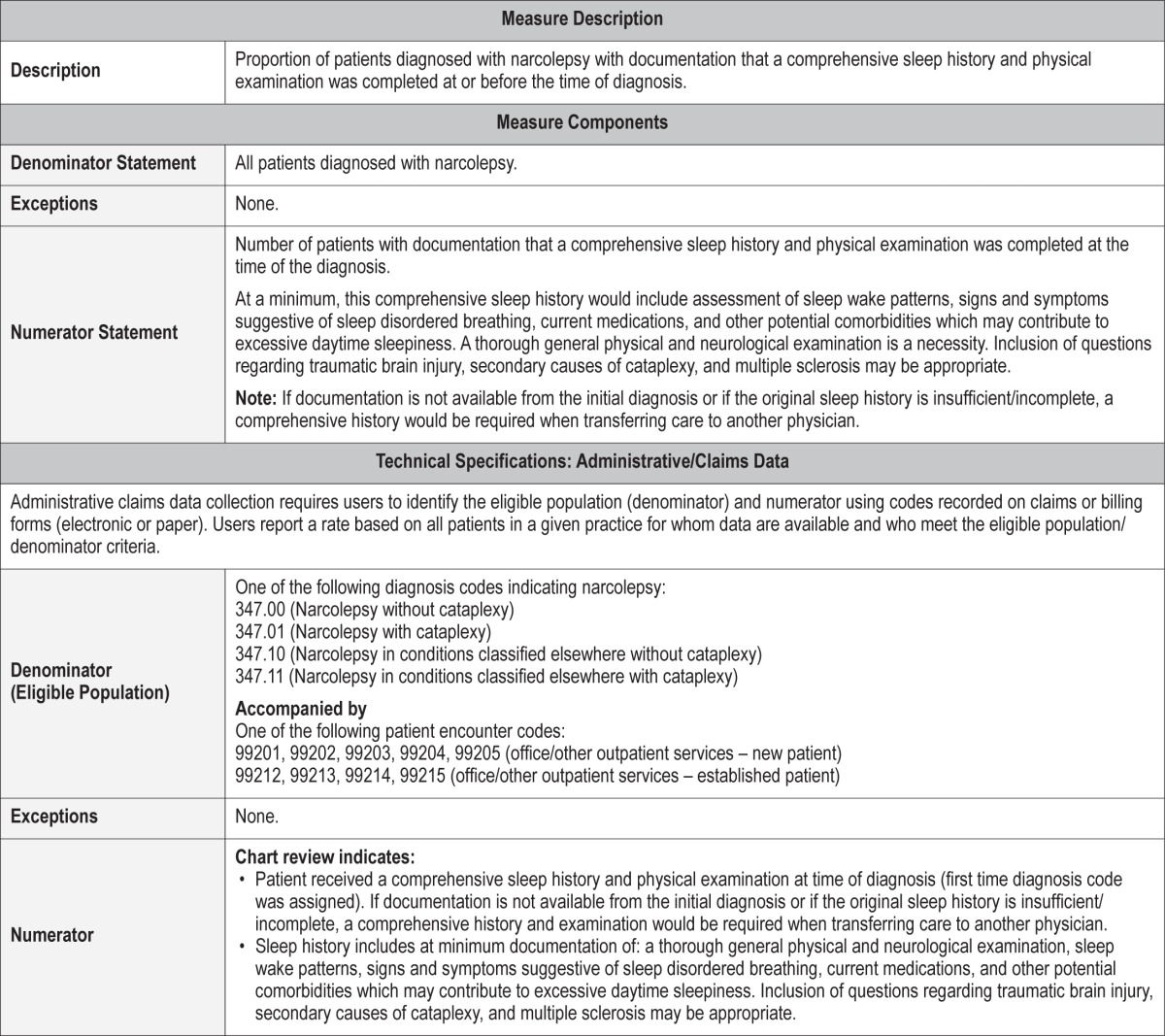
Process Measure 3 – Comprehensive Sleep History and Physical Exam
Description
Proportion of patients diagnosed with narcolepsy with documentation that a comprehensive sleep history and physical examination was completed at or before the time of diagnosis.
An accurate diagnosis of narcolepsy requires that other potential causes or contributing factors for excessive daytime sleepiness are considered, evaluated, and adequately treated prior to diagnostic testing. A comprehensive sleep history critically evaluates other potential causes for excessive daytime sleepiness, cataplexy, and sleep-onset REM periods. The history at minimum should review sleep-wake patterns, signs of sleep disordered breathing, and current medications. Inclusion of questions regarding traumatic brain injury, secondary causes of cataplexy, and multiple sclerosis may be appropriate. A thorough general physical and neurological examination is a necessity. Ideally, both are obtained prior to diagnostic testing. In circumstances of a transfer of medical care, a thorough review of the medical record to assure that a sleep history and physical examination was obtained at the time of diagnosis would satisfy this measure. If documentation is unavailable or incomplete, the patient or his/her parents/caretakers can provide the history at the time of transfer of care. The measure can be satisfied by referring the patient to a specialist for a general physical and neurological examination. [Level 4]
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
A comprehensive sleep history that critically evaluates other potential causes for excessive daytime sleepiness and/or cataplexy is essential for an accurate diagnosis of narcolepsy. [Level 4]
Exclusion of other potential causative disorders is essential, as sleepiness may be secondary to obstructive sleep apnea, insufficient sleep syndrome, shift work, the effects of substances or medications, or other sleep disorders. Many of these conditions, including depression, can result in early onset REM sleep as well.15 [Level 4]
Many other conditions produce sleepiness and can mimic or coexist with a hypersomnia of central origin.6 The most common cause of excessive daytime sleepiness (EDS) in modern society is likely due to a combination of insufficient sleep, inadequate sleep hygiene, and work schedules. Many other disorders are associated with excessive daytime sleepiness, including sleep disordered breathing disorders, circa-dian rhythm sleep disorders, medication-induced sleepiness, periodic limb movement disorder, and sleepiness associated with insomnia.
An adequate physical exam can evaluate for other causes of narcolepsy.
