Abstract
The objective of this study was to describe the services, referral and reporting practices, and barriers to utilization of driver rehabilitation programs (DRPs) for older drivers. Identified through two national association databases, 204 driver rehabilitation programs completed an online survey. DRP availability varies, with a median of one program per 64,151 older adults (range: 1,006–676,981). The median cost for a complete evaluation was $400; 36% of DRPs reported no third-party reimbursement. Participants thought barriers to DRP use include cost/reimbursement, lack of program awareness, and issues with evaluator training. Models for insurance reimbursement, and increased awareness of program benefits by healthcare providers and older drivers, are needed.
Keywords: driving evaluation, older driver, driving rehabilitation
INTRODUCTION
Occupational therapists, especially those with Certified Driving Rehabilitation Specialist (CDRS) credentials, have been recognized as ideal providers to assess older adults’ driving abilities (Dickerson & Schold Davis, 2012; Stav et al., 2006; Stephens et al., 2005). Comprehensive driving evaluations include a behind-the-wheel (BTW) component and are considered the most accurate assessment of driving ability (Kay et al., 2008; Kay et al., 2012; Odenheimer et al., 1994; Wheatley & Di Stefano, 2008). Driving rehabilitation programs (DRPs), which are often are staffed by occupational therapists as CDRSs and offer BTW tests, are valuable for evaluating skills and for providing retraining (Stephens et al., 2005; Stutts & Wilkins, 2003).
With the growing population of older drivers – estimated at 35 million in 2011 (NHTSA, 2013)—has come acknowledgment of the need to balance older driver safety and mobility-related independence. To optimize efficiency and cost-effectiveness of older driver assessment, many have recommended the development of “tiered assessment programs” with initial screening in primary care or other medical settings followed by referral of screen-positive drivers to a DRP program for further evaluation (Eby et al., 2009; Eby & Molnar, 2010; Eby & Molnar, 2008; Langford et al., 2008).
There appears to be general support for the concept of DRPs and tiered older driver assessment programs by both older drivers and providers (Kua et al., 2007; Stephens et al., 2005; Stutts & Wilkins, 2003), but there has been slow progress in establishing tiered programs in practice. One concern has been an inadequate supply of trained driving specialists to match the growing number of older drivers (Dickerson, 2013; Korner-Bitensky et al., 2010; Stav et al., 2006). To address this need, some have suggested partnerships with driving schools (Stutts & Wilkins, 2003), which typically perform shorter and less in-depth evaluations than DRPs staffed by occupational therapists. The American Occupational Therapy Association (AOTA) has also partnered with the National Highway Traffic Safety Administration (NHTSA) to encourage general occupational therapists to take on a role in older driver assessments through the Gaps and Pathways project (Schold Davis & Dickerson, 2012; Schold Davis, 2014).
However, there may be other obstacles to development of tiered older driver assessment programs, including cost, logistical considerations (e.g., DRP location), or inadequate driver or healthcare provider knowledge about DRPs. To date, there have been studies describing the types of tools and assessments used by DRPs (Dickerson, 2013; Korner-Bitensky et al., 2006; Yuen et al., 2012) and the degree to which occupational therapy programs including training about driving evaluations (Yuen & Bunk, 2011). Less is known about the general availability of DRPs in the United States, including possible barriers to utilization, as prior studies have focused on older driver retraining programs (Korner-Bitensky et al., 2010; Kua et al., 2007) or on DRPs in a single state (Yanochko, 2005). There is also limited published information concerning referral and reporting practices, beyond that many programs have a large proportion of drivers referred by physicians (Dickerson, 2013; Korner-Bitensky et al., 2006; Stutts & Wilkins, 2003).
In order to improve older drivers’ access to and utilization of DRPs, it is critical to understand the current distribution of programs and to identify barriers. We therefore sought to describe currently available driver evaluation programs (DRPs) in terms of: (1) basic services offered; (2) integration with healthcare system (e.g., referral and reporting practices); and (3) potential barriers to utilization. This information will fill a key knowledge gap and thereby inform future efforts to enhance older driver safety and mobility.
METHOD
Design and Participants
This cross-sectional survey examined the current practices of DRPs in the United States. Eligible DRPs were programs that currently conduct evaluations of older (age 65 years and older) drivers and that are registered in the publicly-available online databases of the American Occupational Therapy Association (AOTA, 2013) or the Association for Driver Rehabilitation Specialists (ADED, 2013). Participation was at the program level, rather than the individual evaluator level, with only one eligible response per program. Each program was invited to complete a confidential on-line survey via email invitation, with the option to opt out of participation. In the case that the databases listed multiple contacts for a single program, initial invitations were sent to the first-listed contact. If that contact did not respond, then new invitations were sent to the subsequent listed contacts until the program either responded or opted out. Programs that did not respond or opt-out by email were contacted by telephone and invited to complete the survey either online or by telephone.
