Abstract
A review of the literature on the effectiveness of educational technologies to teach patient care skills to pharmacy students was conducted. Nineteen articles met inclusion criteria for the review. Seven of the articles included computer-aided instruction, 4 utilized human-patient simulation, 1 used both computer-aided instruction and human-patient simulation, and 7 utilized virtual patients. Educational technology was employed with more than 2700 students at 12 colleges and schools of pharmacy in courses including pharmacotherapeutics, skills and patient care laboratories, drug diversion, and advanced pharmacy practice experience (APPE) orientation. Students who learned by means of human-patient simulation and virtual patients reported enjoying the learning activity, whereas the results with computer-aided instruction were mixed. Moreover, the effect on learning was significant in the human-patient simulation and virtual patient studies, while conflicting data emerged on the effectiveness of computer-aided instruction.
Keywords: computer-aided instruction, human-patient simulators, virtual patients, pharmacy
INTRODUCTION
Effective use of educational technology has become essential to pharmacy curricula. In a 2011 survey of accredited US colleges and schools of pharmacy, nearly all were using some type of technology to present information to students (lecture capture, 69.6%; presentation software, 98.9%; presentation hardware, 75.3%), and most programs were using technologies to actively engage students (web conferencing, 74.2%; interactive videoconferencing, 61.8%; audience response systems, 88.8%; blogging/microblogging, 59.5%; document collaboration, 66.3%; wiki tools, 66.3%).1 While the ubiquitous presence of educational technology in pharmacy schools across the country reflects pedagogical advantages and attraction to these platforms among students, its rapid growth can also be attributed to support from pharmacy organizations and accrediting bodies. The Center for the Advancement of Pharmacy Education (CAPE) and the Accreditation Council for Pharmacy Education (ACPE) continue to promote the use of effective educational technology in pharmacy curricula to enhance graduate skills as patient care providers, problems solvers, patient educators, and health care collaborators.2, 3
To meet the demands of the profession and expectations of pharmacy education leadership, development of patient care skills, with an emphasis on “patient-centered care,” is at the forefront of most pharmacy curricula. These skills are typically taught and assessed through curricular integrated, active-learning sessions involving problem-based learning, team-based learning, and/or case-based learning practica, and typically afford the learner only one opportunity to showcase their abilities.4 Students are expected to retain patient care skills developed through practica in order to hone them during practice experiences. In this model, repetition opportunities, formative faculty feedback, clinical variation, individualized learning, and experience fidelity can be limited. Educational technologies may offer faculty members a more effective means of teaching and assessing patient-care skills in safe, active-learning environments. Computer-aided instruction, mannequin model simulators, and virtual patients offer students high fidelity, yet safe learning environments in which to both succeed and fail. In addition, these individualized, active-learning strategies offer students repetition opportunities in a variety of realistic clinical settings with faculty developed feedback.5
This review summarizes the published studies that assess patient care skill development through educational technology in pharmacy curricula. In this review, educational technology is defined as any computer-aided instruction, human-patient simulation, or virtual patient.
LITERATURE SEARCH
A comprehensive search of the PubMed database was performed and included any publication through February 2014. The Medical Subjects Heading (MeSH) term pharmacy education was combined with the each of the following text search terms: computer-aided instruction, computer-assisted learning, human-patient simulator, and virtual patient. This search was duplicated using the International Pharmaceutical Abstracts database. All studies included in the review reported student learning and satisfaction with the specific educational technology in the development of patient care skills in a pharmacy curriculum. Studies outside the discipline of pharmacy or those that did not meet the listed criteria were excluded. Additional reasons for exclusion included: the use of standardized patients, education of health care professionals (not students), and abstract-only papers. Abstracts that resulted from this initial search were manually screened by the authors for relevance to the review. Additionally, a review of citations of the pertinent literature was performed.
The following information was extracted from the selected articles: (1) type of educational technology employed, (2) number of students involved, (3) educational year of the students, (4) institution at which technology was utilized, (5) course/setting of the technology use, (6) evaluation and assessments of technology and student performance, (7) student satisfaction, (8) role of instructors, (9) limitations, and (10) authors’ conclusions.
