Abstract
The live-attenuated Japanese encephalitis virus (JEV) SA14-14-2 vaccine, produced in primary hamster kidney cells, is safe and effective. Past attempts to adapt this virus to replicate in cells that are more favorable for vaccine production resulted in mutations that significantly reduced immunogenicity. In this study, 10 genetically distinct Vero cell-adapted JEV SA14-14-2 variants were isolated and a recombinant wild-type JEV clone, modified to contain the JEV SA14-14-2 polyprotein amino acid sequence, was recovered in Vero cells. A single capsid protein mutation (S66L) was important for Vero cell-adaptation. Mutations were also identified that modulated virus sensitivity to type I interferon-stimulation in Vero cells. A subset of JEV SA14-14-2 variants and the recombinant clone were evaluated in vivo and exhibited levels of attenuation that varied significantly in suckling mice, but were avirulent and highly immunogenic in weanling mice and are promising candidates for the development of a second-generation, recombinant vaccine.
Introduction
Japanese encephalitis virus (JEV), a member of the genus flavivirus, is maintained in a zoonotic cycle between Culex mosquitoes and ardeid birds or domestic swine and is responsible for significant epidemics of viral encephalitis in Asia.1–3 Three billion people live in regions with endemic JEV transmission resulting in an estimated 60,000 annual cases, of which 20–40% are fatal and 45–70% of survivors have neurologic sequelae.3,4 The JEV has a single-strand, plus-sense, RNA genome of ∼11 kb in length, which contains a single open reading frame (ORF) that is flanked by 5′ and 3′ untranslated regions (UTRs).5 The single ORF codes for a polyprotein that is processed by viral and host cellular proteases into the capsid (C), precursor-membrane (prM), and envelope (E) structural proteins and non-structural proteins NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5.6 Humoral immunity is an essential component of protection from flavivirus disease and the E protein is the primary target of virus neutralizing antibodies.7–9 Innate-immune antiviral mechanisms like those induced by type I interferon (IFN) are critical for controlling virus dissemination within the host,10 whereas adaptive immune cell-mediated responses are important for virus clearance.11–13
Inactivated JEV vaccines have been available since the mid-1950s and have been important for controlling the incidence of disease caused by JEV.14–16 However, their high production costs and requirement for multiple doses make inactivated vaccines less practical for mass vaccination campaigns in most rural JEV-endemic areas. The live-attenuated JEV SA14-14-2 vaccine (Chengdu Institute of Biological Products, China) was licensed in China in 1988 and has more recently become available for use in Cambodia, India, Korea, Laos, Myanmar, Nepal, Sri Lanka, and Thailand.15,17,18 Immunization with JEV SA14-14-2 has been shown to result in 88–96% efficacy after a single dose (105.4–106.8 plaque-forming units [PFU]/dose, depending on the study19–22) and has been administered to millions of children with no reported serious adverse events.15,23–26 The World Health Organization (WHO) prequalified the JEV SA14-14-2 vaccine in October of 2013.
The SA14-14-2 vaccine strain was derived from wild-type (WT) JEV strain SA14, which was originally isolated from mosquito larvae by numerous passages in mouse brain. The JEV SA14 underwent 100 passages in primary hamster kidney (PHK) cells, several plaque purifications in primary chick embryo cells, peripheral passages in Syrian hamsters, and suckling mice, followed by additional plaque purifications in PHK cells, which resulted in the accumulation of attenuating mutations found in the JEV SA14-14-2 genome.27–30 There appear to be multiple attenuating mutations in the JEV SA14-14-2 E protein,31 however E-E138K seems to be particularly important.31–35 Interestingly, a recombinant WT JEV Nakayama virus bearing the 5′ UTR, C, prM, and E genes of JEV SA14-14-2 had residual neurovirulence in mice, indicating that mutations located outside the structural protein genes might also contribute to attenuation.36 More recently it was shown that a single nucleotide change in the JEV SA14-14-2 NS2A coding region that ablates NS1′ formation contributes to the attenuation phenotype.37 Furthermore, JEV SA14-14-2 appears to be more sensitive to type I IFN in tissue culture than some WT JEV strains,38 which might be a result of less efficient type I IFN signaling antagonism by its NS5 protein,39 and this probably contributes to its attenuation as well. However, the complete set of mutations that contribute to balanced attenuation and immunogenicity of JEV SA14-14-2 have not been fully elucidated.
International use of the JEV SA14-14-2 vaccine was limited, for many years, by safety concerns related to its production in PHK cells, which require maintenance of pathogen-free hamster colonies as a source of kidneys for cell culture in medium containing bovine serum.18 The continuous Vero cell line, originally derived from African green monkey kidney, offers several advantages over PHK cells. A qualified WHO Vero cell bank was established for the production of biological products40 and methods for large-scale vaccine production are well established.41,42 Furthermore, Vero cells are highly permissive to viral infection,43 which is likely caused by a defect in type I IFN production.44 Previous attempts have been made to adapt JEV SA14-14-2 to more suitable cell substrates and have resulted in mutations in the virus that reduced vaccine immunogenicity.22,27,45 In the current study, several genetically distinct Vero cell-adapted JEV SA14-14-2 variants were isolated and a recombinant clone bearing the polyprotein amino acid sequence of JEV SA14-14-2 was constructed and recovered in Vero cells. The in vitro and in vivo phenotypes of these viruses were compared and suggest that Vero cells are a suitable substrate for the development of a safe and immunogenic, second-generation, live-attenuated JEV SA14-14-2 vaccine.
Materials and Methods
Cells.
The WHO Vero (African green monkey kidney) cells were maintained at 37°C in OptiPRO SFM (serum-free medium) (Gibco) supplemented with 4 mM L-glutmaine (Gibco). Raji (human B-cell lymphoblast) cells were maintained at 37°C in RPMI 1640 medium (Gibco) supplemented with 10% FBS (HyClone, GE Healthcare Life Sciences, Logan, UT), 2 mM L-glutamine, and 100 U/mL penicillin-streptomycin (Gibco). The HEK-293T (human kidney) cells were maintained at 37°C in EMEM (Lonza, Basel, Switzerland) supplemented with 10% FBS, 2 mM L-glutamine, and 100 U/mL penicillin-streptomycin.
Viruses.
The JEV genotype I strain M859 (Cambodia/67), genotype II strain B1065 (Thailand/83), genotype III strain 7812474 (India/78), and genotype IV strain JKT7003 (Indonesia/Java/81)46 were obtained from the World Reference Center for Emerging Viruses and Arboviruses (University of Texas Medical Branch (UTMB), Galveston, TX). Virus stocks were passed once in Vero cells to generate working stocks. The recombinant (r) JEV strain (rJEV India/78) was derived from a complementary DNA (cDNA) clone that has been described previously.47 The JEV SA14-14-2 strain was obtained from laboratory archives and was passed once in Vero cells to obtain a working stock that was sequenced.
Generation of Vero-adapted JEV SA14-14-2 variants.
Vero cell-adapted JEV SA14-14-2 variants were isolated by performing at least two rounds of terminal endpoint dilutions of the JEV SA14-14-2 laboratory stock in Vero cells. These biological clones underwent two additional rounds of amplification in Vero cells to generate working stocks that were sequenced. The JEV SA14-14-2 stock also underwent multiple passages in Vero cells stimulated with 10 U/mL of human IFN-α A/D (Sigma-Aldrich St. Louis, MO, catalog no. I4401) that is active on Vero cell monolayers. This was followed by biological cloning and amplification in Vero cells, in the absence of IFN-treatment, and sequencing.
Construction of rJEVmut14-14-2.
The cDNA clone of WT rJEV India/78, which has been described previously,47 was modified to closely match the polyprotein amino acid sequence of the JEV SA14-14-2 GenBank reference strain (accession no. JN604986)48 and was designated pJEVmut14-14-2. Synthesized cDNA gene segments encoding point mutations were cloned into pJEV India/78 (Figure 1). The T39A (5′ UTR) and T292C (C-L66S) mutations were cloned as an AscI-BsiWI cDNA fragment. Mutations G4403T/A4408G (NS2B-E63D/D65G) and A4782G/C4921G/T4922C (NS3-M59V/A105G) were cloned as an FseI-StuI fragment. Mutation A7227G (NS4B-I106V) was cloned as a BclI-MluI fragment. Mutations T9688C (NS5-V671A) and T10428C (3′ UTR) were cloned as a PmlI-Acc65I fragment. The remaining portions of the recombinant clone were derived from polymerase chain reaction (PCR) amplified cDNA segments of JEV SA14-14-2 (Figure 1). Nucleotides 625–2496, which include a large portion of prM and the entire E gene, were cloned as a BsiWI-PvuI cDNA fragment. Nucleotides 2491–4226, which include the NS1 and NS2A genes, were cloned as a PvuI-FseI cDNA fragment. A portion of the NS5 gene (nucleotides 8162–8952) was cloned as an MluI-PmlI cDNA fragment. To improve stability of the pJEVmut14-14-2 cDNA construct in Escherichia coli, a DNA linker containing multiple stop codons was synthesized with forward sequence 5′-CGTGACTTAACTTAGACTACGAT-3′ and reverse sequence 5′-CGTAGTCTAAGTTAAGTCACGAT-3′. The DNA oligo nucleotides were annealed in vitro and ligated into the PvuI restriction site.
