SUMMARY
We present a new surgical technique for the treatment of snoring and mild obstructive sleep apnoea syndrome. This is a modification of anterior palatoplasty, and its main features are the use of self-locking (barbed) threads and the possibility of stabilise the palatal suture by fixing it to anatomical bone and fibrous structures. The technique is described in detail and some preliminary results are presented.
KEY WORDS: Snoring, Pharyngoplasty, Palatoplasty, Snoring surgery
RIASSUNTO
Viene presentata una nuova tecnica per il trattamento chirurgico del russamento delle forme di OSAS lieve. Si tratta di una modifica della classica palatoplastica anteriore, caratterizzata dall'impiego di fili autobloccanti e dalla possibilità di stabilizzare la sutura palatale ancorandola a strutture anatomiche osteo-fibrose vicine. Tale tecnica viene dettagliatamente descritta e vengono forniti alcuni risultati preliminari.
Introduction
It is well known that the noise of snoring is generated mainly at the level of soft palate and surrounding structures; therefore, surgical treatment of snoring has been based on procedures that aimed to shorten/reduce soft palate or to stiffen the soft palate itself to decrease vibrancy 1-3. Taking into account surgical proposals of several authors, we developed a new pharyngoplasty technique to reduce snoring and prevent obstruction in mild obstructive sleep apnoea syndrome (OSAS). Its main indication, according to our protocol, is represented by a anteroposterior pattern of palatal vibration/ obstruction.
In 2007, Pang and Woodson 4 presented the expansion sphincter pharyngoplasty (ESP), a new method of treating sleep respiratory obstruction due to palatal collapse; this technique requires dissection of the lower edge of palatopharyngeal muscle and its attachment to " the arching fibers of the soft palate anteriorly... through the muscle bulk itself " on both pharyngeal sides. ESP, which can be associated with tonsillectomy when needed, proved to be effective in OSAS treatment and is now widely performed.
In 2009, Pang et al. 5 published the results of anterior palatoplasty 6, a modified CA PSO 7 technique that was used for treatment of 77 patients with mild or moderate OSAS. Their results showed the effectiveness of this procedure considering both obstruction and snoring.
Lately, in 2012 Mantovani et al. 8 designed the "Roman Blinds" technique, a non-resective surgical procedure that shortens and stiffens the soft palate by means of threads anchored to fibro-osseous attachments: the posterior nasal spine and both the pterygoid hamuli. Later, they considered the possibility of utilising self-locking threads to perform this type of uvulo-palatal lifting 9.
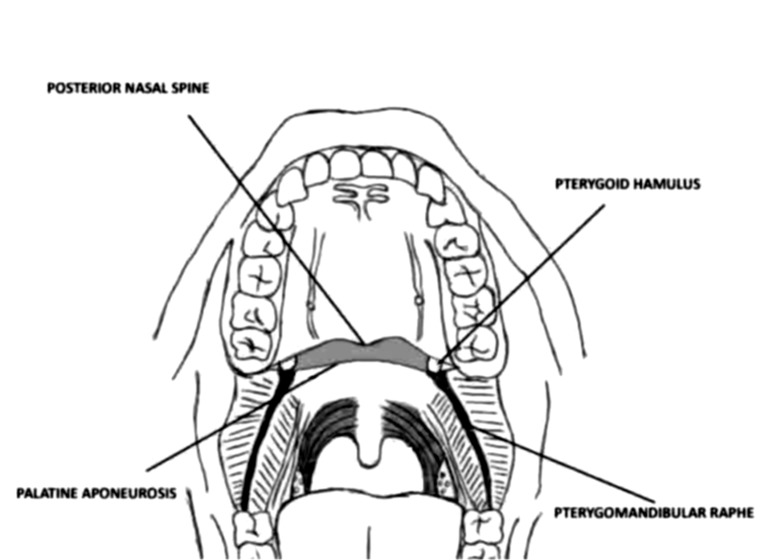
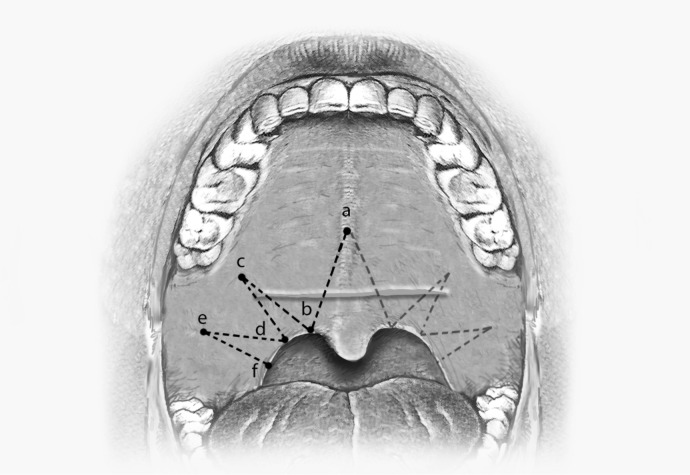
Our method allows stabilisation of the palatal suture (after removing the mucosal flap), and anchoring it to fixed points such as pterygoid hamuli, palatal aponeurosis and both pterygo-mandibular raphes (Fig. 1) employing barbed self-locking threads with no need for knots: this can be considered an evolution of anterior palatoplasty that can be referred to as barbed anterior pharyngoplasty (BAPh).
