Abstract
Background
Recent experimental evidence supports a role for binocular visual experience in the treatment of amblyopia. The purpose of this study was to determine whether repeated binocular visual experience with dichoptic iPad games could effectively treat amblyopia in preschool children.
Methods
A total of 50 consecutive amblyopic preschool children 3–6.9 years of age were assigned to play sham iPad games (first 5 children) or binocular iPad games (n = 45) for at least 4 hours per week for 4 weeks. Thirty (67%) children in the binocular iPad group and 4 (80%) in the sham iPad group were also treated with patching at a different time of day. Visual acuity and stereoacuity were assessed at baseline, at 4 weeks, and at 3 months after the cessation of game play.
Results
The sham iPad group had no significant improvement in visual acuity (t4 = 0.34, P = 0.75). In the binocular iPad group, mean visual acuity (plus or minus standard error) improved from 0.43 ± 0.03 at baseline to 0.34 ± 0.03 logMAR at 4 weeks (n = 45; paired t44 = 4.93; P < 0.0001). Stereoacuity did not significantly improve (t44 = 1.35, P = 0.18). Children who played the binocular iPad games for ≥8 hours (≥50% compliance) had significantly more visual acuity improvement than children who played 0–4 hours (t43 = 4.21, P = 0.0001).
Conclusions
Repeated binocular experience, provided by dichoptic iPad game play, was more effective than sham iPad game play as a treatment for amblyopia in preschool children.
Although patching treatment results in improved visual acuity for 73%–90% of amblyopic children, 15%–50% fail to achieve normal visual acuity after months or years of treatment.1–9 Even among children who do achieve normal visual acuity with amblyopia treatment, the risk for recurrence of amblyopia is high.1,2,10–13 Patching treatment is based on the premise that amblyopia is a monocular disorder that can be treated by eliminating the etiologic factor (blur or misalignment) and forcing use of the amblyopic eye.14 However, recent studies have elucidated a clear link between binocular dysfunction and the complex constellation of deficits that characterizes amblyopia, including visual acuity, vernier acuity, fixation instability, fusional suppression, and risk for residual and recurrent amblyopia.15 The association of binocular dysfunction and the myriad of monocular and binocular deficits in amblyopia has led several investigators to propose the hypothesis that amblyopia is a monocular consequence of a primary binocular obstacle to normal visual development.
The classic view hypothesizes that habitual suppression of one eye eliminates the diplopia or visual confusion that results from strabismus or anisometropia and causes a reduction in the number of binocularly driven cortical excitatory neurons. However, recent evidence refutes this hypothesis; although binocular interaction does not normally occur in amblyopia, it can occur when fellow-eye contrast is reduced.16 Recent physiological evidence also suggests that weak, noisy signals from the amblyopic eye can contribute to binocular vision if suppression by the fellow eye is reduced by signal attentuation (eg, reducing stimulus contrast).17,18 In addition, the lack of binocular responsiveness of V1 neurons in amblyopia is reversible when interocular suppression is removed by ionophoretic applications of bicuculline (a selective blocker of GABA receptors that blocks GABAergic inhibition).19 Taken together, the psychophysical and physiological data support the hypothesis that active suppression renders a structurally intact binocular visual system functionally monocular in amblyopia.
Reduced fellow-eye contrast to equate the visibility for the amblyopic and fellow eyes allows at least some amblyopic adults to experience binocular vision.16,20 In small cohorts of amblyopic adults and schoolchildren, repeated practice with dichoptic perceptual judgments or dichoptic games with reduced fellow-eye contrast yielded reduction in the strength of interocular suppression and modest visual acuity improvement after just 1–5 weeks.21–24
Moving the dichoptic game to an iPod platform with lenticular overlay was a first step toward clinical application of a binocular approach to amblyopia treatment.23 However, to date there have been only two lab-based studies of small samples of amblyopic adults using the iPod display with a lenticular overlay to play a dichoptic falling blocks game, a challenging game app in which falling blocks must be moved and rotated in order to fit together to build a wall. In addition, the iPod with lenticular overlay relies on stable head position for adequate dichoptic separation, excellent fine motor skills to manipulate the blocks, and cognitive skills to understand the complicated task. These requirements may make it difficult for young amblyopic children to play the iPod falling blocks game. In order to determine whether a binocular treatment approach could be effective for home use by amblyopic preschool children, we conducted an exploratory cohort study of four anaglyphic (red-green dichoptic) games presented on a larger iPad display for amblyopic children ages 3 to <7 years.