A variety of medical and neurological conditions are associated with hypersomnia, including Parkinson disease and other neurodegenerative conditions, head trauma, stroke, encephalitis, inflammatory conditions, metabolic and toxic conditions, tumors and other lesions of the central nervous system, and genetic disorders. Examples of genetic disorders associated with hypersomnia include myotonic dystrophy, Prader-Willi syndrome, Niemann Pick type C disease, and fragile X syndrome.14 [Level 3]
In a series of children with narcolepsy with cataplexy neurological examination revealed frequently overlapping abnormal findings in 17 cases (44%): 16 patients (41%) had mildly reduced muscle tone overall, and 10 subjects (26%) had an abnormal gait, characterized by wide-based swaying. Overall, nine children (23%) had a combination of hypotonia and abnormal gait, whereas seven (18%) and one (3%) presented only mild hypotonia or abnormal gait, respectively.16 [Level 4]
A systematic review of physical examination findings was not present in a 2005 case series of secondary narcolepsy done by Nishino et al.,17 but abnormal physical examination findings were described in multiple cases and were elucidatory that a secondary cause of narcolepsy was possible. Narcolepsy symptoms can also occur during the course of other conditions (e.g., secondary narcolepsy). This case series defined secondary narcolepsy as those cases that meet the International Sleep Disorders Narcolepsy Criteria, which were associated with a significant underlying neurological disorder that accounts for excessive daytime sleepiness (EDS). To date, this case series counted 116 secondary cases of narcolepsy reported in literature. As several authors previously reported, inherited disorders, tumors, and head trauma are the three most frequent causes for secondary narcolepsy. Of the 116 cases, 10 are associated with multiple sclerosis, one case of acute disseminated encephalomyelitis, and relatively rare cases were reported with vascular disorders, encephalitis and degeneration, and heredo-degenerative disorder (three cases in a family).17
Relationship to Desired Outcome
A comprehensive sleep history and physical examination including neurological elements improves the accuracy of the diagnosis of narcolepsy by excluding other etiologies for excessive daytime sleepiness, sleep-onset REM periods, and cataplexy-like symptoms. The sleep history is vital in the evaluation of cataplexy as it can exclude cataplexy-like symptoms that are suggestive of cataplexy but do not meet diagnostic criteria.4
Opportunities for Improvement/Gaps
A sleep history and physical examination that evaluates other etiologies for excessive daytime sleepiness, cataplexy, and sleep-onset REM periods, may circumvent an inaccurate diagnosis, avoid potential inappropriate medical or medication interventions, and most importantly, provide an opportunity to treat the underlying causative disorder.
Issues Addressed During Development
There were several areas of concern in the development of this measure. The primary concern was what constituted a “comprehensive” sleep history and physical examination including neurological elements. The consensus was reached that a sleep history and physical examination must evaluate other potential causes of excessive daytime sleepiness, cataplexy-like symptoms, and sleep onset-REM periods. The history at minimum should review sleep-wake patterns, signs and symptoms of sleep disordered breathing, and current medications. This is the minimal history required, and although not mandatory, it is highly recommended that questions to help exclude evidence of traumatic brain injury, secondary causes of cataplexy or similar symptoms, and multiple sclerosis be included. The definition of an adequate physical exam was also a source of debate. The primary goal again is to exclude a secondary cause of narcolepsy or symptoms that might otherwise be construed as cataplexy; therefore, a complete general medical and neurological exam is necessary in all patients when a diagnosis of narcolepsy is being considered.
The optimal time to obtain the sleep history and physical examination is prior to diagnostic testing. There was debate about the term; “at the time of diagnosis,” which was thought to be when the PSG/MSLT was reviewed with the patient and the patient was given the formal diagnosis of narcolepsy. Therefore, the history and examination should be completed before or during this appointment.
An additional area of concern was related to patients that transfer their care from another provider. This measure could be satisfactorily completed by the new physician at the time of transfer of medical care by a thorough review of the medical record, or by reviewing the initial sleep history as provided by the patient, and then completing a general physical and neurological examination.
Feedback on this process measure was generally positive, with providers agreeing that an accurate diagnosis is a necessary requirement for quality care of the narcoleptic patient.
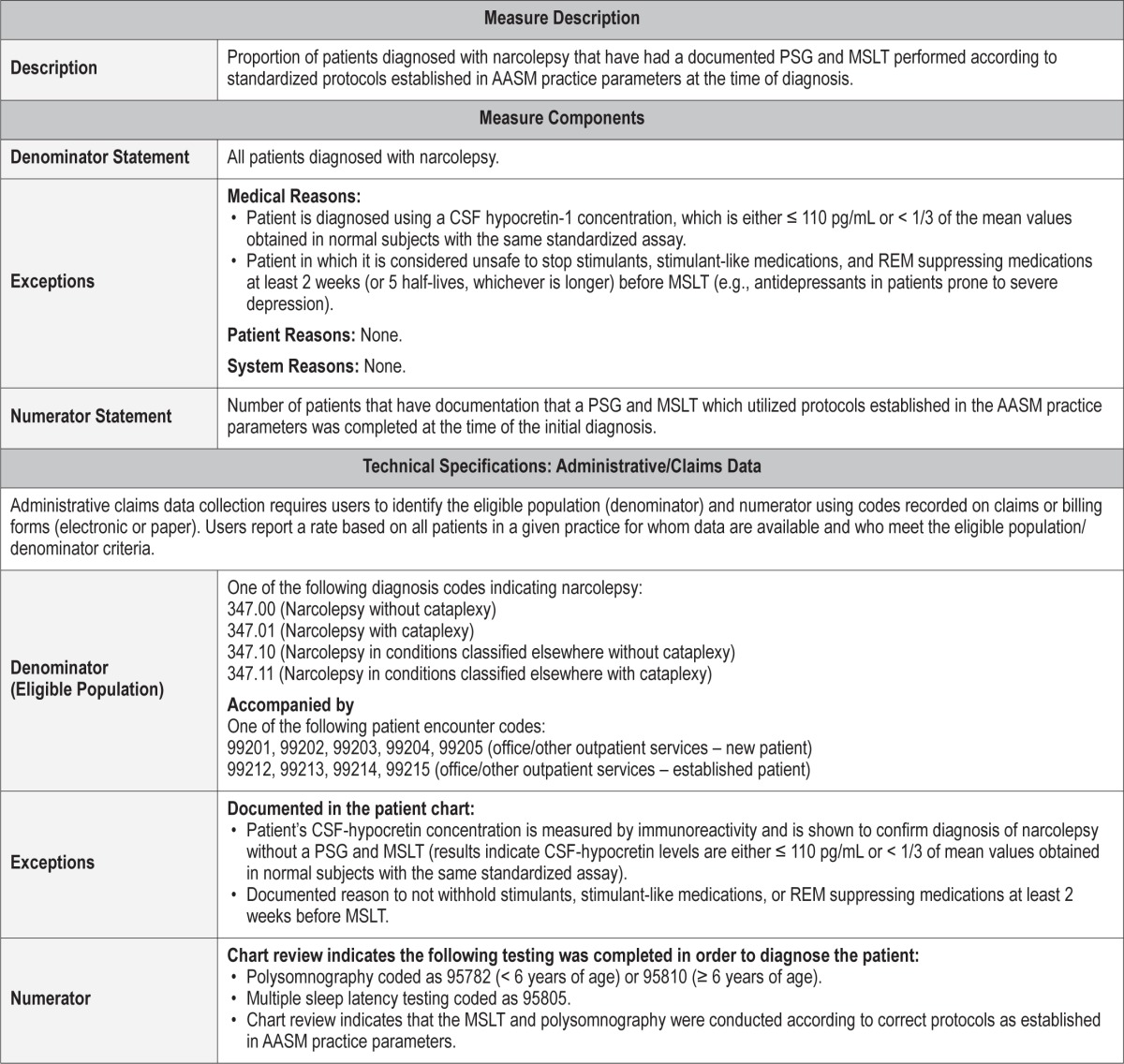
Process Measure 4 – Objective Sleep Assessment
Description
Proportion of patients diagnosed with narcolepsy that have had a documented PSG and MSLT performed according to standardized protocols established in AASM practice parameters at the time of diagnosis.
