SUMMARY
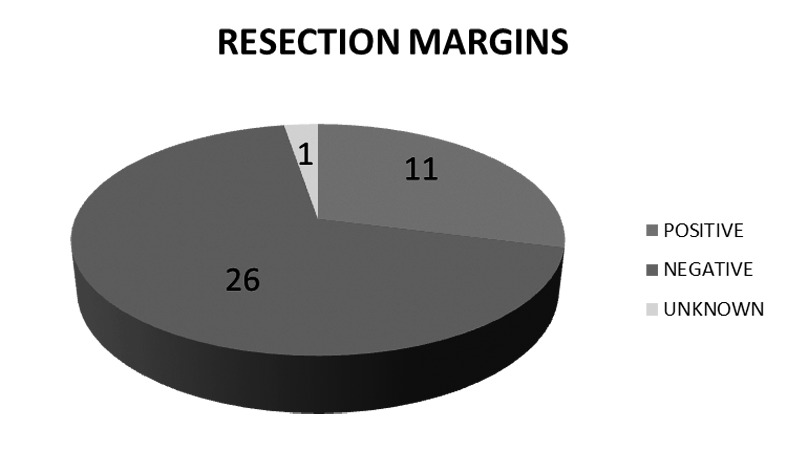
Organ preservation treatment for advanced head and neck squamous cell carcinoma is associated with poor outcomes due to locoregional recurrences. Salvage surgery is the main therapeutic option for some of these patients. The aim of this study was to analyse the results of salvage surgery for advanced pharyngolaryngeal squamous cell carcinoma previously treated with radiochemotherapy. We performed a retrospective study on 38 patients (36 men, 2 women). The median age at diagnosis was 60 years with a mean follow-up period of 49.8 months. Recurrences were diagnosed at a mean of 395 days after finalising organ preservation treatment. Patients went under different salvage surgeries, including 22 total laryngectomies, 6 partial laryngectomies (3 transoral laser surgeries and 3 opened surgeries), 8 functional neck dissections and 2 tongue base surgeries. Nineteen patients had no postoperative complications after a mean hospital stay of 2 weeks. However, 5 patients died of significant recurrent bleedings. There were 4 salivary fistulas that responded to conservative management, while 7 patients had important pharyngostomas that required reconstruction with either regional or free flaps. The mean hospital stay was of 61.60 days for all patients. Five-year overall survival from diagnosis, overall survival after salvage surgery and survival after salvage surgery were 44.20, 37.90 and 45.70%, respectively. In summary, we conclude that salvage surgery is an optimal treatment for pharyngolaryngeal and regional recurrences and provides improvement in locoregional control and survival, despite the severe complications.
KEY WORDS: Salvage surgery, Pharyngocutaneous fistula, Organ preservation, Total laryngectomy
RIASSUNTO
Il trattamento con protocollo di preservazione d'organo per i carcinomi squamocellulari avanzati del distretto testa-collo è associato a una bassa sopravvivenza a causa delle recidive locoregionali. Per alcuni di questi pazienti la chirurgia di salvataggio è la principale opzione terapeutica. L'obiettivo di questo studio è stato quello di analizzare i risultati della chirurgia di salvataggio per i carcinomi faringolaringei a cellule squamose trattati in precedenza con radio-chemioterapia. Abbiamo effettuato uno studio retrospettivo su 38 pazienti (36 uomini, 2 donne). L'età mediana alla diagnosi è stata di 60 anni, con un periodo di follow-up medio di 49,8 mesi. Le recidive sono state diagnosticate dopo una media di 395 giorni dal trattamento con preservazione d'organo. I pazienti sono stati sottoposti a diversi tipi di chirurgia di salvataggio, fra i quali 22 laringectomie totali, 6 laringectomie parziali (3 con chirurgia laser transorale e 3 con chirurgia open), 8 svuotamenti laterocervicali funzionali e 2 interventi sulla base della lingua. Dopo una permanenza media in ospedale di 2 settimane, 19 pazienti non hanno avuto complicanze postoperatorie. Tuttavia 5 pazienti sono deceduti per importanti sanguinamenti nel postoperatorio, 4 hanno presentato fistole salivari che hanno risposto positivamente ad una gestione conservativa, mentre 7 pazienti hanno avuto delle importanti fistole faringee che hanno richiesto ricostruzioni con lembi regionali o liberi. La permanenza media in ospedale è stata di 61,60 giorni. L'overall survival a 5 anni dalla diagnosi, l'overall survival dopo chirurgia di salvataggio e il disease specific survival dopo chirurgia di salvataggio sono stati rispettivamente del 44,2, 37,9 e 45,7%. Possiamo concludere che la chirurgia di salvataggio risulta un trattamento ottimale per le recidive faringolaringee e regionali e determina un miglioramento nel controllo regionale e nella sopravvivenza, nonostante le gravi complicanze associate.
