Abstract
Objective
To conduct a randomized controlled trial to evaluate the preliminary efficacy of family-based interpersonal psychotherapy (FB-IPT) for treating depression in preadolescents (ages 7–12) as compared to child-centered therapy (CCT), a supportive and nondirective treatment that closely approximates the standard of care for pediatric depression in community mental health.
Method
Preadolescents with depression (N=42) were randomly assigned FB-IPT or CCT. Pre- and posttreatment assessments included clinician-administered measures of depression, parent- and child-reported depression and anxiety symptoms, and parent-child conflict and interpersonal impairment with peers.
Results
Preadolescents receiving FB-IPT had higher rates of remission (66.0% vs. 31%), a greater decrease in depressive symptoms from pre- to posttreatment, and lower depressive symptoms at posttreatment (R2=0.35, Δ R2 = 0.22; B= -8.15, SE= 2.61, t(37)= -3.13, p=0.002, F2=0.28) than did preadolescents with depression receiving CCT. Furthermore, preadolescents in the FB-IPT condition reported significant reductions in anxiety and interpersonal impairment than did preadolescents in the CCT condition. Changes in social and peer impairment from pre- to posttreatment were associated with preadolescents’ posttreatment depressive symptoms. There was a significant indirect effect for decreased social impairment accounting for the association between the FB-IPT and preadolescents’ posttreatment depressive symptoms.
Conclusion
Findings indicate FB-IPT is an effective treatment for preadolescent depression and support further investigation of interpersonal mechanisms by which FB-IPT may reduce preadolescent depression.
Clinical trial registration information
Phase II Study of Family Based Interpersonal Psychotherapy (FB-IPT) for Depressed Preadolescents; http://clinicaltrials.gov/show/NCT02054312; NCT02054312.
Keywords: depression, preadolescent, randomized controlled trial, IPT, treatment
Introduction
Depression in children increases markedly during the transition from childhood to adolescence, and elevated depressive symptoms in preadolescent youth (ages 7–12) are strong predictors of adolescent depression1. Although studies approximate that 0.4 to 2.5 percent of preadolescent children experience depression, they underestimate the number of preadolescents who do not meet full diagnostic criteria for major depressive disorder (MDD) but present for outpatient treatment with clinically significant depressive symptoms and functional impairment2. As such, preadolescents with depressive disorders may be under-diagnosed and go untreated.
Because preadolescent depression occurs during a sensitive period of pubertal, social, and neural development, it may disrupt socio-affective processes and increase preadolescents’ risk for recurring depression across adolescence and young adulthood3. Although longitudinal studies indicate that most children with depression recover within a 9-month period, the children remain at significant risk for having repeated and more severe episodes of depression within the subsequent 2-year period4. Longitudinal studies also reveal that compared to normal controls, preadolescents with depression continue to experience significantly more difficulties in interpersonal relationships with parents and peers after their symptoms remit5. Because symptom improvement does not always result in improved interpersonal functioning, residual impairment in preadolescents’ interpersonal functioning may be a pathway for depression recurrence.
Prevention-of-depression research on offspring of parents with depression identifies poor parent and peer relationships as risk factors for adolescent depression6. Parental depression is associated with parent-child conflict and less frequent positive interactions with children7. In prospective longitudinal studies of school-aged children, higher levels of family conflict predict higher levels of depressive symptoms over a 1-year follow-up period8. Because parental depression is related to poor interpersonal communication, preadolescents may model poor family communication and problem solving in other relationships, thereby increasing the likelihood of experiencing interpersonal stress and subsequent depression9. Peer stressors, such as peer exclusion and rejection, are also consistent predictors of depressive symptoms from middle childhood to early adolescence10; experiences of peer victimization in preadolescence are associated with suicidality and poor mental health outcomes in young adults11. Peer stress may intensify preadolescents’ depressive symptoms and increase social withdrawal. The high rates of comorbid anxiety disorders (up to 70% in clinically-referred youth)12 may further impair their ability to engage in social situations13. Positive parent-child relationships may buffer preadolescents from the stress of peer relationships, and in doing so, may decrease their risk for depression in adolescence14.
To date, no psychosocial intervention has been established as the superior treatment for preadolescents diagnosed with depression15. While there is well-established support for the efficacy of cognitive-behavioral therapy (CBT) relative to no-treatment control conditions in treating community samples of preadolescents with elevated depressive symptoms15, no differences have been found in the few studies of preadolescents with depression randomized to CBT or relaxation training16 or to supportive, non-directed therapy17. Two CBT treatment protocols, Taking ACTION18 and Primary and Secondary Control Enhancement Training (PASCET)19, have demonstrated promise in effectively treating children with elevated depressive symptoms as compared to waitlist control groups, but have not been compared to active treatments. However, a recent efficacy trial found no differences between PASCET and supportive therapy in reducing depressive symptoms in preadolescents with irritable bowel disorder20.
A primary limitation of existing CBT models may be the lack of parental involvement in treating children with depression. Because they are embedded in a family context, parental involvement in treatment for preadolescent depression is a critical developmental concern21. Multi-family psychoeducation therapy (MF-PEP) has been found to be an effective augmentation strategy to treatment as usual in children between the ages of 8 and 12 with a diagnosed depressive or bipolar disorder as compared to treatment as usual alone22. In addition, small, uncontrolled treatment development trials involving a family-focused CBT intervention (N = 9)23 and a contextual emotion regulation therapy for conjoint parent-child delivery (N = 20)24 have demonstrated promise in reducing depressive symptoms but have not examined parent-child conflict and social impairment, pathways that may sustain poor interpersonal functioning in preadolescents with depression.
To date, there are very few controlled treatment studies for preadolescent depression, and a clear need exists for treatments that actively involve parents and address interpersonal impairment in these preadolescents. Interpersonal psychotherapy for depressed adolescents (IPT-A)25 is an effective, time-limited, psychosocial treatment for depression in adolescents that focuses on the relationship between interpersonal stressors and depressive symptoms and aims to decrease depressive symptoms by improving adolescents’ interpersonal functioning26,27. Treatment is structured around 1 of 4 “problem areas” temporally associated with the onset of depressive symptoms (loss, role disputes, role transitions, and interpersonal deficits). Family- based interpersonal psychotherapy (FB-IPT) is an adaptation of IPT-A that actively involves parents in weekly sessions and directly addresses parent-child conflict and interpersonal impairment, two domains that may contribute to preadolescents’ depression. In an open-treatment trial28, Dietz et al. demonstrated the feasibility and acceptability of FB-IPT with high rates of treatment compliance and significant reductions in depressive and anxiety symptoms in preadolescents from pre- to posttreatment.
