Abstract
The health impacts of exposure to summertime heat are a significant problem in New York City (NYC) and for many cities and are expected to increase with a warming climate. Most studies on heat-related mortality have examined risk factors at the municipal or regional scale and may have missed the intra-urban variation of vulnerability that might inform prevention strategies. We evaluated whether place-based characteristics (socioeconomic/demographic and health factors, as well as the built and biophysical environment) may be associated with greater risk of heat-related mortality for seniors during heat events in NYC. As a measure of relative vulnerability to heat, we used the natural cause mortality rate ratio among those aged 65 and over (MRR65+), comparing extremely hot days (maximum heat index 100 °F+) to all warm season days, across 1997–2006 for NYC's 59 Community Districts and 42 United Hospital Fund neighborhoods. Significant positive associations were found between the MRR65+ and neighborhood-level characteristics: poverty, poor housing conditions, lower rates of access to air-conditioning, impervious land cover, surface temperatures aggregated to the area-level, and seniors’ hypertension. Percent Black/African American and household poverty were strong negative predictors of seniors’ air conditioning access in multivariate regression analysis.
Keywords: Neighborhood characteristics, Vulnerability, Heat-related mortality, Health disparities, Housing quality
1. Introduction
The adverse health impacts of summertime heat are a signifi-cant problem in New York City (NYC) and many other cities around the world, and are expected to increase with a warming climate (Knowlton et al., 2007). Excessive exposure to high heat is associated with increased rates of heat stress, heat stroke, and premature death (O'Neill and Ebi, 2009). Heat-associated mortality typically presents as excess mortality due to cardiovascular or respiratory causes during hot weather (Hoshiko et al., 2010). As a result of extreme events such as the premature deaths of 14,800 people in France during the August 2003 heat wave (Observatoire régional de santé (ORS), 2003), awareness of heat-related mortality has increased. As cities create climate adaptation plans to protect vulnerable populations, understanding the causes of intra-urban spatial heterogeneity of these premature deaths should help identify locations and population groups at greatest risk while informing the search for modifiable exposures.
A number of studies have identified individual risk factors for vulnerability to heat waves. Those over 65 years of age and people with pre-existing cardiovascular and/or respiratory illnesses are especially vulnerable populations (Basu and Samet, 2002). Vulnerable populations also include young children, the obese, and those using medications that impede thermoregulation (New York City Department of Health and Mental Hygiene (NYCDOHMH), 2012).
There is also a growing understanding of the role of place in creating increased risk for heat-associated mortality. Analysis of mortality data in France indicates that deaths during the 2003 heat wave were disproportionately concentrated in poorer neighborhoods with higher levels of immigrants and substandard housing (Observatoire régional de santé (ORS), 2003). People at elevated risk of mortality during a Chicago heat wave in 1995, which led to more than 700 excess deaths, included the elderly, the poor, those with limited mobility and little social contact, and those with pre-existing medical or psychiatric conditions, as well as those with place-based risk factors such as poor access to public transportation or air-conditioned neighborhood places (Klinenberg, 2002; O'Neill and Ebi, 2009; Semenza et al., 1996). Risk of mortality in that event was higher in the Black community; for people living in certain types of low income and multi-tenant housing, such as single-room occupancy apartment buildings; and for those living on the top floors of buildings (Klinenberg, 2002; Semenza et al., 1996). Access to and use of home air conditioning was protective against heat-related death and risk of heat stroke in four U.S. cities (O'Neill et al., 2005; Semenza et al., 1996). Black residents of these cities had one-half the access to home air conditioning as other racial/ethnic groups, and a higher risk of heat-mortality (O'Neill et al., 2005).
In New York, as in other cities, summertime heat can lead to elevated mortality and morbidity rates, especially during the extended periods of hot weather (Basu and Samet, 2002; Braga et al., 2002; Ellis et al., 1975; Kalkstein and Greene, 1997; Marmor, 1975; McGeehin and Mirabelli, 2001). In NYC, the effects of temperature on mortality were observable above a threshold temperature range, with a minimum mortality temperature of approximately 66.4 °F (Curriero et al., 2002; O'Neill and Ebi, 2009). In a study of the daily variation in warm season natural-cause mortality for 1997–2006 in New York City, Metzger et al. (2010) found that the same-day maximum heat index (HI) was linearly related to mortality risk across its range. Heat waves in July and August 2006 in NYC were associated with 46 confirmed heat stroke deaths within the city, with a greater proportion in Queens neighborhoods (New York City Department of Health and Mental Hygiene (NYCDOHMH), 2006). Additionally, approximately 100 excess deaths occurred during the July 27-August 5, 2006 heat wave, an 8% increase over the average daily death rate (New York City Department of Health and Mental Hygiene (NYCDOHMH), 2006). Chronic diseases such as cardiovascular disease, mental health disorders and obesity were common comorbidities in heat illness and deaths in NYC between 2000 and 2011 (Centers for Disease Control and Prevention (CDC), 2013). Among hyperthermia deaths with information available, none of the deceased had used a working air conditioner (Ibid.). “Rates of heat illness and death increased with age, were typically higher among males than females for those aged <65 years, and increased with neighborhood poverty” and the homeless were at greater risk for heat-related mortality and illness (Centers for Disease Control and Prevention (CDC), 2013, p. 618).
These health effects could worsen during the 21st century due to a changing climate. Temperature projections for the NYC metropolitan region using a global-to-regional climate modeling system and two greenhouse gas emissions scenarios, A2 and B2, yielded a mean increase of 70% in heat-related mortality rates by the 2050s within the region compared to the 1990s (Knowlton et al., 2007). A net increase in annual temperature-related deaths of 15.5–31% was estimated for Manhattan, New York, in the 2080s as compared with the 1980s, as increases in heat-related mortality outweighed reductions in cold-related mortality using the B1 and A2 emissions scenarios and 16 downscaled global climate models (Li et al., 2013).
Research suggests that the physical and social characteristics of neighborhoods are important for understanding the spatial and social distribution and variability of heat-related mortality within cities (Clarke, 1972; Harlan et al., 2006, 2013; Klinenberg, 2002; Smoyer, 1998). The urban heat island effect, which leads to higher surface and near-surface air temperatures in dense urban areas than surrounding suburban and rural areas, may increase the health effects of summer temperatures, as micro-urban temperature variation and elevated nighttime temperatures increase exposure to heat for those without air conditioning and increase the risk of heat-related disease and mortality (Patz et al., 2005; Smargiassi et al., 2009; Uejio et al., 2011).
Heat island intensity is spatially heterogeneous in urban landscapes, so that some areas may be significantly cooler than others during a heat wave (Harlan et al., 2006; Smoyer, 1998). The thermal environment (microclimates) within cities varies because of physical layout and urban design, land use mix, and vegetative cover and street trees (Hart and Sailor, 2008; Slosberg et al., 2006). Hart and Sailor (2008) found that roadway area density was an important determinant of local heat island magnitudes for Portland, Oregon, while the main factor distinguishing warmer from cooler areas in the Portland metropolitan region was tree canopy cover. Using thermal infrared data derived from Landsat imagery, Slosberg et al. (2006) found that spatial variability in NYC's surface temperatures was most associated with changes in albedo and a measure of vegetation coverage, the Normalized Difference Vegetation Index (NDVI). The association between the thermal environment of neighborhoods and demographic risk factors for heat-related health effects was found to be significant in the city of Phoenix, where “lower socioeconomic and ethnic minority groups were more likely to live in warmer neighborhoods with greater exposure to heat stress” (Harlan et al., 2006). Jesdale et al. (2013) found that non-Hispanic Blacks, non-Hispanic Asians and Hispanics were more likely than non-Hispanic Whites to live in block groups with heat risk-related land cover (HRRLC), where at least half the population “experienced the absence of tree canopy and at least half of the ground was covered by impervious surface” (p. 811).
Although temperature varies within cities in ways relevant for heat exposures, little is known in NYC about how this affects health outcomes. Because this knowledge may suggest possible interventions to reduce heat-associated health problems, we examined the relationship between characteristics described at the neighborhood scale, including biophysical, demographic and population health characteristics, and heat-related mortality rates within New York City.
1.1. Place and health
The conceptual basis for this research is located in the growing body of scholarship examining the influence of place-based characteristics and context on population health. For much of the post-World War II period, environmental health research focused on understanding the individual-level risk factors and their associated biological mechanisms that may lead to disease causation and disparities in mortality rates (Corburn et al., 2006; Diez Roux, 2001; Schwartz, 1994). More recently, recognition of the effects of place as a determinant of the distribution of health outcomes has increased. Researchers from medicine, epidemiology and the social sciences are increasingly interested in understanding the cumulative effects of the spatial clustering of physical and psychosocial hazards often experienced in low-income neighborhoods and communities of color (Bullard, 1990; Corburn et al., 2006; Northridge et al., 2003).
The impacts of neighborhood conditions on population health are important and should be analyzed to target climate adaptation strategies (Rosenthal et al., 2007). Health researchers have theorized that neighborhood conditions and characteristics may exert an effect on health through influence on behaviors, such as risk-taking and levels of physical activity, or by acting to modify the influence of environmental exposures on individual-level health, through impacts on individual stress and the immune system (Clougherty and Kubzansky, 2009). Examining a range of models for how neighborhoods may influence health outcomes, Ellen et al. (2001) summarized four main pathways for these effects: (1) the availability of neighborhood institutions and resources; (2) stresses in the physical environment; (3) stresses in the social environment; and (4) impacts on neighborhood-based networks and norms. In New York City, neighborhood built environments and urban design characteristics may create hotter microclimates that enhance heat exposures, while creating more or less inviting streetscapes that may also influence exposures and behaviors.
Health and social science researchers frequently use ecological analysis, in which populations or groups are the units of analysis, rather than individuals, to examine determinants of population health (Kawachi et al., 1997; Krieger et al., 1997; McLaughlin Centre for Population Health Risk Assessment, 2012; Susser, 1994). This study uses both aggregate population health data and data on community properties to examine their association with the temperature–mortality relationship in New York City
2. Methods
We evaluated the spatial association between independent variables that describe neighborhood-scale characteristics (socioeconomic, demographic, the built and biophysical environment, health status and risk behaviors) and senior citizens’ rates of excess deaths during heat events in New York City.
As a measure of relative vulnerability to heat, we used the natural cause mortality rate ratio among those aged 65+ (MRR65+), comparing the natural deaths rate (per days) on extremely hot days (maximum heat index 100 °F+) to the natural deaths rate on all days in the warm season between May and September. Data were pooled across the years 1997–2006 at the neighborhood-level.
3. Data
3.1. Neighborhood boundaries
The administrative boundaries of NYC's Community Districts (CDs) and United Hospital Fund (UHF) areas are used as proxies for neighborhoods in this study; they are the levels at which the spatially-disaggregated data necessary are available. Other studies on the effect of the built environment on health outcomes in NYC have used the census tract as the spatial unit of analysis (Rundle et al., 2007); that approach was not possible for this study due to data instability caused by the relatively small number of death counts at that finer-scale. Despite this limitation and the heterogeneity within these areas, the places and populations contained within Community Districts and UHF areas often share common histories, built environments and socio-economic characteristics, and their use in ecological analysis is a much finer scale of spatial disaggregation compared with previous ecological studies that used either NYC or the metropolitan region as the reference spatial unit. There are 42 United Hospital Fund designated neighborhoods in the city, defined by several adjoining zip codes, and 59 Community Districts. We used both types of geographic areas because each has different covariates available for analysis.
3.2. Mortality data
The dependent variable in this analysis is a measure of the relative risk of mortality by seniors aged 65 and older on very hot days. Daily counts of natural cause deaths at the census tract level for persons age 65 and over from May through September for the period 1997 through 2006 were obtained by the NYC Department of Health and Mental Hygiene Office of Vital Statistics. We aggregated total mortality counts at the Community District (CD) and United Hospital Fund (UHF) area levels for all days when the maximum heat index was 100 °F or above (very hot days) and also for all other days during this time period. We calculated the mortality rate ratio by dividing the natural deaths rate on extremely hot days (maximum heat index 100 °F+) by the natural deaths rate on all warm season days (May 1–Sept. 30th) for each neighborhood area.
