Abstract
Introduction: Healthcare quality is usually evaluated through analysing medical outcomes including neonatal readmission and patient and family satisfaction. Parental involvement in neonatal care is considered as one of the most important factors, which directly affects these outcomes. The aim of the present study was to determine the effect of family-centered care including maternal participation, presence, and information about neonatal care, on maternal satisfaction and neonatal readmission; the care services were provided by the primiparous mothers of preterm infants.
Materials and Methods: One hundred and ten primiparous mothers with preterm infants participated in this clinical trial. All samples were randomly divided into family-centered care (FCC) and control groups, through simple random sampling. The FCC program, which consisted of information about neonatal care, maternal presence, and participation in the care process, was implemented in the FCC group, while the control group was provided with routine care. Data were obtained using demographic and satisfaction questionnaires and readmission checklist.
Results: In the FCC group, the mean score of satisfaction increased after the implementation of the program (22.36 and 59.28 before and after the program, respectively) (p<0.001); however, this increase in the control group was not significant. The obtained results regarding the different aspects of satisfaction indicated that mothers in the FCC group were more satisfied with maternal presence in the neonatal intensive care unit (NICU), compared with aspects of information and participation. In addition, the number of neonatal readmission was less in the FCC group compared with the control group, and the mean duration of hospitalization was 6.96 and 12.96 days in the FCC and control groups, respectively (p<0.001).
Conclusion: FCC program seems to be effective in increasing maternal satisfaction and decreasing neonatal readmission. Therefore, it seems necessary that healthcare authorities of the departments of obstetrics and gynecology in Iran provide the opportunity for the implementation of such programs in clinical environments, which follow the policy of parental absence and participation in the intensive care units.
Keywords: Neonatal intensive care unit, Readmission, Satisfaction
Introduction
Every year, an estimated 15 million preterm neonates are born (before 37 completed wk of gestation), and this number seems to be rising. Preterm birth is the leading cause of neonatal mortality (neonates in the first four wk of life), and over 1 million infants die annually from the related complications. It is also the second leading cause of death after pneumonia in children under five y of age [1].
Readmission is considered a marker of morbidity in preterm infants [2]. In some cases, readmission is not directly related to the infants’ medical history, but is associated with parental perceptions of infants’ vulnerability or their unfittness to provide care for their preterm infants at home [3]. As the study of Ell (2000) indicates parental perceptions and attitudes (especially mothers’ perceptions) toward their infants’ disease can determine the success or failure of treatment plans and neonatal readmission [4].
The study of Johnson et al., also showed that active parental involvement is essential to providing care for infants, and facilitates the neonatal development during hospitalization and after discharge. In addition, early discharge reduces the costs and risks of hospital-acquired infections [5]. By encouraging maternal-infant contact (through Kangaroo Mother Care and touching) and infant feeding, and parental involvement in neonatal healthcare, the neonates’ responses and signs can be better recognized. In addition, the mothers’ confidence will improve, and the rate of referrals to medical centers, and therefore neonatal readmissions will reduce [6].
Macnab et al., indicated that parents’ daily visits and their active participation in the neonatal care affect the infants’ mental and behavioral problems; active participation can also reduce the impact of small gestational age, low birth weight, and other risks threatening the infants [7].
In recent years, the number of infants admitted to NICUs has increased; consequently, parents experience problems related to prolonged neonatal hospitalization [8]. Therefore, it is suggested that human care be provided based on the psychological needs of these infants; one of the strategies is mothers' 24 h presence at the hospital [9].
Since the framework of infant’s nursing care is family-centered, thus unlimited presence of parents in NICUs and their involvement in the care process improve the maternal experience of infant care, and significantly reduce their dissatisfaction during hospitalization and after discharge [6].
In recent years, a lot of attention has been paid to complications due to neonatal hospitalization; therefore, more actions should be taken in order to reduce the related difficulties for both neonates and their families [10]. The majority of Iranian hospitals do not permit the parents, even mothers, to stay in NICUs for a long time, and they are not allowed to participate in the care process of their neonates. Therefore, this study was performed with the aim to determine the effect of family-centered care including maternal participation, presence, and information about neonatal care, on maternal satisfaction and neonatal re-admission.
