Abstract
Chronic beryllium disease (CBD) is an exposure-related granulomatous disease mimicking sarcoidosis. Beryllium exposure-associated disease occurs mainly via inhalation, but skin may also be a source of sensitization. A 65-year-old male with a history of war-related shrapnel wounds was initially diagnosed with pulmonary sarcoidosis. Twenty years later, the possibility of a metal-related etiology for the lung disease was raised. A beryllium lymphocyte proliferation test, elemental analysis of removed shrapnel, and genetic studies were consistent with a diagnosis of CBD. This case demonstrates that retained beryllium-containing foreign bodies can be linked to a pathophysiologic response in the lung consistent with CBD.
Keywords: beryllium sensitization, shrapnel, chest wall
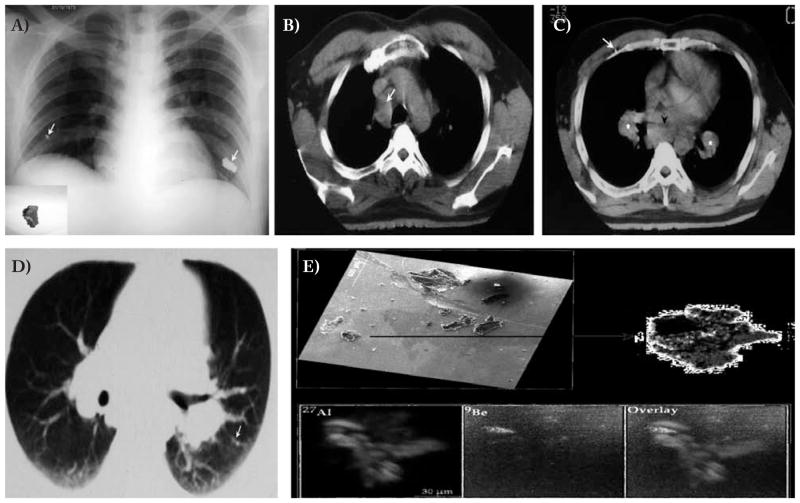
A 41-year-old non-smoking male was referred due to persistent dyspnea and non-productive cough. Thirteen years previously, serving as a paramedic in the Suez Canal in the 1973 Yom Kippur War, he experienced a traumatic injury from an 81 mm mortar shell explosion, with retained shrapnel in the chest wall. Some fragments were surgically removed prior to his presentation in 1986 (Fig. 1, Panel A). At the time of his initial evaluation, the physical examination was unremarkable except for a few scars in the chest wall. Radiographic assessment, including computerized tomography (CT) (Fig. 1, Panels B–D), demonstrated bilateral hilar and mediastinal lymphadenopathy, a few small subpleural nodular opacities, and confirmed retained metallic shrapnel in the right chest wall. Pulmonary function testing revealed a minimal restrictive pattern (total lung capacity [TLC] 79% of predicted) and a slightly reduced diffusing capacity for carbon monoxide adjusted for alveolar volume (DLco/VA, 78% of predicted).
Fig. 1.
Panel A shows the initial (1973) chest radiograph revealing the two pieces of shrapnel in the chest wall (white arrows). The piece of shrapnel from the left chest wall was excised later (Panel A insert). Panels B and C show the 1986 computerized tomogram (CT) of the chest (axial images, soft tissue window): note in B, right paratracheal adenopathy (white arrow) and in C, bilateral hilar adenopathy (asterisks), subcarinal adenopathy (black arrowhead) and retained metallic shrapnel in the right chest wall, deep to the pectoralis muscles (white arrow). Panel D shows an image from the same the chest CT (axial image, lung window): a few subpleural micro-nodules can be seen adjacent to the left fissure. Panel E shows selected scanning electron microscopy (SEM) and secondary ion mass spectrometry (SIMS) images of shrapnel material: SEM of several fragments pressed in indium substrate and a detailed view of one fragment (indicated by arrow to insert) and the SIMS elemental imaging analysis of that fragment. The 27Al+ SIMS image shows the micron scale distribution of aluminum in the fragment in red. The presence of beryllium in this fragment was detected in the 9Be+ SIMS image, shown in green. The overlaying of these two images reveals that the shrapnel fragment region rich in beryllium is depleted in aluminum. The recorded 27Al+ SIMS image was integrated for one second and the 9Be+ SIMS image was integrated for two minutes.