This project was reviewed and deemed exempt by the [blinded] Institutional Review Board.
Questionnaire
The survey was developed by a team of experts after review of the existing literature and consideration of important issues relevant to access of and utilization of DRPs. The survey was reviewed by five experienced researchers with edits made as indicated. Questions covered three primary areas: (1) program characteristics; (2) referral and reporting practices; and (3) perceptions of DRP programs. Program characteristics included location, number of evaluations per month, program staffing, and type and cost of services. Questions about referral and reporting practices asked about how drivers are referred to the program and who receives a written report or recommendations after the evaluation. The final group of questions assessed respondents’ perceptions of DRP programs, including possible barriers to evaluations and needed actions at the national level to improve older driver safety. For these questions concerning perceptions, participants could choose one or more responses from a list of choices but also had the option to submit additional comments.
Survey responses were entered directly by participants into a secure, web-based application (Harris et al., 2009) and data were then exported to Stata for analyses.
Primary Outcomes and Analyses
We described responses using proportions for categorical variables or medians for continuous variables. For medians, we reported interquartile ranges (IQRs) rather than standard deviations because the responses were not normally distributed. We calculated the number of DRPs by state populations of older adults using data from the United States 2010 Census (Howden & Meyer, 2011). We also used qualitative techniques for thematic analysis of the responses participants provided to the open-ended comment space at the end of the survey.
RESULTS
From the AOTA and ADED online databases we identified 379 unique potentially-eligible DRPs, and we contacted each one via email or telephone. Of these, 48 (13%) were ineligible because at the time of the study they did not offer senior driver evaluations. Of the remaining 331 potentially eligible programs, 204 (62%) completed the survey.
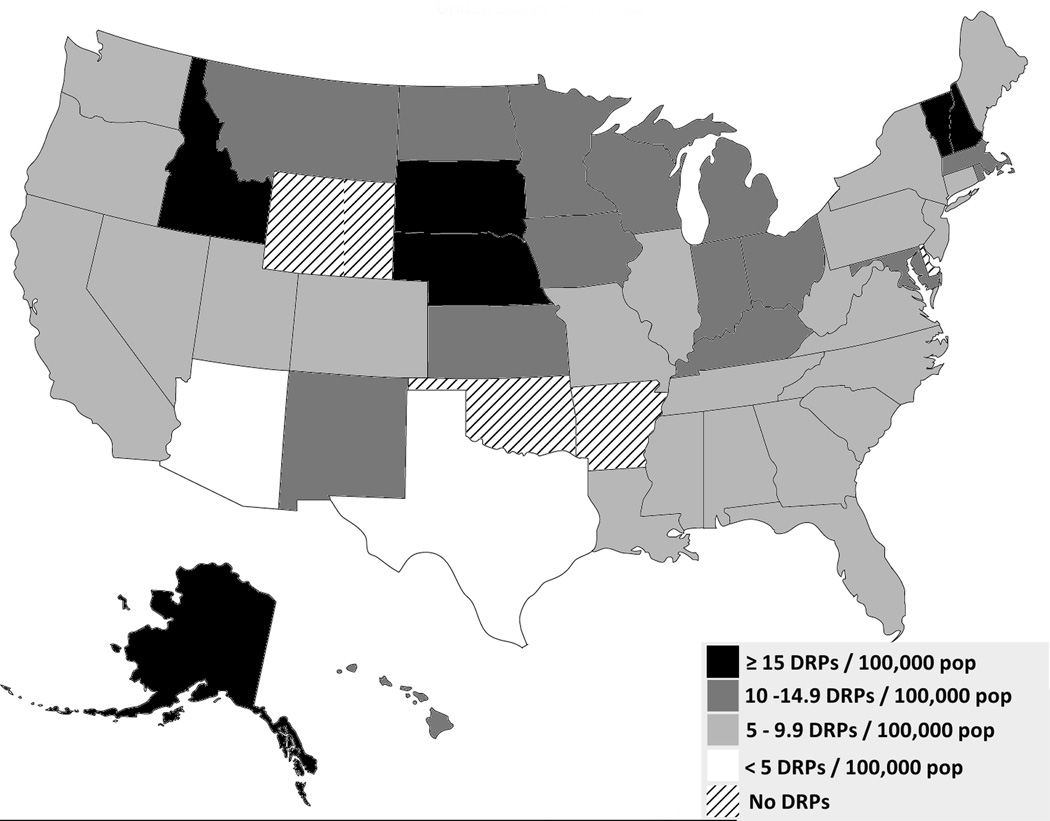
The 331 potentially eligible programs were distributed across the country, with a median of 9.4 DRPs per 100,000 older adults (Figure 1a). Viewed another way, this translates to a median of 64,151 older adults per DRP (Figure 1b), with a range of from 1,006 older adults per DRP in Alaska to over 676,981 older adults per DRP in Texas. At the time of the study, four states (Arkansas, Delaware, Oklahoma and Wyoming) had no eligible programs registered in the AOTA or ADED databases.
