Abstract
The thyroid hormone, 3,3,5-triiodo-l-thyronine (T3), modulates several physiological processes, including cellular growth, differentiation, metabolism, inflammation and proliferation, via interactions with thyroid hormone response elements (TREs) in the regulatory regions of target genes. Infection and inflammation are critical processes in placental development and pregnancy-related diseases. In particular, infection is the leading cause of neonatal mortality and morbidity worldwide. However, to date, no successful approach has been developed for the effective diagnosis of infection in preterm infants. Pre-eclampsia (PE) is a serious disorder that adversely affects ~5% of human pregnancies. Recent studies identified a multiprotein complex, the inflammasome, including the Nod-like receptor (NLR) family of cytosolic pattern recognition receptors, the adaptor protein apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) and caspase-1, which plays a vital role in the placenta. The thyroid hormone modulates inflammation processes and is additionally implicated in placental development and disease. Therefore, elucidation of thyroid hormone receptor-regulated inflammation-related molecules, and their underlying mechanisms in placenta, should facilitate the identification of novel predictive and therapeutic targets for placental disorders. This review provides a detailed summary of current knowledge with respect to identification of useful biomarkers and their physiological significance in placenta.
Keywords: thyroid hormone receptor, infection, inflammasome, proteomics, placenta
1. Introduction
Pioneering proteomic approaches have been continually developed over several decades. Numerous technologies aimed at investigating protein-level regulation have been established, including one-dimensional SDS-PAGE, two-dimensional gel-electrophoresis, differential in-gel electrophoresis (DIGE), isotope-coded affinity tags (ICAT), isobaric tags for relative and absolute quantification (iTRAQ), and stable isotope labeling with amino acid in cell culture (SILAC) [1,2]. Recently, the global proteomics approach was successfully applied to the systemic investigation of the regulatory proteins of tumor-associated genes [3,4,5], biomarkers for pregnancy and inflammation-associated factors [6,7,8]. Furthermore, quantitative proteomic approaches have been utilized extensively in various biological fields, such as cancer biology, protein profiling, biomarker identification and quantification, and inflammasome regulation [9,10,11,12].
Transthyretin identified as a thyroid hormone-binding protein was discovered in human cerebrospinal fluid and serum [13]. Schreiber et al. [14] demonstrated that transthyretin is a typical negative acute-phase plasma protein, and the expression level was decreased following trauma, surgery and inflammation in liver and blood. Dickson et al. [14] proposed that when the body is in trauma or under inflammatory conditions, the transthyretin transcription rates in the choroid plexus would protect the brain against hypothyroidism. Transthyretin synthesis has been identified in various organs such as liver, choroid plexus of brain and placenta. Transthyretin synthesis is implicated in transporting thyroid hormones (THs) in the brain, and brain development depends on the effects of THs [15]. Furthermore, Roef et al. [16] reported the ratio of free T3-to-free T4 is positively associated with the adiposity-related inflammation markers interleukin-6 and C-reactive protein, and concluded that the higher ratio of free T3 to free T4 is consistently associated with numerous markers of adverse metabolic profile and cardiovascular risk. Therefore, we speculate that the thyroid hormone may play a role in inflammation processes. Here, we provide a detailed overview of the known regulatory processes of inflammation-related proteins and their physiological significance.
2. The Relationship between Inflammatory Processes and Placental Disorders
The immune system plays a crucial role in regulating the processes of both term and preterm labor characterized by altering pro-inflammatory cytokines significantly in gestational tissues [17,18]. Romero et al. [19] displayed several factors such as uteroplacental ischemia, cervical disease, decidual hemorrhage, stress, infection, and inflammation involved in the initiation of prematurity. Labor-associated inflammatory cytokines are characterized by immunocyte infiltration and the expression of tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, IL-8, and monocyte chemoattractant protein (MCP)-1 in the fetal membranes, cervix, amniotic fluid, and placenta are elevated. Expression of pro-inflammatory mediators resulted in (i) increases in prostaglandins, which promote uterine contractility; (ii) degradation of the chorioamnion extracellular matrix; and (iii) ripening of the cervix matrix metalloproteinases and reduced expression of tissue metalloproteinase inhibitors [18]. The magnitude of inflammation identified in term labor is commonly thought to be lower than in preterm labor [20]. Goldenberg et al. [21] suggested that the innate immune system plays an important role to trigger pro-inflammatory signaling in response to injury or infection in the premature initiation of labor. Infection is most commonly identified in the earliest preterm labors, those occurring before 28 weeks of gestation. Goldenberg and colleagues reported that 25%–40% of preterm deliveries resulted from intrauterine infection [21].
Previously, scientists have clarified that pre-eclampsia is a placental pathology with insufficient uteroplacental circulation leading to placental oxidative stress, hypoxia and infarction [22,23]. Redman et al. [24] proposed that pre-eclampsia develops when systemic inflammation, common to all pregnant women in the second half of pregnancy, cause one or other maternal systems to decompensate. Pre-eclampsia exhibits many classical features of inflammation and these are striking in late gestation [24,25]. Several groups have demonstrated a systemic maternal inflammatory response occurs in pre-eclampsia to affect circulating leukocytes. The granulocytes, monocytes and lymphocytes all displayed some degree of activation in pre-eclampsia compared with non-pregnant individuals [25,26]. Additionally, several scientists reported circulating pro-inflammatory cytokines are involved in pre-eclampsia. The circulating levels of TNF-α, IL-6 and IL-8 are significantly elevated in blood [27,28,29,30]. Furthermore, Xie et al. [31] reported that expression levels of TLR2, TLR4, IL-1β and NLRP3 are elevated in neutrophils of women with pre-eclampsia compared with normal pregnant women [32]. Recently, the NLRP3 inflammasome was demonstrated to be involved in placenta dysfunction in antiphospholipid syndrome-induced pre-eclampsia . According to these studies, we suggest that preterm labor and pre-eclampsia are inflammatory-associated disorders, and thus discuss these issues here.
3. Nuclear Receptor Family
The nuclear receptor (NR) superfamily is a highly conserved and extensively expressed group of ligand-mediated transcription factors in metazoans [33,34]. To date, numerous NRs have been identified in humans and mice, including classical, orphan and adopted orphan receptors [35]. Almost all NRs contain two highly conserved domains: a central DNA-binding domain and ligand-binding domain positioned along the C-terminus [36,37]. NRs are activated upon binding to their ligands or undergo ligand-independent activation via post-translational modifications, such as phosphorylation. These receptors mediate specific gene expression by binding to DNA or recruit coregulatory factors to influence various biological processes, including reproduction, metabolism and homeostasis. NRs have been shown to play critical roles, not only in normal homeostatic and metabolic processes, but also diseases, such as inflammation, cancer and obesity [38,39]. Furthermore, Liu et al. [40] used DNA constructs of hormone response elements and mass spectrometry to profile the DNA binding activity of the NR superfamily in mouse liver. Consequently, 35 members of the NR family were detected at the protein level in this study. This approach provides a useful tool to increase coverage of the whole NR proteome for application in studies on DNA binding, cellular translocation and other physiological and pathological conditions, such as inflammation, pregnancy and cancer processes [40].