Figure 1.
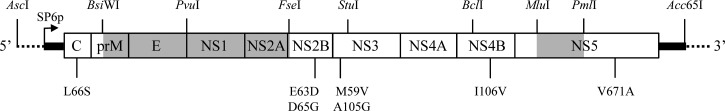
Construction of recombinant Japanese encephalitis virus (JEV)mut14-14-2 cDNA clone. Restriction enzyme recognition sites used for cloning are indicated above the molecule. Synthesized cDNA gene segments were used to introduce amino acid substitutions and these are indicated below the molecule. Regions of the open reading frame (ORF) containing polymerase chain reaction (PCR) amplified cDNA segments of the JEV SA14-14-2 laboratory strain are shaded in gray. The untranslated region (UTR) sequences are indicated in black and flanking vector sequence is indicated with a dotted line. The SP6 polymerase start site (SP6p) used for generating infectious transcripts is indicated.
Recovery of rJEVmut14-14-2.
Recovery of rJEVmut14-14-2 was accomplished by first removing the PvuI stop codon linker sequence with a PvuI digest, followed by in vitro ligation to recircularize the cDNA plasmid. The cDNA construct was subsequently linearized with Acc65I and full genome-length capped RNA transcripts were synthesized with the AmpliCap SP6 Message Maker Kit (Epicentre Biotechologies, Madison, WI). Purified transcripts were transfected in Vero cells using DOTAP liposomal transfection reagent (Roche Basel, Switzerland). Transfected cell culture supernatant was harvested 3 days later and titered in Vero cells. Recovered virus underwent multiple terminal dilutions, followed by amplification in Vero cells to generate a biological clone, which was sequenced.
Virus replication in Vero cells.
Vero cells were infected with viruses at a multiplicity of infection (MOI) of 0.01 PFU/cell for 1 hr, and then washed twice with phosphate buffered saline (PBS) (Gibco) followed by addition of media. The media was harvested on Day 3 post-infection, which corresponded to peak virus titer, and was titered in Vero cells. Plaques were visualized on Day 3 by immunostaining and their relative size (small < 1 mm, medium 1–2 mm, and large > 2 mm) was determined. The results are an average of at least two experiments done in duplicate per virus.
Type I IFN sensitivity assay.
Virus was added to Vero cells in 24-well plates at an MOI of 0.01 PFU/cell and incubated for 1 hr followed by addition of media-only or media containing 10 U/mL of IFN-α A/D (Sigma-Aldrich), in duplicate per experiment. Virus dilutions used for infection were immediately back titrated in Vero cells to ensure consistent doses/well. The supernatant was harvested 72 hr post-infection and titered in Vero cells. Dilution of the supernatant > 100-fold during titering reduced any residual IFN-α to a concentration at which plaque count was not affected (data not shown). The cell monolayers were washed once with PBS, removed with TrypLE select (Life Technologies), transferred to 5 mL tubes with growth medium, and pelleted by centrifugation. Cell pellets were resuspended with FACS Permeabilizing Solution 2 (BD Biosciences, San Jose, CA) and incubated for ∼1 hr at room temperature. The JEV Ag-positive cells were detected by incubating with a JEV hyperimmune mouse ascitic fluid (ATCC, Manassas, VA) diluted in PBS containing 10% albumin (wash solution) and then with a FITC-goat anti-mouse H+L antibody (Biolegend, San Diego, CA) diluted in wash solution. The cells were washed twice with PBS, resuspended in PBS with 0.01% EDTA, and data were collected using an Accuri C6 flow cytometer (BD Biosciences) and analyzed with Flowjo software version X.0.7 (Flowjo, Ashland, OR).
Mouse studies.
Studies in mice were performed in accordance with the regulations and guidelines of the National Institutes of Health (NIH) (Bethesda, MD) and approved by the Animal Care and Use Committee of National Institute of Allergy and Infectious Diseases (NIAID). Viruses were tested for neuroinvasiveness by intraperitoneal (IP) inoculation and neurovirulence by intracerebral (IC) inoculation of 3-week-old (weanling) female Swiss Webster (SW) mice (Taconic, Derwood, MD). Groups of 10 mice were administered a 0.1 mL dose IP or a 0.01 mL dose IC of virus dilution and monitored for 21 days for signs of encephalitis. On Day 28, serum was collected from IP inoculated mice for neutralization assays. Viruses were also tested for neurovirulence by IC inoculation of 3-day-old (suckling) SW mice. Litters of 10 mice were administered a 0.01 mL dose of virus dilution and monitored for 21 days for signs of encephalitis. Clinical signs of encephalitis leading to a moribund state included tremors, seizure, and paralysis. Moribund mice were humanely euthanized to minimize pain and distress. The LD50 values were determined by the method of Reed and Muench.49
Production of JEV reporter virus particles (RVPs).
A BsiWI-MfeI cDNA fragment corresponding to the JEV SA14-14-2 E gene and a portion of prM was cloned into mammalian expression vector pJEV-CprME.47 The JEV SA14-14-2 RVPs expressing green fluorescent protein (GFP) were produced in HEK 293T cells, as described previously.47,50,51 The RVP titers were determined by serial dilution of JEV RVP stocks and infecting Raji cells in 96-well plates. The RVP-infected cells were fixed with paraformaldehyde and the percentage of GFP expressing cells was determined by flow cytometry.
JEV RVP serum neutralization assay.
The JEV RVP serum neutralization assay was carried out as described previously.47 The data were analyzed using GraphPad Prism (GraphPad Software, La Jolla, CA) and were fit by a dose–response curve (variable slope) to determine the 50% effective neutralization concentration (EC50). An immunized mouse seroconverted if its serum had a detectable EC50. Titers are reported as the reciprocal geometric mean EC50 titer.
Statistical analysis.
Statistical analyses were done using GraphPad Prism. Virus titer or number of virus Ag-positive cells with or without IFN-α treatment was analyzed using a two-way analysis of variance (ANOVA). The Pearson correlation coefficient (r) was calculated, with P < 0.05 required for significance, to assess relationships between virus titer, number of virus Ag-positive cells, and IFN-α treatment. Mouse survival analyses were done using the Log-rank (Mantel-Cox) test, with P < 0.05 required for significance.
Results
Sequence comparison of JEV SA14-14-2 variants.
The consensus sequence of the JEV SA14-14-2 laboratory stock differed by a single amino acid substitution (NS3-A235V) relative to a recently published “reference sequence” (GenBank accession no. JN604986) of a commercial batch of JEV SA14-14-2 vaccine (Table 1).48 Careful examination of the sequence chromatograms revealed that there were also minor secondary peaks at several positions throughout the genome indicating there was a mixture of nucleotides and predicted amino acid substitutions (Table 1). Biological cloning of this virus stock in Vero cells resulted in the isolation of six genetically distinct, Vero cell-adapted variants (A, B, C, D, G, and H). These virus variants all contained nucleotide change C292T (S66L amino acid change) in the C protein gene, which appeared as a mixture of C and T nucleotides in the consensus sequence of the original laboratory virus stock (Table 1). Therefore, the principal virus in the JEV SA14-14-2 laboratory stock, bearing C-S66, was negatively selected during Vero cell-adaptation, which resulted in reversion to the Leu codon found in WT JEV. The sequence of all six Vero-adapted JEV SA14-14-2 variants also differed from the reference sequence by nucleotide change C5311T, resulting in mutation NS3-A235V, just like the original virus stock. The sequences of JEV SA14-14-2 variants A and G also contained four unique mutations compared with the reference sequence (Table 1). The sequences of JEV SA14-14-2 variants B, C, and D each contained a total of seven reversion mutations (> 90% frequency in WT JEV strains), including C-S66L, and variants B and C each had two unique changes compared with the reference sequence (Table 1). All of the mutations in variants A and D appeared as mixtures of nucleotides and predicted amino acids in the consensus sequence of the JEV SA14-14-2 stock, suggesting that these variants had been dominant (Table 1).
Table 1.
