Abstract
The characteristics of coronary artery disease (CAD) are gradual thickening of the coronary walls and narrowing of the vascular lumen due to the built-up of atherosclerosis plaques. Those morphological changes can be noninvasively detected by coronary MRI/MRA. In addition, functional changes, such as coronary wall distensibility and flow changes may also be evaluated with MRI. However, the application of current MRI/MRA techniques is limited in clinical practice due to several adverse technical and physiological factors, such as cardiac motion and respiratory motion. Many technical innovations have been adopted to address those problems from multiple aspects.
Keywords: Coronary artery disease, magnetic resonance imaging, noninvasive
Introduction
Coronary artery disease (CAD) is the leading cause of death on the world. The characteristics of CAD are gradual thickening of the coronary walls and narrowing of the vascular lumen due to the build-up of atherosclerosis plaques. Subclinical CAD may “silently” progress over a long time period until coronary events, a group of symptoms attributed to myocardial ischemia, affect patients 1,2. Therefore, the detection of CAD in its early stage is clinically significant. However, the morphological and functional features of the remodeled coronary artery, which may convey risk of subclinical CAD, have not been comprehensively investigated in asymptomatic individuals who do not have documented or suspected structural cardiovascular disease. This knowledge gap exists mainly because clinical examinations for detecting coronary wall are either invasive or require X-ray exposure. Therefore, noninvasive imaging methods for the evaluation of coronary artery are highly desired for optimal cardiovascular prevention. Over the past decade, magnetic resonance imaging/angiography (MRI/MRA) has emerged as a promising noninvasive method for observing both morphological and functional changes on coronary walls 3,4. In this review chapter, we will summarize state-of art coronary MRI/MRA techniques for detecting CAD from various aspects, including luminal stenosis, coronary wall plaques and coronary functional changes. In addition, clinical application and limitations of current coronary MRI techniques in clinical practice will also be discussed.
Imaging of coronary lumen using MRI
Traditionally, stenosis of the coronary lumen is an indicator of obstructive CAD and subsequent treatments, such as coronary artery bypass graft surgery (CABG) and percutaneous transluminal coronary angioplasty (PTCA), is based on extent and severity of disease. Multiple bright-blood MRI pulse sequences can be used to rapidly image coronary lumen and detect coronary stenosis, such as spoiled gradient echo and steady-state free precession (SSFP) 5. (Box 1)
Box 1.
| MRI sequences used in the evaluation of coronary luminal stenosis (bright-blood)* | Need contrast agent? | |||
|---|---|---|---|---|
| Spoiled gradient echo | FLASH (Fast low angle shot magnetic resonance imaging) | SPGR (Spoiled Gradient Recall Acquisition using Steady States) | T1 FFE (T1-weighted Fast Field Echo) | Yes |
| SSFP | FISP (Fast Imaging with Steady-state Precession) | GRASS (Gradient Recall Acquisition using Steady States) | FFE (Fast Field Echo) | No |
Names vary from different MRI scanner manufacturers
Regenfus et al. evaluated 50 patients with suspected CAD using a turbo FLASH sequence within one single breath-hold. The authors reported that 268 of 350 (76.6%) coronary segments could be evaluated. In those coronary segments, 48 of 56 luminal stenoses could be detected by MRI 6. With T1-shortening contrast agents, such as gadolinium, spoiled gradient echo sequences can be used to depict contours of the coronary lumen. In a study with 16 healthy volunteer, Li et al. demonstrated that gadolinium may significantly increase the image quality of coronary MRA in 2 breath-holds. However, spatial resolution and coverage of coronary MRA may be limited by the length of breath-hold and the duration of sustainable blood pool enhancement generated by contrast agents 7. Using a free-breathing technique and a scheme of slow infusion (0.3 ml/s) of the contrast agent (for prolonged T1 contrast between vessel wall and the blood pool), Bi et al. demonstrated that coronary MRA (FLASH sequence) is capable of imaging the whole coronary tree within a relatively short period (4.5 +/- 0.6 min) for 8 volunteers 8. In a single center study, Yang et al. performed contrast-enhanced whole-heart MRA in 69 consecutive patients with suspected CAD. The authors found that whole-heart MRA could identify clinically significant coronary stenosis in 32 patients and could rule out CAD in 23 patients. On a per-segment basis, MRA had high sensitivity (91.6%), specificity (83.1%), and accuracy (84.1%) for the detection of CAD (using X-ray angiography as the “gold standard”). On a per-patient basis, these values for accurate CAD diagnosis were 94.1%, 82.1%, and 88.7%, respectively 9. Recently, the same group also demonstrated a comparable diagnostic accuracy for the detection of CAD (significant coronary luminal stenosis) in 110 patients using similar imaging techniques with a 32 channel coil 10.
Some CAD patients may have varying degrees of co-existing kidney dysfunction 11. Therefore, noncontrast coronary MRA techniques may provide added benefits in that patient population by avoiding nephrotoxic contrast agents and risk of Nephrogenic Systemic Fibrosis (NSF). The high T2/T1 ratio of the blood provides strong blood signal and may serve as an intrinsic contrast agent for the SSFP technique in coronary MRA 12,13. Using noncontrast whole-heart coronary MRA, Kato et al. detected significant CAD in 138 patients with suspected CAD with high sensitivity and high negative predictive value (88%) 14. Using quantitative analysis of coronary MRA, Yonezawa et al. found that ROC curve analysis in a segment-based analysis for identifying significant coronary stenosis was 0.96 15. In a multi-center study, coronary MRA provided an accuracy of 72 % (95 CI, 63% to 81%) in diagnosing CAD 16. Stuber et al. demonstrated good agreement of anatomy and pathology between coronary MRA and X-ray angiography in depicting the coronary tree in 7 CAD patients confirmed by X-ray angiography and 15 healthy adult volunteers 17. Indicated by higher sensitivity, specificity and area under the ROC curve (AUC), Liu et al. found that noncontrast coronary MRA is superior to coronary CTA for delineating luminal narrowing of the coronary artery in the segments with heavy calcification 18. Yoon et al. studied 207 patients with suspected CAD using noncontrast whole-heart coronary MRA. The authors observed 10 coronary events (half of them were deadly events) in 84 patients with significant coronary stenosis identified with MRA during a follow-up of 25 months. While only 1 coronary event happened in 123 patients without CAD (also defined using MRA findings). Cox regression demonstrated that a coronary stenosis on MRA is an independent risk factor associated with significant increase for all cardiac events (RR= 20.78, p = 0.001) 19. Figure 1 and 2 demonstrate that coronary MRA (with and without contrast enhancement) is able to show coronary stenosis.