Materials and Methods
This study was a randomized clinical parallel trial with a prospective posttest two groups design. This study was conducted at a large university maternity hospital in Tehran, Iran, between June 2010 and September 2010 after obtaining permission from the Ethics Committee of the Iran University of Medical Sciences. The study was performed on 110 primiparous mothers of preterm infants (30-37 wk) with respiratory distress syndrome. The subjects were admitted to the NICU of Akbar-Abadi hospital, a baby-friendly hospital, which was a large university hospital. They were equally allocated to FCC group and a control group (55 women per group) by blocking randomization method.
Flow of the subjects through the trial is presented in [Table/Fig-1].
[Table/Fig-1]:
Legalknowledgebasedonnursingqualification
The sample size is defined using the following equation (confidence level of 95% and power of 80%): [1]
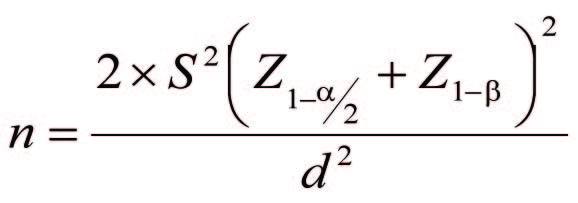 |
It has been assumed that the family-centered care will increase the satisfaction degree by d=6. Using equation 1, the sample size for each group was evaluated as n=44. It should be mentioned that the standard deviation (SD) of the satisfaction has been evaluated as 10, based on the pilot study. In addition, considering the likelihood of sample dropping, the sample size of each group was calculated as 55 cases.
The inclusion criteria for the mothers were as follows: 1) within the age range of 18-35 y, 2) ability to take care of the infant, 3) lack of chronic physical or mental illnesses, 4) literacy, and 5) long-term presence at the hospital by the infant’s side (at least 18 h a day). The neonatal deaths during the study and the mothers’ refusal to continue the study were considered as the exclusion criteria.
All the studied subjects had preterm infants weigh more than 2000g, with the gestational age of 30-37 wk, and respiratory distress syndrome; the subjects were included 24 h after neonatal admission. Furthermore, the infants had no congenital abnormalities or other serious diseases requiring ventilator.
In this study, the primary outcome measure was maternal satisfaction and the secondary outcome measure was infants' hospital readmission frequency.
In order to evaluate maternal satisfaction, a modified satisfaction questionnaire was used, based on the parental satisfaction instrument [11,12] also, readmission checklist (readmission frequency, duration of hospitalization ) was used for assessing the frequency of the infants' readmissions. (readmission defined as an admission to hospital or physician home within 30 d after discharge).
The content validity of the modified questionnaire was determined by 10 faculty members, and its reliability was calculated using Alpha coefficient method (78 %). The modified satisfaction questionnaire consisted of 18 items, considering three aspects of parental satisfaction: parental presence, participation in neonatal care, and information about neonatal care. The questionnaire was graded from zero (very dissatisfied) to four (very satisfied). The grading system of parental satisfaction was as follows: 0-40 for information about neonatal care (including 10 items), 0-24 for participation (including 6 items), and 0-8 for parental presence (including 2 items). The overall satisfaction rate was classified based on the mean scores (score<50%, between 75-50%, and > 75%).
A pilot study was performed on 10 mothers to determine the reliability of the satisfaction tool and to approve the educational pamphlet; the obtained results were removed in the data analysis. Readmission checklist, including two items about neonatal readmission one month after discharge were completed (answers: yes or no), and the frequency of readmission (three options: never, once, twice) was measured.
Twenty-four h after neonatal hospitalization, written consents, demographic information, and satisfaction questionnaires were obtained and completed by the included mothers. The FCC program was practically conducted in the presence of mothers for 30-45 min.
The study was started by informing the FCC group about infection-control strategies, cause of their infants’ hospitalization, breathing exercises, changing infant’s positions, the importance of skin-to-skin contact, feeding methods (gavage and breastfeeding), and leaving the unit at specific times (due to changing shifts, physician’s visits, and cardiopulmonary resuscitation). They were also given educational pamphlets on burping, milk storage, frequency of feeding, showering the infant, and frequency of washing hands with disinfectant solutions.
In order to instruct the mothers, neonatal care services were first provided by the researcher in the presence of the mother; after the maternal skill was confirmed by the researcher, she was responsible for the care of the neonate. On the other hand, the control mothers were only allowed to be present at the time of the infant’s entry to the neonatal care unit, and were only routinely informed.
The questionnaires were again completed by the mothers at the time of discharge. The mean time to complete the questionnaire was approximately 10 min.