Introduction
In 2012, 299,264 new cases of pharyngolaryngeal cancers were diagnosed worldwide with an estimated 179,466 deaths 1. Squamous cell carcinomas are the most frequent neoplasms of the head and neck, and 60% are in an advanced stage (stage III-IV) at initial diagnosis 2 3. Treatment of advanced pharyngolaryngeal squamous cell carcinomas has undergone substantial changes in the last two decades. Concurrent chemoradiotherapy (CCRT) has become the standard of care for nonsurgical organ preservation after two landmark trials, the VA study in 1991 4 and RTOG 91-11 in 2003 5. For patients with unresectable disease, the current standard of treatment is concurrent cisplatin- based chemoradiation. This is also the standard for patients with resectable disease when nonsurgical organ preservation is desired and, as adjuvant treatment, for patients with high-risk pathological findings at surgical resection. Lefebvre et al. reported the 10-year results of the EORTC trial 24,891 which compared a larynx-preserving approach to immediate surgery in hypopharynx and lateral epilarynx squamous cell carcinoma. Their results did not compromise disease control or survival (which remained poor) and allowed more than half of survivors to retain their larynx 6. Despite such an approach, the majority of patients develop local and/or regional recurrences, and distant metastases occur in 20-30% of patients 3. Depending on the site, recurrence rates range from 25 to 50% and patients with advanced-stage disease may expect only a 30 to 60% cure rate 7. Hoffman et al. attribute the decrease in survival in patients with laryngeal cancer during the past 2 decades in the United States to the increase in nonsurgical treatment 8. Kerry Olsen critically analysed the studies of the VA and RTOG, concluding that their results cannot be easily transferred to a normal population of patients that does not conform to the selection markers in a study setting 9. According to American statistics, the global survival for laryngeal cancer has significantly decreased from 66 to 63% in the last years 10. However, a significant increase in the global survival rates for cancer of the oral cavity and pharynx has been described, up to 65%, compared to 54% in prior decades. In addition, the European statistics for pharyngolaryngeal cancers have not shown such a decrease in survival of these patients. In fact, an important improvement in survival has been described in the latest statistics 11 12. The favourable trends in cancer mortality can be largely attributed to changes in exposure to specific environmental and lifestyle risk factors. Alcohol and tobacco consumption has been steadily declining over the last decades in southern Europe, with a consequent favourable impact on oral, pharyngeal, esophageal and laryngeal cancers 13 14.
Human papillomavirus (HPV) has an important role in the pathogenesis and prognosis of oropharyngeal cancers. HPV-associated oropharyngeal squamous cell carcinoma has been shown to be more responsive to therapy and to have a better outcome than HPV-negative tumours. HPV has also been detected to varying degrees in hypopharynx and laryngeal cancers 15. Nonetheless, no differences in outcome have been seen in patients with HPV-positive nonoropharyngeal primary cancers 16 17.
Over the past decades, the role of the head and neck surgeon in the treatment of advanced pharyngolaryngeal cancer has completely changed. Surgery has lost ground as the first therapy in this setting, and it is increasingly reserved as salvage treatment in cases of recurrent disease after chemoradiation therapy 18, and it may also be indicated for surgical functional rehabilitation or palliation 19. Many authors have advocated surgical salvage as the primary option for recurrent pharyngolaryngeal tumours. For patients with resectable recurrence and adequate performance status, surgery offers the best chance of achieving locoregional control and prolonged survival 20. However, salvage surgery is accompanied with significantly more complications, both local and general, compared with primary surgery 21, and significantly affects morbidity, hospitalisation and costs of treatment 22. The aim of this study was to analyse the results of salvage surgery for recurrence of advanced pharyngolaryngeal squamous cell carcinoma previously treated with radiochemotherapy in our department.
Materials and methods
We performed a restrospective study on 103 patients with advanced pharyngolaryngeal squamous cell carcinoma (hypopharyngeal or laryngeal, Stage III/IV) treated with CCRT at our institution between 1997 and 2010. Patients who suffered from distant metastasis (Stage IVc) or with an unresectable local tumour (T4b) were excluded. 86 patients were treated with CCRT, which consisted of an association of cycles of cisplatin and 5-fluorouracil with a continuous course of external radiotherapy until a final dose of 70 Gy. Induction chemotherapy was used in 9 patients. Eight patients were not eligible for chemotherapy due to low performance status, and were treated with radiotherapy alone. During follow-up, 60 patients (58.3%) suffered a locoregional recurrence. Salvage surgery was offered to 41 of these patients, and was rejected by 3 patients. Moreover, 19 patients were not eligible for surgical treatment. Therefore, 22 patients received palliative care for recurrent disease.
We analysed the results of the 38 patients who underwent salvage surgery, including epidemiology, surgical complications, prognosis and survival.
Results
The study included 38 patients (36 men, 2 women). The median age at diagnosis was 60 years with a mean follow- up of 49.8 months. Recurrences were diagnosed at a mean of 395 days after finaliaing organ preservation treatment. Table I shows the clinical characteristics of patients at initial diagnosis. Table II indicates the characteristics of recurrences and salvage surgery. Patients went under different salvage surgeries, including 22 total laryngectomies, 6 partial laryngectomies (3 transoral laser surgeries and 3 open surgeries), 8 functional neck dissections and 2 tongue base surgeries. Eight patients with local recurrence required a functional neck dissection to complete the salvage surgical treatment. All patients had partial defects of the pharynx. We performed 5 reconstructions of pharynx with regional flaps (pectoralis mayor myocutaneal flap) at the time of surgery. The remaining 20 patients going under open surgeries had direct closure of the pharynx. Thirteen patients did not undergo resection of the pharynx. Ten patients required second salvage surgeries for persistence of locoregional disease.