The heat index (HI), or apparent temperature, is a measure that combines relative humidity and ambient temperature (Steadman, 1979). This analysis used the same meteorological data set developed by Metzger et al. (2010). Hourly meteorological data from the National Climatic Data Center were obtained for the three New York City stations located at Central Park, La Guardia airport, and John F. Kennedy airport for 1997–2006. Meteorological data from La Guardia airport was used because it had the most complete records during the study period (Metzger et al., 2010). The heat index (HI) was calculated using ambient temperature (F) and relative humidity (%) for ambient temperature of < or = 80 °F and relative humidity of < or 40% (Metzger et al., 2010). There were 49 days during the reference time period where the HI equaled 100 °F or above. The total reference period of the entire May–September warm seasons during the study period is 1530 days.
Associations of the mortality rate ratios (MRR65+) with the vulnerability factors described below were evaluated.
3.3. Vulnerability factors
A range of neighborhood-level characteristics that might influence the risk of heat-related mortality during excessively warm days was examined. An inventory of over 30 independent variables was derived from the substantial literature documenting the public health effects of excess heat in the epidemiology, sociology, urban climate and urban planning fields. These were categorized into three main groups: (1) demographic and area-level socioeconomic status and (2) health risk characteristics describing neighborhood-level prevalence of health conditions (e.g., diabetes, obesity, hyper-tension) and risk characteristics (e.g., living alone, being at risk for social isolation), in Tables 1 and 3 factors in the built environment (housing conditions and land-use) and characteristics describing the neighborhood's biophysical environment, in Table 2. These characteristics were used as the independent variables in linear regression and correlation analysis with the neighborhood-level mortality rate ratio (MRR65+), described above. The correlat ions between independent variables and MRR65+ are shown in Tables 1 and 2, along with the source of the data.
Table 1.
Pearson's correlation of neighborhood-level characteristics with the mortality rate ratio (MRR65+), a measure of seniors (age 65 +) vulnerability to heat-related mortality in New York City, 1997-2006.
| Characteristics | |||||
|---|---|---|---|---|---|
| Demographic and socioeconomic status | Pearson's |
95% CI Lower, upper | Data | ||
| Scale | r | p-Value | |||
| Seniors (age 65 + ) living alone (percent of households) | CD | –0.074 | 0.578 | (–0.323, 0.185) | b |
| Total population below poverty rate | CD | 0.255 | 0.051* | (–0.001, 0.479) | b c |
| UHF | 0.395 | 0.01a | (0.104, 0.624) | ||
| Median household income | CD | –0.213 | 0.106 | (–0.444, 0.045) | b c |
| Mean household income | UHF | –0.288 | 0.064* | (–0.544, 0.017) | b c |
| Educational attainment | |||||
| Percent high school graduate and above | CD | –0.245 | 0.062* | (–0.471, 0.011) | b c |
| Percent no high school diploma | UHF | 0.255 | 0.103 | (–0.053, 0.518) | b c |
| Neighborhood racial/ethnic composition | |||||
| Percent Black/African-American | CD | 0.117 | 0.377 | (–0.143, 0.362) | b |
| UHF | 0.162 | 0.305 | (–0.149, 0.444) | ||
| Percent White | CD | –0.122 | 0.36 | (–0.366, 0.138) | b |
| UHF | –0.238 | 0.129 | (–0.505, 0.071) | ||
| Percent Hispanic (all races) | CD | 0.161 | 0.222 | (–0.099, 0.40) | b |
| UHF | 0.260 | 0.096* | (–0.047, 0.522) | ||
| Percent Asian | CD | –0.305 | 0.019 a | (–0.52, –0.054) | b |
| UHF | –0.232 | 0.096* | (–0.5, 0.077) | ||
| Percent non-White | UHF | 0.238 | 0.129 | (–0.071, 0.505) | c |
| Measures of possible social and/or cultural isolation | |||||
| Percent of households with no phone service | CD | 0.21 | 0.11 | (–0.048, 0.442) | b |
| Health and risk characteristics | |||||
| Percent age 65+ reporting hypertension diagnosis | UHF | 0.308 | 0.047a | (0.005, 0.559) | d |
| Percent age 65 + with diabetes | UHF | 0.281 | 0.071* | (–0.023, 0.539) | d |
| Percent age 45 + at risk for social isolation | UHF | 0.234 | 0.135 | (–0.074, 0.502) | d |
| Percent age 65 + living alone | UHF | 0.082 | 0.608 | (–0.228, 0.376) | d |
| Percent age 65 + with self-reported general health status of fair/poor | UHF | 0.102 | 0.52 | (0.208, 0.393) | d |
| Percent obese all ages (BMI ≥ ≥ 30) | UHF | 0.176 | 0.266 | (–0.135, 0.455) | d |
| Proportion current asthmatics all ages | UHF | –0.088 | 0.58 | (–0.381, 0.221) | d |
| Percent with frequent mental distress (all ages) | UHF | 0.039 | 0.806 | (–0.268, 0.338) | d |
Notes: Variables are at the Community District (CD, n=59) and United Hospital Fund (UHF, n=42) level.
Significant at p < 0.10.
Significant at p < 0.05.
Census 2000 from NYC DCP.
Census 2000 from NYC DOHMH.
NYC DOHMH Community Health Survey 2007 (CHS).
Table 3.
Mortality counts and hot days in New York City, 1997-2006.
| Event | Frequency |
|---|---|
| Average year-round natural cause deaths/day, all ages | ≈ 145 |
| Average warm-season natural-cause deaths/day for age 65+a | ≈ 95 (95.5) |
| Average natural-cause deaths/day for age 65 + on very hot daysa,b | ≈ 100 (100.3) |
| Total warm-season natural-cause deaths, 1997-2006, for New York City | ≈ 150,000 |
| Average by Community District for the warm season, 1997-2006 | 2531 (SD 1134) |
Difference between the average warm-season and very hot day natural-cause deaths/day for age 65+ is significant at p-value=0.0015 (t-test for paired samples; t-observed value = –3.396).
Heat index ≥ 100 °F.
Table 2.
Pearson's correlation of neighborhood characteristics with intra-urban mortality rate ratios (MRR65+); built and biophysical environment variables used in the study
| Characteristics | |||||
|---|---|---|---|---|---|
| Housing conditions: | Pearson's |
95% CI |
|||
| Scale | r | p-Value | Lower, upper | Data | |
| Percent 65 + who own and use AC | UHF | –0.341 | 0.027 | (–0.584, –0.042) | a |
| Rate of total housing violations, 2000 | CD | 0.237 | 0.071* | (–0.02, 0.464) | b |
| Rate of total housing violations, 2000-2005 | CD | 0.302 | 0.02 | (0.05, 0.518) | b |
| Rate of serious housing violations, 2000-2005 | CD | 0.323 | 0.013 | (0.073, 0.534) | c |
| Rate of property tax delinquencies, 2005 | CD | 0.38 | 0.003 | (0.138, 0.579) | c |
| Rate of property tax delinquencies, five-year mean | CD | 0.334 | 0.01 | (0.086, 0.543) | d |
| Percent of households in dilapidated or deteriorating residential buildings, 2002 | UHF | 0.257 | 0.1* | (–0.05, 0.52) | b |
| Percent homes near structures rated good or excellent, 2002 & 2005 two-year mean | UHF | –0.409 | 0.007 | (–0.634, –0.12) | b |
| Housing stock and land use | |||||
| Percent of housing stock that is rent- stabilized units, 2002 | CD | 0.249 | 0.064* | (–0.014, 0.48) | b |
| Percentage of housing stock that is public housing, 2002 | CD | 0.086 | 0.517 | (–0.173, 0.334) | b |
| Percent vacant housing units | CD | 0.189 | 0.152 | (–0.07, 0.424) | |
| Percent owner-occupied housing units | UHF | –0.413 | 0.007 | (–0.636, –0.125) | e |
| CD | –0.207 | 0.116 | (–0.439, 0.051) | ||
| Population density | CD | 0.177 | 0.180 | (–0.082, 0.414) | e |
| Percent of residential buildings that are walk-ups | CD | 0.126 | 0.342 | (–0.134, 0.37) | f |
| Land cover | |||||
| Vegetated land cover as percent of residential tax lots (outlier 208 removed) | CD | –0.061 | 0.649 | (–0.312, 0.198) | g |
| Vegetated land cover (trees and grass) as percent of land area | UHF | –0.219 | 0.163 | (–0.49, 0.09) | g |
| CD | –0.041 | 0.758 | (–0.293, 0.217) | ||
| Trees as percent of total land cover (outliers UHF 101 and CD 208 removed) | UHF | –0.216 | 0.175 | (–0.491, 0.098) | |
| CD | –0.062 | 0.646 | (–0.313, 0.197) | g | |
| Percent impervious of total land cover | UHF | 0.237 | 0.131 | (–0.072, 0.504) | |
| Percent impervious of total land cover (outlier UHF 101 removed) | UHF | 0.3 | 0.057* | (–0.008, 0.556) | g |
| Remotely sensed surface temperature/surface urban heat island | |||||
| Landsat 7: August 14, 2002 (daytime) | UHF | 0.225 | 0.152 | (–0.084, 0.495) | h |
| CD | 0.115 | 0.386 | (–0.145, 0.36) | ||
| Landsat 7: September 8, 2002 (daytime) | UHF | 0.224 | 0.154 | (–0.085, 0.494) | h |
| CD | 0.109 | 0.411 | (–0.151, 0.355) | ||
| Landsat 7: September 8, 2002 (outlier UHF 101 removed) | UHF | 0.302 | 0.055* | (–0.002, 0.554) | h |
| CD | 0.152 | 0.255 | (–0.108, 0.392) | ||
Bolded variables significant at p < 0.05.
Significant at p < 0.10.
NYC DOHMH Community Health Survey (CHS), 2007, access to air conditioning (AC).
NYC Housing and Vacancy Survey (HVS).
NYC Department of Housing Preservation and Development (HPD).
NYC Department of Finance.
Census 2000, NYC Department of City Planning (DCP).
NYC Dept. of City Planning (DCP), PLUTO dataset 2003.
US Forest Service, Northeastern Research Station, EMERGE dataset, 2001-2002.
NASA Goddard Institute for Space Studies (NASA GISS), Landsat 7 data.
Sources for these data were the 2000 US Census, the New York City Department of Health and Mental Hygiene (NYCDOHMH), the New York City Department of City Planning (DCP), the New York City Department of Housing Preservation & Development (HPD), the New York City Department of Finance, the United States Forest Service (USFS), and the National Aeronautics and Space Administration (NASA). A geographic information system (GIS) for NYC was created, with layers corresponding to each of the independent variables used in the analysis. Surface temperatures derived from NASA's Landsat 7 ETM thermal data were averaged to the Community District and UHF-neighborhood level.
3.4. Analysis
Bivariate and multivariate ordinary least squares (OLS) linear regression was used to assess the relationships between the mortality rate ratio (MRR65+) and the vulnerability measures noted above and listed in Tables 1 and 2. First, bivariate relationships between the mortality rate ratios and each of the candidate variables were analyzed through OLS linear regression. Correlations between explanatory variables were also assessed using Pearson's correlation coefficient to identify groups of variables tending to capture the same phenomena. For example, the percent of population in poverty and measures of educational attainment (e.g., percent adults without a high school diploma) are so strongly correlated (r = 0.89) at the neighborhood scale in New York City that it does not make sense to include both variables in multivariate modeling.
The Pearson's r correlations between independent variables and the bivariate regression models (R-squared values) were used to select among the correlated metrics of similar factors for use in multivariate linear OLS regression. An examination of the statistical significance of the variables in bivariate analysis with the mortality rate ratios (MRR65+) was part of the selection process, including all of the categories (e.g., demographic, biophysical, built environment).
