Abstract
Cysticercosis has become increasingly recognized as an important infection in the United States in recent decades. Despite its potential impact, there is a lack of comprehensive information on the nationwide burden of disease. To better define the burden of cysticercosis in the United States, we analyzed in-patient records using the Nationwide Inpatient Sample for 1998–2011 to estimate cysticercosis-related hospitalizations and patient/institutional characteristics. There were an estimated 33,060 (95% confidence interval [95% CI] = 29,610.5–36,510.3) cysticercosis-related hospitalizations nationwide, representing a hospitalization rate of 8.03 per million population. The highest proportion of cases were male (54.8%), Hispanic (62.0%), aged 18–44 (58.8%), and occurred in the West (45.1%). An estimated 459 deaths occurred, representing an in-hospital case-fatality rate of 1.4%. These findings indicate the burden of cysticercosis-related hospitalizations in the United States is considerable and may be greater than currently appreciated. Cysticercosis should be a nationally reportable disease.
Introduction
Cysticercosis is an important parasitic infection caused by the larval stage of the pork tapeworm, Taenia solium. Neurocysticercosis (NCC), which occurs when larvae invade the central nervous system, is one of the most common parasitic diseases of the human nervous system and a leading cause of symptomatic epilepsy worldwide.1,2 Common in lower-income countries where the parasite is endemic, cysticercosis, particularly NCC, has become increasingly important in the United States in recent decades.1,2
Taenia solium has an intricate lifecycle involving both humans and pigs.1,3 Humans are the natural definitive host, harboring the adult tapeworm in the intestinal tract in a condition known as taeniasis.1,3 Eggs, which are directly infectious, are shed in the feces of humans infected with the adult tapeworm. When these eggs are ingested by pigs, larvae emerge from the eggs, penetrate the intestinal mucosa and disseminate through the bloodstream to various tissues where the larval stage, or cysticercus, develops. To complete the cycle the adult tapeworm will develop in the small intestine of the human host after the ingestion of raw or undercooked pork containing cysticerci.1,3 Human cysticercosis occurs when viable eggs are ingested, typically in contaminated food or water.1,3 Taeniasis may be asymptomatic or present with mild symptoms, though it usually produces no serious pathology.3 Human cysticercosis, however, can produce severe symptoms depending on the number, size, and location of cysticerci, and may include loss of vision, meningitis, hydrocephalus, and in some cases, death.4
Relatively limited information on cysticercosis in the United States has included data from several hospital-based case series, a single emergency department study, three hospital discharge analyses, mortality data, surveillance information from two jurisdictions and limited surveys in selected populations.2,5–22 Only one of these studies, however, examined the country-wide burden of disease using a national-level database.18 These studies have contributed vital information toward describing the occurrence of this disease in the United States, however they reflect only a portion of actual cases.22 Cysticercosis is currently only reportable in Arizona, California, New Mexico, Oregon, Texas, and Alaska, though even within these jurisdictions underreporting may exist, leaving the true impact of the disease largely unknown.22 Given the potential severity and impact of cysticercosis and the lack of comprehensive data on the burden of cysticercosis in the United States, additional national-level studies are needed. To help better define the burden of cysticercosis in the United States, cysticercosis-related hospitalizations were analyzed for the 14-year period 1998–2011.
Methods
Data source.
In-patient hospitalization records were examined using the Nationwide Inpatient Sample (NIS), part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality.23,24 Annual NIS data sets from 1998 to 2011 contain ∼7–8 million hospital discharge records each year from around 1,000 hospitals throughout the country, and are designed to approximate a 20% stratified sample of United States community hospitals.24 The NIS also contains weighting variables allowing for the calculation of national estimates of hospitalizations. The data contain more than 100 clinical and nonclinical data elements for each hospital stay, including demographic, institutional and hospital stay characteristics, such as age, regional hospital location, and up to 15 diagnostic and procedural codes (up to 25 diagnostic codes in 2009–2011).24 Further description of the NIS data sets can be found through the Agency for Healthcare Research and Quality.23
Case identification and inclusion.
