Abstract
Purpose
Extremely elderly patients who present with complicated gallstone disease are less likely to undergo definitive treatment. The use of laparoscopic cholecystectomy (LC) in older patients is complicated by comorbid conditions that are concomitant with advanced age and may increase postoperative complications and the frequency of conversion to open surgery. We aimed to evaluate the results of LC in patients (older than 80 years).
Methods
We retrospectively analyzed 302 patients who underwent LC for acute cholecystitis between January 2011 and December 2013. Total patients were divided into three groups: group 1 patients were younger than 65 years, group 2 patients were between 65 and 79 years, and group 3 patients were older than 80 years. Patient characteristics were compared between the different groups.
Results
The conversion rate was significantly higher in group 3 compared to that in the other groups. Hematoma in gallbladder fossa and intraoperative bleeding were higher in group 3, the difference was not significant. Wound infection was not different between the three groups. Operating time and postoperative hospital stay were significantly higher in group 3 compared to those in the other groups. There was no reported bile leakage and operative mortality. Preoperative percutaneous transhepatic gallbladder drainage and endoscopic retrograde cholangiopancreatography were performed more frequently in group 3 than in the other groups.
Conclusion
LC is safe and feasible. It should be the gold-standard approach for extremely elderly patients with acute cholecystitis.
Keywords: Laparoscopic cholecystectomy, 80 and over aged, Treatment outcome
INTRODUCTION
Gallstone disease is the most common global indication for abdominal surgery. The prevalence of gallstones increases with age in both sexes and in nearly all populations; in older individuals the prevalence ranges from 20% to 30% and increases to 80% for institutionalized patients older than 90 years [1,2,3]. Since the introduction of laparoscopic cholecystectomy (LC) nearly two decades ago, and the more recent use of it as an outpatient procedure, many surgeons now view cholecystectomy as a relatively simple procedure from which patients recover quickly [4]. Cholecystectomy for symptomatic gallstone disease is more common in elderly patients as the incidence of gallstones increases with age [5]. Also, advanced age with its concomitant comorbid conditions may be associated with increased postoperative LC complications [6]. Few studies have demonstrated the advantages of LC for the geriatric population, and most have only investigated LC in patients older than 65 years, while very few have investigated LC in patients, older than 80 years [7,8].
As global life expectancy continues to increase, the proportion of patients over 80 years who are undergoing LC is increasing; therefore, we aimed to evaluate their clinical outcomes.
METHODS
A retrospective study was conducted in 302 patients who had undergone LC for acute cholecystitis (AC) in a single institution and performed by one surgeon between January 2011 and December 2013. The study population included 147 females (48.7%) and 155 males (51.4%), with a median age of 58 years (range, 19-96 years). Patients were classified into three groups according to their age. Group 1 included 176 patients (58.3%) younger than 65 years (91 males and 85 females), with a median age of 46 years (range, 19-64 years). Group 2 included 91 patients (30.1%) aged 65 to 79 years (46 males and 45 females), with a median age of 70 years (range, 63-77 years). Group 3 included 35 patients (11.6%) older than 80 years (18 males and 17 females), with a median age of 83 years (range, 80-96 years). Exclusions from the study included patients with gallbladder polyps, adenomyomatosis, and gallbladder cancer.