The variables significant at p<0.10 in bivariate analyses (or close to p<0.10; we did not use a strict cut-off value) were tested in multivariate linear OLS regression. Our variable selection was also informed by our interest in evaluation of biophysical predictors such as surface temperatures as well as other landscape characteristics that represent possible (known or unknown) vulnerability factors for heat-related mortality that are also potentially amenable to public intervention to reduce health impacts. Although it has been long asserted that the temperatures of the impervious streets and urban canyons of NYC's neighborhoods could result in unhealthy exposures to heat during extreme heat events (Clarke, 1972; Marmor, 1975), the relationship between surface temperatures and the distribution of heat-related mortality within New York City had not been tested prior to this analysis. The ecological scale of our study required converting Landsat-derived thermal infrared data to estimated land surface temperatures, and then aggregating these data through averaging the finer-scale (60 m) raster data to the CD and UHF-level. High-resolution data (3-foot pixels) from the analysis of NYC's land cover by the USFS, also averaged to the Community District and UHF-neighborhood scale, enabled us to test relationships between vegetative (tree and grass cover) and impervious surface cover with the mortality rate ratios.
Along with the search for statistical significance and the avoidance of excessive collinearity, we sought to identify predictors of vulnerability to premature death during heat events in NYC at the ecological scale, and develop and use new methods of geospatial analysis of the urban thermal environment, while providing guidance, methods and findings for further finer-scale vulnerability research and policy interventions. Regression analysis proceeded in a stepwise fashion, testing variables as described above as predictors of the mortality rate ratios and eliminating models that did not achieve significance at p<0.10 or very close to it. Analysis of the independent variables with the mortality rate ratios, MRR65+, is summarized in Tables 1, 2 and 4.
Table 4.
Mortality rate ratio (MRR65+) models: ordinary least squares (OLS) linear regression.
| Predictor variables | R 2 | Adj. R2 | Pr > F |
Unstandardized coefficient
|
Standardized coefficient
|
t | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| B | Std. Error of B | 95% CI for B (lower, upper) | β | 95% CI for β (lower, upper) | ||||||
| UHF-neighborhood models | ||||||||||
| 1. Homeownership (percent) | 0.17 | 0.15 | 0.007 | –0.003 | 0.001 | (–0.004, –0.001) | –0.413 | (–0.704, –0.122) | –2.87 | 0.007 |
| 2. Deteriorating or dilapidated buildingsa | 0.159 | 0.138 | 0.01 | 0.013 | 0.005 | (0.003, 0.023) | 0.399 | (0.102, 0.696) | 2.72 | 0.01 |
| 3. Percent below poverty | 0.156 | 0.135 | 0.01 | 0.004 | 0.002 | (0.001, 0.007) | 0.395 | (0101, 0.688) | 2.72 | 0.01 |
| 4. Impervious coverb | 0.23 | 0.186 | 0.008 | 0.003 | 0.001 | (0.0005, 0.006) | 0.346 | (0.054, 0.637) | 2.4 | 0.021 |
| Hypertensionb | 0.004 | 0.0016 | (0.001, 0.007) | 0.376 | (0.085, 0.668) | 2.613 | 0.013 | |||
| 5. Air conditioning access, age 65 + | 0.117 | 0.094 | 0.027 | –0.004 | 0.002 | (–0.008, –0.001) | –0.341 | (–0.642, –0.041) | –2.3 | 0.027 |
| 6. Homes near structures rated good or excellent | 0.168 | 0.147 | 0.007 | –0.003 | 0.001 | (–0.006, –0.001) | –0.409 | (–0.701, –0.118) | –2.838 | 0.007 |
| Community District models | ||||||||||
| 1. Property tax delinquenciesc | 0.112 | 0.096 | 0.01 | 0.01 | 0.004 | (0.003, 0.018) | 0.334 | (0.084, 0.584) | 2.677 | 0.01 |
| 2. Serious housing violationsd | 0.104 | 0.089 | 0.013 | 0.001 | 0.0005 | (0.0003, 0.002) | 0.323 | (0.156, 0.830) | 2.577 | 0.013 |
| 3. Percent below poverty | 0.065 | 0.049 | 0.051 | 0.003 | 0.001 | (0.00, 0.006) | 0.255 | (–0.001, 0.511) | 1.991 | 0.051 |
| 4. Percent Asian population | 0.093 | 0.077 | 0.019 | –0.005 | 0.002 | (–0.008, –0.001) | –0.305 | (–0.558, –0.053) | –2.422 | 0.019 |
Note: N=42 UHF-neighborhoods and 59 Community Districts. The dependent variable is the mortality rate ratio for age 65 + (MRR65+).
Percent of households, 2002; influential point UHF 501 removed (Port Richmond, Staten Island).
Influential point UHF 101 removed (Kingsbridge-Riverdale, the Bronx).
Five-year mean, 2000-2003 and 2006. The share of 1-3 residential unit properties (Tax Class 1) with over $500 in unpaid property tax.
Six-year mean, 2000-2005. The number of class C (immediately hazardous) housing code violations issued by the NYC HPD per 1,000 rental units.
To assess the interaction and effect modification of income and neighborhood poverty rates, which are fundamental characteristics used to describe population vulnerability to climate variability hazards, we also stratified bivariate analyses by rates of neighborhood poverty and income measures (Cutter et al., 2009; Fothergill and Peek, 2004). Community Districts (CDs) were stratified into two groups, above and below the average of the median household income for 59 CDs, and UHF-areas were stratified into two groups, above and below the average proportion of population poverty in UHF-areas, for use in OLS linear regression analysis with the mortality rate ratio as the dependent variable, based on the factors described above. The results are described below.
We were also interested in examining relationships between characteristics that may increase the risk of heat-related mortality: air conditioning access and the urban heat island effect, expressed here as area-based surface temperatures, with other neighborhood-scale characteristics. We used multivariate OLS linear and spatial error and spatial lag regression to analyze the neighborhood-level predictors of these characteristics, using rates of air conditioning access for seniors and area-based measures of surface temperatures as dependent variables, with sociodemo-graphic, built environment, and biophysical characteristics as predictors. These analyses are summarized in Tables 6 and 7 and discussed below.
Table 6.
Neighborhood (UHF-area) predictors for access to home air conditioning, age 65 and older: ordinary least squares (OLS) and spatial regression.
| Predictors | Model 1 |
Model 2 |
Model 3–spatial lag model |
|||
|---|---|---|---|---|---|---|
| Standardized coefficients t | Lower and upper bound (95% CI) | Standardized coefficients t | Lower and upper bound (95% CI) | Unstandardized coefficients z-Value | Lower and upper bound (95% CI) | |
| Socioeconomic status | ||||||
| Percent below poverty | –0.528*** (–4.597) | –0.760 –0.295 |
||||
| Homeownership | 0.446*** (3.891) | 0.214 0.677 |
||||
| Built environment | ||||||
| Percent of households near boarded-up buildings | –0.366*** –4.389 |
–0.534 –0.198 |
||||
| W_AC65a | 0.132* 2.028 |
0.000 0.263 |
||||
| Race/ethnicity | ||||||
| Black/African American | –0.368** (–3.203) | –0.6 –0.135 |
–0.484*** (–4.231) | –0.716 –0.253 |
||
| Percent non-White | –0.112** –2.85 |
–0.191 –0.033 |
||||
| Adjusted R-squared | 0.528 | 0.476 | 0.601b | |||
Notes: The dependent variable is access to home air conditioning, age 65 + by UHF areas, 2007. No spatial autocorrelation was observed in Model 1 and 2. Significant spatial dependence was observed in Model 3's Robust LM (lag), and a spatial lag model was used to address spatial correlation and bias.The constant in Model 3 is 82.437, with an SE of 5.871, z-value of 13.04 and p=0.000.
p < 0.05.
p < 0.01.
p< 0.0001.
Spatial autoregressive parameter.
Pseudo R-squared.
Table 7.
Spatial models for New York City's land surface temperature: Standardized coefficients, z-values and 95% Confidence Intervals (CI).
| UHF Neighborhoods | Coeff. | SE | z-Value | p Value | 95% CI | Pseudo R-Squared |
|---|---|---|---|---|---|---|
| Model 1: 8/14/02 | ||||||
| Spatial lag modela | 0.752 | |||||
| Pct below 200% of poverty | 0.201 | 0.026 | 7.658 | 0.000 | (0.148, 0.254) | |
| Pct home ownership | 0.134 | 0.028 | 4.810 | 0.000 | (0.077, 0.191) | |
| Impervious cover | 0.156 | 0.026 | 5.899 | 0.000 | (0.103, 0.209) | |
| W_AUG_14a | 0.086 | 0.015 | 5.779 | 0.000 | (0.056, 0.116) | |
| Model 2: 9/8/2002 | ||||||
| Spatial error model b | 0.875 | |||||
| Constant | 87.878 | 0.971 | 90.519 | 0.000 | (85.911, 89.845) | |
| Mean household income | –3.85E–05 | 0.000 | –4.647 | 0.000 | (0.000, 0.000) | |
| Impervious cover | 0.112 | 0.011 | 10.598 | 0.000 | (0.090, 0.134) | |
| Pct Black/African American | 0.019 | 0.005 | 3.551 | 0.000 | (0.009, 0.029) | |
| Lambda | ||||||
| Community Districts (CD) | ||||||
| Model 1: 9/8/02 | ||||||
| Spatial error model c | 0.86 | |||||
| Constant | 89.524 | 0.883 | 101.376 | 0.000 | (87.754, 91.294) | |
| Impervious cover | 0.104 | 0.010 | 10.346 | 0.000 | (0.084, 0.124) | |
| Mean household income | –4.94E–05 | 7.29E – 06 | –6.778 | 0.000 | (0.000, 0.000) | |
| Pct Black/African American | 0.017 | 0.004 | 3.734 | 0.000 | (0.009, 0.025) | |
| Lambda | 0.806 | 0.058 | 13.964 | 0.000 | (0.690, 0.922) | |
| Model 2: 7/22/2002 | ||||||
| Spatial error model d | 0.823 | |||||
| Constant | 93.901 | 1.171 | 80.158 | 0.000 | (91.553, 96.249) | |
| Impervious cover | 0.128 | 0.015 | 8.317 | 0.000 | (0.098, 0.158) | |
| Percent below poverty | 0.084 | 0.017 | 4.977 | 0.000 | (0.050, 0.118) | |
| Pct Black/African American | 0.024 | 0.007 | 3.609 | 0.000 | (0.010, 0.038) | |
| Lambda | 0.795 | 0.060 | 13.175 | 0.000 | (0.675, 0.915) | |
| Model 3: 7/22/2002 | ||||||
| Spatial error model e | 0.844 | |||||
| Constant | 93.866 | 1.133 | 82.807 | 0.000 | (91.593, 96.138) | |
| Percent below poverty | 0.083 | 0.016 | 5.208 | 0.000 | (0.051, 0.115) | |
| Impervious cover | 0.12 | 0.015 | 8.071 | 0.000 | (0.090, 0.150) | |
| Pct Black/African American | 0.025 | 0.006 | 3.908 | 0.000 | (0.013, 0.037) | |
| Population density | 0.00003499 | 1.497E–05 | 2.338 | 0.019 | (0.000, 0.000) | |
| Lambda | 0.833 | 0.051 | 16.352 | 0.000 | (0.731, 0.935) | |
| Model 4: 8/14/02 | ||||||
| Spatial error model f | 0.859 | |||||
| Constant | 93.654 | 1.857 | 50.426 | 0.000 | (89.931, 97.377) | |
| Impervious cover | 0.141 | 0.019 | 7.467 | 0.000 | (0.103, 0.179) | |
| Percent below poverty | 0.092 | 0.029 | 3.161 | 0.002 | (0.034, 0.150) | |
| Percent White | –0.025 | 0.011 | –2.202 | 0.028 | (–0.047, –0.003) | |
| Lambda | 0.951 | 0.017 | 56.213 | 0.000 | (0.917, 0.985) | |
| Model 5: 7/22/2002 | ||||||
| Spatial error model g | 0.828 | |||||
| Constant | 111.238 | 0.795 | 139.930 | 0.000 | (109.644, 112.832) | |
| Pct of CD covered by trees, grass and vegetation | –0.138 | 0.016 | –8.769 | 0.000 | (–0.170, –0.106) | |
| Mean household income | –6.71E – 05 | 0.0000107 | –6.267 | 0.000 | (0.000, 0.000) | |
| Pct Black/African American | 0.023 | 0.007 | 3.525 | 0.000 | (0.009, 0.037) | |
| Lambda | 0.778 | 0.064 | 12.076 | 0.000 | (0.650, 0.906) |
Notes: The dependent variable is the mean daytime surface temperature measured by Landsat 7, averaged to the Community District and UHF-level. Data sources for the independent variables noted in Tables 1 and 2.