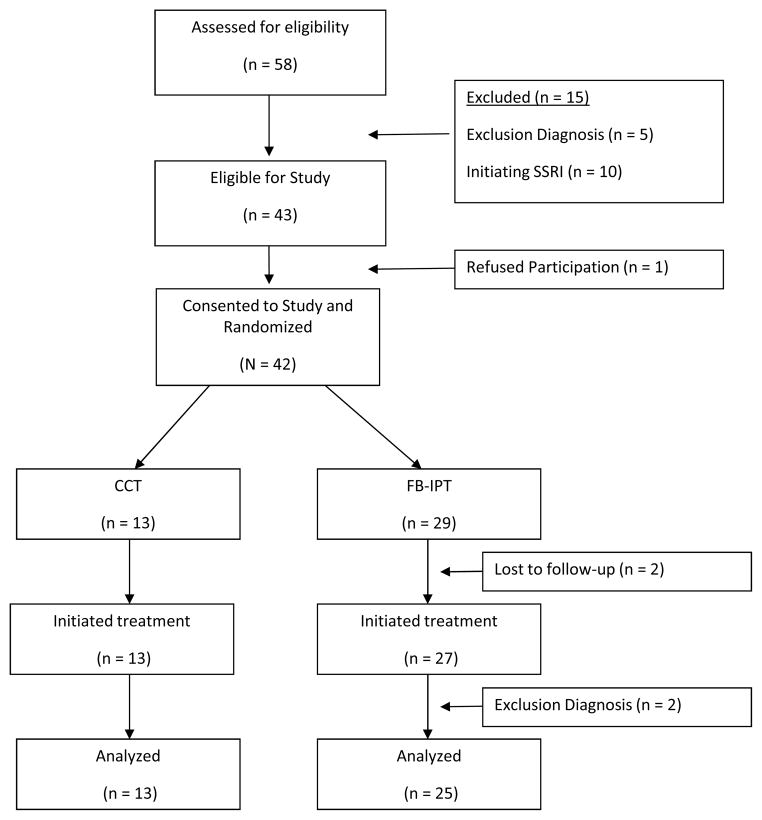
The current study examined the efficacy of FB-IPT in a sample of 42 treatment-seeking preadolescents (ages 7–12) who met DSM-IV criteria for a depressive disorder. Preadolescents with depression were randomized to FB-IPT or child-centered therapy (CCT), a supportive and nondirective treatment that closely approximates the standard of care for pediatric depression in community mental health29. We hypothesized preadolescents receiving FB-IPT would evidence higher rates of remission, endorse fewer depressive symptoms at posttreatment, and demonstrate a greater reduction in depressive symptoms from pre- to posttreatment than those receiving CCT. We also hypothesized parent-child conflict, anxiety, and interpersonal impairment would significantly decrease in the FB-IPT condition compared to CCT (see Figure 1, path A), and that decreases in these domains would be correlated with lower posttreatment depression severity scores (Figure 1, path B). Lastly, we hypothesized that changes in parent-child conflict, anxiety, and interpersonal impairment with peers would have significant indirect effects on the association between FB-IPT and preadolescents’ posttreatment depression scores, as compared to CCT (Figure 1, path C).
Figure 1.
An illustration of planned analyses for hypotheses testing. Note: CCT = child-centered therapy; CDRS = Children’s Depression Rating Scaled; FB-IPT = family-based interpersonal psychotherapy. a Each treatment condition is represented by a dummy-coded variable: FB-IPT=1, CCT=0. b Path A represents the association between treatment condition and changes in hypothesized mediators, parent-child conflict, anxiety, social impairment, and peer impairment. c Parent-child conflict, indexed by the Conflict Behavior Questionnaire, Child and Parent Report (CBQ-C/P), anxiety, as indexed by the Self-Report for Childhood Anxiety Related Emotional Disorders, Child and Parent Versions (SCARED-C/P), and social impairment and peer impairment, as indexed by subscales on the Social Adjustment Scale – Self-Report (SAS-SR), were assessed before and after treatment. d Path B represents the association between changes in hypothesized mediators, parent-child conflict, anxiety, social impairment, and peer impairment on posttreatment depression severity as indexed by the CDRS-Revised (R). e Path C’ (the apostrophe denotes an indirect path) represents the indirect effects of treatment condition on posttreatment CDRS-R scores through changes in hypothesized mediators, parent-child conflict, anxiety, social impairment, and peer impairment.
Method
Sample and Recruitment
Children presenting for a psychiatric assessment at a specialty clinic for youth depression were eligible for this study if they were 1) between 7 and 12 years old, 2) diagnosed with a current depressive disorder (MDD, dysthymia, depressive disorder not otherwise specified [NOS]), and 3) provided informed consent to be contacted about ongoing research. All diagnoses were made by masters-level clinicians and attending psychiatrists employed by the outpatient clinic as part of their routine assessment of youth with depression; none of these clinicians were affiliated with this study. Preadolescents with diagnoses of bipolar disorder, pervasive developmental disorder (PDD), posttraumatic stress disorder, and obsessive-compulsive disorder were excluded from participation. Preadolescents on a stable dose of selective serotonin reuptake inhibitor (SSRI) medication for at least 2 months were included in the study, providing they met diagnostic criteria and would remain on the same stable dose of SSRI (n=2). Preadolescents with comorbid attention-deficit/hyperactivity disorder (ADHD) were included in this study, providing they met diagnostic criteria and were on a stable dose of stimulant medication for at least 1 month (n=12). This study was approved by the institutional review board of the University of Pittsburgh School of Medicine.