Fig. 1.
The landmarks of barbed anterior pharyngoplasty.
Materials and methods
Subjects
We performed our technique on a group of 24 selected subjects presenting heavy snoring or with a mild OSAS syndrome (AHI < 15); mean AHI = 7.2, range from 0.7 to 14. The group was composed of 17 men and 7 women, with mean age of 46 (range from 34 to 55) and an average BMI of 28.6 (from 24.3 to 30.1).
We recruited, in this first stage, only patients with tonsil grade 0 and 1, or who had formerly been subjected to tonsillectomy.
All subjects had requested surgical treatment because the intense noise during the night represented an important discomfort for their bed partners. Each patient underwent sleep endoscopy (preliminarily or in the same session of surgery) to confirm the actual site and pattern of vibration and obstruction 10 11.
Hardware
Surgical instruments used for our procedure are the same used in classical Pang anterior palatoplasty: i.e. McIvor mouth gag, electrocautery, bipolar cautery forceps, needle holder and scissors.
The specific device for this procedure is the barbed thread, which allows to suture the different muscular and mucosal planes and to suspend the suture itself to the support points without tying knots. Barbed threads allow better maintenance of the suture itself since the tension is distributed along the entire length of the wire, and not only in correspondence of knots as in normal sutures. Among the available types of barbed threads we chose the QUILL® knotless tissue closure device, Angiotech Pharmaceutical Inc., Vancouver, Canada, because it is provided with two needles. We used the 0 polydioxanone absorbable (in six months) thread in the 24 × 24 ½ cm configuration, with two 36.5 mm circle needles (Fig. 2). This is a 48 cm thread, with a barb direction transition point in the middle; the two halves of the thread, with an opposite direction of barbs, can be used to perform the different layer of palatal suture.
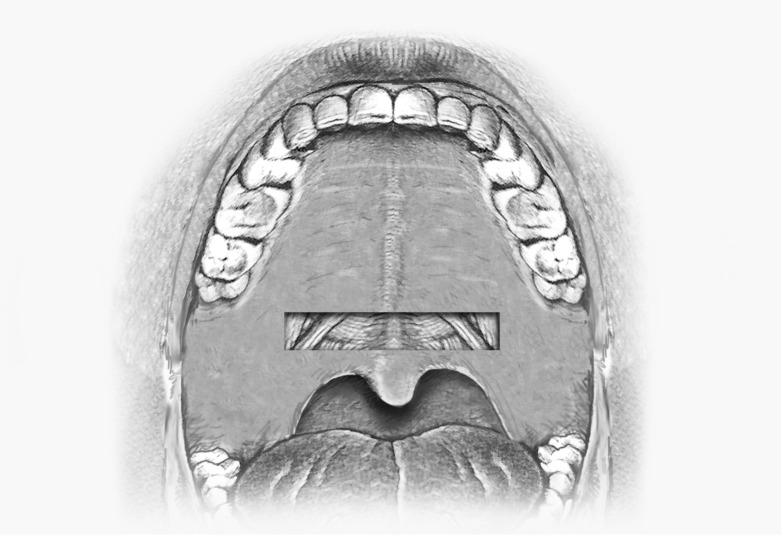
Fig. 2.
The area of mucosal removal.
Anaesthesia
Surgery was conducted under general anaesthesia with oral-tracheal intubation; the surgeon sits at the head of the patient without magnification of the surgical field.
Surgical technique
The first step in our procedure is to mark reference points with a dermographic pen: the end point of osseous palate on the midline (the posterior nasal spine), the relief of pterygoid hamulus and pterygomandibular raphe of both sides.