4. Thyroid Hormone Involvement in Inflammation Processes
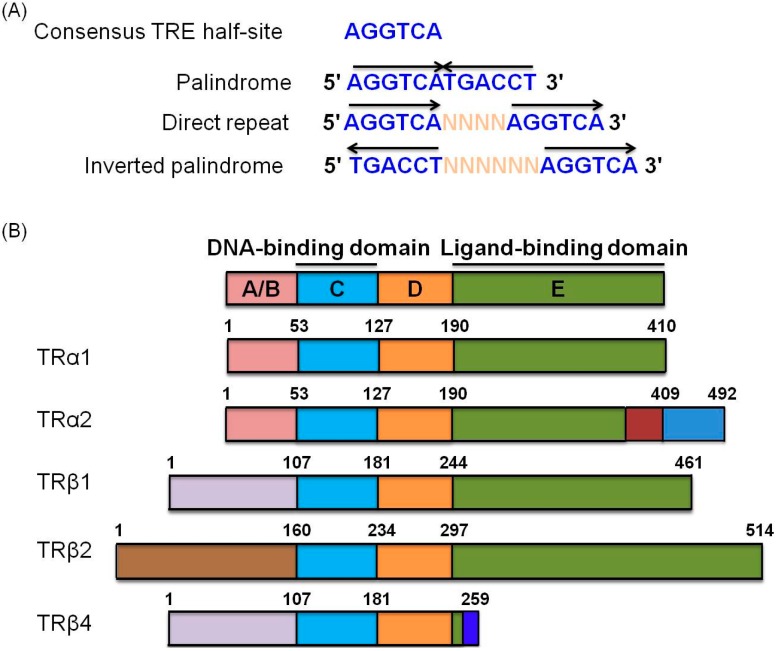
Thyroid hormone receptors (TRs) belong to the superfamily of nuclear hormone receptors that modulate transcription of various genes [41,42]. TH acts as a pleiotropic regulator of growth, differentiation, proliferation and other physiological processes through interactions with thyroid hormone response elements (TREs) located in the regulatory regions of target genes [43] (Figure 1A). Previously, Chang et al. [44] reported that the putative consensus hexamer half-site sequence of TRE is AGGTCA. TREs are arranged as direct repeats (DR), palindromes and inverted palindromes (IP), and vary considerably in terms of nucleotide sequence as well as spacing, number and orientation of half-sites [41,44]. Importantly, TH is required to maintain the metabolic rate and oxygen consumption in almost all tissues [37]. TRs contain several domains analogous to other nuclear receptors, including the amino terminal A/B domain, DNA-binding domain (DBD), hinge region containing the nuclear localization signal, and a carboxy-terminal ligand-binding domain (LBD) with specific functions [45,46,47,48] (Figure 1B). These receptors interact with the retinoid X receptor (RXR) to form heterodimers that influence expression of target genes by binding to their TRE regions [49]. Numerous genes, including coagulation factor system components [50], plasma proteins [50,51], nuclear receptor coactivator [52], anti-metastatic proteins [53], proteases [49] oncogenes [5] and inflammatory-associated genes [54], are regulated by thyroid hormone receptors. Proteomic approaches have identified several coregulators that interact with the thyroid hormone receptor, such as steroid receptor coactivator 1–3, thyroid hormone receptor-associated protein 220, Peroxisome Proliferator-activated Receptor-γ Coativator-1, Thyroid Hormone Receptor-binding Protein, p300, Androgen Receptor Activator 70, receptor interacting protein 140, dosage-sensitive sex reversal-adrenal hypoplasia congenital critical region of the X chromosome 1, small heterodimer partner, nuclear receptor corepressor and silencing mediator of retinoid and thyroid hormone receptors [55].
Figure 1.
Schematic representation of consensus TRE half-sites and TRα and TRβ isoforms. (A) The consensus half-site of TRE is divided into palindrome, direct repeat and inverted palindrome sequences. Each half-site presents different orientations and nucleotide spacing (N: nucleotide; arrows: half-site orientation); (B) TRα1 and TRβ1 are generated by alternative splicing and promoter usage from TRα and TRβ. TR isoforms contain several functional domains, including an amino terminal region (A/B domain), conserved DNA-binding domain (DBD) (C domain), hinge region that links the DBD and ligand-binding domains (LBD) (D domain), and LBD responsible for receptor dimerization (E domain). Functional domains with similar amino acid sequences are depicted in the same color.
Thyroid hormone levels are associated with major physiological regulatory processes during nutritional adaptation. Recent studies have reported that leptin signaling, mediated by the JAK/STAT pathway, plays a vital role in maintaining TRH, TSH and thyroid hormone expression [56]. Obesity, enhanced by nutrient excess, is characterized by enlarged adipose cells and chronic inflammation [57]. Moreover, hyperleptinemia is reported to increase the index of autoimmune disease via regulation of proinflammatory cytokines and macrophages [58]. Thyroid hormones were linked with obesity more than a century ago, and obesity plays a critical factor in hypothyroidism [59]. Duntas et al. [59] reported that thyroid autoimmunity is highly related with the regulation of inflammasome-related cytokines in obesity [59]. Based on the above evidence, we speculate that inflammation may be regulated through interactions between coregulators and the thyroid hormone receptor.
5. Thyroid Hormone Is Associated with Placental Development and Disease
Abnormalities of the maternal thyroid hormone in pregnancy are associated with neurodevelopmental deficiencies in offspring [60,61]. Additionally, T3 and T4 exert effects in several fetal organs, including limbs, brain and liver, from 6–12 weeks of gestation [62]. TH receptors, TH transporters and deiodinase enzymes are expressed in the fetal cerebral cortex at seven weeks gestation. Hence, maternal THs play an essential role in early gestation [63,64]. Maternal T4 crosses the placenta in the first and third trimester of pregnancy. Clinical studies have shown that decreased TH levels can result in serious adverse effects on intellectual development of fetus [65,66,67]. Maternally-derived TH, when transported through the placenta, influences neural progenitor proliferation, migration and differentiation within the developing embryo before the onset of endogenous TH production [68,69]. Oki et al. [70] reported the effects of maternal thyroid dysfunction on placental development. Furthermore, THs have been shown to influence villous and extravillous trophoblast proliferation, invasion and viability in vitro [71]. Larijian et al. [72] reported that free T4 and TSH levels were increased significantly in patients with mild pre-eclampsia compared with healthy controls. Furthermore, in severe pre-eclampsia cases, the TSH value was higher, but free T3 and free T4 were significantly lower than in controls. The evidence provided a hint that hypofunctioning of the thyroid can result in mild pre-eclampsia and possibly contribute to the pathogenesis. Kumar et al. [73] reported that TSH levels were significantly higher in pre-eclampsia patients compared with controls. However, thyroid hormones values were in the normal range. The TSH titers were over 5 mIU/mL in about 40% pre-eclamptic patients in the study group compared with 12.2% in the controls. Additionally, the T3, free T3 and free T4 levels were lower in preterm infants born to pre-eclamptic mothers with placental insufficiency than preterm infants born to mothers without placental insufficiency. However, the TSH value was higher in preterm infants born to pre-eclamptic mothers with placental insufficiency. Hence, high levels of TSH and low levels of thyroid hormones in cord blood of premature infants born to pre-eclamptic mothers with placental insufficiency imply intrauterine hypothyroidism [73]. Kurlak and co-workers similarly reported lower thyroid hormone levels in pre-eclampsia pregnancy cases [74]. Collectively, we speculate that the levels of thyroid hormone or TSH or hypothyroidism may be a factor to influence pre-eclampsia.
6. Inflammasome Functions in Placental Disease
The innate immune system is activated under conditions of microbial infection, such as pathogen-associated molecular patterns (PAMP), damage-associated molecular patterns (DAMP), and tissue damage. Macrophages are vital players in the innate defense system. Activated macrophages secrete proteins to influence the immune response and recruit other immune cells to the tissue damaged area of infected sites [75]. Valimaki et al. [76] analyzed the human primary macrophage secretome stimulated with monosodium urate (MSU) using the high-throughput quantitative gel electrophoresis liquid chromatography-mass spectrometry/mass spectrometry (GeLC-MS/MS) approach combining protein separation via SDS-PAGE and identification with liquid chromatography-MS/MS. MSU, a metabolite released by uric acid, acts as an endogenous DAMP molecule [77]. Results based on bioinformatic analyses clearly indicate that MSU stimulates protein secretion via an unconventional mechanism. Several proteins within the secretome are secreted via vesicle-mediated processes, including the pro-inflammatory cytokines IL-18, IL-1β, interferon-induced proteins and danger signal proteins. Additionally, active forms of lysosomal proteases belonging to the cathepsin family are secreted after MSU stimulation, and cathepsin activity is essential for MSU-induced unconventional protein secretion. MSU mediates protein secretion via the cathepsin-src-Pyk2-PI3 kinase signal cascade in human macrophages [76]. Cysteinyl aspartate-specific proteases (caspases) play critical roles in inflammation and apoptosis [78]. In humans, 11 members of the caspase family have been identified, which are divided into three phylogenetic groups depending on their function [79]. Aspartate-specific cysteine protease caspase-1 is activated in the inflammasome-mediated inflammation process, and responsible for the maturation and release of the cytokines IL-1β and IL-18 during infection and inflammation [80]. Lamkaanfi and co-workers applied a proteome-wide gel-free differential peptide sorting methodology to identify novel caspase-1 substrates. Among the 1022 proteins identified, 20 were validated as caspase-1 substrates for the first time. The results additionally revealed the existence of a nucleotide binding and oligomerization domain-like receptor/caspase-1/caspase-7 cascade in response to microbial stimuli and bacterial infection [81].
