Abstract
In the present study, we have evaluated the in vitro antibacterial activity of essential oils from Origanum vulgare, Thymus vulgaris, Lavandula angustifolia, Mentha piperita, and Melaleuca alternifolia against 32 erythromycin-resistant [Mininum Inhibitory Concentration (MIC) ≥1 μg/mL; inducible, constitutive, and efflux-mediated resistance phenotype; erm(TR), erm(B), and mef(A) genes] and cell-invasive Group A streptococci (GAS) isolated from children with pharyngotonsillitis in Italy. Over the past decades erythromycin resistance in GAS has emerged in several countries; strains combining erythromycin resistance and cell invasiveness may escape β-lactams because of intracellular location and macrolides because of resistance, resulting in difficulty of eradication and recurrent pharyngitis. Thyme and origanum essential oils demonstrated the highest antimicrobial activity with MICs ranging from 256 to 512 μg/mL. The phenolic monoterpene carvacrol [2-Methyl-5-(1-methylethyl) phenol] is a major component of the essential oils of Origanum and Thymus plants. MICs of carvacrol ranged from 64 to 256 μg/mL. In the live/dead assay several dead cells were detected as early as 1 h after incubation with carvacrol at the MIC. In single-step resistance selection studies no resistant mutants were obtained. A synergistic action of carvacrol and erythromycin was detected by the checkerboard assay and calculation of the Fractional Inhibitory Concentration (FIC) Index. A 2- to 2048-fold reduction of the erythromycin MIC was documented in checkerboard assays. Synergy (FIC Index ≤0.5) was found in 21/32 strains and was highly significant (p < 0.01) in strains where resistance is expressed only in presence of erythromycin. Synergy was confirmed in 17/23 strains using 24-h time-kill curves in presence of carvacrol and erythromycin. Our findings demonstrated that carvacrol acts either alone or in combination with erythromycin against erythromycin-resistant GAS and could potentially serve as a novel therapeutic tool.
Keywords: group A streptococci, essential oils, thyme, origanum, carvacrol, erythromycin, synergy
INTRODUCTION
The increase in antibiotic-resistant bacteria has revived the interest in plant products as alternative/adjunct antimicrobial agents to control pathogenic micro-organisms (Cowan, 1999; Hemaiswarya et al., 2008; Hyldgaard et al., 2012). A major group of plant antimicrobial compounds is represented by essential oils, which are complex mixtures of volatile secondary metabolites. They are used in the food industry because of their preservative potency against food-borne pathogens—thanks to their antimicrobial, antibacterial, and antifungal properties. Besides antimicrobial activity, essential oils and their components can act in synergy with some antibiotics, enhancing their antimicrobial activity (Langeveld et al., 2014). The phenolic monoterpene carvacrol [2-Methyl-5-(1-methylethyl) phenol, isomeric with thymol] is a major component of the essential oils of plants of the Labiatae family, including Origanum and Thymus, which are commonly used as seasoning and in traditional medicine since ancient times (Nostro and Papalia, 2012). Carvacrol has been classified as GRAS (Generally Recognized As Safe) and approved for food use (EAFUS, 2006; Hyldgaard et al., 2012; European Parliament and Council, 1996). Beside anti-inflammatory, antioxidant, antitumor, analgesic, anti-hepatotoxic, and insecticidal properties, several studies have demonstrated that carvacrol has antimicrobial properties (Hyldgaard et al., 2012). Findings regarding the latter properties are the subject of a recent review (Hyldgaard et al., 2012). The antibacterial action of carvacrol, which is stronger against Gram-positive than Gram-negative bacteria, principally relies on bacterial membrane damage; it results in dissolution of the proton motive force and subsequent reduction in ATP synthesis that lead to reduction in other energy-dependent cell processes, including synthesis of enzymes and toxins (Nostro and Papalia, 2012). In particular, carvacrol has extensively been tested as an antimicrobial agent in food to control Gram-positive and Gram-negative pathogens, including Bacillus cereus, Enterococcus faecalis, Listeria monocytogenes, Staphylococcus aureus, Escherichia coli O157:H7, Pseudomonas fluorescens, Salmonella typhimurium, Vibrio cholerae, and V. vulnificus (Hyldgaard et al., 2012; Langeveld et al., 2014). The ability of carvacrol to exert synergistic effects in combination with a number of antibiotics, including macrolides, has been recently reported (Langeveld et al., 2014).