Comparison of genetic differences between Vero cell-adapted JEV SA14-14-2 variants
| Nucleotide | Gene | Amino acid | GenBank Ref* | Laboratory stock† | H | 2IFN | 1IFN | A | G | D | 3IFN,‡ | B | C | 5IFN | Type of mutation§ | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 59 | 5′UTR | − | G | • | /A | • | • | A | A | • | • | • | • | • | • | Rare | |
| 292 | C | 66 | Ser | • | /Leu | Leu | Leu | Leu | Leu | Leu | Leu | Leu | Leu | Leu | Leu | Reversion | |
| 937 | prM | 154 | Val | • | • | • | • | • | Ala | • | • | • | • | • | Rare | ||
| 995 | E | 6 | Met | • | • | Ile | • | • | • | • | • | • | • | • | Rare | ||
| 1506 | E | 177 | Ala | • | /Thr | • | • | • | • | • | Thr | Thr | Thr | Thr | Thr | Reversion | |
| 1769 | E | 264 | His | • | /Gln | • | • | • | • | • | Gln | Gln | Gln | Gln | Gln | Reversion | |
| 2159 | E | 394 | His | • | • | • | • | • | • | • | • | • | Gln | • | Rare | ||
| 2445 | E | 490 | Val | • | • | • | • | • | Leu | • | • | • | • | • | Rare | ||
| 2630 | NS1 | 51 | Lys | • | • | • | • | • | Asn | • | • | • | • | • | Rare | ||
| 2998 | NS1 | 174 | Glu | • | /Gly | • | • | • | Gly | • | • | • | • | • | • | Rare | |
| 3528 | NS1 | 351 | His | • | /Asp | • | • | • | • | • | Asp | Asp | Asp | Asp | Asp | Reversion | |
| 3599¶ | NS2A | 22 | Glu (A) | • | /(G) | • | • | • | • | • | (G) | (G) | (G) | (G) | (G) | Reversion | |
| 3652 | NS2A | 40 | Val | • | • | • | • | • | • | • | Ala | • | • | • | Reversion | ||
| 4295 | NS2B | 27 | Glu | • | • | • | • | • | • | • | • | • | • | Asp | Rare | ||
| 4656 | NS3 | 17 | Asp | • | • | • | • | • | • | • | • | Asn | • | • | Rare | ||
| 4672 | NS3 | 22 | Val | • | • | • | • | • | • | • | • | • | • | Ala | Rare | ||
| 4786 | NS3 | 60 | Ser | • | /Asn | • | • | Asn | Asn | • | • | • | • | • | • | Rare | |
| 4924 | NS3 | 106 | Ala | • | • | • | • | • | • | • | • | • | Val | • | Rare | ||
| 5311 | NS3 | 235 | Ala | Val | Val | • | Val | Val | Val | Val | Val | Val | Val | Val | Rare | ||
| 6474 | NS4A | 4 | Ser | • | • | Gly | • | • | • | • | • | • | • | • | Rare | ||
| 6702 | NS4A | 80 | Met | • | /Leu | • | • | Leu | Leu | • | • | • | • | • | • | Rare | |
| 9549 | NS5 | 625 | Leu | • | • | • | • | • | Met | • | • | • | • | • | Rare | ||
| 9593 | NS5 | 639 | His | • | /Gln | • | • | • | • | • | Gln | Gln | Gln | Gln | Gln | Reversion | |
| 9688 | NS5 | 671 | Ala | • | /Val | • | • | • | • | • | Val | Val | Val | Val | Val | Reversion | |
| 9718 | NS5 | 681 | Thr | • | • | • | • | • | • | • | • | Met | • | • | Rare | ||
| Reversion mutations: | – | 0 | / 7 | 1 | 1 | 1 | 1 | 1 | 7 | 8 | 7 | 7 | 7 | ||||
| Total mutations: | – | 1 | / 12 | 2 | 3 | 5 | 6 | 6 | 8 | 9 | 10 | 10 | 10 | ||||
Consensus sequence of JEV SA14-14-2 laboratory stock with mixed nucleotides and encoded amino acids indicated.
JEV SA14-14-2 variant 4IFN had an identical sequence.
Reversion mutations (> 90% frequency) or rare mutations (< 10% frequency) among wild-type JEV sequences determined using FLAVIdB (http://cvc.dfci.harvard.edu/flavi/index.php).
¶Nucleotide change in NS2A identified as a virulence determinant.37 Both A and G nucleotides code for Glu.
The PHK cells used for propagation of vaccine lots of JEV SA14-14-2 are capable of producing type I IFN in response to viral infection,52 and this could be important for maintaining genetic and phenotypic properties of the vaccine. Vero cells, however, have a defect in type I IFN production, but are capable of responding to stimulation by these cytokines.44 Therefore, the JEV SA14-14-2 stock was also passaged in Vero cells treated with a low dose of IFN-α followed by biological cloning and a total of five virus variants were isolated (1IFN–5IFN). These virus variants shared the C-S66L mutation and all but one had the NS3-A235V mutation (Table 1). The sequence of JEV SA14-14-2 variant 1IFN was most similar to variant A, but contained substitution NS1-G174E, a change to the reference sequence at this position (Table 1). The JEV SA14-14-2 variant 2IFN differed from the reference sequence and variant H by three mutations and had unique mutations in E and NS4A (Table 1). The JEV SA14-14-2 variants 3IFN, 4IFN, and 5IFN shared NS3-A235V and the six reversion mutations specific to variants B, C, and D (Table 1). The JEV SA14-14-2 variants 3IFN and 4IFN had identical sequences, and differed from variant D by reversion mutation NS2A-V40A (Table 1). The JEV SA14-14-2 variant 5IFN differed from variant D by unique substitutions in NS2B and NS3 (Table 1). Thus, Vero-adapted JEV SA14-14-2 variants isolated with IFN-α treatment were genetically distinct but representative of those isolated without treatment.
Recovery of rJEVmut14-14-2.
The polyprotein amino acid sequence of rJEVmut14-14-2 was designed to closely match the sequence of a commercial batch of vaccine virus (Table 2).48 Other JEV SA14-14-2 full genome sequences that have been published are shown in Table 2 for comparison and differ considerably from one another. Recombinant JEVmut14-14-2 was recovered and biologically cloned in Vero cells and the sequence of this virus matched that of the cDNA clone. The genetic stability of this virus was determined by performing six additional passages in Vero cells, in duplicate, followed by sequencing of the virus genomes. At passage six, a single nucleotide change (C292T) was identified for both independent passages, resulting in reversion mutation C-S66L that was also found in all Vero-adapted JEV SA14-14-2 variants, confirming that this single mutation is important for Vero cell-adaptation.
Table 2.
Comparison between published JEV SA14-14-2 reference sequence, rJEVmut14-14-2, and two additional full genome sequences of JEV SA14-14-2
| nt | Gene | aa | JN604986a | rJEVmut 14-14-2 | D90195* | AF315119* |
|---|---|---|---|---|---|---|
| 2317 | E | 447 | Gly | • | • | Asp |
| 4475 | NS2B | 87 | Leu | • | • | Phe |
| 5311 | NS3 | 235 | Ala | • | Val | Val |
| 5634 | NS3 | 343 | Arg | • | Trp | • |
| 6634 | NS4A | 27 | Ile | • | Thr | • |
| 7768 | NS5 | 31 | Ala | • | • | Gly |
| 7809 | NS5 | 45 | Arg | • | • | Ser |
| 8261 | NS5 | 195 | Met | • | • | Ile |
| 9593 | NS5 | 639 | His | Gln | Gln | • |
| 9954 | NS5 | 759 | Ala | • | • | Pro |
| 9978 | NS5 | 767 | Leu | • | • | Val |
| 10407 | 3′UTR | − | T | C | • | • |
| 10414 | 3′UTR | − | G | A | • | • |
| 10417 | 3′UTR | − | G | A | • | • |
| 10447 | 3′UTR | − | C | T | • | • |
| 10451 | 3′UTR | − | C | T | • | • |
| 10455 | 3′UTR | − | T | C | • | • |
| 10511 | 3′UTR | − | T | C | • | • |
| 10550 | 3′UTR | − | A | G | • | • |
| 10574 | 3′UTR | − | C | • | • | T |
| 10585 | 3′UTR | − | T | C | • | • |
| 10648 | 3′UTR | − | A | G | • | • |
| 10701 | 3′UTR | − | G | • | − | − |
| 10785 | 3′UTR | − | C | • | T | • |
| 10800 | 3′UTR | − | C | T | • | • |
| 10950 | 3′UTR | − | G | • | • | C |
| 10951 | 3′UTR | − | C | • | • | G |
Phenotype in Vero cells.
All JEV SA14-14-2 variants produced small plaques (< 1 mm) and had mean peak titers of 7.0–7.8 log10 PFU/mL (Table 3). Recombinant JEVmut14-14-2 also produced small plaques but had a moderately lower mean peak titer of 6.4 log10 PFU/mL (Table 3), which is consistent with the titer reported for JEV SA14-14-2 in baby hamster kidney cells.48 Recombinant JEVmut14-14-2-C292T, with reversion mutation C-S66L, replicated to a significantly higher mean peak titer of 7.1 log10 PFU/mL, similar to most JEV SA14-14-2 variants (Table 3). The JEV SA14-14-2 variant 3IFN had a single unique reversion mutation, NS2A-V40A, relative to JEV SA14-14-2 variant D (Table 1) that significantly increased mean peak virus titer (Table 3). The WT JEV strains produced large plaques (> 2 mm) and had the highest mean peak titers of 7.9–8.3 log10 PFU/mL in Vero cells (Table 3).
Table 3.
