Abstract
Introduction:
Pulmonary vein (PV) isolation is considered as a key to atrial fibrillation (AF) treatment. Cryoballoon ablation is an effective therapy for PV isolation for AF with minimal side effects and was approved by the US Food and Drug Administration (FDA) several years ago. Successful isolation of PVs during cryoablation depends on the balloon temperature and helps in early identification of noneffective cryoballoon applications. A lower balloon temperature has been associated with long-term success in isolation of PVs.
Case Presentation:
At the start of the procedure, the cryoconsole displayed “low refrigerant level”. After a few cycles of successful cryoballoon applications, for a fresh application for a new PV, the optimal temperature was not obtained in spite of obtaining good grade of occlusion and ostial positioning for right inferior pulmonary vein (RIPV). Later, immediately after changing the refrigerant cylinder, suitable temperature was obtained. We faced this situation thrice in a span of eight months.
Conclusion:
Low refrigerant level may cause nonoptimal temperature during cryoablation, which can be resolved by premature change of a gas cylinder.
Keywords: Atrial Fibrillation, Cryoablation, Pulmonary vein, refrigeration
1. Introduction
Cryoballoon ablation is an effective therapy for pulmonary vein (PV) isolation for atrial fibrillation (AF) with minimal side effects (1-3). The US Food and Drug Administration (FDA) approved cryoballoon several years ago. Recently, this technology has also been used concomitantly with epicardial radiofrequency ablation with good long-term success results for AF ablation (4). The second-generation cryoballoon (CB-2G) has been introduced recently with more cooling points, thus delivering more uniform lesions around the PVs, resulting in afaster and less complicated procedure (5-8). Successful isolation of PVs during cryoablation depends on the balloon temperature and helps in early identification of noneffective cryoballoon applications (9). A lower balloon temperature has been associated with long-term success of isolation of the PVs (10). To the best of our knowledge, low refrigerant level has never been reported to cause nonoptimal temperature during cryoablation; moreover, it has been resolved by premature change of gas cylinder. Given the widespread use of this technology and its increasing usage in the medical community, this situation commands better attention and understanding.
2. Case Presentation
A 59-year-old man had a history of four years of paroxysmal AF. He was normotensive and euglycemic. Due to recurrent symptomatic AF episodes and subsequent failure of antiarrhythmic drugs, he underwent a cryoballoon ablation of the PV. Under local anesthesia, His and coronary sinus catheter were inserted via the left groin. Cryoconsole was switched on for cryotherapy, but it displayed “low refrigerant level”. After trans-septal puncture, angiogram of the left atrium revealed left-sided common PV ostia of 29.4 mm, right superior PV of 24 mm, and right inferior PV of 14 mm. Successful ablation of all other PVs except for the right inferior PV were performed using six application cycles of four minutes each with 28 mm cryoballoon (Arctic FrontTM, Medtronic; CB, Medtronic, Minneapolis, MN, USA). Then cryoballoon was positioned to the ostium of right inferior PV. Vein occlusion was monitored for cryoballoon-to-PV contact by observing during the injection of a 50%-diluted contrast medium distally into the PV. This is graded on a 1 to 4 scale, with 1 being minimum occlusion and 4 being complete occlusion. For this PV, the grade of occlusion obtained was 4/4 (Figure 1). Freezing was started. In spite of waiting for more than 60 seconds, the minimum temperature did not cross beyond -34°C. Special maneuvers as “pull-down technique” and “hockey stick technique” were tried, without any success (11). The application was stopped considering the nonoptimal temperature (9). The cryoballoon was repositioned for better PV contact, reverified by diluted contrast injection to be 4/4 of grade of occlusion. However, the temperature again did not cross beyond -30°C. The application was again stopped at 60 seconds. After optimal positioning cryoablation was reattempted. Surprisingly, again, the temperature did not cross beyond -28°C. We were intrigued for the reason behind this. Afterwards, a final try with cryoballoon was thought for before switching to cryocatheter for AchieveTM (Medtronic Inc.) guided touchups. Finally, after observing the 4/4 occlusion grade, freezing was restarted for the third time. To our disappointment even after 60 seconds, the temperature was still hovering around -9°C. The moment the freezing application was to be stopped, the cryoconsole screen flashed, “The pressure is low in the system. Ensure the refrigerant tank is open”. Ultimately, the refrigerant cylinder was changed. Cryoablation was reinitiated after ensuring the 4/4 occlusion and optimal positioning. Minimum ablation temperature of -47°C was reached with acute successful isolation of PVs (Figure 2). We faced similar situation described above three times in a span of nine months for different PVs. After communicating about this problem to Medtronic’s local representative, data was retrospectively collected from cryoconsole for further investigations. The flow of the gas through the umbilical (displayed at a cryoconsole) was measured and investigated in the data files. However, the analysis showed no known technical issues.
