Abstract
Objective
To evaluate the effectiveness of the contraceptive implant and the 52mg hormonal intrauterine device (IUD) in women using the method beyond the current U.S. Food and Drug Administration–approved duration of 3 and 5 years respectively.
Methods
Women willing to continue using their implant or 52mg levonorgestrel IUD (LNG-IUD) beyond the FDA-approved duration were followed prospectively for contraceptive effectiveness. Unintended pregnancy rate per 100 women-years was calculated. Implant users are offered periodic venipuncture for analysis of serum etonogestrel levels. The Kruskal-Wallis test was used to compare the etonogestrel levels across BMI groups.
Results
Implant users (n=237) have contributed 229.4 women-years of follow-up, with 123 using the etonogestrel implant for 4 years, and 34 using it for 5 years. Zero pregnancies have been documented, for a failure rate of 0 (one-sided 97.5% CI: 0, 1.61) per 100 women-years. Among 263 LNG-IUD users, 197.7 women-years of follow-up have been completed. One pregnancy was confirmed, for a failure rate of 0.51 (95% CI: 0.01, 2.82) per 100 women-years. Among implant users with serum etonogestrel results, the median and range of etonogestrel level at 3 years of use was 188.8 pg/mL (range 63.8, 802.6) and 177.0 pg/mL (67.9, 470.5) at 4 years of use. Etonogestrel levels did not differ by BMI at either time point (3 years: p=0.79; 4 years: p=0.47).
Conclusion
Preliminary findings indicate the contraceptive implant and 52mg hormonal IUD continue to be highly-effective for an additional year, beyond the FDA approved 3 and 5 years..
Serum etonogestrel levels indicate the implant contains adequate hormone for ovulation suppression at the end of both 3 and 4 years of use.
Introduction
The family planning community has identified improving knowledge, access and uptake of long-acting reversible contraception (LARC) as a winning strategy for reducing unintended pregnancy. [1-4] Increasing use of LARC, specifically the intrauterine devices (IUD) and implants, has been shown to decrease the rate of unintended pregnancy because its effectiveness is not user-dependent. [5-7] There are many advantages to these methods beyond their user-independence[8]: desirable side-effects, highly-effective pregnancy prevention, safety in medically complicated patients [9-11], and cost-effectiveness.[3, 12]
Despite the intention of the Affordable Care Act, LARC methods are still not available to all reproductive age women in the United States. Furthermore, access to LARC methods globally and in developing nations continues to be difficult. With many women experiencing access barriers, knowledge regarding the extended use of these methods beyond the current FDA-approved duration would allow women to continue to confidently use their current method in the event they could not access or afford a new device. Although rare, insertion of LARC methods is associated with potential complications; avoiding removal and reinsertion at the time of method expiration may be of interest to the individual patient. Lastly, the potential to further improve the cost-effectiveness by extending the life of these devices provides tremendous economic benefit to insurers and to society.
This study (the Effectiveness of Prolonged use of the IUD and Implant for Contraception study) begins to fill gaps in the literature regarding extended use of the etonogestrel implant and 52mg LNG-IUD. The objective of this report is to present the preliminary results of this study, focusing on the effectiveness of the implant and IUD in the year beyond FDA-approved expiration.
Materials and Methods
We analyzed data from participants enrolled between January 2012 and November 2014 in this ongoing prospective observational study. The study protocol was approved by the Institutional Review Board at Washington University in St. Louis prior to participant recruitment.
Participants were recruited through advertisements in local clinics and newspapers, by alerting clinicians regarding the Effectiveness of Prolonged use of the IUD and Implant for Contraception study protocol, and through previous participation in the Contraceptive CHOICE Project (CHOICE). CHOICE was a prospective cohort study of reproductive-aged women in St. Louis designed to promote the use of LARC by eliminating cost, access, and knowledge barriers. [14] Women were eligible to participate in the Effectiveness of Prolonged use of the IUD and Implant for Contraception study if English or Spanish speaking, aged 18-45 years, were within 3 months of or beyond the current FDA-approved duration of use, sexually active with a male partner, and wanted to avoid pregnancy for a minimum of 12 months.