Virus phenotype in Vero cells
| Virus | Plaque size* | Mean peak titer† |
|---|---|---|
| rJEVmut14-14-2 | Small | 6.4 ± 0.0 |
| rJEVmut14-14-2-C292T | Small | 7.1 ± 0.1‡ |
| JEV SA14-14-2 | Small | 7.2 ± 0.3 |
| JEV SA14-14-2 A | Small | 7.1 ± 0.3 |
| JEV SA14-14-2 B | Small | 7.4 ± 0.3 |
| JEV SA14-14-2 C | Small | 7.1 ± 0.4 |
| JEV SA14-14-2 D | Small | 7.3 ± 0.4 |
| JEV SA14-14-2 G | Small | 7.0 ± 0.4 |
| JEV SA14-14-2 H | Small | 7.2 ± 0.3 |
| JEV SA14-14-2 1IFN | Small | 7.3 ± 0.2 |
| JEV SA14-14-2 2IFN | Small | 7.3 ± 0.1 |
| JEV SA14-14-2 3IFN | Small | 7.8 ± 0.2§ |
| JEV SA14-14-2 5IFN | Small | 7.3 ± 0.1 |
| JEV Cambodia/67 (GI)¶ | Large | 8.3 ± 0.1 |
| JEV Thailand/83 (GII)¶ | Large | 8.0 ± 0.0 |
| rJEV India/78 (GIII)¶ | Large | 8.1 ± 0.2 |
| JEV Indonesia/Java/81 (GIV)¶ | Large | 7.9 ± 0.0 |
Measured 3 days post-infection: small < 1 mm, large > 2 mm.
Log10 PFU/mL ± SD from at least two experiments in duplicate per virus.
Significantly different from rJEVmut14-14-2 by ANOVA with Tukey's test (P < 0.05).
Significantly different from JEV SA14-14-2 D by ANOVA with Tukey's test (P < 0.05).
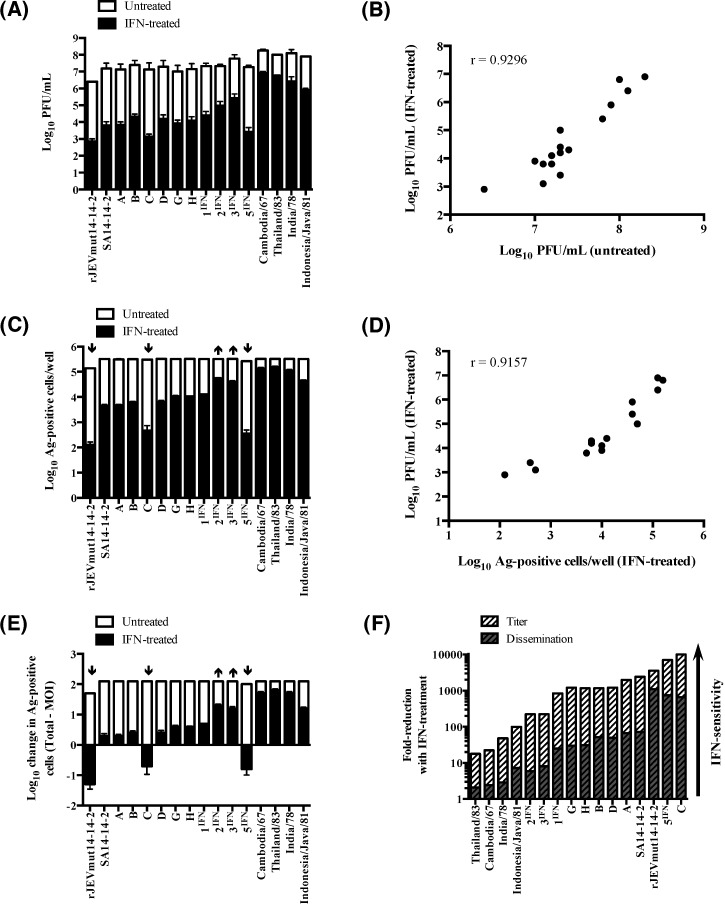
Increased sensitivity to type I IFN is an additional phenotype that has previously been associated with JEV SA14-14-2 and can be observed in IFN-treated tissue culture cells.38,39 Therefore, virus titer and virus Ag-positive cells were measured at 3 days post-infection in IFN-α-treated Vero cell monolayers. This time-point was chosen because it accurately represented the cumulative effect of IFN-α treatment on virus replication over the course of 3 days in tissue culture. The IFN-α treatment significantly reduced virus titer for all JEV strains tested (Figure 2A) and there was a significant, positive correlation (r = 0.9296, P = < 0.0001) between virus titer with and without treatment (Figure 2B), indicating that virus replicative fitness is important for overcoming the antiviral effects of type I IFN-stimulation. Recombinant JEVmut14-14-2 had significantly less Ag-positive cells compared with other JEV strains that disseminated to the entire Vero cell monolayer (≈5.5 log10 cells/well), however this was reduced significantly with IFN-α treatment (Figure 2C). There was also a significant, positive correlation (r = 0.9157, P = < 0.0001) between the number of Ag-positive cells and virus titer, with IFN-α treatment, whereby viruses that infected more cells grew to higher titer (Figure 2D). In IFN-α treated Vero cell monolayers, WT JEV strains disseminated most effectively beyond the initial MOI (≈3.4 log10 cells), whereas most JEV SA14-14-2 variants had low or intermediate levels of dissemination by comparison (Figure 2E). Interestingly, JEV SA14-14-2 variants 2IFN and 3IFN disseminated in IFN-α treated Vero cell monolayers to a similar extent as WT JEV strain Indonesia/Java/81 and significantly more than rJEVmut14-14-2, JEV SA14-14-2, and other variants (Figure 2C and E). By contrast, cell-to-cell spread of rJEVmut14-14-2 and JEV SA14-14-2 variants C and 5IFN was completely restricted by treatment with IFN-α and consequently these viruses had significantly less Ag-positive cells than all other viruses (Figure 2C and E).
Figure 2.
Sensitivity of Japanese encephalitis virus (JEV) strains to type I interferon (IFN)-treatment of Vero cells. Vero cells were infected at an multiplicity of infection (MOI) of 0.01 PFU/cell, followed by addition of medium-only (untreated) or medium containing 10 U/mL of IFN-α (IFN-treated) and the supernatant and cells were harvested 72 hours post-infection. (A) The supernatants were titered in Vero cells. (B) There was a significant positive correlation between virus titer with and without IFN-α treatment (r = 0.9296, P = < 0.0001). (C) The number of virus antigen (Ag)-positive cells was determined by immunostaining and flow cytometry. (D) There was a significant positive correlation between the number of virus Ag-positive cells and virus titer, with IFN-α treatment (r = 0.9157, P = < 0.0001). All viruses experienced significant reductions in titer and Ag-positive cells with IFN-α treatment (P < 0.05 by analysis of variance [ANOVA] with Sidak's test). (E) The amount of virus dissemination beyond the initial MOI (≈ 3.4 log10 cells) is presented. Viruses with significant increases (↑) or decreases (↓) in virus Ag-positive cells (panel C) and dissemination beyond the MOI (panel E) relative to JEV SA14-14-2 and other virus variants are indicated (P < 0.05 by ANOVA with Tukey's test). (F) The mean fold-reductions in virus titer and dissemination with IFN-α treatment are presented and the viruses are arranged according to their relative level of type I IFN-sensitivity. For panels A, C, and E, error bars represent the SD from two or more experiments performed in duplicate per virus.
The level of type I IFN-sensitivity was quantified by calculating fold-reductions in virus titer and dissemination in the cell monolayer with IFN-α treatment. In Figure 2F, the viruses are arranged according to their relative level of type I IFN-sensitivity. For all viruses, fold-reductions in titer exceeded fold-reductions in dissemination. The WT JEV strains were the least sensitive to IFN-α treatment, having ≤ 7-fold reductions in dissemination and ≤ 100-fold reductions in titer (Figure 2F). Most JEV SA14-14-2 variants had an intermediate level of type I IFN-sensitivity, with ≥ 25-fold reductions in dissemination and > 800-fold reductions in titer, with IFN-α treatment (Figure 2F). Recombinant JEVmut14-14-2 and JEV SA14-14-2 variants C and 5IFN had remarkably high levels of type I IFN-sensitivity caused by their inability to disseminate in IFN-α treated Vero cell monolayers, resulting in 1,000-fold reductions in dissemination and > 3,000-fold reductions in virus titer (Figure 2F). Whereas, JEV SA14-14-2 variants 2IFN and 3IFN had type I IFN-sensitivity levels similar to WT JEV strain Indonesia/Java/81, indicating that passage of the original virus stock in IFN-α treated Vero cells enriched for more resistant virus variants (Figure 2F). It is difficult to ascribe IFN-sensitivity to specific mutations, however, at least one of three amino acid substitutions (E-M6I, NS3-V235A, and NS4A-S4G) that differentiated JEV SA14-14-2 variant 2IFN from variant H and the NS2A-V40A mutation that differentiated JEV SA14-14-2 variant 3IFN from variant D (Table 1) conferred a ≥ 5-fold significantly decreased level of sensitivity to IFN-α treatment (Figure 2F).
Mouse studies.