Figure 1. Number of DRPs per 100,000 older adults.
DRPs are programs listed in the AOTA and ADED online databases that currently provide older driver evaluations (n=331). Population estimates are from the 2010 Census (U.S. Census Bureau, 2010).
Responding programs estimated evaluating a median of 8 (IQR: 4–13.5) older drivers in the past 30 days. Almost all programs (197, 96.6%) offered clinical evaluations and most (168, 82.4%) offered in-vehicle evaluations. Smaller proportions offered retraining or simulator services (Table 1). Programs employed a median of 1.0 full-time-equivalent driving evaluators, and 13% of programs were trying to hire at least one evaluator.
Table 1.
Characteristics of Responding DRPs (N=204)
| Characteristic | N (%) |
|---|---|
| Region of the United States | |
| West | 43 (21.1) |
| Midwest | 57 (27.9) |
| Northeast | 47 (23.0) |
| South | 57 (27.9) |
| Approximate number of older drivers evaluated in past 30 days (Median, IQR) | 8.0 (4.0–13.5) |
| Services offered* | |
| Clinical evaluation (office-based testing) | 197 (96.6) |
| Clinical re-training | 113 (55.4) |
| In-vehicle evaluation | 168 (82.4) |
| In-vehicle re-training | 153 (75.0) |
| Driving simulator evaluation | 41 (20.1) |
| Driving simulator re-training | 26 (12.7) |
| Other (including education and adaptive equipment) | 25 (12.3) |
| Number driving evaluators employed (Median, IQR) | 2.0 (1.0–2.0) |
| Full-time equivalents of driving evaluators employed (Median, IQR) | 1.0 (0.5–2.0) |
| Percent employed as full-time as driving evaluators (Median) | 66.70% |
| Percent occupational therapists (Median) | 100.00% |
| Percent Certified Driving Rehabilitation Specialists (Median) | 60.00% |
| Percent Certified Driving Instructors (Median) | 2.10% |
| Currently trying to hire ≥1 driving evaluator | 26 (12.9) |
| Approximate time for a complete driver evaluation | |
| 30 minutes to 1 hour | 3 (1.5) |
| 1–2 hours | 42 (20.9) |
| 2–3 hours | 101 (50.3) |
| 3–4 hours | 50 (24.9) |
| >4 hours | 5 (2.5) |
| Approximate cost for a complete driver evaluation (Median, IQR) | $399.50 ($297.50–$477.50) |
| Cost covered at least in-part by insurance* | 124 (63.9) |
| Workman’s compensation | 103 (83.1) |
| Vocational rehabilitation | 83 (66.9) |
| Health insurance | 35 (28.2) |
| Automobile insurance | 13 (10.5) |
| Other (including military benefits and foundations) | 22 (17.7) |
| Unknown | 3 (2.4) |
| Method of patient referral* | |
| From a physician or other healthcare provider | 201 (98.5) |
| Self-referral by patients or family members | 128 (62.8) |
| From the department of motor vehicles state licensing agency | 77 (37.8) |
| From the police | 13 (6.4) |
| Soonest a patient could be seen after calling for an appointment | |
| < 1 week (including date of call) | 32 (15.8) |
| 1–2 weeks | 88 (43.6) |
| 2–3 weeks | 37 (18.3) |
| 3–4 weeks | 27 (13.4) |
| >4 weeks | 16 (7.9) |
| Unsure | 2 (1.0) |
| Recipient of written report/recommendations after evaluation* | |
| The referring physician or healthcare provider | 192 (94.1) |
| The driver him/herself | 123 (60.3) |
| The department of motor vehicles/licensing agency | 56 (27.5) |
| The driver’s primary care provider | 47 (23.0) |
| The police | 1 (0.5) |
| No one/Unsure | 0 (0.0) |
DRP, Driver rehabilitation program; IQR, interquartile range
Multiple responses allowed
Half (50.3%) of responding programs said a complete driver evaluation requires 2–3 hours, and the median reported cost for a complete evaluation was $399.50 (IQR: $297.50–$477.50). Median cost was highest in the Western United States ($449.00) and lowest in the South ($378.00), but these regional differences were not statistically significant. Almost two thirds of programs (124, 63.9%) said that the cost of a driver evaluation could be covered at least in-part by some form of insurance. However, in the majority of cases this was workman’s compensation (83.1%) or vocational rehabilitation (66.9%), while coverage by health insurance (28.2%) or automobile insurance (10.5%) was less common (Table 1).