Erythromycin and related molecules are the second-line drugs used to treat pharyngotonsillitis and other infections caused by Streptococcus pyogenes [Group A streptococci (GAS)], an important human pathogen. GAS cause a variety of clinical manifestations ranging from non-invasive disease, such as pharyngitis and impetigo, to more severe, invasive infections including necrotizing fasciitis, sepsis, toxic shock-like syndrome, and post-streptococcal sequelae such as acute rheumatic fever, rheumatic heart disease, and glomerulonephritis (Cunningham, 2008). In particular, GAS are the most common bacterial cause of pharyngotonsillitis in children. Over the past decades erythromycin resistance in GAS has emerged in several countries, including Italy (Kaplan and Cornaglia, 2005; Gracia et al., 2009). At present, it has fallen dramatically in Europe and America, while rates >90% have recently been reported in China (Chang et al., 2010; Liang et al., 2012). Several genes are responsible for erythromycin resistance in GAS (Giovanetti et al., 2002). An efflux mechanism encoded by different macrolide efflux (mef) genes causes resistance to 14- and 15-membered macrolides (M phenotype); in contrast, ribosomal modification by erythromycin resistance methylase (erm) genes causes co-resistance to macrolide-lincosamide-streptogramin B (MLS) antibiotics. MLS resistance is constitutive when it is encoded by the erm(B) gene (cMLS phenotype); it is inducible, i.e., expressed only in presence of the antibiotic, when it is encoded by the erm(TR) or the variant erm(B) gene (iMLS phenotype). An association between erythromycin resistance and ability to invade and survive within human respiratory cells has been documented in Italy among GAS isolated from children with pharyngotonsillitis (Facinelli et al., 2001): these strains may escape β-lactams because of intracellular location and macrolides—which unlike β-lactams enter eukaryotic cells and are active in intracellular compartments—because of resistance, resulting in difficulty of eradication and recurrent pharyngitis.
In this study, we evaluated the antibacterial activity of different essential oils and of carvacrol, alone and in combination with erythromycin, against erythromycin-resistant GAS isolated from children with pharyngotonsillitis in Italy.
MATERIALS AND METHODS
GAS STRAINS AND GROWTH MEDIA
Test strains were 32 erythromycin-resistant [Mininum Inhibitory Concentration (MIC) ≥1 μg/mL] GAS strains isolated from children with pharyngotonsillitis in a nationwide survey in Italy (Varaldo et al., 1999; Table 1). Erythromycin-resistant GAS isolates were genotypically and phenotypically heterogeneous: erm(TR)/iMLS (n = 6); erm(B)/iMLS (n = 6); erm(B)/cMLS (n = 8); mef(A)/M (n = 12). The strains had previously been investigated for the association between erythromycin resistance and ability to enter and persist inside human respiratory A549 cells (Facinelli et al., 2001; Spinaci et al., 2004, 2006); they had also been typed at the molecular level (Spinaci et al., 2004, 2006). Each of the 32 strains included in the study represents a clone identified among Italian erythromycin-resistant GAS. Blood agar base (BAB) supplemented with 5% sheep blood, Müller-Hinton agar (MHA) supplemented with 5% sheep blood, Müller-Hinton cation-adjusted broth (CAMHB) supplemented with 3% laked sheep blood, and brain heart infusion broth (BHIB; Oxoid, Basingstoke, UK) were used throughout the study. Isolates were maintained in glycerol at -70∘C and sub-cultured twice on BAB before testing.
Table 1.
Characteristics of erythromycin-resistant GAS, each strain representing an erythromycin-resistant Italian GAS clone.