Figure 1.
A 75 year-old male patient with atypical chest pain. A lumen stenosis on the LCX was identified by contrast-enhanced MRA (courtesy of Dr. Debiao Li)
Source of the figure: reference # 9, with permission of Dr. Debiao Li
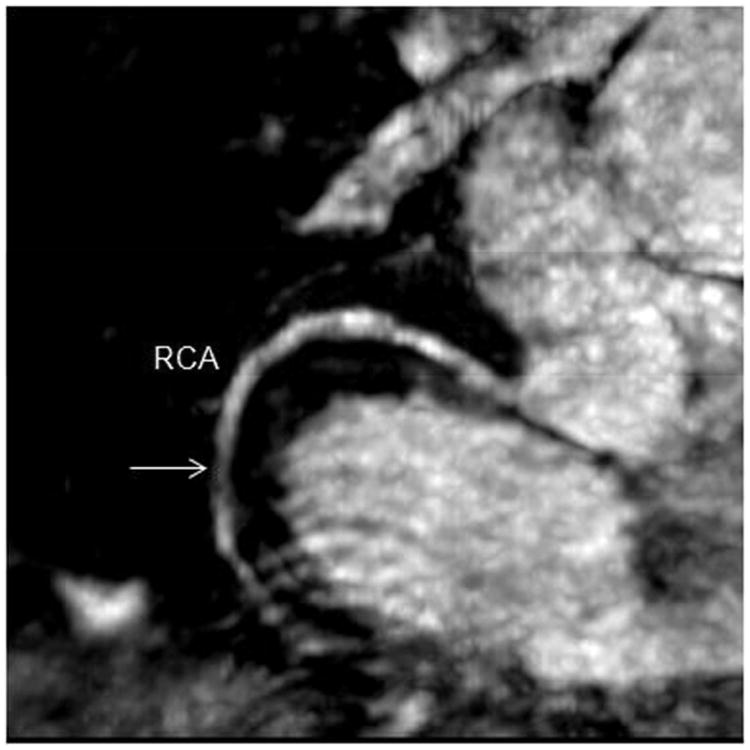
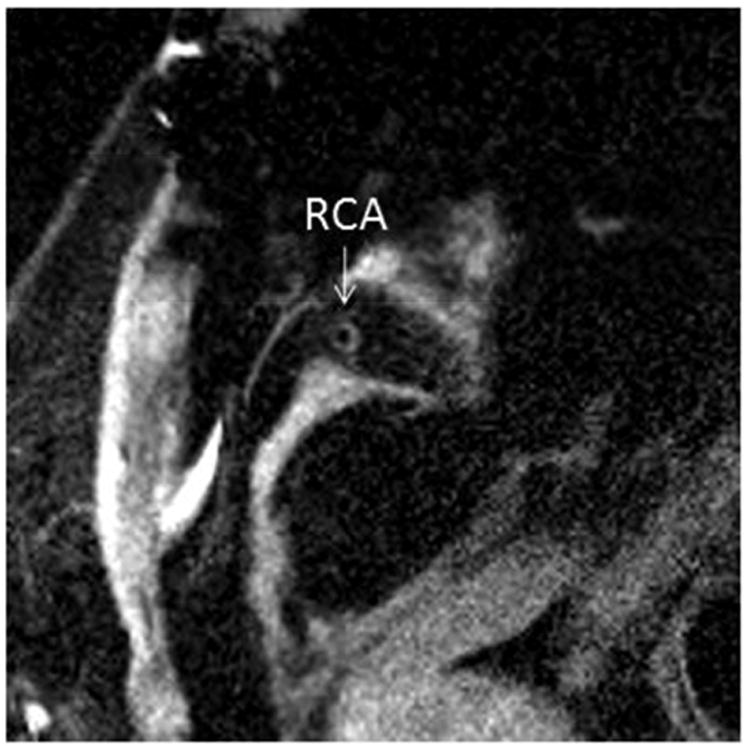
Figure 2.
A 74 year-old asymptomatic male. A lumen stenosis on the RCA could be identified by noncontrast MRA (confirmed by coronary angiogram)
Source of the figure: unpublished data of our group.
Imaging coronary dilation and flow using MRI
Coronary MRA may also be used to evaluate coronary dilation or stiffness (indicated by changes on lumen area). Terashima et al. studied 12 CAD patients and 20 healthy controls before and after the administration of vasodilator (sublingual nitroglycerin, NTG) 20. In 20 healthy adults and 17 patients with CAD, Hays et al. observe impaired coronary endothelial function associated with CAD (indicated by less cross-sectional coronary dilation after the administration of vasoactive medication) 21. Similar impaired endothelial function could also be found in CAD patients before and after isometric handgrip exercise, another endothelial-dependent stressor, by the same group 22. Using 3D coronary MRA pictures acquired at diastole and systole, Lin et al. calculated coronary dispensability index (CDI), an index of coronary stiffness, within cardiac cycles based on the differences of cross-sectional coronary lumen areas. The authors found that older type 2 diabetes mellitus (T2DM) patients without documented cardiovascular disease have lower CDIs in all coronary branches than healthy elderly 23. Figure 3 shows the measurement of coronary distensibility.
Figure 3.