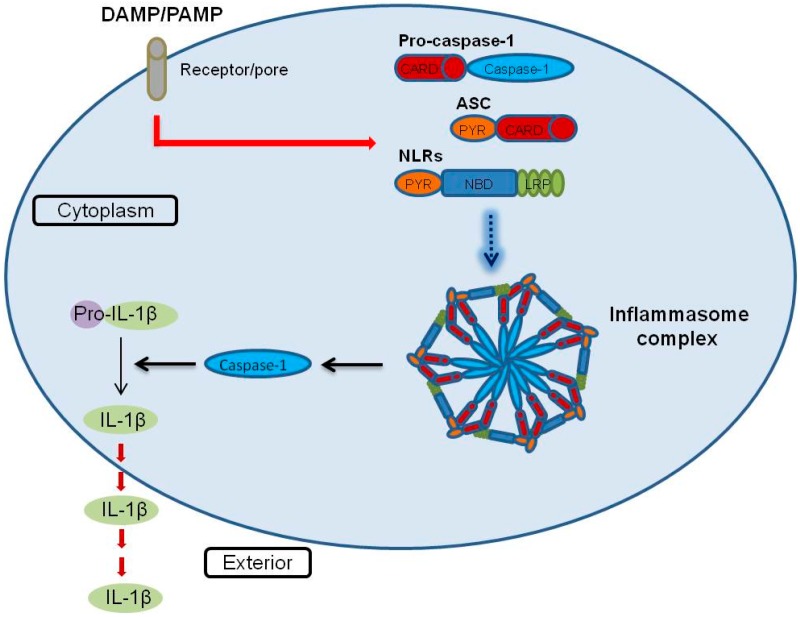
Proteases are distributed extensively, constituting more than 2% of the total human genome, and play diverse roles in cellular processes, such as cell death, catabolism and immune function [82,83]. Human caspases (cysteine aspartyl proteases) consist of 12 homodimeric cysteine proteases that cleave various proteins. The human caspase family is divided into three categories based on their sequences and functional similarities. Caspase-1, -4, and -5 are inflammatory caspases, identified as activators of proinflammatory cytokines [84]. Although caspase-1 is known to be involved in the inflammasome mechanism, the underlying mechanisms by which inflammatory caspases exert their effects are yet to be elucidated [85]. The inflammasome has been recently defined as a multiprotein complex including a Nod-like receptor (NLR) family of cytosolic pattern recognition receptors, the adaptor protein apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC), and caspase-1 [86]. Inflammasomes are activated by damage-associated molecular patterns (DAMPs) and pathogen-associated molecular patterns (PAMPs), such as bacterial toxins, viral DNA and RNA, extracellular ATP and reactive oxygen species (ROS) [87,88,89,90]. Inflammasome assembly leads to caspase-1-dependent cleavage and release of proinflammatory cytokines, IL-1β and IL-18 [91] (Figure 2). The substrates of these inflammatory caspases remain to be fully clarified. Agard et al. [92], using a quantitative stable isotope labeling with amino acids in cell culture (SILAC) approach in THP-1 cells, identified 82 putative caspase-1-cleaved products and three putative caspase-4 substrates, but no substrates for caspase-5 [92]. Since caspase-1 possesses an extensive range of substrates, it may play a more critical role in inflammatory processes than caspases-4 and -5 in macrophage cells.
Figure 2.
Schematic representation of the inflammasome activation model. Model depicting the regulation of inflammasome activation. Foreign factors, such as DAMP and PAMP, stimulate NLRs, ASC and pro-caspase-1, followed by formation of the inflammasome complex. Subsequently, pro-caspase-1 is cleaved into caspase-1 via activation of the inflammasome complex. Pro-IL-1β is cleaved into mature IL-1β and secreted to the macrophage extracellular matrix. (DAMP: damage-associated molecular patterns, PAMP: pathogen-associated molecular patterns, NLR: Nod-like receptor, ASC: apoptosis-associated speck-like protein containing a caspase recruitment domain, IL-1β: interleukin-1β).
Abrahams et al. [93,94,95] reported that placental trophoblasts express not only Toll-like receptors (TLRs) but also NLRs. Several NLRs and known activators of DAMPs and PAMPs have recently been identified (Table 1). To date, 14 NLR proteins (NLRPs) have been discovered in addition to NOD proteins, and some receptors are activated by infectious stimuli, such as pathogens in trophoblasts [96]. Among the NLRs, Nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinases possess diverse roles and activate different signaling pathways in inflammation processes [97,98]. Clinical studies have demonstrated a significant correlation between placental infection/inflammation and prematurity [99].
Table 1.
NLRs-recognized damage-associated molecular pattern DAMP and pathogen-associated molecular patternPAMP.
| NLRs | DAMP | PAMP |
|---|---|---|
| NOD1 | Bacterial peptidoglycan, γ-d-glutamyl-meso-diaminopimelic acid | |
| NOD2 | Bacterial peptidoglycan, Muramyl dipeptide | |
| IPAF | Bacterial (Salmonella typhimurium, Pseudomonas aeruginosa, Legionellapneumophila) | |
| NALP1 | Bacterial | |
| NALP3 | Hyaluronan, uric acid crystals, ATP, silica, asbestos, alum | Bacteria (Staphylococcus aureus, Shigella flexneri), viruses (Adenovirus, Influenza virus), fungi (Saccharomyces cerevisiae), muramyl dipeptide, bacterial pore-forming toxin, bacteria RNA, malarial crystals |
The inflammasome plays a vital role in both macrophage immunity and cancer cell progression [8,80]. Wang et al. [8] systematically investigated the interactome components of inflammasomes in nasopharyngeal carcinoma using the iTRAQ quantitative assay. Using this method, 172 non-redundant proteins were identified in the inflammasome-interacting complex of HK1/ASC cells. Within the interactome profile, the end-binding protein 1 (EB1) is crucial for stimulating the inflammasome via direct interactions with AIM2 and ASC, both in vitro and in vivo [8]. EB1 is an adenomatous polyposis coli (APC)-binding protein that regulates microtubule polymerization [100]. Several studies have demonstrated crucial roles of EB1 in biological processes, such as mitosis and signal transduction [101,102]. Furthermore, numerous microtubule-associated proteins are highly expressed during macrophage activation [103]. Based on these findings, microtubule-associated proteins are proposed to play a role in pre-activation or stabilization of the inflammasome [104].
Pre-eclampsia (PE) is a serious disorder that adversely affects ~5% human pregnancies. No useful biomarkers or approaches are currently available to identify and treat pre-eclampsia [105]. Subgroup classification is an effective approach to improve the accuracy of predictions for pregnancy outcomes to individualize breast cancer prognosis and treatment [106]. Clinically, gestational hypertension and proteinuria are the basis of the diagnosis in pre-eclampsia [107]. Cox et al. [108] used the shotgun proteomics approach to identify biomarkers of pre-eclampsia with diverse subgroups from plasma membrane proteins at the blood interfaces. In total, 1181 plasma membrane proteins were identified, among which 171 were highly expressed at the maternal blood-trophoblast interface and 192 at the fetal endothelial interface. Various genes from distinct subgroups were enriched. The finding that clinically similar pre-eclampsia patients display distinct gene expression profiles in the placenta implies the existence of divergent molecular mechanisms in pre-eclampsia [108].
A considerable number (12.3%) of live pregnancies are influenced by preterm delivery in the US, which is a main risk of neonatal mortality and morbidity and a considerable burden on the healthcare system [109]. Infection is common and a leading cause of neonatal mortality and morbidity worldwide [110,111]. A significant clinical correlation between infection and preterm labor has been demonstrated, especially for infants delivered before 30 weeks [112]. Several studies have demonstrated that numerous pro-inflammatory genes are up-regulated in both myometrium [113,114] and fetal membrane [115,116] with labor onset. The inflammatory cells enter the uterus and elevate levels of pro-inflammatory cytokines in the parturition process with both preterm and term labor [117]. The expression levels of TNF-α, IL-1β, IL-6 are increased in amniotic fluid [118,119]; furthermore IL-1β and IL-6 expression are elevated in the myometrium [120], amnion [121] and choriodecidua [121]. NF-κB is an inflammatory-associated transcription factor, which is activated in response to infection and pro-inflammatory cytokines induced in labor. Numerous labor-associated and pro-inflammatory genes are influenced by NF-κB, and aberrant NF-κB activity can result in a series of inflammatory-related disorders [122,123]. Moreover, scientists have reported the p65 expression level is elevated in both nuclear and cytosolic fractions in fundal uterine segment myometrium in human labor [124]. Stjernholm-Vladic et al. [125] reported that NF-κB expression in the nucleus is increased at parturition in the cervix. Additionally, NF-κB DNA binding activity in the amnion is regulated by IL-1β such as p50/p65 heterodimer, p50 and p65 homodimers [126]. Allport et al. [127] reported that the DNA binding and transcriptional activities of NF-κB are elevated in amnion cells following spontaneous labor compared with amnion cells at term, suggesting that in labor, NF-κB possesses a critical role in the amnion. Take together, we speculate that NF-κB signaling pathway play a vital role in placental development, inflammation and the parturition processes both in term, and preterm labor.
Diagnosis of infection in preterm infants is extremely difficult. Clinical diagnosis is based on a number of non-specific characteristics, such as difficulty in breathing, unstable temperature and heart rate, and jaundice [128,129]. Therefore, a rapid and reliable diagnostic test is essential for the clinical identification of neonatal infection. Kingsmore et al. [7] used immunoassay arrays to detect 142 cytokines in neonatal serum. Eight serum proteins associated with inflammation, fibrinolysis and coagulation were markedly elevated in infected neonates, including interleukin 18, interleukin 2 soluble receptor α, P- and E-selectins, neutrophil elastase, C-reactive protein, urokinase plasminogen activator and its cognate receptor. Multiplexed immunoassays of the serum biomarker panel have utility for rapid diagnosis and improve the diagnostic performance for neonatal infection [7].