To assure and improve the accuracy of a narcolepsy diagnosis, it is vital that diagnostic testing is performed with established protocols. This measure will be satisfied by documentation that a thorough review of PSG/MSLT was performed and that established protocols were followed. Protocols delineated in AASM Practice Parameters help exclude other potential causative disorders of excessive daytime sleepiness and sleep-onset REM periods. If protocol errors occur, repeat testing may be considered before confirming the diagnosis of narcolepsy. If for some reason, established PSG/MSLT protocols could not be followed, the rationale for deviation should be documented with an explanation of the diagnostic implications. In circumstances of a transfer of medical care, documentation that the PSG/MSLT were completed according to AASM protocols would satisfy this measure.
Exceptions and Exception Justifications
Medical Reasons: Patients diagnosed using a CSF hypo-cretin-1 concentration, which is either ≤ 110 pg/mL or < 1/3 of the mean values obtained in normal subjects with the same standardized assay.
If it were deemed that antidepressants or other medications could not be safely discontinued for the PSG/MLST, this rationale needs to be clearly documented. This not uncommon clinical dilemma justifies an exception allowing these patients to be excluded.
Cataplexy is not an exclusion for this measure.4 The presence of cataplexy without the presence of two sleep-onset REM periods does not meet current diagnostic criteria for narcolepsy. Therefore, objective confirmation with PSG/MSLT is required for a new diagnosis of narcolepsy. In an established patient, diagnosed by the presence of cataplexy, who did not have a PSG/MSLT or whose PSG/MSLT did not meet diagnostic criteria for narcolepsy, repeat testing could be considered, but is not required, and these patients would be excluded from this measure.
If established protocols were not followed (e.g., safety issues precluding antidepressant discontinuation), adequate documentation for the reason, and the diagnostic implications should be included in the patients' medical records, and these patients would be excluded from this measure.
Patient Reasons: None.
System Reasons: None.
The development of other objective diagnostic testing in the future could preclude the need for a polysomnogram and MSLT.
Supporting Evidence and Rationale
An accurate diagnosis of narcolepsy is critical to prevent missing other potentially treatable causes of excessive daytime sleepiness. The MSLT is also indicated in children as part of the evaluation for suspected narcolepsy. (Standard) [Level 1]18 To provide a valid assessment of sleepiness or wakefulness the MSLT must be performed under appropriate conditions using proper recording techniques and accepted protocols, with interpretation by a qualified and experienced clinician. Use of standard protocols for the MSLT improves the validity and reliability of results.19
Errors in protocols may result in a false positive test and a lost opportunity to treat the actual cause or contributing factor of a patient's excessive daytime sleepiness. For example, shift-work and the presence of REM suppressing medications are associated with sleep-onset REM periods (SOREMPs).20 Therefore, if clinically safe, and in collaboration with the prescribing physician, it is important that antidepressant medications are held for 14 days or 5 half-lives before the MSLT. SOREMPs do not occur exclusively in patients with narcolepsy; thus it is important to rule out or treat other sleep disorders before evaluating SOREMPs in the diagnosis of narcolepsy. Examples of other sleep disorders associated with SOREMPs include obstructive sleep apnea, or any condition associated with reduced nocturnal REM sleep leading to “REM rebound” during the day.19,21
Relationship to Desired Outcome
Following established protocols on the PSG/MSLT improves the accuracy of diagnostic testing for narcolepsy and aids in excluding other treatable reasons for excessive daytime sleepiness.
Opportunities for Improvement/Gaps
Accurate diagnostic testing culminating in a diagnosis of narcolepsy is the best guidance for counseling, management, and the development of long-term treatment plans. An inaccurate diagnosis of narcolepsy can occur when established protocols are not followed, which can result in a lost opportunity to treat the causative etiology of a patient's sleepiness.
Issues Addressed During Development
There were few areas of concern in the development of this measure, including which established protocol should be referenced. It was decided to use the AASM practice parameters, and updates to the practice parameters would still be applicable. The salient details of the protocol were included in this measure to educate and reinforce proper protocol.
Another area of debate was the need to align this measure with the AASM Practice Parameters and the International Classification of Sleep Disorders, Third Edition (ICSD-3). The major issue with the ICSD-3 is that cataplexy can no longer be used to clinically diagnose narcolepsy. Therefore, this measure mandates that a new diagnosis of narcolepsy must have objective testing with either a PSG/MSLT or CSF hypocretin. Established patients diagnosed by the presence of cataplexy who did not have a PSG/MSLT, or whose PSG/MSLT did not meet diagnostic criteria for narcolepsy, do not require testing and will not be included in this process measure. A 15-minute sleep-onset REM period (SOREMP) during the baseline polysomnogram can be used as one of the SOREMPs to meet diagnostic criteria. Lastly, there are no normative data regarding mean sleep latency time in preschool children. The ICSD-3 states that if the MSLT shows equivocal results, repeating it after a time interval may be helpful.
Another issue is the term “diagnostic testing.” This measure references both the PSG/MSLT and the CSF hypocretin assay, but future diagnostic tests may be developed. Therefore, “the development of objective diagnostic testing in the future could preclude the need for a polysomnogram and MSLT” was included.
Feedback indicated that providers thought that this measure was important and liked the use of the practice parameters. Some people were concerned regarding the utilization of actigraphy and sleep logs and the amount of detail to include when describing the protocols. The entire details of the protocol will not be included in the measure.
Outcome 3 – Reduce Adverse Events
Description
Outcome 3, which is not a measured outcome but rather a broad goal of care, is to reduce adverse events. Avoiding adverse events and preventing harm to a patient is a core tenet of health care.
Supporting Evidence and Rationale
While no convenient measure exists, this goal of providing adequate follow-up, education about medications, and counseling to minimize complications are an important part of any quality assurance program.
Issues Addressed During Development
The Workgroup felt strongly that reducing adverse events for narcolepsy is an important outcome; however, it was recognized that directly measuring and tracking this outcome would be challenging and burdensome beyond the control of a physician or reporting facility.