Age group was the primary independent variable of interest. Clinical covariates included percutaneous transhepatic gallbladder drainage (PTGBD) and endoscopic retrograde cholangiopancreatography (ERCP). Outcomes of interest were preoperative laboratory values, severity grade of AC, indication for surgery, American Society of Anesthesiologists (ASA) score, operating time, conversion to open surgery, complications, mortality, and postoperative hospital stay (from operation to discharge). Severity grade of AC was determined by new diagnostic criteria and severity assessment of AC in revised tokyo guidelines [9]. Grade III (severe) AC is associated with dysfunction of any one of the following organs/systems; (1) cardiovascular dysfunction - hypotension requiring treatment with dopamine ≥5 mcg/kg per minute, or any dose of norepinephrine, (2) neurological dysfunction - decreased level of consciousness, (3) respiratory dysfunction - PaO2/FiO2 ratio <300, (4) renal dysfunction - oliguria, creatinine >2.0 mg/dL, (5) hepatic dysfunction PTinternational normalized ratio (INR) >1.5, (6) hematological dysfunction - platelet count <100,000/mm3. Grade II (moderate) AC is associated with any one of the following conditions; (1) elevated WBC count ( >18,000/mm3), (2) palpable tender mass in the right upper abdominal quadrant, (3) duration of complaints >72 hours, (4) marked local inflammation (gangrenous cholecystitis, pericholecystic abscess, hepatic abscess, biliary peritonitis, emphysematous cholecystitis). Grade I (mild) AC does not meet the criteria of "grade III" or "grade II" AC. Complications included common bile duct (CBD) injury, bile leakage, hematoma in gallbladder fossa, intraoperative bleeding, and wound infection. Hematoma in gallbladder fossa is defined as hematoma formation in a depression lodging the gallbladder on the undersurface of the liver anteriorly, between the quadrate and the right lobes. It could be detected by enhanced computed tomography. Intraoperative bleeding is defined as bleeding from cystic artery and liver that can't stop the bleeding by laparoscopic procedure. Operative time and ASA score were obtained from anesthesia records (Table 1).
Table 1. Demographics of extremely elderly compare with nonelderly patients.
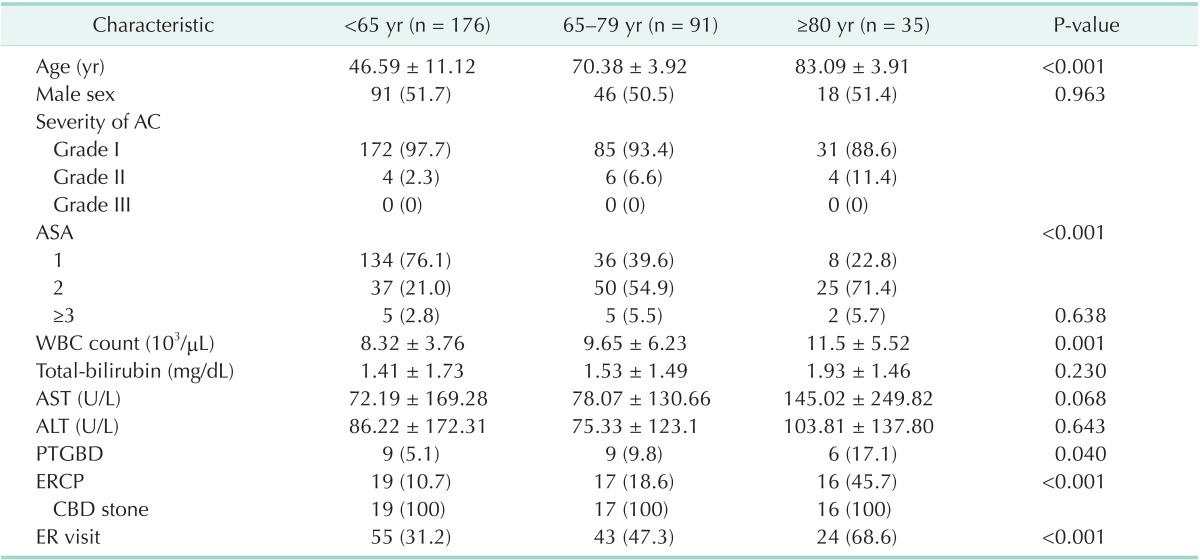
Values are presented as mean ± standard deviation or number (%).
AC, acute cholecystitis; ASA, American Society of Anesthesiologists; PTGBD, percutaneous transhepatic gallbladder drainage; CBD, common bile duct; ERCP, endoscopic retrograde cholangiopancreatography; ER, emergency room.