Procedure
A 2:1 randomization strategy was used to maximize the number of preadolescents treated with FB-IPT, and sex, minority status, and comorbid anxiety disorders were stratified across treatment conditions. All preadolescents received up to 14 sessions of outpatient psychotherapy. Pretreatment diagnoses and pretreatment scores on the Children’s Depression Rating Scale, Revised (CDRS-R) were obtained from data collected during preadolescents’ psychiatric assessment. The majority of posttreatment CDRS-R interviews were conducted by a trained independent evaluator (IE) who was blind to treatment condition (60%; ICC>0.70); however, study therapists administered and coded posttreatment CDRS-R interviews to 40% of participants. There were no significant differences in posttreatment CDRS-R scores obtained from the IE and clinicians, nor was there a significant treatment condition x rater (1=IE, 0=study therapist) association with posttreatment CDRS-R scores. Preadolescents and their parents were asked to complete pre- and posttreatment measures of depressive symptoms, parent-child conflict, anxiety, and interpersonal impairment.
Treatment Conditions
Treatment was delivered by three clinicians, two of whom are authors (L.J.D. and R.B.W.), all with advanced degrees in clinical psychology and training in empirically supported psychotherapies for youths with depression.
Family-Based Interpersonal Psychotherapy (FB-IPT)
FB-IPT included the preadolescent and one parent in a 14-session treatment, although it was not uncommon for 2 parents or the preadolescent’s second parent to attend at least 1 treatment session. Treatment was divided into 3 phases (initial, middle, and termination).
Initial Phase (sessions 1–5)
Therapists met individually with the preadolescent (25 minutes) and then met with the parent (25 minutes). In meetings with preadolescents, therapists linked changes in preadolescents’ depressive symptoms to negative experiences in family and peer relationships and guided preadolescents in constructing the Closeness Circle, an interactive mapping of preadolescents’ relationships, and the Interpersonal Inventory. Parent meetings focused on psychoeducation about depression, ways to help preadolescents maintain routines and reasonable expectations for their performance, and parenting strategies for responding to preadolescents with depression (“Parenting Tips”).
Middle Phase (sessions 6–10)
Therapists met individually with the preadolescent (25 minutes) and then with the parent-child dyad (25 minutes). In meetings with preadolescents, therapists introduced and role-played communication skills relevant to the identified problem area. During dyadic sessions, preadolescents and parents role-played communication skills and/or engaged in problem solving as facilitated by therapists to help parent-child dyads negotiate solutions. Dyadic sessions also focused on increasing preadolescents’ positive experiences with peers. Preadolescents were coached to initiate social experiences with peers, and rehearsed communication skills for approaching peers with both therapists and parents. Parents engaged in problem solving with preadolescents regarding how to increase opportunities for peer interaction; with preadolescents’ approval, parents were enlisted to help initiate social activities with peers.
Termination Phase (sessions 11–14)
Therapists met individually with preadolescents (35 minutes) and then with the dyad (25 minutes) to consolidate skills, discuss maintenance strategies, and establish a plan for depression recurrence.
Child-Centered Therapy (CCT)
CCT is based on a Rogerian model of treatment, whereby changes in children’s mood and behavior are initiated through their experience of a therapeutic relationship marked by unconditional positive regard, empathic understanding, and therapeutic genuineness. Specific techniques included listening and attending skills, and demonstrating acceptance through reflection, clarification, paraphrasing, and summarizing statements. CCT therapists also used nondirective problem solving, helping children to consider alternative responses to a problem without making specific recommendations or offering solutions. Although parents did not participate in sessions, they were invited to join the first 10 minutes of each session to check in about their preadolescents’ symptoms. CCT has been successfully employed as a manualized comparison treatment in efficacy studies of youth depression20,30.
Treatment Fidelity
Each therapy session was reviewed in hour-by-hour supervision with the primary investigator (L.J.D) to ensure that session content was covered and to monitor for any clinical concerns for all participants receiving FB-IPT or CCT. In addition, therapy sessions were audiotaped, and 20% of each therapist’s sessions were scored by two of three authors (L.J.D., R.B.W) using ratings of treatment fidelity to FB-IPT or CCT. Fidelity to FB-IPT was determined by how therapists structured sessions, made connections between interpersonal events and changes in preadolescents’ mood, and adhered to content/tasks specific for that phase of treatment. Fidelity to CCT was indicated by demonstrating active listening, asking open-ended questions, and communicating positive regard and support. Global ratings of fidelity to both FB-IPT and CCT were calculated on a 5-point Likert-like scale, with scores ≥ 3 indicating “satisfactory” treatment fidelity. Ninety-five percent (95%) of audiotaped sessions were rated as at least “satisfactory” on FB-IPT and CCT checklists of treatment fidelity.
Outcome Measures
Depressive Symptoms
Depressive symptoms in children were measured by the CDRS-R31. This scale integrates information from multiple sources (parent, child, clinical observations) and has demonstrated high internal consistency (α=0.85) and good test-retest reliability (r=0.92), in addition to being sensitive to treatment effects in psychotherapy research. Posttreatment CDRS-R scores ≤ 28 were used to create a dichotomous index of remission32. Depressive symptoms were also measured using the Mood Feeling Questionnaire, Child and Parent Versions (MFQ-C/P)33. The MFQ has high internal consistency (α=0.90) and test-retest reliability34. Total scores for child- and parent-report of preadolescents’ depressive symptoms were calculated and analyzed separately.
Parent-Child Conflict
Parent-child conflict was measured by the Conflict Behavior Questionnaire, Child and Parent versions (CBQ-C/P)35, a questionnaire with high internal consistency (α=0.90),36 test-retest reliability, and validity in discriminating between distressed and nondistressed families. Total scores for child- and parent-report of parent-child conflict were calculated and analyzed separately.
Anxiety
The Self-Report for Childhood Anxiety Related Emotional Disorders, Child and Parent Versions (SCARED-C/P)37 was used to assess anxiety symptoms in preadolescents. The SCARED-C/P has demonstrated good internal consistency (α=0.90 for total score) and good test-retest reliability. Total scores for child- and parent-report of preadolescents’ anxiety were calculated and analyzed separately.