Amniotic fluid (AF) is a complex and dynamic biological fluid that provides nutrients and protection required for fetal growth. Hence, qualitative and quantitative integrity of AF is essential for normal fetal development during gestation. Free diffusion occurs between the fetus and the AF through fetal skin, placenta and the umbilical cord at 10 to 20 weeks gestation [130]. Therefore, analysis of AF components before skin keratinization that occurs between 19 and 20 weeks of gestation may provide critical information for predicting the physiological and pathological status of the fetus. Cho and co-workers [6] investigated the complexity of AF using three differential fractionation approaches to increase coverage, specifically, two-dimensional LC-MS/MS as well as LC-SDS-PAGE-LC-MS/MS platforms. Based on these methods, 842 non-redundant proteins were identified in the AF proteome. Within the AF proteome, biomarkers from several categories have been identified, including intra-amniotic infection, preterm delivery and chromosomal anomalies of the fetus. These findings provide clues that aid in determining the capability of amniotic fluid and detection of significant biomarkers for prenatal diagnosis of fetal abnormalities.
7. Conclusions
The thyroid hormone is implicated in various processes, including cancer biology, lipid metabolism, autophagy and inflammation [37,54,131,132]. Inflammation is a critical cellular process in placental development and pregnancy [133]. To date, no useful approaches have been developed to predict pregnancy complications, such as preterm labor. Diagnosis of infection in preterm infants is complex, and clinical identification of neonatal infection is a difficult process based on nonspecific features, such as jaundice, difficulty in breathing and feeding, and unstable temperature [128,134]. However, several cytokines and chemokines are significantly altered in infected neonates [7]. Furthermore, thyroid hormone plays a role in inflammation, placental development and pregnancy-related diseases [70,72]. The inflammasome is clearly implicated in placental trophoblast activity and pregnancy complications [96,135]. In summary, we have provided an overview of several proteomic approaches that may be effectively applied to identify useful biomarkers for the prediction of pregnancy-related diseases and establish specific roles of the thyroid hormone and inflammasome in placenta and pregnancy disorders.
Acknowledgments
This work was supported by grants from Chang-Gung Memorial Hospital, Taoyuan, Taiwan (CMRPD190401, CMRPD190402, CMRPD190403, CMRPD190404).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Everley P.A., Krijgsveld J., Zetter B.R., Gygi S.P. Quantitative cancer proteomics: Stable isotope labeling with amino acids in cell culture (SILAC) as a tool for prostate cancer research. Mol. Cell. Proteomics. 2004;3:729–735. doi: 10.1074/mcp.M400021-MCP200. [DOI] [PubMed] [Google Scholar]
- 2.Uitto P.M., Lance B.K., Wood G.R., Sherman J., Baker M.S., Molloy M.P. Comparing SILAC and two-dimensional gel electrophoresis image analysis for profiling urokinase plasminogen activator signaling in ovarian cancer cells. J. Proteome Res. 2007;6:2105–2112. doi: 10.1021/pr060638v. [DOI] [PubMed] [Google Scholar]
- 3.Planque C., Kulasingam V., Smith C.R., Reckamp K., Goodglick L., Diamandis E.P. Identification of five candidate lung cancer biomarkers by proteomics analysis of conditioned media of four lung cancer cell lines. Mol. Cell. Proteomics. 2009;8:2746–2758. doi: 10.1074/mcp.M900134-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gronborg M., Kristiansen T.Z., Iwahori A., Chang R., Reddy R., Sato N., Molina H., Jensen O.N., Hruban R.H., Goggins M.G., et al. Biomarker discovery from pancreatic cancer secretome using a differential proteomic approach. Mol. Cell. Proteomics. 2006;5:157–171. doi: 10.1074/mcp.M500178-MCP200. [DOI] [PubMed] [Google Scholar]
- 5.Chen C.Y., Chi L.M., Chi H.C., Tsai M.M., Tsai C.Y., Tseng Y.H., Lin Y.H., Chen W.J., Huang Y.H., Lin K.H. Stable isotope labeling with amino acids in cell culture (SILAC)-based quantitative proteomics study of a thyroid hormone-regulated secretome in human hepatoma cells. Mol. Cell. Proteomics. 2012;11 doi: 10.1074/mcp.M111.011270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho C.K., Shan S.J., Winsor E.J., Diamandis E.P. Proteomics analysis of human amniotic fluid. Mol. Cell. Proteomics. 2007;6:1406–1415. doi: 10.1074/mcp.M700090-MCP200. [DOI] [PubMed] [Google Scholar]
- 7.Kingsmore S.F., Kennedy N., Halliday H.L., van Velkinburgh J.C., Zhong S., Gabriel V., Grant J., Beavis W.D., Tchernev V.T., Perlee L., et al. Identification of diagnostic biomarkers for infection in premature neonates. Mol. Cell. Proteomics. 2008;7:1863–1875. doi: 10.1074/mcp.M800175-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang L.J., Hsu C.W., Chen C.C., Liang Y., Chen L.C., Ojcius D.M., Tsang N.M., Hsueh C., Wu C.C., Chang Y.S. Interactome-wide analysis identifies end-binding protein 1 as a crucial component for the speck-like particle formation of activated absence in melanoma 2 (AIM2) inflammasomes. Mol. Cell. Proteomics. 2012;11:1230–1244. doi: 10.1074/mcp.M112.020594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saraon P., Cretu D., Musrap N., Karagiannis G.S., Batruch I., Drabovich A.P., van der Kwast T., Mizokami A., Morrissey C., Jarvi K., et al. Quantitative proteomics reveals that enzymes of the ketogenic pathway are associated with prostate cancer progression. Mol. Cell. Proteomics. 2013;12:1589–15601. doi: 10.1074/mcp.M112.023887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen R., Pan S., Brentnall T.A., Aebersold R. Proteomic profiling of pancreatic cancer for biomarker discovery. Mol. Cell. Proteomics. 2005;4:523–533. doi: 10.1074/mcp.R500004-MCP200. [DOI] [PubMed] [Google Scholar]
- 11.Andreyev A.Y., Shen Z., Guan Z., Ryan A., Fahy E., Subramaniam S., Raetz C.R., Briggs S., Dennis E.A. Application of proteomic marker ensembles to subcellular organelle identification. Mol. Cell. Proteomics. 2010;9:388–402. doi: 10.1074/mcp.M900432-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bell C., English L., Boulais J., Chemali M., Caron-Lizotte O., Desjardins M., Thibault P. Quantitative proteomics reveals the induction of mitophagy in tumor necrosis factor-α-activated (TNFα) macrophages. Mol. Cell. Proteomics. 2013;12:2394–2407. doi: 10.1074/mcp.M112.025775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ingbar S.H. Pre-albumin: A thyroxinebinding protein of human plasma. Endocrinology. 1958;63:256–259. doi: 10.1210/endo-63-2-256. [DOI] [PubMed] [Google Scholar]
- 14.Richardson S.J. Evolutionary changes to transthyretin: Evolution of transthyretin biosynthesis. FEBS J. 2009;276:5342–5356. doi: 10.1111/j.1742-4658.2009.07244.x. [DOI] [PubMed] [Google Scholar]
- 15.Dickson P.W., Aldred A.R., Marley P.D., Bannister D., Schreiber G. Rat choroid plexus specializes in the synthesis and the secretion of transthyretin (prealbumin). Regulation of transthyretin synthesis in choroid plexus is independent from that in liver. J. Biol. Chem. 1986;261:3475–3478. [PubMed] [Google Scholar]
- 16.Roef G.L., Rietzschel E.R., van Daele C.M., Taes Y.E., de Buyzere M.L., Gillebert T.C., Kaufman J.M. Triiodothyronine and free thyroxine levels are differentially associated with metabolic profile and adiposity-related cardiovascular risk markers in euthyroid middle-aged subjects. Thyroid. 2014;24:223–231. doi: 10.1089/thy.2013.0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rinaldi S.F., Hutchinson J.L., Rossi A.G., Norman J.E. Anti-inflammatory mediators as physiological and pharmacological regulators of parturition. Expert Rev. Clin. Immunol. 2011;7:675–696. doi: 10.1586/eci.11.58. [DOI] [PubMed] [Google Scholar]
