Abstract
To investigate arbovirus transmission in North Dakota, we collected and screened mosquitoes for viral infection by Vero cell culture assay. Seven viruses were isolated from 13 mosquito species. Spatial and temporal distributions of the important vectors of West Nile virus (WNV), Cache Valley virus, Jamestown Canyon virus (JCV), and trivittatus virus are reported. Snowshoe hare virus, Potosi virus, and western equine encephalomyelitis virus were also isolated. The risks of Culex tarsalis and Aedes vexans transmitting WNV to humans were 61.4% and 34.0% in 2003–2006, respectively, but in 2003 when the largest epidemic was reported, risks for Ae. vexans and Cx. tarsalis in Cass County were 73.6% and 23.9%, respectively. Risk of humans acquiring an infectious bite was greatest from about the second week of July through most of August. West Nile virus sequences were of the WN02 genotype. Most JCV strains belonged to a single clade of genetically related strains. Cache Valley virus and JCV were prevalent during August and early September and during July and August, respectively.
Introduction
Five arboviruses have been reported from North Dakota mosquitoes. Two of these viruses caused significant epidemics and epizootics in humans and in horses. Western equine encephalomyelitis virus (WEEV; Togaviridae: Alphavirus) infected 1,180 humans and caused 96 deaths in 1941.1 Sixty-one years later in 2002, West Nile virus (WNV; Flaviviridae: Flavivirus) was introduced into North Dakota and caused disease in 17 humans and 577 horses followed by 617 human cases, five human deaths, and 42 equine cases during 2003.2 Since then, North Dakota has reported human WNV cases every year and has one of the highest incidence rates of neuroinvasive disease in the country.2,3 Other arboviruses identified in North Dakota include St. Louis encephalitis virus (SLEV; Flaviviridae: Flavivirus),4 Cache Valley virus (CVV; Bunyaviridae: Orthobunyavirus),4 and trivittatus virus (TVTV; Bunyaviridae: Orthobunyavirus).4 Jamestown Canyon virus (JCV; Bunyaviridae: Orthobunyavirus), which has one of the widest geographical ranges in North America of the California serogroup of viruses, surprisingly, has previously not been documented in North Dakota.4
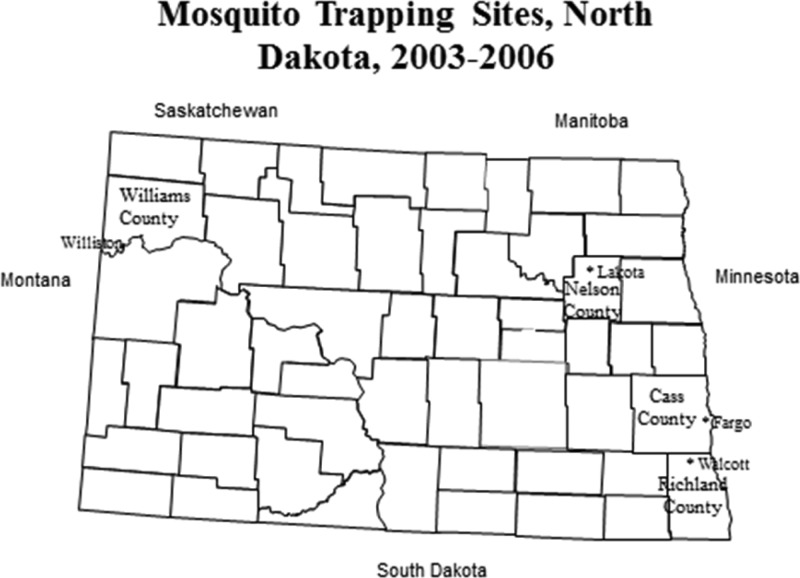
After the first report of WNV in North Dakota in 2002,2 we established a mosquito and virus surveillance program in and around the eastern city of Fargo (Cass County) and near the town of Walcott (Richland County) in 2003–2005, and in the northwestern city of Williston in 2004–2006 (Williams County) (Figure 1). Additionally, collections were made for 3 days in July 2003 in the rural town of Lakota (Nelson County). Our objectives were to conduct an in-depth study of mosquitoes and their viruses throughout the spring and summer in selected locations in North Dakota. We report the isolation of seven viruses from 13 species of mosquitoes, the spatial and temporal distributions of the important vectors of the most abundant arboviruses, the relative risk of mosquito vectors in transmitting WNV to humans, the correlation of temporal numbers of human cases of WNV with mosquito abundance and infection rate, and a genetic analysis of WNV and JCV isolates from different mosquito species, years of isolation, and geographic locations.
Figure 1.
North Dakota Counties where mosquito traps were placed.
Materials and Methods
Mosquito collections and identification.
Trapping of mosquitoes was done in Cass County in 2003–2005 and in Williams County in 2004–2006 (Figure 1). Fargo (46°52′38″N/96°47′21″W), a city of 110,000 people, is the county seat in Cass County and is located on the western side of the Red River, which runs along the North Dakota-Minnesota border. Williston (48°08′49″N/103°37′05″W), a city of about 18,000 inhabitants, is the county seat in Williams County and is situated along the Missouri River near the North Dakota-Montana border. Mosquitoes were also collected in 2003 in Nelson County in the vicinity of Lakota, the county seat. Lakota (48°02″34″N/98°20′10″W) is an agricultural community with < 700 inhabitants and is located in the northwestern portion of the county. Trapping in Lakota was discontinued after 3 nights because of inability to consistently obtain dry ice to supplement the traps. Mosquitoes were collected near Walcott (46°32′52″N/96°56′19″W) in Richland County, which is adjacent to the southern border of Cass County, in 2003–2005 (Figure 1). Trapping was carried out from July 4 to September 26, June 8 to October 6, May 24 to September 29, June 8 to September 7 in 2003, 2004, 2005, and 2006, respectively.
In 2003, five distinct trapping sites were established northeast (two sites in Argusville, near the Sheyenne River (47°03′08″N/96°20′10″W)) and southwest (three sites in Horace (46°45′32″N/96°54′13″W) of Fargo and one site near Walcott. Trapping was not done in Fargo because of an extensive mosquito control program initiated on the day traps were first placed in the field. Traps were often placed weekly at each location. Traps were set for 1 to 2 nights at 10 different locations near Lakota.
In 2004 and 2005, the same six trapping sites northeast and southwest of Fargo were continued. Three additional sites were established in Horace. Seven different geographically different sites were established within the City of Fargo in 2004 and 2005.
In 2004–2006, mosquitoes were trapped at six different locations immediately around Williston, ND. An additional site was trapped in 2004 and 2005. Trapping was not done within the city because of relatively frequent spraying of insecticides for the control of mosquitoes.
Mosquitoes were collected with Centers for Disease Control and Prevention (CDC) miniature light traps baited with dry ice (model 512; John W. Hock Co., Gainesville, FL).5 Traps were placed about 0.9 m off the ground in the afternoon or evening and collected the following morning. Mosquitoes were knocked down in the field or laboratory with dry ice or freezing temperatures, aspirated, and transferred into a 17 × 55 mm flat-bottomed shell vial that was sealed with a rubber stopper. Three layers of water and gas-proof tape were used to seal the juncture of the rubber stopper and vial. The vial was appropriately labeled and immediately stored on dry ice or in a −80°C freezer until packaged in dry ice within a Styrofoam shipping container and sent by overnight mail to The Connecticut Agriculture Experiment Station (CAES). Mosquitoes were stored at CAES in a −80°C freezer until processing. Extremely large collections were placed in 0.47 L or 0.24 L Mason jars that were sealed with three layers of water and gas-proof tape.
Mosquitoes were identified to species.6,7 Specimens were placed on a cold platform and, with the aid of a dissecting microscope, each specimen was identified. Mosquitoes were placed into pools according to species, date, and trap location. Pools contained from 1 to 50 mosquitoes. After identification and pooling, mosquitoes were kept on regular ice until attempted isolation of virus on the same day.
Virus isolation.
Mosquitoes were ground in 0.5 to 1.25 mL of phosphate-buffered saline containing 0.5% gelatin, 30% rabbit serum, and 1% 100× antibiotic-antimycotic (10,000 units μg/mL of streptomycin sulfate, and 25 μg/mL of amphotericin B, Invitrogen, Carlsbad, CA, in 0.85% saline). Mosquitoes and saline were placed in a 2.5 mL plastic centrifuge vial containing a copper BB pellet. A Vibration Mill MM 300 (Retsch Laboratory, Irvine, CA) set at 30 cycles per second and operated for 4 minutes was used inside a biosafety hood to macerate mosquitoes.
After centrifugation at 4°C for 7 minutes at 520 × g, a 100 μL sample of supernatant was placed onto a monolayer of Vero cells, growing in 4 mL of Minimum Essential Medium containing fetal bovine serum, glutamine, and antibiotic-antimycotic (Invitrogen), set up the day before in a 25-cm2 flask kept in a 5% CO2 incubator set at 37°C. Growth medium in each flask was decanted before addition of the inoculum. The flask was rocked for 5 minutes before 4 mL of new growth medium was added to the flask. After flasks were returned to the incubator, cells were examined for cytopathogenic effects (CPE) 3–7 d after inoculation.
Virus identification.
Many viral isolates were identified by virus-dilution serum constant-neutralization tests. Virus dilutions from 10−4 to 10−6 were incubated with a panel of hamster antisera (1:10) directed against JCV, La Crosse virus (LACV; Bunyaviridae, Orthobunyavirus), snowshoe hare virus (SSHV; Bunyaviridae, Orthobunyavirus), Keystone virus (KEYV; Bunyaviridae, Orthobunyavirus), CVV, Potosi virus (POV; Bunyaviridae, Orthobunyavirus), Jerry Slough virus (JSV; Bunyaviridae, Orthobunyavirus) or hyperimmune mouse ascetic fluids (1:10) against eastern equine encephalomyelitis virus (EEEV; Togaviridae: Alphavirus), Highlands J virus (HJV; Togaviridae: Alphavirus), TVTV, WEEV, or WNV for 1 hour at 37°C. The virus–serum mixtures were then assayed for neutralizing activity by infecting Vero cell cultures and screening them for CPE.8
West Nile virus also was identified by a TaqMan reverse transcriptase-polymerase chain reaction (RT-PCR) assay. The QIAamp viral RNA mini kit protocol (Qiagen, Valencia, CA) was used to extract RNA from a 70 μL sample of infectious Vero cell-growth medium. The RT-PCR protocol was used to identify isolates of WNV.9 The positive RNA control for WNV was from an isolate from Culiseta melanura (8094-01) that had been diluted 1:100. Its cycle threshold was 21 to 22. Double processed sterile water (Sigma, St. Louis, MO) was used as the negative control. Primers and probe for WNV used in the TaqMan RT-PCR assay were prepared by QIAGEN. Primers were WNENV-forward 1160-1180 (5′-TCAGCGATCTCTCCACCAAAG-3′) and WNENV-reverse 1229-1209 (5′-GGGTCAGCACGTTTGTCATTG-3′) with probe WNENV 1186-1207 (5′-TGCCCGACCATGGGAGAAGCTC-3′).9 The probe had the 5′ end labeled with FAM reporter dye and the 3′ end labeled with TAMRA quencher dye. Primers, probe, and viral RNA were added to the reagents in the TaqMan RT-PCR Ready-Mix Kit (PE Applied Biosystems, Branchburg, NJ). Each isolate was prepared for testing by adding 2.5 μL of viral RNA, 0.25 μL of 100 μM of each primer, 0.15 μL of 25 μM of probe, 12.5 μL of 2× buffer, 0.5 μL of RT-PCR enzyme, and 8.85 μL of water to a microcentrifuge tube for a total volume of 25 μL. Samples were amplified with a Smart Cycler that was run with Smart Cycler software (Cepheid, Sunnyvale, CA). Amplification included one cycle at 50°C for 20 min, one cycle at 95°C for 10 min, and 50 cycles at 95°C for 15 sec, and at 60°C for 60 sec. Isolates with a cycle threshold value of < 37 were identified as WNV.
