Abstract
Bietti’s crystalline dystrophy (BCD) is a rare disease presenting with the appearance of intraretinal crystalline deposits and varying degrees of chorioretinal atrophy commencing at the posterior pole. Within time, intraretinal crystals gradually disappear and chorioretinal atrophy extends beyond the macula even resulting in complete chorioretinal atrophy. Concomitant corneal crystals can be noted in 1/2 - 1/3 of the patients, and the presence of corneal crystals is not a must for establishing the diagnosis. For the past decade, genetic evaluations and newer imaging modalities expand our knowledge about the disease. CYP4V2 gene is found to be the gene responsible for the disease process and new mutations are still being described. Modern imaging modalities, such as a spectral domain optical coherence tomography (SD-OCT) shed light on the anatomic features of the disease. By this, we reiterate the rare and unusual clinical features of BCD.
Key Words: Bietti’s crystalline dystrophy, cornea, macula, optical coherence tomography, retina
INTRODUCTION
In 1937, Bietti (1) described three cases of glistening, yellow- white intraretinal crystals in the posterior pole, atrophy of the retinal pigment epithelium (RPE), choroid sclerosis, crystals in the superficial paralimbal cornea with onset in the third decade of life. The condition was named after him, and subsequently, more cases with “Bietti’s crystalline dystrophy” (BCD) have been reported in the majority of ethnic groups. Its prevalence is 3% for all retinitis pigmentosa (RP) patients and 10% for autosomal recessive RP patients (2). Bietti crystalline dystrophy is, by all odds, related to aberrant oxidation of cellular lipid metabolism (3), caused by mutations of p450 genes (4). The disease is thought to be inherited in an autosomal recessive manner, and familial cases have also been documented (5, 6). Genetic mutations of the CYP4V2 gene are detected in >93.4% of cases by sequence analysis (7) and thus far, more than 50 mutations have been described (8). Lai et al. (9) evaluated the genotype - phenotype analysis in BCD in a group of 18 Chinese patients in 13 families and showed that BCD with homozygous IVS6-8del17 bp/insGC or compound heterozygous IVS6-8del17 bp/insGC and IVS8-2A_G mutations appeared to have a more severe disease phenotype based on electrophysiological testing. In contrast, Rossi et al (10) described the clinical and genetic features of 15 Italian patients with BCD and illustrated that there was a large range of genotypic and phenotypic variations stressing out the lack of an explicit genotype-phenotype correlation. Wilson and colleagues (11) found crystals resembling cholesterol or cholesterol esters in the retina and complex lipid inclusions in the conjunctiva, cornea, fibroblasts and circulating lymphocytes. Lipid inclusions were also demonstrated in the choroid (12).
CLINICAL FEATURES
Clinical findings are mainly characterized by fundus changes described below and the presence of crystalline corneal deposits.
Fundus Findings
Clinical findings are mainly characterized by fundus Stamp of the disease is the presence of refractive polygonal, yellowish-white intraretinal crystals grouped around the posterior pole and at the transition zone between the normal and atrophic RPE (13-15). During the disease, crystals diminish in number and atrophy of the RPE and choriocapillaris begin to initially appear at the central fundus. With the time, chorioretinal atrophy expands centrifugally spreading to the retinal periphery as well. For that reason, patients between the second and fourth decade of life experience vision impairment, some degree of night blindness and visual field defects. However, age of onset, presenting symptoms and disease severity vary widely from case to case, and there can also be asymmetry between the eyes. Deterioration of vision can become so severe that the patient may even end up in legal blindness by the fifth or sixth decade of life. Patients can be staged into three groups -- early, intermediate and advanced disease, according to the clinical evaluation as suggested by Yuzawa et al. (16) and used later by Mataftsi et al. (2) and Fang et al. (15) with some minor modifications.