Programs were asked about their typical referral and reporting methods, with the option for multiple responses. The most common referral source was a physician or other healthcare provider (98.5%), followed by self-referral by drivers or their family members (62.8%; Table 1). Just over half of responding programs (58.8%) could schedule an evaluation appointment within 2 weeks. In terms of reporting practices, most programs provided a written report to the referring physician or healthcare provider (94.1%), with fewer (23.0%) reporting to primary care provider (Table 1).
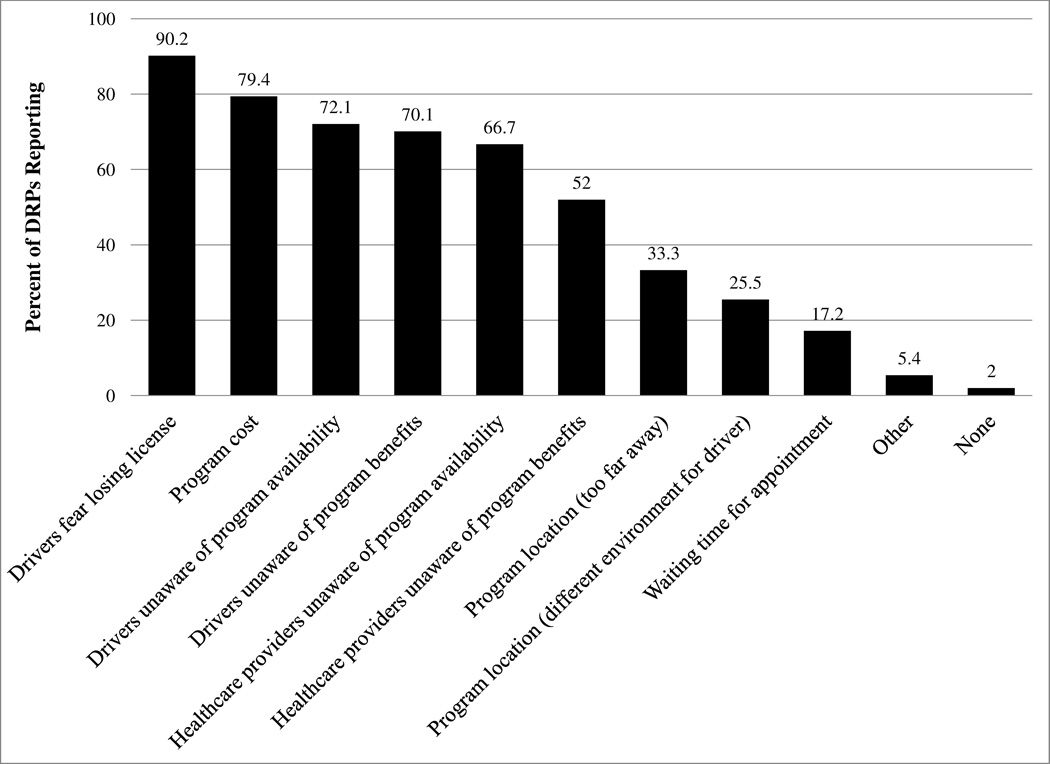
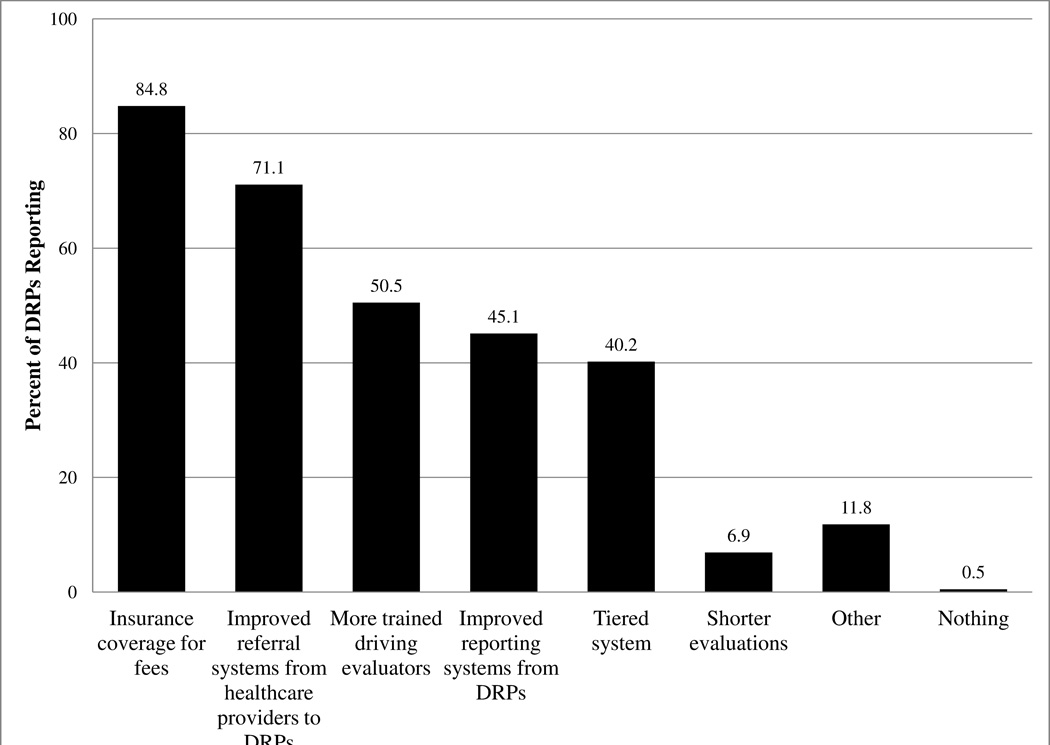
Participants were also asked to provide their opinions concerning current barriers to providing older driver evaluation. The most commonly identified barrier was driver fear over license revocation, followed by program cost (Figure 2). Lack of awareness by both drivers and healthcare providers concerning program availability and benefits were also identified as a key barrier. Regarding needs at the national level to improve older driver safety, 84.8% of responding programs identified insurance coverage for program fees, followed by improved referral systems from healthcare providers (71.1%; Figure 3). Half (50.5%) thought more trained evaluators were needed, but only 6.9% thought the evaluations themselves needed to be shortened.
Figure 2. Perceived barriers to older driver use of DRPs (N=204).
DRP, Driver rehabilitation program; Multiple responses allowed.
Figure 3. Perceived needs, at national level, to address older driver safety issues (N=204).
DRP, Driver rehabilitation program; Multiple responses allowed.
The survey ended with space for participants to leave comments, and 58 participants (28.4%) responded with a total of eight pages of text. Three dominant themes arose from the responses: cost and reimbursement; communication and awareness of program; and training issues. Concerning program cost, many participants commented on the tension in providing a professional service with appropriate compensation while trying to make the program affordable for older adults. As one participant wrote: “Although 3rd party reimbursement would most likely encourage more older adults to take advantage of the service, I understand often the reimbursement rate is significantly lower than the self-pay rate.” Others commented: “I could not operate on the fees that third party payers could cover,” and “The liability insurance and costs compared to the income generated prohibits many facilities from offering this program.” One participant pointed out that while clients were typically happy with the service provided, “Trying to communicate value associated with cost ahead of time is a challenge.”