FINDINGS
The literature search generated a result of 104 articles using the combined search terms in PubMed. The majority of articles were excluded because they included only standardized patients, were not in the discipline of pharmacy, or did not include the education of pharmacy students specifically (ie, technology was developed to educate pharmacists). The remaining articles were excluded because assessment and satisfaction data were not reported, and/or the educational technology was not used to develop patient care skills. The search of the International Pharmaceutical Abstracts database generated 76 articles. The majority of articles indexed in this search were excluded because they included an abstract only with inadequate information, were not focused in patient care, or were developed to educate pharmacists. A comprehensive review of the literature by authors added 3 articles to the search. The final article count was 19. Educational technology was employed with more than 2700 students at 12 colleges and schools around the globe. Tables 1-3 summarize the studies included, which technology was employed, educational year of students, and settings in which the technology was used.
Table 1.
Computer-aided Instruction Studies
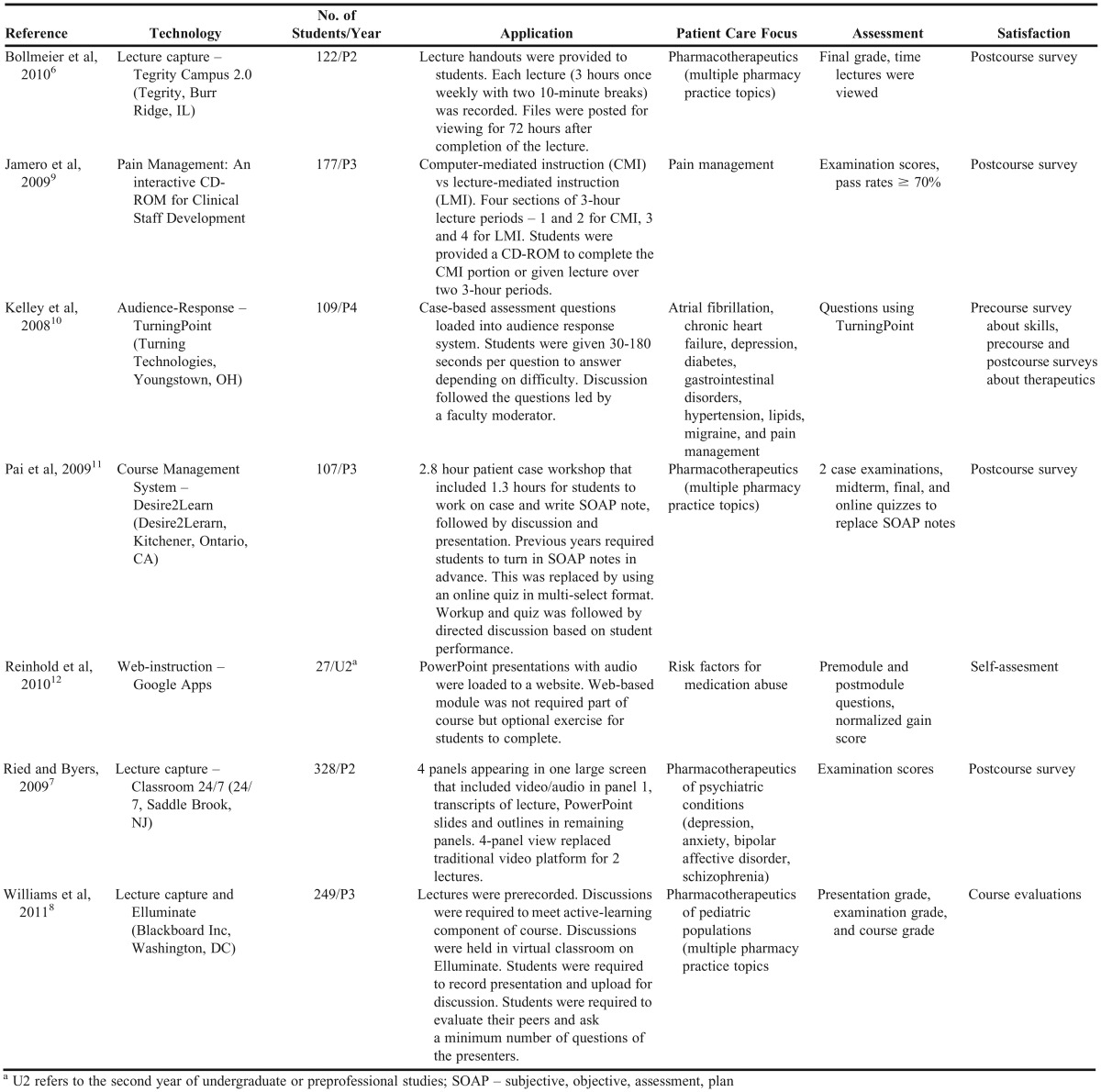
Table 3.
