Abstract
Background:
Cloning of microorganisms on heart endothelium can lead to infective endocarditis (IE). The prototypic lesion of infective endocarditis, the vegetation is a mass of platelets, fibrin, microcolonies of microorganisms, and scant inflammatory cells.
Objectives:
The aim of this study was to evaluate patients with IE and also focusing on echocardiographic data and comparison between TTE (transthoracic echocardiography) and TEE (transesophageal echocardiography) of native and prosthetic valve endocarditis and the final impact of IE (infective endocarditis) in these patients with endocarditis.
Patients and Methods:
All patients with IE admitted to our center between 2007 and 2010 were studied. All echocardiographies were performed by the same echocardiographer. Echocardiography and lab tests were performed for all patients. We used SPSS 16 for data analysis.
Results:
We studied 35 patients, 45% male and 55% female with a mean age of 56.36 ± 12.44 years. Fever (80%) and chills (65.7%) were the most common symptoms. There was only a positive blood culture and enterococci sensitive to vancomycin and amoxicillin. The most involved valve was mitral (54.2%) and then aortic valve (48.5%) (two patients had vegetation on both aortic and mitral valves). In this study, specificity and sensitivity of TEE were 100% and 88.6%. Six patients (17.1%) died and six patients needed surgery.
Conclusions:
Endocarditis is an important disease with a high mortality rate if not treated appropriately. Therefore, these patients need more attention. In echocardiography, vegetation and complications of IE such as abscess and paravalvular leakage can be detected.
Keywords: Transthoracic Echocardiography, Transesophageal Echocardiography, Infective Endocarditis
1. Background
IE (Infective Endocarditis) is a life-threatening infectious disorder with a relatively high mortality rate if misdiagnosed. There are nonspecific and different symptoms in IE diagnosis and in most cases diagnosis is based on fever, vegetation in echocardiography and positive blood culture in some cases (1). In absence of these symptoms, we cannot exclude IE from differential diagnoses of suspected patients. Due to this fact, some diagnostic criteria such as traditional and modified Duke criteria were proposed for IE diagnosis (2-5). The incidence of IE had been raised in the recent years. Epidemiological studies reported that IE features are changed and most of affected patients had been seen in elderly and exposed to nosocomial bacteraemia infection (6-9). Staphylococcus aureus remained the most common cause of IE and less common pathogens are streptococcus strains (8, 10, 11). Although medical management of IE had been developed in the recent years, a half of IE patients develop one complication and their overall mortality remains high (11, 12). In different countries, at risk population for IE are different including elderly patients with valvular diseases, hemodialysis patients and IV drug abusers. Epidemiological studies showed specific features for each country (13). Diagnosis of IE is commonly based on echocardiography, which is the procedure of choice for detection of vegetations (2, 14).
2. Objectives
The present study was designed to evaluate clinical and laboratory presentations of IE patients and comparison between their TTE and TEE findings in Baqiyatallah hospital between 2007 and 2010.
3. Patients and Method
This cross-sectional study was performed between February 2007 and March 2010. We included all patients with endocarditis who were hospitalized in our center. Totally, thirty five patients were included. We confirmed endocarditis diagnosis in these patients according to Duke criteria (2, 15). The definite diagnosis requires positive blood cultures or positive cultures (or histology or PCR of the organism) from vegetation or embolus. TTE and TEE were performed to confirm the diagnosis. Echo features suggestive of IE are moving mass on atrial side of atrioventricular valves or LV side of ventriculoarterial, abscess, new paravalvular or valvular leakage and dehiscence of prosthetic valves. These masses show high frequency movements and could be bulky, linear, round or irregular. In data checklist, age, sex, background cardiac disorders and prosthetic heart valves were recorded in the demographic part. Laboratory tests such as Erythrocyte Sedimentation Rate (ESR), C-reactive Protein (CRP), Complete Blood Cell (CBC) and Blood Culture (in three times) were performed. Dyspnea, fever and cardiac murmur, results of laboratory parameters, blood culture, pathologic, antibiotic resistance, vegetation, pericardial effusion, TTE and TEE, treatment type and results of follow-up were recorded in a check list. After follow-up period for about 13 months, outcome of patients were assessed according to improvement in clinical symptoms and laboratory parameters. To eliminate experimenter bias, all echocardiographies were performed by a same echocardiographer.
3.1. Statistical Analysis
Data was entered SPSS 16.0 for Windows (SPSS Inc., Chicago, Illinois, USA).Student's t-test was used for sub-group analysis. P < 0.05 were assumed to be significant.