Log Likelihood = –80.569; AIC=171.138; Breush-Pagan test (p-value)=0.409. W_AUG_14 is the spatial autoregressive coefficient.
Log Likelihood = –46.273; AIC=100.547; Breush-Pagan test (p-value)=0.84. Lambda is the spatial autoregressive parameter for spatial error models.
Log Likelihood = –64.565; AIC= 137.131; Breush-Pagan test (p-value)=0.854.
Log Likelihood = –87.774; AIC=183.548; Breush-Pagan test (p-value)=0.220.
Log Likelihood = –85.352; AIC=180.704; Breush-Pagan test (p-value)=0.740.
Log Likelihood =–109.088; AIC=226.176; Breush-Pagan test (p-value) = 0.197.
Log Likelihood = –86.462; AIC=180.924; Breush-Pagan test (p-value)=0.798.
The variables used for regression models were assessed for multicollinearity through measures of VIF and Tolerance. All individual variables in the models had a VIF<5 (the majority VIF<2; in multiple regression models, the mean VIF<2) and an acceptable Tolerance >0.50. The use of highly correlated variables in multivariate regression models (e.g., a Pearson's r of over about 0.60–0.70) was avoided. Given the high collinearity of many sociodemo-graphic, built environment and biophysical predictors, the majority of the mortality rate ratio models have only one independent variable, while the air conditioning and surface temperature models include multiple predictors. We report here only models whose predictors are statistically significant at p<0.05 or close to it.3
4. Results
All-cause mortality of seniors aged 65 and over increased significantly in New York City during extremely hot days (HI≥100 °F) from 1997 to 2006 (p=0.001). For 59 Community Districts (CDs), the mortality rate ratio (MRR65+) had a mean weighted by senior population of 1.0479 (95% confidence interval, 1.021, 1.090). For 42 UHF areas, the MRR65+ had a mean weighted by senior population of 1.0464 (95% confidence interval, 1.016, 1.085). Citywide there were over 4% more deaths on days with a Heat Index equal to or above 100 1F compared to all other warm season days from 1997 to 2006. This finding is consistent with other studies that have found excess mortality during high heat days (Hoshiko et al., 2010; Metzger et al., 2010; New York City Department of Health and Mental Hygiene (NYCDOHMH), 2006; Semenza et al., 1996).
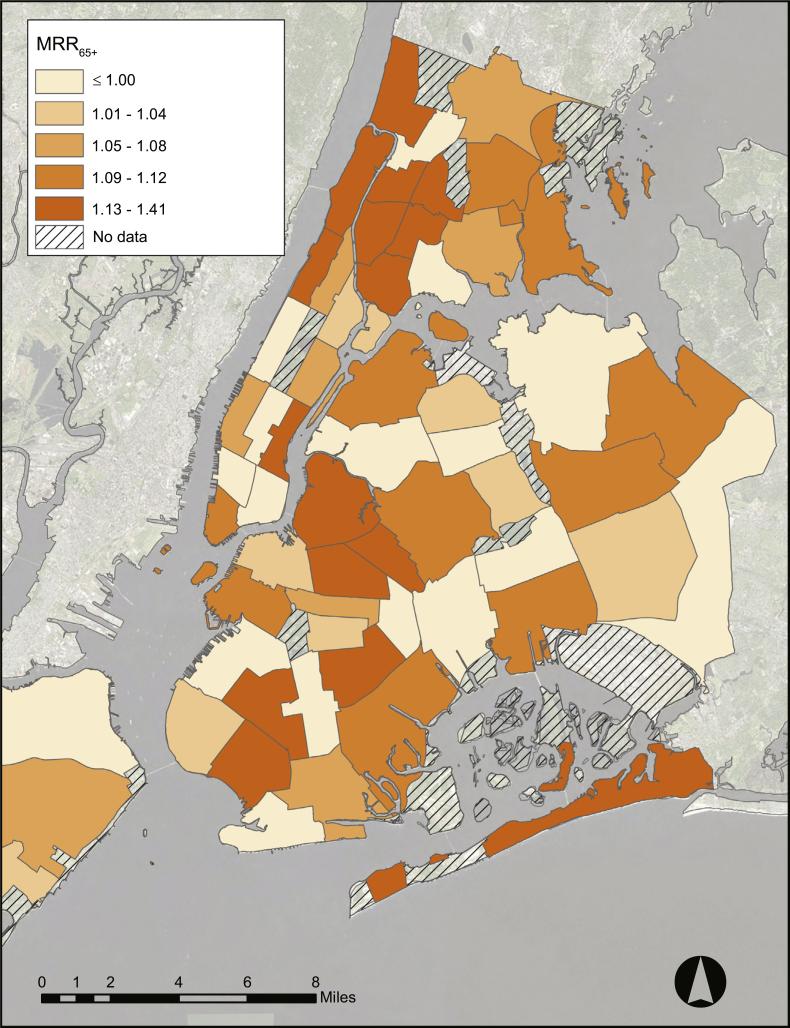
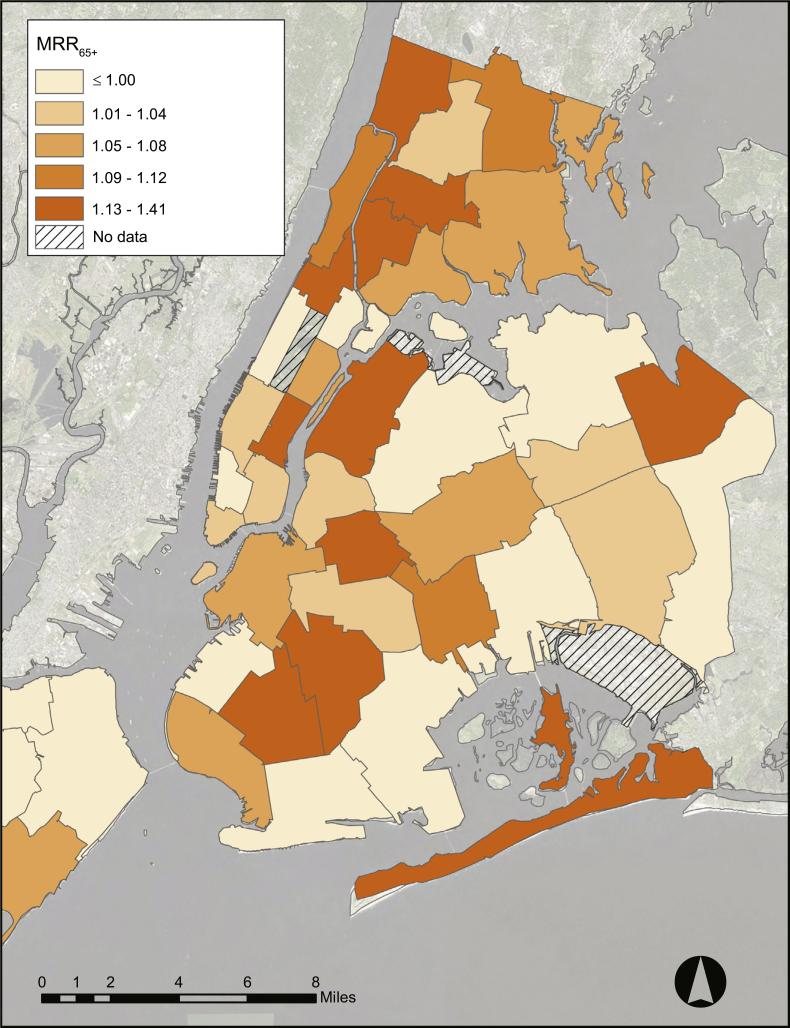
Excess mortality during heat event days was unevenly distributed in New York City's Community Districts and United Hospital Fund (UHF) areas during 1997 through 2006, with higher rates in southern and western parts of the Bronx, northern Manhattan, central Brooklyn and the eastern side of midtown Manhattan (Figs. 1 and 2).
Fig. 1.
Mortality Rate Ratios for seniors age 65 and older (MRR65+) by New York City Community District (n=59). The MRR65+ compares mortality rates during very hot days (maximum heat index=100 °F+) to all May through September days, 1997–2006.
Fig. 2.
Mortality Rate Ratios for seniors age 65 and older (MRR65+) by New York City United Hospital Fund (UHF) neighborhoods (n=42). The MRR65+ shows excess mortality during very hot days (maximum heat index=100 °F+) compared to all May through September days, 1997–2006.
Significant positive associations (p<0.05) were found between heat-mortality rates and neighborhood-level measures of poor housing conditions, poverty, impervious land cover, seniors’ hypertension and the surface temperatures aggregated to the UHF-area level during the warm season (Tables 1, 2 and 4). The rates of owner-occupied housing units and the percent of homes near structures rated good or excellent had the strongest negative associations with the mortality rate ratios, followed by the prevalence of residential air conditioning access and percent Asian population. The negative association between UHF area-based home-ownership rates and the mortality rate ratio was the strongest identified in the study (β=−0.413; p=0.007). Several measures of housing quality were significantly correlated with the mortality rate ratios (MRR65+), including rates of serious housing violations, property tax delinquencies, and deteriorating and dilapidated buildings, suggesting that the quality of seniors’ housing is a population-level risk factor for heat-associated mortality (Table 2).
However, bivariate regression with the mortality rate ratios stratified by poverty rates or income levels resulted in correlations with the vulnerability predictors (e.g., air conditioning access, low educational attainment, surface temperatures and property tax delinquencies) only for the set of neighborhoods with high poverty rates, but not for neighborhoods with relatively low poverty. For example, a negative correlation between the prevalence of air conditioning access and the MRR65+ exists for high-poverty neighborhoods (Pearson's r=−0.317 and p=0.20; n=18), but for low-poverty neighborhoods (Pearson r=0.001 and p0.97; n=24). These differential trends in “high-poverty” versus “low-poverty” neighborhoods were evident for a range of vulnerability predictors. While the small sample size of the stratified analyses reduces the power of these tests, which do not achieve statistical significance at p<0.05, the stratified analyses strongly suggest that poverty rates and income levels act as effect modifiers for the ecological relationship between neighborhood characteristics and higher rates of heat-mortality in New York City. This effect modification reflects the social stratification often seen in natural disasters, where risk, resilience and vulnerability are not evenly distributed within cities, but rather follow the “pre-existing systems of stratification” (Fothergill and Peek, 2004, p. 89).
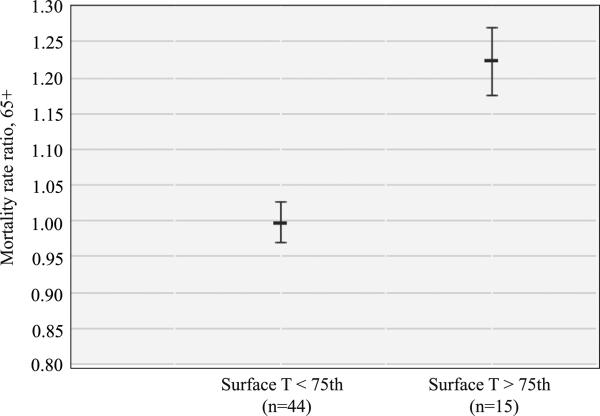
The lowest-income Community Districts and UHF-areas had a trend towards higher heat-associated mortality rates (Table 5). Low-income areas also had a general trend towards hotter surface temperatures and a lower degree of air conditioning access for senior citizens (Table 6).4 The hottest Community Districts and UHF-areas generally had higher mortality rate ratios (Fig. 3); there was a strongly significant (p<0.0001) difference between the mean mortality rate ratio for the quartile of Community Districts (n=15) with the highest surface temperatures (MRR65+ 1.223, SD=0.082) and the mean mortality rate ratio in the 44 “cooler” Community Districts (MRR65+=0.998, SD=0.095).5
Table 5.