Cysticercosis-related hospitalizations were identified as any discharge record with an International Classification of Diseases, Ninth Revision, Clinical Modifications (ICD-9-CM) code of 123.1, defined as Cysticercosis (Cysticerciasis - Infection by Cysticercus cellulosae [larval form of T. solium]), listed for either primary or non-primary diagnoses.
Data analysis.
Both the overall and annual numbers of cysticercosis-related hospitalizations were recorded and characteristics of those hospitalized were examined. Data analysis was completed using SAS version 9.2 (SAS Institute, Cary, NC), using procedures designed to account for the complex stratified cluster sampling design of the data set. Hospital and discharge weights provided with the NIS data and documentation were used to produce national estimates of cysticercosis-related hospitalizations.24,25 Primary demographic characteristics of interest included age at admission, gender and race/ethnicity (white, black, Hispanic, Asian or Pacific Islander [A/PI], Native American [NA], and other).25 To aid in interpretation, “age at admission” was analyzed both by calculating mean age (in years) and by separating age into five categories of age groups (1–17, 18–44, 45–64, 65–84, and 85+ years of age). Associations between race/ethnicity and age group, gender and region were examined using χ2 tests (with a significance level of 0.05) accounting for the sampling design of the NIS. The U.S. Census Bureau population estimates were used to calculate characteristic-specific estimated rates of cysticercosis-related hospitalizations.26–28
Primary institutional and hospital stay characteristics examined included regional location of hospital (Northeast, Midwest, South, and West), hospital teaching status (non-teaching versus teaching), hospital location type (rural versus urban), hospital bed size (small, medium, and large, with designated categories based on the hospital's region, teaching status, and location), and average length of hospital stay (in days) per discharge for cysticercosis-related hospitalizations.25 Estimates for the total number of national in-hospital deaths among cysticercosis-related hospitalizations were also calculated. Patient records were also stratified by those with primary and non-primary diagnoses of cysticercosis. Differences in demographic factors including age group, gender, and race between those with and without a primary diagnosis of cysticercosis among all cysticercosis-related hospitalizations were tested using χ2 tests with a significance level of 0.05, with techniques accounting for the sampling design of the NIS. Among patients with a listed primary diagnosis other than cysticercosis, the most common primary diagnoses were identified. For those with cysticercosis listed as the primary diagnosis, the most common secondary diagnoses were identified. For analysis of comorbidities, unweighted estimates from the NIS were used for ease of interpretability. Notations were added to tables where appropriate to indicate missing data.
Results
Cysticercosis-related hospitalizations.
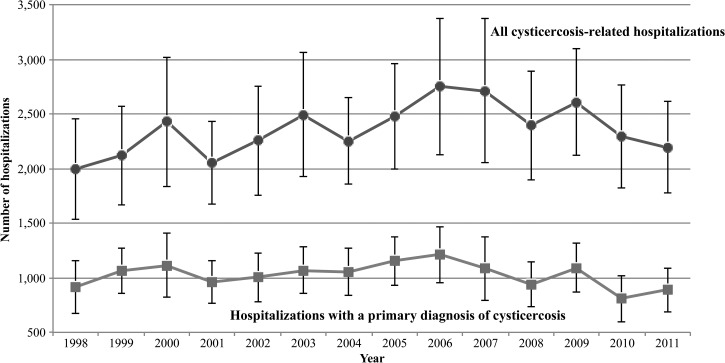
Over the entire study period, there were an estimated 33,060 (95% confidence interval [CI] [29,610.5–36,510.3]) cysticercosis-related hospitalizations in the United States (Table 1), based on the 6,774 discharges that included a diagnosis of cysticercosis within the 14 yearly NIS data sets. Of the total estimated cysticercosis-related hospitalizations, 14,365 (95% CI [12,952.8–15,776.3]), or 43.5%, listed a primary diagnosis of cysticercosis. Estimated annual numbers of hospitalizations varied from 1,998.1 to 2,753.1 with an average of 2,361.5 hospitalizations per year (Figure 1 ). The estimated number of hospitalizations with a primary diagnosis of cysticercosis ranged from a low of 807.3 in 2010 to a high of 1,211.6 in 2006. An estimated 459.2 (95% CI [328.9–589.5]) cysticercosis-related in-hospital deaths were recorded, representing a 1.4% in-hospital fatality rate. Cysticercosis-related hospitalizations were reported from 42 states, with the highest percentages of unweighted discharges from hospitals in California, Texas, Illinois, and New York (accounting for 38.0%, 12.0%, 8.0%, and 7.4% of total discharges, respectively).