| Genotype/phenotype of erythromycin resistance (no. of strains) | Mininum Inhibitory Concentration (MIC; μg/mL) |
Fractional Inhibitory Concentration (FIC) Index |
||||||
|---|---|---|---|---|---|---|---|---|
| ERYa | CARb | Best combinationc |
FIC |
≤0.5 | >0.5 | |||
| ERYa | CARb | ERYa | CARb | |||||
| erm(TR)/iMLS (n = 6) | ||||||||
| SP1900d | 256 | 128 | 4 | 32 | 0.0156 | 0.2500 | 0.2656 | |
| SP1161 | 8 | 64 | 1 | 8 | 0.1250 | 0.1250 | 0.2500 | |
| SP55 | 8 | 128 | 0.5 | 32 | 0.0625 | 0.2500 | 0.3125 | |
| SP1160 | 16 | 128 | 4 | 8 | 0.2500 | 0.0625 | 0.3125 | |
| SP4502 | 64 | 128 | 16 | 8 | 0.2500 | 0.0625 | 0.3125 | |
| 11613 | 8 | 64 | 2 | 16 | 0.2500 | 0.2500 | 0.5000 | |
| erm(B)/iMLS (n = 6) | ||||||||
| SP1188 | 512 | 128 | 0.5 | 32 | 0.0009 | 0.2500 | 0.2509 | |
| 11414 | 512 | 128 | 0.5 | 32 | 0.0009 | 0.2500 | 0.2509 | |
| 11107 | 512 | 128 | 1 | 32 | 0.0019 | 0.2500 | 0.2519 | |
| SP1181 | 512 | 128 | 2 | 32 | 0.0039 | 0.2500 | 0.2539 | |
| SP114 | 512 | 128 | 0.5 | 32 | 0.0009 | 0.2500 | 0.2509 | |
| SP1189 | 512 | 64 | 0.25 | 32 | 0.0005 | 0.5000 | 0.5005 | |
| erm(B)/cMLS (n = 8) | ||||||||
| SP2130 | 512 | 128 | 2 | 32 | 0.0039 | 0.2500 | 0.2539 | |
| 10039 | 512 | 128 | 2 | 32 | 0.0039 | 0.2500 | 0.2539 | |
| SP9707 | 512 | 64 | 0.25 | 32 | 0.0005 | 0.5000 | 0.5005 | |
| SP9103 | 512 | 64 | 0.25 | 32 | 0.0005 | 0.5000 | 0.5005 | |
| 37014 | 512 | 64 | 0.25 | 32 | 0.0005 | 0.5000 | 0.5005 | |
| SP1791 | 512 | 64 | 0.25 | 32 | 0.0005 | 0.5000 | 0.5005 | |
| SP1003 | 512 | 128 | 0.25 | 64 | 0.0005 | 0.5000 | 0.5005 | |
| SP1070 | 512 | 128 | 0.25 | 64 | 0.0005 | 0.5000 | 0.5005 | |
| mef(A)/M (n = 12) | ||||||||
| 10911 | 8 | 64 | 2 | 16 | 0.2500 | 0.2500 | 0.5000 | |
| SP9721 | 16 | 64 | 0.5 | 16 | 0.0313 | 0.2500 | 0.2813 | |
| 9407 | 32 | 64 | 8 | 16 | 0.2500 | 0.2500 | 0.5000 | |
| SP1180 | 16 | 128 | 4 | 32 | 0.2500 | 0.2500 | 0.5000 | |
| 10239 | 16 | 128 | 4 | 32 | 0.2500 | 0.2500 | 0.5000 | |
| SP118 | 16 | 256 | 0.5 | 64 | 0.0313 | 0.2500 | 0.2813 | |
| 10244 | 16 | 128 | 4 | 32 | 0.2500 | 0.2500 | 0.5000 | |
| 10313 | 16 | 128 | 4 | 32 | 0.2500 | 0.2500 | 0.5000 | |
| SP1013 | 1 | 128 | 0.25 | 64 | 0.2500 | 0.5000 | 0.7500 | |
| 13962 | 16 | 128 | 0.5 | 64 | 0.0313 | 0.5000 | 0.5313 | |
| 128–192 | 16 | 128 | 0.5 | 64 | 0.0313 | 0.5000 | 0.5313 | |
| SP1951 | 16 | 128 | 0.03 | 64 | 0.0019 | 0.5000 | 0.5019 | |
aErythromycin; bCarvacrol; cCombination of carvacrol and erythromycin giving thelowest FIC Index value; d(Palmieri et al., 2006).