Average mortality rate ratios (MRR65+) by poverty ranking for NYC Community Districts (CDs).
| Group by poverty | Mean population | Percent age 65+ (mean) | Percent below 1999 poverty level(mean) | Median household income | MRR65+ (mean) | SD (mean MRR65+) |
|---|---|---|---|---|---|---|
| 20 least impoverished CDs | 140,133 | 13.13 | 10.57 | $55,683 | 1.026 | 0.111 |
| 20 median CDs | 142,445 | 11.97 | 20.39 | $37,010 | 1.0319 | 0.092 |
| 19 most impoverished CDs | 123,876 | 9.18 | 36.89 | $22,645 | 1.1104 | 0.172 |
| All CD average | 135,681 | 11 | 22.38 | $38,714 | 1.0552 | 0.134 |
Fig. 3.
Mean Community District (CD) mortality rate ratios (MRR65+), stratified by the 75th percentile daytime surface temperature (August 14, 2002), with 95% CIs (n=59). Landsat-derived surface temperatures were averaged to the CD-level. The mean MRR65+ for the hottest quartile of CDs (Surface Temperature >75th)=1.223; the mean MRR65+ for the relatively cooler 44 CDs (Surface Temperature<75th)=0.998.
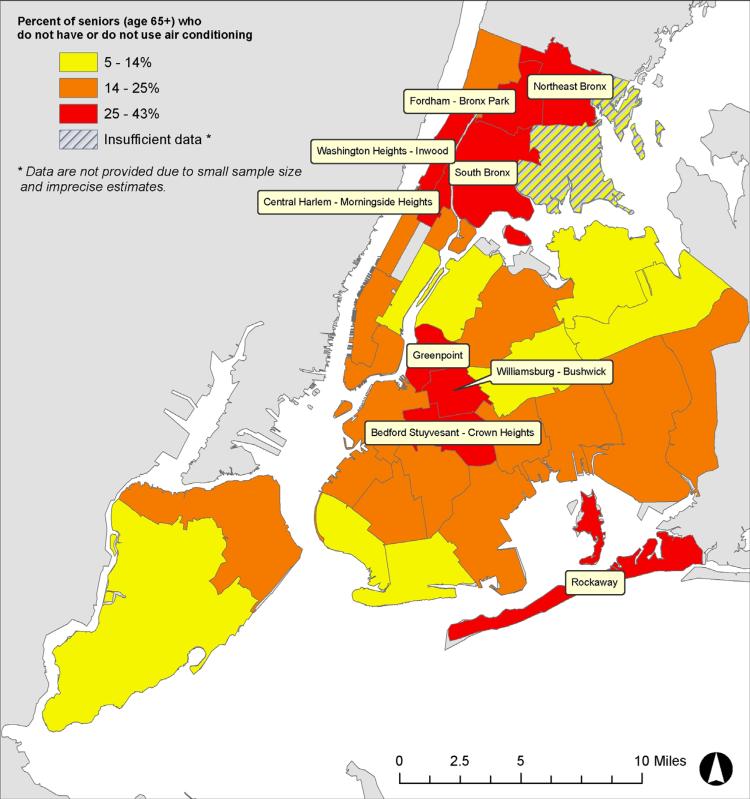
In multivariate spatial regression, elevated surface temperatures in NYC were significantly and positively associated with impervious cover, poverty rates and percent Black/African American, and significantly and negatively associated with percent vegetative land cover, percent White and mean household income. Disparities in the prevalence of air conditioning ownership and use in United Hospital Fund (UHF) areas among seniors aged 65 years and older were found, with nine UHF areas in which over 25% of the senior citizens were not protected by air conditioning during the warm season in 2007 (Fig. 4). Percent Black/African American and percent poverty by UHF area were strong negative predictors of seniors’ air conditioning access in multivariate regression (Table 6). There was a trend for an increasing mortality rate ratio for areas with the least proportion of White population. Percent of seniors living alone was not significantly correlated with increasing mortality rate ratios in New York City neighborhoods, although this was found to be a risk factor in earlier studies of high mortality events such as the Chicago 1995 heat wave (Semenza et al., 1996).
Fig. 4.
Air-conditioning ownership and use by United Hospital Fund neighborhoods, data from the 2007 NYCDOHMH Community Health Survey (n=42).
We used GeoDa software to test for the presence of spatial dependence and spatial autocorrelation in all significant (p<0.05) models. GeoDa is an open source software program that provides spatial data analysis, including spatial autocorrelation statistics and spatial regression functions (Anselin et al., 2005). The residuals for each OLS model were examined with Global Moran's I, the Lagrange Multiplier (LM, lag and error) and the Robust LM lag and error tests with the queens contiguity weights matrix. We used this weights matrix to assess spatial autocorrelation and dependence as it is contiguity-based and thus provides a logical approach for considering the effects that area-based characteristics such as poor housing conditions or land cover might have on their surrounding locations.
No spatial autocorrelation was observed in the mortality rate ratio models (Table 4) and two of the air conditioning (AC) access models (Table 6). However, one of the AC access models and all of the surface temperature models were significantly autocorrelated and required use of spatial lag or spatial error regression. All but one of the surface temperature models required a spatial error model, which is appropriate as a finding of spatial error can be an indication that relevant processes may be occurring at different scales as well as signifying spatially autocorrelated residuals (Table 7). This is obviously true in our use of remotely-sensed surface temperatures averaged to the neighborhood-scale in New York City, as microclimates are influenced by land cover and dimensions of the built environment at finer scales. Use of the spatial error and spatial lag regression improved the fit of the models in all measures; improving the significance of independent variables, increasing R-squared (a pseudo-R2 in spatial regression) and the log-likelihood, and decreasing the Akaike info criterion (AIC) and Schwarz criterion relative to the OLS regression.
5. Discussion
Measures of housing quality that can also be interpreted as indicators of socioeconomic status (SES) – homeownership rates, air conditioning access, proportion of dilapidated and deteriorating residential buildings, property tax delinquency and serious housing violations rates – provided the strongest correlations to the area-based mortality rate ratios. These findings reaffirm prior research that highlights the quality of the neighborhood built environment and social determinants as relevant for heat-associated mortality risk. They provide evidence for the utility of NYC's program to provide air conditioners to low-income seniors, and raise questions about how planners may address the role of poor housing quality and concentrated poverty in creating vulnerability to heat-associated mortality.
The proportion of owner-occupied housing units by UHF area has the strongest association with the MRR65+, which may be an indicator of the stronger community ties, stability and the array of resources and capacity typically associated with homeownership and possessed by homeowners (Dietz and Haurin, 2003). Neighborhoods with higher rates of homeownership may have a buffering, protective effect on the risk of heat-associated mortality due to their positive community externalities. Prior research has found areas with high degrees of homeowners to typically be associated with stronger locally-based social networks, greater involvement in local community, lengthier resident tenure, and familiarity with a great number of neighbors—all factors supported by prior research as potentially protective against adverse heat-health outcomes (Dietz and Haurin, 2003; Kawachi and Berkman, 2003).
The metrics of property tax delinquencies and housing violations are worth examining for what they might reveal about how the quality of the built environment may create higher risk for seniors. The highest correlation values at the CD-scale are rates of property tax delinquencies in Class 1 properties, which are primarily smaller residential buildings: one-, two- and three-family homes and condos of three stories or less. Property tax delinquencies, generally a warning sign of foreclosures, may be seen as a measure of neighborhood stability and economic stress that may result in declining building conditions. Similarly, the rate of housing violations in a neighborhood describes the quality of housing and the physical environment and may be a metric relevant to climate-health outcomes (Klinenberg, 2002). These findings are notable given the recent economic recession. Housing foreclosures increased in New York City during the 2000s, especially following 2007, affecting minority (over 50% Black and Hispanic) and low-income neighborhoods in Queens and Brooklyn more than others (Chan et al., 2013). The city's goals for the creation of new affordable housing units were not met during the study period (1997–2006) and in subsequent years through the Bloomberg mayoralty, and reflecting the national economic downturn post-2008, rates of homelessness in the city rose by over 30% (Bosman, 2010; Brash, 2011; Gross, 2009).
This suggests that health burdens resulting from housing foreclosures and economic recession may include increased vulnerability to heat-related morbidity and mortality for affected communities, as increased housing instability creates greater stress in the physical and social environment for individuals and disrupts neighborhood-based social networks and norms. It also suggests that the development of urban climate adaptation programs should explicitly consider means for addressing housing inadequacies and instability in their planning. Beyond New York City, research on intra-urban differences in climate-health outcomes may be especially relevant in the context of the increasing spatial concentration of poverty and substandard housing conditions related to a weak economy and income inequality. A growing body of scholarship documenting the relationships between measures of the built environment, particularly housing, socioeconomic and racial disparities, and intra-urban variability in heat exposure as risk factors for heat-health impacts (Harlan et al., 2013; Uejio et al., 2011) highlights the importance of the social justice dimensions of urban planning for climate adaptation. We discuss these issues of housing quality, place and risk further below.
The positive correlation between increasing surface temperatures and heat-mortality rates for the lower-income Community Districts and UHF-areas suggests that hot spots of summertime surface temperatures increase the risk of heat-associated mortality in New York City, especially in poorer neighborhoods. Further research should incorporate methods, such as case-control studies, that can consider the effect of microclimates at the individual building scale and block-group level that may be more relevant to individual exposures.
The surface urban heat island is influenced by land cover, including the percent of tree coverage and impervious cover. Previous research has shown both surface and ambient air temperatures to be related to tree coverage, total vegetative cover, the albedo (or reflectivity) of surfaces, and impervious land cover (Slosberg et al., 2006). The multivariate model (Table 4) includes percent impervious cover as a neighborhood-level predictor of increased heat-mortality rates (p<0.10), suggesting that the City's programs to increase vegetative cover – through forestry (Million-Trees), Greenstreets and green infrastructure, vegetated swales, and green roof incentives – may help to create a more healthful environment.
Our analysis was informed by conceptual frameworks that describe how interactions between different levels of social structures – from the individual, to the family, to the neighborhood context and the macro-level characteristics of the political economy – may express the impacts of place on health (Morello-Frosch and Shenassa, 2006; Clougherty and Kubzansky, 2009; Link and Phelan, 1995; Phelan et al., 2004). To interpret regression results for predictors of increased mortality rates and environmental exposures such as surface temperatures we sought insights from the literature on health disparities and urban environmental history.
Low-income and communities of color have borne a disproportionate exposure to pollutants and facilities with hazardous emissions, while often also sharing in fewer of the amenities such as parks and recreational space (Maantay, 2001; Sze, 2007). We found that at all scales examined, surface temperatures are significantly negatively associated with household income, so that higher-income neighborhoods tend to have cooler mean surface temperatures, with hotter daytime surface temperatures found in neighborhoods or census tracts with higher rates of poverty. Racial/ethnic variables (percent non-White and Black/African American) are included in this research as predictors in multivariate spatial models of the surface urban heat island effect. District-level poverty rates were significant predictors of higher surface temperatures during a heat wave (Table 7); additional predictors include percent impervious land-cover and percent Black/African American, while percent White of total population, mean household income and percent vegetated land cover were significant negative predictors of higher surface temperatures. The predictive ability of these variables in these models is interpreted as a representation of how decades of economic and housing development, frequently discriminatory, manifest in the array of land-use, land cover and urban design factors that influence the physical phenomenon of the urban heat island (e.g., see Schill, 1995). In effect, these racial/ethnic variables may act as an index variable in these models, measuring the ways in which the social processes that sort out neighborhoods socially intersect with the characteristics of the built environment. The associations between socioeconomic status, race/ethnicity and demographics with the intra-urban variability of temperatures reflects an emergent form of spatial inequality in regards to climate risks—the environmental exposures and adverse impacts of extreme weather events and climate change. Excess heat is conceptualized as an unevenly distributed urban pollutant that may be relatively higher in minority and low-income neighborhoods due to the design and maintenance of the built environment and housing conditions. This is consistent with the literature on heat-health impacts discussed earlier that found greater exposures and impacts for residents of low-income neighborhoods and communities of color.