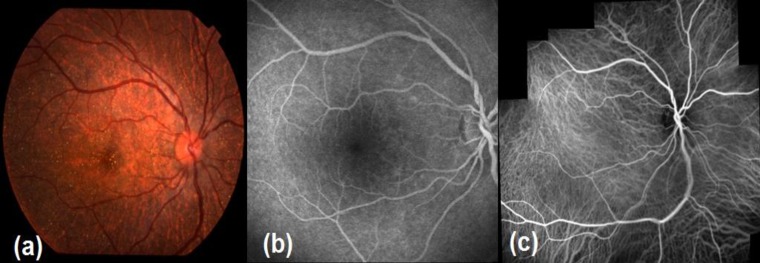
Early disease: Crystals are scattered throughout the posterior pole and mid periphery. On fluorescein and indocyanine angiographies atrophy is limited to the posterior pole solely (Fig. 1a, b and c).
Figure 1.
Early disease, color fundus (1a), fluorescein angiographic (1b) and indocyanine green angiographic appearance (1c)
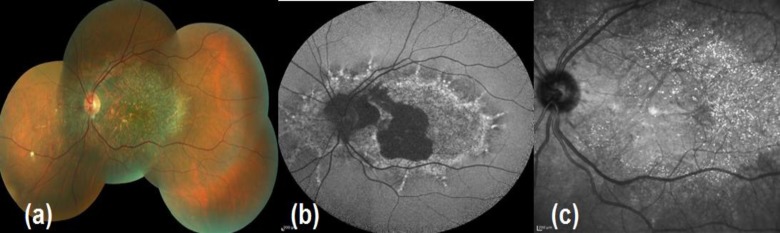
Intermediate disease: Crystals are very few or absent at the posterior pole, but still visible outside the area of central atrophy extending up to the equator (Fig. 2a and b).
Figure 2.
Intermediate disease, color fundus (2a), auto-fluorescence image (2b) and infrared image (2c)
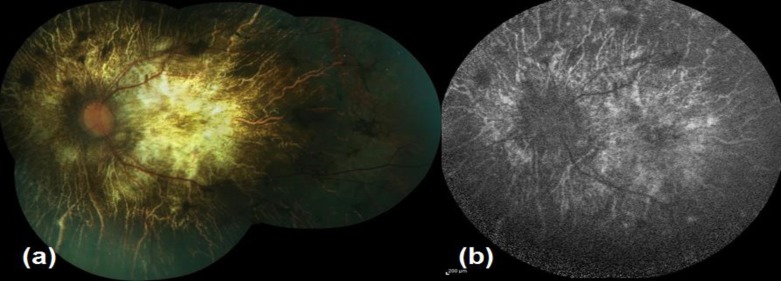
Advanced disease: There is almost complete chorioretinal atrophy with very occasional crystals (Fig. 3a and b).
Figure 3.
Advanced disease, color fundus (3a) and auto-fluorescence image (3b)
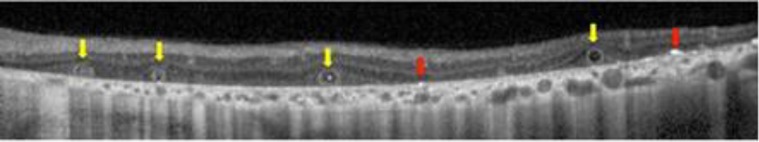
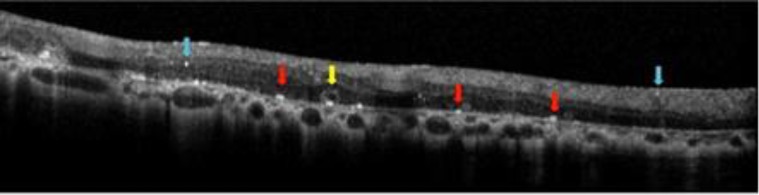
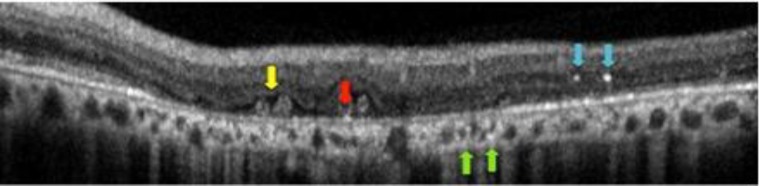
Besides the ancillary tests such as fluorescein and indocyanine angiographies, newer imaging modalities such as spectral domain optical coherence tomography (SD-OCT) and auto-fluorescence imaging reveals additional morphological features of the disease process such as outer retinal tubulations (ORT) and hyper-reflective dot-like lesions localized in almost all retinal layers (8, 17-22) (Figure 4-6). Outer retinal tubulations are more frequently described in BCD when compared with other retinal dystrophies such as RP and cone dystrophy (20, 21).