In the present single-blind study, the neonatal care information sessions were held in the NICU, where the mothers of the control group were not allowed to enter. In addition, all of the steps in the FCC program were practical, and the mothers in the FCC group performed these activities during their regular presence at the hospital.
Results
Based on the results, the mean age of the subjects was 25.3 and 26.5 y in the FCC and control groups, respectively. Most of the participating mothers did not have any academic diplomas (60%).
In addition, the FCC (84%) and control (76%) groups were provided with good family support [Table/Fig-2].
[Table/Fig-2]:
Maternal Demographic Background Varibles
* t-test, ** Chi-square, *** Fisher’s exact test
| FCC group (n=50) | Control group (n=50) | p-value | |
|---|---|---|---|
| Occupation, n/N (%) *: | 1.00 | ||
| housekeeper | 2(4) | 2(4) | |
| Maternal age, mean± SD**: | 25.3±4.3 | 6.5±4.2 | |
| >20 y old | 8(16} | 4(8) | |
| 25-21 y old | 17(34) | 17(34) | |
| 26-30 y old | 19(38) | 23(46) | |
| 35-31 y old | 6(12) | 6(12) | |
| Economic status n/N (%)*: | |||
| low | 9(38) | 13(26) | |
| average | 40(80) | 36(72) | |
| high | 1(2) | 1(2) | |
| History of abortion or stillbirth | |||
| n/N ***: | 0.50 | ||
| yes | 13(26) | 16(32) | |
| no | 37(4) | 34(68) |
Regarding the demographic information about neonatal care, the difference between the mothers in the FCC and control groups was insignificant except gestational age [Table/Fig-3].
[Table/Fig-3]:
Infants’ Medical Background Variables
* t-test
| FCC group (n=50) | Control group (n=50) | p-value | |
|---|---|---|---|
| Gestational age (week) mean± SD*: | 34/16±1.96 | 33.90± 2.33 | 0.51 |
| 30- 34wk | 31(62) | 35(70) | |
| 34-37 wk | 19(38) | 15(30) | |
| Neonatal weight (g) mean±SD*: | 2373/60±403/01 | 2391/98±438/34 | 0.82 |
| >2500g | 35(70) | 33(66) | |
| 2501- 3000g | 8(16) | 10(20) | |
| <3000 g | 7(14) | 7(14) |
In addition, the follow-up test indicated there was a significant difference between the FCC group and the control group regarding the infants' hospital readmission (p<0.001) [Table/Fig-4].
[Table/Fig-4]:
Comparison of the neonatal outcomes one month after discharge
* Chi-square, ** t-test
| FCC group (n= 47) | Control group (n= 44) | p-value | |
|---|---|---|---|
| Frequency of hospitalization (n/N) *: | 0.04 | ||
| never | 45(95.7) | 36 (81.8) | |
| once | 2(4.3) | 6 (13.6) | |
| twice | 0 (0) | 2 (4.5) | |
| Hospitalization duration (mean±SD) **: | 6.96±4.90 | 12.96±6.90) | < 0.001 |
| < 7 days | 30(60) | 7(14) | |
| 7- 14days | 18(36) | 16(32) | |
| >14 days | 2(4) | 27(54) |
Results show a high level of satisfaction among the FCC group (p < 0.001) after the program implementation, compared with the control group [Table/Fig-5].
[Table/Fig-5]:
Comparison of maternal satisfaction in the FCC and control groups before and after the intervention
| Intervention Groups | Before | After | ||
|---|---|---|---|---|
| FCC | Control | FCC | Control | |
| X ± SD | 22.36±8.90 | 22.06±9.77 | 59.28±6.86 | 30.18±14.09 |
| p-value | 0.87 | <0.01 | ||
According to the results, mothers in the FCC group were more satisfied with maternal presence in NICUs, in comparison with information and participation aspects [Table/Fig-6].
[Table/Fig-6]:
Distribution of satisfaction scores regarding various aspects in the FCC group after the intervention
Discussion
According to the obtained results, the implementation of FCC program increases the satisfaction of mothers with premature infants; the mean overall satisfaction increased to 59.28 in the FCC group after the intervention. In contrast, the increase of overall satisfaction in the control group was insignificant, which is consistent with the findings of Scott et al., who conducted a study with the aim to assess the impact of parental presence in a post anesthesia care unit. It was revealed that parental satisfaction increased after parental presence, information, and participation. However, this study included the parents (both mother and father) and children within the age range of 1-7 y, who had undergone adenoidectomy, tonsillectomy and elective oral surgery [11].