Communication was also recognized as contributing to a general lack of awareness about the benefits of driving evaluations. One participant wrote, “Doctors’ reluctance to refer can sometime be a hindrance. Awareness of such evaluation programs is minimal. National awareness programs to educate the general public would be beneficial.” Another suggested a need to reframe the issue: “We need to find away to make it fashionable or remove the stigma seniors have somehow associated with a driving evaluation.”
Many participants also commented on barriers to obtaining and maintaining CDRS certification, which may be necessary for reimbursement through vocational rehabilitation or other programs. One wrote: “I am personally fearful of not having enough trained professionals to keep this programming alive for occupational therapists. … I estimate I may have spent close to $10,000 to achieve the necessary education to practice in a driving rehab program. Some people just cannot make that investment. Many employers who at one time did invest in a person for their driving rehab program, have decided to close the program rather than invest that amount of money into an individual.” Another noted specific concerns of providers in rural areas: “The issue of being certified as a Rehab Drivers Safety Specialist is frustrating. Living in a rural county, we haven't the client referrals for a full time program. As a result we are excluded from sitting for the exam.”
DISCUSSION
In this national survey of DRPs, we identified several barriers to program utilization by older drivers, filling a gap in the current literature with implications for future policy and development of tiered assessment programs. DRP program costs are a major concern. The respondents describe significant investment in training and certification process for driving evaluators which slows program development and expansion. Older drivers may not be able or willing to pay professional evaluators at a rate commensurate with the services provided, and third party reimbursement is inadequate. Another barrier is awareness of the benefits offered by these programs, which may result in lower rates of referral by healthcare providers. Although waiting times for appointments were identified in this survey as generally less than two weeks, program availability varies greatly across states, which supports continued national efforts to match drivers to the level of resources needed. Opposing these barriers, however, is the clear dedication of driving evaluators to the issue of older driver safety, as noted by our high response rate and number of passionate comments from participants.