Interpersonal Impairment
The Social Adjustment Scale-Self Report (SAS-SR)38 is a 23-item questionnaire that assesses children’s interpersonal impairment in school, social activities, and in family and peer relationships (α=0.88)39. Scores on the SAS-SR have been found to discriminate between individuals with and without depression38 and have been shown to be sensitive to treatment effects in an efficacy study of IPT-A26. Two subscales of the SAS-SR, social impairment and peer impairment, were calculated per scoring protocol38 and were analyzed separately.
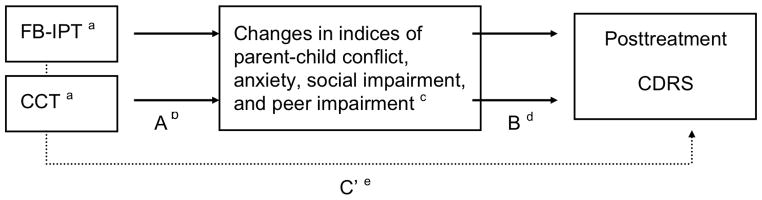
Participants
Figure 1 outlines the recruitment of participants for this study. Data was censured for 4 participants: 2 did not receive treatment after randomization, and 2 had diagnoses of PDD confirmed in sessions 1–4 of treatment. All of the remaining 38 participants were included in the between-group analyses of FB-IPT (n=25) and CCT (n=13). Preliminary analyses revealed no differences in the demographic and clinical characteristics of preadolescents in each treatment condition (see Table 1), nor in pretreatment indices of depression, parent-child conflict, anxiety, or in social or peer impairment (see Table 2). At the request of their parents, six preadolescents (n=6) started an SSRI trial in weeks 1–4 of the study. Although not significant (Fisher’s exact test [FET], p=0.06), a higher percentage of preadolescents in the CCT condition initiated adjunctive treatment with an SSRI than did those in the FB-IPT condition (67% [n=4] as compared to 33% [n=2], respectively). Across treatment conditions, SSRI augmentation was correlated with higher pretreatment scores on the CDRS-R (r= 0.26, p=0.11), MFQ-P (r= 0.27, p=0.10), and MFQ-C (r=0.28, p=0.10). Because pretreatment depression severity may have differed between groups, all analyses controlled for adjunctive SSRI treatment.
Table 1.
Demographic and Clinical Characteristics of Randomized Sample
| FB-IPT (n= 29) | CCT (n= 13) | Statistic | p | |
|---|---|---|---|---|
| Age (Mean, SD) | 10.6 (1.2) | 11.1 (1.1) | F(1, 41) = 1.54 | .22 |
| Female (n, %) | 18 (62.1) | 10 (76.9) | FET | .49 |
| Ethnic/Racial Minority (n, %) | 6 (20.7) | 3 (23.13) | FET | 1.00 |
| Two-Parent Family (n, %) | 13 (44.8) | 7 (53.8) | X2(n =42, df = 1) = 0.29 | .59 |
| Medical Assistance (n, %) | 5 (17.2) | 3 (23.1) | FET | .69 |
| Diagnosis | X2(n =42, df = 1) = 0.06 | .81 | ||
| Major Depressive Disorder (n, %) | 19 (65.5) | 9 (69.2) | ||
| Depressive Disorder NOS (n, %) | 10 (34.5) | 4 (30.8) | ||
| Suicidal Ideation (n, %) | 21 (72.4) | 11 (84.6) | FET | .47 |
| Non-Suicidal Self-Injury (n, %) | 6 (20.7) | 4 (30.8) | FET | .70 |
| SSRI augmentation | 2 (33.3) | 4 (66.7) | FET | .06 |
| Comorbid ADHD | 9 (31.0) | 3 (23.1) | FET | .72 |
| Comorbid Anxiety Disorder | 15 (51.7) | 7 (53.8) | X2(n =42, df = 1) = 0.02 | .90 |
| Number of Sessions Attended (Mean, SD) | 10.9 (3.5) | 9.0 (3.9) | t (37) = -1.51 | 0.13 |
Note: ADHD = attention-deficit/hyperactivity disorder; CCT = child-centered therapy; FB-IBT = family-based interpersonal psychotherapy; FET = Fischer’s exact test; NOS = not otherwise specified; SSRI = selective serotonin reuptake inhibitor.
Table 2.
Descriptive Statistics for Pre- and Posttreatment Measures in Family-Based Interpersonal Psychotherapy (FB-IPT) and Child-Centered Therapy (CCT)
| Measures | FB-IPT (n = 25) | CCT (n = 13) | t-statistic | p |
|---|---|---|---|---|
| Pretreatment Measures (Mean, SE) | ||||
| CDRS-R | 44.3 (1.4) | 47.2 (2.6) | 1.07 | 0.28 |
| MFQ-P | 19.8 (2.2) | 26.9 (3.6) | 1.78 | 0.08 |
| MFQ-C | 24.9 (4.5) | 23.6 (4.6) | -0.19 | 0.85 |
| SCARED-P | 25.3 (4.0) | 21.8 (2.6) | 0.78 | 0.44 |
| SCARED-C | 28.2 (3.7) | 26.3 (4.9) | -0.30 | 0.76 |
| CBQ-P | 9.4 (1.0) | 9.7 (1.3) | 0.17 | 0.86 |
| CBQ-C | 5.3 (0.9) | 8.2 (1.6) | 1.70 | 0.09 |
| SAS-SR, Peer Impairmenta | 10.3 (1.2) | 10.6 (1.3) | 0.20 | 0.84 |
| SAS-SR, Social Impairmenta | 12.1 (1.3) | 11.6 (1.4) | -0.26 | 0.80 |
| Posttreatment Measures (Mean, SE) | ||||
| CDRS-R | 26.7 (1.1) | 34.5 (2.8) | 3.01 | 0.003 |
| MFQ-P | 5.8 (1.1) | 11.4 (1.6) | 2.90 | 0.004 |
| MFQ-C | 5.6 (1.2) | 12.1 (2.9) | 2.49 | 0.01 |
| SCARED-P | 14.7 (2.3) | 19.1 (2.9) | 1.14 | 0.25 |
| SCARED-C | 12.7 (2.8) | 23.1 (4.7) | 2.00 | 0.05 |
| CBQ-P | 6.5 (0.9) | 8.8 (1.4) | 1.49 | 0.14 |
| CBQ-C | 3.9 (0.8) | 5.4 (1.6) | 0.98 | 0.33 |
| SAS-SR, Peer Impairmenta | 6.8 (0.9) | 9.7 (1.7) | 1.74 | 0.08 |
| SAS-SR, Social Impairmenta | 7.7 (0.9) | 11.6 (1.6) | 2.25 | 0.03 |
Note: CBQ-P/C = Conflict Behavior Questionnaire, Parent or Child Report; CDRS-R = Childhood Depression Rating Scale-Revised; MFQ-P/C = Mood and Feelings Questionnaire, Parent or Child Report; SAS-SR = Social Adjustment Scale, Self-Report; SCARED-P/C = Self-Report for Childhood Anxiety-Related Emotional Disorders, Parent or Child Versions.