ANTIMICROBIALS AND SUSCEPTIBILITY TESTS
Five different essential oils [origanum (W282812), thyme (W306401), lavender (W262218), tea tree (W390208), and peppermint (W284815)], carvacrol (W224502, >98% purity), and erythromycin (E-5389) were all purchased from Sigma–Aldrich (St. Louis, MO, USA). Essential oils (10 mg/mL stock solutions) were stored in DMSO at -20∘C; carvacrol and erythromycin (10 mg/mL stock solutions) were stored in absolute ethanol at -20∘C. MIC is defined as the lowest concentration of an antimicrobial that will inhibit the visible growth of a microorganism after overnight incubation. MICs of essential oils and carvacrol were determined by agar dilution (in blood-supplemented MHA) and microdilution (in blood-supplemented CAMHB) methods, respectively, as recommended by Clinical and Laboratory Standards Institute [CLSI] (2014) guidelines. All experiments were performed in triplicate.
LIVE/DEAD ASSAY
Group A streptococci survival in presence of carvacrol was studied by the live/dead assay as described previously (Zandri et al., 2012) using SYBR Green I (Invitrogen, Eugene, OR, USA) and propidium iodide (Sigma–Aldrich), two nucleic acid dyes differing in their ability to penetrate bacterial cells: bacteria with intact cell membranes stain fluorescent green, whereas those with damaged membranes stain fluorescent red. Briefly, overnight grown streptococci were suspended in 1 mL carvacrol-supplemented BHIB (∼1 × 108 CFU/mL) and incubated for 1, 3, or 24 h at 37∘C in 5% CO2. After staining with 1 × SYBR Green I and 40 μg/mL propidium iodide, samples were incubated at room temperature for 25 min in the dark, harvested on GTBP filters (Ø = 0.2 μm, Millipore, Billerica, MA, USA), and examined under an epifluorescence microscope (Axioskop 2, Zeiss, Milano, Italy).
CHECKERBOARD TEST
Synergy was tested by the checkerboard method, a two-dimensional array of serial concentrations of test compounds, that has been used most frequently to assess antimicrobial combinations in vitro (Pillai et al., 2005). The tested dilutions were based on the MIC of the two substances. The checkerboard test was used as the basis to calculate a Fractional Inhibitory Concentration (FIC) Index (Pillai et al., 2005) according to the formulas: FICA = MICA+B/MICA, FICB = MICB+A/MICB, FIC Index = FICA+FICB. The MICA+B value is the MIC of compound A in the presence of compound B, and vice versa for MICB+A. FIC Index values were interpreted accordingly to Odds (Odds, 2003): synergy (FIC Index ≤0.5), antagonism (FIC Index >4.0), and no interaction (FIC Index >0.5–4.0).
The test was performed in blood-supplemented CAMHB using 96-well microtiter plates containing erythromycin and carvacrol in twofold serial concentrations. Bacterial suspensions were prepared to yield final inocula of ∼5 × 105 CFU/mL. Plates were read after overnight incubation at 37∘C in 5% CO2. Each test was performed in triplicate. Test results were also represented by isobolograms constructed by plotting synergistic concentrations of carvacrol and erythromycin (Mulyaningsih et al., 2010).
TIME-KILL CURVES
Time-kill experiments were performed in BHIB in microtiter plates containing different combinations of carvacrol and erythromycin at different sub-MICs. Briefly, streptococci (∼5 × 105 CFU/mL) were placed on microtiter plates, incubated for 24 h at 37∘C and read at OD690 at 1-h intervals using Multiscan Ascent (Thermo Scientific, Waltham, MA, USA). Controls also included growth in presence of carvacrol and erythromycin alone. All experiments were performed in triplicate.
SEARCH FOR CARVACROL MUTANTS
In these experiments, bacterial cells were grown overnight in BHI agar plates, scraped off, washed once with BHIB, and resuspended to a final concentration of 1 × 1010 to 1 × 1011 CFU/mL. An aliquot (50 μL) of bacterial suspension was spread on carvacrol-containing BAB plates at 1, 2, and 4 times the MIC. The plates were incubated at 37∘C in CO2 for 72 h. Experiments were repeated twice.
STATISTICAL ANALYSIS
Synergy data were analyzed using Fisher’s exact test. Fisher’s test was used to evaluate whether the association between phenotype iMLS and synergy in erm-carrying strains was significant. Significance was set at p-value < 0.01.