Virulence was tested in weanling mice by IP and IC routes of inoculation for rJEVmut14-14-2, JEV SA14-14-2, and several JEV SA14-14-2 variants and compared with WT rJEV India/78. Recombinant JEVmut14-14-2, JEV SA14-14-2, and variants A, B, C, D, G, H, and 3IFN caused no mortality by either route of inoculation, similar to mock-infected animals (Table 4). By contrast, WT rJEV India/78 caused significant mortality (Table 4). Immunogenicity was evaluated in weanling mice that were inoculated IP. Immunization with rJEVmut14-14-2 at a 105 PFU dose resulted in 100% seroconversion and high neutralizing antibody titers (Table 4). The other viruses were tested at a 104 PFU dose. The JEV SA14-14-2 stock and all the variant viruses induced 90–100% seroconversion. The JEV SA14-14-2 variants B and D elicited the highest levels of neutralizing antibody, with variant G eliciting the lowest level. However, mean titers of neutralizing antibodies elicited by all the variants, except variant G, differed no more than 2-fold compared with JEV SA14-14-2 (Table 4).
Table 4.
Virulence and immunogenicity of JEV SA14-14-2 variants in weanling mice
| Virus | Dose (PFU) | Virulence by indicated Inoculation route | Immunogenicity* | |||
|---|---|---|---|---|---|---|
| Number alive/total | Seroconversion | Reciprocol EC50 | ||||
| IC | IP | GMT | Range | |||
| rJEVmut14-14-2 | 105 | 10/10 | 10/10 | 10/10 | 1951 | 357–7194 |
| JEV SA14-14-2 | 104 | 10/10 | 10/10 | 10/10 | 584 | 167–2790 |
| JEV SA14-14-2 A | 104 | 10/10 | 10/10 | 9/10 | 357 | < 8–2195 |
| JEV SA14-14-2 B | 104 | 10/10 | 10/10 | 10/10 | 791 | 107–4852 |
| JEV SA14-14-2 C | 104 | 9/9† | 10/10 | 10/10 | 319 | 56–1062 |
| JEV SA14-14-2 D | 104 | 9/9† | 10/10 | 10/10 | 1058 | 349–4172 |
| JEV SA14-14-2 G | 104 | 10/10 | 10/10 | 9/10 | 137 | < 8–657 |
| JEV SA14-14-2 H | 104 | 10/10 | 10/10 | 9/10 | 316 | < 8–1702 |
| JEV SA14-14-2 3IFN‡ | 104 | 10/10 | 10/10 | 10/10 | 624 | 337–1467 |
| Mock | − | 10/10 | 10/10 | 0/10 | < 8 | < 8 |
| rJEV India/78 | 102 | 0/5 | 2/5 | ND§ | ND | ND |
Evaluated for mice inoculated with virus by the IP route.
A single mouse died of trauma at the injection site.
This virus was evaluated in a second, independent experiment.
ND = not determined.
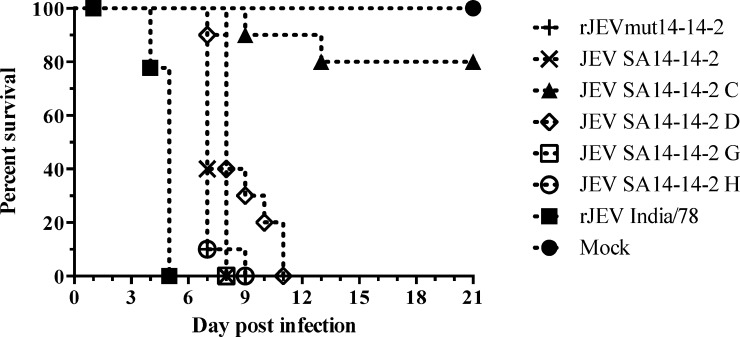
Neurovirulence was tested in suckling mice for a subset of viruses. Recombinant JEV India/78 was the most virulent in this model with an IC LD50 of 0.2 PFU and mice had a median survival time of 5 days (Table 5). The IC LD50 level for JEV SA14-14-2 variant H was similar to rJEV India/78 but mice had a significantly longer, 7 days, median survival time (Table 5 and Figure 3). The JEV SA14-14-2 and rJEVmut14-14-2 infected mice had the same median survival time as variant H, but slightly higher IC LD50 levels (Table 5). The other JEV SA14-14-2 variants that were tested were significantly more attenuated. The JEV SA14-14-2 variant G differed from variant H by four amino acid substitutions and had a 10-fold higher IC LD50 and mice had a significantly longer, 8 days, median survival time (Table 5 and Figure 3). Similarly, JEV SA14-14-2 variant D differed from variant H by six reversion mutations (Table 1), and had a 17-fold higher IC LD50 and mice had an 8-day median survival time (Table 5 and Figure 3). The most attenuated virus was JEV SA14-14-2 variant C, which differed by two unique mutations from variant D (Table 1) that increased the IC LD50 level > 60-fold and 80% of mice survived a 102 PFU dose (Table 5 and Figure 3 ). Thus, increased amino acid sequence divergence of Vero-adapted JEV SA14-14-2 variants from the reference vaccine strain appears to correlate with increased attenuation in suckling mice.
Table 5.
Virulence of JEV SA14-14-2 variants in suckling mice
| Virus | IC LD50 (PFU) | Median survival time (days)* | Amino acids different from variant H |
|---|---|---|---|
| rJEV India/78 | 0.2 | 5 | 30 |
| JEV SA14-14-2 H | 0.1 | 7† | − |
| JEV SA14-14-2 | 0.7 | 7† | 1 |
| rJEVmut14-14-2 | 0.8 | 7† | 3 |
| JEV SA14-14-2 G | 1.0 | 8†‡ | 4 |
| JEV SA14-14-2 D | 1.7 | 8†‡ | 5 |
| JEV SA14-14-2 C | > 100.0 | > 21†§ | 7 |
| Mock | NA | > 21 | − |
102 PFU dose (highest dose tested) (N = 10).
Survival curve is statistically different from rJEV India/78 by Log-rank test.
Survival curve is statistically different from JEV SA14-14-2 variant H by Log-rank test++.
Survival curve is statistically different from all other viruses tested by Log-rank test.
Figure 3.
Survival of suckling mice after virus inoculation. Groups of 10 mice were inoculated intracerebral (IC) with 102 PFU of virus or mock infected and monitored for 21 days for signs of encephalitis. Survival curves after inoculation with rJEVmut14-14-2, JEV SA14-14-2, and variants C, D, G, and H were statistically different from WT rJEV India/78 (Log-rank test, P ≤ 0.0001). The survival curve for Japanese encephalitis virus (JEV) SA14-14-2 variant C was statistically different from all other viruses tested (Log-rank test, P ≤ 0.0001). The survival curves for JEV SA14-14-2 variants D and G were statistically different from variant H by Log-rank test (P = 0.0023).
Discussion
The live-attenuated JEV SA14-14-2 vaccine has a proven record of safety and efficacy,15,27 but its current production in PHK cells requires maintenance of pathogen-free hamster colonies as a source of kidneys for cell culture, which is a safety concern and adds to production costs.18 In addition, several laboratories have sequenced the JEV SA14-14-2 vaccine strain over the last 20 years with significantly different results27,28,48 (Table 2), suggesting that the vaccine seed virus is not clonal, and this could affect attenuation and immunogenicity between vaccine lots. It was for these reasons that we initiated the development of a second-generation, recombinant JEV SA14-14-2 live-attenuated vaccine produced in WHO qualified Vero cells.
In this study, we isolated 10 genetically distinct Vero cell-adapted JEV SA14-14-2 variants. Because Vero cells are defective in type I IFN production, unlike PHK cells, a subset of virus variants was isolated after passage in Vero cells treated with a low dose of IFN-α. A single C-S66L reversion mutation was present in all Vero-adapted virus variants and indicated that the dominant strain in the original virus stock containing Ser at amino acid 66, was negatively selected during biological cloning steps in Vero cells. A similar observation was very recently reported by Yang and colleagues35 following serial passage of JEV SA14-14-2 in Vero cells. A recombinant JEV mutant (rJEVmut14-14-2) containing a polyprotein amino acid sequence nearly identical to the JEV SA14-14-2 GenBank reference sequence (accession no. JN604986) was constructed and recovered in Vero cells. Although the rJEVmut14-14-2 virus retained the engineered Ser at amino acid 66 after biological cloning steps, six additional passages resulted in reversion of this mutation to Leu, which also significantly increased virus titer. These observations strongly suggest that reversion mutation C-S66L is required for adaptation of JEV SA14-14-2 to replication in Vero cells.
The host type I IFN response is critical for restricting replication and dissemination of flaviviruses10,54–57 and JEV SA14-14-2 is capable of inducing morbidity in IFN-deficient mice,58 indicating that innate-immune antiviral mechanisms contribute to its attenuated phenotype. Studies in primary human monocyte-derived macrophages showed that JEV SA14-14-2 induced similar levels of type I IFN as WT JEV but is more sensitive to its affects.38 Therefore, we determined the type I IFN-sensitivity phenotype in Vero cells for the JEV SA14-14-2 derived virus variants generated in this study. Overall, viruses that replicated most effectively in Vero cells, like WT JEV strains, were more resistant to the antiviral effects of type I IFN-treatment. Consequently, reversion mutations like C-S66L and NS2A-V40A that improved replication in Vero cells also appeared to increase resistance to type I IFN-stimulation. The combination of these two reversion mutations in JEV SA14-14-2 variant 3IFN significantly improved type I IFN-resistance in Vero cells to nearly WT levels. Previously, it was shown that the JEV NS2A protein antagonizes the activity of type I IFN-induced protein kinase R that contributes to inducing an intracellular antiviral state, and mutation NS2A-T33I abolished this activity, decreased virus titer in tissue culture, and reduced virulence in mice.59 Therefore, mutation NS2A-A40V, which is proximal to NS2A-T33I, might contribute to type I IFN-sensitivity and attenuation of JEV SA14-14-2 by a similar mechanism, but was not critical for attenuation of JEV SA14-14-2 variant 3IFN in weanling mice.