Lower scores indicate less impairment.
Data Analyses
Multiple imputation was employed to account for missing posttreatment data for 21% of participants that terminated treatment unexpectedly and did not complete the posttreatment assessment (n=8; range of sessions attended, 3–10). Data was imputed using the fully conditional specification (FCS) or chained equations imputation algorithm through SPSS (IBM SPSS Statistics, IBM Corporation; Predictive Analytics Software [PASW] 22) to create 5 imputed datasets. Results of pooled analyses are subsequently reported. Chi-square was calculated to determine differences in posttreatment remission rates (dummy coded 0=not remitted, 1=remitted) by treatment condition (dummy coded 0=CCT, 1=FB-IPT). Linear regressions, controlling for pretreatment scores and SSRI augmentation, were conducted to assess differences between treatment conditions on posttreatment indices of depression. Linear regressions using change scores (post - pretreatment scores) examined differences between groups on changes in depression, parent-child conflict, anxiety, social impairment, or peer impairment across treatment. Effect sizes were calculated using Cohen’s F2 because of unequal participants in each treatment condition (values of 0.10, 0.20, and 0.40 represent small, medium, and large effect sizes, respectively)40. Linear regressions were used to test the effects of treatment condition on changes in parent-child conflict, anxiety, and interpersonal impairment (see Figure 1, path A), and the effects of changes in parent-child conflict, anxiety, and interpersonal impairment on preadolescents’ posttreatment CDRS-R scores (see Figure 1, path B). An indirect effects model was tested if there was a: 1) a significant relationship between treatment condition and changes in the proposed mediator (path A); 2) a significant relationship between changes in the proposed mediator and posttreatment CDRS-R scores (path B)41. The “product of coefficients” method was used to test the significance of the indirect effect of the proposed mediator on the association between treatment condition and outcome measure (see Figure 1, path C’). Indirect effects were estimated by calculating the product of the unstandardized betas from regression equations that represent path A and path B. Approximate z-scores for each indirect effect were calculated by dividing the product of the unstandardized betas from paths A and B by the product of the standard error (SE) from the regression equations that represent path A and B, where SE (path A* path B)2 = (SE of the unstandardized beta from path A)2* (unstandardized beta from path B)2 + (SE of the unstandardized beta from path B)2* (unstandardized beta from path A)2. Z-scores above 1.96 indicate a statistically significant indirect effect (p < 0.05). Analyses testing a priori hypotheses were conducted without adjusting for multiple comparisons.
Results
Treatment Condition and Clinical Response (path C)
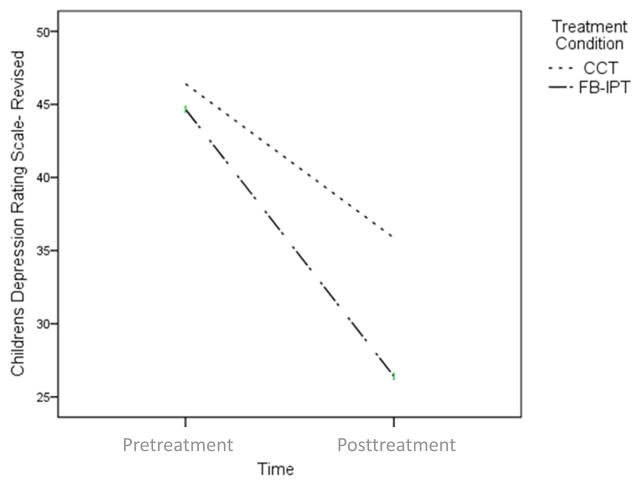
Preadolescents in the FB-IPT condition were more likely to achieve remission at posttreatment than those in CCT (16 [66%] vs. 4 [31%], Χ2[1, n=38]=4.17, p=0.04). Preadolescents in the FB-IPT group had significantly lower posttreatment CDRS-R scores (R2=0.35, ΔR2= 0.22; B=-8.15, SE=2.61, t[37]=-3.13, p=0.002, F2=0.28), parent-reported MFQ scores (R2=0.32, ΔR2=0.15; B=-5.23, SE= 2.12, t[37]=-2.47, p=0.01, F2=0.18), and preadolescent-reported MFQ scores (R2=0.22, ΔR2=0.11; B=-7.54, SE=2.77, t[37]=-2.72, p=0.007, F2=0.12) than preadolescents in the CCT group. Preadolescents receiving FB-IPT exhibited a greater decrease in CDRS-R scores from pre- to posttreatment compared to those receiving CCT, as depicted in Figure 2 (R2=0.18, Δ R2 = 0.12; B= -6.98, SE= 3.15, t[37]= -2.21, p=0.03, F2 = 0.22).
Figure 2.
Flowchart of recruitment, participant randomization, and engagement in the clinical trial. Note: CCT = child-centered therapy; FB-IPT = family-based interpersonal psychotherapy; SSRI = selective serotonin reuptake inhibitor.
Indirect effects of changes in parent-child conflict on the association between treatment condition and treatment response
There were no differences between the FB-IPT and CCT groups in the rate of change in parent-child conflict from pre- to posttreatment (path A), although a nonsignificant trend suggested a greater decrease in parental report of the CBQ from pre- to posttreatment for preadolescents treated with FB-IPT compared to preadolescents treated with CCT (R2=0.17, Δ R2 = 0.13; B= -2.74, SE= 1.61, t[37]= -1.70, p=0.09). Because there were no significant associations between changes in parent-child conflict and posttreatment CDRS-R scores (path B), criteria for testing indirect effects were not satisfied, and further analyses were not conducted.