At study enrollment participants provide written informed consent and complete a staff-administered demographic and reproductive health survey that includes questions regarding intercourse frequency, other contraceptive method use, menstrual cycle regularity, partner characteristics, and presence of comorbidities that may affect fertility. Participants also undergo objective measurement of height and weight, as well as venipuncture if they were consenting implant users. Telephone follow-up surveys are completed every 6 months for 36 months or until the date of removal. In addition to baseline assessment, venipuncture is offered annually (at the anniversary of the patient's implant insertion), at the time of method removal, or if a pregnancy is experienced during method use. Participants are compensated with a $20 gift card at enrollment, completion of each survey, and for each venipuncture. Participants are informed that the results from their etonogestrel assay will not be individually revealed and will not impact their eligibility for study participation or their clinical care. Participants are instructed to call study staff at any time if they suspect pregnancy or if they desire method removal.
At the time of venipuncture, 7 mL of whole blood are collected and allowed to sit upright for clot formation for 1-2 hours. Samples are then centrifuged for 10 minutes at 4° C at 3000 rpm. Serum is aliquoted off and stored in a laboratory freezer at −80° C. Samples are then sent to the Columbia University Medical Center Core Laboratory for etonogestrel analysis where liquid chromatography tandem mass spectrometry is performed by the Biomarkers Core Laboratory of the Irving Institute of Clinical and Translational Research at Columbia University Medical Center.[13]
Our primary outcome is unintended pregnancy during prolonged use of the LNG-IUD and implant. Follow-up time was calculated from FDA-approved method expiration date to the last contact date during the study. Secondary outcomes include serum etonogestrel levels at various time points during prolonged use of the implant, and comparison of etonogestrel levels across body mass index (BMI) classes. We defined 3 year to be any sample contributed through 6 months of additional use (3.5 years), and a 4-year sample to have been collected between 3.5 years and 4.5 years of use. Eighty-eight percent of participants (N=442) were enrolled from CHOICE and 58 were from outside clinics. Method expiration was validated for all former CHOICE participants and for 30% of participants recruited from outside clinics with medical record review; thus, we validated 459 of 500 (91.8%) participants’ method expiration date. At 12 months, there was a 2.6% loss to follow-up rate. BMI was calculated as weight in kilograms divided by height in meters squared . Participants were classified into one of three BMI categories as defined by the World Health Organization, combining the underweight and normal weight categories. [14] Normal weight women were defined as those with a BMI less than 25.0, overweight as 25.0-29.9, obese as greater than or equal to 30.0. [15]
All statistical analyses were performed using SAS Software (v.9.4.; SAS Institute, Cary, NC). Significance levels (α) were set at 0.05. Demographic characteristics of all participants are presented as means, standard deviations and percentages stratified by IUD and Implant. Unintended pregnancy rate was calculated using number of unintended pregnancies divided by total women years of follow-up time, and 95% confidence interval (CI) was calculated. Since there was no pregnancy outcome in Implant use, one-sided 97.5% CI was presented. Etonogestrel levels were not normally distributed and thus the Kruskal-Wallis test was used to compare the median etonogestrel levels across the three BMI categories at 3 years and at 4 years of implant use.
Results
At the time of analysis, 237 implant users were enrolled contributing 229.4 women-years of time to this analysis. Of those 123 have used their method for at least one additional year, and 34 for an additional 2 years. The median duration of prolonged use in the implant cohort is 12.5 additonal months (Range: 5.1-40.5 months). Characteristics of the study population by method are shown in Table 1.
Table 1.