- 18.Challis J.R., Lockwood C.J., Myatt L., Norman J.E., Strauss J.F., Petraglia F. Inflammation and Pregnancy. Reprod. Sci. 2009;16:206–215. doi: 10.1177/1933719108329095. [DOI] [PubMed] [Google Scholar]
- 19.Romero R., Espinoza J., Kusanovic J.P., Gotsch F., Hassan S., Erez O., Chaiworapongsa T., Mazor M. The preterm parturition syndrome. BJOG. 2006;113:17–42. doi: 10.1111/j.1471-0528.2006.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gotsch F., Romero R., Erez O., Vaisbuch E., Kusanovic J.P., Mazaki-Tovi S., Kim S.K., Hassan S., Yeo L. The preterm parturition syndrome and its implications for understanding the biology, risk assessment, diagnosis, treatment and prevention of preterm birth. J. Matern. Fetal Neonatal Med. 2009;22:5–23. doi: 10.1080/14767050902860690. [DOI] [PubMed] [Google Scholar]
- 21.Goldenberg R.L., Culhane J.F., Iams J.D., Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brosens I., Renaer M. On the pathogenesis of placental infarcts in pre-eclampsia. J. Obstet. Gynaecol. Br. Commonw. 1972;79:794–799. doi: 10.1111/j.1471-0528.1972.tb12922.x. [DOI] [PubMed] [Google Scholar]
- 23.Pijnenborg R., Anthony J., Davey D.A., Rees A., Tiltman A., Vercruysse L., van Assche A. Placental bed spiral arteries in the hypertensive disorders of pregnancy. Br. J. Obstet. Gynaecol. 1991;98:648–655. doi: 10.1111/j.1471-0528.1991.tb13450.x. [DOI] [PubMed] [Google Scholar]
- 24.Redman C.W., Sargent I.L. Pre-eclampsia, the placenta and the maternal systemic inflammatory response—A review. Placenta. 2003;24:S21–S27. doi: 10.1053/plac.2002.0930. [DOI] [PubMed] [Google Scholar]
- 25.Redman C.W., Sacks G.P., Sargent I.L. Preeclampsia: An excessive maternal inflammatory response to pregnancy. Am. J. Obstet. Gynecol. 1999;180:499–506. doi: 10.1016/S0002-9378(99)70239-5. [DOI] [PubMed] [Google Scholar]
- 26.Sacks G.P., Studena K., Sargent K., Redman C.W. Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. Am. J. Obstet. Gynecol. 1998;179:80–86. doi: 10.1016/S0002-9378(98)70254-6. [DOI] [PubMed] [Google Scholar]
- 27.Greer I.A., Lyall F., Perera T., Boswell F., Macara L.M. Increased concentrations of cytokines interleukin-6 and interleukin-1 receptor antagonist in plasma of women with preeclampsia: A mechanism for endothelial dysfunction? Obstet. Gynecol. 1994;84:937–940. [PubMed] [Google Scholar]
- 28.Vince G.S., Starkey P.M., Austgulen R., Kwiatkowski D., Redman C.W. Interleukin-6, tumour necrosis factor and soluble tumour necrosis factor receptors in women with pre-eclampsia. Br. J. Obstet. Gynaecol. 1995;102:20–25. doi: 10.1111/j.1471-0528.1995.tb09020.x. [DOI] [PubMed] [Google Scholar]
- 29.Ellis J., Wennerholm U.B., Bengtsson A., Lilja H., Pettersson A., Sultan B., Wennergren M., Hagberg H. Levels of dimethylarginines and cytokines in mild and severe preeclampsia. Acta Obstet. Gynecol. Scand. 2001;80:602–608. doi: 10.1080/j.1600-0412.2001.800703.x. [DOI] [PubMed] [Google Scholar]
- 30.Benyo D.F., Smarason A., Redman C.W., Sims C., Conrad K.P. Expression of inflammatory cytokines in placentas from women with preeclampsia. J. Clin. Endocrinol. Metab. 2001;86:2505–2512. doi: 10.1210/jcem.86.6.7585. [DOI] [PubMed] [Google Scholar]
- 31.Mulla M.J., Salmon J.E., Chamley L.W., Brosens J.J., Boeras C.M., Kavathas P.B., Abrahams V.M. A role for uric acid and the Nalp3 inflammasome in antiphospholipid antibody-induced IL-1β production by human first trimester trophoblast. PLoS One. 2013;8:e65237. doi: 10.1371/journal.pone.0065237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie F., Hu Y., Turvey S.E., Magee L.A., Brunham R.M., Choi K.C., Krajden M., Leung P.C., Money D.M., Patrick D.M., et al. Toll-like receptors 2 and 4 and the cryopyrin inflammasome in normal pregnancy and pre-eclampsia. BJOG. 2010;117:99–108. doi: 10.1111/j.1471-0528.2009.02428.x. [DOI] [PubMed] [Google Scholar]
- 33.Margolis R.N., Christakos S. The nuclear receptor superfamily of steroid hormones and vitamin D gene regulation. An update. Ann. N. Y. Acad. Sci. 2010;1192:208–214. doi: 10.1111/j.1749-6632.2009.05227.x. [DOI] [PubMed] [Google Scholar]
- 34.Mangelsdorf D.J., Thummel C., Beato M., Herrlich P., Schutz G., Umesono K., Blumberg B., Kastner P., Mark M., Chambon P., et al. The nuclear receptor superfamily: The second decade. Cell. 1995;83:835–859. doi: 10.1016/0092-8674(95)90199-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang Z., Burch P.E., Cooney A.J., Lanz R.B., Pereira F.A., Wu J., Gibbs R.A., Weinstock G., Wheeler D.A. Genomic analysis of the nuclear receptor family: New insights into structure, regulation, and evolution from the rat genome. Genome Res. 2004;14:580–590. doi: 10.1101/gr.2160004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jin L., Li Y. Structural and functional insights into nuclear receptor signaling. Adv. Drug Deliv. Rev. 2010;62:1218–1226. doi: 10.1016/j.addr.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen C.Y., Tsai M.M., Chi H.C., Lin K.H. Biological significance of a thyroid hormone-regulated secretome. Biochim. Biophys. Acta. 2013;1834:2271–2184. doi: 10.1016/j.bbapap.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Arrese M., Karpen S.J. Nuclear receptors, inflammation, and liver disease: Insights for cholestatic and fatty liver diseases. Clin. Pharmacol. Ther. 2010;87:473–478. doi: 10.1038/clpt.2010.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trauner M., Halilbasic E. Nuclear receptors as new perspective for the management of liver diseases. Gastroenterology. 2011;140:1120–1125. doi: 10.1053/j.gastro.2011.02.044. [DOI] [PubMed] [Google Scholar]
- 40.Liu Q., Ding C., Liu W., Song L., Liu M., Qi L., Fu T., Malovannaya A., Wang Y., Qin J., et al. In-depth proteomic characterization of endogenous nuclear receptors in mouse liver. Mol. Cell. Proteomics. 2013;12:473–484. doi: 10.1074/mcp.M112.022319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aranda A., Pascual A. Nuclear hormone receptors and gene expression. Physiol. Rev. 2001;81:1269–1304. doi: 10.1152/physrev.2001.81.3.1269. [DOI] [PubMed] [Google Scholar]
- 42.Walters M.R., Nemere I. Receptors for steroid hormones: Membrane-associated and nuclear forms. Cell. Mol. Life Sci. 2004;61:2309–2321. doi: 10.1007/s00018-004-4065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim W.G., Cheng S.Y. Thyroid hormone receptors and cancer. Biochim. Biophys. Acta. 2012;1830:3928–3936. doi: 10.1016/j.bbagen.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cheng S.Y. Multiple mechanisms for regulation of the transcriptional activity of thyroid hormone receptors. Rev. Endocr. Metab. Disord. 2000;1:9–18. doi: 10.1023/A:1010052101214. [DOI] [PubMed] [Google Scholar]
- 45.Izumo S., Mahdavi V. Thyroid hormone receptor α isoforms generated by alternative splicing differentially activate myosin HC gene transcription. Nature. 1988;334:539–542. doi: 10.1038/334539a0. [DOI] [PubMed] [Google Scholar]