Virtual Patient Studies
Computer-aided Instruction
Seven studies examined computer-aided instruction (CAI), consisting of lecture capture, CD-ROM, audience response systems, course management systems, and/or web instruction and delivered to more than 1100 students. Of the 7 studies, 3 employed lecture capture,6-8 1 employed a CD-ROM,9 1 employed an audience response system,10 1 a learning management system,11 and 1 used web-based instruction.12 Assessment of the CAI tools was measured mostly by examination scores, course grades, and/or preCAI and postCAI questions. The most common method of collecting satisfaction data was a postcourse survey. Descriptions of how this technology was utilized and how assessment and satisfaction data was collected are summarized in Table 1.
Results of using various methods of CAI were mixed. Lecture capture had no effect on presentation grades, and while some studies reported higher examination grades, though not higher final grades compared to historical controls; others reported higher examination grades in historical controls.6-8 The method of delivering the lecture capture was different among the 3 studies. One allowed the videos to be available for 72 hours,6 1 used a 4-panel view for streaming the lectures,7 and 1 used pre-recorded lectures.8 Additionally, 1 study reported that there was no difference in final course grades for the number of lectures viewed or the minutes of lectures viewed, although the average total number of accessions was low (3.4 out of 24 available).6 The use of CD-ROM as a means of CAI did not improve examination scores either (p=0.85).9 This study did report, however, a significant increase in efficiency and student perception of learning.9 When an audience response system was utilized in an orientation prior to APPEs, students reported an increase in confidence in the majority of therapeutic areas, despite the average class scores ranging from a 32% in the area of nonprescription products to 93% in the area of headaches.10 The aim of the study using the audience response system, it should be noted, was to review therapeutics and gather assessment level data; it was not developed to measure the effectiveness of the technology. A patient-case workshop that used a learning management system, redesigned to provide more immediate feedback to students, found that students significantly improved in outcomes related to managing adverse drug events, drug interactions, monitoring, and patient education (p≤0.02).11 A web-based application was used to teach preprofessional students in a course on drug abuse and diversion. This study found that knowledge increased after using the application (median percent knowledge gain: 20%; p<0.0001) and that more students achieved a passing score (defined as at least 70%) on the posttest compared to the pretest (pretest pass rate: 33% vs posttest pass rate: 93%; p<0.0001).12
Satisfaction data regarding CAI also returned varied results. With lecture capture, satisfaction data was mixed, although survey response rates were high (56-95%).6-12 One study reported no difference in survey scores,8 while another reported that more students preferred traditional lecture vs the 4-panel method (51% vs 36.6%),7 and the third study reported that more students used the lectures for completing handouts than studying for examinations.6 The CD-ROM study reported a perception among students that they learned more (p<0.001) than they did with traditional teaching, but that there was less time for faculty members to answer questions (75% vs 38%; p=0.01).9 The audience response system was well received by students, with 89% stating the method was useful.10 Students reported that the learning management system redesign allowed them to think on their feet, stimulate their critical-thinking, rational decision-making, and problem-solving skills.11 Finally, students agreed in a self-assessment that web-based instruction allowed them to identify drugs that may be abused (100%), identify potential methods of abuse (95%), understand the role of a pharmacist (90%), identify drug diversion as a problem (90%), and have confidence in knowing what action to take (80%).12
The means by which CAI can be delivered to students are numerous and the outcomes and satisfaction among the students vary. The advantages of this technology are that it is easily employed with larger numbers of students, it can allow for repetition opportunities and immediate faculty feedback, and it promotes individualized learning. In this review, more students used CAI than human-patient simulation, and similar numbers used virtual patients, potentially highlighting versatility and usability of this educational technology along with its broader definition. The different technologies also offer flexibility so that the faculty member may optimize the content of the course. Some of these technologies allow for quick generation of assessment data, while others are merely information vestibules. In order for these technologies to be implemented successfully, careful planning should go into determining which technology is best suited for a course, how the effectiveness of the technology will be measured, the satisfaction of the students, and most importantly, the impact on student learning.