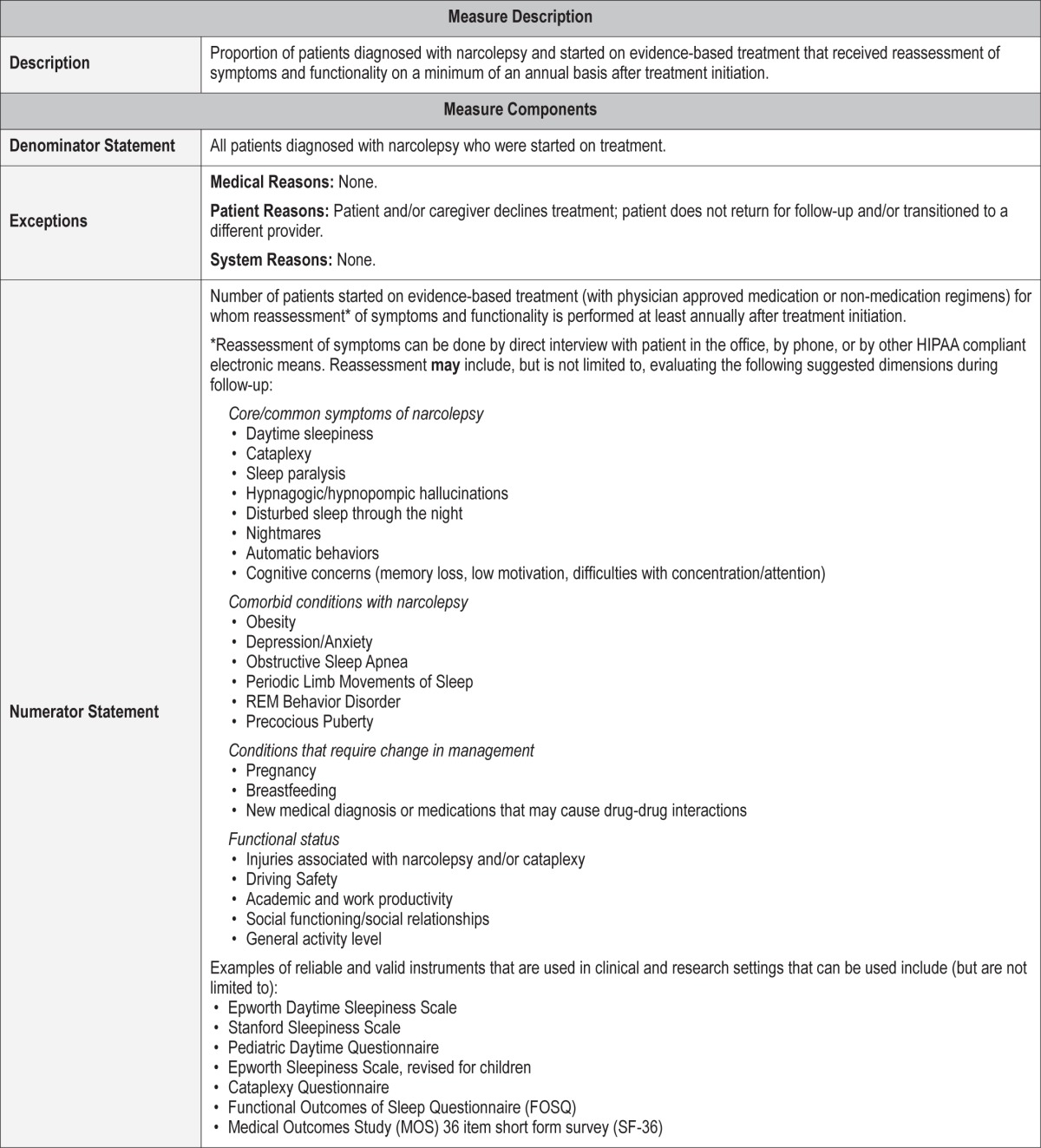
Process Measure 5 – Treatment Follow-Up
Description
Proportion of patients diagnosed with narcolepsy and started on evidence-based treatment who received reassessment of symptoms and functionality on a minimum of an annual basis after treatment initiation.
Reassessment of symptoms and treatments would ideally be done in a clinic office setting, but the Workgroup recognizes that documented phone calls, emails, or other forms of communication also may provide sufficient communication.
Exceptions and Exception Justifications
Medical Reasons: None.
Patient Reasons: Patient and/or caregiver declines treatment; patients who do not return for follow-up and/or transitioned to a different provider.
System Reasons: None.
Supporting Evidence and Rationale
The foundation for this process measure is based on clinical practice guidelines. Successful treatment of narcolepsy requires individual tailoring of therapy to produce the fullest possible return of normal function, and regular follow-up to monitor response to treatment.6
Regular follow-up of patients with narcolepsy is necessary to monitor response to treatment, to respond to potential side effects of medications, and to enhance the patient's adaptation to the disorder [4.10] (Standard).6 [Level 1] Regular follow-up is useful in order to monitor response to treatment, to assess presence of comorbid sleep disorders such as obstructive sleep apnea or periodic limb movement disorder, and address the psychosocial issues that often arise.14
Patients with narcolepsy have high comorbidity of medical conditions and psychiatric disorders that need to be addressed when developing a treatment plan.22 [Level 4]
Obesity affects more than 50% of narcoleptic children, mostly younger at disease onset, and has a deleterious impact on sleep quality as well as on school attendance.23 [Level 4]
Relationship to Desired Outcome
Adequate follow up is necessary to ensure treatment efficacy for symptoms including excessive daytime sleepiness and medication side effects. Follow-up visits also allow physicians to monitor patient safety in a timely fashion (e.g., monitor if medication side effects or drug-drug interactions are present), assess efficacy of treatment, determine tolerance effects to stimulants, evaluate driving safety on current treatment regimen, readjust treatment plan if the patient is pregnant/breast-feeding, as well as evaluate for the development and severity of comorbid conditions.
Opportunities for Improvement/Gaps
While no evidence can be cited showing that gaps in follow-up care exist, timely and high quality follow-up care produce beneficial effects for a range of chronic diseases.24–26 Missed appointments result in reductions in the continuity and effectiveness of health care delivery, monitoring of health status, and increased cost of care.27
Issues Addressed During Development
The time frame for follow-up was based on the Workgroup's expert consensus, as there is no relevant literature on timeliness of care in this population. Ideally, the Workgroup felt that treatment follow-up should be at least 3 months after treatment initiation but wanted to set a baseline for acceptable clinical practice. The Workgroup recognizes that access may limit follow-up visits. Consequently, the Workgroup specified that documented phone and institution-approved communication might be sufficient to assess treatment efficacy. However, the Workgroup considers follow-up clinical visits more clinically useful, allowing the provider to answer patient questions and concerns in an efficient and timely manner and evaluate bio-metrics such as weight and blood pressure for those on stimulant medications.
Stakeholders expressed concerns that annual visits or check-ins with patients who had initiated treatment would not be timely enough for good patient care. The Workgroup has set an upper limit for what constitutes timely care, specifying that the interval time between diagnosis and a follow-up clinic visit should be no longer than one year. The Workgroup encourages earlier and more frequent reassessments as needed.
Process Measure 6 – Documented Medication Counseling
Description
Proportion of patients diagnosed with narcolepsy with documentation that counseling was received regarding side effects of medications or interactions with other medications before or at the time of initial prescription.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
The current statistics regarding the lag-time between the time of diagnosis to initiation of treatment for narcolepsy is not known; however, the Workgroup agrees that treatment should be initiated as soon as possible. The treatment of narcolepsy requires use of drug classes with high side-effect potential. In the pediatric population, treatment may include medications whose safety and efficacy have not been formally studied and/ or carry black box warnings regarding risks of suicidal behavior/ideations in those with a history of psychiatric disorders (e.g., fluoxetine, venlafaxine).14 Tolerance and abuse of stimulants or sedative/hypnotics may occur with the use of antidepressants. Modafinil (and armodafinil) may reduce hormonal birth control efficacy, and inappropriate use of sodium oxybate may lead to respiratory depression, coma, or even death. Thus, good communication between the clinicians and patients (and their parents/caregivers in the case of pediatric patients) is vital to provide important information regarding proper medication use, potential side effects, and a safety plan when necessary.