Indirect effects of changes in preadolescent anxiety on the association between treatment condition and treatment response
Preadolescents in the FB-IPT condition evidenced a greater decrease in self-reported anxiety symptoms from pre- to posttreatment as compared to those in the CCT condition (R2=0.14, ΔR2=0.13; B=-14.65, SE= 6.28, t[37]=-2.33, p=0.02, F2= 0.15). Although approaching statistical significance (R2=0.29, ΔR2=0.19; B=-0.14, SE=0.07, t[37]=1.86, p=0.06), there was not a significant relationship between change in preadolescents’ anxiety symptoms across treatment and posttreatment depression scores (path B). Hence, the criteria for testing indirect effects were not satisfied, and further analyses were not conducted.
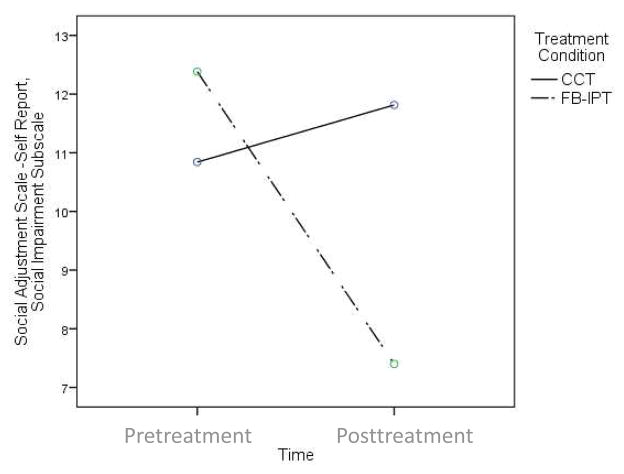
Indirect effects of changes in interpersonal impairment on the association between treatment condition and treatment response
Preadolescents in the FB-IPT condition had a significantly greater decrease in social impairment (R2=0.36, ΔR2=0.22; B=-6.32, SE=1.92, t[37]=-3.30, p=0.001, F2=0.28), and peer impairment (R2=0.34, ΔR2=0.15; B= -4.36, SE= 1.71, t[37]=-2.55, p=0.01, F2=0.18) from pre- to posttreatment than did preadolescents in the CCT condition. Furthermore, significant associations between posttreatment CDRS-R scores and changes in preadolescents’ report of social impairment (R2=0.19, ΔR2=0.18; B=0.71, SE=0.22, t[37]=3.31, p=0.001, F2 = 0.22) and peer impairment (R2=0.28, ΔR2=0.27; B=0.68, SE=0.30, t[37]=2.24, p=0.03, F2=0.37) were found, indicating that lower depression scores at posttreatment were associated with greater decreases in preadolescents’ social and peer impairment across treatment (path B). Indirect effects models were tested for preadolescents’ social impairment and peer impairment as mediators of the association between FB-IPT and posttreatment CDRS-R scores. Results yielded a significant effect for changes in social impairment (z=-2.30, p<0.05), accounting for the association between FB-IPT and preadolescents’ depressive symptoms at posttreatment.
Discussion
Preadolescents receiving FB-IPT had higher rates of remission, lower scores of depressive symptoms at posttreatment by clinician interview and parent and child-reported measures, and a greater decrease in depressive symptoms from pre- to posttreatment than did preadolescents with depression receiving CCT. These findings provide strong support for FB-IPT as an effective treatment for preadolescent depression with medium to larger effect sizes. Preadolescents receiving FB-IPT also evidenced a greater reduction in anxiety symptoms and interpersonal impairment across treatment course than did those receiving CCT. Of these variables, only changes in social and peer impairment were associated with preadolescents’ posttreatment depressive symptoms. There was a significant indirect effect for decreased social impairment mediating the association between the FB-IPT and preadolescents’ posttreatment depressive symptoms. This may suggest that reducing social impairment is one mechanism by which FB-IPT may decrease preadolescents’ depressive symptoms.
Findings from this study must be understood in light of several limitations. First, both FB-IPT and CCT were delivered by the same therapists in order to assure equivalence across treatment groups in therapist characteristics and experience. However, this strategy may increase the likelihood of cross-treatment contamination. Although therapists were adherent to CCT techniques, their case conceptualizations of participants may have been contaminated by FB-IPT, possibly increasing the efficacy of CCT. Because therapists were not blinded to treatment condition or study hypotheses, they may have been biased towards the FB-IPT condition when coding posttreatment CDRS-R measures for 40% of the sample. However, given the similar patterns of results found using preadolescent- and parent-rated depression ratings at posttreatment, the potential for therapist bias in rating the CDRS-R is low. Another limitation of the current study is the lack of blinding in the fidelity coding for both treatments. Because the first author (L.J.D.) has developed and piloted FB-IPT, she served as the primary evaluator of therapists’ treatment fidelity in this first efficacy trial of FB-IPT. This study used a broad criterion for determining treatment fidelity across groups and did not specifically measure treatment contamination. Still, it is likely that deviations from therapeutic stance would likely be reflected in fidelity ratings because of how FB-IPT and CCT differed in content and structure. In addition, the strategy of randomization may have been less effective than using a matched control group for this small sample. Although we controlled for SSRI augmentation, our low statistical power may have limited our ability to detect significant pretreatment differences between FB-IPT and CCT. Although high in external validity, pretreatment diagnoses and CDRS-R scores obtained by “real world” mental health professionals before preadolescents were enrolled in the study precluded our ability to obtain reliability estimates of these measures. Lastly, findings from indirect effects analyses must be considered exploratory as measures of hypothesized mediators were collected at the same time as pre- and posttreatment outcome measures. Adequately powered future studies are needed to confirm our findings, suggesting that decreased social impairment may mediate the effects of FB-IPT on preadolescents’ depressive symptoms.