Baseline Demographic and Reproductive Characteristics by Method
| Etonogestrel implant (N=237) | 52mg LNG-IUD (N=263) | |||
|---|---|---|---|---|
| Mean(SD) | Mean(SD) | |||
| Age, years | 26.0 (5.4) | 32.2 (5.9) | ||
| n | % | n | % | |
| Age, years | ||||
| 18-22 | 73 | 30.8% | 4 | 1.5% |
| 23-29 | 115 | 48.5% | 97 | 36.9% |
| 30-34 | 28 | 11.8°% | 73 | 27.8% |
| 35-45 | 21 | 8.9% | 89 | 33.8% |
| Race | ||||
| Missing (n = 1) | ||||
| Black | 168 | 70.9% | 133 | 50.8% |
| White | 50 | 21.1% | 114 | 43.5% |
| Other | 19 | 8.0% | 15 | 5.7% |
| Hispanic | ||||
| Hispanic | 10 | 4.2% | 6 | 2.3% |
| Non-Hispanic | 227 | 95.8% | 257 | 97.7% |
| Education | ||||
| High school or less | 79 | 33.3% | 47 | 17.9% |
| Some college/vocational school | 123 | 51.9% | 93 | 35.4% |
| Completed college or greater | 35 | 14.8% | 123 | 46.8% |
| Insurance Status | ||||
| Missing (n = 1) | ||||
| None | 89 | 37.7% | 80 | 30.4% |
| Private | 101 | 42.8% | 145 | 55.1% |
| Public | 46 | 19.5% | 38 | 14.5% |
| Low socioeconomic status | ||||
| Yes | 136 | 57.4% | 105 | 39.9% |
| No | 101 | 42.6% | 158 | 60.1% |
| Marital Status | ||||
| Single/Never married | 158 | 66.7% | 100 | 38.0% |
| Married/Not married, but living with partner | 74 | 31.2% | 143 | 54.4% |
| Separated/Divorced/Widowed | 5 | 2.1% | 20 | 7.6% |
| Gravidity | ||||
| Missing (n = 10) | ||||
| 0 | 72 | 30.6% | 69 | 27.1% |
| 1-2 | 104 | 44.3% | 100 | 39.2% |
| ≥3 | 59 | 25.1% | 86 | 33.7% |
| BMI, kg/m2 | ||||
| <25 | 67 | 28.3% | 84 | 31.9% |
| 25-30 | 52 | 21.9% | 60 | 22.8% |
| >=30 | 118 | 49.8% | 119 | 45.3% |
* Low SES is defined as any participant reporting difficulty paying for basic needs such as food shelter or childcare or receiving public assistance
To date, we have documented zero pregnancies in the implant group. With zero pregnancies during this follow-up period, the estimated failure rate per 100 women-years after expiration is 0 (one-sided 97.5% CI: 0, 1.61) in our cohort.
Of the 237 implant users, 92 contributed 3-year samples for etonogestrel analysis and 47 contributed 4-year samples. Participant BMIs ranged from 16.6 to 53.2. We noted the following distribution across BMI groups: 29% (N=27) normal weight, 25% (N=23) overweight, 46% (N=42) obese or morbidly obese. The median etonogestrel level at 3 years of use was 188.8pg/ml (Range: 63.8, 802.6) and 170.0pg/ml (Range: 67.9, 470.5 )at 4 years of use. We found no differences in median serum etonogestrel levels across BMI groups at method expiration (p=0.79), or at the end of the 4th year of use (p=0.47). The median etonogestrel levels at 3 years and 4 years of use for each BMI class are shown in Table 2 and box plot distributions are shown in Figures 1 and 2.
Table 2.
Median Etonogestrel levels at the end of 3rd and 4th years of Implant use by BMI categories
| 3rd year (N = 92) (p=.79) | |||
|---|---|---|---|
| BMI Category | n | Etonogestrel (pg/ml) (MEDIAN) | Range |
| <25 | 27 | 193.7 | (118.3, 802.6) |
| 25-30 | 23 | 178.5 | (63.8, 464.7) |
| >=30 | 42 | 188.3 | (75.9, 520.9) |
| 4th year (N = 47) (p=.14) | |||
| <25 | 11 | 170.1 | (99.2, 319.0) |
| 25-30 | 10 | 210.6 | (67.9, 450.5) |
| >=30 | 26 | 167.8 | (72.5, 470.5) |
Figure 1.