Four Orthobunyavirus isolates (JCV, POTV, CVV, and TVTV) also were identified by RT-PCR. RNA was extracted from primary viral isolates using the viral RNA Kit (Qiagen), and RT-PCR was performed using the Titan One-Tube RT-PCR System (Roche Diagnostics, Indianapolis, IN). Primers BUNS+new: 5-TGACCAGTAGTGTACTCCAC-3_ and BUNS-new: 5_-CAAGCAGTAGTGTGCTCCAC-3_ that targeted the conserved terminal ends of the S-segment of the Orthobunyavirus genus were used as previously described.10,11 The amplification product of each unknown virus was digested with one or more of four restriction enzymes in separate reactions. The master mix for each restriction enzyme consisted of 13.55 μL of water, 2.0 μL 10× reaction buffer, 0.2 μL 100× BSA, and 0.25 μL of the specific restriction enzyme to which was added 4 μL of the amplified reagent and then incubated overnight at 37°C.
Each digestion product was separated on a 2% agarose gel and stained with ethidium bromide. The restriction enzymes used and their fragment sizes for specific viruses were as follows: EcoRV cut JCV at 364 bps and 627 bps, CAC81 severed POTV at 256 bps and 677 bps, Swal cut CVV at 411 bps and 539 bps, and Xhol cut TVTV at 233 bps and 740 bps.
Alternatively for isolates that could not be specifically identified using restriction enzymes or that were not identified by virus-dilution serum constant-neutralization tests, amplification products were purified using the PCR purification kit (Qiagen) and commercially sequenced at the DNA Analysis Facility (Yale University, New Haven, CT). Edited nucleotide sequences were compared with those available on GenBank using the Blastn search algorithm http://blast.ncbi.nlm.nih.gov/Blast.cgi.
Genetic analyses of West Nile virus.
The NS3 gene of WNV was selected for analysis because this gene was previously shown to have a strong phylogenetic signal.12 The RNA was extracted from primary viral isolates using the Viral RNA Kit (Qiagen). The RT-PCR was performed using the Titan One-Tube RT-PCR System (Roche Diagnostics, Indianapolis, IN) and primers WNV4532f (TCGCGATTAGTGCGTACACC) and WNV6516r (GAAGTGCTCAGGCATCTTTCC). Amplification was performed as follows: 1 cycle of 50°C for 30 min and 94°C for 2 min, 10 cycles of 94°C for 15 sec, 55°C for 30 sec, and 68°C for 2 min, followed by 25 cycles of 94°C for 15 sec, 55°C for 30 sec, and 68°C for 2 min + 5 sec per cycle, and 1 cycle of 68°C for 7 min. The PCR products (length = 1,984 bps) were commercially sequenced at the Yale DNA Analysis Facility and edited sequences were aligned using the ClustalW algorithm in MEGA 5.13 A phylogenetic tree was reconstructed by maximum-likelihood (ML) analysis in MEGA using the substitution model TN93 + G. The optimal nucleotide substitution model was identified after performing ML fits of 24 different models in MEGA. Support for individual nodes was obtained by performing 1,000 bootstrap replicates.
Genetic analyses of Jamestown Canyon, snowshoe hare, and trivittatus viruses.
The RNA was extracted from primary virus cultures, the S segment was amplified by RT-PCR, and amplification products were purified and sequenced according to previously described methods.14 A total of 48 sequences were combined with another 19 sequences available on GenBank and aligned using MEGA. The final alignment consisted of 832 characters that included the nucleocapsid open reading frame and flanking portions of the 5′ and 3′ non-coding regions. Phylogenetic analysis was performed by ML analysis as described earlier for WNV sequences except using a different substitution model (T92 + G+I) that was selected after performing ML fits in MEGA.
GenBank.
The WNV, JCV, SSHV, and TVTV edited nucleotide sequences were submitted to GenBank (accession nos. KM215518–KM215607).
Statistics.
The field infection rates for each species of mosquito infected with a specific virus within Cass, Richland, Nelson, or Williams Counties for each week and year was determined per 1,000 specimens using the bias-corrected maximum likelihood estimation method.15
Relative risk of infected vectors transmitting WNV to humans in North Dakota in 2003–2006 was assessed using information on mosquito abundance, infection rate, vector competence, and biting behavior.16 Relative abundance was determined by dividing the total numbers of a specific species captured during the 4-year study by the total number of mosquitoes collected and identified (Table 1). It is noteworthy that relative abundance was determined from numbers of mosquitoes captured in CDC miniature light traps placed relatively near the ground and may not reflect the abundance of specific species feeding on humans. Infection rate was determined using a previously published formula.15 Vector competence (fraction of infected mosquitoes that will transmit virus in a later feeding) was obtained from previously published studies on specific species. The fraction of blood meals of specific species that contained mammalian blood published by others was used as a relative estimate of the likelihood of the species feeding on humans. Humans shelter themselves from mosquitoes and have significantly less exposure to mosquitoes compared with wild and large domestic mammals. The use of the fraction of specimens feeding on mammals is a relative estimate of the approximation that a specific species would feed on humans.16 All mosquito species reported in this study feed on humans.
Table 1.
Thirteen mosquito species infected with virus,* North Dakota, 2003–2006
| Species | Number of specimens by year | Totals | Percent | |||
|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | |||
| Aedes cinereus | 0 | 593 | 5,867 | 218 | 6,678 | 0.2 |
| Aedes vexans | 223,693 | 519,443 | 1,477,623 | 591,152 | 2,811,911 | 83.2 |
| Anopheles earlei | 21 | 6 | 72 | 79 | 178 | < 0.1 |
| Coquillettidia perturbans | 1,021 | 1,574 | 2,199 | 246 | 5,040 | 0.2 |
| Culex tarsalis | 3,028 | 20,608 | 48,615 | 478 | 72,729 | 2.2 |
| Culiseta inornata | 983 | 6,336 | 21,566 | 508 | 29,393 | 0.9 |
| Ochlerotatus dorsalis | 2,511 | 15,279 | 36,953 | 1,375 | 56,118 | 1.7 |
| Ochlerotatus flavescens | 579 | 463 | 938 | 310 | 2,290 | 0.1 |
| Ochlerotatus melanimon | 403 | 8,381 | 35,559 | 46,306 | 90,649 | 2.7 |
| Ochlerotatus spencerii | 0 | 479 | 368 | 26 | 873 | < 0.1 |
| Ochlerotatus sticticus | 176 | 7,555 | 25,985 | 416 | 34,132 | 1.0 |
| Ochlerotatus triseriatus | 95 | 56 | 106 | 0 | 257 | < 0.1 |
| Ochlerotatus trivittatus | 16,017 | 94,904 | 135,873 | 12,757 | 259,551 | 7.7 |
| Other species* | 393 | 1,751 | 3,274 | 2,666 | 8,084 | 0.2 |
| Totals | 248,920 | 677,428 | 1,794,998 | 656,537 | 3,377,883 | |
Viruses were not isolated from 21 species; these species are not listed.
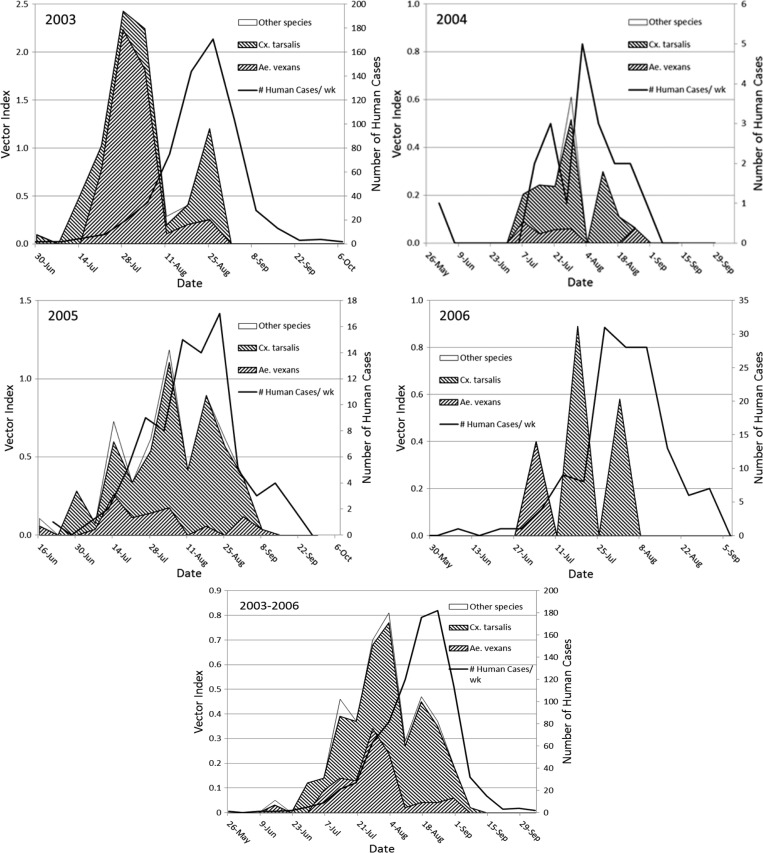
A vector index was used to correlate weekly numbers of documented WNV-infected humans with mosquito abundance and infection rate.17 Human cases were recorded as the number for a specific week and were plotted at the middle of that week (numbers were reported at the end of the week by the North Dakota Department of Health).18 The average numbers of a specific vector per trap-night per week were multiplied by its infection rate (IR)/1,000 to give the vector index, the average number of infected mosquitoes per trap-night.
Results
Mosquitoes.
A total of 3,377,883 specimens representing 34 species were collected and identified in 2003–2006 (Table 1). Data for mosquito species (N = 21) that did not yield virus are not included. Aedes vexans was dominate throughout the state and represented 83.2% of the specimens identified. Ochlerotatus trivittatus, Ochlerotatus melanimon, Culex tarsalis, and Ochlerotatus dorsalis made up 7.7%, 2.7%, 2.2%, and 1.7%, respectively.
Viruses.
Seven distinct viruses were identified among the 816 isolates (Table 2). Trivittatus virus (46.4%), WNV (22.8%), CVV (18.5%), and JCV (10.8%) were the most prevalent. Trivittatus virus was isolated from mosquitoes collected from June 2 through the week of October 6. The other viruses tended to be isolated from mosquitoes collected from mid to late June and early July through the second week of September. Potosi virus was an exception and was isolated during the weeks of August 18 through September 22.
Table 2.
Viruses isolated from mosquitoes collected in Nelson, Cass, Richland, and Williams Counties, North Dakota, 2003–2006
| Virus | Year and Counties | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | ||||||||
| Nelson | Cass | Richland | Cass | Richland | Williams | Cass | Richland | Williams | Williams | ||
| West Nile | 2 | 37 | 1 | 19 | 0 | 13 | 67 | 0 | 41 | 6 | 186 |
| Trivittatus | 0 | 35 | 11 | 85 | 1 | 14 | 123 | 4 | 73 | 33 | 379 |
| Jamestown Canyon | 5 | 11 | 1 | 10 | 0 | 1 | 14 | 0 | 44 | 2 | 88 |
| Cache Valley | 1 | 1 | 0 | 0 | 0 | 0 | 53 | 0 | 96 | 0 | 151 |
| Snowshoe Hare | 0 | 0 | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 0 | 4 |
| Western Equine Encephalomyelitis | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Potosí | 0 | 0 | 0 | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 6 |
| Total | 8 | 84 | 13 | 115 | 1 | 30 | 266 | 4 | 254 | 41 | 816 |
Viruses were isolated from 13 species of mosquitoes (Table 3). The largest numbers of viral isolations were from Oc. trivittatus (N = 313), Ae. vexans (N = 289), and Cx. tarsalis (N = 131). Six different viral species were isolated from Ae. vexans (CVV, JCV, POTV, SSHV, TVTV, and WNV). Five different viruses were isolated from Cx. tarsalis (CVV, JCV, TVTV, WNV, and WEEV), Oc. dorsalis (CVV, JCV, POTV, TVTV, and WNV), and Oc. trivittatus (CVV, JCV, SSHV, TVTV, and WNV). Four and three different viruses were isolated from Culiseta inornata (CVV, JCV, POTV, and WNV) and Ochlerotatus flavescens (CVV, JCV, and WNV).