Table I.
Clinical characteristics of patients at initial diagnosis.
| Variables | N | % |
|---|---|---|
| Tumour site | ||
| Supraglottis | 29 | 76.31% |
| Glottis | 3 | 7.89% |
| Hypopharynx | 6 | 15.78% |
| Initial T | ||
| T1-2 | 2 | 5.26% |
| T3 | 24 | 63.15% |
| T4 | 9 | 23.68% |
| Unknown | 3 | 7.89% |
| Initial N | ||
| N0 | 15 | 39.47% |
| N1 | 5 | 13.15% |
| N2 | 13 | 34.21% |
| N3 | 2 | 5.26% |
| Unknown | 3 | 7.89% |
| Initial stage | ||
| Stage III | 14 | 36.84% |
| Stage IV | 21 | 55.26% |
| Unknown | 3 | 7.89% |
Table II.
Characteristics of recurrences and salvage surgery.
| Variables | N | % |
|---|---|---|
| Type of recurrence | ||
| Local | 22 | 57.89% |
| Regional | 8 | 21.05% |
| Locoregional | 8 | 21.05% |
| Salvage surgery | ||
| Total laryngectomy | 22 | 57.89% |
| Partial opened laryngectomy | 3 | 7.89% |
| Partial transoral laser laryngectomy | 3 | 7.89% |
| Base of the tongue resection | 2 | 5.26% |
| Functional neck dissection | 8 | 21.05% |
Surgical complications
19 patients had no postoperative complications, with a mean hospital stay of 2 weeks. However, 5 patients died of significant recurrent bleedings. There were 4 salivary fistulas that responded to conservative management, while 7 patients had important pharyngostomas that required reconstruction with pedicled flaps. Three of these patients underwent reconstruction with pectoralis major flap at salvage surgery.
Prognosis and survival
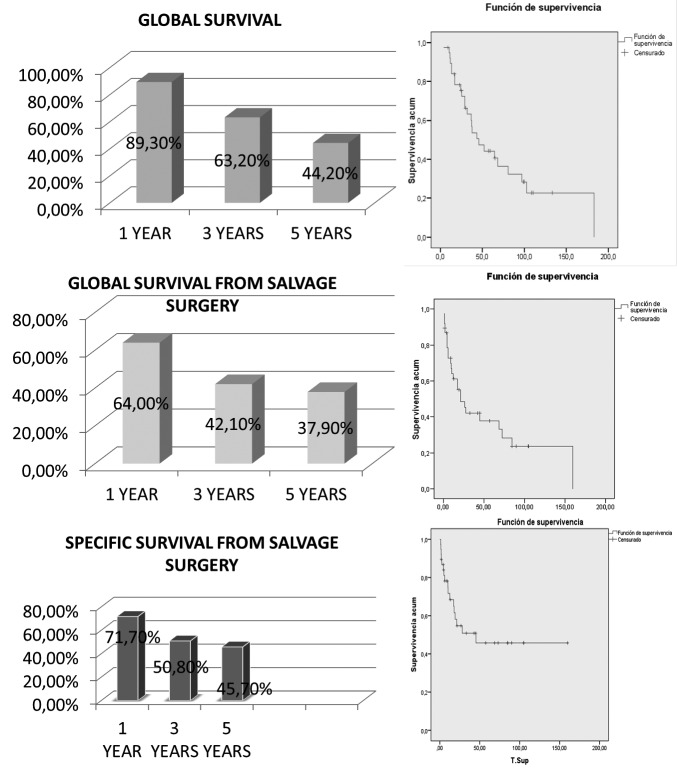
The mean hospital stay was 61.60 days for all patients. Overall, 5 year disease-free period was 31.57%. Total laryngectomy was performed in 65.78% of patients, and 47.36% were treated for regional recurrences. Two of the three partial surgeries required total laryngectomy due to second recurrences, and the third was rescued with partial laser surgery. None of the partial laser surgeries required other surgical treatments. Resection margins were not significantly associated with prognosis (Fig. 1). Fiveyear overall survival from diagnosis, overall survival after salvage surgery and survival after salvage surgery were 44.20, 37.90 and 45.70%, respectively (Fig. 2).
Fig. 1.
Resection margins.
Fig. 2.
Overall survival from diagnosis, overall survival after salvage surgery and survival after salvage surgery.