Evaluation for suspected sarcoidosis, including bronchoalveolar lavage, revealed lymphocytosis (27%), a CD4/CD8 ratio of 2.6, a positive Kveim-Siltzbach (Kveim) skin test, and gallium scanning demonstrating increased uptake consistent with pulmonary disease. A transbronchial biopsy was nondiagnostic. A presumptive diagnosis of Stage I sarcoidosis was made; his shrapnel exposure was not considered in his differential diagnosis at that time. The patient’s respiratory symptoms improved without specific treatment; he was clinically stable in yearly follow-up. Twenty years later (2006), he was invited to take part in a clinical trial involving sarcoidosis. Repeat CT imaging demonstrated improvement of the lymphadenopathy and no parenchymal involvement. The DLco/VA, however, had fallen to 65% predicted; the TLC was reduced to 90% predicted. His occupational history was non-contributory: he had been an office worker since military discharge.
At this point, the patient himself raised the possibility of a link between his war wound and sarcoidosis, providing a piece of the previously excised shrapnel. The possibility of beryllium-sensitization with associated pulmonary disease mimicking sarcoidosis was considered, because beryllium may be present in military hardware. A beryllium lymphocyte proliferation test (BeLPT), genetic susceptibility evaluation, and scanning electron microscopy (SEM) and secondary ion mass spectrometry (SIMS) of the shrapnel were performed.
The BeLPT was performed as described elsewhere (1), yielding two strongly positive tests after 4–6 days of incubation at varying beryllium concentrations of (Test 100 μM=4.1–7.6; 10 μM=3.3–25.3; 1 μM=1.76–23; Test 2: 100 μM=2.7–4.2; 10 μM=10.9–4.27; 1 μM=3.91–2.3). Genomic DNA genotyping for HLA-DPB1 using a rapid nonenzymatic method and sequence-specific primers-polymerase chain reaction demonstrated heterozygosity for HLA DPB1Glu 69 with 0201(Glu69+)/0402(Glu69−) alleles, consistent with genetic susceptibility to chronic beryllium disease (CBD) (2).
In light of the positive BeLPT, previously removed shrapnel (still in the patient’s possession) was analyzed by an ASPEX® SEM using a 20 KV beam. Major contents were aluminum and brass (copper and zinc); no beryllium was detected. Because SEM is insensitive for low-level beryllium detection, however, we additionally employed SIMS methodology (3), confirming traces of beryllium within the matrix of the predominantly aluminum shrapnel fragment (Fig. 1, Panel E). The 27Al SIMS image is shown in red, while the beryllium (9Be) image shown in green.
Discussion
This is the first reported case of shrapnel-induced beryllium sensitization with pulmonary involvement in a presentation consistent with CBD. As is common with CBD, the patient long carried a sarcoidosis diagnosis. Sarcoidosis is an idiopathic, systemic disorder with a variable clinical presentation; non-caseating granulomatous inflammation is the hallmark of disease. This pathology, however, is a nonspecific finding also associated with CBD and, rarely, following the inhalation of other metals as well. Indeed, CBD is the paradigmatic example of a metal-related immune-mediated response mimicking sarcoidosis (2). Our case underscores the cautionary principle that CBD should always be considered in the differential diagnosis of an otherwise sarcoid-like lung response, particularly when a history has been elicited of exposure to beryllium or to metals likely contaminated with beryllium. Consistent with the challenge of such case detection, we previously demonstrated the crucial role of occupational history in the differential diagnosis of granulomatous lung disease, finding that 6% of patients occupationally exposed to metals and labeled as having sarcoidosis, actually had CBD (1).
We confirmed the presence of beryllium in the matrix of the shrapnel using SIMS, even though the sample was predominantly comprised of aluminum. Of note, beryllium sensitization has been shown among aluminum smelter workers, albeit at a fairly low prevalence (4). The bauxite ore from which aluminum is extracted is known to contain beryllium not completely removed in smelting, thus end-use aluminum may still contain traces of beryllium. The beryllium content of the shrapnel was quite low but consistent with well-recognized, inherent beryllium content of aluminum, rather than as an intentional additive.
This case also raises intriguing questions regarding non-inhalational triggers of beryllium-related disease. Skin contact is believed to be a potential route for systemic sensitization for beryllium (5). This exposure route is difficult to isolate, because in any occupational milieu with skin contact, some degree of concomitant inhalation exposure is also likely. In our case, there was little likelihood of beryllium inhalation. One must assume, therefore, that either some amount of the metal was carried to effector cells resident in the lung or, conversely, that cells immunologically activated elsewhere migrated to the lung. Peripheral blood T cells tested before and after patch testing in sensitized patients provide evidence for the mobilization of beryllium-reactive T cells into the circulating blood pool (6). Our patient’s genetic susceptibility is also likely to have further contributed to the pathogenesis of his disease (2).