Table 1.
Estimated cysticercosis-related hospitalizations and rates in the United States, stratified by demographic and institutional characteristics, 1998–2011*†
| n | 95% CI | % Of total cysticercosis-related hospitalizations | Rate/million population | |
|---|---|---|---|---|
| Total cysticercosis-related hospitalizations, any diagnosis | 33,060.0 | [29,610.5–36,510.3] | − | 8.03 |
| Cysticercosis-related hospitalizations, primary diagnosis | 14,365.0 | [12,952.8–15,776.3] | 43.5% | 3.49 |
| Sex | ||||
| Male | 18,129.0 | [16,328.5–19,929.6] | 54.8% | 8.96 |
| Female | 14,702.0 | [12,925.3–16,478.9] | 44.5% | 7.01 |
| Missing | 0.7% | − | ||
| Race/ethnicity | ||||
| White | 2,552.8 | [2,227.7–2,877.8] | 7.7% | 0.93 |
| Black | 1,464.3 | [1,069.0–1,859.5] | 4.4% | 2.92 |
| Hispanic | 20,494.0 | [17,611.6–23,375.8] | 62.0% | 34.83 |
| Asian or Pacific Islander | 614.1 | [392.3–835.9] | 1.9% | 3.42 |
| Native American | 66.3 | [27.3–105.3] | 0.2% | 2.18 |
| Other | 2,466.0 | [1,824.0–3,107.9] | 7.5% | − |
| Missing | 16.3% | − | ||
| Age group | ||||
| 1–17 | 2,438.4 | [2,004.9–2,872.0] | 7.4% | 2.51 |
| 18–44 | 19,427.0 | [17,444.3–21,410.7] | 58.8% | 12.34 |
| 45–64 | 7,315.8 | [6,301.0–8,330.7] | 22.1% | 7.31 |
| 65–84 | 3,417.0 | [2,837.1–3,996.8] | 10.3% | 7.55 |
| 85+ | 422.8 | [306.9–538.8] | 1.3% | 6.35 |
| Missing | 0.1% | − | ||
| Mean age (in years) | 39.6 | [38.7–40.5] | − | |
| Region of hospital | ||||
| Northeast | 4,524.4 | [3,685.9–5,363.0] | 13.7% | 5.94 |
| Midwest | 4,238.3 | [3,217.8–5,258.9] | 12.8% | 4.61 |
| South | 9,371.5 | [7,477.4–11,265.6] | 28.3% | 6.26 |
| West | 14,926.0 | [12,363.1–17,489.3] | 45.1% | 15.83 |
| Missing | 0.0% | − | ||
| Hospital teaching status | ||||
| Non-teaching | 12,654.0 | [10,795.2–14,512.2] | 38.3% | − |
| Teaching | 20,239.0 | [17,332.6–23,146.2] | 61.2% | − |
| Missing | 0.5% | − | ||
| Hospital location | ||||
| Rural | 702.8 | [540.6–865.0] | 2.1% | − |
| Urban | 32,190.0 | [28,744.0–35,636.7] | 97.4% | − |
| Missing | 0.5% | − | ||
| Bed size of hospital | ||||
| Small | 2,567.6 | [2,041.9–3,093.3] | 7.8% | − |
| Medium | 8,333.1 | [7,042.9–9,623.2] | 25.2% | − |
| Large | 21,992.0 | [18,836.1–25,148.8] | 66.5% | − |
| Missing | 0.5% | − | ||
| Mean length of hospital stay (in days) | 6.3 | [6.0–6.6] | − | |
Figure 1.