Methods
Eligible amblyopic children (3.7–6.9 years old) were referred to the study by five Dallas-area pediatric ophthalmologists. For the purposes of this study, amblyopia was defined as best-corrected visual acuity ≥0.2 logMAR and an interocular difference of ≥0.2 logMAR associated with the presence or history of strabismus, anisometropia, or both in an otherwise healthy child who had been wearing spectacle correction for a minimum of 3 months. Strabismic amblyopia was defined as amblyopia in the presence of a heterotropia at distance and/or near fixation, a history of strabismus surgery, or resolution of misalignment following hyperopic spectacle correction, with a spherical equivalent interocular difference <1.00 D and <1.50 D interocular difference in astigmatism in any meridian. Anisometropic amblyopia was defined as amblyopia in the presence of a spherical equivalent interocular difference ≥1.00 D or ≥1.50 D interocular difference in astigmatism in any meridian with no measureable heterotropia at distance or near fixation. Combined mechanism amblyopia was defined as amblyopia in the presence of a heterotropia at distance and/or near fixation, a history of strabismus surgery, or a history of resolution of misalignment following a hyperopic spectacle correction and a spherical equivalent interocular difference ≥1.00 or ≥1.50 D interocular difference in astigmatism in any meridian. Children with >5Δ of strabismus were excluded. In addition, children with prematurity of ≥8 weeks, developmental delay, or coexisting ocular or systemic diseases were excluded. Best-corrected visual acuity was independently assessed at our laboratory to confirm eligibility.
Informed consent was obtained from a parent prior to enrollment in the study. The study was reviewed and approved by the UT Southwestern Medical Center Institutional Review Board and was compliant with the US Health Insurance Portability and Accountability Act of 1996.
Study Design
A total of 50 consecutive amblyopic preschool children were enrolled. The first 5 children were assigned to the sham iPad group and the remaining 45 children to the binocular iPad group. Data from a larger sham iPad group (n = 25) have been previously reported.25 Because the prior sham iPad had no significant improvement in visual acuity in the prior study, only a small concurrent sham iPad group was included in the present study.
Best-corrected visual acuity and stereoacuity were measured at the baseline visit. Children and their parents were familiarized with the iPad and red-green glasses and practiced playing the iPad games. Subjects were provided with red-green glasses and headbands and written instructions about their use. They were instructed to play the iPad games for 4 hours per week for 4 weeks (16 hours total).
Visual acuity and stereoacuity were retested 3 months after the cessation of game play. Monocular best-corrected visual acuity was obtained for each eye using the ATS-HOTV protocol26 presented on an electronic visual acuity (EVA) tester.27 Stereoacuity was evaluated using 3 random dot tests, the Randot Preschool Stereoacuity Test (Stereo Optical Co Inc, Chicago, IL), the Stereo Butterfly Test (Stereo Optical Co Inc, Chicago, IL), and the Lang-Stereotest I (Lang-Stereotest AG, Küsnacht, Switzerland). The Randot Preschool Stereoacuity Test was administered first followed by the random dot butterfly page of the Stereo Butterfly Test (the circles page was not used). Children who did not comprehend the Randot Preschool Stereoacuity Test (was unable to point to the correct black-and-white pretest images) were tested with the Lang-Stereotest I. All tests were administered and scored according to manufacturer’s instructions and stereoacuity was the recorded as the finest disparity that the child was able to discriminate.