Figure 1. Fluoroscopy Image Showing Complete Occlusion of Right Inferior Pulmonary Vein Using 50% Diluted Contrast With Cryoballoon and in-Situ Catheters.
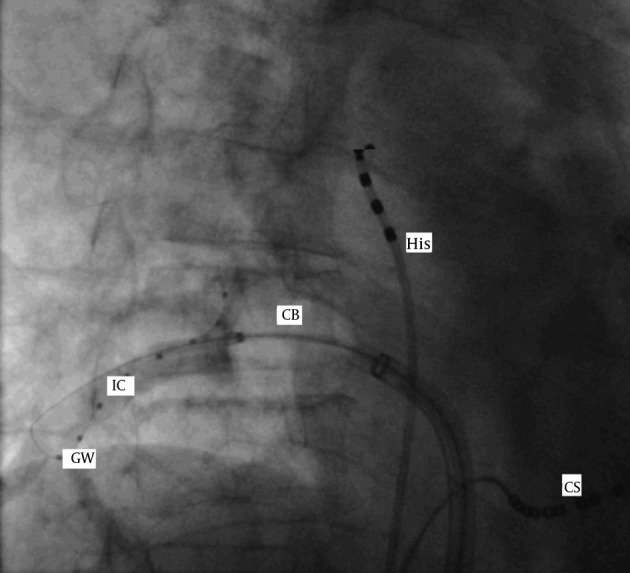
GW, achieve catheter; IC, impending contrast; CB, cryoballoon; His, His catheter; CS, coronary sinus catheter.
Figure 2. The Cryoconsole Screen.
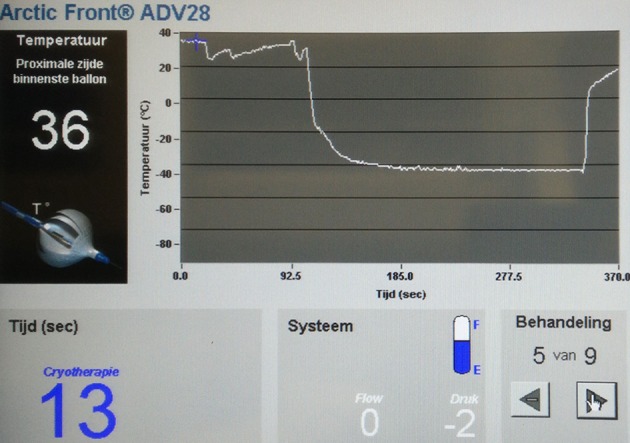
The minimal temperature achieved (-47°C) following the change of the refrigerant tank.
If nonoptimal temperature is obtained in spite of good grade of occlusion of cryoballoon and optimal positioning, early change of a refrigerant cylinder ought to be considered in case of “low refrigerant level” cryoconsole display. Earlier change may be considered in spite of absence of the system notice, stating “The pressure is low in the system”, to decrease the procedure time and unnecessary radiation exposure. Retrospectively, it may be suggested to the device manufacturer for use of better pressure-sensitive refrigerant cylinder valve or earlier system notification for change of the refrigerant cylinder.
3. Discussion
It is advisable to consider premature change of a refrigerant cylinder while it is working at “low refrigerant level” and is still unable to obtain the optimal temperature, in spite of obtaining good occlusion of a PV during cryoablation.