Human-Patient Simulation
Five articles were identified in which human-patient simulation (HPS) technology with mannequin models was used to educate nearly 400 pharmacy students in P2 or P3 level courses. Four of the 5 articles described the use of SimMan/SimBaby (Laerdal Medical, Wappingers Falls, NY) technology,13-16 while the fifth utilized METI (METI, Sarasota, FL).17 The assessment of the HPS tool included presimulation and postsimulation quizzes, examination scores, grading of the simulation activity, and blood pressure and pulse assessments. Student satisfaction data was collected using postcourse/simulation surveys. Descriptions of how the technology was utilized and how assessment and satisfaction data was collected are summarized in Table 2.
Table 2.
Human-Patient Simulator Studies
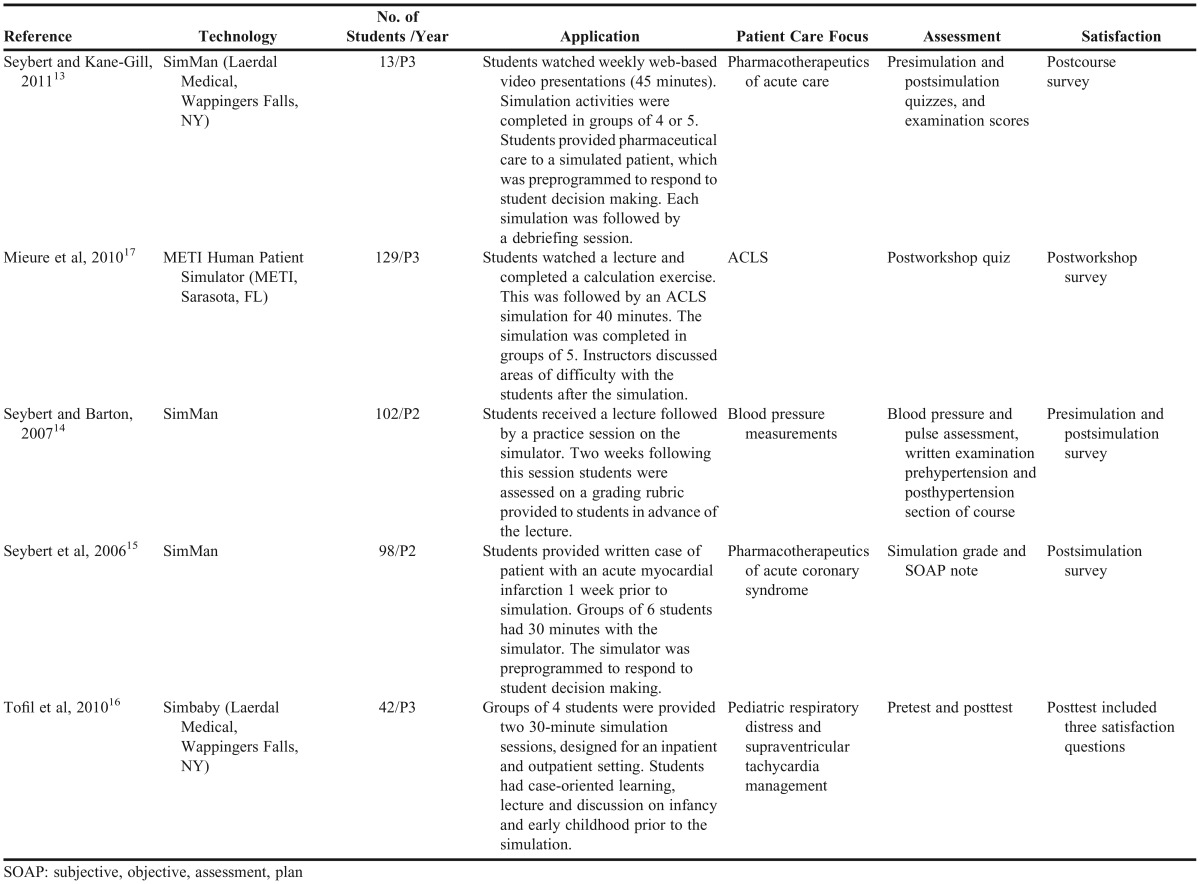
The studies showed that postsimulation quiz scores were significantly higher than presimulation scores (p≤0.05); this includes naming and treating a condition, and medication administration.13,14,16 Examination scores were reported in 1 study, which showed that the average examination score did improve, but not significantly. However, scores on data collection and interpretation questions on the examination did improve significantly (p<0.001).13 Grades specific to the simulation were high and significantly improved (p=0.029),14 including blood pressure measurement accuracy (p<0.05);14 but in another study using HPS, median scores on knowledge-based questions in advanced cardiac life support were low.17 Students were able to correctly calculate medication rates (78%), but