Table 3.
Seven viruses isolated from 13 species of mosquitoes, North Dakota, 2003–2006
| Species | Viruses | |||||||
|---|---|---|---|---|---|---|---|---|
| Cache Valley | Jamestown Canyon | Potosi | Snowshoe Hare | Trivittatus | West Nile | Western Equine Encephalomyelitis | Total | |
| Aedes cinereus | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Aedes vexans | 92 | 58 | 4 | 3 | 77 | 55 | 0 | 289 |
| Anopheles earlei | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Coquillettidia perturbans | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Culex tarsalis | 4 | 2 | 0 | 0 | 2 | 121 | 2 | 131 |
| Culiseta inornata | 27 | 4 | 1 | 0 | 0 | 2 | 0 | 34 |
| Ochlerotatus dorsalis | 15 | 8 | 1 | 0 | 1 | 1 | 0 | 26 |
| Ochlerotatus flavescens | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 3 |
| Ochlerotatus melanimon | 6 | 2 | 0 | 0 | 1 | 0 | 0 | 9 |
| Ochlerotatus spencerii | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Ochlerotatus sticticus | 0 | 1 | 0 | 0 | 3 | 0 | 0 | 4 |
| Ochlerotatus triseriatus | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| Ochlerotatus trivittatus | 2 | 12 | 0 | 1 | 295 | 3 | 0 | 313 |
| Total | 151 | 88 | 6 | 4 | 379 | 186 | 2 | 816 |
West Nile virus.
This invasive Flavivirus was isolated in 2003–2006 from five genera and nine species collected in Nelson, Cass, Richland, and Williams Counties (Tables 2 and 3). The largest numbers of isolations were from Cx. tarsalis (N = 121) and Ae. vexans (N = 55). The WNV IR per thousand pooled mosquitoes for all species by year and county are shown in Supplemental Table 1. Culex tarsalis and Ae. vexans IRs by county and year ranged from 1.12 to 12.26 and < 0.01 to 0.19 per thousand specimens, respectively.
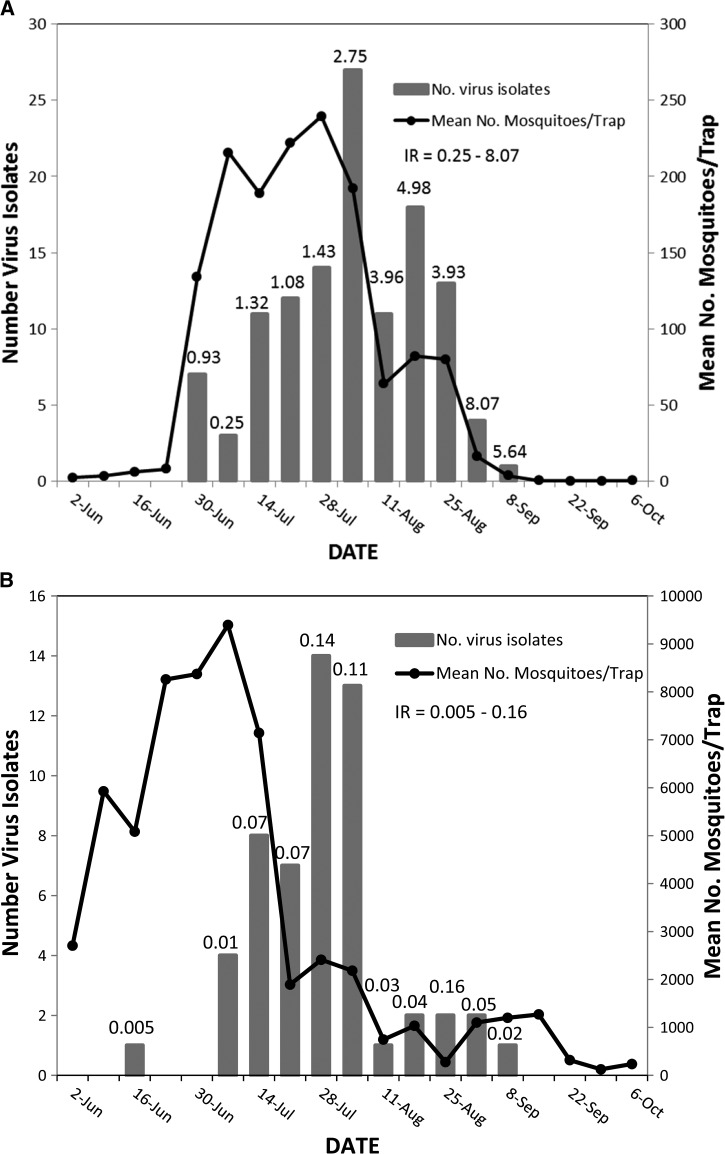
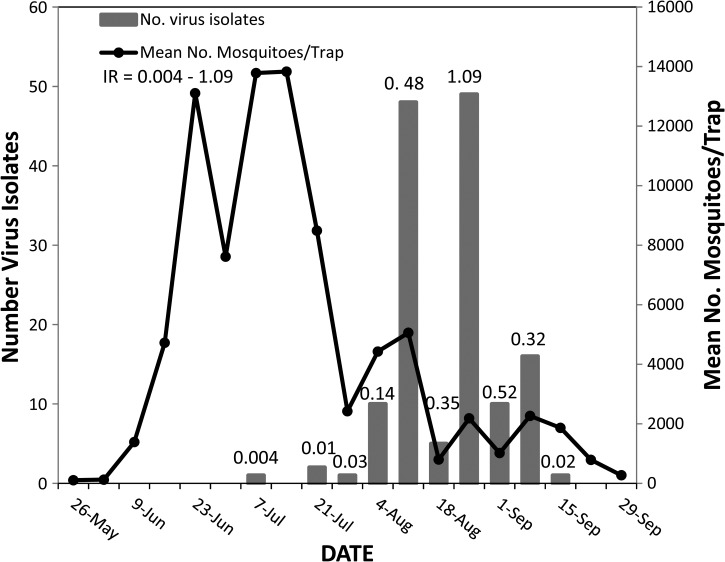
Culex tarsalis was collected from the first week of June into the first week of October (Figure 2A). Largest numbers were collected from the week June 30 through the week August 4 when numbers per trap-night averaged 134 to 239. West Nile virus was isolated from Cx. tarsalis from the last week of June through the second week of September. Eighty-eight percent of the isolations from Cx. tarsalis were made during a 7-week period from the week beginning July 14 through the week beginning August 25. The IRs for Cx. tarsalis tended to increase as the season progressed from 0.93 per thousand specimens on June 30 to 8.07 and 5.64 during the weeks of September 1 and 8.
Figure 2.
(A) Weekly number of West Nile virus isolations and infection rates (IR) relative to mean numbers of Culex tarsalis per trap-night, North Dakota, 2003–2006. (B) Weekly number of West Nile virus isolations and infection rates relative to mean numbers of Aedes vexans per trap-night, North Dakota, 2003–2006.
Aedes vexans averaging 2,705 per trap-night were collected during the week of June 2 and continued to be collected through the week of October 6 (Figure 2B). Populations averaged 5,083 to 9,394 specimens per trap-night from the week of June 16 through the week of July 14. Numbers averaged 1,270 per trap-night during the week of September 15. West Nile virus was first isolated from Ae. vexans during the week of June 16, but consistent isolations began during the week of July 7 and continued through the week of September 8. Eighty-four percent of the 55 isolations were obtained during a 5-week period from July 7 through the week of August 4.
Smaller numbers of isolations were made from Coquillettidia perturbans, Cs. inornata, Oc. dorsalis, Oc. flavescens, Oc. spencerii, Ochlerotatus triseriatus, and Oc. trivittatus (Table 3, Supplemental Table 1). West Nile virus was isolated from Oc. dorsalis during the week of June 16.
The risk of seven infected species for transmitting WNV to humans in North Dakota was assessed using a risk-assessment method, which used information on mosquito abundance, infection rate, vector competence, and biting behavior (Supplemental Table 2).16 The greatest seasonal risk of 61.4% was from Cx. tarsalis. The second largest risk was from Ae. vexans with a value of 34.0%. The risks of five other species were much lower, ≤ 1.8%.
We evaluated the importance of specific species on transmission of WNV in Cass County during the years of 2003–2005. Mosquitoes were trapped at the same five trapping sites during the 3 years when numbers of human cases in Cass County were 32, 0, and 12. The risks of the five species that were infected are shown in Supplemental Table 3. The largest number of human cases was in 2003 when the risks of being bitten by infected Ae. vexans and Cx. tarsalis were 73.6% and 23.9%. In 2004 and 2005, risks of being infected by Ae. vexans were 24.8% and 17.3% and by Cx. tarsalis were 61.3% and 76.6%, respectively, when numbers of human cases were 0 and 12. The IRs for Ae. vexans were 9.5 and 6.3 times greater in 2003 than in 2004 and 2005, respectively. The IRs for Cx. tarsalis were 5.6 and 2.6 times greater in 2003 than in 2004 and 2005. These data suggest that infected Ae. vexans participated in vectoring WNV in North Dakota in 2003 when 617 people were documented to have been infected.
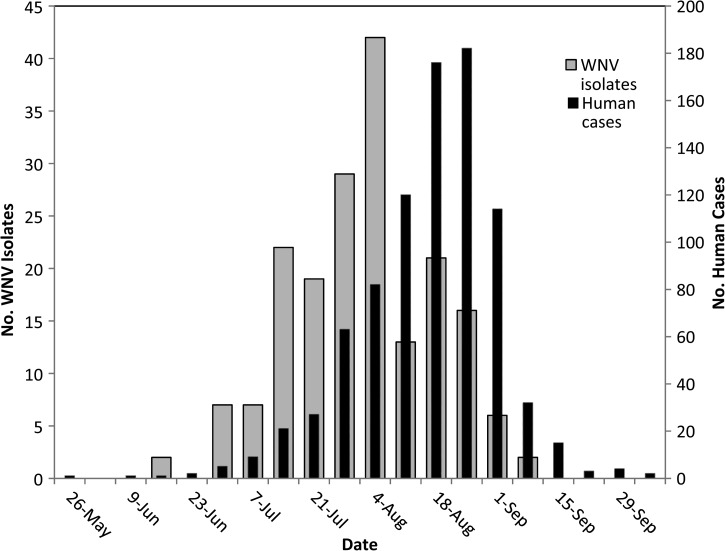
Dates of onset of humans infected with WNV and the weekly numbers of isolations of WNV from all mosquitoes for 2003–2006 are shown in Figure 3. The earliest human case was reported during the week of May 26 and the last cases were reported during the week of October 6. A steady increase in numbers of human cases began in mid-June and peaked during the last week of August with a 182 cases. West Nile virus was first isolated on June 16. Numbers of isolations increased from the last week of June through July and peaked on August 4, when 42 isolations were made, 2 to 3 weeks before the peaks of human cases. The decline of human cases beginning during the week of September 1 followed by 3 weeks the reduction in numbers of isolations that began during the week of August 11.
Figure 3.
Relation between onset of human disease and total number of West Nile virus isolates from all mosquito species, North Dakota, 2003–2006.
The weekly risk of humans being bitten by an infectious mosquito was also evaluated (Supplemental Table 4). The risks of being bitten by Cx. tarsalis were greater than being bitten by Ae. vexans and five other vector species during most weeks beginning in mid-July through August. However during this time period, the weekly risk of being bitten by infectious Ae. vexans plus the lesser important vectors varied from 10.3% to 57.8%.