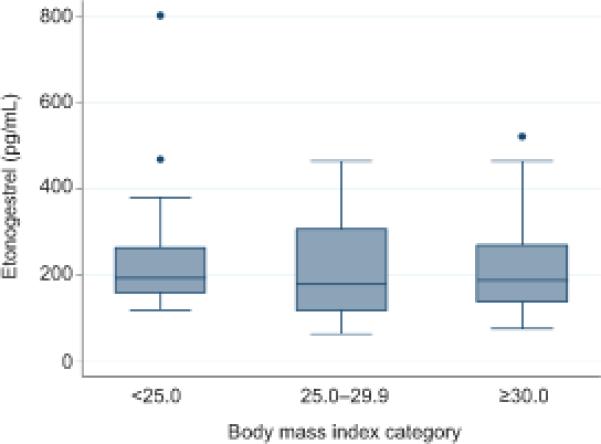
Box plot of etonogestrel level at the end of third year of implant use by body mass index category.
Figure 2.
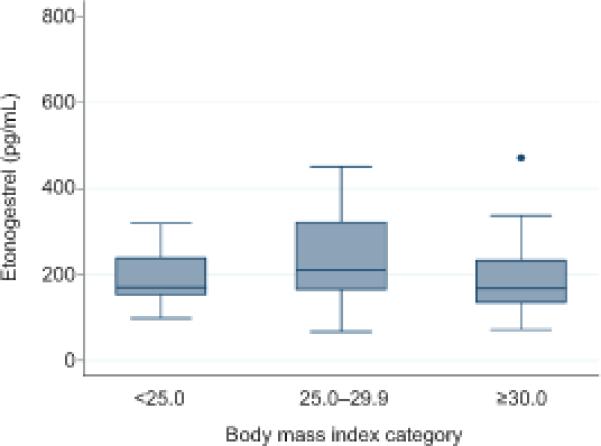
Box plot of etonogestrel levels at the end of fourth year of implant use by body mass index category.
At the time of analysis 263 LNG-IUD users were enrolled contributing 197.7 women-years of time. Of those, 108 have used their method for at least one additional year. The median duration of prolonged use in the LNG-IUD cohort is 11.7 additional months (Range: 4.7, 36.2 months). Characteristics of the study population by method are shown in Table 1.
To date, we have documented one pregnancy in the IUD group. The participant presented less than one month after FDA-approved duration with pregnancy symptoms (nausea and breast tenderness). On exam she was found to have a partially expelled IUD (stem of the IUD visualized outside the cervix) and at 6 weeks gestation. With one failure during this follow-up period, the estimated failure rate is 0.51 (95% CI: 0.01, 2.82) per 100 women-years.
Given that age is a strong predictor of fertility, a sensitivity analysis excluding participants greater than 35 years old at enrollment was performed and showed the estimated failure rate per 100 women-years after the FDA-approved duration is 0 (one-sided 97.5% CI: 0, 1.74) for Implant and 0.79 (95% CI: 0.02, 4.39) for IUD, respectively.