Figure 4.
Outer retinal tubulations (yellow arrow), Bright plaque (red arrow)
Figure 6.
Outer retinal tubulations (yellow arrow), Bright plaque (red arrow), Intraretinal bright spots (blue arrow)
Only in Yin’s et al. study comprising 17 patients, ORT was present in just 13.6% of eyes with BCD (23).Countless bright reflective spots of various configurations such as highly reflective spots in the inner retina, bright reflective plaques on top of Bruch membrane or partially encapsulated reflective plaques are all shown in SD-OCT sections of patients with BCD (19). However, only some of the hyper-reflective dots seem to correspond to the crystalline deposits (17, 19). The rest of the hyper-reflective dots may also be related to the inflammatory cells, protein deposits, a glial response to retinal degeneration, or even be artefacts (8).
Toto et al. (22) argued that choroidal hyper-reflective dots were in fact crystals resided in the choroid, thus they just added to the controversy of presence of hyper-reflective dots in the choroid.
Figure 5.
Outer retinal tubulations (yellow arrow), Bright plaque (red arrow), Intraretinal bright spots (blue arrow), Choroidal bright spots (green arrow)
Auto-fluorescence imaging shows decreased auto-fluorescence corresponding to the areas of RPE loss; punctual increase of auto-fluorescence corresponds to pigment dots, possible RPE hyperplasia or limited hyperauto-fluorescence of the crystals (17).
Trailing the evolving disease, macular function deteriorates as well. Some very rarely encountered macular changes may further affect the visual acuity devastatingly. Subfoveal neurosensory detachment (24), subretinal neovascular membrane (25-28), macular hole (29, 30) and cystoid macular edema (31, 32) are among those.
As the diagnosis mainly relies upon clinical features, electrophysiological tests are not as mandatory as in other retinal dystrophies. However, electrophysiological tests can be helpful to show the extent of the damage. The full field ERG can show extent of rod and cone dysfunction ranging from normal to reduced amplitudes of scotopic and photopic response to undetectable stimuli (33). On the other hand, multifocal ERG may detect regional areas of abnormal function wherever the full field ERG is normal (34).
Differential diagnosis of intraretinal crystalline deposits includes primary hyperoxaluria type 1 and 2, cystinosis, Sjögren-Larsson syndrome, drug-toxicity (tamoxifen, methoxyflurane and canthaxanthin) and talc retinopathy (7).
CORNEAL FEATURES
Corneal crystals (figure 7) are very fine and located mainly in the subepithelial and superficial anterior stroma near the limbus. In 1/3 - 1/2 of cases can be observed at the slit-lamp examination (12). However, corneal crystals can easily be overlooked, even by an experienced ophthalmologists as these deposits are very subtle (35). Specular microscopy (36) and in vivo confocal microscopy (37) were used to detect the corneal crystalline deposits very recently.
Figure 7.
Limbal Crystals
CONCLUSION
The diagnosis of BCD is made by the typical clinical findings of discrete glistening crystals within the retina. After excluding other causes of crystalline retinopathy with the help of clinical history and systemic evaluation diagnosis is confirmed by finding of the mutations in CYP4V2 gene. New imaging modalities such as SD-OCT provide novel information about the anatomic location and clinical implications of retinal crystals.
DISCLOSURE
Conflicts of Interest: None declared.