We compared the weekly vector indexes for Cx. tarsalis, Ae. vexans, and the seven other vectors to the onset of human cases for 2003–2006 (Figure 4).17 The weekly vector index for all vectors exceeded two only in 2003 when the largest outbreak of West Nile fever erupted with 617 cases. The weekly vector indexes for Ae. vexans in 2003 were greater than indexes for Cx. tarsalis the last 2 weeks of July through the first week of August, and were similar during the second and third weeks of August (Figure 4, Supplemental Table 5). The vector index for all species combined in 2003 exceeded one during the third week of July and exceeded two during the last week of July and first week of August. The increasing onset of human disease of 75 to 171 cases per week lagged by about 2 to 3 weeks the increasing vector index. The weekly vector indexes in the years 2004–2006, when numbers of human cases varied from 20 to 137, exceeded one only in 1 week in 2005 (Figure 4, Supplemental Table 6–8). Cx. tarsalis had a higher weekly vector index compared with Ae. vexans during most weeks during these 3 years. The composite weekly vector indexes during 2003–2006 for Cx. tarsalis were similar to those for Ae. vexans plus the other vectors from the middle of June through the last week of July, but weekly vector indexes throughout August were higher for Cx. tarsalis (Figure 4, Supplemental Table 9).
Figure 4.
Stacked area graphs showing weekly vector index for Culex tarsalis, Aedes vexans, and seven other species relative to weekly numbers of human cases diagnosed with West Nile virus infection 2003, 2004, 2005, 2006, and 2003–2006. The other species were Coquillettidia perturbans, Culiseta inornata, Ochlerotatus dorsalis, Ochlerotatus flavescens, Ochlerotatus spencerii, Ochlerotatus triseriatus, and Ochlerotatus trivittatus.
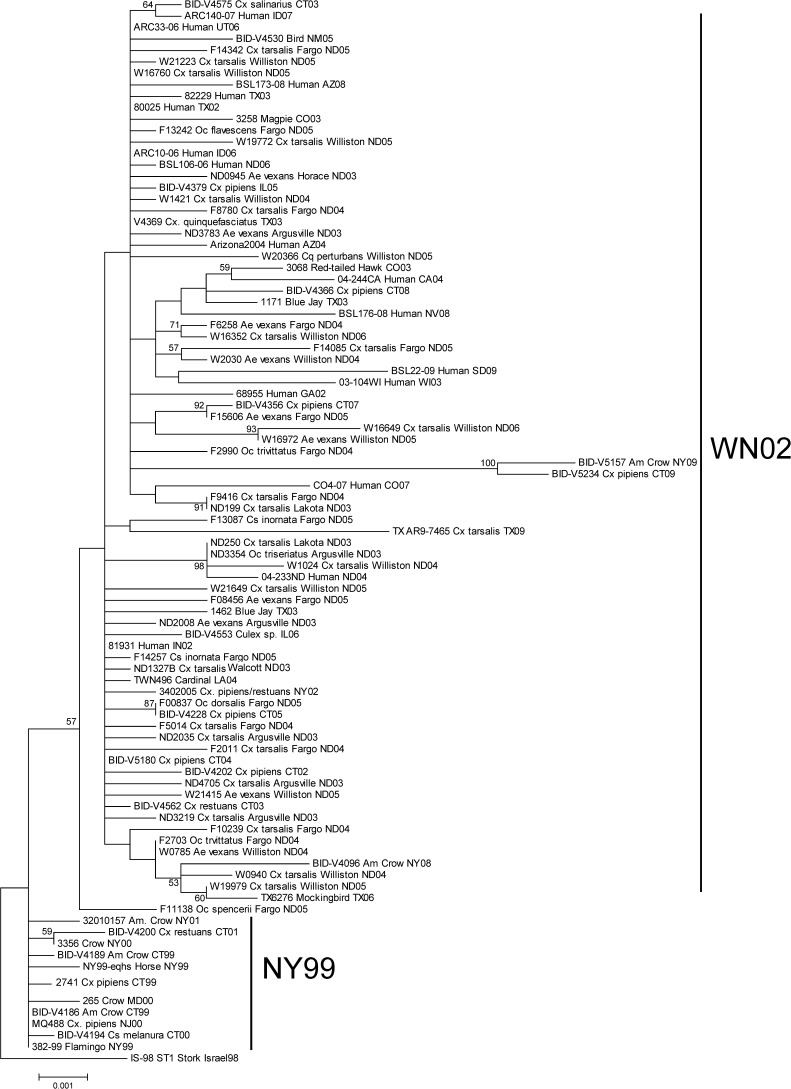
Figure 5 depicts the ML tree of WNV sequences from North Dakota. The overall topology is consistent with prior analyses and shows that viruses segregate into two major groups termed the NY99 and WN02 genotypes in North America.19,20 Earlier WNV isolates from the northeastern United States form the NY99 genotype, whereas later strains from North Dakota and the rest of the US cluster into the WN02 genotype.
Figure 5.
Phylogenetic tree depicting relationships of WNV isolates from North Dakota based on ML analysis of NS3 sequences. Branch lengths are proportional to the number of nucleotide substitutions. Numbers at node indicate bootstrap P values ≥ 50%.
Cache Valley virus.
This Bunyamwera serogroup virus of the genus Orthobunyavirus was isolated from mosquitoes captured in 2003 and 2005 but not in 2004 and 2006 (Table 2). Single pools of Cs. inornata collected on July 4 in Nelson County and of Oc. trivittatus collected on July 22 in Cass County yielded positive Vero cell cultures in 2003. In 2005, CVV was widespread and prevalent in both eastern (Cass County) and western (Williams County) North Dakota. Pools from five genera and nine species were positive for CVV (Table 3). The largest numbers of isolations were from Ae. vexans (N = 92), Cs. inornata (N = 27), and Oc. dorsalis (N = 15). The IRs for each species by year and county are shown in Supplemental Table 10 and ranged from 0.03 in Oc. trivittatus to 16.55 in Anopheles earlei in Williams County, and from 0.04 in Ae. vexans to 1.94 in Cs. inornata in Cass County. Ninety-seven percent of the isolations were made during the weeks of August 1 through September 8 (Figure 6). The weekly IRs were relatively high during this 6-week period, ranging from 0.14 to 1.09. Most isolations of CVV were made in August and early September when mosquito populations were significantly reduced from mid-June through mid-July.
Figure 6.
Weekly numbers of Cache Valley virus isolations and infection rates (IR) relative to the mean number per trap-night of Aedes vexans, Aedes cinereus, Anopheles earlei, Culex tarsalis, Culiseta inornata, Ochlerotatus dorsalis, Ochlerotatus flavescens, Ochlerotatus melanimon, and Ochlerotatus trivittatus, North Dakota, 2005.
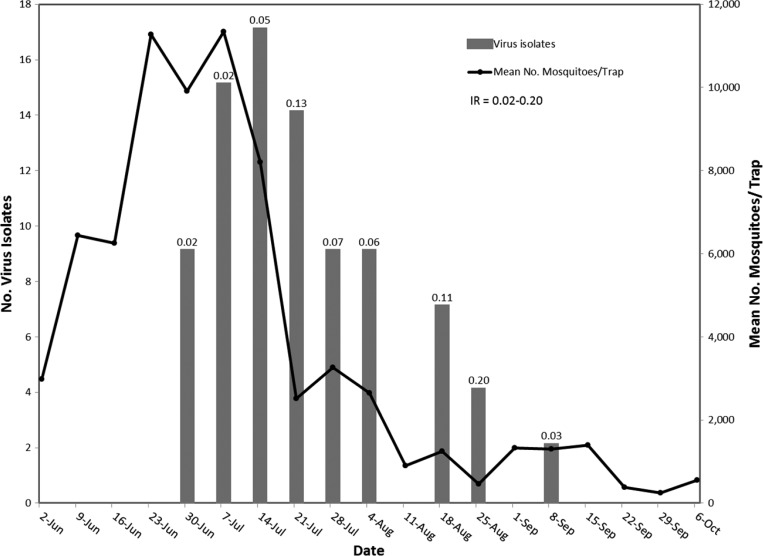
Jamestown Canyon virus.
This widely distributed Orthobunyavirus in the United States was isolated in 2003–2006 from mosquitoes captured in four counties (Table 2). Eighty-eight isolations were made from four genera and eight species (Table 3). The largest numbers of isolations were from Ae. vexans (N = 58), Oc. trivittatus (N = 12), and Oc. dorsalis (N = 8) (Table 3). The IRs for year and county ranged from 0.01–0.08, 0.02–0.51, and 0.07–1.21 for Ae. vexans, Oc. trivittatus, and Oc. dorsalis, respectively (Supplemental Table 11). Isolations were made from mosquitoes collected from the week of June 30 through the week of September 8 (Figure 7). Ninety-eight percent of the isolations were from mosquitoes collected from the week of June 30 through the week beginning August 25.
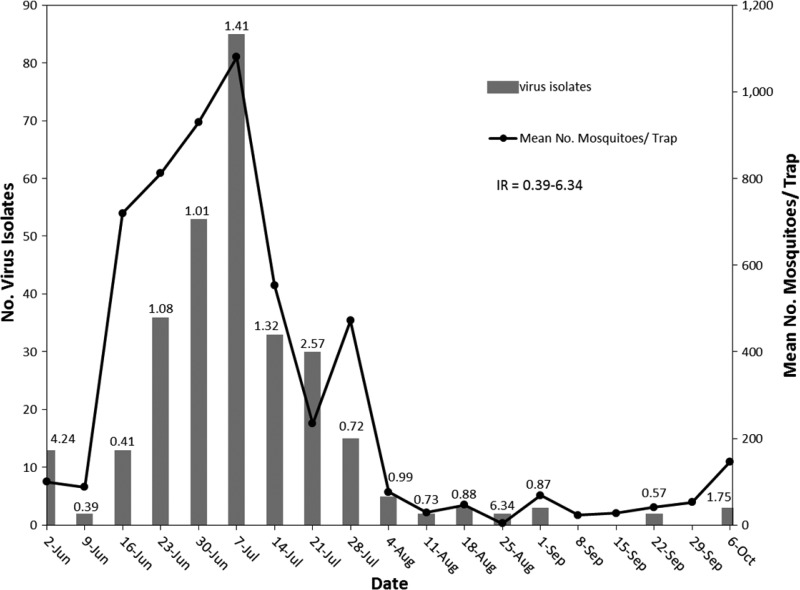
Figure 7.
Weekly numbers of Jamestown Canyon virus isolations and infection rates (IR) relative to the mean number per trap-night of Aedes vexans, Culex tarsalis, Culiseta inornata, Ochlerotatus dorsalis, Ochlerotatus flavescens, Ochlerotatus melanimon, Ochlerotatus sticticus, and Ochlerotatus trivittatus, North Dakota, 2003–2006.
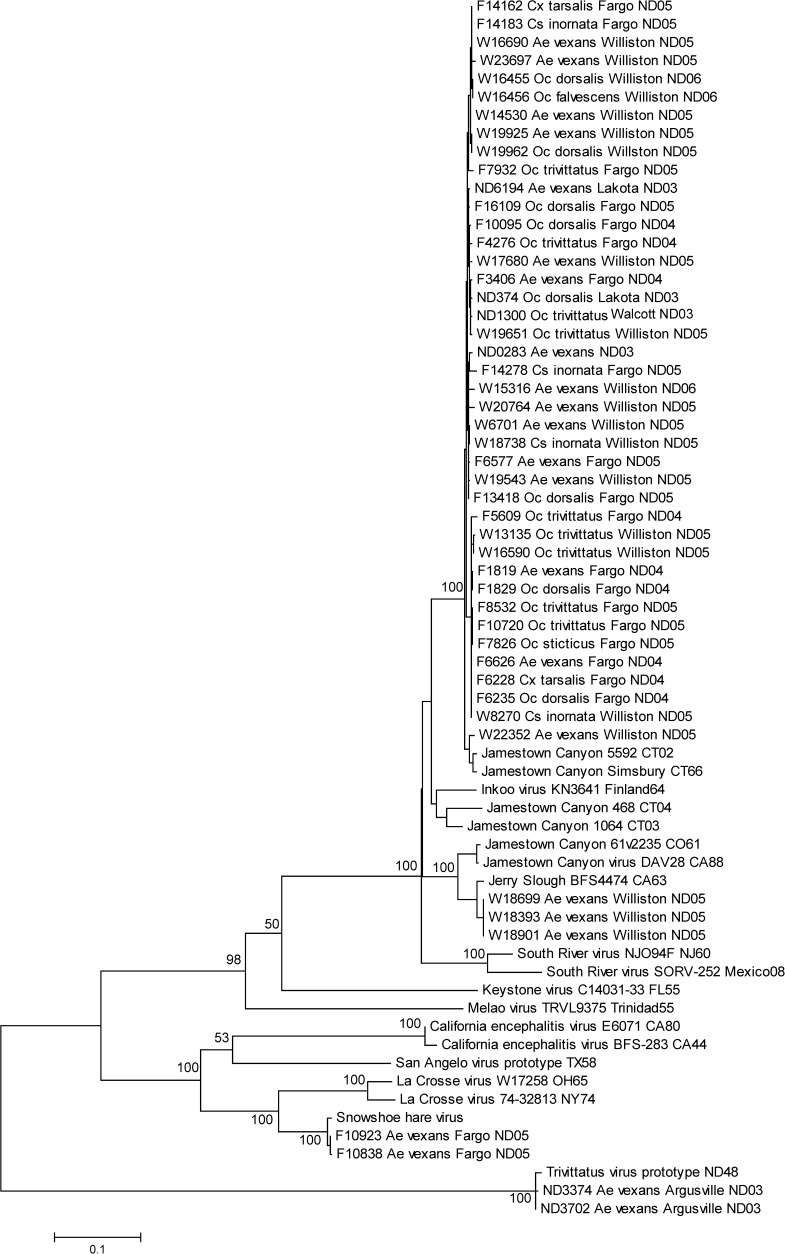
Phylogenetic analysis of 44 isolates of JCV showed that the vast majority belonged to a single clade of genetically related strains (Figure 8). Forty-one isolates from seven species, four different counties, and four different years were similar to the lineage A isolates from Connecticut.14 Three isolates sorted by phylogenetic analysis and by virus-dilution serum constant-neutralization tests were the Jerry Slough variant of JCV.