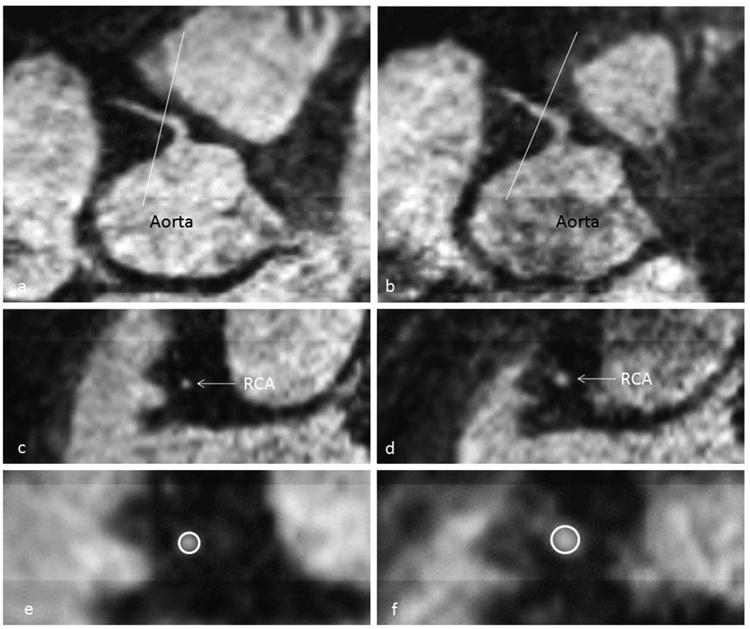
A 73 year-old healthy male. His peripheral blood pressure was 130/70 mmHg (PP= 60mmHg). (a) Longitudinal view of the RCA in mid-diastole (b) Longitudinal view of the RCA in end-systole. (c) Transverse view of lumen in mid-diastole (d) Transverse view of lumen in end-systole (e) Zoomed diastolic lumen with contour shows the area is 7.61mm2. (f) Zoomed systolic lumen with contour shows the area is 15.05 mm2. CDI= (15.05-7.61)/7.61/60×1000= 16.29 (mmHg-1)
Source of the figure: reference #23 from our group
Coronary flow is another important index for evaluating coronary atherosclerosis and endothelial function of the coronary wall. Altered blood flow usually accompanies luminal narrowing. Phase contrast (PC)-MRI is a traditional technique for quantifying 2D blood flow in the vessel. Shibata et al. demonstrate good agreement between MRI-derived coronary flow velocity reserve (calculated with flow difference before and after the administration of dipyridamole) and that measured using Doppler guide wire in 19 patients with heart disease (r = 0.91) 24. Insufficient coronary flow reserve (calculated on measurements before and after stress) was identified in diagnosed CAD patients (with flow-limiting luminal stenosis) as compared to healthy volunteers 21,22.
Imaging coronary wall using MRI
As a major manifestation of CAD, coronary remodeling involves the long-term, active modification of the vessel structure in response to pathological changes in its milieu, such as the development of atherosclerotic plaques. Because remodeled coronary wall (positive or negative) is the underlying source of myocardial ischemia, coronary remodeling becomes a reliable indicator of CAD and serves as a strong predictor of near-term coronary events 25. Coronary “culprit” plaque is the immediate source of cardiovascular events 25,26. Therefore, imaging of the coronary artery is of great clinical significance because it proves the existence of coronary plaques. The patterns of coronary remodeling have been found to be associated with clinical presentations of CAD. Currently, X-ray angiography is the standard clinical examination for the diagnosis of CAD. With X-ray angiography, Nahser et al. observed a reduction in coronary vasodilation and impaired regulation of coronary flow in T2DM patients 27. However, angiography shows only the coronary lumen, whereas CAD is a disease that originates in the vessel wall. Actually, many acute coronary events were triggered by superficial plaque erosion or rupture without obstructive lesions 28,29. Coronary artery plaques with positive remodeling (a nearly normal lumen gauge with compensatory vessel enlargement) have higher plaque vulnerability, indicated by a higher macrophage count and lipid content 30. That means a substantial burden of atherosclerosis can exist without producing stenosis 31. Those individuals with increasing cardiovascular risk may have low-grade narrowing in coronary arteries, which may be ignored by X-ray angiography. Existing studies have demonstrated the relationships between morphological changes of coronary plaques and risk of coronary events. Unfortunately, current clinical methods for coronary wall examination, such as IVUS, are limited by invasiveness. As a noninvasive imaging method, MRI may address this unmet clinical need by detecting risky coronary plaques without significant lumen stenosis. Over the past decade, MRI has emerged as a radiation-free, noninvasive method for the accurate detection of in situ atherosclerotic lesions on the coronary wall 32,33. (Box 2)
Box 2.
| MRI sequences used in the evaluation of coronary wall* | Need contrast agent? | |
|---|---|---|
| FSE (fast spin echo) | TSE (turbo spin echo) | No |
Names vary from different MRI scanner manufacturers
Botnar et al. acquired coronary wall images in 5 healthy volunteers and 5 CAD patients (confirmed by X-ray angiography). Fayad et al. also detected significant difference of maximal coronary wall thickness between subjects with and without CAD (4.38±0.71 mm vs. 0.75±0.17 mm) using 2-dimensional (2D) FSE sequence. In a cross-sectional study, Kim et al found that subjects with type 1 diabetes mellitus (T1DM) and diabetic nephropathy (DN) had a thicker coronary wall than those T1DM patients free of kidney involvements using a three-dimensional (3D) TSE sequence 34. Coronary wall MRI has also been adopted as a quantitative tool for cardiovascular risk estimation in epidemiological studies. In the Multi-Ethnic Study of Atherosclerosis (MESA) study, Miao et al. detected positive coronary remodeling, a predictor for future cardiovascular events, in asymptomatic older adults using MRI (n = 179) 35. Pericardial fat volume, an index of cardiovascular vulnerability, was also found to strongly relate to coronary plaque eccentricity (detected with MRI) in healthy older adults 36. Lin et al. demonstrated the differences of coronary wall thickness and stiffness between subjects with primary hypertension (HTN) and healthy controls 37. Those results suggest that coronary wall features have the potential to serve as quantitative imaging biomarkers in evaluating cardiovascular risks. Figure 4 shows positive remodeling of the coronary wall in an asymptomatic subject with type 2 diabetes mellitus (T2DM).