4. Results
In the present study, 16 (45%) male and 19 (55%) female patients were included. Their mean age was 56.36 ± 12.44 (35-78) years. Seven patients had a history of mitral valve replacement (MVR), two a history of aortic valve replacement (AVR) and two AVR plus MVR. Seven patients had chronic renal failure, two had diabetes, two hypertension and two kidney transplantation. None of included patients had a history of intravenous drug abuse.
4.1. Clinical Symptoms and Laboratory Findings
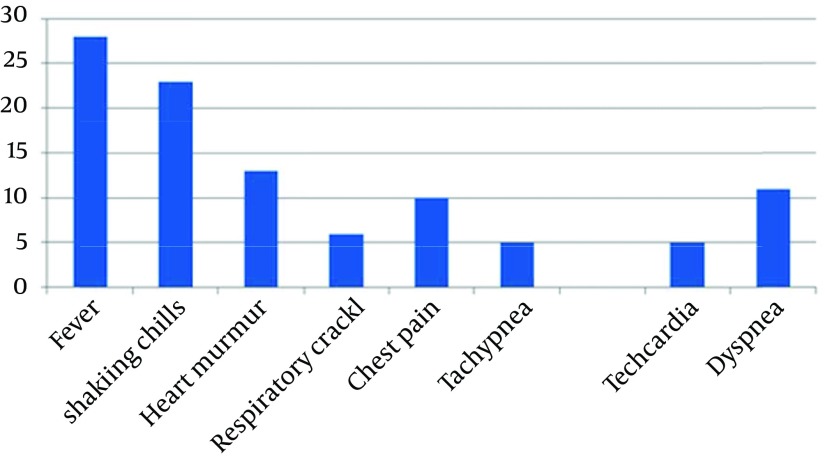
Fever was the most common symptoms among study patients. Cardiac murmur, chest pain and pulmonary crackle had highest frequency, respectively. Details of other symptoms were presented in Figure 1. Mean of white blood cell in study patients was 10530 ± 4490 and 22 (62.8%) patients had leukocytosis. The mean of hemoglobin and ESR in study patients were 10.74 ± 1.47 and 66.79 ± 31.81. Twenty-two (62.8%) patients had positive findings for CRP. Hematuria and proteinuria were present in 5 (13.8%) and 10 (25.7%) patients, respectively. Four patients had pericardial effusion. Only one patient had a positive result for blood culture (Enterococcus sensitive to the Vancomycin and Amoxicillin). Involved valve in 19 patients was mitral including native and prosthetic. Besides, it was aortic valve in 16 patients (including native and prosthetic) and in one patient was native tricuspid valve.
Figure 1. Frequency of Clinical Symptoms in Endocarditis Patients.
4.2. Echocardiographic Findings
In echocardiography examination, five (14.2%) patients had mild, seven (20%) moderate and two (5.7%) severe aortic regurgitation. In patients with mitral valve involvement two, five (14.2%) and three patients had mild, moderate and severe mitral regurgitation, respectively. Mild and moderate tricuspid regurgitation were seen in 15 (42.8%) and six (16.7%) patients. Masses suggestive of vegetation were seen in 31 involved valves by TTE, and TEE revealed vegetations in all patients. In prosthetic AV, one patient presented with abscess and the others with vegetation. In those with prosthetic MV, five patients had vegetations and four vegetations with paravalvular leakage. Comparing TTE and TEE in diagnosis of IE patients, there were four false negative cases without false positive cases in TEE findings. Sensitivity and specificity of TEE in diagnosis of IE patients were 100% and 88.6%, respectively. Other findings of the two echocardiographic methods were the same. Findings of TEE and TTE echocardiographic studies were reported in Table 1.
Table 1. Echocardiographic Parameters a.
| Count Variable | Mean ± SD |
|---|---|
| LVEF | 49.72 ± 4.13 |
| LVEDD, mm | 5.20 ± 0.70 |
| LVESD, mm | 3.47 ± 0.77 |
| IVSD, mm | 1.13 ± 0.1 |
| TRPG | 32.08 ± 10.77 |
| PAP, mm Hg | 39.86 ± 11.40 |
aAbbreviations: IVSD, inter ventricular septal diameter; LVEDD, left ventricle end diastolic diameter; LVEF, left ventricle ejection fraction; LVESD, left ventricle end systolic diameter; PAP, pulmonary artery pressure; TRPG, tricuspid regurgitation (pressure gradient).