Regular follow-up of patients with hypersomnia of central origin is necessary to monitor response to treatment, to respond to potential side effects of medications, and to enhance the patient's adaptation to the disorder [4.10] (Standard).6 [Level 1]
Tolerance to amphetamine may develop in up to one-third of patients.14,28 [Level 4]
Relationship to Desired Outcome
Medications are often used to treat the symptoms of narcolepsy, including hypersomnolence, cataplexy, and sleep fragmentation. Through patient counseling of side effects and potential drug interactions, adverse events such as suicide, unwanted pregnancy, and addiction can be reduced.
Opportunities for Improvement/Gaps
Potential side effects and drug interaction counseling is important following initiation of any medication. The medications used in the management of narcolepsy are of particular concern because of the potential risks involved. Federally controlled substances are often used in this patient population including sodium oxybate, a schedule I drug with a bifurcated schedule III prescription drug use provision. The sodium oxybate risk management program, which includes compulsory physician and patient education among other safeguards, was established to ensure the safe administration of the drug. Similar patient education should occur for schedule II medications such as methylphenidate or amphetamine. Modafinil and armodafinil, schedule IV medications with less abuse potential have other risks including pregnancy in women on hormonal birth control. Expert consensus underscores the importance of addressing these and other concerns with patients. [Level 4]
Issues Addressed During Development
Although medication counseling is extremely important, the Workgroup could not identify a template or standard of reporting and recognized the difficulty in extracting from a patient record. One could consider using the following sentence as an example of medication counseling: “I discussed the potential side effects and medication interactions of XXX with this patient which included but was not limited to YYY.” Further, the Workgroup decided not to identify individual medications or their respective side effects in anticipation of future medications, as well as the common off-label use of various medications for narcolepsy.
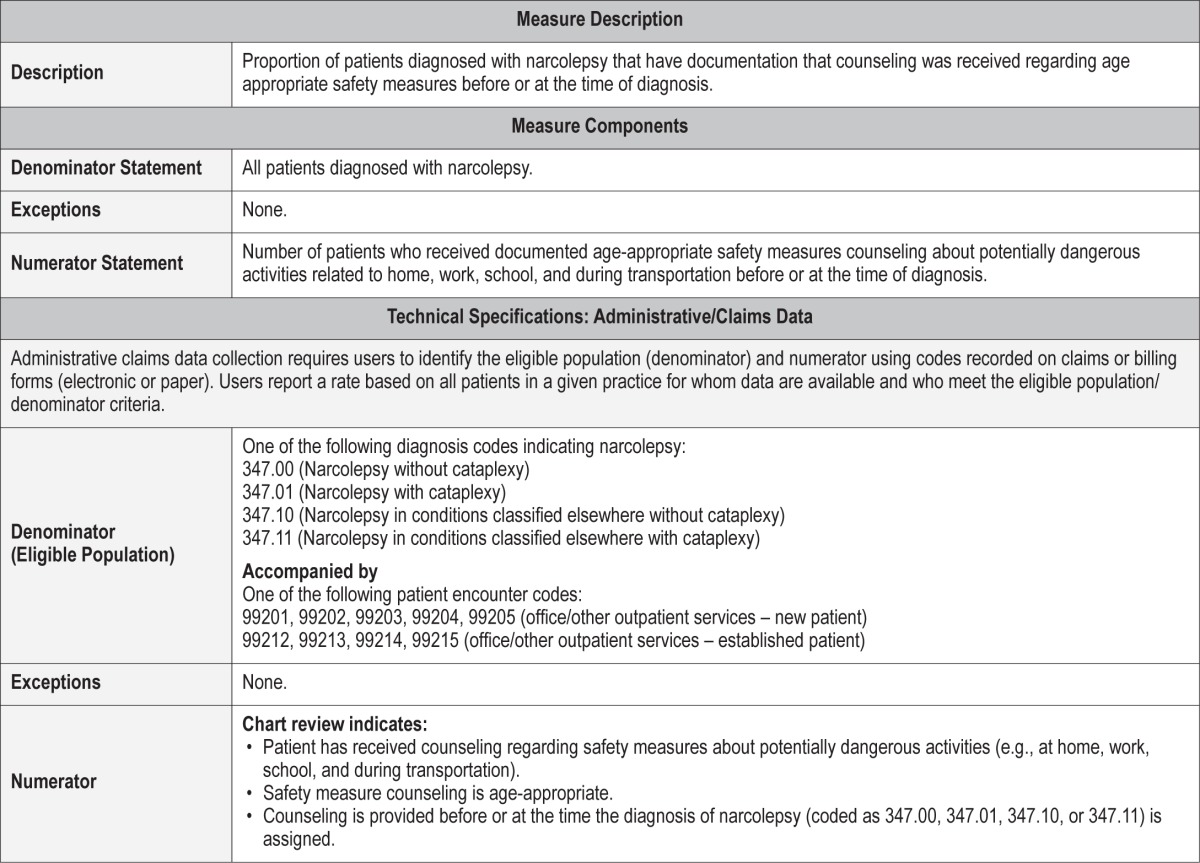
Process Measure 7 – Documented Safety Measure Counseling
Description
Proportion of patients diagnosed with narcolepsy that have documentation that counseling was received regarding age appropriate safety measures before or at the time of diagnosis.
The purpose of this measure is to reinforce the importance of age-appropriate safety counseling of patients with narcolepsy, including recommendations concerning driving, household chores (e.g., cooking, ironing), safety in the work environment, and the operation of hazardous equipment.
Exceptions and Exception Justifications
There are no exceptions for this measure.