Weiss et al., by performing a three-step intervention in NICU, showed that establishing effective communication with the parents and informing them about their infants and the required care can result in increased satisfaction (p<0.01) [13]. It should be noted that Weiss and colleagues in their study, considered parents as the study population, while in the present study, the subjects were primiparous mothers.
Wielenga et al., also believed that encouraging parents to spend time with their infants and have active participation in the care process can facilitate the development of parental roles and increase the satisfaction rate [14].
Bakewell et al., have indicated that active maternal involvement in the neonatal care and mother-infant contact (e.g. touching the baby) will increase maternal confidence to take care of the infant after discharge, and consequently will lead to higher maternal satisfaction [6].
The results of the present study, which considered maternal presence as one of the satisfaction aspects, were consistent with the study of Chan and colleagues, which was conducted with the aim to assess the effect of training programs on parental satisfaction. They found that these programs could increase parental satisfaction (p<0.001), depending on parental needs for participation and their expectations of anesthetic paediatric care units and educational pamphlets [15]. It should be mentioned that they analysed satisfaction rates based on only maternal presence in the unit.
Furthermore, a descriptive study by Bialoskurski et al., which aimed to investigate the nature and organization of maternal needs and priorities in a neonatal unit, was performed on 209 mothers with preterm infants. The results showed that the need for accurate infant-related information was the priority for 93% of the mothers. Moreover, according to this study, maternal satisfaction can affect the mother’s desire to participate in the care process; it can also influence other clinical outcomes such as treatment efficacy [16].
In a study by Reis et al., the parents stated that interaction with nurses and verbal and written information regarding the conditions of their infants were essential; of course, the method of communication was also of significance [17]. In some studies, it has been also revealed that information can lead to parental confusion; therefore, it can decrease confidence in health care systems, increase anxiety, and eventually decrease parental satisfaction [7,18]; these results are not consistent with the findings of the present study.
Satisfaction is a multidimensional concept, and these dimensions reflect the gap between expectations and supplies [19]. Based on the study by Conner et al., 11 important care dimensions were determined which were important to parents with premature infants. These dimensions include assurance, caring, communication, consistent information, education, environment, follow-up care, pain management, participation, proximity, and support [20].
The present study is the first to measure satisfaction rates by comparing three different aspects of parental satisfaction (parental presence, participation in the care, and infant-related information) in the NICU. Espineira et al., investigated three specific aspects of satisfaction including information, privacy, and the friendly approach of medical staff [19].
The other results of this study indicated a decrease in neonatal readmission and the mean of hospitalization duration in the FCC group. This is consistent with the results of Erdve et al., who conducted a study in Thailand. In this study, in the case group, the infants and their mothers were admitted to a private room in the hospital (instead of NICU), and the mothers were involved in the neonatal care; on the other hand, the control infants were admitted to NICU, and the mothers did not participate in their infants’ care. The results showed that the number of readmissions and referrals to physicians decreased in the intervention group [3].
Ortenstrand et al., found a 5-day reduction in the duration of hospitalization for preterm infants, and reported that parental involvement can directly affect the stability and morbidity of the infants [9]; the findings were similar to the results of the present study. Therefore, parents who spend more time with their infants have more opportunities for perceiving the signs of infants’ discomfort and their other needs; consequently, they function better in comparison with nurses who are responsible for the caring of multiple infants [21]. This confirms the findings of Zelkowitz et al., who indicated that mothers' sensitivity about neonatal signs and symptoms increased due to the provided information [22]. In the mentioned study, with the aim to reduce maternal anxiety and improve developmental outcomes in very low birth weight infants, mothers in the intervention group learned specific skills to reduce discomfort, and become more sensitive to infant cues.
Peyman et al., conducted a study on 70 infants under kangaroo mother care program (KMCP), with a mean gestational age of 32.5 wk and mean weight of 1560 g. Almost 58 cases followed this program for at least one year. They found significantly reduced rates of readmission [23], which is consistent with the results of the present study; of course, in this study, the emphasis was on KMCP as a part of family-centered care.
Bhutta et al., performed a study (2004) entitled "Reducing length of stay in hospital for very low-birth-weight infants by involving mothers in a step-down unit” in Pakistan. They showed that the length of stay significantly decreased in infants whose mothers had provided all major nursing care before discharge. The results of this study showed that the active involvement of mothers in the care process of their infants before discharge decreases the length of hospital stay, and results in early discharge and reduced hospital-acquired infections (p<0.05) [24]. These results were consistent with the results of the present study.