The mean of ejection fraction and pulmonary artery pressure were 49.72 ± 4.13 and 39.86 ± 11.40, respectively. Gender of patients had no significant association with cardiac valve involvement. The mean age of patients with mitral valve involvement was not significantly different from other patients (54.45 ± 12.43 vs. 57.20 ± 12.61; P value > 0.05). Patients with aorta valve involvement were significantly older than those without aortic valve involvement (66.64 ± 8.62 vs. 49.82 ± 9.58; P value = 0.00). Vegetation size in nine (25.8%) patients was higher than 10 mm.
4.3. Antibiotic Therapy and Outcome of Patients
Ceftriaxone was prescribed in all patients with a mean duration of 12.68 ± 12.71 days. After that Vancomycin had the highest frequency with a mean duration of 19.97 ± 12.55 days. After treatment period, six patients (17.1%) died so follow-up (FU) was not possible but other patients had FU. Among them two patients had a history of renal transplantation and received immunosuppressive agents and one patient had a history of arterial emboli and coronary artery bypass grafting operation. Six patients needed valve replacement after IE treatment.
5. Discussion
Endocarditis is a fatal disease and most of untreated patients might lose their life few weeks after the diagnosis (15). IE was developed in patients with valvular abnormalities due to several factors such as rheumatic carditis and some variants of streptococcus infection. These symptoms had higher frequency in developing countries due to higher prevalence of rheumatic heart disease (13). IV drug abusers, elderly patients with nosocomial exposure and hemodialysis patients were added to previous at risk patients (7). In the present study, fever had the highest frequency among clinical symptoms. Leukocytosis and high ESR were found in 62.8% of patients. Only one of our patients had positive findings for blood culture. In the present study, male involvement was 45%, but in similar studies male patients had a higher proportion (between four and even eight times more) than females (16). It could be due to more including IV drug abusers (had higher frequency in male patients) in other studies compared to this investigation. Fever and shaking were the most common clinical symptoms; therefore, we must pay more attention to IE diagnosis in suspected patients with risk factors such as cardiac valve replacement and IV-drug abuse. In these cases, more laboratory tests and echocardiographic examination are needed to rollout IE diagnosis.
We had only one patient with positive finding for blood culture, which is the same with other similar studies; only in one study four positive blood cultures were reported among 20 patients with infective endocarditis (17). It could be due to different laboratory techniques for blood culture and previous use of antibiotics. Echocardiography is a noninvasive and available method of choice to evaluate presence of vegetations and its complications. It is recommended to perform TTE in all suspected patients and in both native and prosthetic valves (13, 14) it could help to diagnose IE. Nevertheless, TEE has a high sensitivity for IE, as in our study four patients had vegetations confirmed by TEE (one patient with prosthetic AV, one patient with native valve endocarditis of MV and two with prosthetic MV). However, in other patients with both techniques vegetations, paravalvular leakage or abscess could be evaluated with the same accuracy. Therefore, echocardiography has an important role in IE diagnosis, also repeating the procedure in appropriate intervals is helpful to avoid missing any patient with IE.
5.1. Limitations
The present study had some limitations; first, we performed the study on a small group of IE patients, thus we suggest performing further studies on larger sample size. Second, the present study was performed only in one hospital and multicenter studies with more patients might yield better results. Longer follow-up is also important for better evaluating these patients. Patients with endocarditis need more accurate clinical evaluation and early diagnosis in at risk populations, which can prevent disease progression. It is important to perform echocardiography (TTE and especially TEE) in endocarditis suspected patients after clinical and laboratory evaluation. In dead patients with negative blood culture, PCR was recommended to detect resistant pathogens.
Acknowledgments
Special thanks to echocardiography personnel Miss Sharifi, Miss Ahmadi Pour, Miss Arezoo and Miss Mousavi.
Footnotes
Authors’ Contributions:Dr. Hosseini was the physician who treated patients and referred them to Echolab; Dr. Bakhshian did the analysis; Dr. Moshkani did echocardiographies and filled required data and writing the first and final drafts; Dr. Bahrami did the analysis and writing the first draft; Dr. Sate filled the questionnaires and did the FU; Dr. Abdar gave important recommendations and revised the manuscript.