Binocular iPad Game Apps
The child could play any or all of 4 binocular iPad games using red-green anaglyphic glasses (in addition to spectacle correction, if any; green lens over the amblyopic eye). Images of the game screens are available as an e-Supplement 1 (available at jaapos.org). At the start of each game, an anaglyphic nonius alignment cross appeared to allow the child to adjust the binocular display, if necessary, for any small-angle strabismus (due to game design considerations, this adjustment was limited to ±5Δ).
In Falling Blocks, children moved and rotated falling blocks to fit them together with base blocks. High-contrast red falling blocks were visible to the amblyopic eye, the top two rows of stationary green base blocks were presented at reduced contrast and visible to the fellow eye, and the remaining base blocks were visible to both eyes. This game was similar to the lenticular iPad game used by Hess and colleagues22 and To and colleagues23 with amblyopic adults in a laboratory setting. In Balloon, the child pointed a launcher to try to place at least 3 balloons of identical shape adjacent to each other so that they would “pop” and disappear. High-contrast red balloons were visible to the amblyopic eye, low-contrast green balloons were visible to the fellow eye, and remaining balloons were visible to both eyes. Pong simulated a ping-pong game with one paddle for the iPad and another for the child. Children manipulated their paddle by tilting the iPad from side to side. The high-contrast red paddles were visible to the amblyopic eye and low-contrast green ball to the fellow eye. Labyrinth consists of a ball, a blinking hole, and a number of other holes. The high-contrast red ball was visible to amblyopic eye and the low contrast green holes to the fellow eye. The child tilted the iPad to roll the ball into the blinking hole without letting it fall into any other holes. For all 4 games, amblyopic eye contrast was set to 100% and, initially, fellow eye contrast was set to 15%–20%, based on the child being able to play the games successfully during training. Each game had a criterion score that required the child to play the game successfully for at approximately 15 minutes; the criterion score was constant. Fellow eye contrast was incremented by 10% (eg, 20%–22%) after each day on which the child achieved a criterion score, demonstrating that he or she was successful in combining information from both eyes to play the game. If the child was unable to achieve the criterion score with the increased fellow-eye contrast, fellow-eye contrast was decremented by 10% on the next day.
Children in the sham iPad group also played the dichoptic iPad games, but with the contrast setting reversed, so that reduced-contrast images were presented to the amblyopic eye and high-contrast images to the fellow eye.
Because of the young age of the children and the experimental nature of the iPad dichoptic games, we did not require that the children forgo patching treatment. Some of the referring pediatric ophthalmologists prescribed 2 hours per day of patching concurrently with participation in this study, with patching to be applied at a different time of day. Each child was provided with a personalized calendar to record time spent on game play and patching, separately.
Data Analysis
Using an intent-to-treat approach, overall effectiveness of the binocular iPad games was evaluated by paired t test of baseline versus 4-week outcome best-corrected visual acuity and stereoacuity outcome. Visual acuity improvement was compared for the binocular iPad and sham iPad groups by t test. Descriptive statistics (mean and standard error) were used to characterize improvement in best-corrected visual acuity (baseline minus 4-week visual acuity) of children who played the binocular iPad games ≥8 hours (≥50% compliance) versus children who played 0–4 hours (≤25% compliance) and also of children who played the games ≥8 hours versus children who played the games ≥8 hours and patched 2 hours daily at a different time of day. In addition, the association between number of hours of binocular iPad game play and of patching with visual acuity improvement was evaluated by Pearson product-moment correlation.
Results
Baseline characteristics of each participant are provided in e-Supplement 2 (available at jaapos.org). Patients (23 girls) ranged in age from 3.8 to 6.9 years with a mean age (plus or minus standard deviation) of 5.6 ± 0.9 years. Mean visual acuity was 0.43 ± 0.18 logMAR (range, 0.2–1.0 logMAR). Thirty-seven children (74%) had nil stereoacuity, 6 (12%) had 800–1200 arcsec, and 7 (14%) had 100–200 arcsec. Most children (76%) had 3–18 months’ patching treatment prior to baseline measurement. Three children (6%) had 2Δ–5Δ constant strabismus, and 3 (6%) had 2Δ–4Δ intermittent strabismus at baseline.