Supporting Evidence and Rationale
Because narcolepsy has no cure, patients have to learn to adjust to limitations imposed by their disease in their daily activities. Hence, the patient should be counseled about career limitations, including but not limited to shift work, on-call schedules, and the transportation industry. [Level 4]
All patients and families should be informed that narcolepsy is associated with a significantly increased risk of crashes in commercial and non-commercial motor vehicle drivers, with or without treatment. [Level 4] Sleepiness secondary to narcolepsy has been noted to impair cognitive function, especially for complex processing tasks,29 [Level 4] and existing pharmacotherapy may not return patients to normal levels of daytime alertness.30 [Level 3] Little is known about the effects of pharmacological treatment on crash risk, with some data suggesting continued increased risk despite treatment. A diagnosis of narcolepsy is not, on its own, a sufficient reason to withdraw non-commercial driving privileges. The determining factor should be an individual's driving ability, the presence/absence of cataplexy, and the severity of sleep fragmentation. Relevant state laws regarding notification should be followed. [Level 4] Regarding commercial driving, the medical review board of the Federal Motor Carrier Safety Administration has recommended continued preclusion of narcoleptic patients from commercial motor vehicle operation regardless of treatment status.30 [Level 4] At present, there is insufficient evidence to support clinical and neuropsychological screening tests in assessing fitness to drive as a preventive strategy to reduce motor vehicle crashes among drivers affected by narcolepsy.31 [Level 3] In a recent driver simulator study, the reaction time was the only correlation with accident rate.32 [Level 3] Naps have often been recommended in the management of excessive daytime sleepiness (EDS) associated with narcolepsy-cataplexy. This simple behavioral management strategy has proven to increase daytime functioning in narcoleptic patients.33 [Level 4] Road side naps, frequent breaks, and intake of coffee or other caffeinated beverages are useful recommendations provided to patients engaged in long distance driving. [Level 4]
Accidents at home and in the work place were observed in 33% and 15% of patients, respectively.34 The patient should be advised to enlist family support doing household chores (e.g., cooking, ironing, child care), and only engage in these activities when most alert.14 Scheduled naps of not more than 15–20 minutes,35,36 regular sleep-wake schedule, and good sleep hygiene are important behavioral treatments in narcoleptic patients. [Level 4]
Relationship to Desired Outcome
The National Highway Traffic Safety Administration reports that drivers with medical conditions cause around 20,000 car accidents every year, which represent 1.3% of all accidents.37
Narcolepsy and its associated excessive daytime sleepiness have a negative impact on driving skills. In regular highway drivers, patients suffering from narcolepsy and hypersomnia have a threefold increased risk of traffic accidents in comparison to those without sleep disorders, independent of age, sex, marital status, or socio-professional categories.38 Clinicians should address the risks of driving in patients with narcolepsy for the safety of the patient and everyone on the road.
Up to 67% of narcoleptics report falling asleep at work, and 52% report losing a job because of narcolepsy.34,39,40 Difficulties in home activities are also affected, mainly supervising children (37%) and cooking (33%). Accidents at home and in the work place were observed in 33% and 15% of patients, respectively. People with narcolepsy are at increased risk for accidents but documentation of these events is poor.1 Regular discussion and documentation about home and school/work safety will increase awareness and reduce adverse events in this susceptible population.
Opportunities for Improvement/Gaps
Data regarding how often narcoleptic patients are counseled about safety measures are lacking. Counseling about safety measures is a crucial preventive intervention focused on decreasing the risk of injury to the patient and others, especially in those employed in high risk occupations and public safety. Documentation of safety measure counseling before or at diagnosis will improve patient care quality.
Issues Addressed During Development
The Workgroup left it up to the discretion of the provider to select the appropriate safety recommendations based on patient age, activities, and home and work environment. Although scant systematic studies exist investigating the impact of such counseling on patient quality of life, age-appropriate safety counseling is part of an integrative non-pharmacological treatment of narcolepsy.
IMPLEMENTATION STRATEGIES
The Workgroup aimed to use an evidence-based approach and expert consensus to set quality improvement standards for narcolepsy patient care. Our goal is to improve the health outcomes of patients with narcolepsy. While much thought has gone into development of these outcome and process measures, the Workgroup recognizes that their implementation into clinical practice may be challenging.
Common barriers to implementing quality improvement include lack of awareness of clinical guidelines and practice parameters, lack of consensus about what constitutes quality improvement, lack of motivation among providers to implement quality improvement practices, and difficulties facilitating best practices into busy clinical workdays and patients' access to care. Patients may have problems finding a knowledgeable narcolepsy care provider and obtaining recommended studies and treatment because of transportation issues, long wait times, competing time demands, and financial and/or insurance constraints.
The Workgroup addresses these challenges to implementation below:
Awareness: The Workgroup recognizes that not all providers are aware of the clinical guidelines and practice parameters that guide evidence-based diagnosis and treatment of patients with narcolepsy. The quality improvement measures outlined in this paper are based on the most updated Practice Parameters for the Treatment of Narcolepsy and other Hypersomnia Conditions,6 Practice Parameters for Clinical Use of the Multiple Sleep Latency Test and the Maintenance of Wakefulness Test,19 and the International Classification of Sleep Disorders, Third Edition.4 These quality improvement measures will be publically accessible on the AASM website.
Consensus: The Workgroup recognizes that patients with narcolepsy may seek diagnosis and treatment from care providers from various medical disciplines. The Workgroup itself is composed of sleep medicine clinicians from various backgrounds including pediatrics, neurology, psychiatry, and pulmonology, who developed guidelines with broad implementation potential. We sought feedback from a number of specialty societies including the American Academy of Neurology, American Academy of Family Medicine, and the American Thoracic Society.
Motivation: The Workgroup recognizes that providers must be motivated to improve care in order to accept and adopt the outlined quality improvement measures. Motivation to use survey instruments, follow specified protocols, increase communication and documentation recommended in this paper may be challenging to providers especially if they have competing demands to participate in quality improvement and/ or reporting programs in their own practices.
The Workgroup recognizes that one motivating factor for providers to improve is credible data demonstrating the value of quality improvement measures for narcolepsy. Unfortunately, these data are lacking. Some practices are moving toward using benchmarking data to allow providers to compare performance among peers or care between health care institutions. Such individual data may be more motivating to practitioners, and the AASM may need to consider further development of comparative self-assessment tools for implementation in clinical practices. Furthermore, providers likely require proof that use of quality improvement measures actually improves health outcomes in their patient population. To this end, there is a need for health outcomes research in the narcolepsy literature with use of valid and reliable instruments that are clinically useful as well as a patient data registry to study outcomes. Patient registries can provide information regarding clinical effectiveness, cost effectiveness of health care products and services, and safety concerns about treatment regimens that could dictate quality improvement recommendations.
Lastly, many health care institutions have financial and reputational interests to demonstrate quality of care and improve weaknesses when identified. For example, AASM-accredited sleep entities must have a quality assurance program. For these facilities, the quality assurance program must addresses inter-scorer reliability and at least three other quality assurance indicators for facility accreditation.41 To date, provider engagement of quality improvement in their clinical practice is not necessary for facility accreditation; however, the physicians boarded in sleep medicine must develop quality improvement programs based on their clinical practice for maintenance of certification through the American Board of Neurology and Psychiatry.42 Practitioners should check their respective licensure requirements regarding implementation of quality improvement in their clinical practice.
4. Facilitation: The Workgroup recognizes that implementation of quality improvement is challenging at a time when critical issues about reimbursement and time constraints are central to many practitioners. The Workgroup endeavored to provide references and resources, such as screening tools, that are publicly accessible and can be used in a variety of practice types. These tools can be printed, modified, and scanned into the medical record for future data analysis. Secondly, the Work-group specifies alternative ways to address timeliness of care if providers have long wait times or patient access is an issue. For example, providers are encouraged to document a phone call with patients or use alternate institution-approved methods of communication for notification of diagnosis and treatment initiation. Lastly, the Workgroup acknowledges that the quality improvement parameters will work best for clinicians using electronic health records as templated notes, computer reminder systems, standing orders, and decision support tools. Nevertheless, the Workgroup acknowledges that practitioners may need additional administration staff to help with scheduling, record keeping, documentation, and reporting to provide the desired quality of care outlined in this position paper.