Figure 8.
Phylogenetic tree showing relationships of Jamestown Canyon, snowshoe hare, and trivittatus viruses from North Dakota based on ML analysis of S-segment nucleotide sequences. Branch lengths are proportional to the number of nucleotide substitutions. Bootstrap P values ≥ 50% are given only at major nodes for clarity.
Trivittatus virus.
This California encephalitis virus was the most frequently isolated virus (Table 2). The 379 isolates were from three genera and six species collected in Cass, Williams, and Richland Counties in 2003–2006 (Table 3). Two-hundred ninety-five and 77 of the isolates were from Oc. trivittatus and Ae. vexans, respectively. The IRs for Ochlerotatus trivittatus and Ae. vexans by year and county ranged from 0.70 to 5.09 and 0.01 to 0.42, respectively (Supplemental Table 12).
Virus was isolated from Oc. trivittatus from early June to early October in 2003–2006 (Figure 9). Ninety-seven percent of the isolates were from early June through the week of August 4. Weekly IRs was equal to or > 0.39. No isolates were obtained during the weeks of September 8, 15, and 29. One pool of 50 specimens was dually infected with TVTV and WNV.
Figure 9.
Weekly numbers of trivittatus virus isolations and infections rates (IR) relative to the mean number per trap-night of Ochlerotatus trivittatus, North Dakota, 2003–2006.
Aedes vexans infected with TVTV were collected from June 8 through August 5. Two isolates from Ae. vexans were shown by phylogenetic analysis to be similar to the prototype strain isolated from Oc. trivittatus and distinctly different from JCV (Figure 8).21
Western equine encephalomyelitis virus.
This native Alphavirus was isolated from two pools of Cx. tarsalis collected on August 3 and August 10, 2004 in Williams County (Tables 2 and 3). The IR was 0.30 (Supplemental Table 13).
Snowshoe hare virus.
This California encephalitis virus was isolated in Cass County from one pool of Oc. trivittatus collected on July 1, 2004 and from three pools of Ae. vexans collected on July 13, 2005 (Tables 2 and 3, Supplemental Table 13). The IR for both species was 0.01. Two isolates from Ae. vexans were phylogenetically similar to the snowshoe hare virus (Figure 8).
Potosi virus.
This Orthobunyavirus was isolated from three species collected in Cass County from August 22 through September 28, 2005 (Table 2 and 3, Supplemental Table 13). Four isolations were from Ae. vexans (IR = 0.01). Single isolations were from Oc. dorsalis (IR = 0.04) and from Cs. inornata (IR = 0.08).
Discussion
Seven species of viruses circulated among 13 species of North Dakota mosquitoes during 2003–2006 (Tables 2 and 3). Five of the viruses cause human disease: WNV, JCV, CVV, SSHV, and WEEV. West Nile virus was isolated from four North Dakota counties in 2003–2006 (Table 2). Cache Valley virus was isolated from three counties in 2003 and in 2005. Jamestown Canyon virus was isolated from three counties in 2003–2006. Snowshoe hare virus and WEEV were isolated from one county each in 2004 and 2005 and in 2004, respectively.
Culex tarsalis and Ae. vexans were both important vectors of WNV in North Dakota. This virus was isolated from nine species of mosquitoes and multiple isolations were made from four species, but Cx. tarsalis and Ae. vexans accounted for 95.4% of the total risk for the years 2003–2006 (Supplemental Table 2).16 The relatively high IR for Cx. tarsalis and the abundance of Ae. vexans accounted for their relatively high risks. Culex tarsalis was the more important with a risk factor of 61.4%. However, the largest epidemic of WNV infection in North Dakota was recorded in 2003, and in Cass County with 32 cases, humans had a greater risk of being bitten by infected Ae. vexans (73.6%) (Supplemental Table 3). The abundance and relatively high IR of 0.19 per thousand tested mosquitoes accounted for the risk of Ae. vexans transmitting WNV to humans in 2003. Previous laboratory and field studies identified Cx. tarsalis as one of the most important vectors in western United States,22–25 including North Dakota.26 Our current investigations confirm this conclusion, but we also documented Ae. vexans to be an important vector. Previously, WNV was detected only in Cx. tarsalis in North Dakota.26,27 Unlike studies elsewhere in the United States where Ae. vexans was not as abundant,28–30 numbers per trap-night in North Dakota averaged > 1,890 from June 2 through the week of August 4 and averaged as high as 9,393 per trap-night during the week of July 7 (Figure 2B).
Culex tarsalis feeds on both birds and mammals,31–35 including humans.36 It was relatively abundant in North Dakota from the end of June through the end of August, had a relatively high IR during the summer, is efficient in transmitting this virus horizontally,22,24,25,37 and is relatively efficient in transmitting this virus vertically.24,38,39 Culex tarsalis was collected during the weeks of June 2 to October 6, similar to collections made in Grand Forks, North Dakota,26 but populations were highest from the week of June 30 through August ranging from 63.9 to 239.4 per trap-night (Figure 2A). The Cx. tarsalis weekly risk and vector index was dominant during August except in 2003 (Supplemental Tables 4–9, Figure 4). These data were similar to those reported in Grand Forks, ND.26,27 The IR was near or greater than three per thousand specimens, and populations were relatively abundant (Figure 2A). The IR increased in early September, but populations were drastically reduced and risk of transmission reduced. It is noteworthy that Cx. pipiens, which is a relatively important vector in Illinois and Colorado,17,40 was not prevalent in our collections in North Dakota, although we did not use gravid traps to collect mosquitoes.41
Aedes vexans is the most abundant mosquito in North Dakota,42 and it is an aggressive feeder on humans.43 Infected specimens with WNV were collected during the same weeks of summer as were Cx. tarsalis (Figure 2A, B), and females with a disseminated infection transmit the virus by bite.37 It primarily feeds on mammals, particularly large mammals, and infrequently feeds on birds.31,44–46 More than 1,850 specimens were captured per trap-night from early June through the first week of August, and more than a 1,000 specimens were collected per trap-night in mid-September. Weekly risk of being bitten by infected specimens ranged from 36.2% to 74.0% during most of July and the first week of August, but declined to 10.3–14.5% for the remainder of August (Supplemental Table 4). It increased to 35.5% and 60.0% in early September. Aedes vexans may become infected by feeding on small or medium-sized mammals, which have been reported to have specific antibodies to WNV,47 shown to produce viremias sufficient to infect mosquitoes,48–51 and found naturally infected in the field.52
The risk that humans will acquire an infectious bite was greatest from the middle of July through the end of August with transmission still occurring in early September (Supplemental Table 4). The vector index was highest from the middle of July through the end of August (Supplemental Table 9, Figure 4). Increasing vector indexes preceded onset of human symptoms by 2 to 3 weeks. This time-lag results from a 7–14-day delay for symptoms to appear and a several day WNV extrinsic incubation period in the mosquito.53,54 With the exceptions of weeks June 16, July 7, July 28, and September 8, human risk of being bitten by infected Cx. tarsalis during the weeks of June 30 through September 8 was greater than being bitten by other vector species, including Ae. vexans. Nonetheless, the weekly risk of being bitten by an infectious Ae. vexans plus other vector species, other than Cx. tarsalis, from mid-July through August ranged from 10.3% to 57.8%. Vector indexes were also relatively high for Cx. tarsalis during mid-July through August. The earliest human cases may have resulted from bites from Ae. vexans and Oc. dorsalis, which were relatively abundant during June. Alternatively, humans may have been bitten by Cx. tarsalis that overwintered as adults and were vertically infected.24,38,39 West Nile virus has been isolated from overwintering Cx. pipiens and has been shown to survive winter in unfed, vertically infected Cx. pipiens with amplification initiated in the spring by horizontal transmission.55,56 Human cases reported in October may have resulted from bites by infected Cx. tarsalis or Ae. vexans.
Phylogenetic analysis of WNV sequences of isolates made from 2003 to 2006 showed that strains circulating in North Dakota were members of the WN02 genotype (Figure 5). These findings are consistent with those reported elsewhere in the United States.19,20
Five of the viruses belong to the genus Orthobunyavirus in the family Bunyaviridae. Cache Valley virus, originally isolated from Cx. inornata collected in Cache Valley, Utah in 1956,57 has been reported from four Canadian provinces, 22 states, including North Dakota, northern Mexico, and Jamaica.58–60 Our isolations of CVV from Ae. vexans, Cs. inornata, Oc. dorsalis, and six other species (Table 3, Supplemental Table 10) are consistent with previous findings of its presence in several species of mosquitoes and from mammals, including humans.58,61 It causes congenital defects in fetal or neonatal sheep and cattle,62,63 including those in North Dakota,64 has caused disease in humans,61,65,66 and it may be responsible for birth defects in humans.67
Cache Valley virus was isolated in two of the four years sampled and was prevalent only in 2005 when it was isolated from 149 pools of mosquitoes collected in eastern and western North Dakota (Table 2). These data suggest that CVV becomes epizootic periodically. Although four isolations were made in July when mosquito populations of the nine infected species were highest, 96.7% of the isolations were made throughout August and the first week of September when mosquito abundance was significantly reduced compared with their numbers in June and July (Figure 6). The infection rate in August and the first week of September was relatively high ranging from 0.14 to 1.09 per 1,000 specimens tested and is the time when sheep and cattle are most likely to become infected with virus.
Jamestown Canyon virus is widely distributed in North America and causes a mild febrile illness that may cause central nervous system infection.68,69 Human cases are relatively rare with 15 cases reported from 2004 to 2010, including one from Montana in 2009,69 and two cases were reported during 2012.70 Although not previously reported from North Dakota, we found this virus to be widespread. It is transmitted primarily by mammalian-feeding Aedes and Ochlerotatus mosquitoes.71 Deer are considered the primary hosts, although other ungulates may also be involved.71This virus survives winter in mosquito eggs via vertical transmission.71 Our isolation of JCV from eight species within four genera from four counties during the 4 years confirms earlier findings that several species are likely vectors (Table 2 and 3) The largest numbers of isolations were from Ae. vexans, but IRs were all < 0.1 per thousand specimens tested (Supplemental Table 11). Species less numerous but with larger IRs included Cs. inornata, Oc. dorsalis, Oc. flavescens, Ochlerotatus melanimon, and Oc. trivittatus. Species not previously reported to be infected included Cx. tarsalis and Oc. flavescens. This virus was isolated from the last week of June to the second week of September (Figure 7). Most isolates (98%) were from mosquitoes collected during the week of June 30 through the last week of August. Sequence analysis of 44 isolates from North Dakota showed that most belonged to Lineage A (Figure 8). Forty-one isolates from seven species, collected in four different counties, and four different years were similar to the lineage A isolates from Connecticut.14 Three isolates belonged to the Jerry Slough variant.72 Our findings suggest the JCV strains were stably maintained in North Dakota, infecting a number of different mosquito species.