Then, as in Pang's anterior palatoplasty, the mucosal palatal flap is dissected and removed: this flap consists of a rectangular portion of palatal mucosa whose upper corners are located close to the hamuli, a few mm below their reliefs; the excision area extends for 10-12 mm (depending on soft palate length) in the central part of the soft palate between the edge of osseous palate and the uvula attachment (Fig. 2). When removing the mucosal strip, it is quite important to remove the submucosal layer at the same time, containing many minor salivary glands, in order to expose the naked muscular surface. Haemostasis is performed using bipolar cautery forceps.
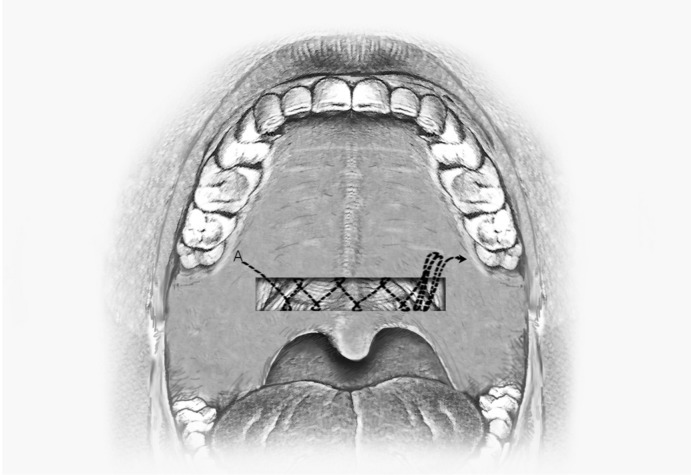
1st Layer: muscular suture (Fig. 3): with one of the two needles we enter into the soft palate in correspondence of right pterygoid hamulus and exit at the level of the lower right angle of the area where the mucosal flap was removed (A); the thread must be pulled out completely until the transition point blocks the progression of the thread itself; starting from here, we tighten the underlying muscles (levator palati, palatoglossal and/or palatopharyngeal muscles) with a 8 shaped intra muscular continuous suture. When this step is completed (5 or 6 passes are requested), it is stitched 2 or 3 times, and once more in the muscular plane, connecting the left edge of the wound to the left hamulus, in order to achieve a firm fixing point. The thread is then cut at the mucosal level.
Fig. 3.
The intramuscular suture.
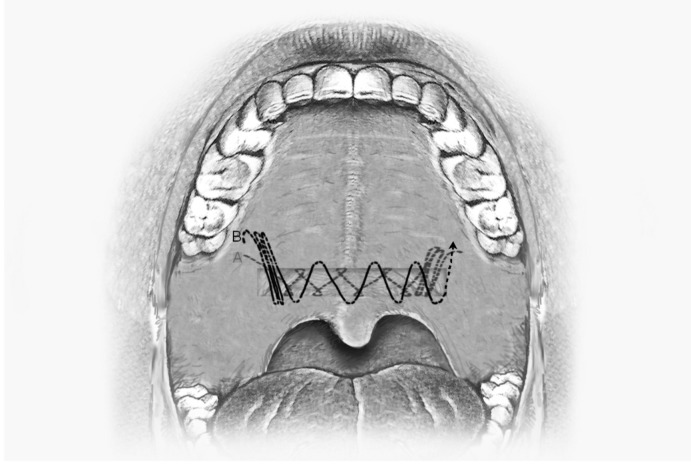
2nd Layer: sub mucosal plane (Fig. 4): The needle of the other segment of the thread that starts from the barbs transition point is used to connect, with 3 or 4 sub mucosal stitches, the right hamulus to the right edge of the wound (B); a submucosal continuous suture is then performed connecting the lower edge of the wound to the palatine aponeurosis and emerging at the level of the left hamulus. The thread is cut again at the exit point. At this time, the distance between horizontal edges of the wound is reduced to about 1.5-2 mm and both the extremities of the suture are well anchored to pterygoid hamuli.
Fig. 4.
The submucosal suture.
The Roman Blind Technique (Fig. 5): in order to further stabilise the soft palate and to juxtapose the edges of the wound, we lastly perform, using another double barbed wire, the Roman Blind Technique as proposed by Mantovani et al.: i.e. intra muscular stitches connecting on both sides the posterior nasal spine (a), the edge of soft palate (b), the hamulus region (c), the posterior pillar (d), the mandibular raphe (e) and back to the posterior pillar (f).
Fig. 5.
The final Roman Blind technique suture.
At the end of the procedure, the soft palate is shortened and pulled forward; the distance between the soft palate and the posterior pharyngeal wall is increased; the wound is closed in the near absence of visible threads.