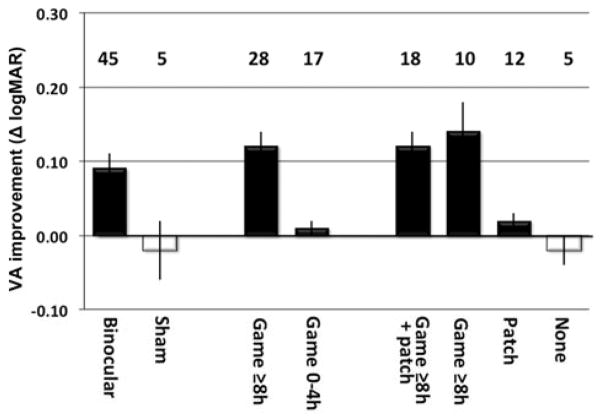
In the binocular iPad group, mean visual acuity (plus or minus standard error) improved from 0.43 ± 0.03 logMAR (20/54 Snellen equivalent) at baseline to 0.34 ± 0.03 (20/44 Snellen equivalent) at 4 weeks (mean improvement = 0.09 logMAR; paired t44 = 4.93; P < 0.0001; Figure 1). Visual acuity results were similar for children with anisometropic, strabismic, and combined mechanism amblyopia (0.10 ± 0.04, 0.07 ± 0.03, and 0.09 ± 0.02 logMAR improvement). Visual acuity results were similar for children who had nil stereoacuity at baseline (n = 35; 0.07 ± 0.03 logMAR improvement) and those who had measureable stereoacuity at baseline (n = 10; 0.10 ± 0.04 logMAR improvement)
FIG 1.
Left, Mean (±SE) change in logMAR visual acuity (baseline minus 4-week outcome) with binocular iPad and sham iPad game play. Middle, Mean change in logMAR visual acuity for children who reported playing the binocular iPad games ≥8 hours (≥50% compliance) and children who reported 0–4 hours (≤25% compliance). Right, Mean change in logMAR visual acuity for children who played the binocular iPad games ≥8 hours and patched for 2 hours per day at a different time of day (game+patch), children who played the binocular iPad games ≥8 hours (game only) and did not patch, children who did not play the binocular iPad games but patched (Patch only), and children who did not play the binocular iPad games or patch (None). Positive values indicate that visual acuity improved. Vertical lines on each bar show standard errors. Numbers above the bars indicate the sample size in each group.
Stereoacuity did not significantly improve (paired t44 = 1.35; P = 0.18). All 35 children in the binocular iPad group who had nil stereoacuity at baseline also had nil stereoacuity at 4 weeks. Of the 10 children who had measureable stereoacuity at baseline, 6 had no change in stereoacuity at 4 weeks, 3 had improved stereoacuity, and 1 had worse stereoacuity.
The sham iPad group had no significant improvement in visual acuity at the 4-week visit; visual acuity was 0.40 ± 0.05 logMAR (20/50 Snellen equivalent) at baseline and 0.38 ± 0.06 (20/48 Snellen equivalent) at 4 weeks (mean improvement = 0.02 logMAR; paired t4 = 0.34; P = 0.75; Figure 1). At the 4-week visit, visual acuity in the binocular iPad group had improved significantly more than in the sham iPad group (t48 = 1.98; P = 0.027).