RESULTS
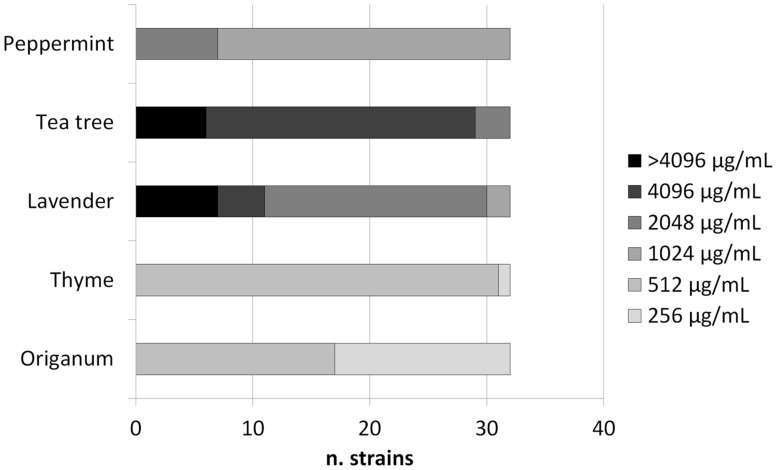
The MICs of origanum and thyme oils ranged from 256 to 512 μg/mL, while those of lavender, tea tree, and peppermint oils ranged from 1024 to >4096 μg/mL (Figure 1). The MICs of carvacrol were 64 μg/mL (n = 10 strains), 128 μg/mL (n = 21 strains), and 256 μg/mL (n = 1 strain; Table 1). In the live/dead assay several red cells were detected as early as 1 h after incubation with carvacrol at the MIC (data not shown).
FIGURE 1.
Mininum Inhibitory Concentrations (MICs) of five essential oils against GAS strains.
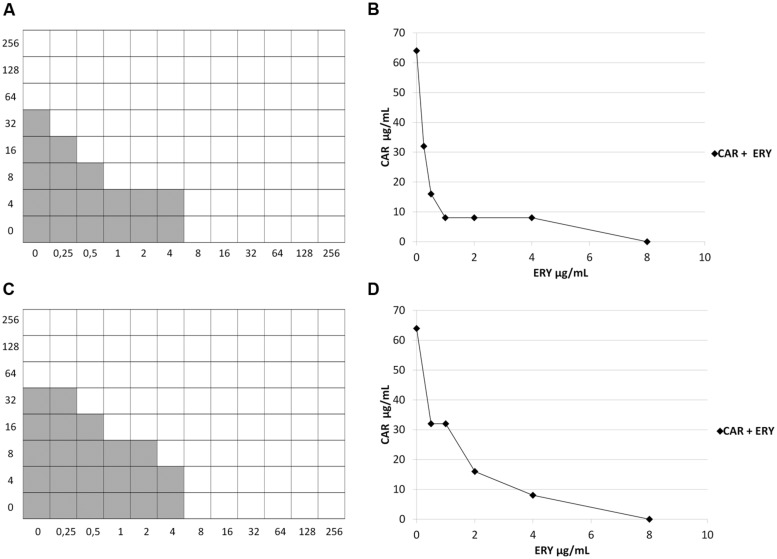
In the checkerboard assay, 77 different combinations of erythromycin and carvacrol were tested for each strain, ranging from several dilutions below the MIC to twice the MIC. A 2- to 2048-fold reduction of the erythromycin MIC was documented in synergy tests with the checkerboard assay (Table 1). FIC Index values were calculated by considering all combinations of carvacrol and erythromycin in which there was no visible growth. The “best combination” of carvacrol and erythromycin, i.e., the one giving the lowest FIC Index value, was indicated in Table 1. FIC Index values ranged from 0.25 to 0.75 (Table 1). Synergy (FIC Index ≤0.5) was detected in 21/32 strains (65.6%) and no interaction (FIC Index >0.5) in the remaining 11 strains (34.4%); antagonism was never observed. Strains where synergy was detected included all 6 erm(TR)/iMLS, 5/6 erm(B)/iMLS, 2/8 erm(B)/cMLS, and 8/12 mef(A)/M isolates. Among erm-carrying strains the association between the iMLS phenotype and synergy was very statistically significant (p = 0.0044). Strains where no interaction was detected included 8 strains with borderline FIC Index values (0.5005, 0.5019). Isobolographic analysis confirmed a synergistic effect against strains with FIC Index ≤0.5 (Figure 2) and no interaction against those with FIC Index >0.5, including those with borderline FIC Index values (data not shown).
FIGURE 2.