Surgical procedure
Pneumoperitoneum was established using Hasson technique. The abdomen was insufflated with carbon dioxide gas with a preset pressures of 12 mmHg. The patient was moved to the reverse Trendelenburg position with the left side down. We used the single surgeon technique three port LC using thirty degree operating telescopes with an 11-mm infraumbilical port, a 5-mm subxyphoid, and a 5-mm subcostal ports were used. There were no cases where the single surgeon needed for additional ports. The cystic duct and cystic artery were clipped using a 5-mm multiple clip application all patients. The resected specimen was inserted into a protective endo-bag and was retrieved through the umbilical port site.
Statistical analysis
Statistical analysis of the data was performed using the IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Quantitative variables were expressed as medians and ranges, and qualitative variables were expressed as frequencies and percentages. The chi-square test was used to evaluate any potential association between three categorical variables. One way analysis of variance was used to assess differences continuous variable between the three groups of patients. Statistical significance was considered for P-values less than 0.05.
RESULTS
The demographic characteristics of the study patients are shown in Table 1. No difference in sex distribution was seen between the groups. Most of underlying disease in group 3 were diabetes mellitus, hypertension, cerebrovascular attack history, and pulmonary disease. Patient's physical status is more important than underlying disease. So, we used ASA score that is a system for assessing the fitness of cases before surgery. ASA score was compared by chi-square. There was a significant differences in each group (P < 0.001). The percentage of the high-risk patients (defined as an ASA score ≥ 3) was not significantly different between the groups (P = 0.638).
Preoperative results
The severity grade of AC was significantly higher in group 3 compared to that in the other groups (P = 0.036). The preoperative laboratory results included WBC counts, and values for serum AST, ALT, and serum total bilirubin. The WBC count was significantly higher group 3 compared to that in the other groups (P = 0.001). Although total bilirubin, AST, and ALT levels were higher in group 3, they were not significantly different from those in the other groups. Preoperative PTGBD was performed more frequently in group 3 than in the other groups (P = 0.040). Additionally, preoperative ERCP with an endoscopic sphincterotomy (ES) was performed more often in group 3 for removal of CBD stones, than in the other groups (P < 0.001). Moreover, group 3 patients had more frequent visits to the emergency room with acute abdomen compared with patients from the other groups (P < 0.001) (Table 1).
Outcomes
Conversion to open cholecystectomy (OC) was required in three out of the 35 patients in group 3 due to inadequate visualization of internal structures. Open surgery was required in three of the 91 patients in group 2 and two of the 176 patients in group 1 and the difference was statistically significant (P = 0.039). Operating time (58 minutes vs. 46 minutes and 50 minutes, P = 0.006), and postoperative hospital stay (6.7 days vs. 3.6 days and 4.2 days, P = 0.002) were higher in group 3 than in the other two groups. Group 3 patients had more severe inflammation with higher WBC count and, AST levels, and more CBD stones, and ER visits. Additionally, group 3 patients had a higher incidence of postoperative hematoma in the gallbladder fossa and intraoperative bleeding, but the difference was not significant (P = 0.100 and P = 0.100). The frequency of wound infection and CBD injury was comparable between the groups (Table 2).
Table 2. Laparoscopic cholecystectomy outcomes according to age.
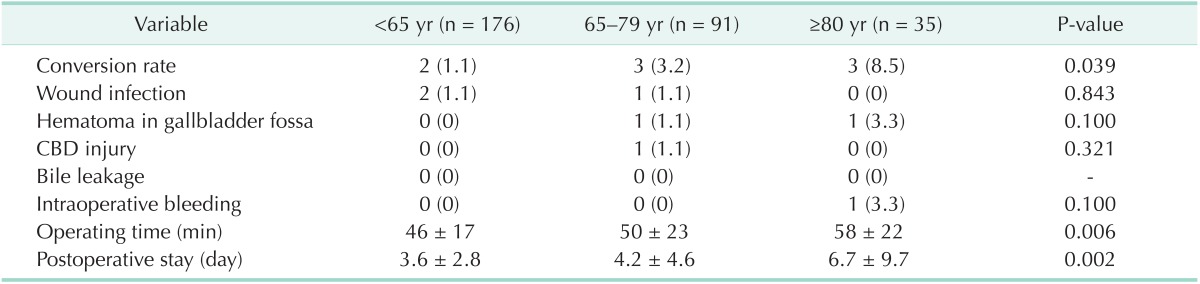
Values are presented as number (%) or mean ± standard deviation.