References
- 1.Bietti GB. Uber familiares vorkommen von “Retinitis punctata albescens” (verbunden mit “Dystrophia marginalis cristallinea corneae”), Glitzern des Glasköpers und anderen degenerativen Augenveranderungen. Klin Monatsbl Augenheilkd. 1937;99:737–756. [Google Scholar]
- 2.Mataftsi A, Zografos L, Millá E, Secrétan M, Munier FL. Bietti's crystalline corneoretinal dystrophy: a cross-sectional study. Retina. 2004 Jun;24(3):416–26. doi: 10.1097/00006982-200406000-00013. PMID: 15187665. [DOI] [PubMed] [Google Scholar]
- 3.Furusato E, Cameron JD, Chan CC. Evolution of cellular inclusions in Bietti's crystalline dystrophy. Ophthalmol Eye Dis. 2010 Mar ;2010(2):9–15. doi: 10.4137/OED.S2821. PMID: 21359135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li A, Jiao X, Munier FL, Schorderet DF, Yao W, Iwata F, Hayakawa M, Kanai A, Shy Chen M, Alan Lewis R, Heckenlively J, Weleber RG, Traboulsi EI, Zhang Q, Xiao X, Kaiser-Kupfer M, Sergeev YV, Hejtmancik JF. Bietti crystalline corneoretinal dystrophy is caused by mutations in the novel gene CYP4V2. Am J Hum Genet. 2004 May;74(5):817–26. doi: 10.1086/383228. PMID: 15042513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan WM, Pang CP, Leung AT, Fan DS, Cheng AC, Lam DS. Bietti crystalline retinopathy affecting all 3 male siblings in a family. Arch Ophthalmol. 2000 Jan;118(1):129–31. PMID: 10636430. [PubMed] [Google Scholar]
- 6.Saatci AO, Yaman A, Oner FH, Ergin MH, Cingil G. Indocyanine green angiography in Bietti's crystalline retinopathy. Can J Ophthalmol. 2002 Oct;37(6):346–51. PMID: 12422917. [PubMed] [Google Scholar]
- 7.Okialda KA, Stover NB, Weleber RG, Kelly EJ. Bietti Crystalline Dystrophy. In: Pagon RA, Bird TD, Dolan CR, Stephens K, Adam MP, editors. Gene Reviews Seattle (WA) University of Washington, Seattle: 1993-2014. [PubMed] [Google Scholar]
- 8.Halford S, Liew G, Mackay DS, Sergouniotis PI, Holt R, Broadgate S, Volpi EV, Ocaka L, Robson AG, Holder GE, Moore AT, Michaelides M, Webster AR. Detailed phenotypic and genotypic characterization of Bietti crystalline dystrophy. Ophthalmology. 2014 Jun;121(6):1174–84. doi: 10.1016/j.ophtha.2013.11.042. PMID: 24480711. [DOI] [PubMed] [Google Scholar]
- 9.Lai TY, Ng TK, Tam PO, Yam GH, Ngai JW, Chan WM, Liu DT, Lam DS, Pang CP. Genotype phenotype analysis of Bietti's crystalline dystrophy in patients with CYP4V2 mutations. Invest Ophthalmol Vis Sci. 2007 Nov;48(11):5212–20. doi: 10.1167/iovs.07-0660. PMID: 17962476. [DOI] [PubMed] [Google Scholar]
- 10.Rossi S, Testa F, Li A, Yaylacioğlu F, Gesualdo C, Hejtmancik JF, Simonelli F. Clinical and genetic features in Italian Bietti crystalline dystrophy patients. Br J Ophthalmol. 2013 Feb;97(2):174–9. doi: 10.1136/bjophthalmol-2012-302469. PMID: 23221965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilson DJ, Weleber RG, Klein ML, Welch RB, Green WR. Bietti's crystalline dystrophy A clinicopathologic correlative study. Arch Ophthalmol. 1989 Feb;107(2):213–21. doi: 10.1001/archopht.1989.01070010219026. PMID: 2783846. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser-Kupfer MI, Chan CC, Markello TC, Crawford MA, Caruso RC, Csaky KG, Guo J, Gahl WA. Clinical biochemical and pathologic correlations in Bietti's crystalline dystrophy. Am J Ophthalmol. 1994 Nov;118(5):569–82. doi: 10.1016/s0002-9394(14)76572-9. PMID: 7977570. [DOI] [PubMed] [Google Scholar]