Checkerboard test and isobolograms. (A,B) strain SP1161 [Fractional Inhibitory Concentration (FIC) Index = 0.2500]; (C,D) strain 10911 (FIC Index = 0.5000). Shading, visible growth. CAR, carvacrol; ERY, erythromycin.
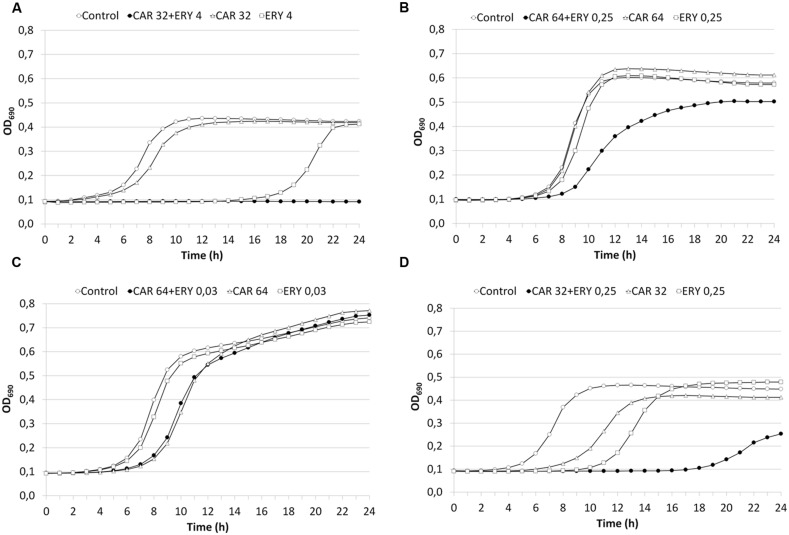
Synergy was also examined in 23 strains (18 strains with FIC Index ≤0.5 and 5 strains with FIC Index >0.5) using 24-h time-kill curves in presence of carvacrol and erythromycin. These findings confirmed the checkerboard data in 13/18 strains with FIC Index ≤0.5 (8/9 iMLS, 1/1 cMLS, and 4/8 M; Figure 3A), and in 4/5 strains with FIC Index >0.5 (1 cMLS, and 3 M; Figure 3B). The time-kill curves of the two strains with borderline FIC Index values (SP1951, FIC Index 0.5019; and SP1189, FIC Index 0.5005) indicated a lack of interaction (Figures 3C,D), even though synergy was seen in strain SP1189 in the first 18 h (Figure 3D). The discrepancy between checkerboard and time-kill data may depend on the media (with/without blood) and/or growth conditions (with/without CO2) (Odds, 2003).
FIGURE 3.
Time-kill curves. (A) strain SP1900 (FIC Index = 0.2656). (B) SP1013 (FIC Index = 0.7500). (C) SP1951 (FIC Index = 0.5019). (D) SP1189 (FIC Index = 0.5005). CAR, carvacrol; ERY, erythromycin.
No carvacrol-resistant mutants were obtained in single-step resistance selection experiments using strains SP2130, SP1188, SP1900, and 10239.
DISCUSSION
One of the alternative strategies to fight antibiotic-resistant bacteria is the use of natural antimicrobial substances such as plant essential oils and their components. Another possibility is to combine existing antibiotics with phytochemicals to enhance the efficacy of antibiotics. Among others, essential oils from Thymus vulgaris and Origanum vulgare contain carvacrol and thymol, whose antibacterial activity and synergistic effect in combination with antibiotics against food-related bacteria have been demonstrated (Hyldgaard et al., 2012; Langeveld et al., 2014).
In this study, the antimicrobial activity of five essential oils from different plants was tested against pharyngeal GAS isolates, all erythromycin-resistant and cell-invasive strains. The antimicrobial activity of thyme and origanum oils was high, with MICs much lower than those of lavender, mint, and tea tree oils. Since carvacrol is a major component of thyme and origanum essential oils, we decided to test the susceptibility of GAS strains to carvacrol. Our findings demonstrated a high activity of carvacrol against GAS, with MICs lower than those reported for other Gram-positive bacteria (Hyldgaard et al., 2012). A bactericidal action of carvacrol, probably through membrane damage, was suggested by the live/dead assay. Attempts to select carvacrol-resistant mutants were unsuccessful, suggesting that carvacrol is not prone to the development of resistance in GAS.