Study Limitations
The obtained results should be cautiously interpreted due to certain limitations of the study design. Firstly, we did not control the confounders, which might have affected satisfaction, e.g., severity of mothers’ genital pain, and their sleep quality. Secondly, significant differences between the two groups in terms of infants' age (p=0.049). However, in many studies, including the study of Macnab et al., which was performed on parental attitude, adequacy, and the extent of family-centered care patterns in NICUs, age was not found as an effective variable.
In other words, parents’ daily regular visits, their active participation in the care process of their infants, and the resultant effects on infants’ mental and behavioral problems are found to be more effective than the impact of gestational age, birth weight or other infant-threatening risks [7]. In addition, the gestational age was considered between 30 to 37 wk, and during this age, infants are not as vulnerable as they are at <30 wk of gestation [25]; therefore, this difference is not highly significant, and does not affect the infants’ survival rate and hospitalization. Lack of precise timing of maternal presence in the FCC group, due to ethical considerations, was another limitation of the study.
Conclusion
Parental participation in neonatal care is the basis of modern neonatal nursing, and parents, especially mothers, can play a significant role in controlling diseases and treatment processes. Therefore, it seems necessary for the health system authorities to provide opportunities for the implementation of these strategies in clinical environments. In future studies, it is recommended that long-term effectiveness of such programs be further investigated.
Acknowledgement
The present study is part of a research project (949/p) approved by Iran University of Medical Sciences. The authors would like to thank all the mothers who participated and completed the questionnaires, and helped us with performing the study. (IRCT2014022216681N1).
Financial or Other Competing Interests
None.
References
- [1]. Preterm birth. Fact sheet N°363 Updated November 2013 http://www.who.int/mediacentre/factsheets/fs363/en/ Accessed 2014 .
- [2].LW Doylea, G Fordc, N Davisc. Health and hospitalisations after discharge in extremely low birth weight infants. Semin Neonatol. 2003;8:137–45. doi: 10.1016/S1084-2756(02)00221-X. [DOI] [PubMed] [Google Scholar]
- [3].O Erdeve, S Arsan, S Yigit, D Armangil, B Atasay, A Korkmaz. The impact of individual room on rehospitalisation and health service utilization in preterm after discharge. Acta pediatr. 2008;97:1351–57. doi: 10.1111/j.1651-2227.2008.00889.x. [DOI] [PubMed] [Google Scholar]
- [4].K Ell. Social network, social support and coping with serious illness: the family connection. Social sicence medical. 2000;42:173–83. doi: 10.1016/0277-9536(95)00100-x. [DOI] [PubMed] [Google Scholar]
- [5].BH Johnson, MR Abraham, RN Parrish. Designing the Neonatal Intensive Care Unit for optimal family involvement. Clin Perinatol. 2004;31:353–82. doi: 10.1016/j.clp.2004.04.008. [DOI] [PubMed] [Google Scholar]
- [6].S Bakewell- sacchs, S Genaros. Parenting the Post- NICU premature infant. MCN Am J Matern Child Nurs. 2004;29:398–403. doi: 10.1097/00005721-200411000-00011. [DOI] [PubMed] [Google Scholar]
- [7].AJ Macnab, P Thiessen, E McLeod, D Hinton. Parent assessment of family centered care practices in a children’s hospital. Child Health Care. 2000;29:113–28. [Google Scholar]
- [8].S-N Chang Lee, A Long, J Boore. Taiwanese womens experience of becoming a mother a very –low-birth-weight preterm infant. Int J Nurs Stud. 2009;46:326–36. doi: 10.1016/j.ijnurstu.2008.10.004. [DOI] [PubMed] [Google Scholar]
- [9].A Ortenstrand, B Westrup, EB Broström, I Sarman, S Akerström, T Brune, et al. The Stockholm Neonatal Family Centered Care Study: Effects on Length of Stay and Infant Morbidity. Paediatrics. 2010;125:278–85. doi: 10.1542/peds.2009-1511. [DOI] [PubMed] [Google Scholar]