CBD, common bile duct.
We also found that the conversion rate was associated with preoperative PTGBD and ERCP. The conversion rate was higher in the PTGBD group, but the difference was not significant (8.3% vs. 1.8%, P = 0.071). Furthermore, the PTGBD group had a significantly longer operating time compared to that in the non-PTGBD group (67 ± 30 minutes vs. 47 ± 18 minutes, P < 0.001). The PTGBD group had a longer, but not significantly different, postoperative stay (5.9 ± 5.7 days vs. 3.9 ± 4.6 days, P = 0.054). The conversion rate was higher, but not significantly different, in ERCP group than in the non-ERCP group (2% vs. 3.8%, P = 0.555). The ERCP group had significantly longer postoperative stay compared to that in the non-ERCP group (5.9 ± 9.2 days vs. 3.7 ± 3 days, P = 0.003). In these cases, ERCP with ES followed by an immediate LC was our standard policy, instead of the laparoscopic CBD clearance procedure preferred by others.
Multivariate logistic regression analyses were performed to evaluate the role of potential confounders on the observed relationship of patients' age group with conversion to open surgery and complications. Being older than 80 years was a strong independent risk factor for conversion to OC (odds ratio, 2.84; 95% confidence interval, 1.15-7.03; P = 0.023). ER visit was associated with conversion to OC (P = 0.043). But severity grade of AC was not independent risk factor for conversion and complications. Moreover, male gender, high AST, and ERCP were associated with higher complication rates. The relationship of conversion to OC and development of complications with patients' characteristics is presented in Table 3. There was no bile leakage and mortality was reported.
Table 3. Preoperative factors associated with conversion and complications.
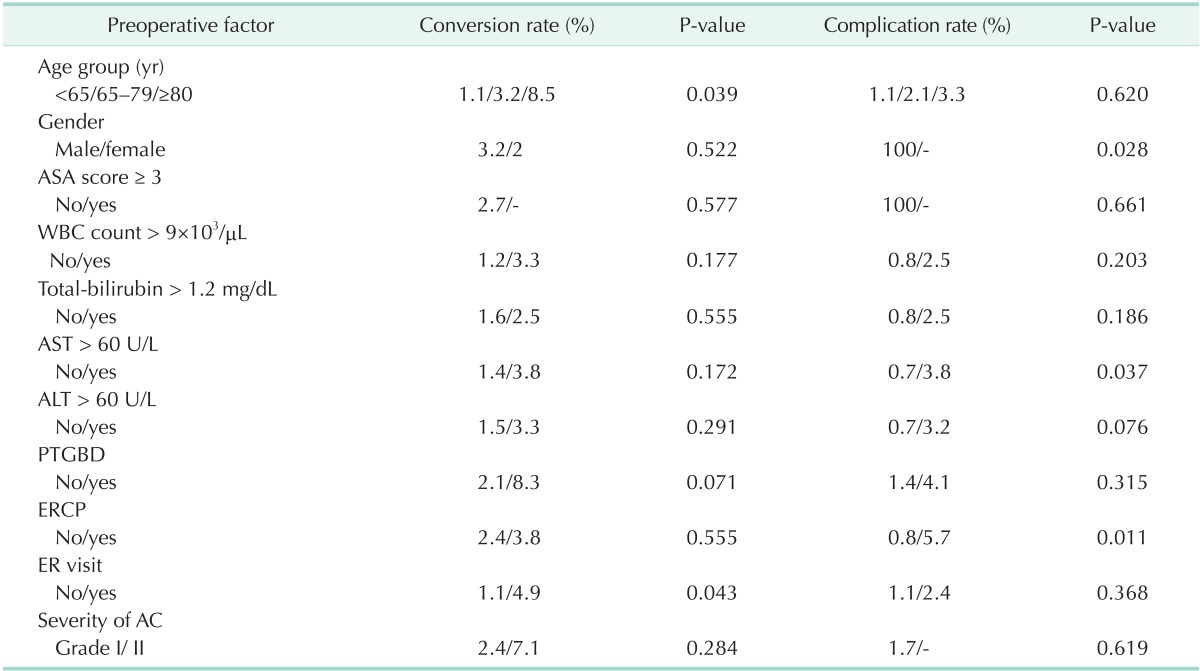
ASA, American Society of Anesthesiologists; PTGBD, percutaneous transhepatic gallbladder drainage; ERCP, endoscopic retrograde cholangiopancreatography; ER, emergency room; AC, acute cholecystitis.