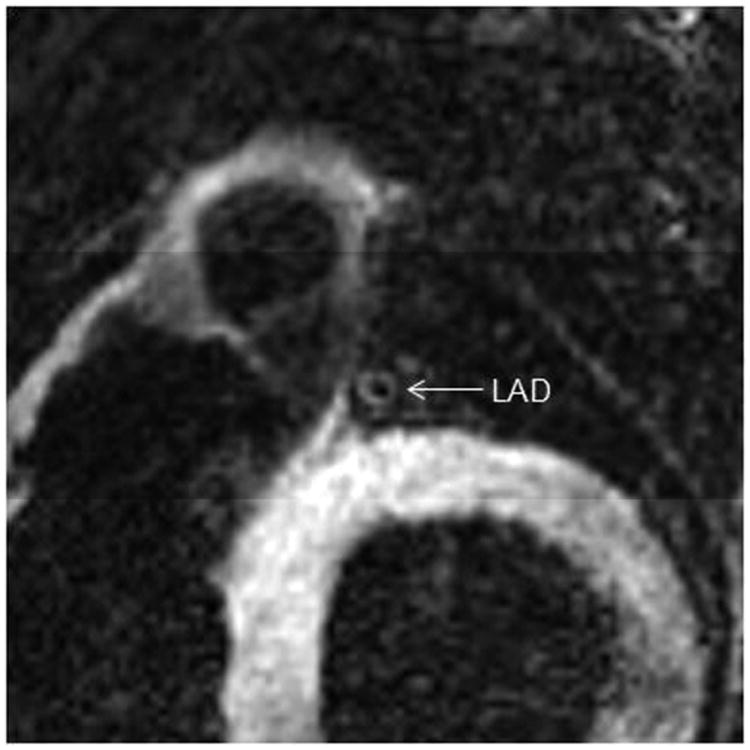
Figure 4.
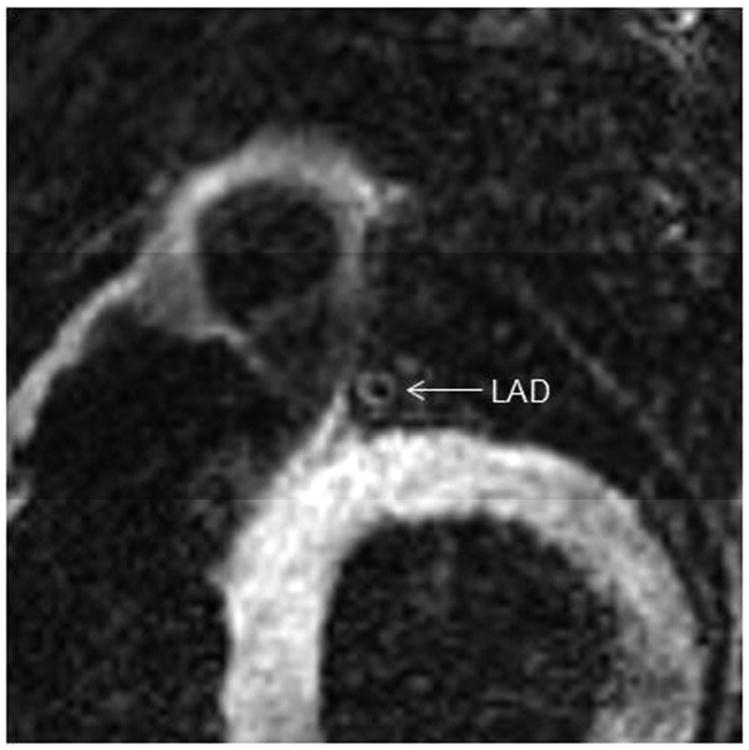
A 71 year-old asymptomatic female with a history of T2DM for 10 years. An eccentrically remodeled coronary segment on the LAD (without significant lumen stenosis) could be identified by MRI.
Source of the figure: unpublished data of our group.
Application and limitations of MRI/MRA for CAD management in clinical practice
Currently, coronary MRI/MRA has not been widely accepted as a regular examination in clinical practice. Many factors may affect image quality of coronary arteries, which may compromise clinical diagnosis. Such a situation is due to several technical limitations of this technique. At the same time, many novel technical innovations have been developed to solve those problems. (Box 3)
Box 3.
| Major challenges for current coronary MRI/MRA techniques | Possible solutions |
|---|---|
| Long scan time | Developing fast imaging techniques |
| Low spatial resolution and SNR | Using high magnetic field and administrating of contrast agents |
| Adverse physiological conditions, such as fast heart rate and irregular breath-modes | Developing novel imaging techniques, suppressing adverse patho-physiological conditions |
When an acute coronary syndrome (ACS) happens, “time is myocardium and time is outcome.”38 Therefore, MRI is not suitable for CAD diagnosis under acute situations due to long scan times. Although MRI can be a useful tool for screening subclinical CAD, MRI may need more time than other noninvasive imaging tools, such as coronary CTA, for the detection of CAD. In addition, a long scan may adversely affect image quality of coronary MRI/MRA due to unexpected motion artifacts and will potentially lower coronary MRI's clinical value. During the last few decades, many technical advances have been applied to shorten coronary MRI scan times. Parallel imaging takes advantages of spatial encoding from multiple parts of phase-array receive coils to shorten the MRI acquisition time 39. Huber at al. reported the implementation and evaluation of sensitivity-encoding (SENSE) free-breathing navigator-gated 3D coronary MRA at 3T. The authors found that SENSE could significantly reduce MRI scan time for the coronary tree in 11 healthy volunteers 40. However, there is usually a trade-off between short acquisition time and lower SNR (representing inferior visualization of coronary branches) 41. Using a 32-channel coil, Nehrke et al. acquired free-breathing whole-heart coronary MRA in 4 minutes with the use of SENSE and partial Fourier encoding for k-space acceleration 42. In a recent study, Akçakaya et al applied a novel B(1) -weighted compressed sensing (CS) technique in 3D whole-heart coronary MRA. With a CS-based acquisition and reconstruction strategy (low-dimensional-structure self-learning and thresholding [LOST]), the authors acquired high resolution coronary MRA in 7 healthy volunteers with a shorter acquisition time than that of the traditional SENSE technique 43.