Annual estimates of cysticercosis-related hospitalizations in the United States, 1998–2011. National estimates based on NIS hospital and sample weights. Bars on data points represent 95% confidence intervals.
Demographic characteristics of hospitalizations.
Overall demographic characteristics of cysticercosis-related hospitalizations are presented in Table 1. Males constituted a larger proportion of estimated cysticercosis-related hospitalizations, with a male/female ratio of 1.23 to 1. Hispanics accounted for the largest proportion (62.0%) of cysticercosis-related hospitalizations, with white, black, A/PI, NA, and “other” race/ethnicity individuals accounting for 7.7%, 4.4%, 1.9%, 0.2%, and 7.5%, respectively. The age group 18–44 years held the largest proportion (58.8%) of cysticercosis-related hospitalizations with the smallest proportion reported in the 85+ years age group (1.3%). The mean age of patients with cysticercosis-related hospitalizations was 39.6 years of age (95% CI [38.7–40.5]). An association was found between age group and race/ethnicity within the overall study period (P < 0.0001), with a higher proportion of 18–44 year olds observed among Hispanics and the “other” race/ethnicity category. An association was also found between gender and race/ethnicity (P = 0.002), with a higher proportion of males observed among Hispanics and the “other” race/ethnicity category.
Differences were also observed between those with primary versus non-primary diagnoses of cysticercosis and the selected demographic variables of race/ethnicity (P = 0.02), gender (P < 0.0001), and age group (P < 0.0001). A higher than average proportion of males, blacks, A/PIs, 1–17 year olds and 18–44 year olds were observed among patients with a primary diagnosis of cysticercosis.
Nationally estimated hospitalization rates for cysticercosis are presented in Table 1. The overall cysticercosis-related hospitalization rate for the study period was 8.03 hospitalizations per million population. The rate for hospitalizations with cysticercosis listed as the primary diagnosis was 3.49 hospitalizations per million population. The age group 18–44 years had the highest cysticercosis-related hospitalization rate of 12.34 hospitalizations per million population, with the lowest in the age group 1–17 years of 2.51 hospitalizations per million population. Hispanics had the highest cysticercosis-related hospitalization rate of 34.83 hospitalizations per million population, followed by A/PIs (3.42 per million), blacks (2.92/million), and NAs (2.18/million) with the lowest rates in those recorded as white (0.93/million). Males had a higher rate than females of 8.96 versus 7.01 cysticercosis-related hospitalizations per million population.
Institutional characteristics of hospitalizations.
Overall institutional characteristics of cysticercosis-related hospitalizations are presented in Table 1. The largest proportion of hospitalizations was observed from hospitals located in the West of the country (45.1%), followed by the South (28.3%), Northeast (13.7%), and Midwest (12.8%). Cysticercosis-related hospitalization rates (Table 1) showed a similar pattern, with the highest rates in the West (15.83 per million population) and the lowest in the Midwest (4.61 per million population). Nearly double the number of estimated cysticercosis-related hospitalizations were from teaching hospitals when compared with non-teaching hospitals throughout the country (61.2% versus 38.3%). In contrast, teaching hospitals represented between 41% and 48% of the total estimated hospital discharges (any diagnosis) per year between 1998 and 2011.29 The vast majority of estimated cysticercosis-related hospitalizations were from hospitals located in urban versus rural locations (97.4% versus 2.1%). Discharges from urban/metropolitan locations represented 84–88% of the total estimated hospital discharges (any diagnosis) per year between 1998 and 2011.29 When examining the distribution of cysticercosis-related hospitalizations from differently sized hospitals (by bed size), 66.5%, 25.2%, and 7.8% of cases came from large, medium, and small hospitals, respectively. Similar hospitalization distributions from large, medium, and small hospitals were observed when examining all hospitalization discharge estimates (any diagnosis) between 1998 and 2011.29 Patients with a cysticercosis-related hospitalization had an average hospital stay of 6.3 days (95% CI [6.0–6.6]). A statistically significant association between hospital region and race/ethnicity for the overall study period was observed (P < 0.0001), with a higher number of observed Hispanics hospitalized in the West.