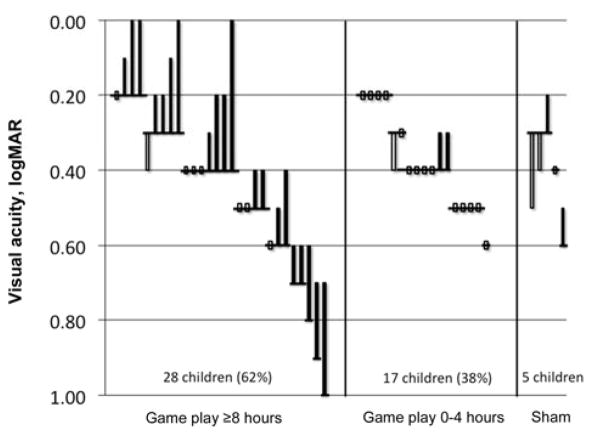
Among the 45 children assigned to the binocular iPad group, 28 (62%) reported that they played the games ≥8 hours during the 4-week study (≥50% compliance) and 17 (38%) reported playing the games 0–4 hours (0%–25% compliance). Overall, 20 of the 28 children (71%) who played ≥8 hours improved by ≥0.1 logMAR, 11 had 0.2–0.4 logMAR improvement, and 4 achieved 0.0 logMAR visual acuity (Figure 2). On the other hand, only 2 of the 17 children (12%) who played 0–4 hours had improved visual acuity, none improved 0.2–0.4 logMAR, and none achieved 0.0 logMAR visual acuity (Figure 2). At the 4-week visit, mean visual acuity (plus or minus standard error) of children who played ≥8 hours had improved by 0.14 ± 0.02 logMAR. There was only 0.01 ± 0.01 logMAR improvement in the group that played 0–4 hours (Figure 1). There were no significant differences in baseline characteristics (age, etiology of amblyopia, history of prior amblyopia treatment, history of prior surgery, visual acuity, stereoacuity) between the 28 children who played the games ≥8 hours and the 17 children who reported playing the games 0–4 hours. There was a moderate correlation between the number of hours of game play and the change in logMAR visual acuity at 4 weeks (N = 45; r = 0.44; 95% CI, 0.17–0.65).
FIG 2.
Visual acuity at baseline and at the 4-week outcome visit. Horizontal lines show baseline visual acuity. Filled bars show children who had visual acuity improvement. Open bars show children with no improvement or visual acuity deterioration. Left, Children who reported playing the binocular iPad games ≥8 hours (≥50% compliance), ordered by their baseline best-corrected visual acuity. Middle, Children who reported 0–4 hours (≤25% compliance) of binocular iPad game play, ordered by their baseline best-corrected visual acuity. Right, Children in the sham iPad group, sorted by baseline best-corrected visual acuity.
Among the 45 children assigned to the binocular iPad group, 30 (67%) reported that they patched 2 hours daily during the 4-week study and 15 (33%) reported no patching. At the 4-week visit, 10 children who played the games ≥8 hours and no patching had mean improvement (plus or minus standard error) in visual acuity of 0.14 ± 0.05 logMAR at 4 weeks; 18 children who played the games ≥8 hours and patched had similar improvement (0.12 ± 0.02 logMAR; Figure 1). In contrast, 12 children who played the games 0–4 hours but reported patching showed only a very small improvement in visual acuity (0.02 ± 0.01), and 5 children who played the games 0–4 hours and had no patching had small decrease in visual acuity at 4 weeks (−0.02 ± 0.02; Figure 1). The number of hours of patching was not correlated with the change in logMAR visual acuity at 4 weeks (N = 45; r = 0.05; 95% CI, −0.24 to 0.34).
Discussion
We evaluated the effectiveness of binocular iPad game play as a home treatment for amblyopia in children 3 to <7 years of age. Visual acuity improved with binocular iPad game play over a 4-week period. Children who played sham iPad games had no significant visual acuity improvement. Children who played the binocular iPad games for 8–18 hours over 4 weeks had visual acuity improvement similar to that achieved by patching for 2 hours daily for 4–6 weeks (56–84 hours patching) in studies that required spectacle wear for 1–4 months prior to baseline.28–30 About 40% had improvement of 0.2 to 0.4 logMAR (2 lines) and 15% achieved visual acuity of 20/20 in 4 weeks. Previous studies of dichoptic game play with reduced fellow-eye contrast in a supervised setting have shown similar improvements in visual acuity in adults and children.24,25
In the present study stereoacuity did not improve significantly in amblyopic children whose visual acuity improved while playing binocular iPad games. Prior studies of dichoptic game play by amblyopic adults have reported improvements in stereoacuity.21–23 Differences between the present study and these prior reports may have resulted from the use of random dot stereoacuity tests in the present study and contour or hybrid stereoacuity tests in the adult studies. The relationship between stereoacuity and visual acuity is complex, and stereoacuity alone does not fully characterize binocular vision. Therefore, lack of change in random dot stereoacuity during the present study should not be construed as inconsistent with the rationale for binocular treatment.