Administration of contrast agents is a common way to improve image quality. Paetsch et al successfully use an intravascular contrast agent, B-22956, to significantly improve the image quality of 3D coronary MRA 44. Yu et al. performed contrast enhanced whole-heart coronary MRA (with SENSE) in 11 healthy volunteers. The authors found that a longer left anterior descending artery (LAD) could be depicted as compared with that presented by noncontrast coronary MRA 45. Many solutions could be applied to jointly improve the performance of coronary MRI/MRA.
Compared to imaging other solid organs, continues motion of the coronary tree in the 3D space is a specific challenge for coronary imaging. Heartbeat and breathing are major sources of coronary motion. In order to minimize the adverse effects of motion on coronary image quality, segmented acquisition schemes were designed to collect imaging data over multiple heartbeat and respiration cycles. Only the signal received within a highly selected “acquisition window” for minimal coronary motion will be accepted for filling k-space. An ideal “acquisition window” should be both “cardiac motion-free” (a “rest period of regional cardiac motion” chosen with ECG) and “respiratory freezing” (identified with 2D motion-adapted navigator [NAV] echo)” 46-48. Unfortunately, current motion correction/suppression strategies are still unable to eliminate the adverse effects of motion on cardiovascular MR scans completely. Severe cardiac motion, associated with faster heart rates and shortened “rest periods” in cardiac cycles, has already been proven to be a prominent determinant of poor image quality in coronary wall MRI 49. Beta-blockers can significantly lower heart rate and increased rest duration in cardiac cycle 50. SSFP is a fast MR imaging pulse sequence (4). With identical spatial resolution and gross imaging time as that used for TSE (FSE), SSFP can therefore acquire data in a shorter time window in a single cardiac cycle. Such a physical characteristic can be particularly utilized in cardiac imaging which is affected by severe cardiac motion. Using a black-blood SSFP sequence, Lin et al. significantly increased image quality of coronary wall under conditions of fast heart rate (> 80 beats/minute) in healthy subjects 51. Compared with traditional TSE(FSE) sequences for coronary wall imaging, SSFP also had better performance in directly observing the coronary wall for the detection of potential cardiac allograft vasculopathy (CAV) in heart transplant (HTx) recipients who usually have extremely fast heart rates due to denervation of “foreign” hearts 52. Figure 5 shows a coronary wall image in an HTx recipient.
Figure 5.
a 61-year-old female, who had a HTx 7 years ago. Her heart rate is 108 beats/minute. We can clearly see the RCA using black-blood SSFP MRI technique.
Source of the figure: reference #52 from our group.
Limited by the length and stability of breath-holding, breath-hold MRI is not suitable for all coronary examinations. Free-breathing coronary MRI/MRA has become the preferred choice in most large-scale clinical/epidemiological studies for guiding cardiovascular prevention, such as the MESA study 35. However, changes of breathing patterns (indicated by changes of the location of diaphram during the scan) may significantly affect image quality 46,48,53. Irregular breathing modes may widely exist in healthy populations. Older subjects were more likely to have inconsistent breathing modes 54. Advanced Respiratory Motion Compensation has been used to suppress such adverse effects due to motion 55. Using 3D-NAV and 3D affine correction, Henningsson et al. demonstrated 100% scan efficiency in performing high-resolution whole-heart 3D coronary MRA with high image quality in a recent study 56. Pang et al. developed a whole-heart coronary MRA technique using motion-corrected sensitivity encoding with 3D projection reconstruction 57. Such a sequence can be used to image the whole coronary tree in 5 minutes with good image quality despite the adverse effects of respiratory motion. In addition, some adjuncts, such as abdominal belts, have been applied to stabilize respiratory motion during coronary MRI/MRA. Ishida et al. used an dedicated abdominal belt to regulate respiratory motion during coronary scans and therefore resulted in a higher scan efficiency, shorten scan time and better image quality 14,58,59.
Future directions
Since coronary MRI/MRA may provide a cluster of quantitative measurements to evaluate the progression of coronary atherosclerosis, it will become more and more important in cardiovascular disease diagnosis and management. In addition, CAD may also be considered as a secondary target-organ involvement of nephrology, endocrinology and rheumatology disorders, including chronic kidney disease (CKD), T2DM and systemic lupus erythematosus (SLE) 60-62. A noninvasive, standardized approach to measure subclinical CAD and related cardiac changes from multiple aspects is important for guiding CAD management and improving patient survival by measuring individual responses to comprehensive target-organ protection. In a recent study, Pang et al. developed a self-gated 4D whole-heart imaging technique to detect coronary anatomy and cardiac function simultaneously 63. However, although coronary MRI/MRI has been developed for CAD estimation for more than 10 years, many technical and physiological conditions still significantly affect its performance in clinical practice. Further work is needed to optimize the technique and extend its clinical application for patient care.
Key points.
MRI is a useful noninvasive tool for the detection of coronary stenosis.
MRI can detect morphological and functional changes of remodeled coronary artery.
Many technical advances have been adopted to improve the performance of coronary MRI/MRA for cardiovascular risk estimation.