Discussion
The etonogestrel subdermal implant and the 52 mg LNG-IUD are among the most effective forms of reversible contraception available with a failure rate of less than 1% over the 3-year and 5-year FDA-approved durations. [16-18] The primary mechanism by which the implant works is ovulation suppression, with secondary effects on cervical mucus and changes in endometrial architecture.[19, 20] Previous literature suggests a serum etonogestrel concentration of 90 pg/mL is sufficient for ovulation suppression.[21] Pharmacokinetic data has shown that serum concentrations at the end of the third year of use are maintained well above this threshold; however, adequate evaluation of clinical outcomes is limited.[19] One small study followed 75 women through 4 years of use and reported no pregnancies during that time.[22] Additionally, studies evaluating serum etonogestrel levels in overweight and obese women have been limited to immediately following, or shortly after insertion. Existing pharmacokinetic data suggests obese women using the method during the FDA-approved duration have lower serum concentrations, but clinical data does not suggest these women are experiencing more unintended pregnancies.[23, 24] Given the growing prevalence of obesity, it is important that we understand how BMI affects serum etonogestrel concentrations, and ultimately the effectiveness of the device. Preliminary findings from our study suggest the implant continues to be highly-effective during the 4th year of use, with the failure rate similar to the published 3-year failure rate. Our findings support the findings of Kiriwat who noted zero pregnancy in 75 Thai women using the implant for an additional year. [22]
We also found no difference in etonogestrel levels across BMI categories at 3 or 4 years of implant use. This data will begin deliniating the relationship of etonogestrel levels and contracpetive efficacy as we will be able to correlate clinical outcomes (unintended pregnancy) to serum etonogestrel levels. Previous data has shown a slow decline in etonogestrel levels (36-84 pg/mL) from year one to year 3, and there is no evidence to suggest the rate of decline would be drastically different in the years to follow [8]. The absolute etonogestrel serum level required for contraception has not been defined and may be lower than 90 pg/mL as other secondary factors, such as cervical mucus changes, can prevent pregancy even if occassional ovulation occurs.
One major strength of this study is the diversity among BMI classes in our population. This provides a unique opportunity to improve our understanding among overweight and obese women, whom represent nearly two-thirds of reproductive age women in the United States. [25] Pharmacokinetic data in this population is especially limited as there are few studies, most with very small sample sizes of women who are within 130% of their ideal body weight, and we found no studies evaluating etonogestrel levels at method expiration or beyond. Mornar et al. published findings from their study in which 13 obese women were found to have lower etonogestrel levels than 4 normal weight comparisons in the 6 months following insertion of the implant. [11] This study extrapolated their findings to suggest etonogestrel levels at method expiration in obese women would be near 90 pg/mL, suggesting potential decreased efficacy at method expiration. Preliminary data from our study does not support that assumption, instead suggests women with a higher BMI are not at increased risk of failure. Furthermore, clinical data has not shown a corresponding increase in the prevalence of unintended pregnancy in overweight and obese women using the implant [12].
The LNG-IUD primarily prevents pregnancy through thickening of the cervical mucous and thus prevention of fertilization. [26] Aside from a single publication by the Population Council in 1991 in which a 7-year cumulative failure rate for the LNG-IUD (60mg) was noted to be 1.1 per 1000, we could find no reports in the US population with today's 52mg device. [27] A recent systematic review explored the available evidence for extended use of IUDs and concluded the 52mg LNG-IUD could be safely used for up to seven years. [28] The data available thus far from our study support this conclusion.
Our study has several strengths. The sample represents a diverse group of contracepting women of varying age, race, BMI, and socioeconomic groups supporting generalizability of our findings to a larger population. The prospective design of the study allows for the evaluation of clinical outcomes such as unintended pregnancy and pharmacokinetic changes among participants. Lastly, objective measurements of weight and height resulted in accurate BMI classification.
Our study is not without limitations, however. Although this study is the only reported U.S cohort of prolonged IUD and implant users, the sample size does limit our ability to find small differences, especially in the evaluation of etonogestrel by BMI class. However, the study is ongoing, and we plan to recruit and follow more than 400 users of each device for an additional 3 years. Despite the ongoing recruitment, we feel publication of these preliminary findings of only 1 pregnancy in 197.7 women-years of prolonged IUD use and zero pregnancies in 229.4 women-years of prolonged implant use to be a major clinical contribution even at this early stage. Although we may not have power to detect small differences between BMI classes, it is reassuring that median levels within each class remain well above 90 pg/mL. As we enroll more participants into the Effectiveness of Prolonged use of the IUD and Implant for Contraception study, the precision of our estimates will improve.