Trivittatus virus, which was originally isolated in Bismarck, North Dakota in 1948,21 was the most frequently isolated virus. Although isolated from six species, 77.8% were from Oc. trivittatus, confirming it as the most important vector (Table 3).73–75 Many of the remaining isolates (20.3%) were from Ae. vexans. The IRs for Oc. trivittatus by county and year ranged from 0.70 to 5.09 and were significantly higher than the IRs for Ae. vexans, which ranged from 0.01 to 0.42 (Supplemental Table 12). This virus, which is transmitted horizontally and vertically by Oc. trivittatus,73–76 was isolated during most weeks of the summer and fall, particularly during June and July when Oc. trivittatus were most abundant (Figure 9). Two isolates were genetically similar to the prototype strain (Figure 8). This virus infects humans,77 but rarely causes clinical symptoms.71
Seasonal relationships between numbers of Oc. trivittatus infected with TVTV and mosquitoes infected with CVV were markedly different (Figures 6 and 9). Differences reflect at least in part the means by which these mosquitoes become infected. Isolations of TVTV were made weekly, with the exception of 3 weeks in September, from Oc. trivittatus throughout the season from early June to the first week of October (Figure 9). Vertical transmission is responsible for early season-infection, and vertical and horizontal transmission cause infection later in the season.73–76 In contrast, horizontal transmission likely is the primary means of infection during summer for CVV. In mid-June through late July, weekly vector numbers per trap-night averaged > 4,000 to > 14,000 and few isolations were recorded (Figure 6). In late July, after numbers of mosquitoes declined, numbers of weekly isolations in August and early September increased to as high as 50 per week. Mosquitoes collected in June and early July likely had not fed on viremic mammals, whereas relative numbers of those collected in late July and into the first week of September likely became infected by feeding on viremic mammals.
Potosi virus originally isolated from Ae. albopictus collected in Potosi, MO in 1989,78 also has been isolated from several species of mammal-feeding mosquitoes in Illinois, Michigan, Ohio, the Carolinas, Connecticut, and New York.79–84 We now report POTV in three species in North Dakota. Isolation of POTV from four pools of Ae. vexans and single pools of Ae. dorsalis and Cx. inornata in 2005 clearly shows its distribution extends into the northern great plains. Infected mosquitoes were collected from late August through the last week of September 2005. This virus is horizontally transmitted by several species to white-tailed deer, Odocoileus virginianus.85,86 Although POTV is not known to cause human disease, related Bunyamwera viruses are known to cause febrile illness, central neurological system disease, and hemorrhagic fever.61,87–89 It is also worth noting that POTV may co-circulate with CVV, which causes congenital defects in sheep and cattle,62,63 during late August and September.
Snowshoe hare virus was initially isolated in 1959 in Montana from a snowshoe hare, Lepus americanus,90 and subsequently from at least 23 species of mosquitoes,91 which were collected in Alaska,91 Montana,91 New York,92 Wisconsin,92 Massachusetts,92 and all Canadian provinces.93,94 Our isolations of SSHV from Ae. vexans and Oc. trivittatus are the first from North Dakota. They were genetically similar to a known strain of SSHV (Figure 8). This virus is transmitted horizontally by several species of mosquitoes in the genera Aedes, Ochlerotatus, and Culiseta, and it is also transmitted vertically.95,96 Snowshoe hares and squirrels are principal reservoir hosts in Canada.93,94 Human infection ranges from absence of clinical disease to non-fatal meningitis and encephalitis.93,94 Disease in domestic animals has occurred infrequently.97
Western equine encephalomyelitis virus causes disease and death in humans and horses in western and central Canada and the United States, Mexico, Guyana, Brazil, Uruguay, and Argentina.98 One of the largest human epidemics of WEEV occurred in North Dakota in 1941.1 Since 1955, a total of 93 cases have been documented in North Dakota, but none has been reported since 1987.99,100 The basic transmission cycle involves Cx. tarsalis and passerine birds. Humans and horses are tangential hosts. Our isolation of WEEV from two pools of Cx. tarsalis in 2005 shows this virus still persists at low levels in North Dakota. The decline of WEEV as a human and equine health problem in North Dakota is similar to declines reported in Kern County, CA and elsewhere in North America.101,102 Both WNV and WEEV are amplified in birds after bites by infected Cx. tarsalis, but WEEV has not amplified sufficiently in recent decades to infect humans and horses. Reasons for the suppression of WEEV in the years preceding and after the introduction of WNV are not known.
Supplementary Material
ACKNOWLEDGMENTS
We thank Loida Tobias, Silka Tobias, David Benth, Chris Bean, and Jacquelin Stenehjem for collecting mosquitoes and sending them on dry ice to our laboratory. Jacquelin Stenehjem made arrangements for the Williston Vector Control, District 1 to collect mosquitoes. The Williston Vector Control Board allowed us to have their employees collect mosquitoes and to use their facilities. Gary Brewer, Chairman, Department of Entomology, North Dakota State University, provided helpful suggestions and arranged the use of their laboratories and equipment and for the employment of Loida and Silka Tobias. We thank many North Dakota citizens for allowing us to trap mosquitoes on their properties, including. William Barker of North Dakota State University who enabled us to trap mosquitoes at the Ekre Ranch. The following provided superb technical assistance at the Connecticut Agricultural Experiment Station: Angela Bransfield, Michael Misencik, Bonnie Hamid, Amanda Rahmann, Michael Vasil, Terrill Goodman, John Shepard, Michael Thomas, Elizabeth Alves, Tanya Petruff, Clare Secker-Walker, Leah Heibi, Alyson Florek, Charles McGee, Susan McKnight, Sarah Reiff, and Leigh Cash. Hyperimmune mouse ascetic fluid (1:10) against TVTV virus was kindly supplied by the late Robert E. Shope and by Robert Tesh, Pathology Department, University of Texas Medical Branch at Galveston.
Footnotes
Financial support: This work was supported in part by USDA Specific Cooperative agreement 58-6615-1-218 and by Laboratory Capacity for Infectious Diseases Cooperative Agreement U50/CCU116806-01-1 from the Centers for Disease Control and Prevention.
Authors' addresses: John F. Anderson, Andrew J. Main, and Philip M. Armstrong, Department of Entomology and Center for Vector Biology and Zoonotic Diseases, The Connecticut Agricultural Experiment Station, New Haven, CT, E-mails: John.F.Anderson@ct.gov, andymain@aucegypt.edu, and Philip.Armstrong@ct.gov. Theodore G. Andreadis, Director's Office and Center for Vector Biology and Zoonotic Diseases, The Connecticut Agricultural Experiment Station, New Haven, CT, E-mail: Theodore.Andreadis@ct.gov. Francis J. Ferrandino, Department of Plant Pathology & Ecology, The Connecticut Agricultural Experiment Station, New Haven, CT, E-mail: Francis.Ferrandino@ct.gov.
References
- 1.Leake JP. Epidemic of infectious encephalitis. Public Health Rep. 1941;56:1902–1905. [Google Scholar]
- 2.U.S. Geological Survey West Nile virus maps. 2012. http://diseasemaps.usgs.gov/wnv_us_humans.html Available at. Accessed April 23, 2014.
- 3.Borchardt SM, Feist MA, Miller T, Loq TS. Epidemiology of West Nile virus in the highly epidemic state of North Dakota, 2002–2007. Public Health Rep. 2010;125:246–249. doi: 10.1177/003335491012500213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karabatsos N. International Catalogue of Arboviruses Including Certain Other Viruses of Vertebrates. San Antonio, TX: American Society of Tropical Medicine and Hygiene; 1985. [DOI] [PubMed] [Google Scholar]
- 5.Sudia WD, Chamberlain RW. Battery-operated light trap, an improved model. Mosq News. 1962;3:311–316. [PubMed] [Google Scholar]
- 6.Andreadis TG, Thomas MC, Shepard JJ. Identification guide to the mosquitoes of Connecticut. Bull Conn Agric Exp Sta. 2005;966:1–173. [Google Scholar]
- 7.Darsie RF, Jr, Ward RA. Identification and Geographical Distribution of the Mosquitoes of North America, North of Mexico. Gainesville, FL: University Press of Florida; 2005. [Google Scholar]
- 8.Hammon WM, Sather GE. Arboviruses. In: Lennette EH, Schmidt NJ, editors. Procedures for Viral and Rickettsial Infections. New York: American Public Health Association, Inc.; 1969. pp. 227–280. [Google Scholar]
- 9.Lanciotti RS, Kerst AJ, Nasci RS, Godsey MS, Mitchell CJ, Savage HM, Komar N, Panella NA, Allen BC, Volpe KE, Davis BS, Roehrig JT. Rapid detection of West Nile virus from human clinical specimens, field-collected mosquitoes, and avian samples by a TaqMan reverse transcriptase-PCR assay. J Clin Microbiol. 2000;38:4066–4071. doi: 10.1128/jcm.38.11.4066-4071.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunn EF, Pritlove DC, Elliott RM. The S RNA genome segments of Batai, Cache Valley, Guaroa, Kairi, Lumbo, Main Drain and Northway bunyaviruses: sequence determination and analysis. J Gen Virol. 1994;75:597–608. doi: 10.1099/0022-1317-75-3-597. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong PM, Andreadis TG. A new genetic variant of La Crosse virus (Bunyaviridae) isolated from New England. Am J Trop Med Hyg. 2006;75:491–496. [PubMed] [Google Scholar]
- 12.Gray RR, Veras VMC, Santos LA, Salemi M. Evolutionary characterization of the West Nile virus complete genome. Mol Phylogenet Evol. 2010;56:195–200. doi: 10.1016/j.ympev.2010.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Tamura K, Peterson D, Peterson N, Stecher G, Nei M, Kumar S. MEGA5: Molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Eiol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armstrong PM, Andreadis TG. Genetic relationships of Jamestown Canyon virus strains infecting mosquitoes collected in Connecticut. Am J Trop Med Hyg. 2007;77:1157–1162. [PubMed] [Google Scholar]
- 15.Biggerstaff BJ. PooledInfRate. Version 3.0: a Microsoft Excel Add-In to compute prevalence estimates from pooled samples. Fort Collins, CO: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 16.Kilpatrick AM, Kramer LD, Campbell SR, Alleyne EO, Dobson AP, Daszak P. West Nile virus risk assessment and the bridge vector paradigm. Emerg Infect Dis. 2005;11:425–429. doi: 10.3201/eid1103.040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention West Nile virus in the United States: Guidelines for Surveillance, Prevention, and Control. 2013. http://www.cdc.gov/westnile/vector control/index.html Available at. 1–69. Accessed August 13, 2014.
- 18.North Dakota Department of Health (NDDPH) West Nile Virus Data Summaries. 2013. http://www.ndhealth.gov/wnv/data/summary.aspx Available at. Accessed April 23, 2014.