To our knowledge the synergistic activity of carvacrol and antibiotics against GAS has never been investigated, with the exception of a recent study of a single erm(B) collection strain (Palaniappan and Holley, 2010). Carvacrol in combination with erythromycin showed a synergistic action against tested GAS isolates; antagonism was never observed.
Interestingly, synergy was highly significant (p < 0.01) in iMLS strains, in which erythromycin resistance is only expressed in presence of an inducing sub-inhibitory concentration of the antibiotic. The molecular basis of the synergy deserves further investigation; an interference with the expression of the inducible methyl-transferases gene or inhibition of the enzyme itself might be involved in carvacrol’s synergistic action against iMLS GAS strains.
Overall, results of the current study suggest a potential use of origanum and thyme essential oils and of carvacrol against GAS. Moreover, the evidence of a synergism between erythromycin and carvacrol suggest a possible re-use of erythromycin against erythromycin-resistant GAS. In particular, carvacrol might be useful against those GAS strains which combine erythromycin resistance and the ability to invade and survive within human respiratory cells (Facinelli et al., 2001), resulting in difficulty of eradication and recurrent pharyngitis. With more knowledge of the mechanism underlying the synergism it may be possible to develop safe drug combinations.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported in part by the Italian Ministry of Education, University and Research (PRIN 2008CBSB9Y).
SUPPLEMENTARY MATERIAL
The Supplementary Material for this article can be found online at: http://www.frontiersin.org/journal/10.3389/fmicb.2015.00165/abstract
REFERENCES
- Chang H., Shen X., Fu Z., Liu L., Shen Y., Liu X., et al. (2010). Antibiotic resistance and molecular analysis of Streptococcus pyogenes isolated from healthy schoolchildren in China. Scand. J. Infect. Dis. 42 84–89 10.3109/00365540903321598 [DOI] [PubMed] [Google Scholar]
- Clinical and Laboratory Standards Institute [CLSI]. (2014). Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Fourth Informational Supplement M100-S24. Wayne, PA: CLSI. [Google Scholar]
- Cowan M. M. (1999). Plant products as antimicrobial agents. Clin. Microbiol. Rev. 12 564–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham M. W. (2008). Pathogenesis of group A streptococcal infections and their sequelae. Adv. Exp. Med. Biol. 609 29–42 10.1007/978-0-387-73960-1_3 [DOI] [PubMed] [Google Scholar]
- EAFUS. (2006). A Food Additive Database. Centre for Food Safety, and Applied Nutrition. Washington, DC: U. S. Food, and Drug Administration. [Google Scholar]
- European Parliament and Council. (1996). Regulation (EC) No 2232/96 the European Parliament, and of the Council on 28 October 1996, Commission Decision of 23 February 1999 adopting a register of flavouring substances used in or on foodstuffs. Off. J. Eur. Commun. L84:1999/217/EC 1–37. [Google Scholar]
- Facinelli B., Spinaci C., Magi G., Giovanetti E., Varaldo P. E. (2001). Association between erythromycin resistance and ability to enter human respiratory cells in group A streptococci. Lancet 358 30–33 10.1016/S0140-6736(00)05253-3 [DOI] [PubMed] [Google Scholar]
- Giovanetti E., Brenciani A., Burioni R., Varaldo P. E. (2002). A novel efflux system in inducibly erythromycin-resistant strains of Streptococcus pyogenes. Antimicrob. Agents Chemother. 46 3750–3755 10.1128/AAC.46.12.3750-3755.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gracia M., Díaz C., Coronel P., Gimeno M., García-Rodas R., Rodríguez-Cerrato V., et al. (2009). Antimicrobial susceptibility of Streptococcus pyogenes in Central, Eastern, and Baltic European Countries, 2005 to 2006: the cefditoren surveillance program. Diagn. Microbiol. Infect. Dis. 64 52–56 10.1016/j.diagmicrobio.2008.12.018 [DOI] [PubMed] [Google Scholar]