Footnotes
Conflict of interest: Nothing to disclosure
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wingard DL, Barrett-Connor EL, Scheidt-Nave C, McPhillips JB. Prevalence of cardiovascular and renal complications in older adults with normal or impaired glucose tolerance or NIDDM. A population-based study. Diabetes Care. 1993 Jul;16(7):1022–1025. doi: 10.2337/diacare.16.7.1022. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Benjamin IJ, Burke GL, et al. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1999 Sep 7;100(10):1134–1146. doi: 10.1161/01.cir.100.10.1134. [DOI] [PubMed] [Google Scholar]
- 3.Worthley SG, Helft G, Fuster V, et al. Noninvasive in vivo magnetic resonance imaging of experimental coronary artery lesions in a porcine model. Circulation. 2000 Jun 27;101(25):2956–2961. doi: 10.1161/01.cir.101.25.2956. [DOI] [PubMed] [Google Scholar]
- 4.Fayad ZA, Nahar T, Fallon JT, et al. In vivo magnetic resonance evaluation of atherosclerotic plaques in the human thoracic aorta: a comparison with transesophageal echocardiography. Circulation. 2000 May 30;101(21):2503–2509. doi: 10.1161/01.cir.101.21.2503. [DOI] [PubMed] [Google Scholar]
- 5.Ishida M, Sakuma H. Magnetic resonance of coronary arteries: assessment of luminal narrowing and blood flow in the coronary arteries. Journal of thoracic imaging. 2014 May;29(3):155–162. doi: 10.1097/RTI.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 6.Regenfus M, Ropers D, Achenbach S, et al. Noninvasive detection of coronary artery stenosis using contrast-enhanced three-dimensional breath-hold magnetic resonance coronary angiography. Journal of the American College of Cardiology. 2000 Jul;36(1):44–50. doi: 10.1016/s0735-1097(00)00672-0. [DOI] [PubMed] [Google Scholar]
- 7.Lin K, Lloyd-Jones DM, Spottiswoode B, et al. T1 contrast in the myocardium and blood pool: a quantitative assessment of gadopentetate dimeglumine and gadofosveset trisodium at 1.5 and 3 T. Investigative radiology. 2014 Apr;49(4):243–248. doi: 10.1097/RLI.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 8.Bi X, Carr JC, Li D. Whole-heart coronary magnetic resonance angiography at 3 Tesla in 5 minutes with slow infusion of Gd-BOPTA, a high-relaxivity clinical contrast agent. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2007 Jul;58(1):1–7. doi: 10.1002/mrm.21224. [DOI] [PubMed] [Google Scholar]
- 9.Yang Q, Li K, Liu X, et al. Contrast-enhanced whole-heart coronary magnetic resonance angiography at 3.0-T: a comparative study with X-ray angiography in a single center. Journal of the American College of Cardiology. 2009 Jun 30;54(1):69–76. doi: 10.1016/j.jacc.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Q, Li K, Liu X, et al. 3.0T whole-heart coronary magnetic resonance angiography performed with 32-channel cardiac coils: a single-center experience. Circulation Cardiovascular imaging. 2012 Sep 1;5(5):573–579. doi: 10.1161/CIRCIMAGING.112.974972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Notaro LA, Usman MH, Burke JF, Siddiqui A, Superdock KR, Ezekowitz MD. Secondary prevention in concurrent coronary artery, cerebrovascular, and chronic kidney disease: focus on pharmacological therapy. Cardiovascular therapeutics. 2009 Fall;27(3):199–215. doi: 10.1111/j.1755-5922.2009.00087.x. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy RM, Shea SM, Deshpande VS, et al. Coronary MR angiography: true FISP imaging improved by prolonging breath holds with preoxygenation in healthy volunteers. Radiology. 2003 Apr;227(1):283–288. doi: 10.1148/radiol.2271011415. [DOI] [PubMed] [Google Scholar]
- 13.Spuentrup E, Katoh M, Buecker A, et al. Free-breathing 3D steady-state free precession coronary MR angiography with radial k-space sampling: comparison with cartesian k-space sampling and cartesian gradient-echo coronary MR angiography--pilot study. Radiology. 2004 May;231(2):581–586. doi: 10.1148/radiol.2312030451. [DOI] [PubMed] [Google Scholar]
- 14.Kato S, Kitagawa K, Ishida N, et al. Assessment of coronary artery disease using magnetic resonance coronary angiography: a national multicenter trial. Journal of the American College of Cardiology. 2010 Sep 14;56(12):983–991. doi: 10.1016/j.jacc.2010.01.071. [DOI] [PubMed] [Google Scholar]
- 15.Yonezawa M, Nagata M, Kitagawa K, et al. Quantitative analysis of 1.5-T whole-heart coronary MR angiograms obtained with 32-channel cardiac coils: a comparison with conventional quantitative coronary angiography. Radiology. 2014 May;271(2):356–364. doi: 10.1148/radiol.13122491. [DOI] [PubMed] [Google Scholar]
- 16.Kim WY, Danias PG, Stuber M, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. The New England journal of medicine. 2001 Dec 27;345(26):1863–1869. doi: 10.1056/NEJMoa010866. [DOI] [PubMed] [Google Scholar]
- 17.Stuber M, Botnar RM, Danias PG, et al. Double-oblique free-breathing high resolution three-dimensional coronary magnetic resonance angiography. Journal of the American College of Cardiology. 1999 Aug;34(2):524–531. doi: 10.1016/s0735-1097(99)00223-5. [DOI] [PubMed] [Google Scholar]
- 18.Liu X, Zhao X, Huang J, et al. Comparison of 3D free-breathing coronary MR angiography and 64-MDCT angiography for detection of coronary stenosis in patients with high calcium scores. AJR American journal of roentgenology. 2007 Dec;189(6):1326–1332. doi: 10.2214/AJR.07.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoon YE, Kitagawa K, Kato S, et al. Prognostic value of coronary magnetic resonance angiography for prediction of cardiac events in patients with suspected coronary artery disease. Journal of the American College of Cardiology. 2012 Dec 4;60(22):2316–2322. doi: 10.1016/j.jacc.2012.07.060. [DOI] [PubMed] [Google Scholar]
- 20.Terashima M, Meyer CH, Keeffe BG, et al. Noninvasive assessment of coronary vasodilation using magnetic resonance angiography. Journal of the American College of Cardiology. 2005 Jan 4;45(1):104–110. doi: 10.1016/j.jacc.2004.09.057. [DOI] [PubMed] [Google Scholar]