- 19.Davis CT, Ebel GD, Lanciotti RS, Brault AC, Guzman H, Siirin M, Lambert A, Parsons RE, Beasley DW, Novak RJ, Elizondo-Quiroga D, Green EN, Young DS, Stark LM, Drebot MA, Artsob H, Tesh RB, Kramer LD, Barrett AD. Phylogenetic analysis of North American West Nile virus isolates, 2001–2004: evidence for the emergence of a dominant genotype. Virology. 2005;342:252–265. doi: 10.1016/j.virol.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Ebel GD, Carricaburu J, Young D, Bernard KA, Kramer LD. Genetic and phenotypic variation of West Nile virus in New York, 2000–2003. Am J Trop Med Hyg. 2004;71:493–500. [PubMed] [Google Scholar]
- 21.Hammon WM, Reeves WC, Sather GE. California encephalitis virus, a newly described agent. II. Isolations and attempts to identify and characterize the agent. J Immunol. 1952;69:493–510. [PubMed] [Google Scholar]
- 22.Goddard LB, Roth AE, Reisen WK, Scott TW. Vector competence of California mosquitoes for West Nile virus. Emerg Infect Dis. 2002;8:1385–1391. doi: 10.3201/eid0812.020536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turell MJ, O'Guinn ML, Dohm DJ, Webb JP, Jr, Sardelis MR. Vector competence of Culex tarsalis from Orange County, California, for West Nile virus. Vector Borne Zoonotic Dis. 2002;2:193–196. doi: 10.1089/15303660260613756. [DOI] [PubMed] [Google Scholar]
- 24.Anderson JF, Main AJ, Cheng G, Ferrandino FJ, Fikrig E. Horizontal and vertical transmission of West Nile virus genotype NY99 by Culex salinarius and genotypes NY99 and WN02 by Culex tarsalis. Am J Trop Med Hyg. 2012;86:134–139. doi: 10.4269/ajtmh.2012.11-0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reisen WK, Fang Y, Martinez VM. Effects of temperature on the transmission of West Nile virus by Culex tarsalis (Diptera:Culicidae) J Med Entomol. 2006;43:309–317. doi: 10.1603/0022-2585(2006)043[0309:EOTOTT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Bell JA, Mickelson NJ, Vaughan JA. West Nile virus in host-seeking mosquitoes within a residential neighborhood in Grand Forks, North Dakota. Vector Borne Zoonotic Dis. 2005;5:373–382. doi: 10.1089/vbz.2005.5.373. [DOI] [PubMed] [Google Scholar]
- 27.Bell JA, Brewer CM, Mickelson NJ, Garman GW, Vaughan JA. West Nile virus epizootiology, central Red River Valley, North Dakota and Minnesota, 2002–2005. Emerg Infect Dis. 2006;12:1245–1247. doi: 10.3201/eid1208.060129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard KA, Maffei JG, Jones SA, Kauffman EB, Ebel GD, Dupuis AP II, Ngo KA, Nicholas DC, Young DM, Shi P-Y, Kulasekera VL, Eidson M, White DJ, Stone WB, Kramer LD, State West Nile Virus Surveillance Team NY. West Nile virus infection in birds and mosquitoes, New York State, 2000. Emerg Infect Dis. 2001;7:679–685. doi: 10.3201/eid0704.010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andreadis TG, Anderson JF, Vossbrinck CR, Main AJ. Epidemiology of West Nile virus in Connecticut: a five-year analysis of mosquito data 1999–2003. Vector Borne Zoonotic Dis. 2004;4:360–378. doi: 10.1089/vbz.2004.4.360. [DOI] [PubMed] [Google Scholar]
- 30.Anderson JF, Andeadis TG, Main AJ, Kline DL. Prevalence of West Nile virus in tree canopy-inhabiting Culex pipiens and associated mosquitoes. Am J Trop Med Hyg. 2004;71:112–119. [PubMed] [Google Scholar]
- 31.Tempelis CH. Host-feeding patterns of mosquitoes, with a review of advances in analysis of blood meals by serology. J Med Entomol. 1974;11:635–653. doi: 10.1093/jmedent/11.6.635. [DOI] [PubMed] [Google Scholar]
- 32.Kent R, Juliusson L, Weissmann M, Evans S, Komar N. Seasonal blood-feeding behavior of Culex tarsalis (Dipter:Culicidae) in Weld County, Colorado, 2007. J Med Entomol. 2009;46:380–390. doi: 10.1603/033.046.0226. [DOI] [PubMed] [Google Scholar]
- 33.Molaei G, Cummings RF, Su T, Armstrong PM, Williams GA, Cheng ML, Webb JP, Andreadis TG. Vector-host interactions governing epidemiology of West Nile virus in Southern California. Am J Trop Med Hyg. 2010;83:1269–1282. doi: 10.4269/ajtmh.2010.10-0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thiemann TC, Lemenager DA, Kluh S, Carroll BD, Lothrop HD, Reisen WK. Spatial variation in host feeding patterns of Culex tarsalis and the Culex pipiens complex (Diptera: Culicidae) in California. J Med Entomol. 2012;49:903–916. doi: 10.1603/me11272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thiemann TC, Reisen WK. Evaluating sampling method bias in Culex tarsalis and Culex quinquefasciatus (Diptera:Culicidae) blood meal identification studies. J Med Entomol. 2012;49:143–149. doi: 10.1603/me11134. [DOI] [PubMed] [Google Scholar]
- 36.Reeves WC, Tempelis CH, Bellamy RE, Lofy MF. Observations on the feeding habits of Culex tarsalis in Kern County, California, using precipitating antisera produced in birds. Am J Trop Med Hyg. 1963;12:929–935. doi: 10.4269/ajtmh.1963.12.929. [DOI] [PubMed] [Google Scholar]
- 37.Turell MJ, Dohm DJ, Sardelis MR, Oguinn ML, Andreadis TG, Blow JA. An update on the potential of North American mosquitoes (Diptera: Culicidae) to transmit West Nile virus. J Med Entomol. 2005;42:57–62. doi: 10.1093/jmedent/42.1.57. [DOI] [PubMed] [Google Scholar]
- 38.Goddard LB, Roth AE, Reisen WK, Scott TW. Vertical transmission of West Nile virus by three California Culex (Diptera:Culicidae) species. J Med Entomol. 2003;40:743–746. doi: 10.1603/0022-2585-40.6.743. [DOI] [PubMed] [Google Scholar]
- 39.Reisen WK, Fang Y, Lothrop HD, Martinez VM, Wilson J, O'Connor P, Carney R, Cahoon-Young B, Shafii M, Brault AC. Overwintering of West Nile virus in southern California. J Med Entomol. 2006;43:344–355. doi: 10.1603/0022-2585(2006)043[0344:oownvi]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 40.Lampman RL, Krasavin NM, Ward MP, Beveroth TA, Lankau EW, Alto BW, Muturi E, Novak RJ. West Nile virus infection rates and avian serology in east-central Illinois. J Am Mosq Control Assoc. 2013;29:108–122. doi: 10.2987/12-6318R.1. [DOI] [PubMed] [Google Scholar]
- 41.Reiter P. A portable, battery-powered trap for collecting gravid Culex mosquitoes. Mosq News. 1983;43:496–498. [Google Scholar]
- 42.Post RL, Munro JA. Mosquitoes of North Dakota. N. D. Agr. Expert. Sta. Bimonthly Bull. 1949;11:173–183. [Google Scholar]
- 43.Horsfall WR, Fowler HW, Moretti LJ, Larsen JR. Bionomics and Embryology of the Inland Floodwater Mosquito Aedes vexans. Urbana, IL: University of Illinois Press; 1973. [Google Scholar]
- 44.Magnarelli LA. Host feeding patterns of Connecticut mosquitoes (Diptera: Culicidae) Am J Trop Med Hyg. 1977;26:547–552. doi: 10.4269/ajtmh.1977.26.547. [DOI] [PubMed] [Google Scholar]
- 45.Nasci RS. Variations in the blood-feeding patterns of Aedes vexans and Aedes trivittatus (Diptera:Culicidae) J Med Entomol. 1984;21:95–99. doi: 10.1093/jmedent/21.1.95. [DOI] [PubMed] [Google Scholar]
- 46.Molaei G, Andreadis TG. Identification of avian- and mammalian-derived blood meals in Aedes vexans and Culiseta melanura (Diptera:Culicidae) and its implication for West Nile virus transmission in Connecticut, USA. J Med Entomol. 2006;43:1088–1093. doi: 10.1603/0022-2585(2006)43[1088:IOAAMB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 47.Root JJ, Hall JS, McLean RG, Marlenee NL, Beaty BJ, Gansowski J, Clark L. Serologic evidence of exposure of wild mammals to flaviviruses in the central and eastern United States. Am J Trop Med Hyg. 2005;72:622–630. [PubMed] [Google Scholar]
- 48.Root JJ, Oesterle PT, Nemeth NM, Klenk K, Gould DH, McLean RG, Clark L, Hall JS. Experimental infection of fox squirrels (Sciurus niger) with West Nile virus. Am J Trop Med Hyg. 2006;75:697–701. [PubMed] [Google Scholar]
- 49.Platt KB, Tucker BJ, Halbur PG, Blitvich BJ, Fabiosa FG, Mullin K, Parikh GR, Kitikoon P, Bartholomay LC, Rowley WA. Fox squirrels (Sciurus niger) develop West Nile virus viremias sufficient for infecting select mosquito species. Vector Borne Zoonotic Dis. 2008;8:225–233. doi: 10.1089/vbz.2007.0182. [DOI] [PubMed] [Google Scholar]
- 50.Platt KB, Tucker BJ, Halbur PG, Tiawsirisup S, Blitvich BJ, Fabiosa FG, Bartholomay LC, Rowley WA. West Nile virus viremia in eastern chipmunks (Tamias striatus) sufficient for infecting different mosquitoes. Emerg Infect Dis. 2007;13:831–837. doi: 10.3201/eid1306.061008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tiawsirisup S, Platt KB, Tucker BJ, Rowley WA. Eastern cottontail rabbits (Sylvilagus floridanus) develop West Nile virus viremias sufficient for infecting select mosquito species. Vector Borne Zoonotic Dis. 2005;5:342–350. doi: 10.1089/vbz.2005.5.342. [DOI] [PubMed] [Google Scholar]
- 52.Anderson JF, Vossbrinck CR, Andreadis TG, Iton A, Beckwith WH, 3rd, Mayo DR. A phylogenetic approach to following West Nile virus in Connecticut. Proc Natl Acad Sci USA. 2001;98:12885–12889. doi: 10.1073/pnas.241472398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chung WM, Buseman CM, Joyner SN, Hughes SM, Fomby TB, Luby JP, Haley RW. The 2012 West Nile encephalitis epidemic in Dallas, Texas. JAMA. 2013;310:297–307. doi: 10.1001/jama.2013.8267. [DOI] [PubMed] [Google Scholar]
- 54.Kramer LD, Styer LM, Ebel GD. A global perspective on the epidemiology of West Nile virus. Annu Rev Entomol. 2008;53:61–81. doi: 10.1146/annurev.ento.53.103106.093258. [DOI] [PubMed] [Google Scholar]
- 55.Nasci RS, Savage HM, White DJ, Miller JR, Cropp BC, Godsey MS, Kerst AJ, Bennett P, Gottfried K, Lanciotti RS. West Nile virus in overwintering Culex mosquitoes, New York City, 2000. Emerg Infect Dis. 2001;7:742–744. doi: 10.3201/eid0704.010426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anderson JF, Main AJ. Importance of vertical and horizontal transmission of West Nile virus by Culex pipiens in the northeastern United States. J Infect Dis. 2006;194:1577–1579. doi: 10.1086/508754. [DOI] [PubMed] [Google Scholar]
- 57.Holden P, Hess AD. Cache Valley virus, a previously undescribed mosquito-borne agent. Science. 1959;130:1187–1188. doi: 10.1126/science.130.3383.1187. [DOI] [PubMed] [Google Scholar]
- 58.Calisher CH, Francy DB, Smith GC, Muth DJ, Lazuick JS, Karabatsos N, Jakob WL, McLean RG. Distribution of Bunyamwera serogroup viruses in North America, 1956–1984. Am J Trop Med Hyg. 1986;35:429–443. doi: 10.4269/ajtmh.1986.35.429. [DOI] [PubMed] [Google Scholar]