- Hemaiswarya S., Kruthiventi A. K., Doble M. (2008). Synergism between natural products and antibiotics against infectious diseases. Phytomedicine 15 639–652 10.1016/j.phymed.2008.06.008 [DOI] [PubMed] [Google Scholar]
- Hyldgaard M., Mygind T., Meyer R. L. (2012). Essential oils in food preservation: mode of action, synergies, and interactions with food matrix components. Front. Microbiol. 3:12 10.3389/fmicb.2012.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan E. L., Cornaglia G. (2005). Persistent macrolide resistance among group A streptococci: the lack of accomplishment after 4 decades. Clin. Infect. Dis. 41 609–611 10.1086/432480 [DOI] [PubMed] [Google Scholar]
- Langeveld W. T., Veldhuizen E. J. A., Burt S. A. (2014). Synergy between essential oil components and antibiotics: a review. Crit. Rev. Microbiol. 40 76–94 10.3109/1040841X.2013.763219 [DOI] [PubMed] [Google Scholar]
- Liang Y., Liu X., Chang H., Ji L., Huang G., Fu Z., et al. (2012). Epidemiological and molecular characteristics of clinical isolates of Streptococcus pyogenes collected between 2005 and 2008 from Chinese children. J. Med. Microbiol. 61 975–983 10.1099/jmm.0.042309-0 [DOI] [PubMed] [Google Scholar]
- Mulyaningsih S., Sporer F., Zimmermann S., Reichling J., Wink M. (2010). Synergistic properties of the terpenoids aromadendrene and 1,8-cineole from the essential oil of Eucalyptus globulus against antibiotic-susceptible and antibiotic-resistant pathogens. Phytomedicine 17 1061–1066 10.1016/j.phymed.2010.06.018 [DOI] [PubMed] [Google Scholar]
- Nostro A., Papalia T. (2012). Antimicrobial activity of carvacrol: current progress and future prospectives. Recent Pat. Antiinfect. Drug Discov. 7 28–35 10.2174/157489112799829684 [DOI] [PubMed] [Google Scholar]
- Odds F. C. (2003). Synergy, antagonism, and what the checkerboard puts between them. J. Antimicrob. Chemother. 52 1 10.1093/jac/dkg301 [DOI] [PubMed] [Google Scholar]
- Palaniappan K., Holley R. A. (2010). Use of natural antimicrobials to increase antibiotic susceptibility of drug resistant bacteria. Int. J. Food Microbiol. 140 164–168 10.1016/j.ijfoodmicro.2010.04.001 [DOI] [PubMed] [Google Scholar]
- Palmieri C., Vecchi M., Littauer P., Sundsfjord A., Varaldo P. E., Facinelli B. (2006). Clonal spread of macrolide- and tetracycline-resistant [erm(A) tet(O)] emm77 Streptococcus pyogenes isolates in Italy and Norway. Antimicrob. Agents Chemother. 50 4229–4230 10.1128/AAC.00943-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai S. K., Moellering R. C., Eliopoulos G. M. (2005). “Antimicrobial combinations,” in Antibiotics in Laboratory Medicine ed. Lorian V. (Philadelphia: Lippincott, Williams and Wilkins) 365–440. [Google Scholar]
- Spinaci C., Magi G., Varaldo P. E., Facinelli B. (2006). Persistence of erythromycin-resistant group a streptococci in cultured respiratory cells. Pediatr. Infect. Dis. J. 25 880–883 10.1097/01.inf.0000238136.63851.4a [DOI] [PubMed] [Google Scholar]
- Spinaci C., Magi G., Zampaloni C., Vitali L. A., Paoletti C., Catania M. R., et al. (2004). Genetic diversity of cell-invasive erythromycin-resistant and -susceptible group A streptococci determined by analysis of the RD2 region of the prtF1 gene. J. Clin. Microbiol. 42 639–644 10.1128/JCM.42.2.639-644.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varaldo P. E., Debbia E. A., Nicoletti G., Pavesio D., Ripa S., Schito G. C., et al. (1999). Nationwide survey in Italy of treatment of Streptococcus pyogenes pharyngitis in children: influence of macrolide resistance on clinical and microbiological outcomes. Artemis-Italy Study Group. Clin. Infect. Dis. 29 869–873 10.1086/520451 [DOI] [PubMed] [Google Scholar]
- Zandri G., Pasquaroli S., Vignaroli C., Talevi S., Manso E., Donelli G., et al. (2012). Detection of viable but not-culturable staphylococci in biofilms from central venous catheters negative on standard microbiological assay. Clin. Microbiol. Infect. 18 259–261 10.1111/j.1469-0691.2012.03893.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.