Comorbid diagnoses.
Cysticercosis was listed as the primary diagnosis in 43.5% of cysticercosis-related hospitalizations. In these cases, common secondary diagnoses included “other convulsions” (in 39.3% of records), “obstructive hydrocephalus” (in 7.2% of records), “cerebral edema” (in 2.9% of records), “epilepsy, unspecified, without mention of intractable epilepsy” (in 2.8% of records), and “headache” (in 2.2% of records). In cases where cysticercosis was not listed as the primary diagnosis, the most common primary diagnoses included “other convulsions,” “obstructive hydrocephalus,” “mechanical complication of nervous system device, implant or graft” (which includes ventricular shunt complications) and “epilepsy, unspecified, without mention of intractable epilepsy” listed as primary diagnosis in 7.3%, 3.6%, 2.6%, and 1.6% of records, respectively. Approximately 27.4% of cysticercosis-related in-hospital deaths included a diagnosis of “obstructive hydrocephalus.”
Discussion
These findings show a substantial burden of cysticercosis-related hospitalizations in the United States and suggest that the impact of this parasitic disease may be greater than is currently appreciated, with all regions of the country impacted. Although in-hospital case fatality was low, a substantial number of deaths were reported.
Our results reinforce previous findings of the typical demographic features of those hospitalized with a diagnosis of cysticercosis.2,9–16,30 Estimated hospitalization frequencies and rates were highest for Hispanics, which is consistent with previous studies, likely reflecting immigration from endemic areas.2,9–16,30 Though Hispanics accounted for the majority of hospitalizations, there were also significant numbers of cases in other racial/ethnic groups, which underscores that physicians should consider a diagnosis of cysticercosis in any individuals reporting symptoms consistent with illness, regardless of race/ethnicity or travel history. The gender distribution of hospitalizations observed is consistent with previous studies showing higher proportions of male cases than females with cysticercosis.2,10,12,30 The mean age and age distribution of hospitalizations is also similar to that reported in previous studies on NCC hospitalizations, showing the highest proportion of cases in early-mid adulthood.2,12 Because the largest number of hospitalizations were of Hispanic race/ethnicity, the observed age and sex distribution may be attributed in part to higher rates of immigration of young adult males in search of employment.18
As expected, the highest number of hospitalizations and hospitalization rates were observed in the West of the country, however there were considerable numbers of hospitalizations found in the South, Northeast, and Midwest during the 14-year study period. The majority of published reports on cysticercosis in the United States have been from the southwestern states, particularly Texas and California.8–11,15,17 These areas tend to have high populations of immigrants from endemic countries, particularly Latin America, where the prevalence of cysticercosis is found to be particularly high.8–11,15,17 Although resources and education campaigns should be prioritized for these areas of higher prevalence, results from this and other studies indicate that prevention/control efforts should not be overlooked in regions not typically thought of as high risk.13,14,16,21
Few studies have examined institutional characteristics of hospitals most frequently reporting cysticercosis-related hospitalizations. The higher proportion of cysticercosis-related hospitalizations observed in hospitals in urban locations, those designated as teaching hospitals, and those classified as large in terms of bed size likely reflects the concentration of immigrants in major cities and possible referral of patients from smaller hospitals and rural areas. Increased physician training in such hospitals regarding proper diagnostic tools and appropriate treatment strategies for various types of cysticercosis may help to reduce the impact of disease, as hospital physicians play critical roles in secondary and tertiary prevention.2
Although the NIS is a large, population-based national data source, our findings should be interpreted with caution because of several limitations. The NIS does not record information about immigration, travel history, country of birth/residence, or behavioral characteristics.2,15,30 The ICD-9-CM coding used for disease diagnosis was not necessarily designed to track infection prevalence and has been previously criticized as clinically imprecise, potentially leading to erroneously classified cases and non-cases.31 As the NIS contains no personal identification codes in the discharge records, it was also impossible to tell whether records were from hospitalizations of different patients. In a previous study conducted in California, multiple hospitalizations of the same patient within a year were found to account for between 16–20% of hospitalizations with a listed discharge diagnosis of cysticercosis.12 The lack of patient identifiers in records also prevents validation of diagnosis and patient characteristic information listed. Finally, several of the variables in the NIS data set included missing observations for a number of records, most notably for the variable race/ethnicity, missing in ∼16.3% of cysticercosis-related hospitalizations over the study period.