DISCUSSION
The global population is aging. Census predictions indicate that from 1995 to 2020 the percentages of the population aged 65 years or older will increase from 12.8% to 15%, 75 years or older will increase from 5.6% to 6.8% and 85 years or older will increase from 1.4% to 2% [10]. The increasing age of the population has lead to an increasing prevalence of gallstones; therefore, cholecystectomy is a common operation in ageing patients [11,12].
The clinical sequelae of AC can include cholangitis, septic shock, and even death. For these reasons, current management of AC is primarily intravenous antibiotics, followed by prompt cholecystectomy [13]. In physiologically compromised patients, biliary drainage can be accomplished percutaneously, with the goal of cholecystectomy or tube removal after several weeks of biliary decompression and medical optimization [14,15,16]. Advanced age is frequently associated with significant comorbidity and limited functional reserve, which is associated with higher rate of complications, and longer hospital stay. The extremely elderly (≥80 years) have the worst outcomes and may be considered as a separate group. Kuy et al. [4] have shown that patients aged ≥80 years are ≥3 times more likely to need blood transfusions and to require continuous mechanical ventilation and ≥5 times more likely to develop aspiration pneumonitis. Therefore, for high-risk elderly patients, a more conservative approach, including the administration of intravenous fluids and antibiotic therapy, is preferred. PTGBD is a minimally invasive radiologic procedure designed to decompress the acutely inflamed gallbladder in patients who are unresponsive to medical therapy, or who are at high risk for cholecystectomy [17,18]. Elderly patients with AC may be categorized into following groups in our institution; (1) PTGBD only, (2) surgery following PTGBD, (3) surgery without PTGBD. Basically the surgical indication for laparosopic cholecystitis in the elderly patients with AC in our institusion depends on patient's physical performance status and general condition. For high-risk elderly patients, a more conservative approach, including PTGBD and antibiotic therapy, is preferred. The extremely elderly frequently present with several biliary diagnoses and complicated gallstone disease, which explains the higher rates of complications, and mortality usually seen in this group (Table 4) [19,20,21,22,23]. The goal of treatment for the elderly is to provide them with the best possible quality of life with the lowest physiological cost. Several retrospective studies have shown that most elderly patients undergoing LC do well, but when compared with younger patients, the elderly have higher rates of conversion to OC, somewhat longer postoperative stays, and more complications [4,7,16]. In this study, the rate of conversion to OC was 8.5% inpatients older than 80 years (group 3) and was higher than that observed for younger patients (group 1, 1.1%, and group 2, 3.2%). The conversion rate from LC to OC in elderly patients is reported to range from 5% to 27% [4,7,16,20,21,22,23,24].
Table 4. Comparative results from published reports.
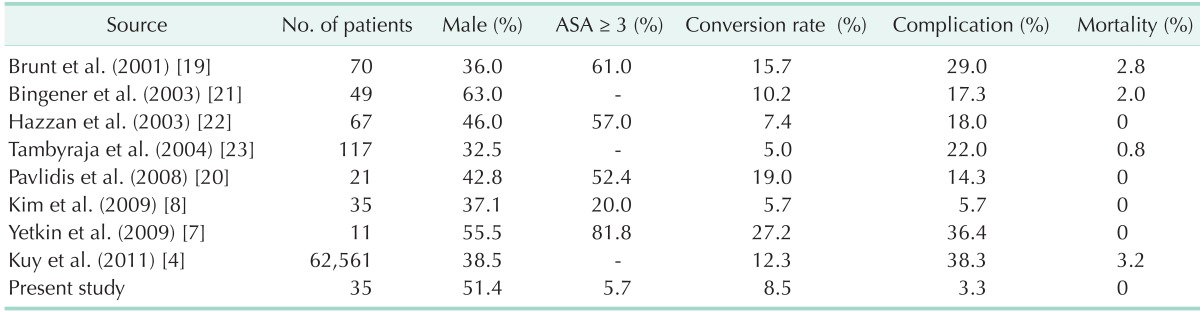
ASA, American Society of Anesthesiologists.