The cost of a driving evaluation, including appropriate compensation and insurance reimbursement, was identified as a major issue related to older driver assessment. The median cost of a complete driver evaluation among responding programs was approximately $400, and 36% of programs reported that costs were not covered by any kind of third-party payer. This cost may not be unreasonable, given the specialized and advanced skills offered by trained DRP evaluators. The issue may be one of awareness and understanding that a comprehensive driving evaluation is a complex evaluation of an instrumental task of daily living by a highly trained professional health care provider, not simply a test of learned driving skills. However, for many older adults, a high cost may be prohibitive; in other work, we have found that older adults were willing to pay only $10–35 for a one-hour BTW evaluation (blinded-A; blinded-B).
In the current study, cost was the second most cited barrier to program utilization, and the need for insurance coverage was the most commonly cited need at a national level to address older driver safety. However, program representatives also brought up concerns over adequate reimbursement for the services provided, including that some programs have faced closure because of high liability and training costs in the face of declining payments. Thus shorter or less-expensive evaluations alone, such as the BTW tests offered by driving schools for approximately $88 (Stutts & Wilkins, 2003) may not be the solution, especially for those older adults with complex medical issues or cognitive impairment. Determining fitness to drive is a critical issue for older adults because of the emotional and practical implications with driving cessation. However, since effects of medical conditions do impact functional abilities, including those needed to drive (e.g., slower processing speed), a thorough evaluation is needed. Therefore, it is essential to have a clear understanding of medical conditions so that observed deficits can be evaluated as to evaluate whether rehabilitation and/or adaptive compensation is possible in order to avoid driving cessation. Those types of evaluations require skilled health care providers such as occupational therapists (Dickerson et al., 2007; Dickerson & Schold Davis, 2012; Eby et al., 2009). New models are needed to meet the growing demand of an aging population (Dickerson, 2013). Future research and policy efforts should focus on determining the most cost-effective approach to older driver screening and assessment (Dickerson, 2013), as well as on developing feasible models for driving evaluation reimbursement through automobile or health insurance.
Another barrier to effective DRP utilization is inadequate awareness of program availability and benefits. Study participants identified this as an issue for healthcare providers—who are the dominant source of referrals— older drivers and the general public. Other studies support this lack of awareness by physicians (Brooks et al., 2011; Drickamer & Marottoli, 1993), and the “Physician’s Guide to Assessing and Counseling Older Drivers” from NHTSA and the American Medical Association includes a section on DRPs to encourage physician utilization of this resource (Carr et al., 2010). Participants in our study cited the need for an improved collaboration and a referral system from healthcare providers to DRPs, which is in line with prior work (Dickerson, 2013). In a tiered system, screening could be performed in general medical settings, with subsequent referral of screen-positive older drivers to a DRP for further evaluation (Stephens et al., 2005). Such an approach could prioritize DRP resources for those most at risk or most likely to benefit (Eby et al., 2009; Eby & Molnar, 2010; Eby & Molnar, 2008; Langford et al., 2008). A pilot tiered program in California, with both screening and evaluation tiers within the Department of Motor Vehicle (DMV), appeared to have restrictive effects on participants’ mobility without significantly reducing future crash risks (Camp, 2013). However, there is great diversity among state DMVs and, to date, there have not been prospective studies of tiered systems within healthcare settings (including DRPs), so further research is needed.
An interesting finding in our study was the wide state variability in number of DRPs compared to the population of older adults. However, these state-level figures do not take into account further geographic disparities, and rural areas are likely especially underserved. Currently there are an estimated 600 driver rehabilitation specialists in the United States, of whom the majority (approximately 80%) are occupational therapists (Dickerson, 2014). There is clearly a need for generalist occupational therapists to become involved in evaluating driving, with the recognition that driving is a fundamental instrumental activity of daily living (Dickerson, 2014; Dickerson et al., 2011). The current Gaps and Pathways Project of the AOTA and NHTSA aims to improve and standardize referral pathways, education, documentation and terminology (Dickerson, 2014), and hopefully these efforts will help expand adequate availability of appropriate driving evaluation services throughout the United States.
Limitations of our study include reliance on the AOTA and ADED databases for program sampling, as these databases may not capture all DRPs. Response bias may be an issue, as participants may have been more interested or supportive of older driver issues compared to nonparticipants. The survey relied on self-report, so the estimates of costs, employees and appointment waiting times may not be accurate. Finally, although participation was at the program level, responses to certain questions (e.g., about program barriers) reflect the opinions of the program representative completing the survey and may not be generalizable to the driver evaluation community as a whole.
CONCLUSIONS
Driving evaluation program availability varies widely across the United States, and the typical cost of most programs—though appropriate for these professional services—may be a barrier for many older drivers without coverage by third-party payers. Additional barriers to program growth and utilization include awareness of program availability and benefits, as well as the stringent and costly requirements for certification. Tiered systems, including ones using occupational therapists in general practice, may be reasonable strategies to pursue. Future research and policy efforts should focus on models for DRP sustainability and reimbursement, increasing healthcare provider and general public awareness of DRPs, and ensuring access to appropriate services across the urban-rural spectrum.