Our findings add to the growing recognition of the importance of cysticercosis in the United States and provide further insight into the nationwide burden of this disease.32 However, hospitalizations reported in these results capture only a portion of the disease burden and do not reflect cases diagnosed and treated in emergency departments, outpatient settings, long-term care facilities, or those who go undiagnosed. Currently, cysticercosis is not a reportable condition in most states and very few surveillance programs have been implemented.5,11 In the absence of effective surveillance and adequate reporting of disease, the true burden of cysticercosis is difficult to define.
Consideration should be given for the compulsory national reporting of cysticercosis cases in the United States.2,5,32,33 The increasingly widespread use of electronic records and ready transfer of such records to health departments may help in efforts to improve the efficiency of disease reporting, though challenges in disease identification remain an obstacle. Once appropriate surveillance systems are in place to detect cases of cysticercosis, limited resources can be prioritized to areas most in need of control efforts, including screening and treatment of the adult tapeworm in cysticercosis cases and contacts preventing potential further transmission of cysticercosis.5 Given that most of the cysticercosis cases in the United States are identified among immigrants from endemic countries, additional support for cysticercosis elimination efforts in these populations should be provided.2,5 If effective prevention campaigns are not implemented in endemic countries, the number of cases observed in the United States may remain steady or increase. Physicians should consider a diagnosis of cysticercosis in any patient with sudden onset seizures or other neurological symptoms consistent with NCC, particularly within immigrant populations from endemic regions.
Disclaimer: The authors declare no form of conflicting financial support was used for this study and the authors have no conflicts of interest to report.
Footnotes
Authors' addresses: Kaitlin A. O'Keefe, Department of Health Sciences, California State University, Northridge, CA, E-mail: kaitlin.okeefe@csun.edu. Mark L. Eberhard and Patricia Wilkins, Division of Parasitic Diseases and Malaria, Centers for Disease Control and Prevention, NE, Atlanta, GA, E-mails: mle1@cdc.gov and pma1@cdc.gov. Shira C. Shafir, Lawrence R. Ash, and Frank J. Sorvillo, Department of Epidemiology, Fielding School of Public Health, University of California, Los Angeles, CA, E-mails: sshafir@ucla.edu, larryash@ucla.edu, and fsorvill@ucla.edu.
References
- 1.García HH, Gonzalez AE, Evans CA, Gilman RH. Cysticercosis Working Group in Peru Taenia solium cysticercosis. Lancet. 2003;362:547–556. doi: 10.1016/S0140-6736(03)14117-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallin MT, Kurtzke JF. Neurocysticercosis in the United States: review of an important emerging infection. Neurology. 2004;63:1559–1564. doi: 10.1212/01.wnl.0000142979.98182.ff. [DOI] [PubMed] [Google Scholar]
- 3.Faust EC, Russell PF, Jung RC. Craig and Faust's Clinical Parasitology. Eighth edition. Philadelphia, PA: Lea & Febiger; 1970. [Google Scholar]
- 4.Ash LR, Orihel TC. Parasites in Human Tissues. Chicago, IL: ASCP Press; 1995. pp. 304–306. [Google Scholar]