- 46.Mitsuhashi T., Tennyson G.E., Nikodem V.M. Alternative splicing generates messages encoding rat C-ERBA proteins that do not bind thyroid hormone. Proc. Natl. Acad. Sci. USA. 1988;85:5804–5808. doi: 10.1073/pnas.85.16.5804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nakai A., Seino S., Sakurai A., Szilak I., Bell G.I., DeGroot L.J. Characterization of a thyroid hormone receptor expressed in human kidney and other tissues. Proc. Natl. Acad. Sci. USA. 1988;85:2781–2785. doi: 10.1073/pnas.85.8.2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yen P.M., Chin W.W. New advances in understanding the molecular mechanisms of thyroid hormone action. Trends Endocrinol. Metab. 1994;5:65–72. doi: 10.1016/1043-2760(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 49.Chen C.Y., Chung I.H., Tsai M.M., Tseng Y.H., Chi H.C., Tsai C.Y., Lin Y.H., Wang Y.C., Chen C.P., Wu T.I., et al. Thyroid hormone enhanced human hepatoma cell motility involves brain-specific serine protease 4 activation via ERK signaling. Mol. Cancer. 2014;13 doi: 10.1186/1476-4598-13-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin K.H., Chen C.Y., Chen S.L., Yen C.C., Huang Y.H., Shih C.H., Shen J.J., Yang R.C., Wang C.S. Regulation of fibronectin by thyroid hormone receptors. J. Mol. Endocrinol. 2004;33:445–458. doi: 10.1677/jme.1.01505. [DOI] [PubMed] [Google Scholar]
- 51.Lin K.H., Lee H.Y., Shih C.H., Yen C.C., Chen S.L., Yang R.C., Wang C.S. Plasma protein regulation by thyroid hormone. J. Endocrinol. 2003;179:367–377. doi: 10.1677/joe.0.1790367. [DOI] [PubMed] [Google Scholar]
- 52.Tai P.J., Huang Y.H., Shih C.H., Chen R.N., Chen C.D., Chen W.J., Wang C.S., Lin K.H. Direct regulation of androgen receptor-associated protein 70 by thyroid hormone and its receptors. Endocrinology. 2007;148:3485–3495. doi: 10.1210/en.2006-1239. [DOI] [PubMed] [Google Scholar]
- 53.Lin K.H., Shieh H.Y., Hsu H.C. Negative regulation of the antimetastatic gene Nm23-H1 by thyroid hormone receptors. Endocrinology. 2000;141:2540–2547. doi: 10.1210/endo.141.7.7570. [DOI] [PubMed] [Google Scholar]
- 54.Kwakkel J., Surovtseva O.V., de Vries E.M., Stap J., Fliers E., Boelen A. A novel role for the thyroid hormone-activating enzyme type 2 deiodinase in the inflammatory response of macrophages. Endocrinology. 2014;155:2725–2734. doi: 10.1210/en.2013-2066. [DOI] [PubMed] [Google Scholar]
- 55.Moore J.M., Guy R.K. Coregulator interactions with the thyroid hormone receptor. Mol. Cell. Proteomics. 2005;4:475–482. doi: 10.1074/mcp.R500001-MCP200. [DOI] [PubMed] [Google Scholar]
- 56.Flier J.S., Harris M., Hollenberg A.N. Leptin, nutrition, and the thyroid: The why, the wherefore, and the wiring. J. Clin. Investig. 2000;105:859–861. doi: 10.1172/JCI9725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Konner A.C., Bruning J.C. Toll-like receptors: Linking inflammation to metabolism. Trends Endocrinol. Metab. 2011;22:16–23. doi: 10.1016/j.tem.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 58.Fresno M., Alvarez R., Cuesta N. Toll-like receptors, inflammation, metabolism and obesity. Arch. Physiol. Biochem. 2011;117:151–164. doi: 10.3109/13813455.2011.562514. [DOI] [PubMed] [Google Scholar]
- 59.Duntas L.H., Biondi B. The interconnections between obesity, thyroid function, and autoimmunity: The multifold role of leptin. Thyroid. 2013;23:646–653. doi: 10.1089/thy.2011.0499. [DOI] [PubMed] [Google Scholar]
- 60.Haddow J.E., Palomaki G.E., Allan W.C., Williams J.R., Knight G.J., Gagnon J., O'Heir C.E., Mitchell M.L., Hermos R.J., Waisbren S.E., et al. Maternal thyroid deficiency during pregnancy and subsequent neuropsychological development of the child. N. Engl. J. Med. 1999;341:549–555. doi: 10.1056/NEJM199908193410801. [DOI] [PubMed] [Google Scholar]
- 61.Li Y., Shan Z., Teng W., Yu X., Fan C., Teng X., Guo R., Wang H., Li J., Chen Y., et al. Abnormalities of maternal thyroid function during pregnancy affect neuropsychological development of their children at 25–30 months. Clin. Endocrinol. 2010;72:825–829. doi: 10.1111/j.1365-2265.2009.03743.x. [DOI] [PubMed] [Google Scholar]
- 62.Costa A., Arisio R., Benedetto C., Bertino E., Fabris C., Giraudi G., Marozio L., Maula V., Pagliano M., Testori O., et al. Thyroid hormones in tissues from human embryos and fetuses. J. Endocrinol. Investig. 1991;14:559–568. doi: 10.1007/BF03346869. [DOI] [PubMed] [Google Scholar]
- 63.Chan S., Kachilele S., McCabe C.J., Tannahill L.A., Boelaert K., Gittoes N.J., Visser T.J., Franklyn J.A., Kilby M.D. Early expression of thyroid hormone deiodinases and receptors in human fetal cerebral cortex. Brain Res. Dev. Brain Res. 2002;138:109–116. doi: 10.1016/S0165-3806(02)00459-5. [DOI] [PubMed] [Google Scholar]
- 64.Chan S.Y., Martin-Santos A., Loubiere L.S., Gonzalez A.M., Stieger B., Logan A., McCabe C.J., Franklyn J.A., Kilby M.D. The expression of thyroid hormone transporters in the human fetal cerebral cortex during early development and in N-Tera-2 neurodifferentiation. J. Physiol. 2011;589:2827–2845. doi: 10.1113/jphysiol.2011.207290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fleming C.E., Mar F.M., Franquinho F., Saraiva M.J., Sousa M.M. Transthyretin internalization by sensory neurons is megalin mediated and necessary for its neuritogenic activity. J. Neurosci. 2009;29:3220–3322. doi: 10.1523/JNEUROSCI.6012-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.James S.R., Franklyn J.A., Kilby M.D. Placental transport of thyroid hormone. Best Pract. Res. Clin. Endocrinol. Metab. 2007;21:253–264. doi: 10.1016/j.beem.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 67.Vulsma T., Gons M.H., de Vijlder J.J. Maternal-fetal transfer of thyroxine in congenital hypothyroidism due to a total organification defect or thyroid agenesis. N. Engl. J. Med. 1989;321:13–16. doi: 10.1056/NEJM198907063210103. [DOI] [PubMed] [Google Scholar]
- 68.Landers K.A., McKinnon B.D., Li H., Subramaniam V.N., Mortimer R.H., Richard K. Carrier-mediated thyroid hormone transport into placenta by placental transthyretin. J. Clin. Endocrinol. Metab. 2009;94:2610–2616. doi: 10.1210/jc.2009-0048. [DOI] [PubMed] [Google Scholar]
- 69.Auso E., Lavado-Autric R., Cuevas E., del Rey F.E., Morreale De Escobar G., Berbel P. A moderate and transient deficiency of maternal thyroid function at the beginning of fetal neocorticogenesis alters neuronal migration. Endocrinology. 2004;145:4037–4047. doi: 10.1210/en.2004-0274. [DOI] [PubMed] [Google Scholar]
- 70.Oki N., Matsuo H., Nakago S., Murakoshi H., Laoag-Fernandez J.B., Maruo T. Effects of 3,5,3'-triiodothyronine on the invasive potential and the expression of integrins and matrix metalloproteinases in cultured early placental extravillous trophoblasts. J. Clin. Endocrinol. Metab. 2004;89:5213–5221. doi: 10.1210/jc.2004-0352. [DOI] [PubMed] [Google Scholar]
- 71.Barber K.J., Franklyn J.A., McCabe C.J., Khanim F.L., Bulmer J.N., Whitley G.S., Kilby M.D. The in vitro effects of triiodothyronine on epidermal growth factor-induced trophoblast function. J. Clin. Endocrinol. Metab. 2005;90:1655–1661. doi: 10.1210/jc.2004-0785. [DOI] [PubMed] [Google Scholar]
- 72.Larijani B., Marsoosi V., Aghakhani S., Moradi A., Hashemipour S. Thyroid hormone alteration in pre-eclamptic women. Gynecol. Endocrinol. 2004;18:97–100. doi: 10.1080/09513590310001652973. [DOI] [PubMed] [Google Scholar]
- 73.Belet N., Imdat H., Yanik F., Kucukoduk S. Thyroid function tests in preterm infants born to preeclamptic mothers with placental insufficiency. J. Pediatr. Endocrinol. Metab. 2003;16:1131–1135. doi: 10.1515/jpem.2003.16.8.1131. [DOI] [PubMed] [Google Scholar]