struggled with concentration calculations (20%) and questions relating to asystole or pulseless electrical activity (21.8%) and ventricular tachycardia (11.7%).17 Results from an HPS study on myocardial infarction were higher, with an average examination score of 88% reported.15
The use of HPS was well-received by students in these studies. Survey response rates were 93-100%.13,15-17 Students reported positive attitudes about simulation prior to and after their experiences, and 88% stated they enjoyed the simulation.13-15 Students reported that using simulation enhanced learning,13,17 that they enjoyed the realistic setting,13,16 and that it increased their confidence.14 Seventy to 94% of students stated they would like more simulation incorporated or would participate again if it was available.15,17 Other student data resulting from how HPS was used included reports of enhanced understanding of the pharmacist’s responsibilities during an advanced cardiac life support event,17 learning of cardiovascular pharmacology and therapeutics,17 improved dose calculations and medication preparation,17 developed abilities to problem solve,15 and better patient outcome realization of clinical decisions.16
Simulation grades, with the exception of those related to advanced cardiac life support, were significantly improved with the implementation of HPS. Examination scores also improved, although more data is needed before a conclusion can be made. The use of HPS in pharmacy education seems not only to be enjoyed by students, but it is also sought after by students. The optimal use of HPS seems to be in higher level courses in which students may act as health care providers. This technology offers the student a safe environment in which to learn, both from their successes and their mistakes. A major disadvantage of this technology is cost. Including the use of high-fidelity patient mannequins in curriculum is typically expensive, with both high start-up and operating costs.18 Assessments of the learner and the activity may be built into the technology with standard grading rubrics used in other patient care activities or with presimulation and postsimulation examinations. Satisfaction data from the students should also be gathered. Postcourse surveys appear to have a good response rate for this type of technology.
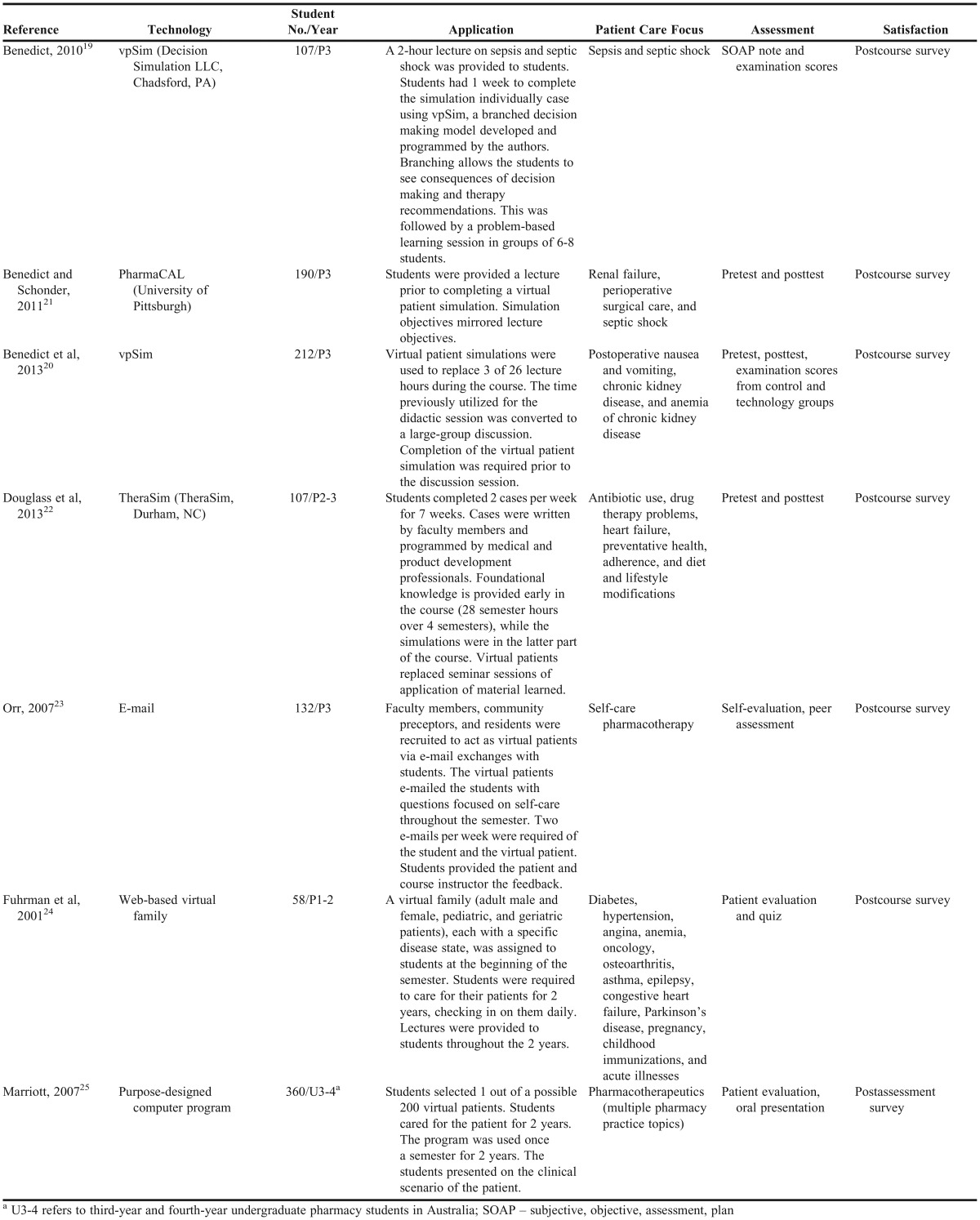
Virtual Patients
The use of virtual patients (VPs) was described by 7 studies involving approximately 1100 pharmacy students (Table 3). Software used included vpSim (Decision Simulation LLC, Chadsford, PA),19,20 PharmaCAL (University of Pittsburgh, PA),21 and TheraSim (TheraSim, Durham, NC).22 One study employed VPs via e-mail to students,23 1 developed a web-based “virtual family,”24 and the last designed their own VP program.25 Assessment data of the tools included Subjective Objective Assessment Plan (SOAP) note and examination scores, presimulation and postsimulation tests, presentations of patient evaluation, self-evaluation, and peer assessment. Satisfaction data was collected in the 7 studies using postcourse surveys. Descriptions of how the technology was utilized and how assessment and satisfaction data was collected are summarized in Table 3.