Results
Preliminary results, based on bed partners' opinions, confirmed that all patients obtained a consistent reduction of snoring and even disappearance of noise in some cases, once the uvular oedema was resolved and palatal fibrosis was established. The mean score in the Snoring Visual Analogic Scale was reduced from 9.2 to 2.9. In mild OSAS patients, which were a minority (7/24), the mean AHI changed from 8.9 to 3.8.
All patients were discharged on the first day after the procedure: antibiotic and analgesic therapy was prescribed; when uvular oedema was present, we prescribed corticosteroid therapy for 5 days. Some dietetic restrictions were applied, as during the course of posttonsillectomy.
Postoperative pain, in the patients' opinions, was mild to moderate for the first 5-6 days, then slowly decreased; after two weeks pain had usually disappeared.
In many cases (19/24), the extremity of the thread was partially extruded for a short segment, due to the natural retraction of the tissue; in these patients, it was necessary to cut the protruding piece of the wire.
We did not observe any velar insufficiency or dehiscence of the wound. After 4 to 6 weeks, a fibrous scar was observed in correspondence of the palatal wound, with a consequent increase in velar stiffness.
Discussion
The innovations we added to Pang's anterior palatoplasty permit, in our opinion, good stability of the suture, producing a better development of palatal fibrosis that provides an effective final stiffness. This effect is further supported by the needful use of barbed self-blocking threads, thanks to their property of spreading the tension along the entire length of the wire. The practical execution of the surgical procedure is, moreover, made easier because knots are not required: this is a considerable advantage in a small field such as the oral cavity.
In our experience, postoperative discomfort is not significantly different from that observed in anterior palatoplasty, when considering both postoperative pain and recovery time.
Conclusions
We believe that barbed anterior pharyngoplasty is an effective surgical procedure for the treatment of snoring and mild OSAS; the indication is represented by the anteroposterior pattern of palatal vibration/obstruction. It ensures valid palatal stiffness with a good shortening of the velum without significant tissue removal. Furthermore, the technique prevents disjunction of the margins of the palatal wound that we sometimes observed in classical anterior palatoplasty.
References
- 1.Fusetti M, Fioretti AB, Valenti M, et al. Cardiovascular and metabolic comorbidities in patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol Ital. 2012;32:320–325. [PMC free article] [PubMed] [Google Scholar]
- 2.Passali D, Caruso G, Arigliano LC, et al. Database application for patients with obstructive sleep apnoea syndrome. Acta Otorhinolaryngol Ital. 2012;32:252–255. [PMC free article] [PubMed] [Google Scholar]
- 3.Passali D, Tatti P, Toraldo M, et al. OSAS and metabolic diseases: Round Table, 99(th) SIO National Congress, Bari 2012. Acta Otorhinolaryngol Ital. 2014;34:158–166. [PMC free article] [PubMed] [Google Scholar]
- 4.Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: A new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137:110–114. doi: 10.1016/j.otohns.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Pang KP, Raymond T, Puraviappan P, et al. Anterior palatoplasty for the treatment of OSAS: Three-year results. Otolaryngol Head Neck Surg. 2009;141:253–256. doi: 10.1016/j.otohns.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 6.Pang KP, Terris DJ. Modified cautery-assisted palatal stiffening operation: new method for treating snoring and mild obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;136:823–826. doi: 10.1016/j.otohns.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 7.Mair EA, Day RH. Cautery-assisted palatal stiffening operation. Otolaryngol Head Neck Surg. 2000;122:547–556. doi: 10.1067/mhn.2000.106475. [DOI] [PubMed] [Google Scholar]
- 8.Mantovani M, Minetti A, Torretta S, et al. The velo-uvulopharyngeal lift or "roman blinds" tecnique for the treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital. 2012;32:48–53. [PMC free article] [PubMed] [Google Scholar]
- 9.Mantovani M, Minetti A, Torrettta S, et al. The "Barbed Roman Blinds" technique: a step forward – letter to the editor. Acta Otorhinolaryngol Ital. 2013;33:128–128. [PMC free article] [PubMed] [Google Scholar]
- 10.Salamanca F, Costantini F, Bianchi A, et al. Identification of obstructive sites and patterns in obstructive sleep apnoea syndrome by sleep endoscopy in 614 patients. Acta Otorhinolaryngol Ital. 2013;33:261–266. [PMC free article] [PubMed] [Google Scholar]
- 11.Corso E, Fiorita A, Rizzotto G, et al. The role of druginduced sleep endoscopy in the diagnosis and management of obstructive sleep apnoea syndrome: our personal experience. Acta Otorhinolaryngol Ital. 2013;33:405–413. [PMC free article] [PubMed] [Google Scholar]