References
- 1.Brouqui P, Raoult D. Endocarditis due to rare and fastidious bacteria. Clin Microbiol Rev. 2001;14(1):177–207. doi: 10.1128/CMR.14.1.177-207.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200–9. doi: 10.1016/0002-9343(94)90143-0. [DOI] [PubMed] [Google Scholar]
- 3.Fournier PE, Casalta JP, Habib G, Messana T, Raoult D. Modification of the diagnostic criteria proposed by the Duke Endocarditis Service to permit improved diagnosis of Q fever endocarditis. Am J Med. 1996;100(6):629–33. doi: 10.1016/s0002-9343(96)00040-x. [DOI] [PubMed] [Google Scholar]
- 4.Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG, Jr., Ryan T, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30(4):633–8. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 5.Bayer AS. Diagnostic criteria for identifying cases of endocarditis--revisiting the Duke criteria two years later. Clin Infect Dis. 1996;23(2):303–4. doi: 10.1093/clinids/23.2.303. [DOI] [PubMed] [Google Scholar]
- 6.Hoen B, Alla F, Selton-Suty C, Beguinot I, Bouvet A, Briancon S, et al. Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA. 2002;288(1):75–81. doi: 10.1001/jama.288.1.75. [DOI] [PubMed] [Google Scholar]
- 7.Que YA, Moreillon P. Infective endocarditis. Nat Rev Cardiol. 2011;8(6):322–36. doi: 10.1038/nrcardio.2011.43. [DOI] [PubMed] [Google Scholar]
- 8.Mouly S, Ruimy R, Launay O, Arnoult F, Brochet E, Trouillet JL, et al. The changing clinical aspects of infective endocarditis: descriptive review of 90 episodes in a French teaching hospital and risk factors for death. J Infect. 2002;45(4):246–56. doi: 10.1053/jinf.2002.1058. [DOI] [PubMed] [Google Scholar]
- 9.Devlin RK, Andrews MM, von Reyn CF. Recent trends in infective endocarditis: influence of case definitions. Curr Opin Cardiol. 2004;19(2):134–9. doi: 10.1097/00001573-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Loupa C, Mavroidi N, Boutsikakis I, Paniara O, Deligarou O, Manoli H, et al. Infective endocarditis in Greece: a changing profile. Epidemiological, microbiological and therapeutic data. Clin Microbiol Infect. 2004;10(6):556–61. doi: 10.1111/j.1469-0691.2004.00884.x. [DOI] [PubMed] [Google Scholar]
- 11.Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med. 2001;345(18):1318–30. doi: 10.1056/NEJMra010082. [DOI] [PubMed] [Google Scholar]
- 12.Cecchi E, Forno D, Imazio M, Migliardi A, Gnavi R, Dal Conte I, et al. New trends in the epidemiological and clinical features of infective endocarditis: results of a multicenter prospective study. Ital Heart J. 2004;5(4):249–56. [PubMed] [Google Scholar]
- 13.Tleyjeh IM, Abdel-Latif A, Rahbi H, Scott CG, Bailey KR, Steckelberg JM, et al. A systematic review of population-based studies of infective endocarditis. Chest. 2007;132(3):1025–35. doi: 10.1378/chest.06-2048. [DOI] [PubMed] [Google Scholar]
- 14.Daniel WG, Schroder E, Nonnast Daniel B, Lichtlen PR. Conventional and transoesophageal echocardiography in the diagnosis of infective endocarditis. Eur Heart J. 1987;8(suppl J):287–92. doi: 10.1093/eurheartj/8.suppl_J.287. [DOI] [Google Scholar]
- 15.Braunwald K, Hauser F, Jameson L. Harrison's Internal Medicine. Infective Endocarditis. 2008. pp. 731–40. [Google Scholar]
- 16.Bayatmakoo J, Bayatmakoo R, Jabbary N, Jafary S. Evaluation of Response to Drug Treatment in Patients with Endocarditis Based on Clinical and Laboratory Findings. Med J Tabriz Univ Med Sci Health Serv. 2007;30(2):41–5. [Google Scholar]
- 17.Alavi S, Ahmadi F, Nashibi R. Comparison of serum levels of CRP, RF and CIC before and after treatment in hospitalized patients with infective endocarditis in Ahvaz- Iran. J Gorgan Univ Med Sci. 2010;12(1):48–55. [Google Scholar]
- 18.Tleyjeh IM, Abdel-Latif A, Rahbi H, Scott CG, Bailey KR, Steckelberg JM, et al. A systematic review of population-based studies of infective endocarditis. Chest. 2007;132(3):1025–35. doi: 10.1378/chest.06-2048. [DOI] [PubMed] [Google Scholar]