- 74.Kurlak L.O., Mistry H.D., Kaptein E., Visser T.J., Broughton Pipkin F. Thyroid hormones and their placental deiodination in normal and pre-eclamptic pregnancy. Placenta. 2013;34:395–400. doi: 10.1016/j.placenta.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 75.Iwasaki A., Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science. 2010;327:291–295. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Valimaki E., Miettinen J.J., Lietzen N., Matikainen S., Nyman T.A. Monosodium urate activates SRC/PYK2/PI3 kinase and cathepsin dependent unconventional protein secretion from human primary macrophages. Mol. Cell. Proteomics. 2013;12:749–763. doi: 10.1074/mcp.M112.024661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shi Y., Evans J.E., Rock K.L. Molecular identification of a danger signal that alerts the immune system to dying cells. Nature. 2003;425:516–521. doi: 10.1038/nature01991. [DOI] [PubMed] [Google Scholar]
- 78.Nicholson D.W. Caspase structure, proteolytic substrates, and function during apoptotic cell death. Cell Death Differ. 1999;6:1028–1042. doi: 10.1038/sj.cdd.4400598. [DOI] [PubMed] [Google Scholar]
- 79.Lamkanfi M., Declercq W., Kalai M., Saelens X., Vandenabeele P. Alice in caspase land. A phylogenetic analysis of caspases from worm to man. Cell Death Differ. 2002;9:358–361. doi: 10.1038/sj.cdd.4400989. [DOI] [PubMed] [Google Scholar]
- 80.Chen L.C., Wang L.J., Tsang N.M., Ojcius D.M., Chen C.C., Ouyang C.N., Hsueh C., Liang Y., Chang K.P., Chang Y.S. Tumour inflammasome-derived IL-1β recruits neutrophils and improves local recurrence-free survival in EBV-induced nasopharyngeal carcinoma. EMBO Mol. Med. 2012;4:1276–1293. doi: 10.1002/emmm.201201569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lamkanfi M., Kanneganti T.D., Van Damme P., Vanden Berghe T., Vanoverberghe I., Vandekerckhove J., Vandenabeele P., Gevaert K., Nunez G. Targeted peptidecentric proteomics reveals caspase-7 as a substrate of the caspase-1 inflammasomes. Mol. Cell. Proteomics. 2008;7:2350–2363. doi: 10.1074/mcp.M800132-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brasier A.R. The NF-κB regulatory network. Cardiovasc. Toxicol. 2006;6:111–130. doi: 10.1385/CT:6:2:111. [DOI] [PubMed] [Google Scholar]
- 83.Pop C., Salvesen G.S. Human caspases: Activation, specificity, and regulation. J. Biol. Chem. 2009;284:21777–21781. doi: 10.1074/jbc.R800084200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fuentes-Prior P., Salvesen G.S. The protein structures that shape caspase activity, specificity, activation and inhibition. Biochem. J. 2004;384:201–232. doi: 10.1042/BJ20041142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Petrilli V., Dostert C., Muruve D.A., Tschopp J. The inflammasome: A danger sensing complex triggering innate immunity. Curr. Opin. Immunol. 2007;19:615–622. doi: 10.1016/j.coi.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 86.Strowig T., Henao-Mejia J., Elinav E., Flavell R. Inflammasomes in health and disease. Nature. 2012;481:278–286. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 87.Kanneganti T.D., Ozoren N., Body-Malapel M., Amer A., Park J.H., Franchi L., Whitfield J., Barchet W., Colonna M., Vandenabeele P., et al. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 2006;440:233–236. doi: 10.1038/nature04517. [DOI] [PubMed] [Google Scholar]
- 88.Mariathasan S., Weiss D.S., Newton K., McBride J., O'Rourke K., Roose-Girma M., Lee W.P., Weinrauch Y., Monack D.M., Dixit V.M. Cryopyrin activates the inflammasome in response to toxins and ATP. Nature. 2006;440:228–232. doi: 10.1038/nature04515. [DOI] [PubMed] [Google Scholar]
- 89.Martinon F., Agostini L., Meylan E., Tschopp J. Identification of bacterial muramyl dipeptide as activator of the NALP3/cryopyrin inflammasome. Curr. Biol. 2004;14:1929–1934. doi: 10.1016/j.cub.2004.10.027. [DOI] [PubMed] [Google Scholar]
- 90.Zhou R., Yazdi A.S., Menu P., Tschopp J. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469:221–225. doi: 10.1038/nature09663. [DOI] [PubMed] [Google Scholar]
- 91.Mariathasan S., Monack D.M. Inflammasome adaptors and sensors: Intracellular regulators of infection and inflammation. Nat. Rev. Immunol. 2007;7:31–40. doi: 10.1038/nri1997. [DOI] [PubMed] [Google Scholar]
- 92.Agard N.J., Maltby D., Wells J.A. Inflammatory stimuli regulate caspase substrate profiles. Mol. Cell. Proteomics. 2010;9:880–893. doi: 10.1074/mcp.M900528-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Abrahams V.M. Pattern recognition at the maternal-fetal interface. Immunol. Investig. 2008;37:427–447. doi: 10.1080/08820130802191599. [DOI] [PubMed] [Google Scholar]
- 94.Costello M.J., Joyce S.K., Abrahams V.M. NOD protein expression and function in first trimester trophoblast cells. Am. J. Reprod. Immunol. 2007;57:67–80. doi: 10.1111/j.1600-0897.2006.00447.x. [DOI] [PubMed] [Google Scholar]
- 95.Mulla M.J., Yu A.G., Cardenas I., Guller S., Panda B., Abrahams V.M. Regulation of Nod1 and Nod2 in first trimester trophoblast cells. Am. J. Reprod. Immunol. 2009;61:294–302. doi: 10.1111/j.1600-0897.2009.00694.x. [DOI] [PubMed] [Google Scholar]
- 96.Abrahams V.M. The role of the Nod-like receptor family in trophoblast innate immune responses. J. Reprod. Immunol. 2011;88:112–117. doi: 10.1016/j.jri.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 97.Girardin S.E., Tournebize R., Mavris M., Page A.L., Li X., Stark G.R., Bertin J., DiStefano P.S., Yaniv M., Sansonetti P.J., et al. CARD4/NOD1 mediates NF-κB and JNK activation by invasive Shigella flexneri. EMBO Rep. 2001;2:736–742. doi: 10.1093/embo-reports/kve155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ogura Y., Inohara N., Benito A., Chen F.F., Yamaoka S., Nunez G. Nod2, a Nod1/Apaf-1 family member that is restricted to monocytes and activates NF-κB. J. Biol. Chem. 2001;276:4812–4818. doi: 10.1074/jbc.M008072200. [DOI] [PubMed] [Google Scholar]
- 99.Pettker C.M., Buhimschi I.A., Magloire L.K., Sfakianaki A.K., Hamar B.D., Buhimschi C.S. Value of placental microbial evaluation in diagnosing intra-amniotic infection. Obstet. Gynecol. 2007;109:739–749. doi: 10.1097/01.AOG.0000255663.47512.23. [DOI] [PubMed] [Google Scholar]
- 100.Jiang K., Akhmanova A. Microtubule tip-interacting proteins: A view from both ends. Curr. Opin. Cell Biol. 2011;23:94–101. doi: 10.1016/j.ceb.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 101.Wen Y., Eng C.H., Schmoranzer J., Cabrera-Poch N., Morris E.J., Chen M., Wallar B.J., Alberts A.S., Gundersen G.G. EB1 and APC bind to mDia to stabilize microtubules downstream of Rho and promote cell migration. Nat. Cell Biol. 2004;6:820–830. doi: 10.1038/ncb1160. [DOI] [PubMed] [Google Scholar]
- 102.Morrison E.E. The APC-EB1 interaction. Adv. Exp. Med. Biol. 2009;656:41–50. doi: 10.1007/978-1-4419-1145-2_4. [DOI] [PubMed] [Google Scholar]
- 103.Patel P.C., Fisher K.H., Yang E.C., Deane C.M., Harrison R.E. Proteomic analysis of microtubule-associated proteins during macrophage activation. Mol. Cell. Proteomics. 2009;8:2500–2514. doi: 10.1074/mcp.M900190-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dagenais M., Skeldon A., Saleh M. The inflammasome: In memory of Dr. Jurg Tschopp. Cell Death Differ. 2012;19:5–12. doi: 10.1038/cdd.2011.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Roberts J.M., Cooper D.W. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001;357:53–56. doi: 10.1016/S0140-6736(00)03577-7. [DOI] [PubMed] [Google Scholar]
- 106.Van’t Veer L.J., Dai H., van de Vijver M.J., He Y.D., Hart A.A., Mao M., Peterse H.L., van der Kooy K., Marton M.J., Witteveen A.T., et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. 2002;415:530–536. doi: 10.1038/415530a. [DOI] [PubMed] [Google Scholar]
- 107.Sibai B.M. Diagnosis and management of gestational hypertension and preeclampsia. Obstet. Gynecol. 2003;102:181–192. doi: 10.1016/S0029-7844(03)00475-7. [DOI] [PubMed] [Google Scholar]