In conclusion, our findings suggest that the etonogestrel implant and 52mg LNG-IUD can be safely used for an additional year beyond the current FDA-approved duration of 3 and 5 years, respectively. Although preliminary, we believe this data provides enough evidence to exclude a pregnancy risk similar to the oral contracpetive pill, transdermal patch, or vagnal ring. Etonogestrel levels at the end of 3 and 4 years do not appear to vary by BMI, and the median level remains above the threshold for ovulation supression. Continued follow-up of the participants in this study will provide important data and has the potential to change the provision of contraceptive services.
PRECIS.
Both the contraceptive implant and the 52mg hormonal intrauterine device remain highly effective at one additional year beyond their current U.S. Food and Drug Administration– approved duration of 3 and 5 years, respectively.
Acknowledgements
The authors thank the Columbia University Medical Center Core Laboratory for assisting with serum etonogestrel testing.
Funding: This project was supported by the Society of Family Planning (SFPRF 12-1). This research is also supported in part by the Washington University Institute of Clinical and Translational Sciences National Center for Research Resources (NCRR) grant UL1 RR024992 from the National Center for Advancing Translational Sciences, and the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number T32HD055172.
Footnotes
Financial Disclosure: Dr. Peipert receives research funding from Bayer, Teva, and Merck and served on Advisory Boards for Teva, Bayer, and Watson/Activitis. The other authors did not report any potential conflicts of interest.
References
- 1.Secura G. Long-acting reversible contraception: a practical solution to reduce unintended pregnancy. Minerva Ginecol. 2013;65(3):271–7. [PubMed] [Google Scholar]
- 2.Baldwin MK, Edelman AB. The effect of long-acting reversible contraception on rapid repeat pregnancy in adolescents: a review. J Adolesc Health. 2013;52(4 Suppl):S47–53. doi: 10.1016/j.jadohealth.2012.10.278. [DOI] [PubMed] [Google Scholar]
- 3.Trussell J, et al. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–61. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: increasing use of long-acting reversible contraception. Hum Reprod Update. 2011;17(1):121–37. doi: 10.1093/humupd/dmq026. [DOI] [PubMed] [Google Scholar]
- 5.Peipert JF, et al. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–7. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finer LB, Sonfield A. The evidence mounts on the benefits of preventing unintended pregnancy. Contraception. 2013;87(2):126–7. doi: 10.1016/j.contraception.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Secura GM, et al. Provision of No-Cost, Long-Acting Contraception and Teenage Pregnancy. N Engl J Med. 2014;371(14):1316–1323. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hubacher D, Grimes DA. Noncontraceptive health benefits of intrauterine devices: a systematic review. Obstet Gynecol Surv. 2002;57(2):120–8. doi: 10.1097/00006254-200202000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Bryant AG, Stuart GS, Narasimhan S. Long-acting reversible contraceptive methods for adolescents with chronic medical problems. J Pediatr Adolesc Gynecol. 2012;25(6):347–51. doi: 10.1016/j.jpag.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Krajewski CM, Geetha D, Gomez-Lobo V. Contraceptive options for women with a history of solid-organ transplantation. Transplantation. 2013;95(10):1183–6. doi: 10.1097/TP.0b013e31827c64de. [DOI] [PubMed] [Google Scholar]
- 11.Cravioto MD, et al. Side effects unrelated to disease activity and acceptability of highly effective contraceptive methods in women with systemic lupus erythematosus: a randomized, clinical trial. Contraception. 2014;90(2):147–53. doi: 10.1016/j.contraception.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Cleland K, et al. Family planning as a cost-saving preventive health service. N Engl J Med. 2011;364(18):e37. doi: 10.1056/NEJMp1104373. [DOI] [PubMed] [Google Scholar]
- 13.Westhoff CL, et al. Pharmacokinetics and ovarian suppression during use of a contraceptive vaginal ring in normal-weight and obese women. Am J Obstet Gynecol. 2012;207(1):39, e1–6. doi: 10.1016/j.ajog.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization Global Database on Body Mass Index. 07/11/2013; Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 15.Centers for Disease Control and Prevention [October 2013];National Health and Nutrition Examination Survey. 2011 Available at: www.cdc.gov.