Radiographic abnormalities and improvement in gas exchange were reportedly reversible in some workers when peak air concentrations of beryllium were decreased (7). This might explain our patient’s clinical improvement over the years following surgical excision of the shrapnel, although this is speculative. The positive reaction to the Kveim test raises the question of our patient being sensitized to beryllium with concomitant, but unrelated sarcoidosis. While this is possible, the positive Kveim test might have been due to cross-reactivity between sarcoidosis and CBD disease biomarkers, an etiological pathway common to both diseases, or to some other, un-characterized property of the Kveim test material. Non-specificity of the Kveim Test is supported by its positivity in selected Crohn’s disease patients (8).
Chronically retained shrapnel and bullet fragments have been shown to carry the risk of delayed complications after a relatively long latency. The new onset of sterile inflammatory local reactions associated with shrapnel locally retained for decades has been described, although without pulmonary or other distant site complications (9). Case reports of local tumors, including in the lung, believed to have been caused by shrapnel or bullet fragments rarely have been reported as well (10). We now add to the sparse literature on this subject this case of shrapnel-induced beryllium sensitization and associated pulmonary disease, findings consistent with CBD. The question remains unanswered as to whether other cases of disease due to similar exposures have occurred, yet have been misdiagnosed as sarcoidosis. At the very least, patients with retained shrapnel and a clinical presentation consistent with sarcoidosis should be assessed for beryllium sensitization. This may also include consideration of shrapnel removal where feasible. To date, this has not been recommended for the remaining fragment deeply-imbedded in the chest wall of our patient.
Acknowledgments
We thank NYSTAR support for Cornell SIMS Laboratory and Department of Pathology, SUNY Upstate Medical University.
References
- 1.Fireman E, Haimsky E, Neudorfer M, Priel I, Lerman Y. Misdiagnosis of sarcoidosis in patients with chronic beryllium disease. Sarcoidosis Vasc Diffuse Lung Dis. 2003;20:144–8. [PubMed] [Google Scholar]
- 2.Sawyer RT, Maier LA. Chronic beryllium disease: an updated model interaction between innate and acquired immunity. Biometals. 2011;24 (1):1–17. doi: 10.1007/s10534-010-9376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hervig RL. Beryllium analyses by secondary ion mass spectrometry. Rev Minerol Geochem. 2002;50:319–32. [Google Scholar]
- 4.Taiwo OA, Slade MD, Cantley LF, et al. Beryllium sensitization in aluminum smelter workers. J Occup Environ Med. 2008;50:157–62. doi: 10.1097/JOM.0b013e318161783f. [DOI] [PubMed] [Google Scholar]
- 5.Tinkle SS, Antonini JM, Rich BA, et al. Skin as a route of exposure and sensitization in chronic beryllium disease. Environ Health Perspect. 2003;111:1202–8. doi: 10.1289/ehp.5999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fontenot AP, Maier LA, Canavera SJ, et al. Beryllium skin patch testing to analyze T cell stimulation and granulomatous inflammation in the lung. J Immunol. 2002;168:3627–34. doi: 10.4049/jimmunol.168.7.3627. [DOI] [PubMed] [Google Scholar]
- 7.Sprince NL, Kanarek DJ, Weber AL, Chamberlin RI, Kazemi H. Reversible respiratory disease in beryllium workers. Am Rev Respir Dis. 1978;117:1011–7. doi: 10.1164/arrd.1978.117.6.1011. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell DN, Dyer NC, Cannon P, Hinson KF, Willoughby JM. The Kveim test in Crohn’s disease. Postgrad Med J. 1970;46:491–4. doi: 10.1136/pgmj.46.538.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eylon S, Mosheiff R, Liergall M, Wolf E, Brocke L, Peyser A. Delayed reaction to shrapnel retained in soft tissue. Injury. 2005;36:275–81. doi: 10.1016/j.injury.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Knox J, Wilkinson A. Shrapnel presenting with symptoms 62 years after wounding. (Letter) Br Med J. 1981;283:193. doi: 10.1136/bmj.283.6285.193. [DOI] [PMC free article] [PubMed] [Google Scholar]