Discussion
Advanced pharyngolaryngeal cancers are often treated by a combination of radiochemotherapy for an organ preservation approach. It may also be indicated in those patients whose tumour is unresectable or inoperable. However, 30% of patients suffer from locoregional recurrence 8. First of all, we would like to point out the fact that after failure of CCRT, a high proportion of patients are not considered candidates for salvage treatment. In our series of cases, a third of patients suffering from recurrences were not eligible for salvage surgery. In the paper by Esteller et al., 54% of patients did not have salvage surgery and died as a consequence of disease progression after a median of 3.5 months 18. Kowalski et al. published a study on 797 patients with recurrent HNSCC who chose supportive care rather than salvage treatment, and reported a median survival of 3.8 months 23. These results were substantially confirmed by another study in which the estimated 5-year survival rate of patients suitable for salvage surgery was 55.8%, which was much higher than those who were unsuitable for salvage surgery (17.4%, p < 0.001) 24. A short disease-free interval (DFI) has been shown to have significant negative prognostic impact 25. A review of 68 consecutive patients, primarily treated by irradiation or endoscopic surgery, and surgically salvaged by total laryngectomy or supracricoid partial laryngectomy, showed significantly poorer prognosis for recurrences occurring in the first 10 months after primary treatment 26. In our study, there were 20 patients with recurrences within 10 months following chemoradiotherapy, and 18 of these were rescued after this period. During a 5-year follow-up after salvage treatment, 11 patients in the first group died and 9 patients in the second group died, with no significant difference between groups. This may be explained by the fact that our study included only advanced primary tumours treated with organ preservation therapies, while the study mentioned above took into account both early and advanced tumours, as well as those primarily treated by surgery.
When patients have initially undergone radiation (with or without chemotherapy), then surgery is considered the primary salvage modality when complete resection with negative margins is considered possible. Total laryngectomy remains the gold-standard salvage procedure against which all other surgical techniques are judged 26. Laryngeal recurrence, in particular, appears to have distinctly favourable survival outcomes relative to other sites 21, and as such, salvage total laryngectomy continues to be an effective means of disease control, with recent studies reporting 5-year overall survival rates of 68 to 70% 27. Nevertheless, prognosis is poor when a recurrence or new primary head and neck cancer develops in an area previously treated with radiation 28. 1621 consecutive patients with neoplasms of the larynx were observed at the Sun Yat-sen University Cancer Center. After a median follow- up of 49.5 months (range, 7-176 months), recurrent disease was diagnosed in 253 patients (16.3%). Survival after recurrence was significantly influenced by variables related to both primary and recurrent tumour: age, smoking index, grade, primary site, initial T stage, initial UICC stage and nodal status of the primary tumour, as well as the DFI, extent and location of the recurrence and suitability for surgery were powerful prognostic factors for survival 24 29. The stage of the recurrent tumour appears to be of substantial importance in predicting prognosis. A prospective study by Goodwin on 109 patients identified a prominent difference in 2-year disease-free survival (DFS) based on recurrent stage (67% for rStage II vs. 33% for rStage III and 22% for rStage IV), underscoring the difficulty of successful treatment of advanced disease 7. In our retrospective study, we did not analyse this aspect due to the lack of information.
In some cases of small recurrent tumours, laryngeal conservation surgery with or without postoperative radiation therapy may be considered. Such partial laryngeal procedures are performed with transoral laser microsurgery or open partial laryngectomy. They may give a second chance for organ preservation in a significant proportion of patients 30. However, open partial laryngectomy for salvage after failed radiotherapy is more frequently associated with postoperative complications, with reported complication rates of 20 to 28% and with fistula rates of 8 to 14% 31. In fact, we performed only three partial open surgeries, and all required total laryngectomy due to postoperative complications and second recurrences. Nevertheless, we had good results from transoral laser surgeries (TOL), despite our modest experience with laser for salvage surgeries. Grant et al. evaluated TOL microsurgery in a cohort of patients with recurrent disease (supraglottic and glottis) and reported a locoregional control rate of 88% at 2 years. Furthermore, Steiner et al. reported local control in 74% of patients with glottic recurrences undergoing TOL microsurgery 32 33. While the complications associated with TOL microsurgery in the primary setting are relatively rare, the risks associated with this procedure in the recurrent setting have yet to be determined. The greatest concern after extensive salvage TOL procedures following prior radiation is the ability of the larynx to heal by secondary intention 26.
Neck recurrences may signal the greater likelihood of distant metastases and consequently poorer prognosis 34. Wong et al. compared regional recurrence versus local recurrence, showing that patients with regional recurrence had a higher likelihood of successful disease control at the time of surgery (42% vs. 29%), but lower 5-year disease free survival (26% vs. 42%) 35. 16 of our patients required a neck dissection at the moment of salvage surgery; only a third survived after 5 years. Regarding elective neck dissection, most studies have reported that neck dissection does not provide any advantage in patients who develop recurrent laryngeal cancer without clinical evidence of nodal metastases after radiation 36-38.