New York City has a long history of providing “cooling” to low-income residents to ameliorate the harsh impacts of extreme heat. The distribution of cooling to the poor as a health strategy started during a 10-day heat wave in 1896, an innovation personally organized by Theodore Roosevelt, then president of the Board of Police Commissioners, who convinced the city to purchase and distribute 350 t of ice to low-income New Yorkers during the 1896 heat wave (Kohn, 2008, p. 11). Subsequently, the city opened “ice stations” for the poor in 1919. A modern form of this cooling initiative continues today in the city's distribution of free air conditioners to low-income senior citizens, one of several programs of the NYCDOHMH to prevent heat-associated morbidity and mortality. New York State (NYS) also has a program6 that purchases and installs air conditioners or fans for eligible low-income households with individuals susceptible to extreme heat.
However, the use of home air conditioning (AC) during heat events is limited by concern over the expense of electricity bills for some. Respondents for a recent survey of New Yorkers considered most vulnerable to heat-health impacts7 reported several barriers to their use of AC during hot weather; 54% without an AC said that they could not afford AC (95% CI; 37, 69), and of those that reported never or infrequently using AC, 12% were concerned about their electricity bill (95% CI; 5, 26) (Lane et al., 2013, p. 6).
Given the evidence that some seniors feel they cannot afford the use of air conditioning, even if they own one, examining the benefits and costs of reduced-electricity rates for low-income seniors may be a timely avenue of policy research. Although a review of this subject is beyond the scope of this analysis, our preliminary research indicates that the resources available for energy assistance to low-income seniors in NYC is limited, and many households fall into the gaps between the modest and short-term programs that do exist. New York State does not require regulated investor-owned electric utilities to provide reduced-cost electricity rates to low-income seniors, such as those provided by Massachusetts’ Energy & Utility Assistance Programs (MassResources.org, 2014). Such “lifeline” rate programs may assist residents with long-term income instability and provide protection against heat-health impacts to vulnerable populations. As required by the MA Department of Public Utilities, the benefit for qualified low-income residential customers is a 25% discount based on the total charges in their monthly electricity bill, including supply, delivery and all charges (National Grid, 2014). In light of the increasing importance of policies for carbon mitigation, design and efficiency interventions that might accompany energy assistance for low-income seniors should be investigated as concurrent approaches. Initiatives like the Philadelphia Energy Coordinating Agency's weatherization programs, which provide cool roof coatings, insulation, ceiling fans, energy efficient appliances and other environmental benefits for the homes of low-income seniors as well as job training for developing low-income energy service delivery, are good models that integrate climate adaptation and mitigation for multiple benefits.
5.1. Housing and the spatial concentration of risk
Given these results, we asked how housing quality and its distribution in NYC's diverse neighborhoods intersected with the spatial concentration of seniors. Areas with higher rates of poor quality housing (e.g., increased violations or property tax delinquencies) had significant positive associations with higher mortality rates; neighborhoods with indicators of better quality housing (e.g., buildings rated good or excellent, rates of homeowners) had significant negative associations with higher mortality rates (Table 4). These data suggests that housing quality is one of the salient characteristics through which poverty fosters risk of heat-related mortality. In this interpretation, the characteristics of housing and the built environment may amplify or buffer the risk of heat-related health impacts. More generally, housing conditions are a locus and expression of population vulnerability during extreme heat events, and housing quality a substrate through which poverty influences risk for seniors during conditions of environmental extremes. Health disparities arise in part due to the differential access to options for quality housing that higher income provides and low-income limits (Bashir, 2002).
The analysis of housing affordability and assistance in NYC reveals “a rich, complex neighborhood topography of poverty, wealth, and housing subsidy that defies the simplistic stereotypes of policy and popular discourse” (Wyly and DeFilippis, 2010, p. 2). Given the long-history and complexity of these issues, we limit our discussion here to a few key points about rent-regulated apartments, the rising concentration of immigrant seniors, the geography of Naturally Occurring Retirement Communities (NORCs), and concerns for the future in light of present trends.
According to the NYC Rent Guidelines Board, “available rental housing in NYC falls into three main categories”: market-rate housing, rent regulated housing (rent controlled or rent stabilized), and subsidized housing (public housing and “Section 8” with voucher assistance for rent in private housing)8 (New York City Rent Guidelines Board (NYCRGB), 2014). Roughly one-half of the city's total rental housing stock is rent-regulated units, with rent-stabilized units being the greatest share compared to the relatively small number of rent-controlled units (Furman Center, 2012). In 2011, rent-stabilized units were 45.4% of all rental units, while only 1.8% of units were rent-controlled (Ibid). Rent-stabilization is intended to provide certain protections to tenants, in addition to regulated annual rent increases, including the right to renew one's lease, requirements for building services and succession rights for family members and partners (New York City Rent Guidelines Board (NYCRGB), 2014).
To understand the uneven spatial distribution of elevated mortality rates, we considered the location of rent-regulated apartments. The percent of housing stock that is rent-stabilized units had a positive (p<0.10) correlation with the mortality rate ratio. The seven neighborhoods with the city's highest proportion of regulated to total rental units (>50% in 2011) had a mean mortality rate ratio of 1.112 (SD=0.083). Although this was not significantly different (p=0.19; 95% CI, 1.028, 1.195) than the mean mortality rate ratio for all CDs (1.055), it raises questions about the conditions in rent-stabilized housing for low-income seniors in neighborhoods where they are concentrated.
The percent of housing units that are public housing by Community District had no association with the mortality rate ratio (Pearson's r=0.086, p=0.52). This lack of correlation should be interpreted with caution; it may be due to a true lack of association, or because spatial disaggregation to the census tractor individual level is necessary for a robust evaluation of the links between risk of heat-related mortality with residence in public housing. Higher prevalence of asthma in children was reported in NYC public housing compared to a range of housing types in studies at the census tract and individual-level (Corburn et al., 2006; Northridge et al., 2010). Public officials and non-profit organizations described a range of maintenance deficiencies within NYC public housing following our study period and delays in addressing housing repairs for mold, moisture and infestations of cockroaches and mice, as well as long waits for structural and appliance repairs, including air conditioners (De Blasio, 2013; Natural Resources Defense Council (NRDC), 2013), although data on the rates of these problems were lacking. The two public housing developments with the City's most delayed repairs, the Woodside Houses in Queens and Melrose Houses in the Bronx, are located in Community Districts above the median mortality rate ratio (1.063) and over one SD above the mean (MRR65+ >1.098) (De Blasio, 2013). With a largely low-income resident population – about 60% of residents are 30% or less of the city's median income – a finer-scale analysis of the relationship of public housing quality to heat-mortality vulnerability is recommended.
A demographic trend of note since 2000 is the increase in senior immigrants. Roughly one-half (46%) of NYC's seniors in 2013 were immigrants (Center for an Urban Future, 2013). Often linguistically isolated, this group is growing in size and proportion faster than native-born seniors and is potentially vulnerable due to cultural barriers, more limited access to support services, limited English proficiency, and limited retirement savings and use of Social Security compared to other seniors (Center for an Urban Future, 2013, p. 3–5). Three of the four communities with both the city's highest rates of rent-regulated apartments and high mortality rate ratios (MRR65+ >1.10) also had above-average rates of foreign-born seniors; these were Washington Heights/Inwood, Manhattan (79% of seniors foreign-born, 9% of total population; 86.7% rental units regulated), University Heights/Fordham, The Bronx (55% of seniors foreign-born, 3% of total population; 75.7% of rental units regulated), and Astoria, Queens (63% of seniors foreign-born, 7% of total population; 53% of rental units regulated) (Furman Center, 2012; Center for an Urban Future, 2013). However, across the city, there was no correlation between the percent of households that speak a language other than English at home (by Community District, Census 2000) and the mortality rate ratio (Pearson's r=0.000).
Finally, we were also interested in assessing the geography of naturally occurring retirement communities, or NORCs, in NYC. NORCs are neighborhoods or housing developments where seniors represent a substantial proportion of the residents, in buildings not originally designed for older persons (see the New York State Office of the Aging for specific thresholds; often building-based NORCs are defined as having at least 50% of units with a senior occupant). NORCs are a nationally recognized urban phenomenon related to concentrated “aging in place” – older adults who remain in their home for a long tenure rather than leave them for retirement communities or assisted living – or they may also develop due to the arrival of older adults or the departure of young people (Vladeck and Segel, 2010, p. 1–2). Both NYS and NYC developed supportive service programs in NORC areas to assist seniors who remained living at home. New York City had 43 NORC supportive service programs in 2010 (NORC-SSP); all received some form of public funding (Ibid, p. 3). The majority of these programs were city-funded (34) and located in public and private housing developments (32); only two city-funded programs were neighborhood-based.
Our qualitative, visual assessment of these geographies using maps of NORC developments could not discern any association between the areas of elevated heat-mortality rates and the location of NORC developments in NYC (Armborst et al., 2010). With the majority of NYC NORCs in housing developments, this may be that they are small proportions of each area's population, or it may relate to the availability of supportive services in many NORC developments. According to the NYC Department for the Aging, residents of the City's housing development-based NORCs “can access health and social services right in their own building or building complex” (New York City Department for the Aging (NYCDFA), 2014). Health analysts hope that further developing neighborhood-based NORCs may hold the potential to integrate the range of housing, health and social services that can aid older New Yorkers in successful aging in place (Vladeck and Segel, 2010).
The trends for the future are concerning. As the large baby boomer cohort ages, NYC experienced a dramatic increase in its older population of 60 years and over between 2000 and 2010, increasing to over 17% of the population (New York City Department for the Aging (NYCDFA), 2012). The proportion of those aged 65 years and over in the city is projected to expand rapidly by 2030, to over 1.35 million (NYC Department of City Planning (NYCDCP), 2006).
However, for the past decade at least, there has been a chronic and severe shortage of affordable housing in NYC in general, and in particular for seniors (Gotbaum, 2008; Lui, 2013). The discourse of crisis is often used in discussions of the availability of affordable housing for low-income seniors in NYC (Wyly and DeFilippis, 2010). Policies to provide affordable housing opportunities to this group have fallen far short of need since the 1990s. Waiting lists for public housing or other forms of subsidized housing are long, if open at all, in NYC; it can take many years for those on the list to be placed. For some forms of housing subsidies, even those that receive them have no guarantee that the benefit will translate into an ability to secure adequate housing (as, for example, many landlords refuse to accept vouchers that subsidize rent) (DeFilippis and Wyly, 2008).9 A recent (April 2014) New York Times article on housing insecurity of seniors reported “About 51% of renter households led by an older New Yorker pay at least 35% of their income in rent, or above what the federal government considers affordable, making residents 65 and over among the most rent burdened in the city” (Navarro and Yee, 2014). With housing insecurity on the rise since the 2008 recession for low-income New Yorkers, there is concern about the potential for an increase in homelessness among senior citizens, along with continued housing inadequacy (Lui, 2013). Seen in this NYC context, it is not unusual to find that measures of housing quality are consistently significant in association with the area-based mortality rate ratios.
6. Limitations
These findings reflect the limits of an ecologic analysis: the presence or absence of a linear relationship between neighborhood-level characteristics and mortality rates does not imply that such a relationship necessarily will or will not exist at the individual level. Disaggregating data at the intra-urban level alleviates some concerns regarding ecologic bias. Limitations of this analysis include:
Mortality has an association with warm weather at a range of temperatures in New York City, and heat-related mortality occurs on days below the Heat Advisory threshold of Heat Index >100 °F (Curriero et al., 2002; Metzger et al., 2010). Therefore the mortality rate ratios MRR65+ do not represent the full range of heat-associated mortality that actually occurred during the study period, and it is possible that the magnitude of associations with neighborhood characteristics would change with use of a more inclusive exposure metric. Similarly, although seniors are at greatest risk, heat-associated mortality occurs in NYC at ages below 65 years, and factoring in all age groups might influence these findings (New York City Department of Health and Mental Hygiene (NYCDOHMH), 2006).
The health outcome measure, MRR65+, is based on the same-day heat index (HI), which has a linear association with daily mortality in New York City (Metzger et al., 2010). However, heat-related mortality in the city is best predicted by a nonlinear association that incorporates the previous 2-day temperature and the same-day heat index (Metzger et al., 2010). Future research may use additional modeling methods to evaluate community characteristics using a lag time with same day and previous 1-and 2-day temperature as a predictor. It may be useful to examine excess mortality using different heat exposure periods (e.g., during heat waves rather than HI ≥100 °F) and more complex spatially-stratified time series models.