The conversion rate most likely depends on the relative experience of the surgeon with the procedure and on individual patient factors or selection. In this series, we did not select of patients and we performed an analysis to determine if there were factors that had an impact on the outcome of LC. The correlation between age and conversion has been previously reported in elective surgery for cholelithiasis [7,16] as well as in AC [23]. In this series, age was an independent predictor of conversion. Compared with previous published reports, we showed ER visit was an independent predictor of conversion. We showed preoperative WBC count, AST level, and ER visit were significantly higher in group 3 than in the other groups. This study highlights the severity grade of AC seen in older people and it may explain the prolonged operating time and postoperative hospital stay. The degree of inflammation and adhesions in the region of the gallbladder is particularly severe in the elderly and was responsible for most of the conversions in our study. The most important advantage of LC in elderly patients may be the associated reduction in morbidity and mortality rates. In our study, we found that the complication rate was higher in patients older than 80 years (group 3, 3.3%) compared with younger patients (group 1, 1.1% and group 2, 2.1%; P = 0.620). This compares favorably with previous reports of the rates of complications [4,7,16,19,20,21,22,23,25,26,27]. Factors that were found to be associated with complications in group 3 patients were male gender, high AST, and ERCP.
This study has several limitations. First, retrospective analysis carries the potential for selection bias and systematic error. We acknowledge, however, the possibility for residual confounding from both measured and unmeasured variables. Second, the study is limited in that it lack an economic analysis; total cost may be more important than merely length of hospital stay in terms of making healthcare decisions. Third, we did not analyze long-term quality of life and functional outcome. It is not clear that short-term benefits translate into better outcomes in the long term. For instance, a recent study demonstrated no differences in health-related quality of life between patients randomized to OC or LC, either 1 month or 1 year postoperatively [28]. Fourth, we did not consider partial cholecystectomy. Chang et al. [29] were reported that among high-risk patients with AC, 88.3% were managed with percutaneous cholecystostomy (PC) without relapse within a median follow-up period of 38.1 months, despite radiologically severe AC in some patients. Our study did analyze clinical outcome for only surgery patients. We did not consider that a temporary PC can be a first-line treatment for AC without interval cholecystectomy. PC can be alternative techniques to standard cholecystectomy as a safe procedure for treating complicated AC. It should be evaluated in future studies. Fifth, we did not evaluate physiologic complications of pneumoperitoneum. Pneumoperitoneum for laparoscopic surgery may be harmful to elderly patients with underlying comorbidity, especially cardiopulmonary disease, because pneumoperitoneum itself can be physical stress during longer operation time for them. The pneumoperitoneum required for laparoscopic surgery leads to several important hemodynamic alterations. Cardiac output decreases by up to 30% during laparoscopic surgery, due to a decrease in stroke volume. Pneumoperitoneum also causes an increase in systemic vascular resistance. As a result, mean arterial pressure remains unchanged or increases up to 16% [30]. Therefore, patients with marginal cardiac performance may warrant invasive cardiac monitoring to assure they tolerate pneumoperitoneum.