Acknowledgments
Funders: This work was supported by: the Paul Beeson Career Development Award Program (The National Institute on Aging, AFAR, The John A. Hartford Foundation, and The Atlantic Philanthropies; K23AG043123-Betz); Colorado Clinical & Translational Sciences Institute with the Development and Informatics Service Center (NIH/NCRR Colorado CTSI Grant Number UL1 RR025780). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies. No sponsor had any direct involvement in study design, methods, subject recruitment, data collection, analysis, or manuscript preparation.
REFERENCES
- Occupational Therapy Association, Inc. Find a Driving Specialist (AOTA) 2013 Available online at: http://myaota.aota.org/driver_search/index.aspx. [Google Scholar]
- Association for Driver Rehabilitation Specialists (ADED) ADED Member Directory. 2013 Available online at: http://www.driver-ed.org/custom/directory/ [Google Scholar]
- Blinded-A. Recruitment of older drivers from primary care clinics for on-road fitness-to-drive testing: Results of a pilot study. doi: 10.1111/jgs.12913. (Under review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinded-B. “It’s in how you present the question:” Perspectives on screening older drivers in primary care settings. (Under review). [Google Scholar]
- Brooks JO, Dickerson A, Crisler MC, Logan WC, Beeco RW, Witte JC. Physician knowledge, assessment, and reporting of older driver fitness. Occupational Therapy in Health Care. 2011;25(4):213–224. doi: 10.3109/07380577.2011.607227. [DOI] [PubMed] [Google Scholar]
- Camp BJ. The overall program effects of California's 3-Tier Assessment System pilot on crashes and mobility among senior drivers. Journal of Safety Research. 2013;47:1–8. doi: 10.1016/j.jsr.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Carr DB, Schwartzberg JG, Manning L, Sempek J. Physician's Guide to Assessing and Counseling Older Drivers. 2nd Edition. Washington, DC: National Highway Traffic Safety Administration and American Medical Association; 2010. [Google Scholar]
- Dickerson AE. Driving Assessment Tools Used by Driver Rehabilitation Specialists: Survey of Use and Implications for Practice. American Journal of Occupational Therapy. 2013;67(5):564–573. doi: 10.5014/ajot.2013.007823. [DOI] [PubMed] [Google Scholar]
- Dickerson AE. Driving with Dementia: Evaluation, Referral, and Resources. Occupational Therapy in Health Care. 2014;28(1):62–76. doi: 10.3109/07380577.2013.867091. [DOI] [PubMed] [Google Scholar]
- Dickerson AE, Molnar LJ, Eby DW, Adler G, Bedard M, Berg-Weger M, et al. Transportation and aging: a research agenda for advancing safe mobility. Gerontologist. 2007;47(5):578–590. doi: 10.1093/geront/47.5.578. [DOI] [PubMed] [Google Scholar]
- Dickerson AE, Reistetter T, Davis ES, Monahan M. Evaluating Driving as a Valued Instrumental Activity of Daily Living. American Journal of Occupational Therapy. 2011;65(1):64–75. doi: 10.5014/ajot.2011.09052. [DOI] [PubMed] [Google Scholar]
- Dickerson AE, Schold Davis E. Welcome to the Team! Who are the Stakeholders? In: Maguire M, Schold Davis E, editors. Driving and Community Mobility: Occupational Therapy Strategies Across the Lifespan. Bethesda, MD: AOTA Publishing; 2012. pp. 49–77. [Google Scholar]
- Drickamer MA, Marottoli RA. Physician Responsibility in Driver Assessment. American Journal of the Medical Sciences. 1993;306(5):277–281. doi: 10.1097/00000441-199311000-00001. [DOI] [PubMed] [Google Scholar]
- Eby DW, Molnar LJ. Driving fitness and cognitive impairment: issues for physicians. Journal of the American Medical Association. 2010;303(16):1642–1643. doi: 10.1001/jama.2010.495. [DOI] [PubMed] [Google Scholar]
- Eby DW, Molnar LJ, editors. Proceedings of the North American License Policies Workshop. Washington, DC: AAA Foundation for Traffic Safety; 2008. [Google Scholar]
- Eby DW, Molnar LJ, Kartje PS. Maintaining Safe Mobility in an Aging Society. Boca Raton, FL: Taylor & Francis Group, LLC; 2009. [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden LM, Meyer JA. Age and Sex Composition: 2010. (2010 Census Briefs) U.S. Census Bureau; 2011. [Google Scholar]