Near-surface air temperature measurements would likely provide a more health-relevant measure of the urban heat island's spatial variability, but were not available across the city at the spatial resolution necessary for this analysis. As well, daily variations in ozone and fine particulate matter (PM10 and 2.5) are associated with daily mortality in cities (Kinney, 1999; Koken et al., 2003; Thurston and Ito, 1999). Ozone is a photochemical pollutant whose formation from precursor emissions is accelerated during hot and sunny days. This research did not control for air quality during heat events.
The administrative boundaries of CDs and UHF define different areas, and associations between the same independent variables (e.g., owner occupied housing units) with the health outcome metric are not identical. There was, however, no reversal of trend at these two spatial scales; correlations at the UHF and CD-scale agree in the direction of association and are generally in the same range, but differ in magnitude. The differences correspond to the expectations of the modifiable area unit problem (MAUP)'s general influence on statistical results—that larger sized areas tend to have a greater correlation when used in regression analysis. This methodological concern could be alleviated by the use of multi-level studies that incorporate individual and household-level data to test neighborhood effects (Subramanian et al., 2009).
The multivariate models that achieved statistical significance were limited due to the multicollinearity of independent variables.
Finally, there is possible but unknown instability in the data due to the limited number of days with the Heat Index equal to or above 100 °F during the study period.
Despite the limitations noted above, these findings affirm the importance of neighborhood characteristics and social determinants in targeting heat illness prevention and emergency response activities. The findings suggest that planning and design strategies for urban heat island mitigation should target resources to improve conditions in lower-income areas and residences, and incorporate local data on neighborhood vulnerability to reduce health impacts of extreme heat.
7. Conclusions
Within the city, different neighborhoods experienced differential rates of excess heat-related mortality, and this variation was correlated with neighborhood factors including rates of poverty, air conditioning access, educational attainment, housing quality, rates of home ownership, land cover and land surface temperatures. These findings suggest that low-income neighborhoods should be targeted in the city's climate adaptation planning, and that disparities in access to residential air conditioning are associated with heat-related mortality rates, as are metrics of neighborhood stability, economic hardship, and building conditions in New York City neighborhoods.
Programs that provide access to cooling for seniors during extreme hot weather, for example, through cooling centers and air-conditioned public spaces are widely acknowledged as protective interventions. Given the importance of access to cooling during periods of extreme heat, further research on the spatial distribution and use of cool spaces within neighborhoods – including parks, air conditioned stores, public buildings and pools – may help identify and characterize resources for seniors able to leave their homes. Our results suggest that research on the effects of residential building design on indoor temperatures and building thermal performance is important to inform adaptive planning, even while outreach and prevention measures such as home air conditioner distribution for low-income seniors will continue to be needed for an increasing elderly NYC population.
Policies to improve the housing conditions of elderly residents could play a role in reducing heat-related mortality in New York City, although these policies are not yet explicitly considered as part of climate adaptive planning. Climate adaptation and heat island mitigation programs that seek to identify neighborhood hot spots within cities and address economic disparities may help to reduce the health impacts of climate extremes and variability. Towards that end, a community-based adaptation planning process may help address the social justice dimension of the impacts of extreme events and climate change in New York City while increasing the effectiveness of adaptive programs and policies.
Acknowledgments
A portion of this research was supported under a cooperative agreement from the Centers for Disease Control and Prevention (CDC) through the Association of Schools of Public Health (ASPH) Grant Number CD300430, a grant from the CDC through the TKC Integration Services, LLC, and an internship with the New York City Department of Health and Mental Hygiene (DOHMH). The contents are solely the responsibility of the authors and do not necessarily represent the official views of DOHMH, CDC, or any government agency. We thank Thomas Matte of DOHMH for his input during the research and comments on earlier versions of the manuscript, and Grant Pezeshki and Sarah Johnson of DOHMH for their expert advice on mapping and data; Erica Blonde of the Harvard University Graduate School of Design (GSD) for comments on the manuscript, research assistance and help with revisions; Meg Howard for mapping assistance; Sumeeta Srinivasan of the Center for Geographic Analysis at Harvard University for advice on spatial analysis; and Elliott Sclar of Columbia University for insightful comments on the research. We gratefully acknowledge the anonymous reviewers of the manuscript for their feedback and valuable input.
Abbreviations
- CD
community district
- heat wave
three or more consecutive days of equal to or greater than 90°F maximum temperatures
- HI
the heat index (HI), or apparent temperature: a measure that combines relative humidity and ambient temperature (Steadman, 1979)
- MRR65+
mortality rate ratio of persons aged 65 and older
- UHF
United Hospital Fund
- UHI
urban heat island
Footnotes
Percent below poverty has a p-value=0.051 for Community Districts.
Air conditioning access is defined as owning and using home air conditioning according to data from the 2007 Community Health Survey (CHS, DOHMH).
The relatively “hotter” and “cooler” Community Districts calculated from the Landsat-derived daytime surface temperatures averaged to the CD-level for August 14, 2002, a heat wave day.
For households that meet certain low-income requirements and other eligibility criteria, the Home Energy Assistance Program's Cooling Assistance Component may purchase and install an air conditioner or fan up to $800. The website notes, however, that the funding for this program is “very limited” and distributed on a first-come first-serve basis (The Home Energy Assistance Program (HEAP), 2014).
Defined as those who “reported not having AC, or using AC either “never” or “less than half the time” and were either 65 years+ or reported “poor” or “fair” health status” (Lane et al., 2013, p. 6).
Other subsidized housing includes Mitchell-Lama housing, and other rental units include In Rem, HUD-regulated, Loft Board regulated units, and Article 4. The NYU Furman Center for Real Estate and Urban Policy's Data Search Tool is a recommended resource for data on housing types and markets.
“In tight housing markets like New York City, a voucher is akin to a hunting license: There is no guarantee that the assistance can actually be used (DeFilippis and Wyly, 2008, p. 784).”
References
- Anselin L, Syabri I, Kho Y. GeoDa: an introduction to spatial data analysis. Geogr. Anal. 2005;38(1):5–22. http://dx.doi.org/10.1111/j.0016-7363.2005.00671.x. [Google Scholar]
- Armborst T, D'Oca D, Theodore G. NORCs in NYC. [9 June 2014];Urban Omnibus. 2010 Retrieved from: 〈 http://urbanomnibus.net/2010/03/norcs-in-nyc/〉.
- Bashir SA. Home is where the harm is: inadequate housing as a public health crisis. Am. J. Public Health. 2002;92(5):733–738. doi: 10.2105/ajph.92.5.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol. Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. http://dx.doi.org/10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- Braga ALF, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect. 2002;110:859–863. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosman J. Number of People Living on New York Streets Soars. New York Times; New York, NY: 2010. [30 July 2012]. 〈 http://www.nytimes.com/2010/03/20/nyregion/20homeless.html〉. [Google Scholar]
- Brash J. Bloomberg's New York: Class and Governance in the Luxury City. Vol. 6. University of Georgia Press; 2011. [Google Scholar]
- Bullard RD. Dumping in Dixie: Race, Class, and Environmental Quality. Westview Press; Boulder, CO.: 1990. [Google Scholar]
- Center for an Urban Future [6 June 2014];The New Face of New York's Seniors. 2013 Retrieved from: 〈 http://nycfuture.org/research/publications/the-new-face-of-new-yorks-seniors〉.
- Centers for Disease Control and Prevention (CDC) MMWR. Vol. 62. U.S. Department of Health and Human Services; Atlanta, GA: 2013. Heat Illness and Deaths— New York City, 2000–2011. pp. 617–621. 2013. [PMC free article] [PubMed] [Google Scholar]
- Chan S, Gedal M, Been V, Haughwout A. The role of neighborhood characteristics in mortgage default risk: evidence from New York City. J. Hous. Econ. 2013;22(2):100–118. http://dx.doi.org/10.1016/j.jhe.2013.03.003. [Google Scholar]
- Clarke JF. Some effects of the urban structure on heat mortality. Environ. Res. 1972;5:93–104. doi: 10.1016/0013-9351(72)90023-0. http://dx.doi.org/10.1016/0013-9351(72)90023-0. [DOI] [PubMed] [Google Scholar]
- Clougherty JE, Kubzansky LD. A framework for examining social stress and susceptibility in air pollution and respiratory health. Environ. Health Perspect. 2009;117(9):1351–1358. doi: 10.1289/ehp.0900612. http://dx.doi.org/10.1289/ehp.0900612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corburn J, Osleeb J, Porter M. Urban asthma and neighborhood environment in New York City. Health Place. 2006;12:167–179. doi: 10.1016/j.healthplace.2004.11.002. http://dx.doi.org/10.1016/j.healthplace.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Curriero FC, Heiner KS, Samet JM, Zeger SL, Strug L, Patz JA. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002;155:80–87. doi: 10.1093/aje/155.1.80. http://dx.doi.org/10.1093/aje/155.1.80. [DOI] [PubMed] [Google Scholar]
- Cutter SL, Emrich CT, Webb JJ, Morath D. Social Vulnerability to Climate Variability Hazards: A Review of the Literature. Final Report to Oxfam America. 2009:1–44. [Google Scholar]
- De Blasio [16 June 2014];Office of the New York City Public Advocate. 2013 Retrieved from: 〈 http://advocate.nyc.gov/sites/advocate.nyc.gov/files/DeBlasio-NYCHA-Repairs-Fact-Sheet.pdf〉.