- 5.Sorvillo F, Wilkins P, Shafir S, Eberhard M. Public health implications of cysticercosis acquired in the United States. Emerg Infect Dis. 2011;17:1–6. doi: 10.3201/eid1701.101210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorvillo FJ, Portigal L, DeGiorgio C, Smith L, Waterman SH, Berlin GW, Ash LR. Cysticercosis-related deaths, California. Emerg Infect Dis. 2004;10:465–469. doi: 10.3201/eid1003.020749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schantz PM, Moore AC, Munoz JL, Hartman BJ, Schaefer JA, Aron AM, Persaud D, Sarti E, Wilson M, Flisser A. Neurocysticercosis in an Orthodox Jewish community in New York City. N Engl J Med. 1992;327:692–695. doi: 10.1056/NEJM199209033271004. [DOI] [PubMed] [Google Scholar]
- 8.Richards FO, Jr, Schantz PM, Ruiz-Tiben E, Sorvillo FJ. Cysticercosis in Los Angeles County. JAMA. 1985;254:3444–3448. [PubMed] [Google Scholar]
- 9.del la Garza Y, Graviss EA, Daver NG, Gambarin KJ, Shandera WX, Schantz PM, White AC., Jr Epidemiology of neurocysticercosis in Houston, Texas. Am J Trop Med Hyg. 2005;73:766–770. [PubMed] [Google Scholar]
- 10.Serpa JA, Graviss EA, Kass JS, White AC., Jr Neurocysticercosis in Houston, Texas: an update. Medicine (Baltimore) 2011;90:81–86. doi: 10.1097/MD.0b013e318206d13e. [DOI] [PubMed] [Google Scholar]
- 11.Sorvillo FJ, Waterman SH, Richards FO, Schantz PM. Cysticercosis surveillance: locally acquired and travel-related infections and detection of intestinal tapeworm carriers in Los Angeles County. Am J Trop Med Hyg. 1992;47:365–371. doi: 10.4269/ajtmh.1992.47.365. [DOI] [PubMed] [Google Scholar]
- 12.Croker C, Redelings M, Reporter R, Sorvillo F, Mascola L, Wilkins P. The impact of neurocysticercosis in California: a review of hospitalized cases. PLoS Negl Trop Dis. 2012;6:e1480. doi: 10.1371/journal.pntd.0001480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Townes JM, Hoffman CJ, Kohn MA. Neurocysticercosis in Oregon, 1995–2000. Emerg Infect Dis. 2004;10:508–510. doi: 10.3201/eid1003.030542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Neal S, Noh J, Wilkins P, Keene W, Lambert W, Anderson J, Compton Luman J, Townes J. Taenia solium tapeworm infection, Oregon, 2006–2009. Emerg Infect Dis. 2011;17:1030–1036. doi: 10.3201/eid1706.101397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shandera WX, White AC, Jr, Chen JC, Diaz P, Armstrong R. Neurocysticercosis in Houston, Texas. A report of 112 cases. Medicine (Baltimore) 1994;73:37–52. doi: 10.1097/00005792-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Ong S, Talan DA, Moran GJ, Mower W, Newdow M, Tsang VC, Pinner RW. EMERGEncy ID NET Study Group Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis. 2002;8:608. doi: 10.3201/eid0806.010377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeGiorgio C, Pietsch-Escueta S, Tsang V, Corral-Leyva G, Ng L, Medina MT, Astudillo S, Padilla N, Leyva P, Martinez L, Noh J, Levine M, del Villasenor R, Sorvillo F. Sero-prevalence of Taenia solium cysticercosis and Taenia solium taeniasis in California, USA. Acta Neurol Scand. 2005;111:84–88. doi: 10.1111/j.1600-0404.2005.00373.x. [DOI] [PubMed] [Google Scholar]
- 18.Sorvillo FJ, DeGiorgio C, Waterman SH. Deaths from cysticercosis in the United States. Emerg Infect Dis. 2007;13:230–235. doi: 10.3201/eid1302.060527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Croker C, Reporter R, Mascola L. Use of statewide hospital discharge data to evaluate the economic burden of neurocysticercosis in Los Angeles County (1991–2008) Am J Trop Med Hyg. 2010;83:106–110. doi: 10.4269/ajtmh.2010.09-0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O'Neal SE, Townes JM, Wilkins PP, Noh JC, Lee D, Rodriguez S, Garcia HH, Stauffer WM. Seroprevalence of antibodies against Taenia solium cysticerci among refugees resettled in United States. Emerg Infect Dis. 2012;18:431–438. doi: 10.3201/eid1803.111367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenfeld EA, Byrd SE, Shulman ST. Neurocysticercosis among children in Chicago. Clin Infect Dis. 1996;23:262–268. doi: 10.1093/clinids/23.2.262. [DOI] [PubMed] [Google Scholar]