There is limited information about hospital stay and the costs of salvage surgeries. The median hospital stay in our study was 61.60 days. However, the median hospital stay for patients without complications was much lower (19 days, range 13-30 days) than for those with surgical complications (37 days, range 14-74 days). The study of Esteller et al. 18 found a significant difference in hospital stay in relation to the appearance of surgical complications (p = 0.001) in patients who had surgery on the primary tumour. Our most frequent complication of salvage surgery after chemoradiation was pharyngocutaneous fistula, consistent with earlier studies 25 26 39. According to other investigations, patients undergoing total laryngectomy after radiation therapy have a significantly increased risk of fistualae of approximately 30%; the risk is highest in patients who undergo concurrent chemoradiation 40. Ganly et al. 42 described that initial treatment with CCRT was the only significant predictor of local complications on multivariate analysis. Moreover, it appears that the severity of fistula increases in patients who underwent preoperative radiotherapy vs. those who did not 43. Another factor is extent of surgery 18 41 44. Extensive resections and reconstructions were performed after chemoradiation due to a larger extent of the tumour, resulting in more compromised healing and susceptibility to infections. The most likely explanation for this is related to the nutritional and immune status of patients. These patients have poor nutritional and immune status in the initial months and it may take several months to return to normality 18. Schwartz et al. 22 reported that a history of weight loss 6 months before surgery, preoperative hypoalbuminaemia and anaemia were independent predictors of wound complications after laryngectomy. Some groups refer that the morbidity of CCRT may be limited by the use of prophylactic gastrostomy tubes as reported by Lee et al. and Barbaro et al. 46 47. We usually use nasogastric tubes in our patients rather than gastrostomies. In all likelihood, we could improve our results if gastrostomies were used more frequently and earlier.
As mentioned above, pharyngocutaneous fistula remains a troublesome complication following salvage laryngectomy. Both length of hospital stay and time until oral diet initiation are markedly prolonged for these patients. The recent study of Patel et al. showed that the use of either a pectoralis myofascial onlay flap or a fasciocutaneous free flap interposed into the pharyngeal defect resulted in a decreased incidence of fistula formation. These patients might also suffer from pharyngocutaneous fistulas, but the healing period is shorter 41. Simon et al. performed a retrospective study on 21 patients treated previously with chemo/radiotherapy, and concluded that surgical interventions for salvage, palliation, or functional improvement can be safely performed once vascularised grafts are used 48. However, studies on the incidence of major peri-and postoperative complications after procedures use vascularised tissue transfer still show highly variable rates that range between 10 and 66% (for doubly irradiated patients). There is still debate whether or not flaps help to decrease the incidence of such fistulas 7 19 49. There is no doubt that pedicled flaps represent the standard choice for salvage surgery after primary chemoradiation protocols due to poor general conditions, advanced stage of disease and low life expectancy 50. Moreover, microvascular anastomosis is less favourable in an anatomical site previously subjected to surgery or radiation therapy 51. Deganello et al. reported that the use of alternative nonmicrovascular techniques in high-risk patients is functionally and oncologically sound, and can even lead to cost savings 52. This is particularly important in elderly patients and in those affected by severe medical comorbidities in which the extended surgical time and stress of free flap reconstruction are contraindicated 53. In our series, we performed 5 salvage surgeries with pectoralis major myocutaneal flaps, and 7 of our patients suffering from a pharyngostoma required a pedicled flap for closure. Nowadays, we always associate a pectoralis major flap in all salvage surgeries after any type of previous treatment with radiotherapy in order to prevent fistula complication.
Our study shows a 5-year overall survival from diagnosis and overall survival after salvage surgery of 44.20 and 37.90% respectively, which are similar to other studies 6 54. It is interesting that the specific survival after salvage surgery (45.70%) is higher than overall survival. This might be explained by the fact that these patients usually suffer from other concomitant diseases which may compromise survival. We found no significant difference regarding resection margins for salvage surgery. A British study of 352 patients with recurrent head and neck squamous cell carcinoma who underwent salvage surgery found no significance difference in 5-year survival between patients with positive margins and those with negative margins 55. As explained by those authors, a negative resection margin does not guarantee residual tumour is not present within unresected tissue. Although margins are always carefully studied, they form a three-dimensional structure and hence it is possible that tumour cells may be missed by the pathologist as a result of sampling errors during preparation of specimens. Recurrent disease, moreover, differs from primary malignancy in that it is typically infiltrative and multifocal, and spreads broadly in microscopic deposits that may be outside the initial radiated or operative field 56. These small foci are undetectable on imaging or clinical exam, but can lead to treatment failures or geographic radiotherapy misses. However, there are some studies in which resections margins did have a significant impact on survival 19 30.
The most important limitation of our study is that it is retrospective. The major criticism of retrospective studies is that the data collected were not originally designed for a research application. Therefore, some factors responsible for the treatment outcomes might be omitted in the analysis, thereby contributing to bias 24. We encourage further prospective studies to validate the available data from this and previous investigations.
Conclusions
Despite the severe complications of salvage surgery, it remains the best option to treat recurrences of advanced head and neck squamous cell carcinoma after organ preservation protocols. Pharyngocutaneous fistula remains the main complication after surgery, but the use of either locoregional or free flaps seems to reduce its frequency and severity. The final decision for treatment of pharyngolaryngeal recurrences depends on the experience acquired by the medical group in charge of each case. Therefore, further studies are required to define standard protocols to provide the best option treatment. New modalities of treatment such as intensity-modulated radiation therapy may be included to improve the results of salvage surgery.