FUTURE DIRECTIONS
The Workgroup recognizes that further testing and refining of measures may be needed as parameters are implanted into clinical practices in large scales. Important considerations are the expenses and potential burden to practitioners to utilize these quality tools. Ideally, implementing widely accepted quality measures will facilitate communication with third party payers leading to more rational treatment guidelines and pre-authorization protocols. In the future, more optimal electronic health records could be designed to facilitate data extraction and quality improvement activities. Since narcolepsy is a less common sleep disorder, there may be benefits in developing databases that are collaborative, multisite efforts. Going forward it would be desirable to use databases to measure the impact of a quality improvement program using these measures on patient health. This would inform efforts to revise or update the outcome and process measures at predetermined time points. Additionally, future measures could focus on appropriate treatment plans, continuing care and increased patient productivity.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Maski has received research support from Jazz Pharmaceuticals. Dr. Rifkin has received research support from UCB and Shire. Ms. Loeding is an employee of the American Academy of Sleep Medicine. Dr. Watson is a current member of the American Academy of Sleep Medicine Board of Directors. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The American Academy of Sleep Medicine would like to thank the following parties for their review of these measures, and for providing feedback and suggestions to improve the relevancy and utility of these measures in their field of practice: Ruth Boland, RN; Rajdeep Kakar, MD; Scott Leibowitz, MD; Bonnie Norris, RN; R. Bart Sangal, MD; American Academy of Neurology (AAN), and the Narcolepsy Network. The AASM did not seek or receive endorsement of these measures from any of the reviewers or organizations who provided feedback. The authors carefully considered all feedback provided, and implemented as many suggestions as were feasible in the refining of these measures. We would also like to thank Carolyn Winter-Rosenberg, AASM Director of Coding and Compliance, for guidance in compiling the technical specifications associated with these quality measures.
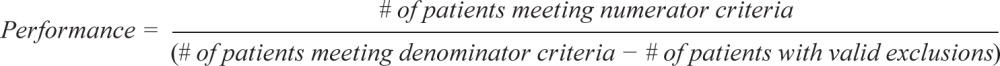
APPENDIX
The following are the technical specifications for the narcolepsy quality measures, which can be used to calculate an individual provider's performance in meeting these measures. Tracking and periodically reviewing this performance data will help providers identify opportunities for improvement within their own practices.
 |
Outcome Measure #1: Reduce excessive daytime sleepiness
Process Measure #1: Assessment of sleepiness
Process Measure #2: Treatment initiation following initial diagnosis
Process Measure #3: Comprehensive sleep history and physical exam
Process Measure #4: Objective sleep assessment
Process Measure #5: Treatment follow-up
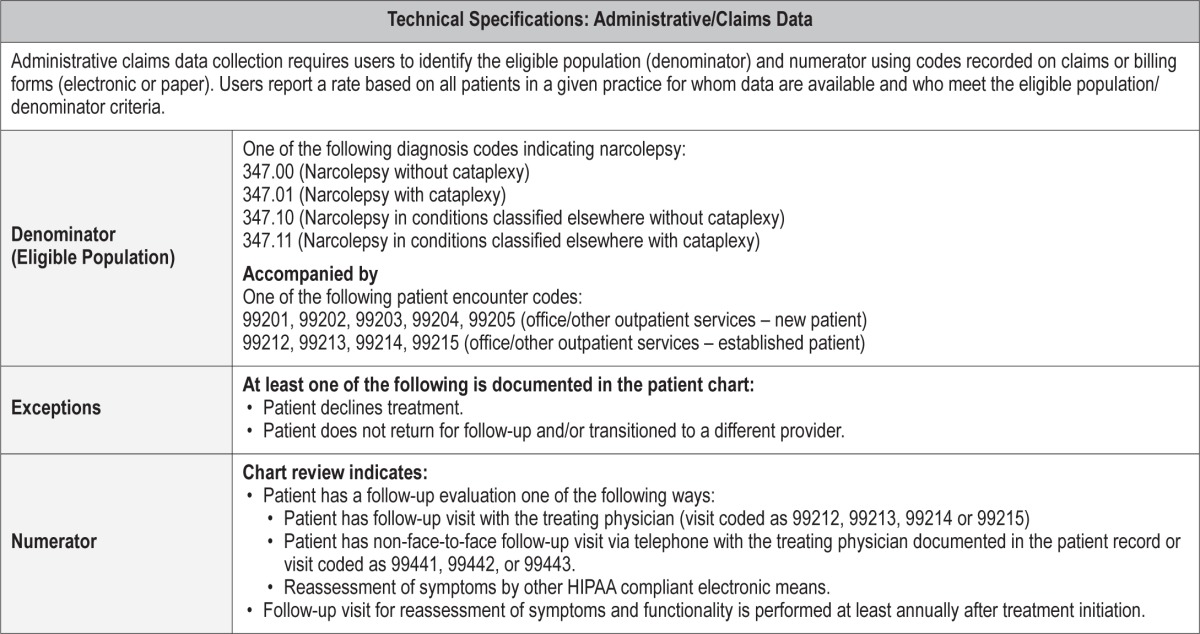
Process Measure #6: Documented medication counseling
Process Measure #7: Documented safety measure counseling
REFERENCES
- 1.Longstreth WT, Jr., Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007;30:13–26. doi: 10.1093/sleep/30.1.13. [DOI] [PubMed] [Google Scholar]
- 2.Aran A, Einen M, Lin L, Plazzi G, Nishino S, Mignot E. Clinical and therapeutic aspects of childhood narcolepsy-cataplexy: a retrospective study of 51 children. Sleep. 2010;33:1457–64. doi: 10.1093/sleep/33.11.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okun ML, Lin L, Pelin Z, Hong S, Mignot E. Clinical aspects of narcolepsycataplexy across ethnic groups. Sleep. 2002;25:27–35. doi: 10.1093/sleep/25.1.27. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 5.Morgenthaler TI, Aronsky AJ, Carden KA, Chervin RD, Thomas SM, Watson NF. Measurement of quality to improve care in sleep medicine. J Clin Sleep Med. 2015;11:279–91. doi: 10.5664/jcsm.4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgenthaler TI, Kapur VK, Brown T, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30:1705–11. doi: 10.1093/sleep/30.12.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guy W. Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. ECDEU Assessment Manual for Psychopharmacology. [Google Scholar]
- 8.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz JR, Khan A, McCall WV, Weintraub J, Tiller J. Tolerability and efficacy of armodafinil in naive patients with excessive sleepiness associated with obstructive sleep apnea, shift work disorder, or narcolepsy: a 12-month, open-label, flexible-dose study with an extension period. J Clin Sleep Med. 2010;6:450–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Harsh JR, Hayduk R, Rosenberg R, et al. The efficacy and safety of armodafinil as treatment for adults with excessive sleepiness associated with narcolepsy. Curr Med Res Opin. 2006;22:761–74. doi: 10.1185/030079906X100050. [DOI] [PubMed] [Google Scholar]
- 11.Weaver TE, Cuellar N. A randomized trial evaluating the effectiveness of sodium oxybate therapy on quality of life in narcolepsy. Sleep. 2006;29:1189–94. doi: 10.1093/sleep/29.9.1189. [DOI] [PubMed] [Google Scholar]
- 12.Mitler MM, Harsh J, Hirshkowitz M, Guilleminault C. Long-term efficacy and safety of modafinil (PROVIGIL (R)) for the treatment of excessive daytime sleepiness associated with narcolepsy. Sleep Med. 2000;1:231–43. doi: 10.1016/s1389-9457(00)00031-9. [DOI] [PubMed] [Google Scholar]