- 21.Hays AG, Hirsch GA, Kelle S, Gerstenblith G, Weiss RG, Stuber M. Noninvasive visualization of coronary artery endothelial function in healthy subjects and in patients with coronary artery disease. Journal of the American College of Cardiology. 2010 Nov 9;56(20):1657–1665. doi: 10.1016/j.jacc.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 22.Hays AG, Kelle S, Hirsch GA, et al. Regional coronary endothelial function is closely related to local early coronary atherosclerosis in patients with mild coronary artery disease: pilot study. Circulation Cardiovascular imaging. 2012 May 1;5(3):341–348. doi: 10.1161/CIRCIMAGING.111.969691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin K, Lloyd-Jones DM, Liu Y, Bi X, Li D, Carr JC. Noninvasive evaluation of coronary distensibility in older adults: a feasibility study with MR angiography. Radiology. 2011 Dec;261(3):771–778. doi: 10.1148/radiol.11110573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shibata M, Sakuma H, Isaka N, Takeda K, Higgins CB, Nakano T. Assessment of coronary flow reserve with fast cine phase contrast magnetic resonance imaging: comparison with measurement by Doppler guide wire. Journal of magnetic resonance imaging : JMRI. 1999 Oct;10(4):563–568. doi: 10.1002/(sici)1522-2586(199910)10:4<563::aid-jmri9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 25.Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000 May;20(5):1262–1275. doi: 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]
- 26.Waxman S, Ishibashi F, Muller JE. Detection and treatment of vulnerable plaques and vulnerable patients: novel approaches to prevention of coronary events. Circulation. 2006 Nov 28;114(22):2390–2411. doi: 10.1161/CIRCULATIONAHA.105.540013. [DOI] [PubMed] [Google Scholar]
- 27.Nahser PJ, Jr, Brown RE, Oskarsson H, Winniford MD, Rossen JD. Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. Circulation. 1995 Feb 1;91(3):635–640. doi: 10.1161/01.cir.91.3.635. [DOI] [PubMed] [Google Scholar]
- 28.Burke AP, Farb A, Malcom GT, Liang YH, Smialek J, Virmani R. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. The New England journal of medicine. 1997 May 1;336(18):1276–1282. doi: 10.1056/NEJM199705013361802. [DOI] [PubMed] [Google Scholar]
- 29.Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation. 1995 Aug 1;92(3):657–671. doi: 10.1161/01.cir.92.3.657. [DOI] [PubMed] [Google Scholar]
- 30.Varnava AM, Mills PG, Davies MJ. Relationship between coronary artery remodeling and plaque vulnerability. Circulation. 2002 Feb 26;105(8):939–943. doi: 10.1161/hc0802.104327. [DOI] [PubMed] [Google Scholar]
- 31.Arnett EN, Isner JM, Redwood DR, et al. Coronary artery narrowing in coronary heart disease: comparison of cineangiographic and necropsy findings. Annals of internal medicine. 1979 Sep;91(3):350–356. doi: 10.7326/0003-4819-91-3-350. [DOI] [PubMed] [Google Scholar]
- 32.Nagata M, Kato S, Kitagawa K, et al. Diagnostic accuracy of 1.5-T unenhanced whole-heart coronary MR angiography performed with 32-channel cardiac coils: initial single-center experience. Radiology. 2011 May;259(2):384–392. doi: 10.1148/radiol.11101323. [DOI] [PubMed] [Google Scholar]
- 33.He Y, Zhang Z, Dai Q, et al. Accuracy of MRI to identify the coronary artery plaque: a comparative study with intravascular ultrasound. J Magn Reson Imaging. 2012 Jan;35(1):72–78. doi: 10.1002/jmri.22652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim WY, Astrup AS, Stuber M, et al. Subclinical coronary and aortic atherosclerosis detected by magnetic resonance imaging in type 1 diabetes with and without diabetic nephropathy. Circulation. 2007 Jan 16;115(2):228–235. doi: 10.1161/CIRCULATIONAHA.106.633339. [DOI] [PubMed] [Google Scholar]
- 35.Miao C, Chen S, Macedo R, et al. Positive remodeling of the coronary arteries detected by magnetic resonance imaging in an asymptomatic population: MESA (Multi-Ethnic Study of Atherosclerosis) Journal of the American College of Cardiology. 2009 May 5;53(18):1708–1715. doi: 10.1016/j.jacc.2008.12.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miao C, Chen S, Ding J, et al. The association of pericardial fat with coronary artery plaque index at MR imaging: The Multi-Ethnic Study of Atherosclerosis (MESA) Radiology. 2011 Oct;261(1):109–115. doi: 10.1148/radiol.11110346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lin K, Lloyd-Jones DM, Liu Y, Bi X, Li D, Carr JC. Potential quantitative magnetic resonance imaging biomarkers of coronary remodeling in older hypertensive patients. Arteriosclerosis, thrombosis, and vascular biology. 2012 Jul;32(7):1742–1747. doi: 10.1161/ATVBAHA.112.245266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gibson CM. Time is myocardium and time is outcomes. Circulation. 2001 Nov 27;104(22):2632–2634. [PubMed] [Google Scholar]
- 39.Sodickson DK, McKenzie CA. A generalized approach to parallel magnetic resonance imaging. Medical physics. 2001 Aug;28(8):1629–1643. doi: 10.1118/1.1386778. [DOI] [PubMed] [Google Scholar]
- 40.Huber ME, Kozerke S, Pruessmann KP, Smink J, Boesiger P. Sensitivity-encoded coronary MRA at 3T. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2004 Aug;52(2):221–227. doi: 10.1002/mrm.20062. [DOI] [PubMed] [Google Scholar]
- 41.Bluemke DA, Achenbach S, Budoff M, et al. Noninvasive coronary artery imaging: magnetic resonance angiography and multidetector computed tomography angiography: a scientific statement from the american heart association committee on cardiovascular imaging and intervention of the council on cardiovascular radiology and intervention, and the councils on clinical cardiology and cardiovascular disease in the young. Circulation. 2008 Jul 29;118(5):586–606. doi: 10.1161/CIRCULATIONAHA.108.189695. [DOI] [PubMed] [Google Scholar]
- 42.Nehrke K, Bornert P, Mazurkewitz P, Winkelmann R, Grasslin I. Free-breathing whole-heart coronary MR angiography on a clinical scanner in four minutes. Journal of magnetic resonance imaging : JMRI. 2006 May;23(5):752–756. doi: 10.1002/jmri.20559. [DOI] [PubMed] [Google Scholar]