In conclusion, this study has shown that LC can be performed safely in the extremely elderly patients. However, the presence of inflammation is the main factor that influences the adverse outcome of LC in the elderly. Although the current study group was small, we found that LC in older than 80 years is a relatively safe procedure that can be accomplished with acceptable low morbidity and mortality. This is consistent with the findings of previous studies. Therefore, LC should be considered and encouraged for this age group of patients with uncomplicated gallstone disease before advanced disease develops. Given that the elderly now lead increasingly active lifestyles, the rapid return to baseline functional status may be a hallmark benefit of a minimally invasive surgical approach.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Marcari RS, Lupinacci RM, Nadal LR, Rego RE, Coelho AM, de Matos Farah JF. Outcomes of laparoscopic cholecystectomy in octogenarians. JSLS. 2012;16:271–275. doi: 10.4293/108680812X13427982376428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Festi D, Dormi A, Capodicasa S, Staniscia T, Attili AF, Loria P, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project) World J Gastroenterol. 2008;14:5282–5289. doi: 10.3748/wjg.14.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng SP, Chang YC, Liu CL, Yang TL, Jeng KS, Lee JJ, et al. Factors associated with prolonged stay after laparoscopic cholecystectomy in elderly patients. Surg Endosc. 2008;22:1283–1289. doi: 10.1007/s00464-007-9610-4. [DOI] [PubMed] [Google Scholar]
- 4.Kuy S, Sosa JA, Roman SA, Desai R, Rosenthal RA. Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg. 2011;201:789–796. doi: 10.1016/j.amjsurg.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 5.Borzellino G, de Manzoni G, Ricci F, Castaldini G, Guglielmi A, Cordiano C. Emergency cholecystostomy and subsequent cholecystectomy for acute gallstone cholecystitis in the elderly. Br J Surg. 1999;86:1521–1525. doi: 10.1046/j.1365-2168.1999.01284.x. [DOI] [PubMed] [Google Scholar]
- 6.Pessaux P, Tuech JJ, Derouet N, Rouge C, Regenet N, Arnaud JP. Laparoscopic cholecystectomy in the elderly: a prospective study. Surg Endosc. 2000;14:1067–1069. [PubMed] [Google Scholar]
- 7.Yetkin G, Uludag M, Oba S, Citgez B, Paksoy I. Laparoscopic cholecystectomy in elderly patients. JSLS. 2009;13:587–591. doi: 10.4293/108680809X1258998404604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HO, Yun JW, Shin JH, Hwang SI, Cho YK, Son BH, et al. Outcome of laparoscopic cholecystectomy is not influenced by chronological age in the elderly. World J Gastroenterol. 2009;15:722–726. doi: 10.3748/wjg.15.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci. 2012;19:578–585. doi: 10.1007/s00534-012-0548-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Projections of the population of the United States by age, sex, and race: 1983-2080. Washington, DC: U.S. Government Printing Office; 1975. U.S. Bureau of the Census Current population reports, series P-25, N. 952. [Google Scholar]
- 11.Kurbanov FS, Abbasova SF, Aliev IuG, Sushko AN, Dobrovol'skii SR. The laparoscopic cholecystectomy in elderly patients. Khirurgiia (Mosk) 2012;(9):38–41. [PubMed] [Google Scholar]
- 12.Elwood DR. Cholecystitis. Surg Clin North Am. 2008;88:1241–1252. doi: 10.1016/j.suc.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Strasberg SM. Clinical practice. Acute calculous cholecystitis. N Engl J Med. 2008;358:2804–2811. doi: 10.1056/NEJMcp0800929. [DOI] [PubMed] [Google Scholar]
- 14.Csikesz N, Ricciardi R, Tseng JF, Shah SA. Current status of surgical management of acute cholecystitis in the United States. World J Surg. 2008;32:2230–2236. doi: 10.1007/s00268-008-9679-5. [DOI] [PubMed] [Google Scholar]