- DeFilippis J, Wyly E. Running to stand still: through the looking glass with federally subsidized housing in New York City. Urban Aff. Rev. 2008;43(6):777–816. [Google Scholar]
- Dietz RD, Haurin DR. The social and private micro-level consequences of homeownership. J. Urban Econ. 2003;54(3):401–450. http://dx.doi.org/10.1016/S0094-1190(03)00080-9. [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. Am. J. Public Health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. http://dx.doi.org/10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellen IG, Mijanovich T, Dillman KN. Neighborhood effects on health: exploring the links and assessing the evidence. J. Urban Aff. 2001;23(3–4):391–408. http://dx.doi.org/10.1111/0735-2166.00096. [Google Scholar]
- Ellis FP, Nelson F, Pincus L. Mortality during heat waves in New York City July, 1972 and August and September, 1973. Environ. Res. 1975;10:1–13. doi: 10.1016/0013-9351(75)90069-9. http://dx.doi.org/10.1016/0013-9351(75)90069-9. [DOI] [PubMed] [Google Scholar]
- Fothergill A, Peek L. Poverty and disasters in the United States: a review of recent sociological findings. Nat. Hazard. 2004;32(1):89–110. [Google Scholar]
- Furman Center . Rent Stabilization in New York City. The New York University Furman Center for Real Estate and Urban Policy; Apr, 2012. [5 June 2014]. 2012. Retrieved from: 〈 http://furmancenter.org/files/publications/HVS_Rent_Stabilization_fact_sheet_FINAL_4.pdf〉. [Google Scholar]
- Gotbaum B. Sharing Old Age: Alternative Senior Housing Options. Office of the New York City Public Advocate; Mar, 2008. [8 June 2014]. 2008. Retrieved from: 〈 http://www. docstoc.com/docs/119908151/Sharing-Old-Age〉. [Google Scholar]
- Gross C. Affordable Housing Not Included. Gotham Gazette; New York, NY: 2009. [3 June 2014]. Retrieved from: 〈 http://www.gothamgazette.com/article/housing/20091005/10/3045〉. [Google Scholar]
- Harlan SL, Declet-Barreto JH, Stefanov WL, Petitti DB. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ. Health Perspect. 2013;121197(2) doi: 10.1289/ehp.1104625. http://dx.doi.org/10.1289/ehp.1104625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlan SL, Brazel AJ, Prashad L, Stefanov WL, Larsen L. Neighborhood microclimates and vulnerability to heat stress. Soc. Sci. Med. 2006;63:2847–2863. doi: 10.1016/j.socscimed.2006.07.030. http://dx.doi.org/10.1016/j.socscimed.2006.07.030. [DOI] [PubMed] [Google Scholar]
- Hart M, Sailor DJ. Quantifying the influence of land-use and surface characteristics on spatial variability in the urban heat island. J. Theor. Appl. Climatol. 2008;95:397–406. http://dx.doi.org/10.1007/s00704-008-0017-5. [Google Scholar]
- Hoshiko S, English P, Smith D, Trent R. A simple method for estimating excess mortality due to heat waves, as applied to the 2006 California heat wave. Int. J. Public Health. 2010;55:133–137. doi: 10.1007/s00038-009-0060-8. http://dx.doi.org/10.1007/s00038-009-0060-8. [DOI] [PubMed] [Google Scholar]
- Jesdale BM, Morello-Frosch R, Cushing L. The racial/ethnic distribution of heat risk-related land cover in relation to residential segregation. Environ. Health Perspect. 2013;121(7):811–817. doi: 10.1289/ehp.1205919. http://dx.doi.org/10.1289/ehp.1205919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkstein LS, Greene JS. An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ. Health Perspect. 1997;105:84–93. doi: 10.1289/ehp.9710584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney PL. The pulmonary effects of outdoor ozone and particle air pollution. Semin. Respir. Crit. Care Med. 1999;20:601–607. http://dx.doi.org/10.1055/s-2007-1009479. [Google Scholar]
- Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am. J. Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinenberg E. Heat Wave: A Social Autopsy of Disaster. University of Chicago Press; Chicago: 2002. [DOI] [PubMed] [Google Scholar]
- Knowlton K, Lynn B, Goldberg RA, Rosenzweig C, Hogrefe C, Rosenthal JK, Kinney PL. Projecting heat-related mortality impacts under a changing climate in the New York City region. Am. J. Public Health. 2007;97:2028–2034. doi: 10.2105/AJPH.2006.102947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn EP. The Scourge of Summer. 1. Vol. 8. New York Archives Trust; 2008. [6 June 2014]. pp. 8–11. Retrieved from: 〈 http://www.archives.nysed.gov/apt/magazine/archivesmag_summer08.pdf〉. [Google Scholar]
- Koken PJM, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ. Health Perspect. 2003;111(10):1312–1317. doi: 10.1289/ehp.5957. http://dx.doi.org/10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu. Rev. Public Health. 1997;18(1):341–378. doi: 10.1146/annurev.publhealth.18.1.341. http://dx.doi.org/10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Lane K, Wheeler K, Charles-Guzman K, Ahmed M, Blum M, Gregory K, Matte T. Extreme heat awareness and protective behaviors in New York City. J. Urban Health. 2013:1–12. doi: 10.1007/s11524-013-9850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, Horton RM, Kinney PL. Projections of seasonal patterns in temperature-related deaths for Manhattan, New York. [19 May 2013];Nat. Clim. Change. 2013 doi: 10.1038/nclimate1902. http://dx.doi.org/10.1038/NCLIMATE1902. [DOI] [PMC free article] [PubMed]
- Link BG, Phelan JC. Social conditions as fundamental causes of disease. J. Health Soc. Behav. (Extra Issue) 1995:80–94. [PubMed] [Google Scholar]
- Lui J. [6 June 2014];Senior Housing in New York City: The Coming Crisis. Office of the New York City Comptroller. 2013 Retrieved from: 〈 http://comptroller.nyc.gov/wp-content/uploads/documents/NYC_SeniorHousing.pdf〉.
- Maantay J. Zoning, equity and public health. Am. J. Public Health. 2001;91(7):1033–1041. doi: 10.2105/ajph.91.7.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmor M. Heat wave mortality in New York City, 1949–1970. Arch. Environ. Health. 1975;30:130–136. doi: 10.1080/00039896.1975.10666661. [DOI] [PubMed] [Google Scholar]
- MassResources.org [5 June 2014];Massachusetts Energy & Utility Assistance Programs; “Utility and Telephone Discounts.”. 2014 Retrieved from: 〈 http://www.massresources.org/utility-discounts.html〉.
- McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ. Health Perspect. 2001;109(Suppl. 2):185–198. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin Centre for Population Health Risk Assessment [18 May 2014];Glossary. 2012 Retrieved from: 〈 http://www.rfcom.ca/glossary/index.shtml〉.
- Metzger KB, Ito K, Matte TD. Summer heat and mortality in New York City: how hot is too hot? Environ. Health Perspect. 2010;118:80–86. doi: 10.1289/ehp.0900906. http://dx.doi.org/10.1289/ehp.0900906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ. Health Perspect. 2006;114(8) doi: 10.1289/ehp.8930. http://dx.doi.org/10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Grid [5 June 2014];Billing and Rates: Low Income (R-2) Service Rates. 2014 Retrieved from: 〈 http://www.nationalgridus.com/masselectric/home/rates/4_lowincome.asp〉.
- Navarro N, Yee V. Up in Years and All but Priced Out of New York. The New York Times; Apr 29, 2014. [29 April 2014]. Retrieved from: 〈 http://www.nytimes.com/2014/04/30/nyregion/older-new-yorkers-face-acute-pain-in-finding-homes.html〉. [Google Scholar]
- Kawachi I, Berkman L, editors. Neighborhoods and Health. Oxford University Press; New York, NY.: [Google Scholar]
- Northridge M, Stover G, Rosenthal J, Sherard D. Environmental equity and health: understanding complexity and moving forward. Am. J. Public Health. 2003;93(2):209–214. doi: 10.2105/ajph.93.2.209. 10.2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J. Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natural Resources Defense Council (NRDC) [16 June 2014];Rampant Mold & Moisture Problems in NYC Public Housing. 2013 Retrieved from: 〈 http://www.nrdc.org/ej/mold-and-moisture-in-public-housing.asp〉.
- NYC Department of City Planning (NYCDCP) [10 June 2014];New York City Population Projections by Age/Sex & Borough, 2000-2030 Report. 2006 Dec; 2006 Retrieved from: 〈 http://www.nyc.gov/html/dcp/pdf/census/projections_report.pdf〉.
- New York City Department for the Aging (NYCDFA) Census 2010: Changes in the Elderly Population of New York City, 2000 to 2010. Planning Division/ Research Unit. 2012 Jul; 2012. [Google Scholar]
- New York City Department for the Aging (NYCDFA) [22 May 2014];NORC Programs. 2014 Retrieved from: 〈 http://www.nyc.gov/html/dfta/html/services/retirement.shtml〉.
- New York City Department of Health and Mental Hygiene (NYCDOHMH) [2 October 2013];Deaths Associated With Heat Waves in 2006. NYC Vital Signs Investigation Report. 2006 Retrieved from: 〈 http://www.nyc.gov/html/doh/downloads/pdf/survey/survey-2006heatdeaths.pdf〉.
- New York City Department of Health and Mental Hygiene (NYCDOHMH) [20 August 2012];Heat Illness. 2012 Retrieved from: 〈 http://www.nyc.gov/html/doh/html/cd/cdheat-illness-and-waves.shtml〉.
- New York City Rent Guidelines Board (NYCRGB) [10 June 2014];What Type of Housing is Available in the New York City Rental Market? 2014 Retrieved from: 〈 http://www.nycrgb.org/html/guide/basics.html〉.
- O'Neill MS, Ebi KL. Temperature extremes and health: impacts of climate variability and change in the United States. J. Occup. Environ. Med. 2009;51(1):13–25. doi: 10.1097/JOM.0b013e318173e122. http://dx.doi.org/10.1097/JOM.0b013e318173e122. [DOI] [PubMed] [Google Scholar]
- O'Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J. Urban Health. 2005;82:191–197. doi: 10.1093/jurban/jti043. http://dx.doi.org/10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Observatoire régional de santé (ORS) Conséquences sanitaires de la canicule d’août 2003 en Ile-de-France. Paris: 2003. [Google Scholar]
- Patz JA, Campbell-Lendrum D, Holloway T, Foley JA. Impact of regional climate change on human health. Nature. 2005;438:310–317. doi: 10.1038/nature04188. http://dx.doi.org/10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Diez Roux A, Kawachi I, Levin B. “Fundamental causes” of social inequalities in mortality: a test of the theory. J. Health Soc. Behav. 2004;45:265–285. doi: 10.1177/002214650404500303. http://dx.doi.org/10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- Rosenthal JK, Sclar ED, Kinney PL, Knowlton K, Crauderueff R, Brandt-Rauf PW. Links between the built environment, climate and population health: interdisciplinary environmental change research in New York City. Ann. Acad. Med. Singapore. 2007;36:834–846. [PubMed] [Google Scholar]
- Rundle A, Diez Roux AV, Freeman LM, et al. The urban built environment and obesity in New York City: a multilevel analysis. Am. J. Health Promot. 2007;21:326–334. doi: 10.4278/0890-1171-21.4s.326. http://dx.doi.org/10.4278/0890-1171-21.4s.326. [DOI] [PubMed] [Google Scholar]
- Schill MH. Local enforcement of laws prohibiting discrimination in housing: the New York City human rights commission. Fordham Urban Law J. 1995;23:991. [Google Scholar]
- Schwartz S. The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. Am. J. Public Health. 1994;84(5):819–823. doi: 10.2105/ajph.84.5.819. http://dx.doi.org/10.2105/AJPH.84.5.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL, Wilhelm JL. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 1996;335(2):84–90. doi: 10.1056/NEJM199607113350203. http://dx.doi.org/10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Slosberg R, Rosenzweig C, Solecki W. New York City Regional Heat Island Initiative: Mitigating New York City’s Heat Island With Urban Forestry, Living Roofs, and Light Surfaces (Final Report 06-06) New York State Energy and Research Development Authority (NYSERDA); Albany, NY.: 2006. [Google Scholar]
- Smargiassi A, Goldberg MS, Plante C, Fournier M, Baudouin Y, Kosatsky T. Variation of daily warm season mortality as a function of micro-urban heat islands. J. Epidemiol. Community Health. 2009;63(8):659–664. doi: 10.1136/jech.2008.078147. http://dx.doi.org/10.1136/jech.2008.078147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoyer KE. Putting risk in its place: methodological considerations for investigating extreme event health risk. Soc. Sci. Med. 1998;47(11):1809–1824. doi: 10.1016/s0277-9536(98)00237-8. http://dx.doi.org/10.1016/S0277-9536(98)00237-8. [DOI] [PubMed] [Google Scholar]
- Steadman RG. The assessment of sultriness. Part I: A temperature–humidity index based on human physiology and clothing science. J. Appl. Meteorol. 1979;18(7):861–873. http://dx.doi.org/10.1175/1520-0450(1979)018<0861:TAOSPI4>2.0.CO;2. [Google Scholar]
- Subramanian SV, Jones K, Kaddour A, Krieger N. Revisiting Robinson: the perils of individualist and ecologic fallacy. Int. J. Epidemiol. 2009;38:342–360. doi: 10.1093/ije/dyn359. http://dx.doi.org/10.1093/ije/dyn359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susser M. The logic in ecological: I. The logic of analysis. Am. J. Public Health. 1994;84(5):825–829. doi: 10.2105/ajph.84.5.825. http://dx.doi.org/10.2105/AJPH.84.5.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze J. Noxious New York: The Racial Politics of Urban Health and Environmental Justice. MIT Press; 2007. [Google Scholar]
- Thurston GD, Ito K. Epidemiological studies of ozone exposure effects. In: Holgate ST, Samet JM, Koren HS, Maynard RL, editors. Air Pollution and Health. Academic Press; San Diego, CA: 1999. pp. 485–510. [Google Scholar]
- The Home Energy Assistance Program (HEAP) [7 June 2014];Office of Temporary and Disability Assistance, New York State. 2014 Retrieved from: 〈 http://otda.ny.gov/programs/heap/〉.
- Uejio CK, Wilhelmi OV, Golden JS, Mills DM, Gulino SP, Samenow JP. Intra-urban societal vulnerability to extreme heat: the role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health Place. 2011;17(2):498–507. doi: 10.1016/j.healthplace.2010.12.005. http://dx.doi.org/10.1016/j.healthplace.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Vladeck F, Segel R. Identifying risks to healthy aging in New York City’s varied NORCs. J. Hous. Elderly. 2010;24(3–4):356–372. [Google Scholar]
- Wyly E, DeFilippis J. Mapping public housing: the case of New York City. City Community. 2010;9(1):61–86. [Google Scholar]