Our results support the efficacy of FB-IPT in increasing the likelihood of remission and reducing preadolescents’ depressive symptoms over the course of treatment, and suggest a genuine advantage of FB-IPT over supportive therapy. Preadolescents in the FB-IPT condition demonstrated significant decreases in anxiety and in interpersonal impairment as compared to preadolescents receiving CCT, suggesting that FB-IPT was effective in changing constructs hypothesized to be treatment mechanisms. However, it remains to be established whether this result was due to increased parental involvement in treatment or techniques specific to the FB-IPT intervention. Results also provide preliminary support for decreases in preadolescents’ social impairment as a specific treatment mechanism of FB-IPT in reducing depressive symptoms. Given the lack of temporal precedence in our hypothesized mediator measures, it may be possible that decreases in depressive symptoms accounted for the decreases in preadolescents’ social impairment in the FB-IPT group. It is likely that low statistical power obscured our detection of significant changes in parent-child conflict between treatment groups.
Psychosocial intervention for preadolescents with depression presents an opportunity to reduce family and interpersonal risk factors that may increase the likelihood of recurrent depression in adolescence. The results of this trial suggest that FB-IPT is an efficacious psychosocial intervention for increasing remission and decreasing preadolescents’ anxiety and interpersonal impairment. Given the results of this preliminary efficacy trial, future research studies should test the effectiveness and transportability of FB-IPT, as well as longitudinal outcomes of preadolescents with depression treated with FB-IPT.
Figure 3.
Preadolescents receiving family-based interpersonal psychotherapy (FB-IPT) evidence significantly greater decreases in depressive symptoms across treatment compared to those receiving child-centered therapy (CCT).
Figure 4.
Preadolescents receiving family-based interpersonal psychotherapy (FB-IPT) evidence significantly greater decreases in social impairment across treatment than do those receiving child-centered therapy (CCT).
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health (NIMH: MH 079353, L.J.D.).
The authors would like to acknowledge the children and families who participated in this treatment study for their participation and for sharing their experiences to improve the treatment of mental illness in youths.
Footnotes
Dr. Weinberg reports no biomedical financial interests or potential conflicts of interest.
Disclosure: Dr. Dietz has received research support from NIMH. Dr. Brent has received research support from NIMH; has received royalties from Guilford Press; and has served as UpToDate Psychiatry Editor. Dr. Mufson has received royalties from Guilford Press and has also received research support from NIMH, Substance Abuse and Mental Health Services Administration, and Brain and Behavior Research Foundation (formerly NARSAD), as well as salary support from NYSPI via the New York State Office of Mental Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr Laura J. Dietz, University of Pittsburgh School of Medicine, Pittsburgh.
Dr Rebecca J. Weinberg, University of Pittsburgh School of Medicine, Pittsburgh.
Dr David A. Brent, University of Pittsburgh School of Medicine, Pittsburgh.
Dr Laura Mufson, Columbia University College of Physicians and Surgeons/New York State Psychiatric Institute (NYSPI), New York.
References
- 1.Keenan K, Hipwell A, Feng X, et al. Subthreshold Symptoms of Depression in Preadolescent Girls Are Stable and Predictive of Depressive Disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(12):1433–1442. doi: 10.1097/CHI.0b013e3181886eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angold A, Costello EJ, Farmer EM, Burns BJ, Erkanli A. Impaired but undiagnosed. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(2):129–137. doi: 10.1097/00004583-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL. Adult psychosocial outcome of prepubertal major depressive disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(6):673–677. doi: 10.1097/00004583-200106000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Kovacs M, Feinberg TL, Crouse-Novak M, Paulauskas SL, Pollock M, Finkelstein R. Depressive disorders in childhood. II. A longitudinal study of the risk for a subsequent major depression. Archives of general psychiatry. 1984;41(7):643–649. doi: 10.1001/archpsyc.1984.01790180013001. [DOI] [PubMed] [Google Scholar]
- 5.Puig-Antich J, Lukens E, Davies M, Goetz D, Brennan-Quattrock J, Todak G. Psychosocial functioning in prepubertal major depressive disorders. II. Interpersonal relationships after sustained recovery from affective episode. Archives of general psychiatry. 1985b;42(5):511–517. doi: 10.1001/archpsyc.1985.01790280093010. [DOI] [PubMed] [Google Scholar]
- 6.Beardslee WR, Gladstone TR, O'Connor EE. Transmission and prevention of mood disorders among children of affectively ill parents: a review. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(11):1098–1109. doi: 10.1016/j.jaac.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 7.Beardslee WR, Versage EM, Wright EJ, et al. Examination of preventive interventions for families with depression: evidence of change. Development and psychopathology. 1997;9(1):109–130. doi: 10.1017/s0954579497001090. [DOI] [PubMed] [Google Scholar]
- 8.Seeley JR, Stice E, Rohde P. Screening for depression prevention: identifying adolescent girls at high risk for future depression. Journal of abnormal psychology. 2009;118(1):161–170. doi: 10.1037/a0014741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keenan K, Hipwell AE. Preadolescent Clues to Understanding Depression in Girls. Clinical child and family psychology review. 2005;8(2):89–105. doi: 10.1007/s10567-005-4750-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hazel NA, Oppenheimer CW, Technow JR, Young JF, Hankin BL. Parent relationship quality buffers against the effect of peer stressors on depressive symptoms from middle childhood to adolescence. Developmental psychology. 2014;50(8):2115–2123. doi: 10.1037/a0037192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Copeland WE, Wolke D, Angold A, Costello EJ. Adult psychiatric outcomes of bullying and being bullied by peers in childhood and adolescence. JAMA psychiatry. 2013;70(4):419–426. doi: 10.1001/jamapsychiatry.2013.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Axelson DA, Birmaher B. Relation between anxiety and depressive disorders in childhood and adolescence. Depression and Anxiety. 2001;14(2):67–78. doi: 10.1002/da.1048. [DOI] [PubMed] [Google Scholar]