- [10].DL Wong, M Hockenberry, D Wilson, ML Winkelstein, NE Kline. Nursing care of infants and children. St. Louis: Mosby. 2003;74:669–71. [Google Scholar]
- [11].Teratology. 2006. J H-S. Parental presence in the paediatric post anesthesia care unit: Effects on patient outcomes and parent satisfaction. [Google Scholar]
- [12].JM Latour, JA Hazelzet, HJ Duivenvoorden, JB Goudoever Van. Construction of parent satisfaction instrument: perceptions of paediatric intensive care nurses and physicians. J Crit Car. 2009;24:255–66. doi: 10.1016/j.jcrc.2008.06.002. [DOI] [PubMed] [Google Scholar]
- [13].S Weiss, E Goldlust, YE Vaucher. Improving parent satisfaction: an intervention to increase neonatal parent–provider communication. J Perinatol. 2010;30:425–30. doi: 10.1038/jp.2009.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].JM Wielenga, BJ Smit. How satisfied are parents supported by nurses with the NIDCAP model of care for their preterm infant? J Nurs Care Qual. 2006;21:41–48. doi: 10.1097/00001786-200601000-00010. [DOI] [PubMed] [Google Scholar]
- [15].CSM Chan, A Molassiotis. The effects of an educational programme on the anxiety and satisfaction level of parents having parent present induction and visitation in a postanaesthesia care unit. Paediatr Anaesth. 2002;12:131–39. doi: 10.1046/j.1460-9592.2002.00790.x. [DOI] [PubMed] [Google Scholar]
- [16].MM Bialoskurski, CL Cox, RD Wiggins. The relationship between maternal needs and priorities in a neonatal intensive care environment. J Adv Nurs. 2002;37:62–69. doi: 10.1046/j.1365-2648.2002.02057.x. [DOI] [PubMed] [Google Scholar]
- [17].MD Reis, SD Scott, GR Rempel. Including Parents in the Evaluation of Clinical Microsystems in the Neonatal Intensive Care Unit. Adv Neonatal Care. 2009;9:174–79. doi: 10.1097/ANC.0b013e3181afab3c. [DOI] [PubMed] [Google Scholar]
- [18].JM McGrath. Building relationships with families in the NICU: exploring the guarded alliance. J Perinatal Neonatal Nurs. 2001;15:74–83. doi: 10.1097/00005237-200112000-00007. [DOI] [PubMed] [Google Scholar]
- [19].C Herrera-Espineira, MDM Rodriguez del Agulia, M Rodriguez del Castillo, AF Valdivia, IR Snchez. Relation ship between anxity level of patients and their satisfaction with different aspects of healthcare. J Am Health Policy. 2009;89:37–45. doi: 10.1016/j.healthpol.2008.04.012. [DOI] [PubMed] [Google Scholar]
- [20].JM Conner, EC Nelson. Neonatal intensive care: satisfaction measured from a parent s perspective. Paediatrics. 2010;103:336–48. [PubMed] [Google Scholar]
- [21].L Shields, I Kristensson-Hallström, M O'Callaghan. An examination of the needs of parents of hospitalized children: comparing parents' and staff's perceptions. Scand J Caring Sci. 2003;17:176–84. doi: 10.1046/j.1471-6712.2003.00215.x. [DOI] [PubMed] [Google Scholar]
- [22].P Zelkowitz, N Feeley, I Shrier, R Stremler, R Westreich, D Dunkley, et al. The Cues and Care Trial: A randomized controlled trial of an intervention to reduce maternal anxiety and improve developmental outcomes in very low birthweight infants. BMC Pediatr. 2008;8:38. doi: 10.1186/1471-2431-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].A Peyman, FZ Rabani, F Gachpezon. The impact of kangaro mother care program on preterm feeding and clinical state. New Navid. 2008;37:29–38. [Google Scholar]
- [24].ZA Bhutta, I Khan, S Salat, F Raza, I Khan, H Ara. Reducing length of stay in hospital for very low birthweight infants by involving mothers in a stepdown unit: an experience from Karachi (Pakistan) BMJ. 2004;329:1151–55. doi: 10.1136/bmj.329.7475.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].GJ Escobar, MC McCormick, JAF Zupancic, K Coleman-Phox, MA Armstrong, JD Greene. Un studied infant: Outcomes of moderately premature infants in the neonatal intansive care unit. Arch Dis Child Fetal Neonatal ED. 2006;91:238–44. doi: 10.1136/adc.2005.087031. [DOI] [PMC free article] [PubMed] [Google Scholar]



![[Table/Fig-1]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/bf7e/4347142/795b23bd4f06/jcdr-9-SC04-g001.jpg)
![[Table/Fig-6]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/bf7e/4347142/1b5bceb55916/jcdr-9-SC04-g002.jpg)