- Kay LG, Bundy AC, Clemson L, Cheal B, Glendenning T. Contribution of off-road tests to predicting on-road performance: A critical review of tests. Australian Occupational Therapy Journal. 2012;59(1):89–97. doi: 10.1111/j.1440-1630.2011.00989.x. [DOI] [PubMed] [Google Scholar]
- Kay L, Bundy AC, Clemson L, Jolly N. Validity and reliability of the on-road driving assessment with senior drivers. Accident Analysis and Prevention. 2008;40(2):751–759. doi: 10.1016/j.aap.2007.09.012. [DOI] [PubMed] [Google Scholar]
- Korner-Bitensky N, Bitensky J, Sofer S, Man-Son-Hing M, Gelinas I. Driving evaluation practices of clinicians working in the United States and Canada. American Journal of Occupational Therapy. 2006;60(4):428–434. doi: 10.5014/ajot.60.4.428. [DOI] [PubMed] [Google Scholar]
- Korner-Bitensky N, Menon A, von Zweck C, Van Benthem K. A national survey of older driver refresher programs: Practice readiness for a rapidly growing need. Physical and Occupational Therapy in Geriatrics. 2010;28(3):205–214. [Google Scholar]
- Kua A, Korner-Bitensky N, Desrosiers J. Older individuals’ perceptions regarding driving: Focus group findings. Physical and Occupational Therapy in Geriatrics. 2007;25(4):21–40. [Google Scholar]
- Langford J, Braitman K, Charlton J, Eberhard J, O'Neill D, Staplin L, et al. TRB Workshop 2007: Licensing authorities' options for managing older driver safety--practical advice from the researchers. Traffic Injury Prevention. 2008;9(4):278–281. doi: 10.1080/15389580801895210. [DOI] [PubMed] [Google Scholar]
- Marshall SC, Man-Son-Hing M, Bedard M, Charlton J, Gagnon S, Gelinas I, et al. Protocol for Candrive II/Ozcandrive, a multicentre prospective older driver cohort study. Accident Analysis and Prevention. 2013;61:245–252. doi: 10.1016/j.aap.2013.02.009. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safey Administration (NHTSA), US Department of Transportation. Safey in Numbers: Older Drivers. 2013 Nov-Dec;1 [Google Scholar]
- Odenheimer GL, Beaudet M, Jette AM, Albert MS, Grande L, Minaker KL. Performance-based driving evaluation of the elderly driver: safety, reliability, and validity. Journal of Gerontology. 1994;49(4):153–159. doi: 10.1093/geronj/49.4.m153. [DOI] [PubMed] [Google Scholar]
- Schold Davis E, Dickerson AE. Meeting the driving and community mobility needs of OT Clients. OT Practice. 2012;17:9–19. [Google Scholar]
- Schold Davis E, Wagner E. The Gaps and Pathways Project: The vision, development, and implementation. Occupational Therapy in Health Care. 2014 In press. [Google Scholar]
- Stav WR, Justiss MD, Belchior P, Lanford DN. Clinical practice in driving rehabilitation. Topics in Geriatric Rehabilitation. 2006;22(2):153–161. [Google Scholar]
- Stephens BW, McCarthy DP, Marsiske M, Shechtman O, Classen S, Justiss M, et al. International Older Driver Consensus Conference on Assessment, Remediation and Counseling for Transportation Alternatives: Summary and Recommendations. Physical and Occupational Therapy in Geriatrics. 2005;23(2–3):103–121. doi: 10.1300/J148v23n02_07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stutts JC, Wilkins JW. On-road driving evaluations: a potential tool for helping older adults drive safely longer. Journal of Safety Research. 2003;34(4):431–439. doi: 10.1016/j.jsr.2003.09.014. [DOI] [PubMed] [Google Scholar]
- Wheatley CJ, Di Stefano M. Individualized assessment of driving fitness for older individuals with health, disability, and age-related concerns. Traffic Injury Prevention. 2008;9(4):320–327. doi: 10.1080/15389580801895269. [DOI] [PubMed] [Google Scholar]
- Yanochko P. Building a Network of Convenient, Affordable and Trustworthy Driving Assessment and Evaluation Programs: Reflections of California Occupational Therapists. 2005 [Google Scholar]
- Yuen HK, Brooks JO, Azuero A, Burik JK. Certified driver rehabilitation specialists' preferred situations for driving simulator scenarios. American Journal of Occupuational Therapy. 2012;66(1):110–114. doi: 10.5014/ajot.2012.001594. [DOI] [PubMed] [Google Scholar]
- Yuen HK, Bunk JK. Survey of Driving Evaluation and Rehabilitation Curricula in Occupational Therapy Programs. American Journal of Occupational Therapy. 2011;65(2):217–220. doi: 10.5014/ajot.2011.000810. [DOI] [PubMed] [Google Scholar]