- 16.Sivin I, et al. Long-term contraception with the levonorgestrel 20 mcg/day (LNg 20) and the copper T 380Ag intrauterine devices: a five-year randomized study. Contraception. 1990;42(4):361–78. doi: 10.1016/0010-7824(90)90046-x. [DOI] [PubMed] [Google Scholar]
- 17.Andersson K, Odlind V, Rybo G. Levonorgestrel-releasing and copper-releasing (Nova T) IUDs during five years of use: a randomized comparative trial. Contraception. 1994;49(1):56–72. doi: 10.1016/0010-7824(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 18.Graesslin O, Korver T. The contraceptive efficacy of Implanon: a review of clinical trials and marketing experience. Eur J Contracept Reprod Health Care. 2008;13(Suppl 1):4–12. doi: 10.1080/13625180801942754. [DOI] [PubMed] [Google Scholar]
- 19.Huber J, Wenzl R. Pharmacokinetics of Implanon. An integrated analysis. Contraception. 1998;58(6 Suppl):85S–90S. doi: 10.1016/s0010-7824(98)00120-6. [DOI] [PubMed] [Google Scholar]
- 20.Croxatto HB, Makarainen L. The pharmacodynamics and efficacy of Implanon. An overview of the data. Contraception. 1998;58(6 Suppl):91S–97S. doi: 10.1016/s0010-7824(98)00118-8. [DOI] [PubMed] [Google Scholar]
- 21.Diaz S, et al. Clinical trial with 3-keto-desogestrel subdermal implants. Contraception. 1991;44(4):393–408. doi: 10.1016/0010-7824(91)90030-j. [DOI] [PubMed] [Google Scholar]
- 22.Kiriwat O, Patanayindee A, Koetsawang S, Korver T, Bennink HJ. A 4-year pilot study on the efficacy and safety of Implanon, a single-rod hormonal contraceptive implant, in healthy women in Thailand. Eur J Contracept Reprod Health CAre. 1998 Jun;3(2):85–91. doi: 10.3109/13625189809051409. [DOI] [PubMed] [Google Scholar]
- 23.Mornar S, et al. Pharmacokinetics of the etonogestrel contraceptive implant in obese women. Am J Obstet Gynecol. 2012;207(2):110, e1–6. doi: 10.1016/j.ajog.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Xu H, et al. Contraceptive failure rates of etonogestrel subdermal implants in overweight and obese women. Obstet Gynecol. 2012;120(1):21–6. doi: 10.1097/AOG.0b013e318259565a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flegal KM, et al. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 26.Rivera R, Yacobson I, Grimes D. The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices. Am J Obstet Gynecol. 1999;181(5 Pt 1):1263–9. doi: 10.1016/s0002-9378(99)70120-1. [DOI] [PubMed] [Google Scholar]
- 27.Sivin I, et al. Prolonged intrauterine contraception: a seven-year randomized study of the levonorgestrel 20 mcg/day (LNg 20) and the Copper T380 Ag IUDS. Contraception. 1991;44(5):473–80. doi: 10.1016/0010-7824(91)90149-a. [DOI] [PubMed] [Google Scholar]
- 28.Wu JP, Pickle S. Extended use of the intrauterine device: a literature review and recommendations for clinical practice. Contraception. 2014;89(6):495–503. doi: 10.1016/j.contraception.2014.02.011. [DOI] [PubMed] [Google Scholar]