- 13.Bernauer W, Daicker B. Bietti's corneal-retinal dystrophy A 16-year progression. Retina. 1992;12(1):18–20. PMID: 1565865. [PubMed] [Google Scholar]
- 14.Oner FH, Saatci AO, Ergin MH, Cingil G. Bietti'nin Kristalin Retinopatisi. 2002;32:244–250. [Google Scholar]
- 15.Mansour AM, Uwaydat SH, Chan CC. Long-term follow-up in Bietti crystalline dystrophy. Eur J Ophthalmol. 2007 Jul-Aug;17(4):680–2. doi: 10.1177/112067210701700434. PMID: 17671952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuzawa M, Mae Y, Matsui M. Bietti's crystalline retinopathy. Ophthalmic Paediatr Genet. 1986 Mar;7(1):9–20. doi: 10.3109/13816818609058037. PMID: 3703493. [DOI] [PubMed] [Google Scholar]
- 17.Ayata A, Tatlipinar S, Unal M, Ersanli D, Bilge AH. Autofluorescence and OCT features of Bietti's crystalline dystrophy. Br J Ophthalmol. 2008 May;92(5):718–20. doi: 10.1136/bjo.2008.138958. PMID: 18441184. [DOI] [PubMed] [Google Scholar]
- 18.Querques G, Quijano C, Bouzitou-Mfoumou R, Soubrane G, Souied EH. In-Vivo visualization of retinal crystals in Bietti's crystalline dystrophy by spectral domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2010 Mar;9:1–3. doi: 10.3928/15428877-20100215-94. PMID: 20337279. [DOI] [PubMed] [Google Scholar]
- 19.Pennesi ME, Weleber RG. High-resolution optical coherence tomography shows new aspects of Bietti crystalline retinopathy. Retina. 2010 Mar;30(3):531–2. doi: 10.1097/IAE.0b013e3181c96a15. PMID: 20139800. [DOI] [PubMed] [Google Scholar]
- 20.Kojima H, Otani A, Ogino K, Nakagawa S, Makiyama Y, Kurimoto M, Guo C, Yoshimura N. Outer retinal circular structures in patients with Bietti crystalline retinopathy. Br J Ophthalmol. 2012 Mar;96(3):390–3. doi: 10.1136/bjo.2010.199356. PMID: 21803923. [DOI] [PubMed] [Google Scholar]
- 21.Iriyama A, Aihara Y, Yanagi Y. Outer retinal tubulation in inherited retinal degenerative disease. Retina. 2013 Jul-Aug;33(7):1462–5. doi: 10.1097/IAE.0b013e31828221ae. PMID: 23538577. [DOI] [PubMed] [Google Scholar]
- 22.Toto L, Carpineto P, Parodi MB, Di Antonio L, Mastropasqua A, Mastropasqua L. Spectral domain optical coherence tomography and in vivo confocal microscopy imaging of a case of Bietti's crystalline dystrophy. Clin Exp Optom. 2013 Jan;96(1):39–45. doi: 10.1111/j.1444-0938.2012.00784.x. PMID: 22908902. [DOI] [PubMed] [Google Scholar]
- 23.Yin H, Jin C, Fang X, Miao Q, Zhao Y, Chen Z, Su Z, Ye P, Wang Y, Yin J. Molecular analysis and phenotypic study in 14 Chinese families with Bietti crystalline dystrophy. PLoS One. 2014 Apr;9(4) doi: 10.1371/journal.pone.0094960. PMID: 24739949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padhi TR, Kesarwani S, Jalali S. Bietti crystalline retinal dystrophy with subfoveal neurosensory detachment and congenital tortuosity of retinal vessels: case report. Doc Ophthalmol. 2011 Jun;122(3):199–206. doi: 10.1007/s10633-011-9274-1. PMID: 21611771. [DOI] [PubMed] [Google Scholar]