References
- 1. http://globocan.iarc.fr. (Accesed january 2014).
- 2.Encinas Vicente A, Souvirón Encabo R, Rodríguez Paramás A, et al. [Surgical complications in salvage surgery of patients with head and neck carcinomas treated with concomitant chemoradiotherapy (CCR)]. Acta Otorrinolaringol Esp. 2007;58:454–457. [PubMed] [Google Scholar]
- 3.Vermorken JB, Specenier P. Optimal treatment for recurrent/ metastatic head and neck cancer. Ann Oncol. 2010;21(Suppl 7):vii252–vii261. doi: 10.1093/annonc/mdq453. [DOI] [PubMed] [Google Scholar]
- 4. The Department of Veterans Affairs Laryngeal Cancer Study Group , author. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med. 1991;324:1685–1690. doi: 10.1056/NEJM199106133242402. [DOI] [PubMed] [Google Scholar]
- 5.Forastiere AA, Goepfert H, Maor M, et al. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349:2091–2098. doi: 10.1056/NEJMoa031317. [DOI] [PubMed] [Google Scholar]
- 6.Lefebvre JL, Andry G, Chevalier D, et al. EORTC Head and Neck Cancer Group, author. Laryngeal preservation with induction chemotherapy for hypopharyngeal squamous cell carcinoma: 10-year results of EORTC trial 24891. Ann Oncol. 2012;23:2708–2714. doi: 10.1093/annonc/mds065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin WJ., Jr Salvage surgery for patients with recurrent squamous cell carcinoma of the upper aerodigestive tract: when do the ends justify the means? Laryngoscope. 2000;110(3 Pt 2 Suppl 93):1–18. doi: 10.1097/00005537-200003001-00001. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman HT, Porter K, Karnell LH, Cooper JS, et al. Laryngeal cancer in the United States: changes in demographics, patterns of care, and survival. Laryngoscope. 2006;116(9 Pt 2 Suppl 111):1–13. doi: 10.1097/01.mlg.0000236095.97947.26. [DOI] [PubMed] [Google Scholar]
- 9.Olsen KD. Reexamining the treatment of advanced laryngeal cancer. Head Neck. 2010;32:1–7. doi: 10.1002/hed.21294. [DOI] [PubMed] [Google Scholar]
- 10.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 11.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- 12.Bray F, Ren JS, Masuyer E, et al. Global estimates of cancer prevalence for. 27 sites in the adult population in 2008. Int J Cancer. 2013;132:1133–1145. doi: 10.1002/ijc.27711. [DOI] [PubMed] [Google Scholar]
- 13.Bosetti C, Bertuccio P, Malvezzi M, et al. Cancer mortality in Europe, 2005-2009, and an overview of trends since 1980. Ann Oncol. 2013;24:2657–2671. doi: 10.1093/annonc/mdt301. [DOI] [PubMed] [Google Scholar]
- 14.Bosetti C, Bertuccio P, Levi F, et al. Cancer mortality in the European Union, 1970-2003, with a joinpoint analysis. Ann Oncol. 2008;19:631–640. doi: 10.1093/annonc/mdm597. [DOI] [PubMed] [Google Scholar]
- 15.Zandberg DP, Bhargava R, Badin S, et al. The role of human papillomavirus in nongenital cancers. CA Cancer J Clin. 2013;63:57–81. doi: 10.3322/caac.21167. [DOI] [PubMed] [Google Scholar]
- 16.Duray A, Descamps G, Arafa M, et al. High incidence of high-risk HPV in benign and malignant lesions of the larynx. Int J Oncol. 2011;39:51–59. doi: 10.3892/ijo.2011.1031. [DOI] [PubMed] [Google Scholar]
- 17.Ragin CC, Taioli E. Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: review and meta-analysis. Int J Cancer. 2007;121:1813–1820. doi: 10.1002/ijc.22851. Review. [DOI] [PubMed] [Google Scholar]
- 18.Esteller E, Vega MC, López M, et al. Salvage surgery after locoregional failure in head and neck carcinoma patients treated with chemoradiotherapy. Eur Arch Otorhinolaryngol. 2011;268:295–301. doi: 10.1007/s00405-010-1365-1. [DOI] [PubMed] [Google Scholar]
- 19.Simon C, Bulut C, Fedenspil PA, et al. Assessment of periand postoperative complications and Karnofsky-performance status in head and neck cancer patients after radiation or chemoradiation that underwent surgery with regional or free-flap reconstruction for salvage, palliation, or to improve function. Radiat Oncol. 2011;6:109–109. doi: 10.1186/1748-717X-6-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ho AS, Kraus DH, Ganly I, et al. Decision making in the management of recurrent head and neck cancer. Head Neck. 2014;36:144–151. doi: 10.1002/hed.23227. [DOI] [PubMed] [Google Scholar]