- 22.Cantey PT, Coyle CM, Sorvillo FJ, Wilkins PP, Starr MC, Nash TE. Neglected parasitic infections in the United States: cysticercosis. Am J Trop Med Hyg. 2014;90:805–809. doi: 10.4269/ajtmh.13-0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Healthcare Cost and Utilization Project (HCUP) Overview of the Nationwide Inpatient Sample (NIS) Rockville, MD: Agency for Healthcare Research and Quality; 2011. http://www.hcup-us.ahrq.gov/nisoverview.jsp Available at. Accessed July 2013. [PubMed] [Google Scholar]
- 24.Healthcare Cost and Utilization Project (HCUP) Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2009. Rockville, MD: Agency for Healthcare Research and Quality; 2011. http://www.hcupus.ahrq.gov/db/nation/nis/NIS_Introduction_2009.jsp Available at. Accessed June 2013. [Google Scholar]
- 25.Healthcare Cost and Utilization Project (HCUP) Description of Data Elements, Nationwide Inpatient Sample Hospital Weights File. Rockville, MD: Agency for Healthcare Research and Quality; 2002. [Google Scholar]
- 26.Barrett M, Lopez-Gonzalez L, Coffey R, Levit K. Population Denominator Data for Use with the HCUP Databases (Updated with 2012 Population data) 2013. http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp HCUP Methods Series Report # 2013-01 ONLINE. U.S. Agency for Healthcare Research and Quality. Available at. Accessed June 2013. [Google Scholar]
- 27.United States Census Bureau . Resident Population Estimates of the United States by Sex, Race, and Hispanic Origin: April 1, 1990 to July 1, 1999, with Short-Term Projection to November 1, 2000. http://www.census.gov/popest/data/national/totals/ 1990s/tables/ nat-srh.txt Available at. Accessed May 2013. [Google Scholar]
- 28.United States Census Bureau . National Intercensal Estimates (2000–2010) http://www.census.gov/popest/data/intercensal/national/nat2010.html Available at. Accessed May 2013. [Google Scholar]
- 29.HCUPnet . Healthcare Cost and Utilization Project (HCUP), 1998–2011. Rockville, MD: Agency for Healthcare Research and Quality; http://hcupnet.ahrq.gov/ Available at. Accessed September, 2014. [PubMed] [Google Scholar]
- 30.Ehnert KL, Roberto RR, Barrett L, Sorvillo FJ, Rutherford GW III. Cysticercosis: first 12 months of reporting in California. Bull Pan Am Health Organ. 1992;26:165–172. [PubMed] [Google Scholar]
- 31.Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, Lapetina E, Gemmen E. The burden of Staphylococcus aureus infections on hospitals in the United States: an analysis of the 2000 and 2001 Nationwide Inpatient Sample Database. Arch Intern Med. 2005;165:1756–1761. doi: 10.1001/archinte.165.15.1756. [DOI] [PubMed] [Google Scholar]
- 32.Del Brutto OH, García HH. Neurocysticercosis in nonendemic countries: time for a reappraisal. Neuroepidemiology. 2012;39:145–146. doi: 10.1159/000341693. [DOI] [PubMed] [Google Scholar]
- 33.Roman G, Sotelo J, Del Brutto OH, Flisser A, Dumas M, Wadia N, Botero D, Cruz M, Garcia H, de Bittencourt PR, Trelles L, Arriagada C, Lorenzana P, Nash TE, Spina-França A. A proposal to declare neurocysticercosis an international reportable disease. Bull World Health Organ. 2000;78:399–406. [PMC free article] [PubMed] [Google Scholar]