There were also unique mutations identified in some JEV SA14-14-2 variants that modulated type I IFN-sensitivity in Vero cells and were not linked to improved virus replication. The JEV SA14-14-2 variant 2IFN had a nearly WT level of resistance to type I IFN-treatment that was produced by mutations E-M6I, NS3-V235A, or NS4A-S4G, but lacked the NS2A-V40A mutation associated with IFN resistance in the 3IFN variant. By contrast, JEV SA14-14-2 variants C and 5IFN had remarkably high levels of type I IFN-sensitivity produced by mutations E-H394Q or NS3-A106V and NS2B-E27D or NS3-V22A, respectively. Previously, it was shown that a single JEV E protein mutation (E138K) increased virus sensitivity to type I IFN, but this phenotype was coupled with altered levels of virus replication in tissue culture,60 unlike the E protein mutations in JEV SA14-14-2 variants 2IFN and C. However, the JEV NS4A protein and the NS2B and NS3 proteins of genetically related West Nile virus Kunjin are known to function as type I IFN-antagonists.61,62 Therefore, it is likely that one or more unique non-structural protein mutations in JEV SA14-14-2 variants C, 2IFN and 5IFN modulated sensitivity to type I IFN in Vero cells.
The virulence phenotype for subsets of Vero-adapted JEV SA14-14-2 variants was tested in weanling and suckling mice. The genetically diverse JEV SA14-14-2 variants were avirulent in weanling mice, even though some had as many as 10 mutations, including seven reversion mutations relative to the reference strain. Of importance, this indicated that mutations acquired during Vero cell-adaptation did not alter the attenuated phenotype of the JEV SA14-14-2 variants in weanling mice, although the variants differed in their level of attenuation in suckling mice. Recombinant JEVmut14-14-2 and the JEV SA14-14-2 laboratory stock sequence had the least amino acid sequence divergence from the reference strain and had virulence phenotypes in suckling mice consistent with what has been reported for JEV SA14-14-2.45 The JEV SA14-14-2 variant H differed from the JEV SA14-14-2 laboratory stock sequence by only the reversion mutation C-S66L and had a similar level of virulence. Surprisingly, Vero-adapted virus variants with more amino acid sequence divergence than variant H were significantly more attenuated in suckling mice. The most attenuated virus was JEV SA14-14-2 variant C, which differed from variant D by mutations E-H394Q and NS3-A106V and at least one of these mutations had a dominant attenuating effect in suckling mice, which might be linked to its remarkably high level of type I IFN-sensitivity. The JEV SA14-14-2 variant C also contained a group of six reversion mutations (E-A177T, E-H264Q, NS1-H351D, NS2A nucleotide change A3599G, NS5-H639Q, and NS5-A671V) that were shared with JEV SA14-14-2 variant D and significantly increased attenuation in suckling mice. Only one of these mutations, nucleotide change G3599A that ablates NS1′ formation, was shown to be attenuating in mice.37 Mutations E-T177A and E-Q264H were not critical for the attenuated phenotype of ChimeriVax-JE in weanling mice31 and arose during subcutaneous passages of over-attenuated precursor vaccine strain SA14-5-3 in suckling mice to improve immunogenicity, which produced the SA14-14-2 strain.27,63 Consistent with this are studies showing that mutation E-Q264H significantly increased virulence in suckling mice and immunogenicity in weanling mice of a JEV/DEN4 chimeric virus.47 Thus, the collection of mutations E-T177A, E-Q264H, NS1-D351H, NS2A nucleotide change G3599A, NS5-Q639H, and NS5-V671A might have been important for achieving balanced attenuation and immunogenicity in the JEV SA14-14-2 vaccine strain.
Adaptation of JEV SA14-14-2 to other cell substrates, like primary dog kidney (PDK) cells, had resulted in mutations that reduced immunogenicity.22,27,45 The PDK cell-adapted virus was further adapted to Vero cells64 and was used to generate an inactivated JEV vaccine IC-51 (IXIARO)65 (Intercell AG), but was not developed as a live-attenuated vaccine. Here, we attempted to isolate Vero-adapted JEV SA14-14-2 variants that would be suitable live-attenuated vaccine candidates. Recombinant JEVmut14-14-2, the JEV SA14-14-2 laboratory stock, and virus variants A, B, C, D, G, H, and 3IFN were very immunogenic in mice. This was particularly interesting because five of seven reversion mutations (E-A177T, E-H264Q, NS1-H351D, nucleotide change A3599G, and NS5-A671V) in virus variants B, C, D, and 3IFN were also present in JEV SA14-14-2 PDK,27,30,66 which was reported to be moderately immunogenic.27,66 Genetic differences between these Vero-adapted virus variants and the PDK-adapted virus, including C-S66L, E-K243E, NS3-A235V, NS5-T644N, and NS5-H639Q likely account for their higher level of observed immunogenicity.
There are many advantages to producing viral vaccines in WHO qualified Vero cells, therefore we adapted the JEV SA14-14-2 vaccine strain to replicate in this cell line and isolated a set of Vero-adapted virus variants. The genetic determinants that govern the stable attenuation and high level of immunogenicity of JEV SA14-14-2 are not well understood, which prompted us to assess the in vitro and in vivo phenotypes of several genetically distinct virus variants. We identified a single reversion mutation (S66L) in the capsid protein that appeared to be essential for Vero cell-adaption and this mutation significantly improved virus titer in tissue culture without affecting attenuation in weanling mice. The high level of type I IFN-sensitivity exhibited by JEV SA14-14-2 is likely determined by mutations that reduce replicative fitness and also by rare mutations in non-structural proteins that have previously been implicated as type I IFN-antagonists, and might contribute to attenuation. Vero cell-adapted JEV SA14-14-2 variants B, C, D, and 3IFN had excellent attenuation levels in mice and were highly immunogenic, thereby reducing the possibility of producing vaccine candidates with an inferior phenotype to the current live-attenuated vaccine. Future studies will aim to generate recombinant clones of one or more of these Vero-adapted JEV SA14-14-2 variants with the goal of producing a live-attenuated second-generation vaccine.
ACKNOWLEDGMENTS
We thank the NIAID Comparative Medicine Branch for assisting with animal studies.
Footnotes
Financial support: This work was supported by the National Institute of Allergy and Infectious Diseases Intramural Research Program, National Institutes of Health.
Authors' addresses: Gregory D. Gromowski, Cai-Yen Firestone, José Bustos-Arriaga, and Stephen S. Whitehead, Laboratory of Infectious Diseases, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD, E-mails: gromowskig@niaid.nih.gov, cfirestone@niaid.nih.gov, bustosarriagaj2@mail.nih.gov, and swhitehead@niaid.nih.gov.