- 43.Nam S, Hong SN, Akcakaya M, et al. Compressed sensing reconstruction for undersampled breath-hold radial cine imaging with auxiliary free-breathing data. Journal of magnetic resonance imaging : JMRI. 2014 Jan;39(1):179–188. doi: 10.1002/jmri.24098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paetsch I, Huber ME, Bornstedt A, et al. Improved three-dimensional free-breathing coronary magnetic resonance angiography using gadocoletic acid (B-22956) for intravascular contrast enhancement. Journal of magnetic resonance imaging : JMRI. 2004 Aug;20(2):288–293. doi: 10.1002/jmri.20099. [DOI] [PubMed] [Google Scholar]
- 45.Yu J, Paetsch I, Schnackenburg B, et al. Use of 2D sensitivity encoding for slow-infusion contrast-enhanced isotropic 3-T whole-heart coronary MR angiography. AJR American journal of roentgenology. 2011 Aug;197(2):374–382. doi: 10.2214/AJR.10.5724. [DOI] [PubMed] [Google Scholar]
- 46.Lin K, Lloyd-Jones DM, Bi X, Liu Y, Li D, Carr JC. Effects of respiratory motion on coronary wall MR imaging: a quantitative study of older adults. The international journal of cardiovascular imaging. 2013 Jun;29(5):1069–1076. doi: 10.1007/s10554-013-0187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taylor AM, Jhooti P, Firmin DN, Pennell DJ. Automated monitoring of diaphragm end-expiratory position for real-time navigator echo MR coronary angiography. J Magn Reson Imaging. 1999 Mar;9(3):395–401. doi: 10.1002/(sici)1522-2586(199903)9:3<395::aid-jmri6>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 48.Taylor AM, Jhooti P, Wiesmann F, Keegan J, Firmin DN, Pennell DJ. MR navigator-echo monitoring of temporal changes in diaphragm position: implications for MR coronary angiography. Journal of magnetic resonance imaging : JMRI. 1997 Jul-Aug;7(4):629–636. doi: 10.1002/jmri.1880070404. [DOI] [PubMed] [Google Scholar]
- 49.Malayeri AA, Macedo R, Li D, et al. Coronary vessel wall evaluation by magnetic resonance imaging in the multi-ethnic study of atherosclerosis: determinants of image quality. J Comput Assist Tomogr. 2009 Jan-Feb;33(1):1–7. doi: 10.1097/RCT.0b013e3181648606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jahnke C, Paetsch I, Achenbach S, et al. Coronary MR imaging: breath-hold capability and patterns, coronary artery rest periods, and beta-blocker use. Radiology. 2006 Apr;239(1):71–78. doi: 10.1148/radiol.2383042019. [DOI] [PubMed] [Google Scholar]
- 51.Lin K, Bi X, Taimen K, et al. Coronary wall MR imaging in patients with rapid heart rates: a feasibility study of black-blood steady-state free precession (SSFP) The international journal of cardiovascular imaging. 2012 Mar;28(3):567–575. doi: 10.1007/s10554-011-9852-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lin K, Bi X, Liu Y, et al. Black-blood steady-state free precession (SSFP) coronary wall MRI for cardiac allografts: a feasibility study. Journal of magnetic resonance imaging : JMRI. 2012 May;35(5):1210–1215. doi: 10.1002/jmri.23543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Danias PG, Stuber M, Botnar RM, Kissinger KV, Edelman RR, Manning WJ. Relationship between motion of coronary arteries and diaphragm during free breathing: lessons from real-time MR imaging. AJR American journal of roentgenology. 1999 Apr;172(4):1061–1065. doi: 10.2214/ajr.172.4.10587147. [DOI] [PubMed] [Google Scholar]
- 54.Tobin MJ, Chadha TS, Jenouri G, Birch SJ, Gazeroglu HB, Sackner MA. Breathing patterns. 1. Normal subjects. Chest. 1983 Aug;84(2):202–205. doi: 10.1378/chest.84.2.202. [DOI] [PubMed] [Google Scholar]
- 55.Henningsson M, Botnar RM. Advanced respiratory motion compensation for coronary MR angiography. Sensors. 2013;13(6):6882–6899. doi: 10.3390/s130606882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Henningsson M, Prieto C, Chiribiri A, Vaillant G, Razavi R, Botnar RM. Whole-heart coronary MRA with 3D affine motion correction using 3D image-based navigation. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2014 Jan;71(1):173–181. doi: 10.1002/mrm.24652. [DOI] [PubMed] [Google Scholar]
- 57.Pang J, Sharif B, Arsanjani R, et al. Accelerated whole-heart coronary MRA using motion-corrected sensitivity encoding with three-dimensional projection reconstruction. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2014 Jan 16; doi: 10.1002/mrm.25097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ishida M, Schuster A, Takase S, et al. Impact of an abdominal belt on breathing patterns and scan efficiency in whole-heart coronary magnetic resonance angiography: comparison between the UK and Japan. J Cardiovasc Magn Reson. 2011;13:71. doi: 10.1186/1532-429X-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McConnell MV, Khasgiwala VC, Savord BJ, et al. Comparison of respiratory suppression methods and navigator locations for MR coronary angiography. AJR Am J Roentgenol. 1997 May;168(5):1369–1375. doi: 10.2214/ajr.168.5.9129447. [DOI] [PubMed] [Google Scholar]
- 60.Lin K, Lloyd-Jones DM, Li D, Carr JC. Quantitative imaging biomarkers for the evaluation of cardiovascular complications in type 2 diabetes mellitus. Journal of diabetes and its complications. 2014 Mar-Apr;28(2):234–242. doi: 10.1016/j.jdiacomp.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 61.Briasoulis A, Bakris GL. Chronic kidney disease as a coronary artery disease risk equivalent. Current cardiology reports. 2013 Mar;15(3):340. doi: 10.1007/s11886-012-0340-4. [DOI] [PubMed] [Google Scholar]
- 62.Roman MJ, Shanker BA, Davis A, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. The New England journal of medicine. 2003 Dec 18;349(25):2399–2406. doi: 10.1056/NEJMoa035471. [DOI] [PubMed] [Google Scholar]
- 63.Pang J, Sharif B, Fan Z, et al. ECG and navigator-free four-dimensional whole-heart coronary MRA for simultaneous visualization of cardiac anatomy and function. Magnetic resonance in medicine : official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2014 Sep 12; doi: 10.1002/mrm.25450. [DOI] [PMC free article] [PubMed] [Google Scholar]