Compliance with the recommended binocular iPad game play time of 16 hours was reported to be ≥50% by 62% of our participants; the other 38% reported playing the games for 0–4 hours, with a mean compliance of 59% ± 6%. The mean compliance is similar to the 44%–58% compliance reported in recent studies that objectively monitored patching.31–33
The present study was limited by the fact that it was not a randomized clinical trial; rather, it was an exploratory cohort study that was designed to determine whether an improvement in visual acuity could be observed in amblyopic preschool children following a brief, 4-week experience playing binocular iPad games. This study does provide the first quantitative data on effect size and compliance for a home-based binocular treatment for amblyopia in preschool children, and evaluated the effect of sham iPad treatment in a small concurrent cohort. However, a randomized clinical trial is needed to evaluate the effectiveness of home-based binocular treatment in routine clinical practice and to compare its effectiveness with the current standard of care.
A second limitation of the present study is that patching treatment was not prohibited, as long as it was applied at a different time of day. Although some children did patch 2 hours daily during the 4-week binocular iPad study, patching did not augment the visual acuity improvement observed compared to the visual acuity improvement observed in children who did not patch. Patching alone had little effect on visual acuity during the 4-week study period, likely because 75% of the cohort had 3–18 months patching treatment prior to enrollment. Most of the benefit of patching treatment is seen with 150–250 hours of treatment, that is, 2.5–4 months.30
Amblyopia originates from a binocular discordance of visual inputs to both eyes due to strabismus, anisometropia, or both. It is one of many manifestations of a binocular barrier to normal visual development of central visual pathways. The mainstays of amblyopia treatment, patching and atropine, are monocular treatments that improve visual acuity but do not address the underlying binocular dysfunction. The results of this exploratory cohort study suggest that a binocular approach to amblyopia treatment may be an effective treatment for amblyopia in preschool children.
Supplementary Material
e-Supplement 1. Images of the 4 iPad games. All games used the same anaglyphic approach to separate monocular images. Game pieces (blocks, balloons, balls, paddles) were presented on an orange background composed of the red and green primaries in the RGB color space of the LED iPad display and chromaticities matched to the red and green anaglyphic filters in the glasses. Red and green components of the orange background had equal luminance. Red game pieces were matched to the red chromaticity and luminance of the red component of the orange background; green game pieces were matched to the green chromaticity and the luminance of the green component of the orange background. Therefore, when viewed through the green filter (amblyopic eye), green game pieces had 0% contrast and were invisible but red game pieces appeared black. Likewise, when viewed though the red filter (fellow eye), red game pieces had 0% contrast and were invisible but green game pieces appeared gray or black, depending on the contrast setting.
e-Supplement 2. Baseline characteristics
Acknowledgments
Funding Sources: National Eye Institute (EY022313), ExxonMobil Community Summer Jobs Program, BB Owens Foundation, Harold Simmons Foundation.