- 13.Reijntjes A, Thomaes S, Boelen P, van der Schoot M, de Castro BO, Telch MJ. Delighted when approved by others, to pieces when rejected: children's social anxiety magnifies the linkage between self- and other-evaluations. Journal of child psychology and psychiatry, and allied disciplines. 2011;52(7):774–781. doi: 10.1111/j.1469-7610.2010.02325.x. [DOI] [PubMed] [Google Scholar]
- 14.Young JF, Berenson K, Cohen P, Garcia J. The Role of Parent and Peer Support in Predicting Adolescent Depression: A Longitudinal Community Study. Journal of Research on Adolescence. 2005;15(4):407–423. [Google Scholar]
- 15.David-Ferdon C, Kaslow NJ. Evidence-based psychosocial treatments for child and adolescent depression. Journal of clinical child and adolescent psychology. 2008;37(1):62–104. doi: 10.1080/15374410701817865. [DOI] [PubMed] [Google Scholar]
- 16.Kahn JS, Kehle TJ, Jenson WR, Clark E. Comparison of cognitive-behavioral, relaxation, and self-modeling interventions for depression among middle-school students. School Psychology Review. 1990;19(2):196–211. [Google Scholar]
- 17.Vostanis P, Feehan C, Grattan E, Bickerton W-L. A randomised controlled out-patient trial of cognitive-behavioural treatment for children and adolescents with depression: 9-month follow-up. Journal of affective disorders. 1996;40(1–2):105–116. doi: 10.1016/0165-0327(96)00054-7. [DOI] [PubMed] [Google Scholar]
- 18.Stark K, Kendall PC, McCarthy M, Stafford M, Barron R, Thomeer M. Taking action: A workbook for overcoming depression. Ardmore, PA: Workbook Publishing; 1996. [Google Scholar]
- 19.Weisz JR, Thurber CA, Sweeney L, Proffitt VD, LeGagnoux GL. Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. Journal of Consulting and Clinical Psychology. 1997;65(4):703–707. doi: 10.1037//0022-006x.65.4.703. [DOI] [PubMed] [Google Scholar]
- 20.Szigethy E, Bujoreanu SI, Youk AO, et al. Randomized efficacy trial of two psychotherapies for depression in youth with inflammatory bowel disease. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(7):726–735. doi: 10.1016/j.jaac.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stark KD, Banneyer KN, Wang LA, Arora P. Child and adolescent depression in the family. Couple and Family Psychology: Research and Practice. 2012;1(3):161–184. [Google Scholar]
- 22.Fristad MA, Verducci JS, Walters K, Young ME. Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Archives of general psychiatry. 2009;66(9):1013–1021. doi: 10.1001/archgenpsychiatry.2009.112. [DOI] [PubMed] [Google Scholar]
- 23.Tompson MC, Pierre CB, Haber FM, Fogler JM, Groff AR, Asarnow JR. Family-focused treatment for childhood-onset depressive disorders: results of an open trial. Clinical child psychology and psychiatry. 2007;12(3):403–420. doi: 10.1177/1359104507078474. [DOI] [PubMed] [Google Scholar]
- 24.Kovacs M, Sherrill J, George CJ, Pollock M, Tumuluru RV, Ho V. Contextual emotion-regulation therapy for childhood depression: description and pilot testing of a new intervention. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(8):892–903. doi: 10.1097/01.chi.0000222878.74162.5a. [DOI] [PubMed] [Google Scholar]
- 25.Mufson L, Pollack Dorta K, Moreau D, Weissman M. Interpersonal psychotherapy for depressed adolescents. 2. New York: Guilford Publications, Inc; 2004. [Google Scholar]
- 26.Mufson L, Weissman MM, Moreau D, Garfinkel R. Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of general psychiatry. 1999;56(6):573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- 27.Mufson LH, Dorta KP, Olfson M, Weissman MM, Hoagwood K. Effectiveness research: transporting interpersonal psychotherapy for depressed adolescents (IPT-A) from the lab to school-based health clinics. Clinical Child and Family Psychology Review. 2004;7(4):251–261. doi: 10.1007/s10567-004-6089-6. [DOI] [PubMed] [Google Scholar]
- 28.Dietz LJ, Mufson L, Irvine H, Brent DA. Family-based interpersonal psychotherapy for depressed preadolescents: an open-treatment trial. Early intervention in psychiatry. 2008;2(3):154–161. doi: 10.1111/j.1751-7893.2008.00077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weersing VR, Weisz JR. Community clinic treatment of depressed youth: benchmarking usual care against CBT clinical trials. Journal of consulting and clinical psychology. 2002;70(2):299–310. doi: 10.1037//0022-006x.70.2.299. [DOI] [PubMed] [Google Scholar]
- 30.Brent DA, Holder D, Kolko D, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of general psychiatry. 1997;54(9):877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- 31.Poznanski E, Freeman LN, Mokros HB. Children's Depression Rating Scale-Revised. Psychopharmacology Bulletin. 1985;21:979–989. [Google Scholar]
- 32.Kennard BD, Silva SG, Tonev S, et al. Remission and recovery in the Treatment for Adolescents with Depression Study (TADS): acute and long-term outcomes. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(2):186–195. doi: 10.1097/CHI.0b013e31819176f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International journal of methods in psychiatric research. 1995;5(4):237–249. [Google Scholar]
- 34.Costello EJ, Benjamin R, Angold A, Silver D. Mood variability in adolescents: a study of depressed, nondepressed and comorbid patients. Journal of affective disorders. 1991;23(4):199–212. doi: 10.1016/0165-0327(91)90101-w. [DOI] [PubMed] [Google Scholar]
- 35.Robin AL, Weiss JG. Criterion-related validity of behavioral and self-report measures of problem-solving communication skills in distressed and non-distressed parent-adolescent dyads. Behavioral Assessment. 1980;2:339–352. [Google Scholar]
- 36.Prinz RJ, Foster S, Kent RN, O'Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of applied behavior analysis. 1979;12(4):691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of general psychiatry. 1976;33(9):1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 39.Rzepa S, Weissman M. Social Adjustment Scale Self-Report (SAS-SR) In: Michalos A, editor. Encyclopedia of Quality of Life and Well-Being Research. Springer; Netherlands: 2014. pp. 6017–6021. [Google Scholar]
- 40.Chen S, Chen H. Encyclopedia of Research Design. Thousand Oaks, CA: SAGE Publications, Inc; 2010. Cohen's f Statistic; pp. 186–188. [Google Scholar]
- 41.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]