References
- 1.Rosen L. The natural history of Japanese encephalitis virus. Annu Rev Microbiol. 1986;40:395–414. doi: 10.1146/annurev.mi.40.100186.002143. [DOI] [PubMed] [Google Scholar]
- 2.Buescher EL, Scherer WF. Ecologic studies of Japanese encephalitis virus in Japan. IX. Epidemiologic correlations and conclusions. Am J Trop Med Hyg. 1959;8:719–722. doi: 10.4269/ajtmh.1959.8.719. [DOI] [PubMed] [Google Scholar]
- 3.van den Hurk AF, Ritchie SA, Mackenzie JS. Ecology and geographical expansion of Japanese encephalitis virus. Annu Rev Entomol. 2009;54:17–35. doi: 10.1146/annurev.ento.54.110807.090510. [DOI] [PubMed] [Google Scholar]
- 4.Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, Marfin AA, Solomon T, Tsai TF, Tsu VD, Ginsburg AS. Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ. 2011;89:766–774. doi: 10.2471/BLT.10.085233. 774A–774E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chambers TJ, Hahn CS, Galler R, Rice CM. Flavivirus genome organization, expression, and replication. Annu Rev Microbiol. 1990;44:649–688. doi: 10.1146/annurev.mi.44.100190.003245. [DOI] [PubMed] [Google Scholar]
- 6.Lindenbach BD, Rice CM. Molecular biology of flaviviruses. Adv Virus Res. 2003;59:23–61. doi: 10.1016/s0065-3527(03)59002-9. [DOI] [PubMed] [Google Scholar]
- 7.Pierson TC, Fremont DH, Kuhn RJ, Diamond MS. Structural insights into the mechanisms of antibody-mediated neutralization of flavivirus infection: implications for vaccine development. Cell Host Microbe. 2008;4:229–238. doi: 10.1016/j.chom.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markoff L. Points to consider in the development of a surrogate for efficacy of novel Japanese encephalitis virus vaccines. Vaccine. 2000;18((Suppl 2)):26–32. doi: 10.1016/s0264-410x(00)00038-4. [DOI] [PubMed] [Google Scholar]
- 9.Larena M, Regner M, Lee E, Lobigs M. Pivotal role of antibody and subsidiary contribution of CD8+ T cells to recovery from infection in a murine model of Japanese encephalitis. J Virol. 2011;85:5446–5455. doi: 10.1128/JVI.02611-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diamond MS. Mechanisms of evasion of the type I interferon antiviral response by flaviviruses. J Interferon Cytokine Res. 2009;29:521–530. doi: 10.1089/jir.2009.0069. [DOI] [PubMed] [Google Scholar]
- 11.Turtle L, Griffiths MJ, Solomon T. Encephalitis caused by flaviviruses. QJM. 2012;105:219–223. doi: 10.1093/qjmed/hcs013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suthar MS, Diamond MS, Gale M., Jr West Nile virus infection and immunity. Nat Rev Microbiol. 2013;11:115–128. doi: 10.1038/nrmicro2950. [DOI] [PubMed] [Google Scholar]
- 13.Diamond MS. Evasion of innate and adaptive immunity by flaviviruses. Immunol Cell Biol. 2003;81:196–206. doi: 10.1046/j.1440-1711.2003.01157.x. [DOI] [PubMed] [Google Scholar]
- 14.Beasley DW, Lewthwaite P, Solomon T. Current use and development of vaccines for Japanese encephalitis. Expert Opin Biol Ther. 2008;8:95–106. doi: 10.1517/14712598.8.1.95. [DOI] [PubMed] [Google Scholar]
- 15.Halstead SB, Thomas SJ. New Japanese encephalitis vaccines: alternatives to production in mouse brain. Expert Rev Vaccines. 2011;10:355–364. doi: 10.1586/erv.11.7. [DOI] [PubMed] [Google Scholar]
- 16.Appaiahgari MB, Vrati S. Clinical development of IMOJEV (R)–a recombinant Japanese encephalitis chimeric vaccine (JE-CV) Expert Opin Biol Ther. 2012;12:1251–1263. doi: 10.1517/14712598.2012.704908. [DOI] [PubMed] [Google Scholar]
- 17.Kumar R, Tripathi P, Rizvi A. Effectiveness of one dose of SA 14-14-2 vaccine against Japanese encephalitis. N Engl J Med. 2009;360:1465–1466. doi: 10.1056/NEJMc0808664. [DOI] [PubMed] [Google Scholar]
- 18.WHO . WHO Expert Committee on Biological Standardization. Sixty-third report. Annex 7, Recommendations to assure the quality, safety and efficacy of Japanese encephalitis vaccines (live, attenuated) for human use. Geneva: WHO Press; 2014. [Google Scholar]
- 19.Feroldi E, Pancharoen C, Kosalaraksa P, Chokephaibulkit K, Boaz M, Meric C, Hutagalung Y, Bouckenooghe A. Primary immunization of infants and toddlers in Thailand with Japanese encephalitis chimeric virus vaccine in comparison with SA14-14-2: a randomized study of immunogenicity and safety. Pediatr Infect Dis J. 2014;33:643–649. doi: 10.1097/INF.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 20.Sohn YM, Tandan JB, Yoksan S, Ji M, Ohrr H. A 5-year follow-up of antibody response in children vaccinated with single dose of live attenuated SA14-14-2 Japanese encephalitis vaccine: immunogenicity and anamnestic responses. Vaccine. 2008;26:1638–1643. doi: 10.1016/j.vaccine.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Tsai TF, Yu YX, Jia LL, Putvatana R, Zhang R, Wang S, Halstead SB. Immunogenicity of live attenuated SA14-14-2 Japanese encephalitis vaccine–a comparison of 1- and 3-month immunization schedules. J Infect Dis. 1998;177:221–223. doi: 10.1086/517358. [DOI] [PubMed] [Google Scholar]
- 22.Tsai TF. New initiatives for the control of Japanese encephalitis by vaccination: minutes of a WHO/CVI meeting, Bangkok, Thailand, 13–15 October 1998. Vaccine. 2000;18((Suppl 2)):1–25. doi: 10.1016/s0264-410x(00)00037-2. [DOI] [PubMed] [Google Scholar]
- 23.Bista MB, Banerjee MK, Shin SH, Tandan JB, Kim MH, Sohn YM, Ohrr HC, Tang JL, Halstead SB. Efficacy of single-dose SA 14-14-2 vaccine against Japanese encephalitis: a case control study. Lancet. 2001;358:791–795. doi: 10.1016/s0140-6736(01)05967-0. [DOI] [PubMed] [Google Scholar]
- 24.Chotpitayasunondh T, Sohn YM, Yoksan S, Min J, Ohrr H. Immunizing children aged 9 to 15 months with live attenuated SA14-14-2 Japanese encephalitis vaccine in Thailand. J Med Assoc Thai. 2011;94((Suppl 3)):S195–S203. [PubMed] [Google Scholar]
- 25.Tandan JB, Ohrr H, Sohn YM, Yoksan S, Ji M, Nam CM, Halstead SB. Single dose of SA 14-14-2 vaccine provides long-term protection against Japanese encephalitis: a case-control study in Nepalese children 5 years after immunization. Vaccine. 2007;25:5041–5045. doi: 10.1016/j.vaccine.2007.04.052. [DOI] [PubMed] [Google Scholar]
- 26.Ohrr H, Tandan JB, Sohn YM, Shin SH, Pradhan DP, Halstead SB. Effect of single dose of SA 14-14-2 vaccine 1 year after immunization in Nepalese children with Japanese encephalitis: a case-control study. Lancet. 2005;366:1375–1378. doi: 10.1016/S0140-6736(05)67567-8. [DOI] [PubMed] [Google Scholar]
- 27.Yu Y. Phenotypic and genotypic characteristics of Japanese encephalitis attenuated live vaccine virus SA14-14-2 and their stabilities. Vaccine. 2010;28:3635–3641. doi: 10.1016/j.vaccine.2010.02.105. [DOI] [PubMed] [Google Scholar]
- 28.Aihara S, Rao CM, Yu YX, Lee T, Watanabe K, Komiya T, Sumiyoshi H, Hashimoto H, Nomoto A. Identification of mutations that occurred on the genome of Japanese encephalitis virus during the attenuation process. Virus Genes. 1991;5:95–109. doi: 10.1007/BF00571925. [DOI] [PubMed] [Google Scholar]
- 29.Ni H, Chang GJ, Xie H, Trent DW, Barrett AD. Molecular basis of attenuation of neurovirulence of wild-type Japanese encephalitis virus strain SA14. J Gen Virol. 1995;76:409–413. doi: 10.1099/0022-1317-76-2-409. [DOI] [PubMed] [Google Scholar]
- 30.Nitayaphan S, Grant JA, Chang GJ, Trent DW. Nucleotide sequence of the virulent SA-14 strain of Japanese encephalitis virus and its attenuated vaccine derivative, SA-14-14-2. Virology. 1990;177:541–552. doi: 10.1016/0042-6822(90)90519-w. [DOI] [PubMed] [Google Scholar]
- 31.Arroyo J, Guirakhoo F, Fenner S, Zhang ZX, Monath TP, Chambers TJ. Molecular basis for attenuation of neurovirulence of a yellow fever virus/Japanese encephalitis virus chimera vaccine (ChimeriVax-JE) J Virol. 2001;75:934–942. doi: 10.1128/JVI.75.2.934-942.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao Z, Date T, Li Y, Kato T, Miyamoto M, Yasui K, Wakita T. Characterization of the E-138 (Glu/Lys) mutation in Japanese encephalitis virus by using a stable, full-length, infectious cDNA clone. J Gen Virol. 2005;86:2209–2220. doi: 10.1099/vir.0.80638-0. [DOI] [PubMed] [Google Scholar]
- 33.Chen LK, Lin YL, Liao CL, Lin CG, Huang YL, Yeh CT, Lai SC, Jan JT, Chin C. Generation and characterization of organ-tropism mutants of Japanese encephalitis virus in vivo and in vitro. Virology. 1996;223:79–88. doi: 10.1006/viro.1996.0457. [DOI] [PubMed] [Google Scholar]
- 34.Sumiyoshi H, Tignor GH, Shope RE. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J Infect Dis. 1995;171:1144–1151. doi: 10.1093/infdis/171.5.1144. [DOI] [PubMed] [Google Scholar]
- 35.Yang D, Li XF, Ye Q, Wang HJ, Deng YQ, Zhu SY, Zhang Y, Li SH, Qin CF. Characterization of live-attenuated Japanese encephalitis vaccine virus SA14-14-2. Vaccine. 2014;32:2675–2681. doi: 10.1016/j.vaccine.2014.03.074. [DOI] [PubMed] [Google Scholar]