- 21.Stanković M, Milisavljević D, Stojanov D, et al. Influential factors, complications and survival rate of primary and salvage total laryngectomy for advanced laryngeal cancer. Coll Antropol. 2012;36(Suppl 2):7–12. [PubMed] [Google Scholar]
- 22.Schwartz SR, Yueh B, Maynard C, et al. Predictors of wound complications after laryngectomy: a study of over 2000 patients. Otolaryngol Head Neck Surg. 2004;131:61–68. doi: 10.1016/j.otohns.2003.08.028. [DOI] [PubMed] [Google Scholar]
- 23.Kowalski LP, Carvalho AL. Natural history of untreated head and neck cancer. Eur J Cancer. 2000;36:1032–1037. doi: 10.1016/s0959-8049(00)00054-x. [DOI] [PubMed] [Google Scholar]
- 24.Jin T, Lin H, Lin HX, et al. Treatment and prognosis of patients with recurrent laryngeal carcinoma: a retrospective study. Head Neck Oncol. 2013;5:10–10. [Google Scholar]
- 25.Liao CT, Chang JT, Wang HM, et al. Salvage therapy in relapsed squamous cell carcinoma of the oral cavity: how and when? Cancer. 2008;112:94–103. doi: 10.1002/cncr.23142. [DOI] [PubMed] [Google Scholar]
- 26.Cohen M.A., Nassif R., Goldstein DP, et al. Recurrent Laryngeal Cancer. In: Hishman M., Mehonna K., Kian A, editors. Head and neck cancer recurrence: evidence-based, multidisciplinary management. Ed. Thieme; 2012. [Google Scholar]
- 27.Holsinger FC, Funk E, Roberts DB, et al. Conservation laryngeal surgery versus total laryngectomy for radiation failure in laryngeal cancer. Head Neck. 2006;28:779–784. doi: 10.1002/hed.20415. [DOI] [PubMed] [Google Scholar]
- 28.Tanvetyanon T, Padhya T, McCaffrey J, et al. Prognostic factors for survival after salvage reirradiation of head and neck cancer. J Clin. 2009;27:1983–1991. doi: 10.1200/JCO.2008.20.0691. [DOI] [PubMed] [Google Scholar]
- 29.Tan HK, Giger R, Auperin A, et al. Salvage surgery after concomitant chemoradiation in head and neck squamous cell carcinomas-stratification for postsalvage survival. Head Neck. 2010;32:139–147. doi: 10.1002/hed.21159. [DOI] [PubMed] [Google Scholar]
- 30.Vincentiis M, Virgilio A, Bussu F, et al. Oncologic results of the surgical salvage of recurrent laryngeal squamous cell carcinoma in a multicentric retrospective series: emerging role of supracricoid partial laryngectomy. Head Neck. 2015;37:84–91. doi: 10.1002/hed.23563. [DOI] [PubMed] [Google Scholar]
- 31.Ganly I, Patel SG, Matsuo J, et al. Analysis of postoperative complications of open partial laryngectomy. Head Neck. 2009;31:338–345. doi: 10.1002/hed.20975. [DOI] [PubMed] [Google Scholar]
- 32.Grant DG, Salassa JR, Hinni ML, et al. Transoral laser microsurgery for recurrent laryngeal and pharyngeal cancer. Otolaryngol Head Neck Surg. 2008;138:606–613. doi: 10.1016/j.otohns.2007.12.046. [DOI] [PubMed] [Google Scholar]
- 33.Steiner W, Vogt P, Ambrosch P, et al. Transoral carbon dioxide laser microsurgery for recurrent glottic carcinoma after radiotherapy. Head Neck. 2004;26:477–484. doi: 10.1002/hed.20009. [DOI] [PubMed] [Google Scholar]
- 34.Deschamps DR, Spencer HJ, Kokoska MS, et al. Implications of head and neck cancer treatment failure in the neck. Otolaryngol Head Neck Surg. 2010;142:722–727. doi: 10.1016/j.otohns.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 35.Wong LY, Wei WI, Lam LK, et al. Salvage of recurrent head and neck squamous cell carcinoma after primary curative surgery. Head Neck. 2003;25:953–959. doi: 10.1002/hed.10310. [DOI] [PubMed] [Google Scholar]
- 36.Hilly O, Stern S, Horowitz E, et al. Is there a role for elective neck dissection with salvage laryngectomy? A decisionanalysis model. Laryngoscope. 2013;123:2706–2711. doi: 10.1002/lary.24138. [DOI] [PubMed] [Google Scholar]
- 37.Basheeth N, O'Leary G, Sheahan P. Elective neck dissection for no neck during salvage total laryngectomy: findings, complications, and oncological outcome. JAMA Otolaryngol Head Neck Surg. 2013;139:790–796. doi: 10.1001/jamaoto.2013.3995. [DOI] [PubMed] [Google Scholar]
- 38.Yao M, Roebuck JC, Holsinger FC, et al. Elective neck dissection during salvage laryngectomy. Am J Otolaryngol. 2005;26:388–392. doi: 10.1016/j.amjoto.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Spencer SA, Harris J, Wheeler RH, et al. Final report of RTOG 9610, a multi-institutional trial of reirradiation and chemotherapy for unresectable recurrent squamous cell carcinoma of the head and neck. Head Neck. 2008;30:281–288. doi: 10.1002/hed.20697. [DOI] [PubMed] [Google Scholar]