Footnotes
Authors’ Contributions:Study concept and design, acquisition of data, analysis and interpretation of data and drafting of the manuscript: Narendra Kumar. Critical revision of the manuscript for important intellectual content: Trang Dinh and Suzanne Philippens. Administrative, technical, and material support: Rachel Ter Bekke, Kevin Phan and Randolph Manusama. Study supervision: Jos Maessen and Carl Timmermans.
References
- 1.Kumar N, Timmermans C, Pison L, Crijns H. Hemoptysis: deja vu for cryoballoon use for pulmonary vein isolation for atrial fibrillation ablation. Chest. 2014;145(6):1435. doi: 10.1378/chest.14-0236. [DOI] [PubMed] [Google Scholar]
- 2.Kumar N, Timmermans C, Das M, Pison L, Maessen J, Crijns H. Re: CT imaging of complications of catheter ablation for atrial fibrillation. Clin Radiol. 2014;69(8):e367–8. doi: 10.1016/j.crad.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Kumar N, Timmermans C, Das M, Dassen W, Philippens S, Maessen J, et al. Hemoptysis after cryoablation for atrial fibrillation: truth or just a myth? Chest. 2014;146(5):e173–5. doi: 10.1378/chest.14-1600. [DOI] [PubMed] [Google Scholar]
- 4.Kumar N, Pison L, La Meir M, Maessen J, Crijns HJ. Hybrid approach to atrial fibrillation ablation using bipolar radiofrequency devices epicardially and cryoballoon endocardially. Interact Cardiovasc Thorac Surg. 2014;19(4):590–4. doi: 10.1093/icvts/ivu189. [DOI] [PubMed] [Google Scholar]
- 5.Knecht S, Kuhne M, Osswald S, Sticherling C. Quantitative assessment of a second-generation cryoballoon ablation catheter with new cooling technology-a perspective on potential implications on outcome. J Interv Card Electrophysiol. 2014;40(1):17–21. doi: 10.1007/s10840-014-9883-1. [DOI] [PubMed] [Google Scholar]
- 6.Straube F, Dorwarth U, Schmidt M, Wankerl M, Ebersberger U, Hoffmann E. Comparison of the first and second cryoballoon: high-volume single-center safety and efficacy analysis. Circ Arrhythm Electrophysiol. 2014;7(2):293–9. doi: 10.1161/CIRCEP.113.000899. [DOI] [PubMed] [Google Scholar]
- 7.Kumar N, Blaauw Y, Timmermans C, Pison L, Vernooy K, Crijns H. Adenosine testing after second-generation balloon devices (cryothermal and laser) mediated pulmonary vein ablation for atrial fibrillation. J Interv Card Electrophysiol. 2014;41(1):91–7. doi: 10.1007/s10840-014-9921-z. [DOI] [PubMed] [Google Scholar]
- 8.Kumar N, Dinh T, Phan K, Timmermans C, Dassen W, Phillippens S. Adenosine Testing after Second generation Cryoballoon Ablation (ATSCA) study improves clinical success rate for atrial fibrillation. Europace. 2014 doi: 10.1093/europace/euu352. [DOI] [PubMed]
- 9.Furnkranz A, Koster I, Chun KR, Metzner A, Mathew S, Konstantinidou M, et al. Cryoballoon temperature predicts acute pulmonary vein isolation. Heart Rhythm. 2011;8(6):821–5. doi: 10.1016/j.hrthm.2011.01.044. [DOI] [PubMed] [Google Scholar]
- 10.Schade A, Langbein A, Spehl S, Barth S, Deneke T, Groschup G, et al. Recurrence of paroxysmal atrial fibrillation after cryoisolation of the pulmonary veins. Is a "redo" procedure using the cryoballoon useful? J Interv Card Electrophysiol. 2013;36(3):287–95. doi: 10.1007/s10840-012-9725-y. [DOI] [PubMed] [Google Scholar]
- 11.Chun KR, Schmidt B, Metzner A, Tilz R, Zerm T, Koster I, et al. The 'single big cryoballoon' technique for acute pulmonary vein isolation in patients with paroxysmal atrial fibrillation: a prospective observational single centre study. Eur Heart J. 2009;30(6):699–709. doi: 10.1093/eurheartj/ehn570. [DOI] [PMC free article] [PubMed] [Google Scholar]