Footnotes
Presented at the Annual Meeting of AAPOS in April 2014 at Rancho Mirage, California.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Birch EE, Stager DR., Sr Long-term motor and sensory outcomes after early surgery for infantile esotropia. J AAPOS. 2006;10:409–13. doi: 10.1016/j.jaapos.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 2.Birch EE, Stager DR, Sr, Berry P, Leffler J. Stereopsis and long-term stability of alignment in esotropia. J AAPOS. 2004;8:146–50. doi: 10.1016/j.jaapos.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Repka MX, Beck RW, Holmes JM, et al. Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;12:603–11. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 4.Repka MX, Cotter SA, Beck RW, et al. Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–85. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Repka MX, Wallace DK, Beck RW, et al. Pediatric Eye Disease Investigator Group. Two-year follow-up of a 6-month randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2005;123:149–57. doi: 10.1001/archopht.123.2.149. [DOI] [PubMed] [Google Scholar]
- 6.Rutstein RP, Quinn GE, Lazar EL, et al. Pediatric Eye Disease Investigator Group. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117:998–1004. e1006. doi: 10.1016/j.ophtha.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart CE, Moseley MJ, Stephens DA, Fielder AR. Treatment dose–response in amblyopia therapy: the Monitored Occlusion Treatment of Amblyopia Study (MOTAS) Invest Ophthalmol Vis Sci. 2004;45:3048–54. doi: 10.1167/iovs.04-0250. [DOI] [PubMed] [Google Scholar]
- 8.Wallace DK, Edwards AR, Cotter SA, et al. Pediatric Eye Disease Investigator Group. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology. 2006;113:904–12. doi: 10.1016/j.ophtha.2006.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woodruff G, Hiscox F, Thompson JR, Smith LK. Factors affecting the outcome of children treated for amblyopia. Eye (Lond) 1994;8:627–31. doi: 10.1038/eye.1994.157. [DOI] [PubMed] [Google Scholar]
- 10.Birch EE. Binocular sensory outcomes in accommodative ET. J AAPOS. 2003;7:369–73. doi: 10.1016/j.jaapos.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Birch EE, Fawcett SL, Morale SE, Weakley DR, Jr, Wheaton DH. Risk factors for accommodative esotropia among hypermetropic children. Invest Ophthalmol Vis Sci. 2005;46:526–9. doi: 10.1167/iovs.04-0618. [DOI] [PubMed] [Google Scholar]
- 12.Birch EE, Stager DR, Berry P, Everett ME. Prospective assessment of acuity and stereopsis in amblyopic infantile esotropes following early surgery. Invest Ophthalmol Vis Sci. 1990;31:758–65. [PubMed] [Google Scholar]
- 13.Birch EE, Stager DR, Sr, Wang J, O’Connor A. Longitudinal changes in refractive error of children with infantile esotropia. Eye (Lond) 2010;24:1814–21. doi: 10.1038/eye.2010.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Eye Institute Office. Facts About Amblyopia. 2009 http://www.nei.nih.gov/health/amblyopia.
- 15.Birch EE. Amblyopia and binocular vision. Prog Ret Eye Res. 2013;33:67–84. doi: 10.1016/j.preteyeres.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansouri B, Thompson B, Hess RF. Measurement of suprathreshold binocular interactions in amblyopia. Vision Res. 2008;48:2775–84. doi: 10.1016/j.visres.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Sengpiel F, Jirmann KU, Vorobyov V, Eysel UT. Strabismic suppression is mediated by inhibitory interactions in the primary visual cortex. Cereb Cortex. 2006;16:1750–58. doi: 10.1093/cercor/bhj110. [DOI] [PubMed] [Google Scholar]
- 18.Bi H, Zhang B, Tao X, Harwerth RS, Smith EL, Chino YM. Neuronal responses in visual area v2 (v2) of macaque monkeys with strabismic amblyopia. Cereb Cortex. 2011;21:2033–45. doi: 10.1093/cercor/bhq272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sengpiel F, Vorobyov V. Intracortical origins of interocular suppression in the visual cortex. J Neurosci. 2005;25:6394–400. doi: 10.1523/JNEUROSCI.0862-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker DH, Meese TS, Mansouri B, Hess RF. Binocular summation of contrast remains intact in strabismic amblyopia. Invest Ophthalmol Vis Sci. 2007;48:5332–8. doi: 10.1167/iovs.07-0194. [DOI] [PubMed] [Google Scholar]