- 25.Le Tien V, Atmani K, Querques G, Massamba N, Souied EH. Ranibizumab for subfoveal choroidal neovascularization in Bietti crystalline retinopathy. Eye (Lond) 2010 Nov;24(11):1728–9. doi: 10.1038/eye.2010.116. PMID: 20798693. [DOI] [PubMed] [Google Scholar]
- 26.Gupta B, Parvizi S, Mohamed MD. Bietti crystalline dystrophy and choroidal neovascularisation. Int Ophthalmol. 2011 Feb;31(1):59–61. doi: 10.1007/s10792-010-9406-8. PMID: 20972604. [DOI] [PubMed] [Google Scholar]
- 27.Nachiappan K, Krishnan T, Madhavan J. Ranibizumab for choroidal neovascular membrane in a rare case of Bietti's crystalline dystrophy: a case report. Indian J Ophthalmol. 2012 May-Jun;60(3):207–9. doi: 10.4103/0301-4738.95873. PMID: 22569382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Atmaca LS, Muftuoglu O, Atmaca-Sonmez P. Peripapillary choroidal neovascularization in Bietti crystalline retinopathy. Eye (Lond) 2007 Jun;21(6):839–42. doi: 10.1038/sj.eye.6702673. PMID: 17173010. [DOI] [PubMed] [Google Scholar]
- 29.Bagolini B, Ioli-Spada G. Bietti's tapetoretinal degeneration with marginal corneal dystrophy. Am J Ophthalmol. 1968 Jan;65(1):53–60. doi: 10.1016/0002-9394(68)91028-3. PMID: 5299874. [DOI] [PubMed] [Google Scholar]
- 30.Saatci AO, Yaman A, Berk AT, Söylev MF. Macular hole formation in Bietti's crystalline retinopathy A case report. Ophthalmic Genet. 1997 Sep;18(3):139–41. doi: 10.3109/13816819709057127. PMID: 9361311. [DOI] [PubMed] [Google Scholar]
- 31.Saatci AO, Doruk HC, Yaman A. Cystoid macular edema in Bietti's crystalline retinopathy. Case Rep Ophthalmol Med. 2014;2014:964892. doi: 10.1155/2014/964892. PMID: 24949209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Broadhead GK, Chang AA. Acetazolamide for cystoid macular oedema in Bietti Crystalline Retinal dystrophy. Korean J Ophthalmol. 2014 Apr;28(2):189–91. doi: 10.3341/kjo.2014.28.2.189. PMID: 24688265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Usui T, Tanimoto N, Takagi M, Hasegawa S, Abe H. Rod and cone a-waves in three cases of Bietti crystalline chorioretinal dystrophy. Am J Ophthalmol. 2001 Sep;132(3):395–402. doi: 10.1016/s0002-9394(01)00963-1. PMID: 11530054. [DOI] [PubMed] [Google Scholar]
- 34.Sen P, Ray R, Ravi P. Electrophysiological findings in Bietti's crystalline dystrophy. Clin Exp Optom. 2011 May;94(3):302–8. doi: 10.1111/j.1444-0938.2011.00602.x. PMID: 21488952. [DOI] [PubMed] [Google Scholar]
- 35.Welch RB. Bietti's tapetoretinal degeneration with marginal corneal dystrophy crystalline retinopathy. Trans Am Ophthalmol Soc. 1977;75:164–79. PMID: 306693. [PMC free article] [PubMed] [Google Scholar]
- 36.Wada Y, Abe T, Shiono T, Tamai M. Specular microscopic findings of corneal deposits in patients with Bietti's crystalline corneal retinal dystrophy. Br J Ophthalmol. 1999 Sep;83(9):1095. doi: 10.1136/bjo.83.9.1088k. PMID: 10636693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bozkurt B, Ozturk BT, Kerimoglu H, Irkec M, Pekel H. In vivo confocal microscopic findings of 2 patients with Bietti crystalline corneoretinal dystrophy. Cornea. 2010 May;29(5):590–3. doi: 10.1097/ICO.0b013e3181be22ee. PMID: 20299976. [DOI] [PubMed] [Google Scholar]