- 15.Morse BC, Smith JB, Lawdahl RB, Roettger RH. Management of acute cholecystitis in critically ill patients: contemporary role for cholecystostomy and subsequent cholecystectomy. Am Surg. 2010;76:708–712. doi: 10.1177/000313481007600724. [DOI] [PubMed] [Google Scholar]
- 16.Kim KH, Sung CK, Park BK, Kim WK, Oh CW, Kim KS. Percutaneous gallbladder drainage for delayed laparoscopic cholecystectomy in patients with acute cholecystitis. Am J Surg. 2000;179:111–113. doi: 10.1016/s0002-9610(00)00247-6. [DOI] [PubMed] [Google Scholar]
- 17.Kiviniemi H, Makela JT, Autio R, Tikkakoski T, Leinonen S, Siniluoto T, et al. Percutaneous cholecystostomy in acute cholecystitis in high-risk patients: an analysis of 69 patients. Int Surg. 1998;83:299–302. [PubMed] [Google Scholar]
- 18.Davis CA, Landercasper J, Gundersen LH, Lambert PJ. Effective use of percutaneous cholecystostomy in high-risk surgical patients: techniques, tube management, and results. Arch Surg. 1999;134:727–731. doi: 10.1001/archsurg.134.7.727. [DOI] [PubMed] [Google Scholar]
- 19.Brunt LM, Quasebarth MA, Dunnegan DL, Soper NJ. Outcomes analysis of laparoscopic cholecystectomy in the extremely elderly. Surg Endosc. 2001;15:700–705. doi: 10.1007/s004640000388. [DOI] [PubMed] [Google Scholar]
- 20.Pavlidis TE, Marakis GN, Symeonidis N, Psarras K, Ballas K, Rafailidis S, et al. Considerations concerning laparoscopic cholecystectomy in the extremely elderly. J Laparoendosc Adv Surg Tech A. 2008;18:56–60. doi: 10.1089/lap.2007.0037. [DOI] [PubMed] [Google Scholar]
- 21.Bingener J, Richards ML, Schwesinger WH, Strodel WE, Sirinek KR. Laparoscopic cholecystectomy for elderly patients: gold standard for golden years? Arch Surg. 2003;138:531–535. doi: 10.1001/archsurg.138.5.531. [DOI] [PubMed] [Google Scholar]
- 22.Hazzan D, Geron N, Golijanin D, Reissman P, Shiloni E. Laparoscopic cholecystectomy in octogenarians. Surg Endosc. 2003;17:773–776. doi: 10.1007/s00464-002-8529-z. [DOI] [PubMed] [Google Scholar]
- 23.Tambyraja AL, Kumar S, Nixon SJ. Outcome of laparoscopic cholecystectomy in patients 80 years and older. World J Surg. 2004;28:745–748. doi: 10.1007/s00268-004-7378-4. [DOI] [PubMed] [Google Scholar]
- 24.Maxwell JG, Tyler BA, Maxwell BG, Brinker CC, Covington DL. Laparoscopic cholecystectomy in octogenarians. Am Surg. 1998;64:826–831. [PubMed] [Google Scholar]
- 25.Cho JY, Kim JY, Chang SK, Kim SG, Hwang YJ, Yun YK. Is laparoscopic cholecystectomy safe in octogenarians? J Korean Surg Soc. 2009;76:231–235. [Google Scholar]
- 26.Nenner RP, Imperato PJ, Alcorn CM. Complications of laparoscopic cholecystectomy in a geriatric population group. N Y State J Med. 1992;92:518–520. [PubMed] [Google Scholar]
- 27.Fried GM, Clas D, Meakins JL. Minimally invasive surgery in the elderly patient. Surg Clin North Am. 1994;74:375–387. [PubMed] [Google Scholar]
- 28.Nilsson E, Ros A, Rahmqvist M, Backman K, Carlsson P. Cholecystectomy: costs and health-related quality of life: a comparison of two techniques. Int J Qual Health Care. 2004;16:473–482. doi: 10.1093/intqhc/mzh077. [DOI] [PubMed] [Google Scholar]
- 29.Chang YR, Ahn YJ, Jang JY, Kang MJ, Kwon W, Jung WH, et al. Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and reevaluation of treatment efficacy. Surgery. 2014;155:615–622. doi: 10.1016/j.surg.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 30.Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Hemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. J Am Coll Cardiol. 1998;32:1389–1396. doi: 10.1016/s0735-1097(98)00406-9. [DOI] [PubMed] [Google Scholar]