- 21.Hess RF, Mansouri B, Thompson B. A new binocular approach to the treatment of amblyopia in adults well beyond the critical period of visual development. Restor Neurol Neurosci. 2010;28:793–802. doi: 10.3233/RNN-2010-0550. [DOI] [PubMed] [Google Scholar]
- 22.Hess RF, Thompson B, Black JM, et al. An iPod treatment of amblyopia: an updated binocular approach. Optometry. 2012;83:87–94. [PubMed] [Google Scholar]
- 23.To L, Thompson B, Blum JR, Maehara G, Hess RF, Cooperstock JR. A game platform for treatment of amblyopia. IEEE Trans Neural Sys Rehab Eng. 2011;19:280–89. doi: 10.1109/TNSRE.2011.2115255. [DOI] [PubMed] [Google Scholar]
- 24.Knox PJ, Simmers AJ, Gray LS, Cleary M. An exploratory study: prolonged periods of binocular stimulation can provide an effective treatment for childhood amblyopia. Invest Ophthalmol Vis Sci. 2012;53:817–24. doi: 10.1167/iovs.11-8219. [DOI] [PubMed] [Google Scholar]
- 25.Li S, Jost R, Morale S, Stager D, Dao L, Stager D, et al. A binocular ipad treatment for amblyopic children. Eye (Lond) 2014;28:1246–53. doi: 10.1038/eye.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holmes JM, Beck RW, Repka MX, et al. Pediatric Eye Disease Investigator Group. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 27.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 28.Wallace DK, Edwards AR, Cotter SA, et al. Pediatric Eye Disease Investigator Group. A randomized trial to evaluate 2 hours of daily patching for strabismic and anisometropic amblyopia in children. Ophthalmology. 2006;113:904–12. doi: 10.1016/j.ophtha.2006.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rutstein RP, Quinn GE, Lazar EL, et al. Pediatric Eye Disease Investigator Group. A randomized trial comparing Bangerter Filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117:998–1004. doi: 10.1016/j.ophtha.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart CE, Stephens DA, Fielder AR, Moseley MJ. Modeling dose–response in amblyopia: toward a child-specific treatment plan. Invest Ophthalmol Vis Sci. 2007;48:2589–94. doi: 10.1167/iovs.05-1243. [DOI] [PubMed] [Google Scholar]
- 31.Awan M, Proudlock F, Gottlob I. A randomized controlled trial of unilateral strabismic and mixed amblyopia using occlusion dose monitors to record compliance. Invest Ophthalmol Vis Sci. 2005;46:1435–9. doi: 10.1167/iovs.04-0971. [DOI] [PubMed] [Google Scholar]
- 32.Tjiam AM, Akcan H, Ziylan F, et al. Sociocultural and psychological determinants in migrants for noncompliance with occlusion therapy for amblyopia. Graefes Arch Clin Exp Ophthalmol. 2011;249:1893–9. doi: 10.1007/s00417-011-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallace MP, Stewart CE, Moseley MJ, Stephens DA, Fielder AR Monitored Occlusion Treatment Amblyopia Study (MOTAS) Cooperatives; Randomized Occlusion Treatment Amblyopia Study (ROTAS) Cooperatives. Compliance with occlusion therapy for childhood amblyopia. Invest Ophthalmol Vis Sci. 2013;54:6158–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
e-Supplement 1. Images of the 4 iPad games. All games used the same anaglyphic approach to separate monocular images. Game pieces (blocks, balloons, balls, paddles) were presented on an orange background composed of the red and green primaries in the RGB color space of the LED iPad display and chromaticities matched to the red and green anaglyphic filters in the glasses. Red and green components of the orange background had equal luminance. Red game pieces were matched to the red chromaticity and luminance of the red component of the orange background; green game pieces were matched to the green chromaticity and the luminance of the green component of the orange background. Therefore, when viewed through the green filter (amblyopic eye), green game pieces had 0% contrast and were invisible but red game pieces appeared black. Likewise, when viewed though the red filter (fellow eye), red game pieces had 0% contrast and were invisible but green game pieces appeared gray or black, depending on the contrast setting.
e-Supplement 2. Baseline characteristics