- 108.Cox B., Sharma P., Evangelou A.I., Whiteley K., Ignatchenko V., Ignatchenko A., Baczyk D., Czikk M., Kingdom J., Rossant J., et al. Translational analysis of mouse and human placental protein and mRNA reveals distinct molecular pathologies in human preeclampsia. Mol. Cell. Proteomics. 2011;10 doi: 10.1074/mcp.M111.012526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Martin J.A., Osterman M.J., Sutton P.D. Recent data from the National Vital Statistics System. NCHS Data Brief; 2010. Are preterm births on the decline in the United States? pp. 1–8. [PubMed] [Google Scholar]
- 110.McGuire W., Clerihew L., Fowlie P.W. FInfection in the preterm infant. BMJ. 2004;329:1277–1280. doi: 10.1136/bmj.329.7477.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Stoll B.J., Hansen N., Fanaroff A.A., Wright L.L., Carlo W.A., Ehrenkranz R.A., Lemons J.A., Donovan E.F., Stark A.R., Tyson J.E., et al. Late-onset sepsis in very low birth weight neonates: The experience of the nichd neonatal research network. Pediatrics. 2002;110:285–291. doi: 10.1542/peds.110.2.285. [DOI] [PubMed] [Google Scholar]
- 112.Lamont R.F. The role of infection in preterm labour and birth. Hosp. Med. 2003;64:644–647. doi: 10.12968/hosp.2003.64.11.2343. [DOI] [PubMed] [Google Scholar]
- 113.Chan E.C., Fraser S., Yin S., Yeo G., Kwek K., Fairclough R.J., Smith R. Human myometrial genes are differentially expressed in labor: A suppression subtractive hybridization study. J. Clin. Endocrinol. Metab. 2002;87:2435–2441. doi: 10.1210/jcem.87.6.8439. [DOI] [PubMed] [Google Scholar]
- 114.Charpigny G., Leroy M.J., Breuiller-Fouche M., Tanfin Z., Mhaouty-Kodja S., Robin P., Leiber D., Cohen-Tannoudji J., Cabrol D., Barberis C., et al. A functional genomic study to identify differential gene expression in the preterm and term human myometrium. Biol. Reprod. 2003;68:2289–2296. doi: 10.1095/biolreprod.102.013763. [DOI] [PubMed] [Google Scholar]
- 115.Marvin K.W., Keelan J.A., Eykholt R.L., Sato T.A., Mitchell M.D. Use of cDNA arrays to generate differential expression profiles for inflammatory genes in human gestational membranes delivered at term and preterm. Mol. Hum. Reprod. 2002;8:399–408. doi: 10.1093/molehr/8.4.399. [DOI] [PubMed] [Google Scholar]
- 116.Bethin K.E., Nagai Y., Sladek R., Asada M., Sadovsky Y., Hudson T.J., Muglia L.J. Microarray analysis of uterine gene expression in mouse and human pregnancy. Mol. Endocrinol. 2003;17:1454–1469. doi: 10.1210/me.2003-0007. [DOI] [PubMed] [Google Scholar]
- 117.Young A., Thomson A.J., Ledingham M., Jordan F., Greer I.A., Norman J.E. Immunolocalization of proinflammatory cytokines in myometrium, cervix, and fetal membranes during human parturition at term. Biol. Reprod. 2002;66:445–449. doi: 10.1095/biolreprod66.2.445. [DOI] [PubMed] [Google Scholar]
- 118.Romero R., Yoon B.H., Kenney J.S., Gomez R., Allison A.C., Sehgal P.B. Amniotic fluid interleukin-6 determinations are of diagnostic and prognostic value in preterm labor. Am. J. Reprod. Immunol. 1993;30:167–183. doi: 10.1111/j.1600-0897.1993.tb00618.x. [DOI] [PubMed] [Google Scholar]
- 119.Maymon E., Ghezzi F., Edwin S.S., Mazor M., Yoon B.H., Gomez R., Romero R. The tumor necrosis factor α and its soluble receptor profile in term and preterm parturition. Am. J. Obstet. Gynecol. 1999;181:1142–1148. doi: 10.1016/S0002-9378(99)70097-9. [DOI] [PubMed] [Google Scholar]
- 120.Osman I., Young A., Ledingham M.A., Thomson A.J., Jordan F., Greer I.A., Norman J.E. Leukocyte density and pro-inflammatory cytokine expression in human fetal membranes, decidua, cervix and myometrium before and during labour at term. Mol. Hum. Reprod. 2003;9:41–45. doi: 10.1093/molehr/gag001. [DOI] [PubMed] [Google Scholar]
- 121.Keelan J.A., Marvin K.W., Sato T.A., Coleman M., McCowan L.M., Mitchell M.D. Cytokine abundance in placental tissues: Evidence of inflammatory activation in gestational membranes with term and preterm parturition. Am. J. Obstet. Gynecol. 1999;181:1530–1536. doi: 10.1016/S0002-9378(99)70400-X. [DOI] [PubMed] [Google Scholar]
- 122.Hayden M.S., Ghosh S. Signaling to NF-κB. Genes Dev. 2004;18:2195–2224. doi: 10.1101/gad.1228704. [DOI] [PubMed] [Google Scholar]
- 123.Schmitz M.L., Mattioli I., Buss H., Kracht M. NF-κB: A multifaceted transcription factor regulated at several levels. Chembiochem. 2004;5:1348–1358. doi: 10.1002/cbic.200400144. [DOI] [PubMed] [Google Scholar]
- 124.Lindstrom T.M., Bennett P.R. The role of nuclear factor kappa B in human labour. Reproduction. 2005;130:569–581. doi: 10.1530/rep.1.00197. [DOI] [PubMed] [Google Scholar]
- 125.Stjernholm-Vladic Y., Stygar D., Mansson C., Masironi B., Akerberg S., Wang H., Ekman-Ordeberg G., Sahlin L. Factors involved in the inflammatory events of cervical ripening in humans. Reprod. Biol. Endocrinol. 2004;2 doi: 10.1186/1477-7827-2-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lee Y., Allport V., Sykes A., Lindstrom T., Slater D., Bennett P. The effects of labour and of interleukin 1 β upon the expression of nuclear factor kappa B related proteins in human amnion. Mol. Hum. Reprod. 2003;9:213–218. doi: 10.1093/molehr/gag026. [DOI] [PubMed] [Google Scholar]
- 127.Allport V.C., Pieber D., Slater D.M., Newton R., White J.O., Bennett P.R. Human labour is associated with nuclear factor-κB activity which mediates cyclo-oxygenase-2 expression and is involved with the “functional progesterone withdrawal”. Mol. Hum. Reprod. 2001;7:581–586. doi: 10.1093/molehr/7.6.581. [DOI] [PubMed] [Google Scholar]
- 128.Baltimore R.S. Neonatal sepsis: Epidemiology and management. Paediatr. Drugs. 2003;5:723–740. doi: 10.2165/00148581-200305110-00002. [DOI] [PubMed] [Google Scholar]
- 129.Malik A., Hui C.P., Pennie R.A., Kirpalani H. Beyond the complete blood cell count and C-reactive protein: A systematic review of modern diagnostic tests for neonatal sepsis. Arch. Pediatr. Adolesc. Med. 2003;157:511–516. doi: 10.1001/archpedi.157.6.511. [DOI] [PubMed] [Google Scholar]
- 130.Underwood M.A., Gilbert W.M., Sherman M.P. Amniotic fluid: Not just fetal urine anymore. J. Perinatol. 2005;25:341–348. doi: 10.1038/sj.jp.7211290. [DOI] [PubMed] [Google Scholar]
- 131.Sinha R.A., Singh B.K., Yen P.M. Thyroid hormone regulation of hepatic lipid and carbohydrate metabolism. Trends Endocrinol. Metab. 2014;10:538–545. doi: 10.1016/j.tem.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 132.Tseng Y.H., Ke P.Y., Liao C.J., Wu S.M., Chi H.C., Tsai C.Y., Chen C.Y., Lin Y.H., Lin K.H. Chromosome 19 open reading frame 80 is upregulated by thyroid hormone and modulates autophagy and lipid metabolism. Autophagy. 2014;10:20–31. doi: 10.4161/auto.26126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chen C.P., Chen Y.Y., Huang J.P., Wu Y.H. The effect of conditioned medium derived from human placental multipotent mesenchymal stromal cells on neutrophils: Possible implications for placental infection. Mol. Hum. Reprod. 2014;20:1117–1125. doi: 10.1093/molehr/gau062. [DOI] [PubMed] [Google Scholar]
- 134.Polin R.A. The “ins and outs” of neonatal sepsis. J. Pediatr. 2003;143:3–4. doi: 10.1016/S0022-3476(03)00271-3. [DOI] [PubMed] [Google Scholar]
- 135.Kavathas P.B., Boeras C.M., Mulla M.J., Abrahams V.M. Nod1, but not the ASC inflammasome, contributes to induction of IL-1β secretion in human trophoblasts after sensing of Chlamydia trachomatis. Mucosal Immunol. 2013;6:235–243. doi: 10.1038/mi.2012.63. [DOI] [PMC free article] [PubMed] [Google Scholar]