- 59.Iversen JO, Wagner RJ, Leung MK, Hayles LB, McLintock JR. Cache Valley virus: isolations from mosquitoes in Saskatchewan, 1972–1974. Can J Microbiol. 1979;25:760–764. doi: 10.1139/m79-110. [DOI] [PubMed] [Google Scholar]
- 60.Armstrong PM, Anderson JF, Farajollahi A, Healy SP, Unlu I, Crepeau TN, Gaugler R, Fonseca DM, Andreadis TG. Isolations of Cache Valley virus from Aedes albopictus (Diptera: Culicidae) in New Jersey and evaluation of its role as a regional arbovirus vector. J Med Entomol. 2013;50:1310–1314. doi: 10.1603/me13099. [DOI] [PubMed] [Google Scholar]
- 61.Sexton DJ, Rollin PE, Breitschwerdt EB, Corey GR, Myers SA, Dumais MR, Bowen MD, Goldsmith CS, Zaki SR, Nichol ST, Peters CJ, Ksiazek TG. Life-threatening Cache Valley virus infection. N Engl J Med. 1997;336:547–549. doi: 10.1056/NEJM199702203360804. [DOI] [PubMed] [Google Scholar]
- 62.Crandell RA, Livingston CW, Jr, Shelton MJ. Laboratory investigation of a naturally occurring outbreak of arthrogryposis-hydranencephaly in Texas sheep. J Vet Diagn Invest. 1989;1:62–65. doi: 10.1177/104063878900100117. [DOI] [PubMed] [Google Scholar]
- 63.McConnell S, Livingston C, Jr, Calisher CH, Crandell RA. Isolations of Cache Valley virus in Texas, 1981. Vet Microbiol. 1987;13:11–18. doi: 10.1016/0378-1135(87)90093-9. [DOI] [PubMed] [Google Scholar]
- 64.Redden R. Update on Cache Valley virus. N. D. Sheep Industry Newsletter. 2011;62:2. [Google Scholar]
- 65.Campbell GL, Mataczynski JD, Reisdorf ES, Powell JW, Martin DA, Lambert AJ, Haupt TE, Davis JP, Lanciotti RS. Second human case of Cache Valley virus disease. Emerg Infect Dis. 2006;12:854–856. doi: 10.3201/eid1205.051625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nguyen NL, Zhao G, Hull R, Shelly MA, Wong SJ, Wu G, St George K, Wang D, Menegus MA. Cache valley virus in a patient diagnosed with aseptic meningitis. J Clin Microbiol. 2013;51:1966–1969. doi: 10.1128/JCM.00252-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Calisher CH, Sever JL. Are North American Bunyamwera serogroup viruses etiologic agents of human congenital defects of the central nervous system? Emerg Infect Dis. 1995;1:147–151. doi: 10.3201/eid0104.950409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Andreadis TG, Anderson JF, Armstrong PM, Main AJ. Isolations of Jamestown Canyon virus (Bunyaviridae: Orthobunyavirus) from field-collected mosquitoes (Diptera: Culicidae) in Connecticut, USA: a ten-year analysis, 1997–2006. Vector Borne Zoonotic Dis. 2008;8:175–188. doi: 10.1089/vbz.2007.0169. [DOI] [PubMed] [Google Scholar]
- 69.Centers for Disease Control and Prevention Human Jamestown Canyon virus infection—Montana, 2009. MMWR Morb Mortal Wkly Rep. 2011;60:652–655. [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention West Nile virus and other arboviral diseases–United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:513–517. [PMC free article] [PubMed] [Google Scholar]
- 71.Grimstad PR. California group virus disease. In: Monath TP, editor. The Arboviruses: Epidemiology and Ecology. Boca Raton, FL: CRC Press; 1988. pp. 99–136. [Google Scholar]
- 72.Hammon WM, Sather G. History and recent reappearance of viruses in the California encephalitis group. Am J Trop Med Hyg. 1966;15:199–204. doi: 10.4269/ajtmh.1966.15.199. [DOI] [PubMed] [Google Scholar]
- 73.Turell MJ, LeDuc JW. The role of mosquitoes in the natural history of California serogroup viruses. In: Calisher CH, Thompson WH, editors. California Serogroup Viruses. New York: Alan R. Liss; 1983. pp. 43–56. [PubMed] [Google Scholar]
- 74.Watts DM, DeFoliart GR, Yuill TM. Experimental transmission of Trivittatus virus (California virus group) by Aedes trivittatus. Am J Trop Med Hyg. 1976;25:173–176. doi: 10.4269/ajtmh.1976.25.173. [DOI] [PubMed] [Google Scholar]
- 75.Andrews WN, Rowley WA, Wong YW, Dorsey DC, Hausler WJ., Jr Isolation of trivittatus virus from larvae and adults reared from field-collected larvae of Aedes trivittatus (Diptera: Culicidae) J Med Entomol. 1977;13:699–701. doi: 10.1093/jmedent/13.6.699. [DOI] [PubMed] [Google Scholar]
- 76.Rowley WA, Wong YW, Dorsey DC, Hausler WJ, Jr, Currier RW. California serogroup viruses in Iowa. In: Calisher CH, Thompson WH, editors. California Serogroup Viruses. New York: Alan R. Liss; 1983. pp. 237–246. [PubMed] [Google Scholar]
- 77.Monath TP, Nuckolls JG, Berall J, Bauer H, Chappell WA, Coleman PH. Studies on California encephalitis in Minnesota. Am J Epidemiol. 1970;92:40–50. doi: 10.1093/oxfordjournals.aje.a121178. [DOI] [PubMed] [Google Scholar]
- 78.Francy DB, Karabatsos N, Wesson DM, Moore CG, Jr, Lazuick JS, Niebylski ML, Tsai TF, Craig GB., Jr A new arbovirus from Aedes albopictus, an Asian mosquito established in the United States. Science. 1990;250:1738–1740. doi: 10.1126/science.2270489. [DOI] [PubMed] [Google Scholar]
- 79.Harrison BA, Mitchell CJ, Apperson CS, Smith GC, Karabatsos N, Engber BR, Newton NH. Isolation of Potosi virus from Aedes albopictus in North Carolina. J Am Mosq Control Assoc. 1995;11:225–229. [PubMed] [Google Scholar]
- 80.Mitchell CJ, Haramis LD, Karabatsos N, Smith GC, Starwalt VJ. Isolation of La Crosse, Cache Valley, and Potosi viruses from Aedes mosquitoes (Diptera: Culicidae) collected at used-tire sites in Illinois during 1994–1995. J Med Entomol. 1998;35:573–577. doi: 10.1093/jmedent/35.4.573. [DOI] [PubMed] [Google Scholar]
- 81.Mitchell CJ, Smith GC, Karabatsos N, Moore CG, Francy DB, Nasci RS. Isolations of Potosi virus from mosquitoes collected in the United States, 1989–94. J Am Mosq Control Assoc. 1996;12:1–7. [PubMed] [Google Scholar]
- 82.Wozniak A, Dowda HE, Tolson MW, Karabatsos N, Vaughan DR, Turner PE, Ortiz DI, Wills W. Arbovirus surveillance in South Carolina, 1996–98. J Am Mosq Control Assoc. 2001;17:73–78. [PubMed] [Google Scholar]
- 83.Armstrong PM, Andreadis TG, Anderson JF, Main AJ. Isolations of Potosi virus from mosquitoes (Diptera: Culicidae) collected in Connecticut. J Med Entomol. 2005;42:875–881. doi: 10.1093/jmedent/42.5.875. [DOI] [PubMed] [Google Scholar]
- 84.Ngo KA, Maffei JG, Dupuis AP, 2nd, Kauffman EB, Backenson PB, Kramer LD. Isolation of Bunyamwera serogroup viruses (Bunyaviridae, Orthobunyavirus) in New York state. J Med Entomol. 2006;43:1004–1009. doi: 10.1603/0022-2585(2006)43[1004:iobsvb]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 85.McLean RG, Kirk LJ, Shriner RB, Cook PD, Myers EE, Gill JS, Campos EG. The role of deer as a possible reservoir host of Potosi virus, a newly recognized arbovirus in the United States. J Wildl Dis. 1996;32:444–452. doi: 10.7589/0090-3558-32.3.444. [DOI] [PubMed] [Google Scholar]
- 86.Blackmore CG, Grimstad PR. Cache Valley and Potosi viruses (Bunyaviridae) in white-tailed deer (Odocoileus virginianus): experimental infections and antibody prevalence in natural populations. Am J Trop Med Hyg. 1998;59:704–709. doi: 10.4269/ajtmh.1998.59.704. [DOI] [PubMed] [Google Scholar]
- 87.Beaty BJ, Calisher CH. Bunyaviridae-natural history. Curr Top Microbiol Immunol. 1991;169:27–78. [PubMed] [Google Scholar]
- 88.Nashed NW, Olson JG, el-Tigani A. Isolation of Batai virus (Bunyaviridae: Bunyavirus) from the blood of suspected malaria patients in Sudan. Am J Trop Med Hyg. 1993;48:676–681. doi: 10.4269/ajtmh.1993.48.676. [DOI] [PubMed] [Google Scholar]
- 89.Gerrard SR, Li L, Barrett AD, Nichol ST. Ngari virus is a Bunyamwera virus reassortant that can be associated with large outbreaks of hemorrhagic fever in Africa. J Virol. 2004;78:8922–8926. doi: 10.1128/JVI.78.16.8922-8926.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Burgdorfer W, Newhouse VF, Thomas LA. Isolation of California encephalitis virus from the blood of a snowshoe hare (Lepus americanus) in western Montana. Am J Hyg. 1961;73:344–349. doi: 10.1093/oxfordjournals.aje.a120193. [DOI] [PubMed] [Google Scholar]
- 91.Sudia WD, Newhouse VF, Calisher CH, Chamberlain RW. California group arboviruses: isolations from mosquitoes in North America. Mosq News. 1971;31:576–600. [Google Scholar]
- 92.Whitney E, Jamnback H, Means RG, Roz AP, Rayner GA. California virus in New York State. Isolation and characterization of CEV complex from Aedes cinereus. Am J Trop Med Hyg. 1969;18:123–131. [PubMed] [Google Scholar]
- 93.McLean DM. California group viral infections of Canada. In: Steele JH, Beran GW, editors. Handbook Series in Zoonoses. Section B: Viral Zoonoses. Boca Raton, FL: CRC Press; 1981. pp. 107–111. [Google Scholar]
- 94.Artsob H. California encephalitis (CE) In: Steele JH, Beran GW, editors. Handbook Series in Zoonoses. Section B: Viral Zoonoses. Boca Raton, FL: CRC Press; 1981. pp. 150–154. [Google Scholar]
- 95.McLintock J, Curry PS, Wagner RJ, Leung MK, Iversen JO. Isolation of snowshoe hare virus from Aedes implicatus larvae in Saskatchewan. Mosq News. 1976;36:233–237. [Google Scholar]
- 96.McLean DM, Bergman SK, Gould AP, Grass PN, Miller MA, Spratt EE. California encephalitis virus prevalence throughout the Yukon Territory, 1971–1974. Am J Trop Med Hyg. 1975;24:676–684. doi: 10.4269/ajtmh.1975.24.676. [DOI] [PubMed] [Google Scholar]
- 97.Heath SE, Bell R. Saskatchewan. Snowshoe hare virus encephalitis in a filly. Can Vet J. 1988;29:392. [PMC free article] [PubMed] [Google Scholar]
- 98.Hayes RO. Eastern and western encephalitis. In: Steele JH, Beran GW, editors. Handbook Series in Zoonoses. Section B: Viral Zoonoses. Boca Raton, FL: CRC Press; 1981. pp. 37–57. [Google Scholar]
- 99.McGowan JE, Bryan JA, Gregg MB. Surveillance of arboviral encephalitis in the United States, 1955–1971. Am J Epidemiol. 1973;97:199–207. doi: 10.1093/oxfordjournals.aje.a121500. [DOI] [PubMed] [Google Scholar]
- 100.Centers for Disease Control and Prevention Epidemiologic notes and reports western equine encephalitis—United States and Canada, 1987. MMWR Morb Mortal Wkly Rep. 1987;36:655–659. [PubMed] [Google Scholar]
- 101.Reisen WK, Carroll BD, Takahashi R, Fang Y, Garcia S, Martinez VM, Quiring R. Repeated West Nile virus epidemic transmission in Kern County, California, 2004–2007. J Med Entomol. 2009;46:139–157. doi: 10.1603/033.046.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Reisen WK, Monath TP. Western equine encephalomyelitis. In: Monath TP, editor. The arboviruses: epidemiology and ecology. Volume V. Boca Raton, FL; CRC: 1989. pp. 89–138. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.