- 36.Chambers TJ, Droll DA, Jiang X, Wold WS, Nickells JA. JE Nakayama/JE SA14-14-2 virus structural region intertypic viruses: biological properties in the mouse model of neuroinvasive disease. Virology. 2007;366:51–61. doi: 10.1016/j.virol.2007.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ye Q, Li XF, Zhao H, Li SH, Deng YQ, Cao RY, Song KY, Wang HJ, Hua RH, Yu YX, Zhou X, Qin ED, Qin CF. A single nucleotide mutation in NS2A of Japanese encephalitis-live vaccine virus (SA14-14-2) ablates NS1' formation and contributes to attenuation. J Gen Virol. 2012;93:1959–1964. doi: 10.1099/vir.0.043844-0. [DOI] [PubMed] [Google Scholar]
- 38.Sooryanarain H, Sapkal GN, Gore MM. Pathogenic and vaccine strains of Japanese encephalitis virus elicit different levels of human macrophage effector functions. Arch Virol. 2012;157:1905–1918. doi: 10.1007/s00705-012-1386-8. [DOI] [PubMed] [Google Scholar]
- 39.Laurent-Rolle M, Boer EF, Lubick KJ, Wolfinbarger JB, Carmody AB, Rockx B, Liu W, Ashour J, Shupert WL, Holbrook MR, Barrett AD, Mason PW, Bloom ME, Garcia-Sastre A, Khromykh AA, Best SM. The NS5 protein of the virulent West Nile virus NY99 strain is a potent antagonist of type I interferon-mediated JAK-STAT signaling. J Virol. 2010;84:3503–3515. doi: 10.1128/JVI.01161-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Petricciani JC, Hennessen W, editors. Cells products safety. Background papers from the WHO Study Group on Biologicals. Geneva, 18–19 Nov. 1986. Dev Biol Stand. 1987;68:1–81. [PubMed] [Google Scholar]
- 41.Barrett PN, Mundt W, Kistner O, Howard MK. Vero cell platform in vaccine production: moving towards cell culture-based viral vaccines. Expert Rev Vaccines. 2009;8:607–618. doi: 10.1586/erv.09.19. [DOI] [PubMed] [Google Scholar]
- 42.van Wezel AL, van Steenis G, Hannik CA, Cohen H. New approach to the production of concentrated and purified inactivated polio and rabies tissue culture vaccines. Dev Biol Stand. 1978;41:159–168. [PubMed] [Google Scholar]
- 43.Rhim JS, Schell K, Creasy B, Case W. Biological characteristics and viral susceptibility of an African green monkey kidney cell line (Vero) Proc Soc Exp Biol Med. 1969;132:670–678. doi: 10.3181/00379727-132-34285. [DOI] [PubMed] [Google Scholar]
- 44.Desmyter J, Melnick JL, Rawls WE. Defectiveness of interferon production and of rubella virus interference in a line of African green monkey kidney cells (Vero) J Virol. 1968;2:955–961. doi: 10.1128/jvi.2.10.955-961.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eckels KH, Yu YX, Dubois DR, Marchette NJ, Trent DW, Johnson AJ. Japanese encephalitis virus live-attenuated vaccine, Chinese strain SA14-14-2; adaptation to primary canine kidney cell cultures and preparation of a vaccine for human use. Vaccine. 1988;6:513–518. doi: 10.1016/0264-410x(88)90103-x. [DOI] [PubMed] [Google Scholar]
- 46.Solomon T, Ni H, Beasley DW, Ekkelenkamp M, Cardosa MJ, Barrett AD. Origin and evolution of Japanese encephalitis virus in southeast Asia. J Virol. 2003;77:3091–3098. doi: 10.1128/JVI.77.5.3091-3098.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gromowski GD, Firestone CY, Hanson CT, Whitehead SS. Japanese encephalitis virus vaccine candidates generated by chimerization with dengue virus type 4. Vaccine. 2014;32:3010–3018. doi: 10.1016/j.vaccine.2014.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Song BH, Yun GN, Kim JK, Yun SI, Lee YM. Biological and genetic properties of SA(1)(4)-14-2, a live-attenuated Japanese encephalitis vaccine that is currently available for humans. J Microbiol. 2012;50:698–706. doi: 10.1007/s12275-012-2336-6. [DOI] [PubMed] [Google Scholar]
- 49.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 50.Pierson TC, Sanchez MD, Puffer BA, Ahmed AA, Geiss BJ, Valentine LE, Altamura LA, Diamond MS, Doms RW. A rapid and quantitative assay for measuring antibody-mediated neutralization of West Nile virus infection. Virology. 2006;346:53–65. doi: 10.1016/j.virol.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 51.Pierson TC, Xu Q, Nelson S, Oliphant T, Nybakken GE, Fremont DH, Diamond MS. The stoichiometry of antibody-mediated neutralization and enhancement of West Nile virus infection. Cell Host Microbe. 2007;1:135–145. doi: 10.1016/j.chom.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carver DH, Seto DS, Migeon BR. Interferon production and action in mouse, hamster and somatic hybrid mouse-hamster cells. Science. 1968;160:558–559. doi: 10.1126/science.160.3827.558. [DOI] [PubMed] [Google Scholar]
- 53.Gulati BR, Singha H, Singh BK, Virmani N, Kumar S, Singh RK. Isolation and genetic characterization of Japanese encephalitis virus from equines in India. J Vet Sci. 2012;13:111–118. doi: 10.4142/jvs.2012.13.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Samuel MA, Diamond MS. Alpha/beta interferon protects against lethal West Nile virus infection by restricting cellular tropism and enhancing neuronal survival. J Virol. 2005;79:13350–13361. doi: 10.1128/JVI.79.21.13350-13361.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Keller BC, Fredericksen BL, Samuel MA, Mock RE, Mason PW, Diamond MS, Gale M., Jr Resistance to alpha/beta interferon is a determinant of West Nile virus replication fitness and virulence. J Virol. 2006;80:9424–9434. doi: 10.1128/JVI.00768-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shresta S, Kyle JL, Snider HM, Basavapatna M, Beatty PR, Harris E. Interferon-dependent immunity is essential for resistance to primary dengue virus infection in mice, whereas T- and B-cell-dependent immunity are less critical. J Virol. 2004;78:2701–2710. doi: 10.1128/JVI.78.6.2701-2710.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lobigs M, Mullbacher A, Wang Y, Pavy M, Lee E. Role of type I and type II interferon responses in recovery from infection with an encephalitic flavivirus. J Gen Virol. 2003;84:567–572. doi: 10.1099/vir.0.18654-0. [DOI] [PubMed] [Google Scholar]
- 58.Calvert AE, Dixon KL, Delorey MJ, Blair CD, Roehrig JT. Development of a small animal peripheral challenge model of Japanese encephalitis virus using interferon deficient AG129 mice and the SA14-14-2 vaccine virus strain. Vaccine. 2014;32:258–264. doi: 10.1016/j.vaccine.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tu YC, Yu CY, Liang JJ, Lin E, Liao CL, Lin YL. Blocking double-stranded RNA-activated protein kinase PKR by Japanese encephalitis virus nonstructural protein 2A. J Virol. 2012;86:10347–10358. doi: 10.1128/JVI.00525-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liang JJ, Liao CL, Liao JT, Lee YL, Lin YL. A Japanese encephalitis virus vaccine candidate strain is attenuated by decreasing its interferon antagonistic ability. Vaccine. 2009;27:2746–2754. doi: 10.1016/j.vaccine.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 61.Lin CW, Cheng CW, Yang TC, Li SW, Cheng MH, Wan L, Lin YJ, Lai CH, Lin WY, Kao MC. Interferon antagonist function of Japanese encephalitis virus NS4A and its interaction with DEAD-box RNA helicase DDX42. Virus Res. 2008;137:49–55. doi: 10.1016/j.virusres.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 62.Liu WJ, Wang XJ, Mokhonov VV, Shi PY, Randall R, Khromykh AA. Inhibition of interferon signaling by the New York 99 strain and Kunjin subtype of West Nile virus involves blockage of STAT1 and STAT2 activation by nonstructural proteins. J Virol. 2005;79:1934–1942. doi: 10.1128/JVI.79.3.1934-1942.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ni H, Burns NJ, Chang GJ, Zhang MJ, Wills MR, Trent DW, Sanders PG, Barrett AD. Comparison of nucleotide and deduced amino acid sequence of the 5′ non-coding region and structural protein genes of the wild-type Japanese encephalitis virus strain SA14 and its attenuated vaccine derivatives. J Gen Virol. 1994;75:1505–1510. doi: 10.1099/0022-1317-75-6-1505. [DOI] [PubMed] [Google Scholar]
- 64.Hong SP, Yoo WD, Putnak R, Eckels KH, Rho HM, Kim SO. Nucleotide sequence of envelope protein of Japanese encephalitis virus SA14-14-2 adapted to vero cells. DNA Seq. 2001;12:437–442. doi: 10.3109/10425170109084471. [DOI] [PubMed] [Google Scholar]
- 65.Duggan ST, Plosker GL. Japanese encephalitis vaccine (inactivated, adsorbed) [IXIARO] Drugs. 2009;69:115–122. doi: 10.2165/00003495-200969010-00008. [DOI] [PubMed] [Google Scholar]
- 66.Wills MR, Singh BK, Debnath NC, Barrett AD. Immunogenicity of wild-type and vaccine strains of Japanese encephalitis virus and the effect of haplotype restriction on murine immune responses. Vaccine. 1993;11:761–766. doi: 10.1016/0264-410x(93)90262-v. [DOI] [PubMed] [Google Scholar]