- 13.Ozaki A, Inoue Y, Hayashida K, et al. Quality of life in patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep time: comparison between patients on psychostimulants, drug-naive patients and the general Japanese population. Sleep Med. 2012;13:200–6. doi: 10.1016/j.sleep.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Wise MS, Arand DL, Auger RR, Brooks SN, Watson NF American Academy of Sleep Medicine. Treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30:1712–27. doi: 10.1093/sleep/30.12.1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulz H, Lund R. On the origin of early REM episodes in the sleep of depressed patients: a comparison of three hypotheses. Psychiatry Res. 1985;16:65–77. doi: 10.1016/0165-1781(85)90029-0. [DOI] [PubMed] [Google Scholar]
- 16.Plazzi G, Pizza F, Palaia V, et al. Complex movement disorders at disease onset in childhood narcolepsy with cataplexy. Brain. 2011;134(Pt 12):3480–92. doi: 10.1093/brain/awr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishino S, Kanbayashi T. Symptomatic narcolepsy, cataplexy and hypersomnia, and their implications in the hypothalamic hypocretin/orexin system. Sleep Med Rev. 2005;9:269–310. doi: 10.1016/j.smrv.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Aurora RN, Lamm CI, Zak RS, et al. Practice parameters for the non-respiratory indications for polysomnography and multiple sleep latency testing for children. Sleep. 2012;35:1467–73. doi: 10.5665/sleep.2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 20.Mignot E, Lin L, Finn L, et al. Correlates of sleep-onset REM periods during the Multiple Sleep Latency Test in community adults. Brain. 2006;129(Pt 6):1609–23. doi: 10.1093/brain/awl079. [DOI] [PubMed] [Google Scholar]
- 21.Chervin RD, Aldrich MS. Sleep onset REM periods during multiple sleep latency tests in patients evaluated for sleep apnea. Am J Respir Crit Care Med. 2000;161(2 Pt 1):426–31. doi: 10.1164/ajrccm.161.2.9905071. [DOI] [PubMed] [Google Scholar]
- 22.Ohayon MM. Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med. 2013;14:488–92. doi: 10.1016/j.sleep.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Inocente CO, Lavault S, Lecendreux M, et al. Impact of obesity in children with narcolepsy. CNS Neurosci Ther. 2013;19:521–8. doi: 10.1111/cns.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 25.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 26.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478–88. [PMC free article] [PubMed] [Google Scholar]
- 27.Karter AJ, Parker MM, Moffet HH, et al. Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care. 2004;42:110–5. doi: 10.1097/01.mlr.0000109023.64650.73. [DOI] [PubMed] [Google Scholar]
- 28.Guilleminault C. Amphetamines and narcolepsy: use of the Stanford database. Sleep. 1993;16:199–201. doi: 10.1093/sleep/16.3.199a. [DOI] [PubMed] [Google Scholar]
- 29.Hood B, Bruck D. A comparison of sleep deprivation and narcolepsy in terms of complex cognitive performance and subjective sleepiness. Sleep Med. 2002;3:259–66. doi: 10.1016/s1389-9457(02)00005-9. [DOI] [PubMed] [Google Scholar]
- 30.Hegmann KT, Andersson GB, Greenberg MI, Phillips B, Rizzo M. FMCSA's medical review board: five years of progress in commercial driver medical examinations. J Occup Environ Med. 2012;54:424–30. doi: 10.1097/JOM.0b013e3182480535. [DOI] [PubMed] [Google Scholar]
- 31.Marino M, de Belvis A, Basso D, et al. Interventions to evaluate fitness to drive among people with chronic conditions: systematic review of literature. Accid Anal Prev. 2013;50:377–96. doi: 10.1016/j.aap.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 32.Kotterba S, Mueller N, Leidag M, et al. Comparison of driving simulator performance and neuropsychological testing in narcolepsy. Clin Neurol Neurosurg. 2004;106:275–9. doi: 10.1016/j.clineuro.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 33.Helmus T, Rosenthal L, Bishop C, Roehrs T, Syron ML, Roth T. The alerting effects of short and long naps in narcoleptic, sleep deprived, and alert individuals. Sleep. 1997;20:251–7. doi: 10.1093/sleep/20.4.251. [DOI] [PubMed] [Google Scholar]
- 34.Teixeira VG, Faccenda JF, Douglas NJ. Functional status in patients with narcolepsy. Sleep Med. 2004;5:477–83. doi: 10.1016/j.sleep.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Mullington J, Broughton R. Scheduled naps in the management of daytime sleepiness in narcolepsy-cataplexy. Sleep. 1993;16:444–56. doi: 10.1093/sleep/16.5.444. [DOI] [PubMed] [Google Scholar]
- 36.Rogers AE, Aldrich MS, Lin X. A comparison of three different sleep schedules for reducing daytime sleepiness in narcolepsy. Sleep. 2001;24:385–91. doi: 10.1093/sleep/24.4.385. [DOI] [PubMed] [Google Scholar]
- 37.National Highway Traffic Safety A. The contribution of medical conditions to passenger vehicle crashes. Ann Emerg Med. 2010;55:563–4. doi: 10.1016/j.annemergmed.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 38.Philip P, Chaufton C, Taillard J, et al. Maintenance of wakefulness test scores and driving performance in sleep disorder patients and controls. Int J Psychophysiol. 2013;89:195–202. doi: 10.1016/j.ijpsycho.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 39.Broughton R, Ghanem Q, Hishikawa Y, Sugita Y, Nevsimalova S, Roth B. Life effects of narcolepsy in 180 patients from North America, Asia and Europe compared to matched controls. Can J Neurol Sci. 1981;8:299–304. doi: 10.1017/s0317167100043419. [DOI] [PubMed] [Google Scholar]
- 40.Kales A, Soldatos CR, Bixler EO, et al. Narcolepsy-cataplexy. II. Psychosocial consequences and associated psychopathology. Arch Neurol. 1982;39:169–71. doi: 10.1001/archneur.1982.00510150039009. [DOI] [PubMed] [Google Scholar]
- 41.American Academy of Sleep Medicine. Standards for accreditation. 2014 [Google Scholar]
- 42.American Board of Psychiatry and Neurology, Inc. Maintenance of certification in sleep medicine. 2014. http://www.abpn.com/moc_sm.asp.