- 40.Weber RS, Berkey BA, Forastiere A, et al. Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91-11. Arch Otolaryngol Head Neck Surg. 2003;129:44–49. doi: 10.1001/archotol.129.1.44. [DOI] [PubMed] [Google Scholar]
- 41.Sewnaik A, Keereweer S, Al-Mamgani A, et al. High complication risk of salvage surgery after chemoradiation failures. Acta Otolaryngol. 2012;132:96–100. doi: 10.3109/00016489.2011.617779. [DOI] [PubMed] [Google Scholar]
- 42.Ganly I, Patel S, Matsuo J, et al. Postoperative complications of salvage total laryngectomy. Cancer. 2005;103:2073–2081. doi: 10.1002/cncr.20974. [DOI] [PubMed] [Google Scholar]
- 43.Paydarfar JA, Birkmeyer NJ. Complications in head and neck surgery: a meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch Otolaryngol Head Neck Surg. 2006;132:67–72. doi: 10.1001/archotol.132.1.67. [DOI] [PubMed] [Google Scholar]
- 44.Leon X, Quer M, Orus C, López M, et al. Results of salvage surgery for local or regional recurrence after larynx preservation with induction chemotherapy and radiotherapy. Head Neck. 2001;23:733–738. doi: 10.1002/hed.1104. [DOI] [PubMed] [Google Scholar]
- 45.Sassler AM, Esclamado RM, Wolf GT. Surgery after organ preservation therapy: analysis of wound complications. Arch Otolaryngol Head Neck Surg. 1995;121:162–165. doi: 10.1001/archotol.1995.01890020024006. [DOI] [PubMed] [Google Scholar]
- 46.Lee JH, Machtay M, Unger LD, et al. Prophylactic gastrostomy tubes in patient undergoing intensive irradiation for cancer of the head and neck. Arch Otolaryngol Head Neck Surg. 1998;124:871–875. doi: 10.1001/archotol.124.8.871. [DOI] [PubMed] [Google Scholar]
- 47.Barbaro M, Rispoli G, Diaferia F, et al. [Salvage surgery for advanced head and neck cancer]. G Chir. 2008;29:74–78. [PubMed] [Google Scholar]
- 48.Withrow KP, Rosenthal EL, Gourin CG, et al. Free tissue transfer to manage salvage laryngectomy defects after organ preservation failure. Laryngoscope. 2007;117:781–784. doi: 10.1097/MLG.0b013e3180332e39. [DOI] [PubMed] [Google Scholar]
- 49.Colletti G, Autelitano L, Tewfik K, et al. Autonomized flaps in secondary head and neck reconstructions. Acta Otorhinolaryngol Ital. 2012;32:329–335. [PMC free article] [PubMed] [Google Scholar]
- 50.Putten L, Spasiano R, Bree R, et al. Flap reconstruction of the hypopharynx: a defect orientated approach. Acta Otorhinolaryngol Ital. 2012;32:288–296. [PMC free article] [PubMed] [Google Scholar]
- 51.Mura F, Bertino G, Occhini A, et al. Surgical treatment of hypopharyngeal cancer: a review of the literature and proposal for a decisional flow-chart. Acta Otorhinolaryngol Ital. 2013;33:299–306. [PMC free article] [PubMed] [Google Scholar]
- 52.Deganello A, Gitti G, Parrinello G, et al. Cost analysis in oral cavity and oropharyngeal reconstructions with microvascular and pedicled flaps. Acta Otorhinolaryngol Ital. 2013;33:380–387. [PMC free article] [PubMed] [Google Scholar]
- 53.Montemari G, Rocco A, Galla S, et al. Hypopharynx reconstruction with pectoralis major myofascial flap: our experience in 45 cases. Acta Otorhinolaryngol Ital. 2012;32:93–97. [PMC free article] [PubMed] [Google Scholar]
- 54.Gleich LL, Ryzenman J, Gluckman JL, et al. Recurrent advanced (T3 or T4) head and neck squamous cell carcinoma: is salvage possible? Arch Otolaryngol Head Neck Surg. 2004;130:35–38. doi: 10.1001/archotol.130.1.35. [DOI] [PubMed] [Google Scholar]
- 55.Jones AS, Bin Hanafi Z, Nadapalan V. Do positive resection margins after ablative surgery for head and neck cancer adversely affect prognosis? A study of 352 patients with recurrent carcinoma following radiotherapy treated by salvage surgery. Br J Cancer. 1996;74:128–132. doi: 10.1038/bjc.1996.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zbären P, Nuyens M, Curschmann J, et al. Histologic characteristics and tumour spread of recurrent glottic carcinoma: analysis on whole-organ sections and comparison with tumour spread of primary glottic carcinomas. Head Neck. 2007;29:26–32. doi: 10.1002/hed.20502. 48-54. [DOI] [PubMed] [Google Scholar]