Virtual patients improved scores on examinations and/or poststimulation tests in all 7 studies.20-23 Three studies reported significant increases in postsimulation quiz scores (p<0.001)20-22 with the exception of 1 question in 1 study.22 In 1 study, the average examination score was 76%; however, the section of the examination covering VPs, the average score was 90%.19 When VPs replaced lectures in the same course for different subject material, there was no difference in scores between students who completed the VP case vs those the year before who attended the lecture.20 Final examination scores, an indicator of knowledge retention, were also similar between these groups.20 In addition to postsimulation quiz and examination scores, VP simulation significantly improved knowledge and problem-solving, communication, and professional skills, according to student self-assessments (p<0.001).23 Using 1 VP program, students answered 90% of quiz questions correctly, with a 99% response rate . This study reported no significant difference in quiz scores during the first semester; however, students who used the program had significantly higher scores in the second semester (p<0.05).24 In a study where students selected virtual patients themselves and cared for them for 2 years, the average score on a patient evaluation was 79%.25
As with the other educational technologies, survey response rates were high with VP activities (58.8-98%).20-22,24,25 Despite having little or no experience using VPs in their course work, 88% of pharmacy students reported no apprehension using them.21 This technology provided a positive experience for students, with 82-92% of students stating they enjoyed the use of VP in their coursework.19-21,24 Other data from the postcourse surveys indicated that 63-91% of students stated VPs contributed to their learning,19,20,22 71-88% stated the content was appropriate or covered the learning objectives,19,20 and 97-98% stated they were intellectually challenged.19,20 Specific skill sets improved with the use of VPs including medication therapy management, identification of pertinent patient information, understanding of electronic medical records and self-care skills.22,23 Students agreed that more simulation should be used, that it allowed for a better use of class time, and that they became better self-directed learners after using the simulations.20,21 Forty-three percent of students also stated that simulation helped prepare them for their APPEs.22 One study showed that students enjoyed selecting their own patients and that the majority of students learned more about the subject matter by completing the VP assignment.25
The use of VPs in pharmacy education was effective and provided students with a positive learning experience that could be continually repeated. Additionally, it showed that students were capable of self-directed learning, utilizing the technology with ease.20 This technology may be more easily used with larger numbers of students as it is less resource-intensive than HPS. Virtual patient technology has the ability to provide immediate assessment of student progression and feedback if programmed appropriately. As with HPS assessments, it could be built into the programs or conducted via presimulation and postsimulation examinations. Student satisfaction was effectively gauged using a postcourse survey.
DISCUSSION
The scope of this review included the use of technology in educating pharmacy students on the development of patient care skills. Educational technology is more pervasive than ever before in pharmacy curricula, but so too are the roles and responsibilities pharmacy graduates are expected to learn. Pharmacists with skills to be effective clinical providers, educators, and collaborators are needed. Because faculty members must meet this demand of the profession with innovative and effective teaching and learning methods, the design, development, implementation, and evaluation of educational technology is increasingly important.
This review aimed to summarize the available literature on the effectiveness of 3 broad categories of educational technology used in health care education: CAI, HPS, and VPs. The data collected from the studies in this review showed many similarities among the technologies. It was common for learning to be assessed using pretests and posttests, in addition to traditional methods such as examinations. Using postcourse surveys to collect satisfaction data from students was also common. Differences were noted in how the technology was utilized, in which courses technologies were used, and how many students the technology served. Computer-aided instruction appeared to be the most easily deployed technology and the most diverse, but studies that used it showed varied results in terms of student learning and satisfaction. Human-patient simulation worked well in higher-level learning and hands-on learning that directly affected patient care, was an effective teaching tool, and was widely enjoyed by students. Virtual patients were flexible and could be utilized in a variety of courses. While they did not provide the hands-on learning that HPS did, they could be directed at higher-level learning as well. Virtual patient technology, like HPS, was shown to be effective for student learning and was also enjoyed by students.
Each technology offered advantages over traditional teaching methods. These advantages were mainly the result of improved learning experience fidelity, repetition opportunities, faculty feedback, clinical variation, and individualized learning. However, these technologies were not without limitations. Barriers to implementing technology included student hesitation,9,15,20 the need for technical support/oversight,9,12,21,22 cost,13,21,26 and resource utilization (eg, space, faculty time).13,15,16,19-26
CONCLUSION
Learners of this era are accustomed to using technology, and their learning environments should reflect that. Although educational technology has become common in pharmacy education,1 there are still steps to take. The perception among faculty members and students exposed to technology is positive, from improved perception of learning, to satisfaction, to wanting more simulation activities, 27 and its use is widely encouraged by accreditation standards.3 The experiences reported in this review were overwhelmingly positive, although not all technology showed greater effectiveness in educating pharmacy students when compared to traditional pedagogy. This review should serve as a summary and encourage faculty members to engage students with the use of educational technology.
REFERENCES
- 1.Monaghan MS, Cain JJ, Malone PM, et al. Educational technology use among US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(5) doi: 10.5688/ajpe75587. Article 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medina MS, Plaza CM, Stowe CD, et al. Center for the advancement of pharmacy education 2013 educational outcomes. Am J Pharm Educ. 2013;77(8) doi: 10.5688/ajpe778162. Article 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed December 10, 2013.
- 4.Gleason BL, Peeters MJ, Resman-Targoff BH, et al. An active-learning strategies primer for achieving ability-based educational outcomes. Am J Pharm Educ. 2011;75(9) doi: 10.5688/ajpe759186. Article 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Association of American Medical Colleges Institute for Improving Medical Education. Effective Use of Educational Technology in Medical Education. Colloquium on Educational Technology: Recommendations and Guidelines for Medical Educators. March 2007.
- 6.Bollmeier SG, Wenger PJ, Forinash AB. Impact of online lecture-capture on student outcomes in a therapeutics course. Am J Pharm Educ. 2010;74(7) doi: 10.5688/aj7407127. Article 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ried LD, Byers K. Comparison of two lecture delivery platforms in a hybrid distance education program. Am J Pharm Educ. 2009;73(5) doi: 10.5688/aj730595. Article 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams J, Motycka C, St Onge E. Redesign of a pediatric pharmacotherapy elective course to accommodate budget reductions. Am J Pharm Educ. 2011;75(10) doi: 10.5688/ajpe7510206. Article 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jamero DJ, Borghol A, Mihm L. Comparison of computer-mediated learning and lecture-mediated learning for teaching pain management to pharmacy students. Am J Pharm Educ. 2009;73(1) doi: 10.5688/aj730105. Article 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelley KA, Beatty SJ, Legg JE, McAuley JW. A progress assessment to evaluate pharmacy students’ knowledge prior to beginning advanced pharmacy practice experiences. Am J Pharm Educ. 2008;72(4) doi: 10.5688/aj720488. Article 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pai VB, Kelley KA, Bellebaum KL. A technology-enhanced patient case workshop. Am J Pharm Educ. 2009;73(5) doi: 10.5688/aj730586. Article 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reinhold J, Pontiggia L, Angeles M, Earl G. Web-based instruction on substance abuse and drug diversion. Am J Pharm Educ. 2010;74(4) doi: 10.5688/aj740457. Article 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seybert AL, Kane-Gill SL. Elective course in acute care using online learning and patient simulation. Am J Pharm Educ. 2011;75(3) doi: 10.5688/ajpe75354. Article 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3) doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tofil NM, Benner KW, Worthington MA, Zinkan L, White ML. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740221. Article 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mieure KD, Vincent WR, 3rd, Cox MR, Jones MD. A high-fidelity simulation mannequin to introduce pharmacy students to advanced cardiovascular life support. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740222. Article 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seybert A. Patient simulation in pharmacy education. Am J Pharm Educ. 2011;75(9) doi: 10.5688/ajpe759187. Article 187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benedict N. Virtual patients and problem-based learning in advanced therapeutics. Am J Pharm Educ. 2010;74(8) doi: 10.5688/aj7408143. Article 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benedict N, Schonder K, McGee J. Promotion of self-directed learning using virtual patient cases. Am J Pharm Educ. 2013;77(7) doi: 10.5688/ajpe777151. Article 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benedict N, Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ. 2011;75(2) doi: 10.5688/ajpe75221. Article 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Douglass MA, Casale JP, Skirvin JA, DiVall MV. A virtual patient software program to improve pharmacy student learning in a comprehensive disease management course. Am J Pharm Educ. 2013;77(8) doi: 10.5688/ajpe778172. Article 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2) doi: 10.5688/aj710230. Article 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fuhrman LC, Buff WE, Eaddy M, Dollar M. Utilization of an integrated interactive virtual patient database in a web-based environment for teaching continuity of care. Am J Pharm Educ. 2001;65(3):271–275. [Google Scholar]
- 25.Marriott JL. Use and evaluation of “virtual” patients for assessment of clinical pharmacy undergraduates. Pharm Educ. 2007;7(4):341–349. [Google Scholar]
- 26.Use of Simulation in Pharmacy School Curricula. Health Workforce of Australia. https://www.hwa.gov.au/resources/publications. Accessed March 15, 2014.
- 27.DiVall MV, Hayney MS, Marsh W, et al. Perceptions of pharmacy students, faculty members, and administrators on the use of technology in the classroom. Am J Pharm Educ. 2013;77(4) doi: 10.5688/ajpe77475. Article 75. [DOI] [PMC free article] [PubMed] [Google Scholar]


